Abstract
Valgus malalignment can be corrected with a biplanar lateral opening wedge distal femoral osteotomy (bLOWDFO) in patients with symptomatic lateral compartment disease. Advantages of a lateral opening wedge technique over the medial closing wedge technique include avoidance of vascular structures and theoretically better control of the amount of correction. The advantages of a bLOWDFO over a uniplanar osteotomy are that it creates a larger surface area for healing, and provides inherent stability to control the osteotomy intraoperatively. The purpose of this article is to present a reproducible technique for bLOWDFO and review the indications, preoperative planning, rationale, and clinical outcomes.
Coronal plane malalignment has been treated by osteotomies about the knee for many years.1 More recently, advances in cartilage restoration and meniscal transplant procedures have led to further increased interest in malalignment correction. Appropriate mechanical alignment has been shown to be an important factor in the success of these operations.2
Several techniques have been described for correction of valgus malalignment, including distal femoral and proximal tibial osteotomies with a lateral opening wedge or medial closing wedge. In patients with moderate to severe valgus alignment and lateral compartment arthritis, meniscal deficiency, or focal osteochondral defects our preference is to perform a biplanar lateral opening wedge distal femoral osteotomy (bLOWDFO) to increase healing surface area and mechanical stability. The purpose of this article is to present a reproducible technique for bLOWDFO and review the indications, preoperative planning, rationale, and clinical outcomes.
Surgical Indications and Contraindications
Proper patient selection is paramount for the success of this operation. The primary indications for this procedure are patients with valgus malalignment (up to 12°) with a previous injury to the lateral compartment cartilage or meniscus or lateral compartment arthritis. Frequently, patients have undergone prior surgical procedures including partial lateral meniscectomy, chondroplasty, or other cartilage procedures in the lateral compartment. The bLOWDFO may also be used as an adjunct procedure in patients undergoing concomitant lateral meniscus allograft transplantation or lateral compartment cartilage repair procedures. Absolute contraindications for bLOWDFO include symptomatic medial compartment disease, inflammatory arthritis, severe ligamentous laxity, or joint subluxation greater than 1 cm. Relative contraindications include obesity (body mass index >35), age >60 years, moderate to severe patellofemoral disease, and nicotine use.3
Preoperative Planning
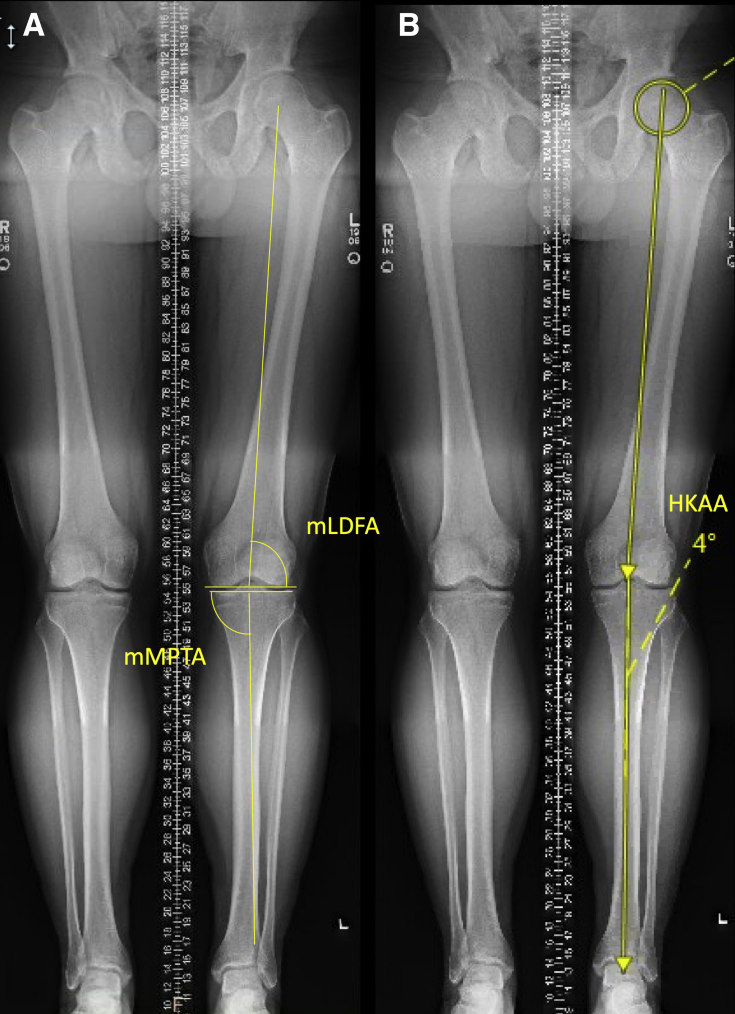
The mechanical axis or hip-knee-ankle angle of the lower limb is measured on full-length bilateral weightbearing radiographs and used to measure the coronal plane deformity (Fig 1). Additionally, the mechanical medial proximal tibia articular angle and mechanical lateral distal femur articular angle are calculated as the angle formed between the mechanical axis of the tibia and tibial plateau, and the mechanical axis of the femur and distal articular angle of the femur respectively (Fig 1). Most often, magnetic resonance imaging scans have been obtained before surgical consultation. Magnetic resonance imaging is not critical unless one is looking to evaluate other potential intra-articular pathology or to use the study to assess the articular cartilage of the medial and patellofemoral compartments.
Fig 1.
Full-length standing anteroposterior radiographs with measurements of the left lower extremity demonstrating (A) the mechanical lateral distal femoral angle (mLDFA) and mechanical medial proximal tibial angle (mMPTA) and (B) measurement of hip-knee-ankle angle (HKAA) with planned 4° correction to the medial tibial spine.
Surgical correction is calculated using the hip-knee-ankle angle (Fig 2). In general, the correction is planned to bring the mechanical axis to the center of the knee joint to create a neutral alignment. In cases of more severe lateral compartment disease, correction to the medial tibial spine may be preferred. The calculated angle of correction is then transposed to the distal femur at the desired level of the osteotomy cut. The trajectory of the primary cut is from just proximal to the lateral metaphyseal flare toward a point about 1 cm medial to the adductor tubercle to preserve a medial “hinge” (Fig 2).
Fig 2.
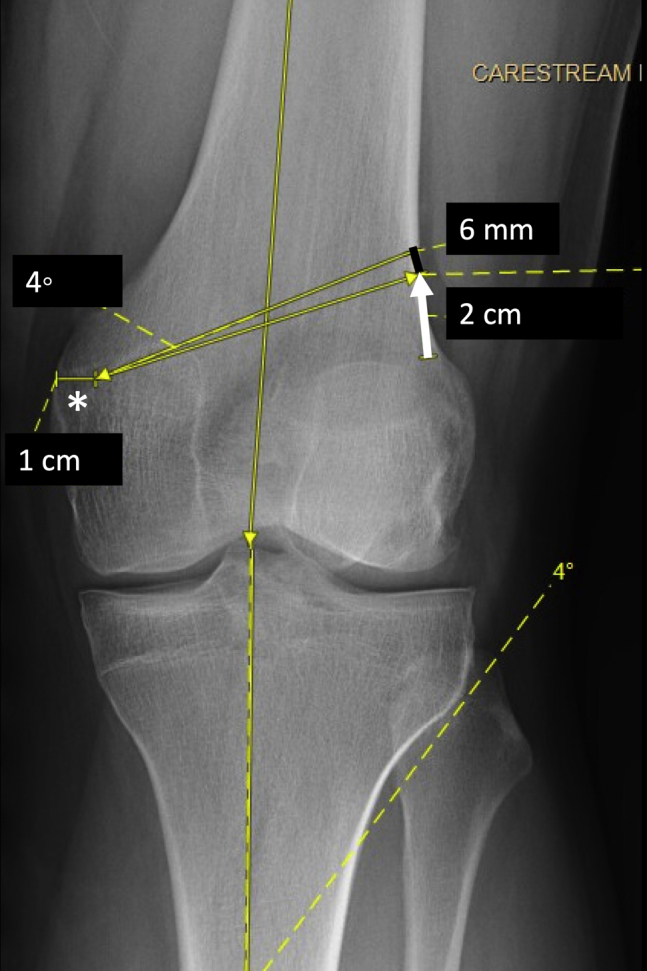
Anteroposterior left knee radiograph with preoperative templating for biplanar lateral opening wedge distal femoral osteotomy. The 4° correction is calculated using the hip knee ankle angle and transposed to the desired cut at the distal femur starting 2 cm above the lateral flare (white arrow) and aiming toward the adductor tubercle while preserving a 1-cm medial hinge (asterisks). The amount of correction is measured at the lateral cortex; in this case, 6 mm (black line).
Patient Positioning
The patient is positioned supine on a radiolucent table that allows fluoroscopy from the hip joint to the ankle. A well-padded thigh tourniquet is placed. A lateral thigh and foot posts are used to maintain a knee flexion angle of 60°. The osteotomy will be performed with the knee in a flexed position to further protect the posterior neurovascular structures.
Surgical Technique
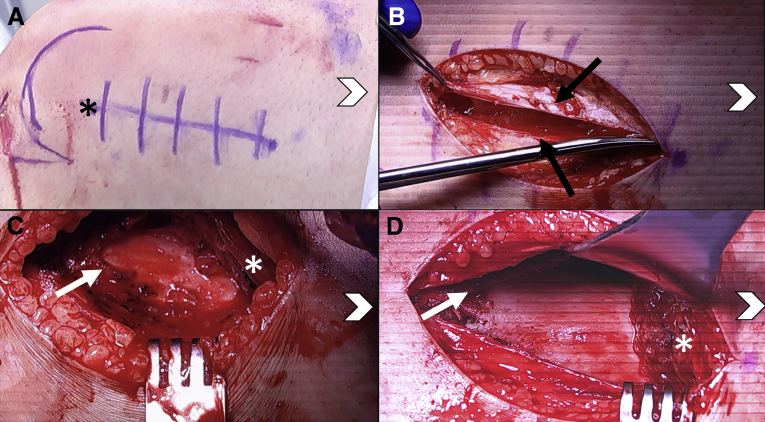
Diagnostic arthroscopy is performed before the osteotomy. Concomitant pathology may be addressed at this time, and the medial compartment is further assessed for any damage that would contraindicate this procedure. In general, we do not use a tourniquet during the procedure. A standard lateral approach to the distal femur is used with an approximately 12- to 15-cm longitudinal incision centered over the lateral epicondyle and lateral femur (Fig 3). (Note: If a concomitant intra-articular procedure is being performed an extended lateral parapatellar approach is used.) A split is then made in line with the incision through the iliotibial band. The vastus lateralis muscle is elevated anteriorly starting in the natural opening under the distal part of the muscle belly from the intermuscular septum with care to coagulate any perforating vessels. The periosteum over the lateral femur is split and elevated subperiosteally anteriorly and posteriorly using a winged tip elevator (Fig 3). The intermuscular septum is elevated from the lateral femur to gain access to the posterior femur. A laparotomy sponge is packed into this space, and a blunt curved retractor is then placed posteriorly and confirmed to be against bone to protect the neurovascular structures. A blunt Hohman retractor or malleable retractor can be placed anteriorly.
Fig 3.
Intraoperative photographs of a left leg with the patient positioned supine with head of the patient on the right side of the figures toward the chevron. (A) The lateral approach to the distal femur is marked on the skin and centered over the lateral epicondyle (asterisks). (B) The iliotibial band (black arrows) is split in line with the incision. (C) The vastus lateralis muscle (white asterisks) is elevated anteriorly and the periosteum (white arrow) is split along the femur. (D) The periosteum (white arrow) is elevated anteriorly and a retractor can be placed beneath the vastus lateralis muscle (white asterisks).
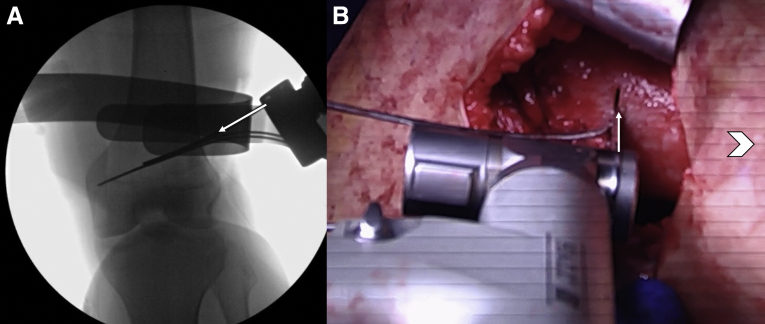
Then using fluoroscopic guidance, the starting point for the initial K-wire is identified about 1 to 2 cm proximal to the flare of the lateral condyle (Fig 4). Additionally, the plate can be placed to bone to confirm adequate position of the osteotomy. A K-wire is then drilled across the femur toward the adductor tubercle (Fig 4). A second K-wire is then placed parallel to the first on an anteroposterior view (Fig 4) and perpendicular to the long axis of the femoral shaft on a lateral view (Fig 5), which is assessed using fluoroscopy and an army/navy retractor.
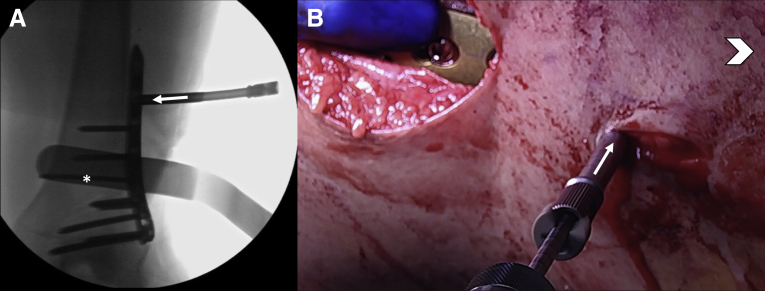
Fig 4.
Anteroposterior fluoroscopic view of a left leg showing placement of the initial K-wire from lateral to medial. The K-wire is started about 2 cm above the flare of the lateral condyle (black arrow) and aiming toward the adductor tubercle medially (asterisks).
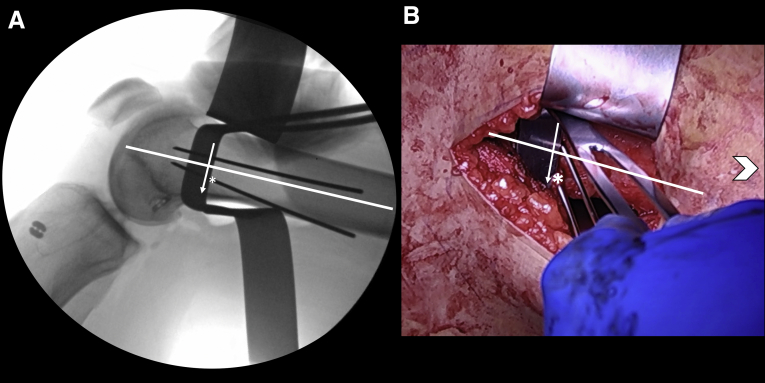
Fig 5.
(A) Lateral fluoroscopic view of a left leg showing placement of the second K-wire. The starting point (asterisks) is obtained on a perfect lateral fluoroscopic view while using an army/navy retractor (white arrow) to assess perpendicular placement of this K-wire with the long axis of the femoral shaft (white line). (B) Intraoperative photograph of a left leg with patient positioned supine with head of the patient on the right side of the figure toward the chevron demonstrating the starting point (asterisks) for the second K-wire using an army/navy retractor (white arrow) to assess perpendicular placement with the long axis of the femoral shaft (white line).
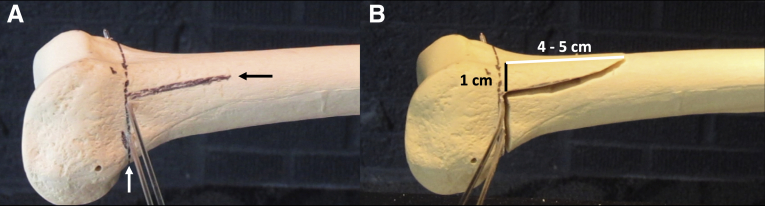
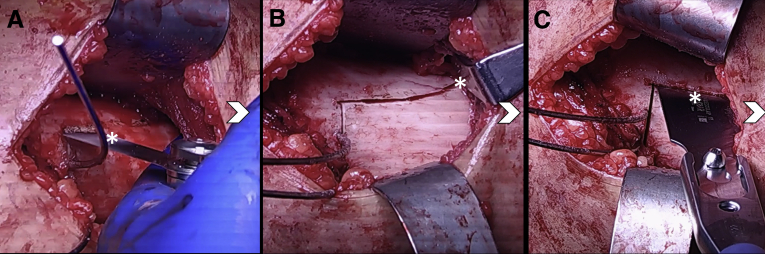
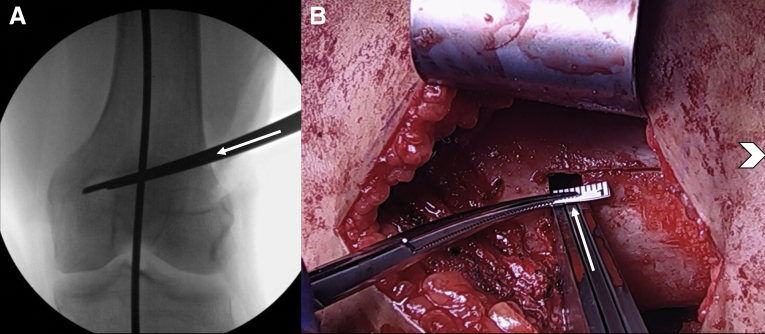
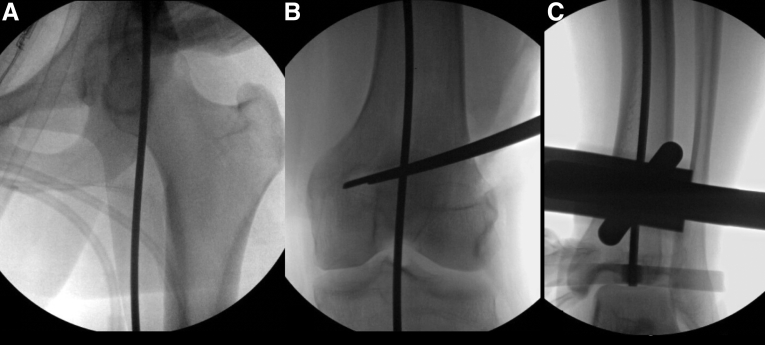
The anticipated saw cuts for the osteotomy and the anterior flange are then marked using electrocautery (Fig 6). The knee is in a flexed position to minimize the risk of iatrogenic injury to the neurovascular bundle. Under fluoroscopic guidance, the initial saw cut is made about 75% across the femur with care to use the malleable retractor posteriorly for protection using an oscillating saw (Conmed, Utica, NY) (Fig 7). The perpendicular biplanar cut is then completed with a smaller quarter-inch saw blade (Conmed) along the anterior cortex to create a 4- to 5-cm anterior flange (Fig 8). A flexible osteotome is used to complete the biplanar cut across and through the medial cortex (Aesculap, Center Valley, PA). Stacked osteotomes (Synthes, West Chester, PA) are then used to gap open the lateral cortex until this corresponds with the preoperative template (Fig 9). If there is excessive rotation, flexion, or extension of the osteotomy, a pointed reduction clamp can be used from anterior to posterior to help maintain the position of the osteotomy. A limb alignment rod is used to confirm the amount of correction with fluoroscopic views centered at the hip, knee, and ankle (Fig 10).
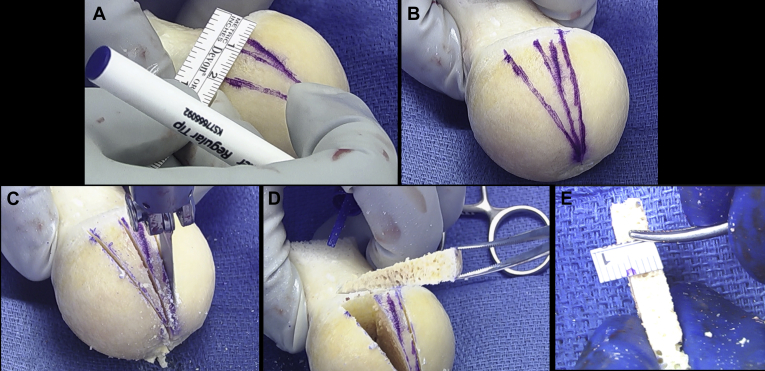
Fig 6.
Sawbones model of a left femur demonstrating: (A) planned cuts drawn for the osteotomy (white arrow) and biplanar anterior flange cut (black arrow on the lateral cortex). (B) Saw cuts have been made to demonstrate the size and shape of the anterior flange that is typically about 1 cm in height and 4 to 5 cm in length.
Fig 7.
(A) Anteroposterior fluoroscopic view of a left leg showing the trajectory of the saw blade (white arrow) along the superior border of the 2 K-wires. Note: The posterior malleable retractor was adjusted to show the trajectory of the saw blade for this image. The retractor will be in line with our saw when making the bone cuts. (B) Intraoperative photograph of a left leg with patient positioned supine with head of the patient on the right side of the figure toward the chevron demonstrating the trajectory of the saw blade (white arrow).
Fig 8.
Intraoperative photographs of a left leg with patient positioned supine with head of the patient on the right side of the figures towards the chevron demonstrating (A) the quarter-inch saw blade for the biplanar cut (asterisks). (B) The biplanar cut is completed through the anterior femoral cortex (asterisks). (C) Flexible osteotome (asterisks) is used to complete the biplanar cut across through the far cortex.
Fig 9.
(A) Anteroposterior fluoroscopic view of a left leg showing the stacked osteotomes (white arrow) to wedge open the lateral distal femur osteotomy. (B) Intraoperative photograph of a left leg with patient positioned supine with head of the patient on the right side of the figure towards the chevron demonstrating the stacked osteotomes (white arrow) to open the distal femur osteotomy to the size corresponding with our preoperative template, in this case 6 mm.
Fig 10.
Anteroposterior fluoroscopic views of a left hip, knee, and ankle using a straight metal alignment rod to assess the intraoperative alignment from (A) the center of the hip, (B) through the knee, and (C) to the center of the ankle.
A wedge of bone is then cut from the femoral head allograft to match the size of the correction (Fig 11). This bone wedge is placed into the osteotomy (Fig 12), and the alignment is again assessed with fluoroscopy to confirm the correction is maintained (Fig 13). Fixation of the osteotomy is achieved using a lateral distal femur locking plate from the Tomofix set (Synthes). The plate is held to the bone using 2 K-wires through the plate distally to assess the position on fluoroscopy (Fig 14). The distal locking screws are placed first into the distal femur. A nonlocking screw can be placed at the oblong hole just above the osteotomy to compress the osteotomy (Fig 15). The remaining proximal holes are filled with locking screws, which can be done percutaneously through additional stab incisions (Fig 16). The nonlocking screw can be left in place or removed and replaced with a locking screw. Final fluoroscopy films are taken to assess the plate and screws are in a safe position.
Fig 11.
A wedge of bone is cut from the femoral head allograft to match the size of the correction. (A) The corresponding measurement is made at the base of the femoral head. (B) Two wedges are marked to be cut. (C) Quarter-inch saw blade is used to cut the bone wedges from the femoral head. (D) The bone wedge is removed. (E) The size of the wedge is measured to confirm accuracy of the saw cuts.
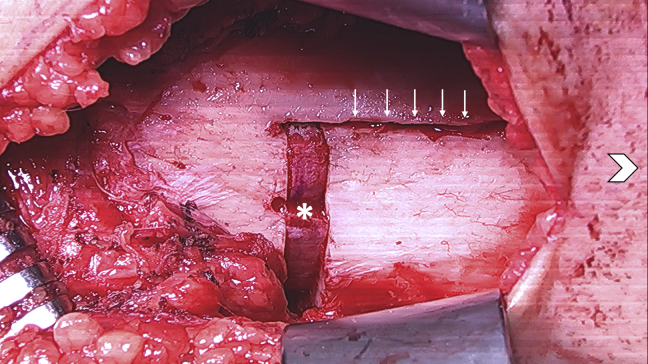
Fig 12.
Intraoperative photograph of a left leg with patient positioned supine with head of the patient on the right side of the figure toward the chevron demonstrating the bone graft wedge (asterisks) is placed in the osteotomy with the cortical edge lined up with the lateral cortex. The biplanar cut is reduced without evidence of flexion or extension of the osteotomy (white arrows).
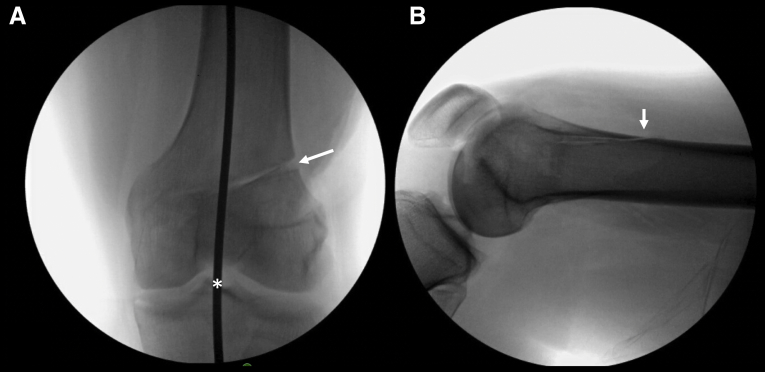
Fig 13.
(A) Anteroposterior fluoroscopic view of a left knee demonstrating the femoral head bone wedge (white arrow) and the correction of our alignment with the alignment rod through slightly medial to the center of the knee (asterisks). (B) Lateral fluoroscopic view of a left knee demonstrating the biplanar cut exiting the anterior femoral cortex (white arrow).
Fig 14.
Lateral fluoroscopic view of a left knee demonstrating placement of the plate along the long axis of the femur and held in place with 2 K-wires (asterisks).
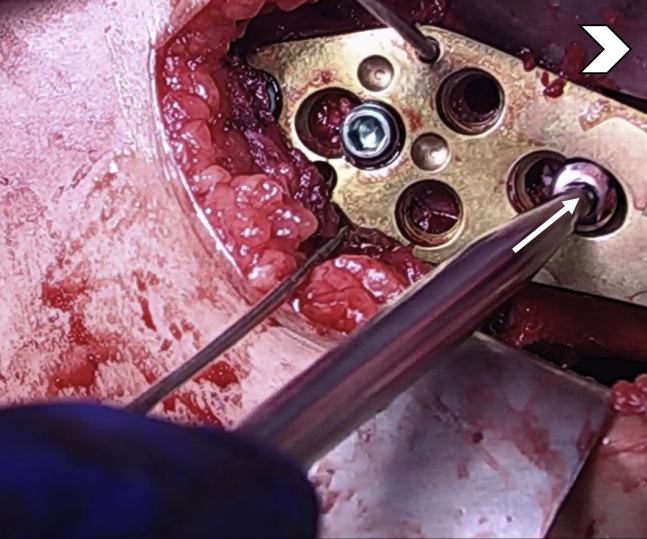
Fig 15.
Intraoperative photograph of a left leg with patient positioned supine with head of the patient on the right side of the figure toward the chevron demonstrating the 2 K-wires through the plate and the distal locking screws have been placed. A nonlocking screw is being placed above the osteotomy to compress the osteotomy through the plate (white arrow).
Fig 16.
(A) Anteroposterior fluoroscopic view of a left leg showing percutaneous placement of the drill guide (white arrow) that is locked into the proximal locking hole of the plate. Additionally, the bicortical nonlocking screw is seen (asterisks). (B) Intraoperative photograph of a left leg with patient positioned supine with head of the patient on the right side of the figure toward the chevron demonstrating the locking guide (white arrow) in place and the drill being used to drill the near cortex for placement of a locking screw.
Additional information regarding the bLOWDFO surgical technique is shown in Video 1. The pearls and pitfalls of this technique are summarized in Table 1. The postoperative protocol is summarized in Table 2. Postoperative radiographs are obtained at 2 weeks, 6 weeks (Fig 17), 6 months, and 1 year. Full-length radiographs are obtained at 6 weeks if patient is weightbearing without pain to assess correction and repeated at 1 year postoperatively.
Table 1.
Pearls and Pitfalls
| Pearls |
|
|
|
|
|
|
| Pitfalls |
|
|
|
|
|
Table 2.
Postoperative Protocol
| Intraoperative |
|
|
| Days 0-1 |
|
|
|
| Weeks 0-2 |
|
|
|
| Weeks 3-4 |
|
|
|
| Weeks 5-6 |
|
| Weeks 7+ |
|
DVT, deep vein thrombosis; HKB, hinged knee brace; ROM, range of motion.
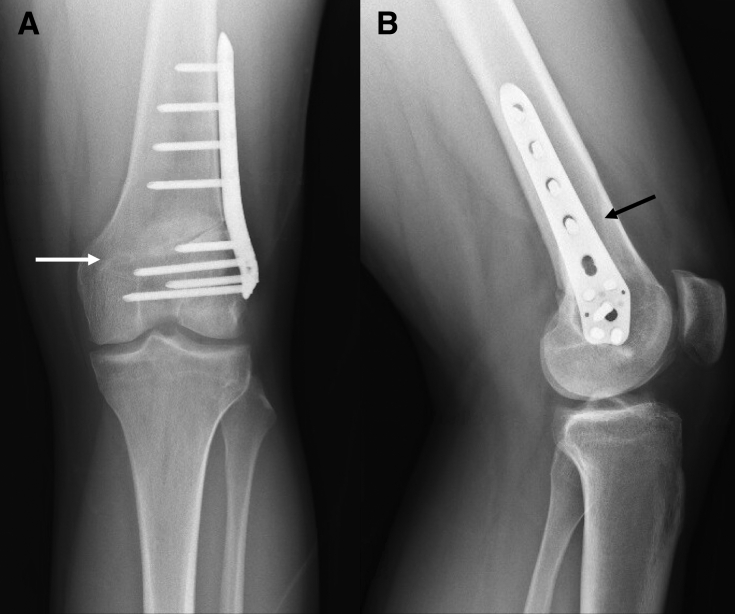
Fig 17.
(A) Anteroposterior and (B) Lateral 6-week postoperative radiographs of a left leg demonstrating the final position of the lateral locking plate and screws to be in a safe position with interval healing of the osteotomy (white arrow) and complete healing of the anterior biplanar cut (black arrow).
Discussion
The primary advantages of performing a biplanar distal femoral osteotomy are the ability to control the osteotomy intraoperatively to avoid excessive rotation, flexion, or extension, as well as the increased bone surface area for healing and early weightbearing. Additionally, the biplanar cut allows the osteotomy to remain completely extra-articular, which can decrease pain and the risk of arthrofibrosis within the suprapatellar recess. The lateral approach to the distal femur is also a well-known and safe surgical approach.4
In a uniplanar technique, authors have described drawing a line along the lateral femoral cortex with a Bovie to monitor the rotation, flexion, and extension of the osteotomy.5 We similarly used this technique, but have converted to this biplanar technique and found it to be more reliable for controlling the position of the osteotomy intraoperatively. Previous studies have demonstrated the increased stability of the osteotomy when using a biplanar technique. Pietsch et al.4 demonstrated increased external torsional stiffness in synthetic femora comparing a bLOWDFO with a uniplanar LOWDFO. Additionally, they cut the medial cortex to simulate an intraoperative fracture of the medial hinge and found that the biplanar technique significantly reduced the external rotation at the osteotomy and showed a significantly increased external torsional stiffness.
In addition to the risk of medial hinge fracture, an important consideration when performing this bLOWDFO is the risk of fracture of the anterior flange. Care must be taken to maintain adequate bone when making the saw cuts (about 1 cm at the anterior flange) and to control the osteotomy throughout the procedure when extending and flexing the knee for fluoroscopic imaging.
Increasing the surface area of the bone cuts can decrease bone healing time and allow for earlier weightbearing. Van der Woude et al.6 reported bone healing time with a biplanar closing wedge technique at a mean of 3.9 ± 2.5 months compared with a uniplanar technique at an average of 6.1 ± 2.7 months, which they defined as full reformation of the bone with the osteotomy recognizable. Bagherifard et al.7 presented a series of 8 patients who underwent various biplanar distal femur osteotomies including closing and opening wedge. They reported a mean union time of 9.2 ± 2.3 weeks, though did not define criteria for union. In the authors experience, patients have less pain and are typically full weightbearing at 6 weeks with crutches.
There are very few published studies on long-term clinical outcomes after a bLOWDFO, though several discussing uniplanar LOWDFO techniques. In the largest series, Cameron et al.8 reported in 30 patients (31 knees) at a mean follow-up of 5 years (range, 2-12 years) 74% survivorship in the arthritis group and 92% survivorship in the joint preservation group. Survivorship was defined as conversion to knee arthroplasty. They also reported significant improvements in International Knee Documentation Committee scores. Interestingly, they also evaluated the accuracy of the correction and found 10 of 21 patients (47%) with postoperative full-length radiographs were within the correction goal of ±3° from neural mechanical alignment. They concluded that LOWDFO was less accurate in correction of valgus deformity than expected, though achieved significant improvements in knee pain and functional scores.
In a recent review of the military health system records, Rensing et al.9 found that 58% of patients in a young, active-duty military population were not able to return to active duty after distal femoral osteotomy for symptomatic lateral compartment disease. The authors concluded in their series of 19 patients with an average age of 30 years (range, 19-50 years) that offloading the lateral compartment improves symptoms at short to midterm follow-up preventing progression to arthroplasty, though young active duty military patients have suboptimal return to duty rates.9
The primary disadvantage of this technique is the inability to offload chondral injuries or arthritis of the posterior femoral condyle in deeper flexion angles. A femoral-based osteotomy will preferentially affect joint contact forces in extension with less effect at higher knee flexion angles and no effect at 90° or beyond.10 In these cases, as well as cases with a primary valgus deformity within the tibia, our preference is to perform a tibial based osteotomy. Other complications inherent to osteotomy procedures include nonunion, malunion, wound complications, infection, thromboembolism, stiffness, and painful hardware requiring reoperation.1,3
In conclusion, this Technical Note describes our preferred technique to correct valgus malalignment in patients with symptomatic lateral compartment disease via a bLOWDFO. Although further studies are needed to evaluate the clinical outcomes using this technique, the authors believe this procedure is a reproducible and effective treatment option to reduce pain and improve function in a younger patient population where arthroplasty is less desirable.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: R.A.D. receives educational support from Arthrex. D.C.F. is a consultant for Depuy Mitek, MTF, KCRN, and Hyalex; received research support form Cartiheal, Anika Therapeutics, Aesculap, and Moximed; and is a consultant and receives research support from Smith & Nephew, Zimmer Biomet, and Vericel. C.C.K. receives educational support from Smith & Nephew and grants from Active Implants, Zimmer Biomet, and Vericel. R.A.M. receives educational support from Arthrex and a grant from Zimmer Biomet. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
A technique for biplanar lateral opening wedge distal femur osteotomy is presented. Arthroscopy is performed before the osteotomy to address intra-articular pathology and assess the medial compartment. The osteotomy is performed through a direct lateral approach to the distal femur. K-wires are placed to guide the primary osteotomy cut and a free hand biplanar cut is made along the anterior cortex. Femoral head allograft wedge is placed to maintain the desired correction. Fixation is then achieved with a lateral locking plate.
References
- 1.Pilone C., Rosso F., Cottino U., Rossi R., Bonasia D.E. Lateral opening wedge distal femoral osteotomy for lateral compartment arthrosis/overload. Clin Sports Med. 2019;38:351–359. doi: 10.1016/j.csm.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 2.Leong N.L., Southworth T.M., Cole B.J. Distal femoral osteotomy and lateral meniscus allograft transplant. Clin Sports Med. 2019;38:387–399. doi: 10.1016/j.csm.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 3.Sherman S.L., Thompson S.F., Clohisy J.C.F. Distal femoral varus osteotomy for the management of valgus deformity of the knee. J Am Acad Orthop Surg. 2018;26:313–324. doi: 10.5435/JAAOS-D-16-00179. [DOI] [PubMed] [Google Scholar]
- 4.Pietsch M., Hochegger M., Winkler M., Sandriesser S., Freude T., Augat P. Opening-wedge osteotomies of the distal femur: Minor advantages for a biplanar compared to a uniplanar technique. Knee Surgery, Sport Traumatol Arthrosc. 2019;27:2375–2384. doi: 10.1007/s00167-018-5332-5. [DOI] [PubMed] [Google Scholar]
- 5.O’Malley M.P., Pareek A., Reardon P.J., Stuart M.J., Krych A.J. Distal femoral osteotomy: Lateral opening wedge technique. Arthrosc Tech. 2016;5:e725–e730. doi: 10.1016/j.eats.2016.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van der Woude J.A.D., Spruijt S., van Ginneken BTJ, van Heerwaarden R.J. Distal femoral valgus osteotomy: Bone healing time in single plane and biplanar technique. Strateg Trauma Limb Reconstr. 2016;11:177–186. doi: 10.1007/s11751-016-0266-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bagherifard A., Jabalameli M., Hadi H.A. The results of biplanar distal femoral osteotomy; a case series study. Arch Bone Jt Surg. 2015;3:35–38. [PMC free article] [PubMed] [Google Scholar]
- 8.Cameron J.I., McCauley J.C., Kermanshahi A.Y., Bugbee W.D. Lateral opening-wedge distal femoral osteotomy: Pain relief, functional improvement, and survivorship at 5 years. Clin Orthop Relat Res. 2015;473:2009–2015. doi: 10.1007/s11999-014-4106-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rensing N., Prabhakar G., Kusnezov N., Zarkadis N.J., Waterman B.R., Pallis M. Distal femoral osteotomy in a young symptomatic population: Outcomes correlate to concomitant pathology. J Orthop. 2019;16:283–288. doi: 10.1016/j.jor.2019.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wylie J.D., Schiederer B., Obopilwe E. The effect of lateral opening wedge distal femoral varus osteotomy on tibiofemoral contact mechanics through knee flexion. Am J Sports Med. 2018 doi: 10.1177/0363546518799353. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A technique for biplanar lateral opening wedge distal femur osteotomy is presented. Arthroscopy is performed before the osteotomy to address intra-articular pathology and assess the medial compartment. The osteotomy is performed through a direct lateral approach to the distal femur. K-wires are placed to guide the primary osteotomy cut and a free hand biplanar cut is made along the anterior cortex. Femoral head allograft wedge is placed to maintain the desired correction. Fixation is then achieved with a lateral locking plate.