Abstract
Background.
Despite increased risks for mental health problems, East Asian Immigrant Women have the lowest overall service utilization rates of any cultural group in the U.S. While the influence of cultural processes as the cause of low service utilization is widely speculated, no empirical study has tested cultural determinants (including culturally specific idioms of distress, culturally based illness interpretations, or concerns about social consequences), social contextual factors, perceived need, and help seeking behaviors.
Method.
This present study examines how cultural determinants, such as symptom experience, beliefs and interpretations, and perceptions about the social environment, affect perceived need and help seeking type for Japanese women living in the US.
Results.
Increasing physical symptom severity increased the predicted probability of endorsing PN. For those participants with PN, 48.6% of them used Medical HS (χ2 = 11.27, p = 0.00), and 12.5 % of them used the Psychological HS (χ2 = 7.43, p = 0.01). Multivariate logistic regression revealed that when PN is considered with the other cultural variables while controlling for structural variables, PN increases the odds of Medical HS (OR=2.78, 95% CI [1.0-5.8], p < 0.01). The odds of Medical HS are also increased with higher social support (OR=1.07, 95% CI [1.0-1.1], p < 0.01). Finally, the presence of interpersonal stigma beliefs decreased the odds of Medical HS (OR=2.4, 95% CI [1.1-5.3], p < 0.03).
Conclusions.
Clinical and research implications are discussed.
The foreign-born population in the U.S. has more than tripled in the last thirty years, and Asians are the fastest-growing immigrant group in the United States, topping 37 million in 2012 (Larsen, 2004; Min, 2006; U.S. Census Bureau, 2007, 2008). Among immigrants, East Asian Immigrant Women (EAIW) have the highest distress (Takeuchi et al., 2007; Williams, 2002; Yeung et al., 2008), with suicide being the 7th leading cause of death for childbearing Asian women only (World Health Organization, 2009). Reported mental health risks for EAIW include separation from extended families; dependency due to migration laws; role changes amplified in new social networks; and unremitting responsibility for the care of others (World Health Organization, 2000). EAIW may share rules for female behavior include notions that women should sacrifice their needs for their family, leading to a tendency to ignore their symptoms (Ro, 2002; Ta & Hayes, 2010; Ta, Juon, Gielen, Steinwachs, & Duggan, 2007; Williams, 2002). Also, the National Latino and Asian American Study (NLAAS) found that depression rates for female immigrants may increase the longer women reside in a new location (Takeuchi, Hong, Gile, & Alegría, 2007 ). Despite these risks, as a group, EAIW also have the lowest overall service utilization rates of any cultural group in the U.S. (Garland, Lau, Yeh, McCabe, et al., 2005; Kimerling & Baumrind, 2005). While the influence of cultural processes as the cause of low service utilization is widely speculated, no empirical study has tested cultural determinants (including culturally specific idioms of distress, culturally based illness interpretations, or concerns about social consequences), social contextual factors, perceived need and help seeking behaviors. This study fills that gap.
EAIW have the lowest overall service utilization rates of any group in the U.S., and this low utilization may be related to physical symptomology as well as low perceived need (Garland, Lau, Yeh, & McCabe, 2005). In a nationally representative sample of individuals with an objective diagnosis of major depressive disorder, only 31% of Asian Americans, 36% of Latinos, and 41% of African Americans reported seeking depression care in the previous 12 months, compared with 60% of non-Latino whites (Interian, Lewis-Fernández, & Dixon, 2013). The NLAAS data showed that Asians had lower rates of mental health-related service use compared with the general population; only 8.6% of Asians sought help from any services, compared with 17.9% of the general population. Help seeking rates varied among individuals with services need 34.1% of Asians with a probable diagnosis sought services, compared with 41.1% of all persons in the National Comorbidity Survey sample (Abe-Kim et al., 2007). In an analysis that looked at the impact of having somatic symptoms on help seeking for data from the NLAAS, Escobar et al. found that Asians with somatic symptoms were less likely than whites to use medical OR mental health services (Escobar, Cook, Chen, Gara, Alegría, et al., 2010).
Help seeking is a process that involves a series of decisions and actions, rather than a single, planned choice. Pescosolido proposed that help seeking actions are embedded within the social network, and that network interactions influence the identification of a problem as well as what should be done it (Pescosolido, 1992). We define help seeking as any action taken to mitigate distress, including seeking advice; seeking social and emotional support; seeking traditional healing; seeking spiritual guidance; and seeking advice and treatment from medical or mental health providers. The process of mental health help seeking begins with the decision about whether to seek care (which is the object of our study), followed by ongoing decisions about whether to remain involved in treatment. Compared to their mainstream counterparts, ethnic minority clients, including EAIW, report experiencing a “distance” in the therapy relationship due to the multiplicity of ethnic and sociocultural differences that distinguish them from the therapist (Yasui & Henry, 2014). Cultural barriers to help seeking can include therapist misunderstanding; feelings of cultural alienation within the host culture; language and economic barriers; mistrust, stigma, and therapist cultural biases (Saint Arnault and Woo, 2017).
The perceived need for mental health services interacts with cultural variables such as stigma and social networks (Kimerling & Baumrind, 2005). The perception of distress has been differentiated from an objective need for help seeking literature. The perceived need may be a better predictor of problem recognition and subsequent help seeking than the nature of the symptoms themselves (Costello & Janiszewski, 1990; Kellam, Branch, Brown, & Russell, 1981; Srebnik, Cauce, & Baydar, 1996). However, the influence of culture on the subjective perception of need has received little empirical study. Anderson and Newman's (1973) help seeking model theorized that problem recognition prompts help seeking (Andersen, 1995). Also, research on structural determinants of health has documented the importance of structural variables that impact help seeking, such as access, language, insurance, poverty, and discrimination (Dean, Williams, & Fenton, 2013).
One subpopulation of EAIW is Japanese immigrants. While they share some characteristics with other EAIW groups, they also have distinct characteristics, making disaggregated research critical (Srinivasan & Guillermo, 2000). Michigan has a sizeable Japanese expatriate population due to the presence of the Japanese auto industry around Detroit. Most of the 8-10,000 Japanese living there work in the automotive industry and related businesses (Consulate General of Detroit, 2008), and the Japanese population in surrounding counties ranges from 4.2 to 8.3% of the total population (U.S. Census Bureau, 2001). While very few studies have examined the experience of the wives of Japanese sojourners in America, most research finds that the spouses of expatriates interact primarily among their social circles and that these women felt that their lives were suspended until their return to their homeland (Flory, 1989). Some spouses report trying to stay happy for the success of their husbands, and frustration with the long hours and demands the experience placed on the husbands (DeCieri, Dowling, & Taylor, 1991). The lead author has studied help seeking for the women in this community since the tragic drowning of a baby by a Japanese expatriate woman during a postpartum psychosis (Saint Arnault & Fetters, 2011). The intercultural dialog between the Japanese community and the clinical community that followed highlighted the need to understand how symptoms interact with social and cultural factors. This present study examines how cultural determinants, such as symptom experience, beliefs and interpretations, and perceptions about the social environment affect help seeking by testing the Cultural Determinants of Help Seeking theory.
Theoretical and Study Model
We theorize that prevailing cultural models influence how people experience suffering, interpret that suffering, anticipate consequences of it, and interact with their social world around it. We refer to these concepts individually as cultural variables, and collectively as the Cultural Determinants of Help Seeking (CDHS) (Saint Arnault, 2018) (See Figure 1). This theory aims to operationalize how these cultural variables may inhibit help seeking for those who might otherwise desire to do so (Saint Arnault, 2009; Saint Arnault & Woo, 2017). Most research has focused on the structural circumstances that may limit access to health care for an immigrant (such as English fluency, age, income, education or length of time abroad). In our theory, we assume that these sociodemographic factors interact with cultural factors to influence help seeking (Dean et al., 2013). In this way, we have responded to calls for cultural theoretical models to guide research and interventions (Caldwell, 1993; Dolatian et al., 2013; Dressler & Oths, 1997; Knutson, 2013; J. Lee, Donlan, Cardoso, & Paz, 2013; Salas, Raine, Vallianatos, & Spence, 2015).
Figure 1:
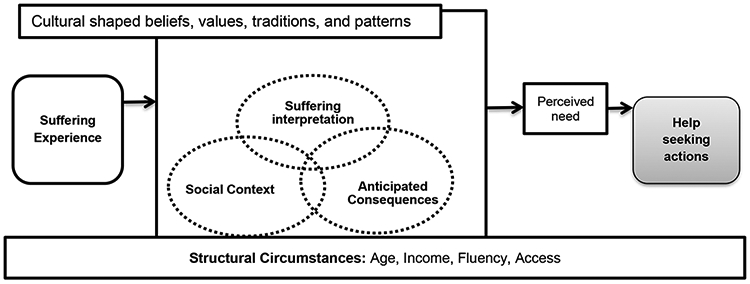
Cultural Determinants of Help Seeking-Revised
We propose that a person’s Suffering Experience is perceived and labeled according to cultural norms, beliefs, and patterns, that this experience initiates the help seeking process, and that the nature of this suffering is the primary impetus for cultural interpretation (de Oliveira & Nisbett, 2017; Hofmann & Hinton, 2014). We theorize that cultural models direct perception of both physical sensations and emotional feelings (Moscovici & Duveen, 1998) and that these are developmentally shaped through interaction with the culture and society (Luria, 1976; Moscovici & Duveen, 1998). In other words, the cultural model “tells” the person what aspects of his or her experience to attend to; as well as which physical and emotional sensations, changes, and experiences should be acknowledged and articulated. This dynamic interaction between symptoms, meaning making and culture is sometimes referred to as “idioms of distress,” and these are a well-documented source of cultural variation (Kirmayer, Dao, & Smith, 1998; Parsons, 1984; Parsons & Wakeley, 1991). We operationalize this concept as symptom type and measure both depression symptoms as well as physical symptoms to capture the varieties of culturally-based symptom patterns. Like others, we have consistently demonstrated the importance of somatic symptoms for Japanese immigrants. In a study of Japanese and Korean students, an examination of the co-occurrence of physical symptoms with depression using a 59 item physical symptom checklist found that women who scored high on the depression screening tool also endorsed more than 20 physical symptoms (Saint Arnault & Kim, 2008), in contrast to depressed American women who endorsed only three physical symptoms (Saint Arnault, Sakamoto & Moriwaki, 2006). Research on the relationship between culture, physical symptoms and use of services can also be found outside of Asian cultures. For example, studies of other cultural groups have found that higher somatic symptoms was associated with higher medical service use (Kiat, Youngmann, & Lurie, 2017), as well as higher use of primary care (Rask, Ørnbøl, Rosendal, & Fink, 2017).
In our theory, a person’s culturally-based understanding of their suffering experience is the core phenomenon of interest, and we believe it is comprised of two interrelated evaluations. Suffering Interpretations are those cultural beliefs about the cause, controllability, expected course (or recurrence), and curability of suffering. Suffering Consequences are a person’s expectations about how others might view their suffering. We operationalize interpretations and consequences as beliefs toward mental illness. For example, in our study of Irish domestic violence survivors, we found that shame fostered a sense of immobilization, and decreased help seeking (Saint Arnault & O'Halloran, 2016). Research has shown that collectivist values held by people in East Asian cultures can cause people to fear that others will judge people with mental illness harshly, which can decrease the likelihood of self-disclosure (Association of Asian Pacific Community Health Organizations, 1995; Iwamasa & Hilliard, 1999; K.-M. Lin & Cheung, 1999; Ma, 1999). We define Social Context as the perceived availability of social support within the one’s social world, and we operationalize this as perceived social support. Research has shown that low social support may inhibit help seeking for the Japanese (Bachnik, 1994; Lebra, 1974, 1976; Lock, 1987; Saint Arnault, 2004, 2014; Saint Arnault & Roels, 2012; Saint Arnault & Shimabukuro, 2016). Our early grounded theory research with 25 Japanese expatriate women in 1997-1998 revealed that high distress and internal pressures to fulfill roles compelled women to use nonverbal, medical, spiritual and social efforts to communicate distress (Saint Arnault, 2002). In qualitative research of the meaning of distress for the 24 highly distressed subsample of the 209 Japanese women examined in this study, we found that a lack of social support was related to stigma, and were both a cause of distress and a barrier to help seeking (Saint Arnault & Shimabukuro, 2016).
An outcome of cultural interpretations of suffering is the perception of the need for help. We define Perceived Need as the personal summative evaluation of one's need for health care. We believe that the evaluation of need results from consideration of symptom type, interpretations about the symptoms, the expected consequences of having the symptoms, and the social context characteristics, and that perceived need precedes help seeking action. In our previous studies examining this sample, we examined the role of depressive symptoms as well as cultural beliefs that inhibited help seeking for the 34% (n=71) of our sample who stated they perceived a need for health care but did not seek help. Of those who perceived a need but did not seek help, women with high depression scores had significantly higher scores for incurability (illness interpretation), as well as shame (illness consequence) when compared with their low depression group. Logistic regression revealed that having somatic symptoms was a significant predictor of NOT seeking help (Saint Arnault & Woo, 2017). In a different study that examined help seeking type in a community-based sample of 402 South Korean women, we also found a positive correlation between perceived need and help seeking for formal mental health help (Saint Arnault, Woo, & Gang, 2018). However, we did not examine the relationships among all of the CDHS variables and help seeking type.
Help seeking is our primary outcome, and our definition of help seeking is “the experiences, expectations, and interpretations that interact with structural variables, as well as context, to influence behavior aimed at reducing suffering and promoting health (Saint Arnault, 2018).” We operationalize help seeking by type of service use, including social, professional and traditional help seeking. These avenues are often interacting and iterative. Little is known about the specific help seeking types used by the population under study; however, some reports suggest that medical help and traditional therapies are favored over psychological therapy and medication (Hsiao et al., 2006).
To test the CDHS theory, we operationalized the concepts into variables, which we examine as theoretical predictors of perceived need and help seeking for Japanese women living in the US. Specifically, controlling for sociodemographic variables, does symptom type and theoretical predictor variables (including interpretations, anticipated consequences, and social context) predict Perceived Need (PN)? Based on our previous work, we hypothesize that physical symptoms will predict PN, but emotional symptoms will not. Second, is PN related to Help Seeking (HS) type (Medical, Psychological, or Traditional)? While we do not find published research in this area, based on our fieldwork, we hypothesize that medical help will be the primary help sought, and that somatic distress will predict medical HS. Finally, controlling for sociodemographic variables, do these predictor variables, along with PN, predict the likelihood of engaging in various HS types? We hypothesize PN, somatic distress and stigma will interact to influence HS types.
Methods
Design
This study uses the quantitative data from a larger mixed method project that examined distress and help seeking for a sample of Japanese immigrant women living in Michigan. The University of Michigan IRB approved all procedures and materials for this study, and all participants gave informed consent (HUM00002837). We sampled Japanese-born women from both primary-care sites and the general community using random start interval sampling over a 5-year enrollment period between the years 2005-2010. All materials were in Japanese, including consent forms and the survey packet.
Sample
Participants were 209 Japanese immigrant women living in the United States. The average length of time they resided in the US was 4.84 ± 4.98 years (see Table 1). Their average English fluency score was 14.18 ± 5.41 (range = 5-30) and average perceived social support score was 51.63 ± 10.59 (range = 0-64). The average depressive symptom score was 7.08 ± 8.11 (range = 0-41), and average physical symptom severity was 19.40 ± 18.87 (range = 0-102).
Table 1:
Measurement of Cultural Determinants of Help Seeking
| Theoretical concept |
Operationalization | Measure |
|---|---|---|
| Sociodemographic factors |
Family income, education, age, years in the US, and English fluency |
FLOSEM |
| Social Context | Social Support | Perceived social resources (PRQ) |
| Suffering Experience |
Symptom type | Depression (CESD-K-R); Physical symptoms (CSC Physical) |
| Suffering Interpretation |
Recurrence, Curability | Recurrence, incurability BMI subscales |
| Suffering Consequences |
Other’s Perception | Dangerousness, embarrassment and interpersonal role BMI subscales |
| Perceived Need | ---- | PN yes or no |
| Help seeking | ---- | Help seeking type |
Measures
The theoretical concepts and their operationalized study variables are depicted in Table 2.
Table 2:
Demographics of Japanese Immigrant Women (N=209)
| Characteristics | Prevalence | |
|---|---|---|
| M | SD | |
| Age | 39.57 | 7.60 |
| Years in the US | 4.84 | 4.98 |
| English Fluency (FLOSEM) | 14.18 | 5.41 |
| Social Support (PRQ) | 51.63 | 10.59 |
| CESD | 7.08 | 8.11 |
| Physical Symptoms | 19.40 | 18.87 |
| Beliefs toward Mental Illness (BMI) | 46.03 | 9.77 |
| N | Percentage | |
| Annual Family Income | ||
| $20,000 – 40,000 | 7 | 3.6 |
| $40,000 – 60,000 | 25 | 12.9 |
| $60,000 – 80,000 | 30 | 15.5 |
| $80,000 – 100,000 | 39 | 20.1 |
| > $100,000 | 47 | 24.2 |
| Unknown | 46 | 23.7 |
| Education | ||
| High school | 25 | 12.1 |
| Technical or Junior College | 86 | 41.5 |
| Undergraduate Degree | 78 | 37.7 |
| Graduate Degree | 12 | 5.8 |
| Other | 6 | 2.9 |
| CESD | ||
| CESD below 16 | 176 | 86.7 |
| CESD above 16 | 27 | 13.3 |
| Help Seeking Needs | ||
| No perceived need | 136 | 65.4 |
| Perceived need but did not seek help | 72 | 34.6 |
| Use of Professional Interventions | ||
| Professional Medical | 70 | 33.5 |
| Professional Psychological | 13 | 6.2 |
The sociodemographic questions were family income, education, age, years in the US, and English fluency. Income was measured with a scale anchored at 20,000 or below to over 100,000 dollars. Education was across a continuum of high school to graduate school. English fluency was measured with the Stanford Foreign Language Oral Skills Evaluation Matrix (FLOSEM) (Padilla & Sung, 1999). The FLOSEM relies on a matrix with five categories of language use in columns of the matrix, including self-assessment of Comprehension, Fluency, Vocabulary, Pronunciation, and Grammar. For each category, there are six possible self-assessment levels: representing a continuum of self-reported competence, ranging from "extremely limited ability" (Level 1) through "native-like ability" (Level 6). For example, for the Fluency category, a level one response is “I can participate only in interactions which involve…offering very short responses to simple questions…” to Level 4 “I can effortlessly express myself, but may occasionally…hesitate as I try to express more complex ideas…(or) search for less-common words and expressions…” FLOSEM scores across the matrix were summed, with a higher score indicating overall self-perceived facility with English. The reliability of the FLOSEM for our study was 0.95.
Suffering Experience.
To capture various idioms of distress, we examined both emotional and physical distress. Depression symptoms were assessed using a cultural adaptation of the Center for Epidemiologic Studies-Depression Scale (CESD), which is a 20-item scale with a higher score indicating greater impairment (Radloff, 1977). The CESD asks participants to rate whether they had experienced the symptoms described in each item during the previous 2 weeks on a 4-point scale from 0 (never) to 3 (more than 5 days), with higher scores (above 16) indicative of clinically significant depression, and was the cut-off used in this study. Noh and colleagues, who reversed the wording of the positive affect items, have substantiated that these modifications improve the performance of the CESD with East Asian populations (Noh, Avison, & Kaspar, 1992). In studies using the CESD-K-R, Cronbach’s alpha coefficients range between 0.71-0.89. Cronbach’s alpha for our study was 0.90. We measured physical symptoms with a modified version of the Pennebaker Inventory of Limbic Languidness (PILL) (Pennebaker, 1982). The original PILL had 54 items and was a self-report checklist designed to measure the severity of experiencing a variety of common physical symptoms and diseases, and we used the same Likert rating scale as the CESD. We modified the PILL by collapsing seven items with others items to allow for natural translation. For example, the three items “sneezing,” “congestion” and “runny nose” were collapsed into “congestion or sneezing.” Also, because of the importance of somatic symptoms in depression in some Asian cultures, we added twelve items: poor appetite, poor sleep, confusion, fatigue, abdominal pain, dizziness, lightheadedness, joints pain, shoulder pain, weakness, palpitations, and tiredness. The final instrument had 59 items. Because no symptom necessarily correlates with any other symptom, internal consistency measures are not appropriate. However, the PILL has shown a 2-month test-retest reliability range from 0.79 to 0.83 (Pennebaker, 1982).
Predictor variables.
Suffering Interpretations were measured with the beliefs about incurability and recurrence subscales of the Beliefs toward Mental Illness Scale (BMI) (Hirai & Clum, 2000). The original BMI consists of value and belief statements about internalized expectations and values related to mental illness, including subscales for dangerousness, recurrence, embarrassment, interpersonal/role, and incurability. Participants rated their level of agreement with belief statements according to a 4-point Likert scale ranging from 1 (strongly disagree) to 4 (strongly agree). The alpha reliabilities for the incurability subscale for our sample was 0.68 and was 0.62 for the recurrence subscale. Suffering Consequences was measured with the dangerous, embarrassment and interpersonal role subscales of the BMI. The alpha reliability scores for our sample were dangerousness (α=0.52); embarrassment (α=0.76); and interpersonal role (α=0.79). Social Context was measured as perceived social support using the Personal Resource Questionnaire (PRQ) (Weinert & Brandt, 1987), which is a measure of perceived social support. The fifteen items are arranged along a 7-point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree), and are summed with total points that range from 15 to 105, with higher scores indicating higher levels of perceived social support. Example questions include “There is someone I feel close to that makes me feel secure,” and “There are people who are available if I need help over an extended period of time.” Cronbach’s alpha for our study was 0.93.
Outcomes.
Outcomes in this study were perceived need (PN) and help seeking (HS) behavior. Perceived Need was determined with two questions. First, “In the last year, did you have problems in your mind or body for which you needed help” (Lin, Goering, Offord, Campbell, & Boyle, 1996). Women who answered “no” were determined to have “No Perceived Need (NPN).” We also asked women “Did you have a physical or emotional problem for which you did not seek help?” Women who answered “yes” to this question we deemed to have “Perceived Need without Help Seeking (PNnoHS).” Help seeking behavior was measured with the Help Seeking Behavior Questionnaire (HSBQ), which asks the participant about recent life events for which they sought help in the last year, the specific sources of help they sought, and includes professional medical, professional psychological, and traditional therapies (Lin, Goering, Offord, Campbell, & Boyle, 1996). Medical help included primary care, nurses, general medical, medications, and specialty medical help; Psychological help included crisis hotlines, counselors, psychiatrists and social workers; and Traditional help included traditional herbs, moxibustion, folk remedies and acupuncture.
Study Procedures
All communication was in the participant’s native language, and all research materials and measures were translated using the three-phase linguistic and cultural translation procedure (Bullinger et al., 1998). Our transcription and translation protocol for all materials used a systematic notation system that includes comments about the implied meaning, and a record of subtleties in meaning, alternative translations and other information (Bullinger et al., 1998). All research packets will be in the native languages of the addressee. The mailed packet included: code number; an IRB approved informational letter; a list of community endorsements; the survey; a multilingual toll-free number for questions; and a referral list of local mental health and domestic violence service providers. We used reminder cards if a survey was not returned within two weeks. Returned surveys were deemed informed consent and women who completed the survey were mailed a $10 gift card.
Analysis
The study variables include symptom type (depressive symptoms, physical symptoms), beliefs about mental illness (BMI subscales of dangerousness, embarrassment, interpersonal role, incurability, and recurrence), perceived social support, perceived need and help seeking type (medical, psychological and traditional). We carried out a descriptive analysis of variable relationships and evaluated the significance of demographic, symptom and predictor variables for inclusion in the regression modeling using bivariate regression against the outcomes of PN and Medical HS. While we generally excluded non-significant variables, we retained age and English fluency because they are described in the literature as critical to HS (Nguyen & Lee, 2012; Sentell, Shumway, & Snowden, 2007). Descriptive analyses were performed to examine how the characteristics of the participants related to the study variables. Chi-square tests were performed to examine relationships among categorical data (PN and HS Type). Multivariate logistic regression analyses were performed to identify contributors to the likelihood of engaging the use of professional services. Then, predicted probabilities were calculated to determine the impact of the predictor variables on the likelihood to perceive a need. The prediction was expressed as odds ratios (ORs) and predicted probabilities are presented in graphical form. An example of a predicted probability calculation is below (Long & Freese, 2006).
Analyses were performed with IBM SPSS (Version 22.0; IBM Corp., 2013) and R (Version 3.2.0; R Core Team, 2015). Statistical significance was considered at p < 0.05.
Results
Descriptive analysis
The number of participants with CESD scores at 16 or above (considered to be at risk for clinical depression) was 27 (13.3%), and the number of those who perceived a need for HS was 72 (34.6%). Seventy women (33.5%) had engaged in Medical HS. There were significant positive relationships between CESD and physical symptoms (r = 0.51, p < 0.01), and between CESD score and total BMI score (r = 0.21, p < 0.01). There were significant inverse relationships between CESD and age (r = −0.15, p = 0.04) and PRQ (r = −0.26, p < 0.01). There were no relationships between age and FLOSEM, between CESD and FLOSEM or between these and the length of time in the US or family income (see Table 2).
RQ1: Predicting PN.
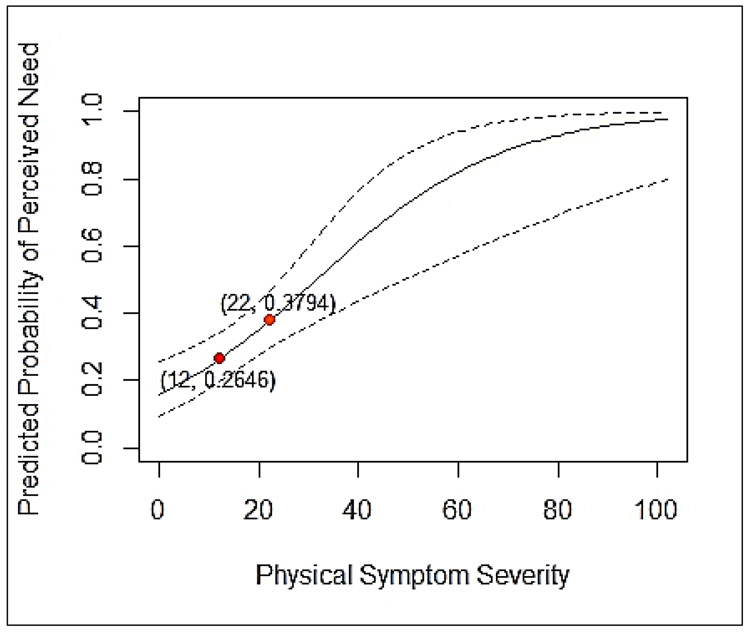
Multivariate logistic regression revealed that, while controlling for age and English fluency, women with physical symptoms were somewhat more likely to endorse PN (OR=1.05, 95% CI [1.0-1.2], p<0.00) (Table 3). The predicted probabilities of PN based on the severity of physical symptoms severity (while holding all other predictors constant) is shown in Figure 2. Using points along the slope, one can see that the predicted probability increases. For example, at physical symptom severity of 12 (four symptoms rated at three or higher), the predicted probability of endorsing PN is 26%, and with seven symptoms at three or higher, this probability that one will have PN rises to 38%.
Table 3:
Logistic Regression Analysis of Perceived Need
| Variable | Perceived Need | |||||
|---|---|---|---|---|---|---|
| B | SE B | Wald | df | p | eB | |
| Physical Symptoms | 0.05 | 0.01 | 13.94 | 1 | 0.00* | 1.05 |
| CESD | 0.002 | 0.03 | 0.01 | 1 | 0.95 | 1.00 |
| Perceived Social Resources | −0.02 | 0.02 | 0.80 | 1 | 0.37 | 0.98 |
| BMI: Interpersonal/Role | −0.02 | 0.42 | 0.003 | 1 | 0.96 | 0.98 |
| BMI: Embarrassment | 0.05 | 0.37 | 0.02 | 1 | 0.89 | 1.06 |
| BMI: Dangerousness | −0.03 | 0.42 | 0.01 | 1 | 0.94 | 0.97 |
| BMI: Recurrent | 0.48 | 0.35 | 1.95 | 1 | 0.16 | 1.62 |
| BMI: Incurability | 0.30 | 0.32 | 0.90 | 1 | 0.34 | 1.35 |
| Constant | −0.94 | |||||
| χ2 | 41.78 | |||||
| df | 10 | |||||
Notes: N = 188. Non-significant control variables (income, education, and years in the US) omitted from analysis. Significant control variables (age and English fluency) omitted from the table. Control variables are age and FLOSEM (omitted from the table). eB = exponentiated B.
Figure 2:
Predicted Probability of Help Seeking based on Perceived Need
RQ2: Relating PN to HS type.
We used chi-square analysis to examine the relationships among the categorical variables of PN (yes/no) and use of the various HS types (Medical HS, Psychological HS, or Traditional HS). For those participants with PN, 48.6% of them used Medical HS (χ2 = 11.27, p = 0.00) and 12.5 % of them used the Psychological HS (χ2 = 7.43, p = 0.01). There was no statistically significant association between PN and use of traditional medicine.
RQ3: Theoretical variables and PN in Predicting HS type.
Multivariate logistic regression revealed that when PN is considered with the other cultural variables, and while controlling for age and English fluency, PN increases the odds of Medical HS (OR=2.78, 95% CI [1.0.5.8], p<0.01). The odds of Medical HS are also increased somewhat with higher social support (OR=1.07, 95% CI [1.0-1.1], p<0.01). Finally, the presence of interpersonal stigma beliefs decreased the odds of Medical HS (OR=2.4, 95% CI [1.1-5.3] p<0.03) (see Table 4). These variables did not significantly predict any other type of help.
Table 4:
Logistic Regression Analysis of Professional Medical Help Seeking
| Variable | Professional Medical Help Seeking | |||||
|---|---|---|---|---|---|---|
| B | SE B | Wald | df | p | eB | |
| Physical Symptoms | 0.01 | 0.01 | 0.42 | 1 | 0.52 | 1.01 |
| CESD | 0.02 | 0.03 | 0.43 | 1 | 0.51 | 1.02 |
| Social Support | 0.07 | 0.03 | 6.49 | 1 | 0.01* | 1.07 |
| Perceived Need | 1.02 | 0.38 | 7.36 | 1 | 0.01* | 2.78 |
| BMI: Interpersonal/Role | 0.89 | 0.40 | 4.89 | 1 | 0.03* | 2.42 |
| BMI: Embarrassment | 0.18 | 0.35 | 0.27 | 1 | 0.61 | 1.20 |
| BMI: Dangerousness | −0.20 | 0.40 | 0.24 | 1 | 0.63 | 0.82 |
| BMI: Recurrent | −0.41 | 0.34 | 1.48 | 1 | 0.23 | 0.67 |
| BMI: Incurability | 0.24 | 0.31 | 0.64 | 1 | 0.43 | 1.28 |
| Constant | −5.16 | |||||
| χ2 | 26.53 | |||||
| df | 11 | |||||
Notes: N = 188. Non-significant control variables (income, education, and years in the US) omitted from analysis. Significant control variables (age and English fluency) omitted from the table. eB = exponentiated B.
Figure 3 shows the predicted probabilities of using Medical HS for those who endorsed PN while controlling for all other predictors. The probability of Medical HS is about 47% for the group who had PN and was 24% for those who did not.
Figure 3.
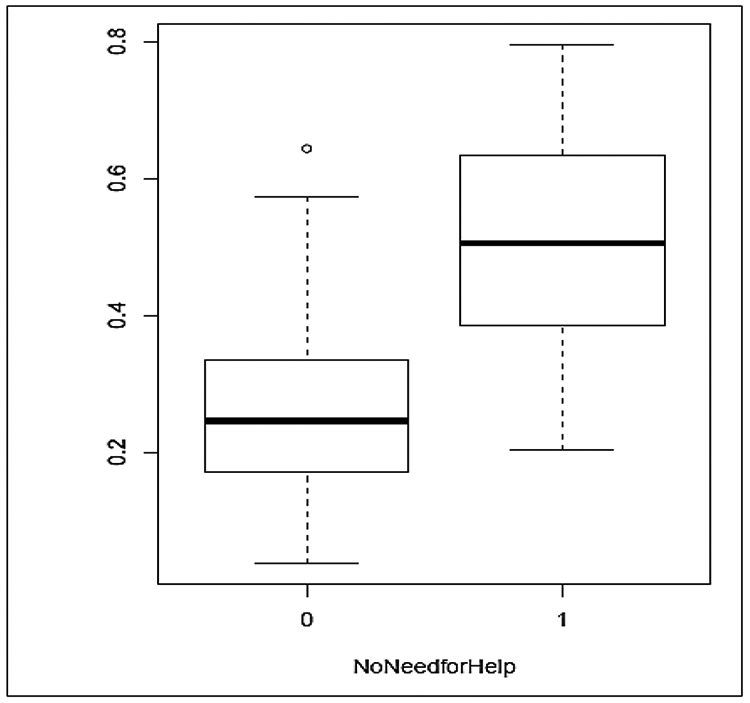
The predicted probabilities of the use of Medical intervention based on perceived need.
Discussion
Our study examined the influence of hypothesized theoretical variables on both perceived need as well as the actual use of medical and psychological services for a sample of Japanese women in the US. This study is significant because Japanese and other East Asian Immigrant women have the lowest psychological service use of any immigrant group despite significant need (Takeuchi et al., 2007; Williams, 2002; Yeung et al., 2008). Therefore, a treatment goal is to foster engagement in treatment for those in need. This research adds to the growing body of research aiming to understand the social and cultural factors that inhibit or promote service use to help mitigate internal barriers to help seeking. Specifically, for Japanese women, providers can explore the interactions among distress, the meaning of it, and concerns about the consequences of seeking care in routine primary care and social services. Moreover, the number of physical symptoms was related to perceived need in this sample. This finding suggests that providers can use the number of physical symptoms as a starting point to discuss the need for help and treatment options.
The link between perceived need and service type is a relatively new domain of exploration. For example, Lee and colleagues, examining the National Latino and Asian American Study (NLAAS) dataset found that perceived need was associated with a higher likelihood of using formal mental health services for those with high level of social support, but only for the people who immigrated as children or teens (1.5 generation) (Lee et al., 2017). However, they did not examine use of medical services. Using this same dataset, Escobar and colleagues found an association between physical symptoms and perceived need (Escobar, Cook, Chen, Gara, Alegria, et al., 2010; Escobar et al., 1987; Escobar, Rubio-Stipec, Canino, & Karno, 1989). Taken together, these studies and ours support the theory that perceived need may be an important variable in predicting service use. This finding are also consistent with our theoretical formulation that perceived need might relate to symptom type, may be moderated by cultural and social factors, and probably precedes help seeking actions. However, much more research is needed to clarify these associations. For example, exploring the associations between symptoms, perceived need, internal barriers and service use can be carried out using mixed methods to examine treatment seeking trajectories. Qualitative interviewing can be used to examine meanings and choice points, and Latent Class Analysis can explore clinically relevant subgroups.
Only the presence of physical symptom severity influenced the perception of need in our sample. We expected women with negative beliefs about mental illness would somehow self-censure their need recognition, especially if they had embarrassment or beliefs that mental illness was incurable (Crisp, 2001; Weiss et al., 1992; Weiss, Ramakrishna, & Somma, 2006). However, in our analysis, stigma beliefs only exerted a negative influence on Medical HS behavior. These patterns is consistent with our qualitative research that has shown that the Japanese women in our samples have and are aware significant symptom burden, but do not necessarily interpret those symptoms to mean that they need help or intervention (Saint Arnault & Shimabukuro, 2016). We know from qualitative work that stigma is essential to understand, and our findings help clarify that there are different types of stigma beliefs that may interact with symptom types and social network characteristics. However, when considering need, we wonder if people also evaluate the potential benefit of any given service in a context-specific way, considering symptoms and stigma and meanings, but also evaluating the specific clinic, service provider, location, clientele, and reputation.
Our study found that the presence of perceived need increased as the severity of physical symptoms increased. This finding signals to us the cultural importance of physical symptoms for this population. If this is the case, attention to the patient’s specific stated physical and emotional problems could be a pathway to mutual understanding and building a therapeutic alliance. For example, if a Japanese patient reports headaches, muscle pain, dizziness and stomach pains, providers should recognize that all these symptoms have relevance to the patient regardless of whether or not the provider understands their cultural significance. Culturally diverse populations often complain that the clinical encounter is dominated by the provider attending to a selected set of indicators, making them feel that their symptoms are not considered relevant by the provider (Yasui & Henry, 2014). Good clinical practice might include a negotiation process about the importance of all noted symptoms since the patient’s symptom experiences and beliefs may not match those offered by the provider (Benish, Quintana, & Wampold, 2011).
Estimating the clinical significance of these findings poses interesting questions. From the cultural ‘idioms of distress’ perspective, certain symptoms carry cultural meanings, and not all symptoms hold equal weight. Also, symptoms rarely stand alone, but come together with others experientially in symptom clusters. Our finding that physical symptom severity was related to both PN and Medical HS does not help us understand which symptoms might drive women to overcome stigma and seek medical care. Also, it might be that a certain set of symptoms, rather than two or three intensely experienced symptoms, that promotes perceived need or help seeking. Certain symptoms, including pain, fatigue, numbness, shortness of breath, palpitations, dizziness, and tinnitus are found in clinical practice in people from Japanese, Chinese and Korean cultures. For example, in China, the concept of neurasthenia remains an important social and cultural marker of distress (Li & He, 2018). Researchers found that Koreans (but not Americans) showed more sympathy in response to distress narratives using somatic words than narratives using emotional words (Choi, Chentsova-Dutton, & Parrott, 2016). In the Japanese, concepts such as futeisheiso and Autonomic Nervous System Dysfunction we an important part of the popular and clinical discourse through the early 2000’s, although recognition of these symptom patterns has mostly been absorbed into the psychosomatic realm (Abe, 1993; Lock, 1987; Saint Arnault, 2014; Tsutsui, 1999). The prevalence of these symptoms, the difficulty to fit them into the somatoform categories, and the cultural significance of them for patients and providers prompted the development of the International Classification of Diseases Bodily Distress Syndrome (Gureje & Reed, 2016). For our purposes here, we can see that clinical attention to physical symptoms, along with perceived need and help seeking type, can assist clinicians in listening for cultural idioms that may be important for their patients.
We found that PN, social support, and interpersonal stigma predicted Medical HS in different ways. Women with PN were much more likely to seek medical help, and it seems that social support affected that likelihood. However, fears about the social consequence (interpersonal stigma) decreased the likelihood of medical HS. This finding indicates the value of examining perceived consequences and hints that social support is in contrast to concerns about community censure. Research shows that social support and perceived social negativity (in this case, anticipated stigma) may not be opposing ends of the same spectrum. For example, in one study, higher levels of negativity within and outside of the family are each associated with higher allostatic load, but only perceived support of the spouse is associated with lower allostatic load (Brooks, Gruenewald, Karlamangla, Hu, Koretz, & Seeman, 2014). While internalized stigma beliefs may not be the same as social negativity, but it is likely that it relates to perceptions of support or negativity. Unfortunately, we did not assess social negativity in this study. However, our qualitative research has found that social negativity and stigma are connected but not the same for these Japanese women (Saint Arnault & Roels, 2012; Saint Arnault & Shimabukuro, 2016).
Limitations of this study include the small sample size, as well as the regionality of the participants. We also only sampled women for this study, and have no comparable data for men; therefore, we cannot draw any definitive conclusions from this sample. Additional work is needed to isolate clinically significant symptom clusters, add social negativity variables, and examine the aspects of the social and cultural help seeking decision-making processes that may relate to use of specific services in specific situations.
Public Policy statement: The low mental health and primary care service utilization of East Asian Immigrant Women contributes to mental health disparities in morbidity and increased suicide rates. Theorizing about the intersection of culture and service use is needed to begin to understand population-level barriers and facilitators. This theorizing allowed the discovery of the critical importance of assessing somatic distress in this population, suggesting that policies that regulate mental health assessment practice should include assessment of somatic distress as well as emotional health symptoms for immigrants.
Acknowledgments
This research was funded by the NIH Office of Behavioral and Social Sciences, the Office of Women’s Health and the National Institute of Mental Health under grant number MH071307.
Contributor Information
Denise Saint Arnault, University of Michigan School of Nursing, 400 N. Ingalls, Room 2303 Ann Arbor, Michigan USA 48109.
Seoyoon Woo, University of Michigan School of Nursing.
References
- Abe-Kim J, Takeuchi DT, Hong S, Zane N, Sue S, Spencer MS, … ,Alegría M (2007). Use of Mental Health–Related Services Among Immigrant and US-Born Asian Americans: Results from the National Latino and Asian American Study. American Journal of Public Health 97(1 ), 91–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abe T (1993). Psychosomatic Medicine and Unexplained Physical Symptoms. Japanese Journal of Psychosomatic Medicine, 33 (2), 103 (In Japanese). [Google Scholar]
- Andersen RM (1995). Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior, 36(1), 1–10. [PubMed] [Google Scholar]
- Association of Asian Pacific Community Health Organizations. (1995). Taking action: Improving access to health care for Asians and Pacific Islanders. Oakland, CA: Author. [Google Scholar]
- Bachnik J (1994). Introduction: Uchi/Soto: Challenging our concept of self, social order, and language In Bachnik JM & Quinn C (Eds.), Situated meaning: Inside and outside in Japan: self, society, and language, (pp. 3–37). Princeton: Princeton University Press. [Google Scholar]
- Benish SG, Quintana S, & Wampold BE (2011). Culturally adapted psychotherapy and the legitimacy of myth: a direct-comparison meta-analysis. Journal of Counseling Psychology, 58(3), 279. [DOI] [PubMed] [Google Scholar]
- Brooks KP, Gruenewald T, Karlamangla A, Hu P, Koretz B, & Seeman TE (2014). Social relationships and allostatic load in the MIDUS study. Health Psychology, 33(11), 1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bullinger M, Alonso J, Apolone G, Leplège A, Sullivan M, Wood-Dauphinee S, … Ware J (1998). Translating Health Status Questionnaires and Evaluating Their Quality The IQOLA Project Approach. Journal of Clinical Epidemiology, 51(11), 913–923. [DOI] [PubMed] [Google Scholar]
- Caldwell JC (1993). Health transition: the cultural, social and behavioural determinants of health in the Third World. Social Science & Medicine, 36(2), 125–135. [DOI] [PubMed] [Google Scholar]
- Choi E, Chentsova-Dutton Y, & Parrott WG (2016). The effectiveness of somatization in communicating distress in Korean and American cultural contexts. Frontiers in Psychology, 7, 383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, & Janiszewski S (1990). Who gets treated? Factors associated with referral in children with psychiatric disorders. Acta Psychiatrica Scandinavica, 81(6), 523–529. [DOI] [PubMed] [Google Scholar]
- Crisp AH (2001). Every family in the land - understanding prejudice and discrimination against people with mental illness. London: Royal Society of Medicine Press Ltd. [Google Scholar]
- De Oliveira S, & Nisbett RE (2017). Culture Changes How We Think About Thinking: From “Human Inference” to “Geography of Thought.” Perspectives on Psychological Science, 12(5), 782–790. [DOI] [PubMed] [Google Scholar]
- Dean HD, Williams KM, & Fenton KA (2013). From theory to action: applying social determinants of health to public health practice. Public Health Reports, 128(Suppl 3), 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeCieri H, Dowling P, & Taylor K (1991). The psychological impact of expatriate relocation on Partners. The International Journal of Human Resource Management., 2(3), 377–414. [Google Scholar]
- Dolatian M, Mirabzadeh A, Forouzan AS, Sajjadi H, Majd HA, & Moafi F (2013). Preterm delivery and psycho-social determinants of health based on World Health Organization model in Iran: a narrative review. Global Journal of Health Science, 5(1), 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dressler WW, & Oths KS (1997). Cultural determinants of health behavior Handbook of Health Behavior Research I: Personal and Social Determinants (Vol. 1, pp. 359–378): Plenum Press; New York. [Google Scholar]
- Escobar JI, Cook B, Chen C-N, Gara MA, Alegría M, Interian A, & Diaz E (2010). Whether medically unexplained or not, three or more concurrent somatic symptoms predict psychopathology and service use in community populations. Journal of Psychosomatic Research, 69(1), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escobar JI, Cook B, Chen CN, Gara MA, Alegria M, Interian A, & Diaz E (2010). Whether medically unexplained or not, three or more concurrent somatic symptoms predict psychopathology and service use in community populations. Journal of Psychosomatic Research, 69(1), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escobar JI, Golding J, Hough R, Karno M, Burnam MA, & Wells K (1987). Somatization in the Community: Relationship to Disability and Use of Services. American Journal of Public Health, 77(7), 837–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escobar JI, Rubio-Stipec M, Canino G, & Karno M (1989). Somatic Symptom Index (SSI): A new and abridged somatization construct: Prevalence and epidemiological correlates in two large community samples. Journal of Nervous and Mental Disease, 177(3), 140–146. [DOI] [PubMed] [Google Scholar]
- Flory M (1989). More Japanese than Japan: Adaptation and social network formation among the wives of Japanese businessmen in Bergen County, New Jersey. (Unpublished Dissertation.), Columbia University, New York. [Google Scholar]
- Garland AF, Lau AS, Yeh M, & McCabe KM (2005). Racial and Ethnic Differences in Utilization of Mental Health Services Among High-Risk Youths. The American Journal of Psychiatry, 162(7), 1336–1343. [DOI] [PubMed] [Google Scholar]
- Gureje O, & Reed GM (2016). Bodily distress disorder in ICD-11: problems and prospects. World Psychiatry, 15(3), 291–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, & Hinton DE (2014). Cross-cultural aspects of anxiety disorders. Current Psychiatry Reports, 16(6), 450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsiao A-F, Wong MD, Goldstein MS, Becerra LS, Cheng EM, & Wenger NS (2006). Complementary and alternative medicine use among Asian-American subgroups prevalence, predictors, and lack of relationship to acculturation and access to conventional health care. Journal of Alternative and Complementary Medicine, 12(10), 1003–1010. [DOI] [PubMed] [Google Scholar]
- Interian A, Lewis-Fernández R, & Dixon LB (2013). Improving treatment engagement of underserved US racial-ethnic groups: a review of recent interventions. Psychiatric Services, 64(3), 212–222. [DOI] [PubMed] [Google Scholar]
- Iwamasa GY, & Hilliard KM (1999). Depression and anxiety among Asian American elders: a review of the literature. Clinical Psychology Review., 19(3), 343–357. [DOI] [PubMed] [Google Scholar]
- Kellam SG, Branch JD, Brown CH, & Russell G (1981). Why teenagers come for treatment: A ten-year prospective epidemiological study in Woodlawn. Journal of the American Academy of Child Psychiatry, 20(3), 477–495. [DOI] [PubMed] [Google Scholar]
- Kiat N, Youngmann R, & Lurie I (2017). The emotional distress of asylum seekers in Israel and the characteristics of those seeking psychiatric versus medical help. Transcultural Psychiatry, 54(5-6), 575–594. [DOI] [PubMed] [Google Scholar]
- Kimerling R, & Baumrind N (2005). Access to specialty mental health services among women in California. Psychiatric Services, 56(6), 729–734. [DOI] [PubMed] [Google Scholar]
- Kirmayer LJ, Dao THT, & Smith A (1998). Somatization and psychologization: Understanding cultural idioms of distress In Okpaku SO (Ed.), Clinical Methods in TransculturalPsychiatry (pp. 233–265). Washington, DC: American Psychiatric Press, Inc. [Google Scholar]
- Knutson KL (2013). Sociodemographic and cultural determinants of sleep deficiency: implications for cardiometabolic disease risk. Social Science & Medicine, 79, 7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen LJ (2004). The Foreign-Born Population in the United States: 2003 Current Population Reports (Vol. P20-551). Washington, D.C.: U.S. Census Bureau. [Google Scholar]
- Lebra T (1974). Reciprocity and the asymmetrical principle: An analytic reappraisal of the Japanese concept of on In Lebra TS and Legra WP (Ed.), Japanese culture and behavior: Selected Readings. Honolulu: University of Hawaii Press. [Google Scholar]
- Lebra T (1976). Japanese patterns of behavior. Honolulu: University of Hawaii Press. [Google Scholar]
- Lee J, Donlan W, Cardoso EEO, & Paz JJ (2013). Cultural and social determinants of health among indigenous Mexican migrants in the United States. Social Work in Public Health, 28(6), 607–618. [DOI] [PubMed] [Google Scholar]
- Lee M, Takeuchi D, Gellis Z, Kendall P, Zhu L, Zhao S, & Ma GX (2017). The Impact of Perceived Need and Relational Factors on Mental Health Service Use Among Generations of Asian Americans. Journal of Community Health, 42(4), 688–700. [DOI] [PubMed] [Google Scholar]
- Li Y, & He Q (2018). The metamorphosis of medical discourse and embedded cultural rationality: a content analysis of health reporting for neurasthenia and depressive disorder in China. Asian Journal of Communication, 28(2), 170–184. [Google Scholar]
- Lin E, Goering P, Offord DR, Campbell D, & Boyle MH (1996). Use of mental health services in Ontario: Epidemiological Findings. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie, 41, 572–577. [DOI] [PubMed] [Google Scholar]
- Lin K-M, & Cheung F (1999). Mental health issues for Asian Americans. Psychiatric Services, 50(774-780). [DOI] [PubMed] [Google Scholar]
- Lock M (1987). Protests of a good wife and wise mother In Lock M & Norbeck E (Eds.), Health illness and medical care in Japan (pp. 130–157). Honolulu: University of Hawaii Press. [Google Scholar]
- Long JS, & Freese J (2006). Regression models for categorical dependent variables using Stata: Stata press. [Google Scholar]
- Luria AR (1976). Cognitive development: Its cultural and social foundations: Harvard university press. [Google Scholar]
- Ma G (1999). Access to health care for Asian Americans In Ma G & Henderson G (Eds.), Ethnicity and Healthcare: A socio-cultural approach (pp. 99–121). Springfield, Il: Charles C. Thomas. [Google Scholar]
- Min PG (Ed.). (2006). Asian Americans: contemporary trends and issues (2nd ed.). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Moscovici S, & Duveen G (1998). The history and actuality of social representations The psychology of the social (pp. 209–247). New York, NY: Cambridge University Press. [Google Scholar]
- Nguyen D, & Lee R (2012). Asian immigrants' mental health service use: An application of the life course perspective. Asian American Journal of Psychology, 3(1), 53. [Google Scholar]
- Parsons CD (1984). Idioms of distress: Kinship and sickness among the people of the Kingdom of Tonga. Culture, Medicine & Psychiatry, 8(1), 71–93. [DOI] [PubMed] [Google Scholar]
- Parsons CD, & Wakeley P (1991). Idioms of distress: Somatic responses to distress in everyday life. Culture, Medicine & Psychiatry, 15(1), 111–132. [DOI] [PubMed] [Google Scholar]
- Pescosolido BA (1992). Beyond rational choice: The social dynamics of how people seek help. American Journal of Sociology, 1096–1138. [Google Scholar]
- Rask MT, Ørnbøl E, Rosendal M, & Fink P (2017). Long-term outcome of bodily distress syndrome in primary care: a follow-up study on health care costs, work disability, and self-rated health. Psychosomatic Medicine, 79(3), 345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ro M (2002). Moving Forward: Addressing the Health of Asian American and Pacific Islander Women. American Journal of Public Health, 92(4), 516–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saint Arnault DM (2002). Help-seeking and social support in Japan Sojourners. Western Journal of Nursing Research, 24(3), 295–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saint Arnault DM (2004). The Japanese In Ember CR & Ember M (Eds.), Encyclopedia of Medical Anthropology (Vol. 1, pp. 765–776): Yale University. [Google Scholar]
- Saint Arnault DM (2009). Cultural Determinants of Help Seeking. Research and Theory for Nursing Practice, 23(4), 259–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saint Arnault DM (2014). The Mental Health System in Japan In Babb J (Ed.), Handbook of Modern Japanese Studies. Thousand Oaks, CA: Sage. [Google Scholar]
- Saint Arnault DM (2018). Defining and Theorizing about Culture: The Evolution of the Cultural Determinants of Help Seeking-Revised. Nursing Research, 67 (2), 161–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saint Arnault DM & Fetters MD (2011). RO1 Funding for Mixed Methods Research: Lessons learned from the Mixed-Method Analysis of Japanese Depression Project. Journal of Mixed Methods Research, 5(4), 309–329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saint Arnault DM & Kim O (2008). Is there an Asian idiom of distress? Somatic symptoms in female Japanese and Korean students. Archives of Psychiatric Nursing, 22(1), 27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saint Arnault DM, Sakamoto S, & Moriwaki A (2006). Somatic and Depressive Symptoms in Female Japanese and American Students: A Preliminary Investigation. Transcultural Psychiatry, 43(2), 275–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saint Arnault DM & O'Halloran S (2016). Using mixed methods to understand the healing trajectory for rural Irish women years after leaving abuse. Journal of Research in Nursing 21 (no. 5-6), 369–383 [Google Scholar]
- Saint Arnault DM& Roels DJ (2012). Social Networks and the Maintenance of Conformity: Japanese sojourner women. International Journal of Culture and Mental Health, 5(2), 77–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saint Arnault DM & Shimabukuro S (2016). Floating on Air Fulfillment and Self-in-Context for Distressed Japanese Women. Western Journal of Nursing Research, 38(5), 572–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saint Arnault DM & Woo S (2017). Cultural Barriers to Help Seeking Despite Perceived Need: Japanese Women Living in America. Archives of Psychiatric Nursing, 31(6):572–577. [DOI] [PubMed] [Google Scholar]
- Saint Arnault DM, Woo S, & Gang M (2018). Factors Influencing Mental Health Help-Seeking Behavior among Korean Women: A Path Analysis. Archives of Psychiatric Nursing, 32(1), 120–126. [DOI] [PubMed] [Google Scholar]
- Salas XR, Raine K, Vallianatos H, & Spence JC (2015). Socio-Cultural Determinants of Physical Activity among Latin American Immigrant Women in Alberta, Canada. Journal of International Migration and Integration, 1–20. [Google Scholar]
- Sentell T, Shumway M, & Snowden L (2007). Access to mental health treatment by English language proficiency and race/ethnicity. Journal of General Internal Medicine, 22(2), 289–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srebnik D, Cauce AM, & Baydar N (1996). Help-seeking pathways for children and adolescents. Journal of Emotional and Behavioral Disorders, 4(4), 210–220. [Google Scholar]
- Srinivasan S, & Guillermo T (2000). Toward improved health: Disaggregating Asian American and Native Hawaiian/Pacific Islander Data American Journal of Public Health, 90(11), 1731–1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ta VM, & Hayes D (2010). Racial Differences in the Association Between Partner Abuse and Barriers to Prenatal Health Care Among Asian and Native Hawaiian/Other Pacific Islander Women. Maternal Child Health Journal, 14(3), 350–359. [DOI] [PubMed] [Google Scholar]
- Ta VM, Juon H, Gielen AC, Steinwachs DM, & Duggan A (2007). Disparities in Use of Mental Health and Substance Abuse Services by Asian and Native Hawaiian/Other Pacific Islander Women. Journal of Behavior and Health Services Research, 35(1), 20–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeuchi DT, Hong S, Gile K, & Alegría M (2007. ). Developmental Contexts and Mental Disorders Among Asian Americans. Research in Human Development, 1(4), 49–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeuchi DT, Zane N, Hong S, Chae DH, Gong F, Gee GC, … Alegría M (2007). Immigration-Related Factors and Mental Disorders Among Asian Americans. American Journal of Public Health, 97(1), 84–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsutsui S (1999). Concept and Clinical Features of the So-called Autonomic Imbalance. The Autonomic Nervous System, 36 (1), 1–9 (In Japanese). [Google Scholar]
- U.S. Census Bureau. (2001). The Asian and Pacific Islander Population in the United States: March 2000 (Update) (PPL-146) Retrieved from http://www.census.gov/population/www/socdemo/race/api.html.
- U.S. Census Bureau. (2007). The American Community—Asians: 2004 In U. S. D. o. Commerce (Ed.), American Community Survey Reports (Vol. 05): US Census Bureau. [Google Scholar]
- U.S. Census Bureau. (2008, Page Last Modified: April 10, 2008). The Asian and Pacific Islander Population in the United States Retrieved March 1, 2018, from http://www.census.gov/population/www/socdemo/race/api.html.
- Weiss MG, Doongaji D, Siddhartha S, Wypij D, Pathare S, Bhatawdekar M, … Fernandes R (1992). The Explanatory Model Interview Catalogue (EMIC). Contribution to cross-cultural research methods from a study of leprosy and mental health. The British Journal of Psychiatry, 150(6), 819–830. [DOI] [PubMed] [Google Scholar]
- Weiss MG, Ramakrishna J, & Somma D (2006). Health-related stigma: Rethinking concepts and interventions 1. Psychology, Health & Medicine, 11(3), 277–287. [DOI] [PubMed] [Google Scholar]
- Williams DR (2002). Racial/Ethnic Variations in Women’s Health: The Social Embeddedness of Health. American Journal of Public Health, 92(4), 588–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2000). Women's Mental Health: An Evidence-Based Review In Mental Health Determinants and Populations (Ed.), (Vol. 2008). Geneva: Department of Mental Health and Substance Dependence. [Google Scholar]
- World Health Organization. (2009). Women and health: today's evidence, tomorrow's agendas. Geneva: Department of Mental Health and Substance Dependence. [Google Scholar]
- Yasui M, & Henry DB (2014). Shared understanding as a gateway for treatment engagement: A preliminary study examining the effectiveness of the culturally enhanced video feedback engagement intervention. Journal of Clinical Psychology, 70(7), 658–672. [DOI] [PubMed] [Google Scholar]
- Yeung A, Fung F, Yu SC, Vorono S, Ly M, Wu S, & Fava M (2008). Validation of the Patient Health Questionnaire-9 for depression screening among Chinese Americans. Contemporary Psychiatry, 49(2), 211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]