Abstract
Coracoid fractures are an uncommon injury and typically occur in the setting of high-energy trauma. Isolated injury to the coracoid is rare; therefore, a high suspicion for concomitant shoulder injuries should exist. These associated injuries have been shown to be acromioclavicular dislocations, clavicular and acromial fractures, scapular spine fractures, rotator cuff tears, and anterior shoulder dislocations. Although most of these shoulder injuries respond to nonsurgical treatment, there are case reports and literature reviews that present more complicated injuries requiring surgical intervention. Shoulder dislocations with associated coracoid fractures can also manifest glenoid bone loss resulting in continued instability. In this scenario, the fractured coracoid can be used to address the glenoid bone loss, as well as the continued instability. Regarding technique, other authors have described an open procedure with screw or anchor fixation. This Technical Note describes our technique for treating a displaced Ogawa type II coracoid process fracture with concomitant anterior shoulder dislocation by an arthroscopic Latarjet procedure using the fractured coracoid.
Coracoid fractures are uncommon and comprise 2% to 13% of all scapular injuries.1,2 Typically, they occur from high-energy direct trauma such as a motor vehicle collision or fall from a height.2,3 Ogawa et al.4 reviewed 67 patients with fractures of the coracoid process and classified them based on the relation between the fracture site and the coracoclavicular (CC) ligament. Fractures located proximal to the CC ligaments are classified as type I, whereas those fractures located distal to the CC ligament are classified as type II. Treatment of these fractures is based on fracture type and displacement. Isolated type II fractures with minimal displacement can be treated conservatively, whereas displaced type II fractures and most type I fractures should be treated surgically.5 In their review article, Galvin et al.2 highlighted the lack of high-quality evidence available to guide treatment, with only Level IV and V evidence available in the literature. Their recommendation is to pursue surgical management for coracoid fractures associated with an unstable superior shoulder suspensory complex, displaced extension into either the scapular body or glenoid fossa, or progression into a painful nonunion. The most common method of surgical fixation of coracoid fractures is screw fixation; however, Kennedy et al.6 reported good outcomes in their case report using suture anchors.
Isolated injury to the coracoid is rare, and definitive treatment should take concomitant shoulder injuries into account. In their case report, Verma et al.7 acknowledged the rarity of shoulder instability with coracoid fracture, citing only 10 known cases in the English-language literature. Ogawa et al.4 and Knapik et al.1 showed that acromioclavicular dislocations, clavicular and acromial fractures, scapular spine fractures, rotator cuff tears, and anterior shoulder dislocations are all commonly associated with coracoid injury. Identifying coracoid fractures can be difficult because most are nondisplaced and can be missed on radiographs. Galvin et al.2 recommended maintaining a high clinical suspicion and obtaining magnetic resonance imaging (MRI) or computed tomography (CT) with 3-dimensional reconstruction to define fracture displacement and morphology.
The Instability Severity Index Score developed by Boileau and Balg8 is used to select patients at high risk of recurrent dislocation after a soft-tissue procedure alone. This score can be used to help dictate treatment for patients with a coracoid fracture and concomitant shoulder instability.8 The case report by Cottias et al.9 described an open Latarjet procedure for treatment of persistent instability in a patient with a greater tuberosity fracture, coracoid fracture, and anterior glenoid bone loss in 1 shoulder after bilateral shoulder dislocation. Schneider et al.10 reported a successful outcome in a patient with chronic anterior shoulder instability and avulsion fracture of the coracoid treated with an open Latarjet procedure.
This Technical Note describes our technique for treating a displaced Ogawa type II coracoid process fracture with concomitant anterior shoulder dislocation, instability, and a fragmented bony Bankart lesion using an arthroscopic Latarjet procedure.
Surgical Technique
Video 1 presents an overview of this technique with narration.
Preoperative Examination
Plain-film imaging shows a minimally displaced fracture at the base of the coracoid with an associated bony Bankart lesion of the anterior inferior glenoid, with loss of contour to the anterior glenoid rim (Fig 1). MRI findings show the fracture of the coracoid; the bony Bankart lesion, which is fragmented; and a Hill-Sachs lesion (Fig 2). The CT scan of the shoulder again shows the bony Bankart lesion, similar to the MRI scan; however, the glenoid track is found to be smaller than that of the Hill-Sachs lesion, therefore making this an off-track lesion, as described by Di Giacomo et al.11 (Figs 3 and 4).
Fig 1.
Radiographic axillary view of left shoulder showing displacement of coracoid fracture (red arrow), bony Bankart lesion, and loss of anterior glenoid contour (yellow arrow).
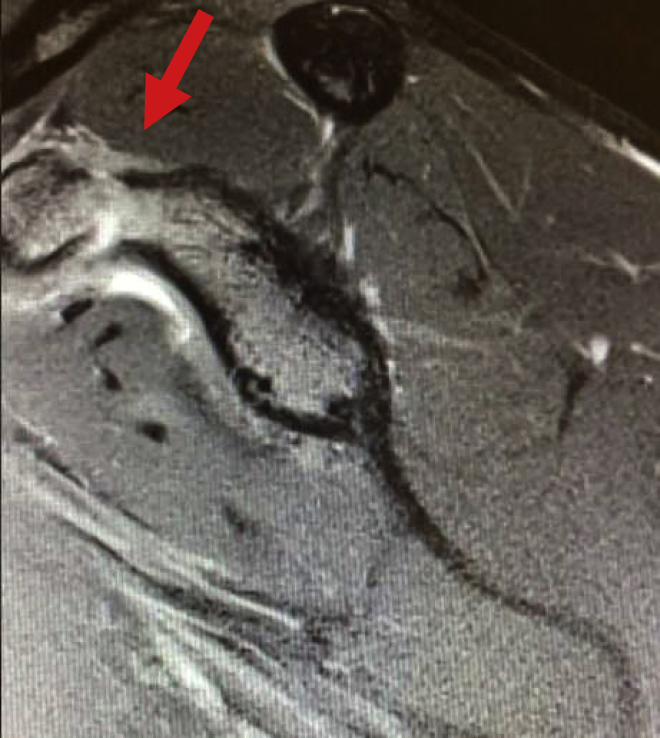
Fig 2.
Sagittal T2 magnetic resonance imaging of left shoulder showing edema surrounding coracoid base fracture (red arrow).
Fig 3.
Axial T2-weighted magnetic resonance image of left shoulder showing displaced bony Bankart lesion (red arrow).
Fig 4.
Three-dimensional reconstruction (A) and axial imaging (B) from computed tomography scan of left shoulder showing anterior bone loss (red arrow), as well as fracture of coracoid base (green arrows).
Patient Positioning and Anesthesia
The patient is placed in the supine position on the operating table, and general anesthesia is used for induction. Single-shot or catheter-infusion regional anesthesia can be used for improved postoperative pain control. Perioperative antibiotic prophylaxis is administered intravenously before incision. The patient is then placed in the modified beach-chair position, with care taken to pad all bony prominences (Fig 5). The head and neck should be carefully placed in the neutral position and slightly turned toward the contralateral shoulder. An arm positioner (Spider; Smith & Nephew, Andover, MA) is placed at the head of the bed out of the way while working in the anterior shoulder space. We find the arm positioner to be a helpful tool during the procedure. Once the patient is appropriately positioned, the arm is prepared and draped in a meticulous sterile fashion.
Fig 5.
The patient is placed in the modified beach-chair position with the right shoulder exposed and the portal sites labeled for reference only (red arrow). [Courtesy of Matthew Ravenscroft, M.B.B.S., F.R.C.S.(Tr&Orth).]
Arthroscopic Latarjet Technique
Anatomic landmarks are drawn, and portal sites A, D, E, H, M, and J are marked in accordance with the portals for the arthroscopic Latarjet technique as described by Lafosse and Boyle12 (Fig 5). A slightly medialized posterior portal (portal A) is used, and a standard diagnostic arthroscopy is conducted to assess the 15 points of Snyder.13 The anterior portal (portal E) is made through the rotator interval under visualization with an outside-in technique. After confirmation that the bony Bankart lesion is not viable, the anterior labrum and anterior rim of the glenoid are debrided and skeletonized using a radiofrequency wand (VAPR Suction Electrode; DePuy Synthes, Raynham, MA) and shaver (Excaliber; Arthrex, Naples, FL). The bony Bankart lesion is visualized and removed. If there is a significant amount of glenoid bone loss and engagement of the humeral head, a Latarjet procedure that uses the fractured coracoid is appropriate.
Next, the joint capsule is opened using the VAPR device, exposing the subscapularis tendon through portal E. The rotator interval is cleaned out to find the coracoid. The coracoacromial ligament is partially removed. The medial sling of the biceps is not removed to prevent medial biceps instability. Next, portal D is created 1 cm lateral and inferior to the anterolateral corner of the acromion to gain a better view of the anterior structures. Visualization from this portal provides a view of anterosuperior and anteroinferior bone loss (Fig 6). The anterior and posterior space around the subscapularis is then carefully defined using a radiofrequency ablator and shaver. The axillary nerve is encountered inferior and medial to the coracoid in its predictable position. Once the axillary nerve has been found, dissection can continue, staying lateral to its location. Portals D and E are used until the coracoid is clearly defined.
Fig 6.
Arthroscopic visualization of left anterior glenoid rim from portal D (anterolateral portal), with patient placed in modified beach-chair position, showing anterosuperior and anteroinferior bone loss of glenoid (red arrow).
Portals M and J are then developed (Fig 5) and used to better define the conjoint tendon and pectoralis minor. The coracoacromial ligament is removed off the coracoid, leaving the conjoined tendon attached. Next, the scope is placed in portal J to view the axis of the coracoid process. A switching stick through portal D is used to retract the superior deltoid and improve visualization of the coracoid. A spinal needle is used to determine the location of portal H over the coracoid (Fig 7). This portal comes down directly over the coracoid. Through this portal, the coracoid drill guide (DePuy Synthes) can be placed. Correct placement of the K-wires must be confirmed. The alpha hole on the coracoid drill guide must be approximately 1 cm proximal to the tip of the coracoid process. The beta hole of the coracoid drill guide is placed appropriately in the center of the coracoid from medial to lateral. The guide can be removed, and the coracoid drill is used over the guidewires in the alpha and beta positions.
Fig 7.
Arthroscopic visualization of left coracoid from portal J (placed midway on arc between portals M and D), with patient placed in modified beach-chair position, showing skeletonized coracoid on profile (red arrow) and spinal needle showing location for portal H (yellow arrow) directly superior to coracoid.
Next, the subscapularis split is created. A switching stick is placed through the posterior portal across the glenoid face and into the subscapularis to define the appropriate position. The previously made portal A is slightly medialized for this portion of the case. Because of its position, the switching stick lies directly on the glenoid face. The subscapularis split is made at the union between the superior two-thirds and inferior one-third of the tendon into the muscle in the same plane as the future graft site location. The split is made using the radiofrequency ablator until the glenoid is appropriately exposed. Care must be taken to avoid injury to the axillary nerve while completing the split medially. In addition, it is important to carefully dissect the subscapularis split with the radiofrequency ablator to prevent iatrogenic injury to the humeral head cartilage. The conjoint tendon can also be visualized medial to the longitudinal split. The anterior glenoid is then prepared to accept the graft using the shaver and burr (BLURR; Arthrex). It is important to make sure there is no soft-tissue interposition on the glenoid neck to prevent nonunion of the graft.
Next, the coracoid osteotomy is performed. The osteotomy is made using straight and curved osteotomes through portal H. It is important to burr circumferentially around the proximal coracoid to serve as a stress riser before making the osteotomy. This prevents the osteotomy from fracturing into the scapular body. Once the osteotomy is completed, 2 coracoid screws are placed into the alpha and beta holes of the post-osteotomy coracoid through portal M using a graft handle (DePuy Synthes). Decortication of the inferior coracoid, as well as any bone off the inferior aspect of the proximal coracoid, is performed to allow for a better fit on the glenoid neck. The coracoid is then mobilized through the subscapularis split. The switching stick from the posterior portal is used to widen the split and facilitate mobilization of the graft through the subscapularis until reaching the prepared glenoid neck.
The scope is placed back into portal J, and the coracoid is placed in the desired position on the anterior rim of the glenoid in the 2- to 5-o’clock position. The graft is lined up with the subchondral bone roughly 3 to 4 mm medial to the glenoid cartilage. Once the surgeon is satisfied with the position, a K-wire can be drilled through the cannulated coracoid screw in the alpha hole across the glenoid until it penetrates out the posterior shoulder through the skin, where it is clamped. Clamping the wire prevents retrograde advancement of the wire back into the shoulder. This process is repeated for the beta hole in the same fashion. The coracoid screw is then removed from the alpha hole, and a 3.2-mm drill is used over the wire into the glenoid. Next, the length is measured, and an appropriate-length Latarjet cortical screw (4.5 mm; DePuy Synthes) is placed over the wire into the coracoid and glenoid. This process is repeated for the beta hole. To prevent malpositioning or fracture of the graft, it is important to not completely tighten either screw initially. Once provisional fixation is completed, it is paramount to alternate between the screws until final fixation is completed (Fig 8). Fixation should be assessed through multiple views, along with confirmation of no soft-tissue interposition. Table 1 is a compilation of pearls and pitfalls to consider while performing this surgical technique. Postoperative radiographs are obtained to evaluate the position of the graft with proper screw positioning (Fig 9).
Fig 8.
Arthroscopic visualization of left anterior glenoid rim from portal J (placed midway on arc between portals M and D), with patient placed in modified beach-chair position, showing coracoid graft fixation to glenoid in 2- to 5-o’clock position with 4.5-mm cannulated screws (red arrow).
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Use an arm positioner that is placed at the head of the bed. | When cleaning out the rotator interval and removing part of the coracoacromial ligament, be careful not to remove the medial sling of the biceps because this can lead to medial biceps instability. |
| Drape out the entire shoulder quarter to prevent contamination of the K-wire once it penetrates the skin posteriorly. | Burr circumferentially around the proximal coracoid prior to osteotomy to prevent fracture propagation into the scapular body. |
| Medialize portal A (posterior portal) slightly to aid in localization of the subscapularis split; this allows a co-plane relation to the glenoid. | Once provisional fixation of the graft is complete, tighten the screws in alternating fashion so as not to malposition or fracture the graft. |
| Clamp the K-wire once it is drilled out of the posterior shoulder to prevent retrograde advancement back into the shoulder. | Take care when visualizing the neurologic structures (i.e., axillary and musculocutaneous nerves) to avoid injury. |
| Decorticate the anterior glenoid and inferior coracoid to assist in bony healing. | Bear in mind that it is important to have a clean bony bed for the graft and confirm no soft-tissue interposition is preventing graft healing. |
Fig 9.
Postoperative radiographic axillary view (A) and scapular-Y view (B) of left shoulder showing intact coracoid graft and proper screw placement (red arrows) postoperatively. (L, left.)
Postoperative Rehabilitation
The patient is placed in a padded abduction shoulder sling that is best able to place the arm as close to a neutral position as possible. The immediate postoperative protocol consists of pendulum exercises and biceps isometrics for 2 weeks. After 2 weeks, formal physical therapy is initiated with passive range of motion (ROM), advancing to active-assisted ROM and then active ROM. A follow-up CT scan is performed at 3 months to evaluate for a healed coracoid fracture and healed graft to the anterior glenoid (Fig 10). If both are present, the patient is allowed to return to sport with no restrictions at 3 months postoperatively.
Fig 10.
Computed tomography scan with 3-dimensional reconstruction and humeral subtraction at 3 months postoperatively showing incorporation of graft (red arrow) in left shoulder.
Discussion
Although rare, coracoid injury due to high-energy trauma and sporting activity has been described in the literature. Benchetrit and Friedman14 reported the first case of a fractured coracoid process associated with an anterior dislocation of the humeral head. The 28-year-old patient underwent closed reduction and was treated conservatively in a Velpeau bandage for 2 weeks. After 8 weeks, the patient had full ROM of the shoulder with normal strength.
Ogawa et al.4 reported on a cohort of 67 patients with coracoid fractures. They looked at associated injuries and their relation to coracoid fracture type, finding that acromioclavicular dislocations were the most commonly associated lesion, observed in 60 of 67 patients. Another 14 patients had clavicular fractures; of these fractures, 12 occurred laterally. All of these patients had type II coracoid fractures. Anterior shoulder dislocations and rotator cuff tears were noted in 3 patients each. All 6 of these patients had type I fractures. All 31 type I fractures (including anterior shoulder dislocations) and 3 unstable type II fractures were treated with open reduction–internal fixation with a malleolar screw in the coracoid process and percutaneous pin fixation for either acromioclavicular dislocation or clavicular fracture. No statistically significant difference between the operative and nonoperative groups or between type I and type II fractures was found.4
Knapik et al.1 conducted a systematic review of the literature from 1970 to 2017 looking at the prevalence of coracoid fractures sustained during sporting activities, as well as management and outcomes of treatment. They found 21 cases of coracoid fractures sustained during sporting activity, with 16 of these due to acute trauma; the remainder were fatigue fractures. Nonoperative management was used in 16 patients, with 3 of 16 reporting complications: One patient had subcoracoid impingement that was treated with physiotherapy, and another had nonunion that was treated with an electric bone-stimulating device. The third complication was a published case report by Chammaa et al.15 They described a patient in whom anterior shoulder instability developed and who required arthroscopic bony Bankart repair.1,15 The review by Knapik et al. showed that return to sport was not statistically different based on fracture mechanism, management, or the presence or absence of acromioclavicular joint injury.
The uniqueness of this pathology involves the associated anterior shoulder instability sustained after anterosuperior dislocation during sport. The literature shows that isolated coracoid fractures have good outcomes when treated conservatively. However, a significant proportion of those with concomitant shoulder injury that were treated conservatively required future surgical intervention. The case reports by Cottias et al.9 and Schneider et al.10 showed good outcomes when performing an open Latarjet procedure in patients with coracoid fractures and associated anterior shoulder instability. Aggressive workup and treatment should be conducted in those with coracoid injury because concomitant shoulder injury necessitating surgical intervention is likely. This includes the use of advanced imaging to better understand the pathology.
One of the disadvantages of the described technique is that it is technically demanding and there is a learning curve associated with performing an arthroscopic Latarjet procedure. Valsamis et al.16 conducted a multiple-surgeon, international, large-volume evaluation of the arthroscopic Latarjet procedure using a continuous learning curve analysis. They reported that experienced shoulder surgeons with prior open Latarjet experience should expect to complete 30 to 50 arthroscopic procedures to attain steady-state operative efficiency. Cerciello et al.17 performed a systematic review and meta-analysis evaluating the early outcomes and perioperative complications of the arthroscopic Latarjet procedure; they reported a higher complication rate and longer operative time with the arthroscopic technique that both seemed to be reduced with increased surgeon experience. Their study noted similar mid-term functional outcomes, reoperation rates, and recurrence rates when comparing the open versus arthroscopic approach.17 Table 2 summarizes advantages and disadvantages of this described technique. On the basis of its technically demanding nature, our technique might be limited to surgeons who perform arthroscopic Latarjet procedures in high volumes.
Table 2.
Advantages and Disadvantages
| Advantages |
| Addresses pain and instability of both glenoid bone loss and coracoid fracture |
| Less morbidity than open technique |
| Possible decreased risk of neurologic injury compared with open Latarjet procedure owing to absence of significant soft-tissue retraction and direct visualization of key structures |
| Easy identification and treatment of associated lesions |
| Potentially faster rehabilitation |
| Offers opportunity to see structures and areas of shoulder not seen with open procedure |
| Disadvantages |
| Increased surgical difficulty with arthroscopic technique; steep learning curve |
| Increased OR time and possibly less accurate graft positioning during learning curve |
| Inability to re-tension capsule due to removal for visualization with arthroscopic technique |
| More difficult osteotomy of coracoid graft |
OR, operating room.
Future prospective studies that evaluate patient outcomes based on coracoid fracture patterns and the presence of concomitant shoulder injuries such as anterior shoulder dislocation need to be completed to better understand this fracture and injury pattern. The described technique is our preferred method to successfully treat a type II coracoid fracture with an unstable, off-track anterior shoulder dislocation.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: S.K.B. is a consultant for Johnson & Johnson. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Step-by-step narrated technique for management of traumatic coracoid fracture and anterior shoulder instability with modified arthroscopic Latarjet technique. The patient is in the modified beach-chair position, and the left arm is held in an arm positioner that is placed at the head of the bed.
References
- 1.Knapik D.M., Patel S.H., Wetzel R.J., Voos J.E. Prevalence and management of coracoid fracture sustained during sporting activities and time to return to sport. Am J Sports Med. 2018;46:753–758. doi: 10.1177/0363546517718513. [DOI] [PubMed] [Google Scholar]
- 2.Galvin J.W., Kang J., Ma R., Li X. Fractures of the coracoid process: Evaluation, management, and outcomes [published online May 7, 2020]. J Am Acad Orthop Surg. https://doi.org/10.5435/JAAOS-D-19-00148 [DOI] [PubMed]
- 3.Gottschalk H.P., Browne R.H., Starr A.J. Shoulder girdle: Patterns of trauma and associated injuries. J Orthop Trauma. 2011;25:266–271. doi: 10.1097/BOT.0b013e3181e47975. [DOI] [PubMed] [Google Scholar]
- 4.Ogawa K., Yoshida A., Takahashi M., Ui M. Fractures of the coracoid process. J Bone Joint Surg Br. 1997;79:17–19. doi: 10.1302/0301-620x.79b1.6912. [DOI] [PubMed] [Google Scholar]
- 5.Ogawa K., Matsumura N., Ikegami H. Coracoid fractures: Therapeutic strategy and surgical outcomes. J Trauma Acute Care Surg. 2012;72:E20–E26. [PubMed] [Google Scholar]
- 6.Kennedy N.I., Ferrari M.B., Godin J.A., Sanchez G., Provencher M.T. Repair of an isolated coracoid fracture with suture anchor fixation. Arthrosc Tech. 2017;6:e1715–e1719. doi: 10.1016/j.eats.2017.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Verma N., Chahar D., Chawla A., Sreenivasan R., Pankaj A. Recurrent anterior instability of the shoulder associated with coracoid fracture—An unusual presentation. J Clin Orthop Trauma. 2016;7(suppl 1):99–102. doi: 10.1016/j.jcot.2016.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boileau P., Balg F. The instability severity index score: A simple pre-operative score to select patients for arthroscopic or open shoulder stabilization. J Bone Joint Surg Br. 2007;89-B:1470–1477. doi: 10.1302/0301-620X.89B11.18962. [DOI] [PubMed] [Google Scholar]
- 9.Cottias P., le Bellec Y., Jeanrot C., Imbert P., Huten D., Masmejean E.H. Fractured coracoid with anterior shoulder dislocation and greater tuberosity fracture—Report of a bilateral case. Acta Orthop Scand. 2000;71:95–97. doi: 10.1080/00016470052943982. [DOI] [PubMed] [Google Scholar]
- 10.Schneider M.M., Balke M., Koenen P., Bouillon B., Banerjee M. Avulsion fracture of the coracoid process in a patient with chronic anterior shoulder instability treated with the Latarjet procedure: A case report. J Med Case Rep. 2014;8:394. doi: 10.1186/1752-1947-8-394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Di Giacomo G., Itoi E., Burkhart S.S. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: From “engaging/non-engaging” lesion to “on-track/off-track” lesion. Arthroscopy. 2014;30:90–98. doi: 10.1016/j.arthro.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 12.Lafosse L., Boyle S. Arthroscopic Latarjet procedure. J Shoulder Elbow Surg. 2010;19:2–12. doi: 10.1016/j.jse.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 13.Snyder SJ, Fasulo GJ. Shoulder arthroscopy: surgical technique. Surg Technol Int 1993;2:447-453. [PubMed]
- 14.Benchetrit E., Friedman B. Fracture of the coracoid process associated with subglenoid dislocation of the shoulder. A case report. J Bone Joint Surg Am. 1979;61:295–296. [PubMed] [Google Scholar]
- 15.Chammaa R., Miller D., Datta P., McClelland D. Coracoid stress fracture with late instability. Am J Sports Med. 2010;38:2328–2330. doi: 10.1177/0363546510371370. [DOI] [PubMed] [Google Scholar]
- 16.Valsamis E.M., Kany J., Bonnevialle N. The arthroscopic Latarjet: A multisurgeon learning curve analysis. J Shoulder Elbow Surg. 2020;29:681–688. doi: 10.1016/j.jse.2019.10.022. [DOI] [PubMed] [Google Scholar]
- 17.Cerciello S., Corona K., Morris B.J., Santagada D.A., Maccauro G. Early outcomes and perioperative complications of the arthroscopic Latarjet procedure: Systematic review and meta-analysis. Am J Sports Med. 2019;47:2232–2241. doi: 10.1177/0363546518783743. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Step-by-step narrated technique for management of traumatic coracoid fracture and anterior shoulder instability with modified arthroscopic Latarjet technique. The patient is in the modified beach-chair position, and the left arm is held in an arm positioner that is placed at the head of the bed.