Abstract
Subchondral acetabular edema and cysts, as a consequence of degenerative changes of the hip, are associated with disability, pain, and worsened function in this joint. The arthroscopic treatment of intra-articular pathologies, such as femoroacetabular impingement syndrome and labral tears, when associated with those alterations, has been suggested to provide inferior outcomes to those in patients without subchondral changes. Yet, the direct treatment of subchondral pathology has been limited. Recently, a technique for insufflating bone substitute into the bone marrow lesions of the knee, Subchondroplasty (Zimmer Knee Creations, Exton, PA), has led to promising results. Subchondroplasty has raised attention as a possible minimally invasive procedure to treat cystic changes in the acetabulum in patients who are not yet candidates for hip replacement. We present the technique of acetabular Subchondroplasty, in which a bone substitute material is injected into subchondral acetabular cysts under fluoroscopic guidance. In this technique, hip arthroscopy is used in conjunction with fluoroscopic guidance to address intra-articular pathologies and assess for possible intra-articular extravasation of the injectable material.
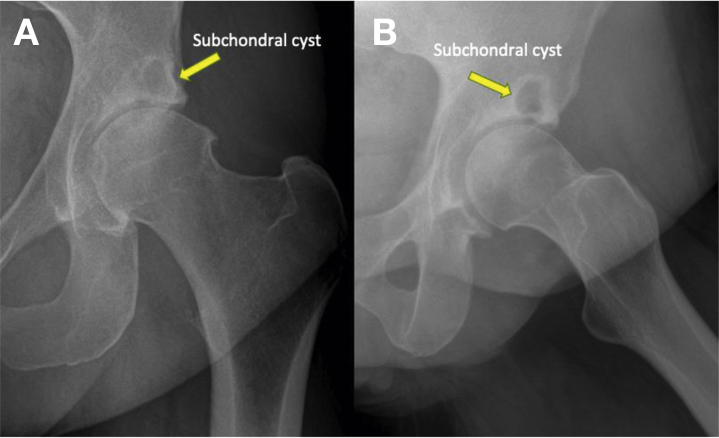
The presence of subchondral degenerative cysts in the acetabulum is a common finding in patients with advanced hip osteoarthritis and an indication for total hip replacement.1 However, subchondral bone cysts in the acetabulum also may be found in a subset of patients presenting with hip pain without radiographic signs of advanced hip osteoarthritis (Fig 1). This subchondral cystic degeneration is associated with increased pain, disability, and functional impairment. When associated with intra-articular pathologies such as femoroacetabular impingement (FAI) syndrome or labral tears, the arthroscopic treatment of these pathologies presents inferior outcomes compared with hip arthroscopy for treating FAI and labral tears alone.2,3
Fig 1.
Preoperative anteroposterior (A) and Dunn (B) radiographs of a left hip in a patient with hip pain, showing the presence of an important subchondral bone cyst of the acetabulum, without significant joint space narrowing.
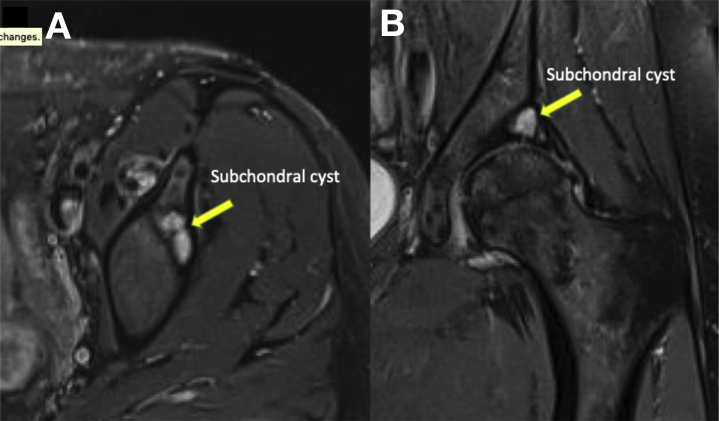
In the early stages, subchondral acetabular bone cysts may not be readily appreciated on conventional radiographs. Magnetic resonance imaging (MRI) is advocated as the best imaging modality to detect these bone marrow lesions (BMLs) (Fig 2). In addition, MRI is better able to visualize acetabular and femoral cartilage and other soft tissues around the hip that may be contributing to the patient's hip pain.2
Fig 2.
Axial (A) and coronal (B) views of fat-suppressed magnetic resonance imaging of a left hip in a patient with left hip pain. Magnetic resonance imaging is used for preoperative planning for the Subchondroplasty, showing the localization of the cyst in the anterosuperior region of the acetabulum.
There are 2 main theories that explain the mechanism for the formation of subchondral cysts. In the first theory, increased intra-articular pressure leads to intrusion of synovial fluid into the subchondral bone through cartilage loss or fissured cartilage.4 The second theory states that subchondral cysts are the sequelae of traumatic bone necrosis after the impact of 2 articulating cartilage surfaces,5 which could explain why some patients with cam-type FAI syndrome often present with associated acetabular bone cysts. In particular, prior histologic analyses of bone cysts revealed a histologic appearance consistent with a nonhealing chronic stress fracture and loss of mechanical integrity in the region of the BML.6,7 In accordance with these 2 theories, Subchondroplasty (Zimmer Knee Creations, Exton, PA) may provide mechanical support and remodeling of the insufficient subchondral bone by injection of a flowable calcium phosphate void filler with osteoconductive properties into the bone cyst. Subchondroplasty has previously shown promising results in BMLs of the knee and is an appealing procedure to treat subchondral bone cysts in the acetabulum.6,8, 9, 10
We present the technique of acetabular Subchondroplasty with the injection of AccuFill bone substitute material (BSM; Zimmer Knee Creations) using fluoroscopic and arthroscopic guidance to treat acetabular subchondral bone cysts in patients with subchondral disease and relatively preserved joint space (Video 1).
Surgical Technique
Patient Positioning
The patient, under general anesthesia, is positioned supine on a traction table (Advanced Supine Hip Positioning System; Smith & Nephew, Andover, MA) with a well-padded perineal post to avoid pudendal nerve and genital injuries. The operative limb is placed in 20° of flexion, 45° of internal rotation to maximize the femoral neck length, and neutral adduction and abduction. Traction is gently applied to the limb until 10 mm of joint space is obtained and confirmed on fluoroscopic imaging to allow access to the central compartment of the hip. The operative field is sterilized, and the patient is draped.
Portal Placement and Intra-articular Assessment
Access to the hip joint is obtained through the anterolateral (AL) and midanterior arthroscopic portals. A 70° arthroscope (Stryker Endoscopy, San Jose, CA) is inserted into the midanterior portal, and the working tools are inserted into the AL portal. A diagnostic arthroscopy is performed, chondral lesions are stabilized to stable margins, and any degenerative labral pathology is debrided using a 4.5-mm shaver (Stryker, Kalamazoo, MI). Because patients undergoing this procedure usually present with some degree of arthritis, we do not usually perform labral repair, acetabular trimming, and femoral osteoplasty.
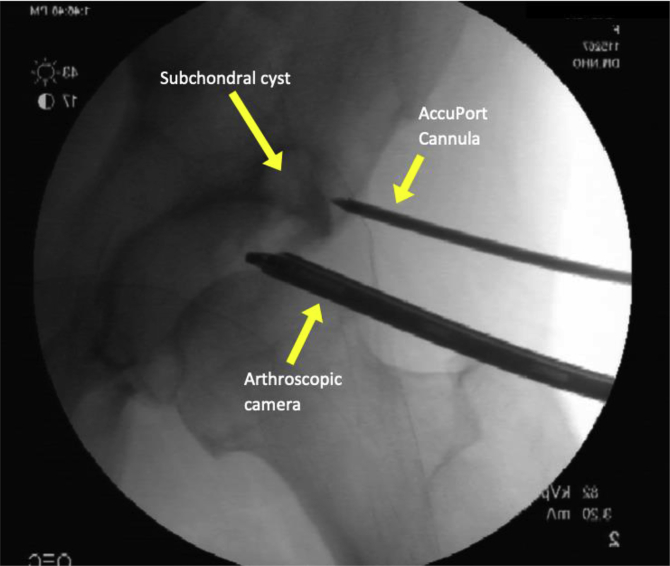
Subchondroplasty
After intra-articular pathologies have been addressed, the working tools are retrieved from the AL portal and the camera is kept in the midanterior portal. By use of the same skin incision used for the AL portal, the AccuPort cannula (Zimmer Knee Creations, West Chester, PA) is drilled into the subchondral bone cyst with a wire driver, parallel to the articular surface, under fluoroscopic guidance (Fig 3). The cannula is inserted according to the preoperative planning based on fat-suppressed MRI views and under direct visualization with the camera to prevent cartilage disruption with the cannula. It is important to check the proper positioning of the cannula with more than 1 incidence of fluoroscopic guidance to avoid injecting the bone substitute outside the cyst cavity.
Fig 3.
Fluoroscopic view of the AccuPort cannula being inserted into the subchondral cyst in a left hip with a wire driver. The arthroscopic camera is inserted through the midanterior portal. Proper positioning of the cannula, confirmed with fluoroscopy and direct visualization through the arthroscopic camera, is important to avoid injecting the bone substitute outside the cyst cavity.
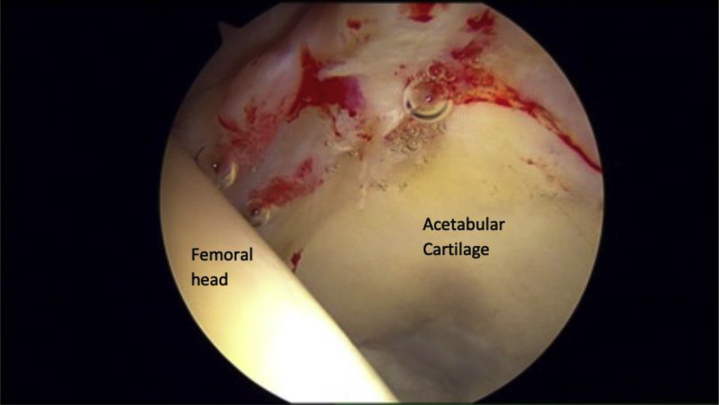
AccuFill BSM (SCP Knee Kit; Zimmer Knee Creations) is prepared by mixing calcium phosphate powder with saline solution in a mixing device until a homogeneous paste is obtained. The paste is then divided into 5 injecting syringes. The inner stylus of the cannula is removed, and the fluid bone substitute is injected into the cyst under fluoroscopic guidance and intra-articular visualization through the camera until back pressure is felt in the syringe (Fig 4). At this point, the surgeon should stop injecting the AccuFill to avoid overfilling the cyst, which is a cause of immediate postoperative pain. The stylus is reinserted into the cannula and left in place for 10 minutes so that the paste can crystallize and harden under an endothermic reaction that occurs only at body temperature. If extravasation of the bone substitute into the hip joint occurs, the extravasated material can be debrided and removed with the shaver.
Fig 4.
Intra-articular visualization of a left hip during injection of calcium phosphate bone substitute with the camera through the midanterior portal. It is possible to visualize cartilage degeneration underneath the area of the subchondral bone cyst. When back pressure is felt in the syringe, the surgeon should stop injecting the bone substitute material to avoid overfilling the cyst, which is a cause of immediate postoperative pain. In this case, no extravasation of the paste occurs.
The cannula is retrieved, traction is released, and skin incisions are closed routinely. A well-padded bandage is applied over the incisions and left for 24 hours to absorb water from the procedure. Anteroposterior radiographs are obtained 2 weeks after the procedure to verify proper filling of the acetabular cyst (Fig 5).
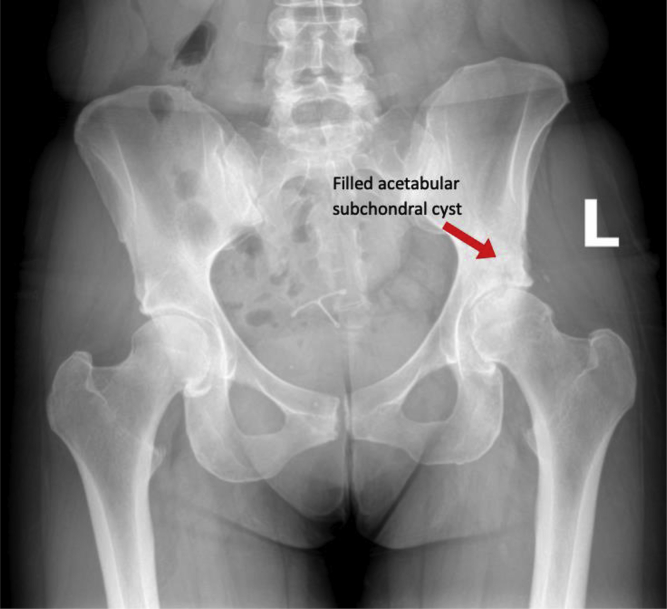
Fig 5.
Anteroposterior radiograph of the hips 2 weeks after the procedure, showing important filling of the subchondral cyst with the calcium phosphate bone substitute material in the left (L) hip.
Postoperative Rehabilitation
The patient is allowed partial weight bearing (20 lb) with crutches for 2 weeks and progresses to full weight bearing for 2 more weeks. Double-leg strengthening is initiated on postoperative day 1 and is maintained for a 6- to 12-week period, together with unrestricted range-of-motion exercises, until adequate strength and full range of motion are obtained.
Discussion
In this Technical Note we have presented a safe and minimally invasive technique to treat subchondral acetabular bone cysts in patients with complaints of hip pain and dysfunction, with early hip osteoarthritis and maintained joint space. In a cross-sectional study, Kumar et al.2 showed that patients with subchondral cysts in the acetabulum reported increased pain, symptoms, disability, and functional impairment when compared with patients without cysts. In addition, they showed that patients with cartilage lesions in the acetabulum had a higher prevalence of BMLs and subchondral cysts. This finding may be an explanation for why patients with acetabular cartilage degeneration have worse outcomes after arthroscopic hip surgery for labral tears or FAI than patients without acetabular cartilage lesions.3,11,12 However, Egerton et al.12 highlighted that hip arthroscopy should still be considered for patients with initial degrees of cartilage degeneration but without significant joint space narrowing.
In this regard, we have found that patients with acetabular bone cysts with complaints of hip pain and disability benefit from arthroscopic Subchondroplasty in the treatment of periacetabular cysts. Through the injection of a viscous, synthetic calcium phosphate bone substitute into the cyst, with osteoconductive properties, the insufficient subchondral bone regains mechanical support and bone remodeling occurs over time. As a result, pain and function are potentially improved in this subset of patients. Corroborating this theory, some studies have reported improved short-term outcomes in patients undergoing Subchondroplasty for the treatment of tibial and femoral BMLs of the knee. In a series of 12 patients who underwent knee Subchondroplasty, Chua et al.8 reported 1-year improvements from baseline of 7.5 to 2.1, 47.8 to 14.3, and 38.5 to 73.2 in visual analog scale pain scores, Western Ontario and McMaster Universities Osteoarthritis Index scores, and Knee Injury and Arthritis Outcome Scores, respectively. In a series of 5 patients undergoing the same procedure, Bonadio et al.9 similarly reported significant improvements in Knee Injury and Arthritis Outcome Scores and visual analog scale pain scores, from 38.4 and 7.8, respectively, at baseline to 71.2 and 0.6, respectively, at 2-year follow-up.
Besides presenting good short-term outcomes, Subchondroplasty has been shown to be a safe surgical procedures. The studies on knee Subchondroplasty have reported 1 case of cannula breakage inside the bone due to excessive manipulation, 1 case of intra-articular extravasation of the paste, 1 case of deep vein thrombosis, and 1 case of postoperative infection.6,8,9 With respect to acetabular Subchondroplasty, the main risks of the procedure are postoperative pain due to overfilling the cyst, which can be avoided by careful injection of the paste, and intra-articular extravasation of the bone substitute, which should be debrided with a shaver, followed by thorough articular irrigation.
There are limitations to acetabular Subchondroplasty that should be taken into account when selecting patients for this procedure. In particular, patients with advanced articular degeneration and significant joint space narrowing may have poorer outcomes after acetabular Subchondroplasty and should not be considered candidates for this procedure.
In conclusion, in our initial experience, Subchondroplasty of the hip appears to be an effective and safe procedure to treat acetabular bone cysts in well-selected patients. Table 1 summarizes the pearls and pitfalls of this technique.
Table 1.
Pearls and Pitfalls of Acetabular Subchondroplasty
| Pearls |
| Preoperative assessment of the cyst location with MRI is paramount for correct placement of the cannula. |
| Positioning of the cannula in the acetabulum must be performed under 2 incidences of fluoroscopic guidance. |
| Intra-articular visualization with the arthroscope through the AL portal during injection is mandatory to assess possible BSM extravasation. |
| Pitfalls |
| Holding the syringes for a long time should be avoided. The calcium phosphate hardens in an endothermic reaction at body temperature. |
| After feeling some resistance, the surgeon should not keep injecting the paste. Overfilling the cyst is a cause of immediate postoperative pain. |
| Proper patient selection is key for achieving good outcomes. Patients with advanced osteoarthritis may not benefit from the procedure. |
BSM, bone substitute material; MRI, magnetic resonance imaging.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: S.N. receives research support from Allosource, Arthrex, Athletico, DJ Orthopaedics, Linvatec, Miomed, Smith & Nephew, and Stryker; serves on the editorial/governing board of the American Journal of Orthopedics; is a board/committee member of the American Orthopaedic Society for Sports Medicine and Arthroscopy Association of North America; receives intellectual property royalties from Ossur; is a paid consultant for Ossur; and receives publishing royalties and financial/material support from Springer, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Technique for performing acetabular Subchondroplasty. The patient is supine on the traction table; the operative hip is the left hip. Intra-articular assessment is performed through the anterolateral and midanterior portals and an interportal capsulotomy. Intra-articular pathology is addressed via midanterior viewing and anterolateral working portals. The cannula is drilled into the subchondral bone cyst with a wire driver under fluoroscopic guidance. The AccuFill bone substitute material is then prepared and inserted into the cyst through the cannula, under fluoroscopic guidance and direct visualization through the camera in the midanterior portal, to assess whether any extravasation of the paste occurs. After the paste hardens, the cannula is retrieved and traction is released.
References
- 1.Rees R.J., Hill S.O., Cassar-Pullicino V., Cool P. The incidence, location and distribution of degenerative subchondral acetabular cysts in primary osteoarthrosis of the hip. Hip Int. 2004;14:24–27. doi: 10.1177/112070000401400103. [DOI] [PubMed] [Google Scholar]
- 2.Kumar D., Wyatt C.R., Lee S. Association of cartilage defects, and other MRI findings with pain and function in individuals with mild-moderate radiographic hip osteoarthritis and controls. Osteoarthritis Cartilage. 2013;21:1685–1692. doi: 10.1016/j.joca.2013.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krych A.J., King A.H., Berardelli R.L., Sousa P.L., Levy B.A. Is subchondral acetabular edema or cystic change on MRI a contraindication for hip arthroscopy in patients with femoroacetabular impingement? Am J Sports Med. 2016;44:454–459. doi: 10.1177/0363546515612448. [DOI] [PubMed] [Google Scholar]
- 4.Landells J.W. The bone cysts of osteoarthritis. J Bone Joint Surg Br. 1953;35-B:643–649. doi: 10.1302/0301-620X.35B4.643. [DOI] [PubMed] [Google Scholar]
- 5.Rhaney K., Lamb D.W. The cysts of osteoarthritis of the hip; a radiological and pathological study. J Bone Joint Surg Br. 1955;37-B:663–675. doi: 10.1302/0301-620X.37B4.663. [DOI] [PubMed] [Google Scholar]
- 6.Cohen S.B., Sharkey P.F. Subchondroplasty for treating bone marrow lesions. J Knee Surg. 2016;29:555–563. doi: 10.1055/s-0035-1568988. [DOI] [PubMed] [Google Scholar]
- 7.Taljanovic M.S., Graham A.R., Benjamin J.B. Bone marrow edema pattern in advanced hip osteoarthritis: Quantitative assessment with magnetic resonance imaging and correlation with clinical examination, radiographic findings, and histopathology. Skeletal Radiol. 2008;37:423–431. doi: 10.1007/s00256-008-0446-3. [DOI] [PubMed] [Google Scholar]
- 8.Chua K, Kang JYB, Ng FDJ, et al. Subchondroplasty for bone marrow lesions in the arthritic knee results in pain relief and improvement in function [published online November 21, 2019]. J Knee Surg. https://doi.org/10.1055/s-0039-1700568. [DOI] [PubMed]
- 9.Bonadio M.B., Giglio P.N., Helito C.P., Pécora J.R., Camanho G.L., Demange M.K. Subchondroplasty for treating bone marrow lesions in the knee—initial experience. Rev Bras Ortop. 2017;52:325–330. doi: 10.1016/j.rboe.2017.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tofighi A., Rosenberg A., Sutaria M., Balata S., Chang J. New generation of synthetic, bioresorbable and injectable calcium phosphate bone substitute materials: Alpha-bsm, Beta-bsmTM and Gamma-bsmTM. J Biomimet Biomat Tissue Eng. 2009;2:39–55. [Google Scholar]
- 11.Streich N.A., Gotterbarm T., Barié A., Schmitt H. Prognostic value of chondral defects on the outcome after arthroscopic treatment of acetabular labral tears. Knee Surg Sports Traumatol Arthrosc. 2009;17:1257–1263. doi: 10.1007/s00167-009-0833-x. [DOI] [PubMed] [Google Scholar]
- 12.Egerton T., Hinman R.S., Takla A., Bennell K.L., O'Donnell J. Intraoperative cartilage degeneration predicts outcome 12 months after hip arthroscopy. Clin Orthop Relat Res. 2013;471:593–599. doi: 10.1007/s11999-012-2594-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technique for performing acetabular Subchondroplasty. The patient is supine on the traction table; the operative hip is the left hip. Intra-articular assessment is performed through the anterolateral and midanterior portals and an interportal capsulotomy. Intra-articular pathology is addressed via midanterior viewing and anterolateral working portals. The cannula is drilled into the subchondral bone cyst with a wire driver under fluoroscopic guidance. The AccuFill bone substitute material is then prepared and inserted into the cyst through the cannula, under fluoroscopic guidance and direct visualization through the camera in the midanterior portal, to assess whether any extravasation of the paste occurs. After the paste hardens, the cannula is retrieved and traction is released.