Abstract
Introduction
The interaction between military and civilian healthcare systems has contributed to the development of medical care. Swedish innovations such as the Seldinger technique for angiography, Leksell Gamma Knife for cranial surgery, and the introduction of pacemakers and ultrasound have contributed to the global development of medicine. Several authors have described the Swedish civilian healthcare system and its development. However, the development and history of its military healthcare system and its influence on the civilian healthcare system remain untold. This review aims to describe the historical development of the Swedish military healthcare system and its path toward civilian-military collaboration and a total defense healthcare system.
Material and Methods
A search for all published scientific papers in Swedish and English, along with available legal documents and directives, was made. We used CINAHL, PubMed, Scopus, and Gothenburg University’s databases and search engines. The following keywords, Swedish, military, civilian, healthcare, collaboration, and development, were searched for, alone or in combination, using a PRISMA flow chart. Duplicates, abstracts, and nonscientific publications were excluded.
Results
Each of the four distinct periods of historical development in the Swedish military healthcare system can be characterized by the changes necessary for transforming Sweden from an aggressive to a defensive and collaborative nation, with national and international engagement. Collaboration not only encompasses readiness and willingness to share resources and information, and to adjust routines and guidelines, but also needs a culture of consensus and respect for each other’s limitations and capabilities. The definition of military medicine and the military physician’s role in Sweden is imperative for further civilian-military collaboration.
Conclusions
Recent global sociopolitical changes necessitate civilian-military healthcare collaboration. Although civilian-military healthcare partnerships in various medical fields have been reported earlier, the Swedish concept of total defense’s healthcare system integration and collaboration may be a more fruitful approach. The collaboration within the total defense healthcare system will result in technical achievements, innovations, and medical advancements for the benefit of the whole nation.
Introduction
The interaction between military and civilian healthcare systems has contributed to the development of medical care. It was during the Napoleonic Wars in the early nineteenth century that the organized form of military healthcare appeared. The use of ambulances during combat (ambulance volante), the introduction of triage, and the use of field hospitals a few miles back from the battlefield were all important factors in the development of military medicine. The need to support troops over long distances contributed to the development of medical logistics. The introduction of new evacuation systems and principles of resuscitation and trauma management from the point of injury is another important step that has gradually increased the survival rates in the military population. All these contributions have since then been disseminated successfully within the civilian healthcare system by physicians and others, many of whom were serving reservist physicians.1–4
Swedish innovations have contributed to the global development of medicine. Olof Rudbeck discovered the lymph vessels in 1652. Nils Rosén von Rosenstein published the first textbook in pediatric medicine and initiated the use of medical records in daily hospital care. Carl von Linné, a botanist, zoologist, and physician, became the father of modern taxonomy.5,6 Seldinger introduced the modern technique for angiography.7 The Gamma Knife for cranial surgery8 and pacemakers and ultrasound were introduced in medicine in the 1950s and 1970s, respectively.9,10 Omeprazole was introduced in the twentieth century.11 Several authors have described the advancement of the Swedish civilian healthcare system,12 but there are few, if any, descriptions regarding the development of the Swedish military healthcare system. Such a report can be of interest since, as a neutral country, Sweden has not been involved in a declared conflict for the last 200 years (since 1814), yet is actively engaged in multinational peacekeeping missions.
The objective of this review is to describe the Swedish military healthcare system’s path toward civilian-military collaboration from a historical point of view and the current policy aiming at civilian-military collaboration and total defense healthcare.
Method and Material
A search for all published scientific papers in Swedish and English, along with available legal documents and directives, was made. We used CINAHL, PubMed, Scopus, and Gothenburg University’s databases and search engines. The following keywords, Swedish, military, civilian, healthcare, collaboration, and development, were searched for, alone or in combination, using the PRISMA flow chart.13Figure 1 shows the process of search and the number of hits in each step. Duplicates, abstracts, and nonscientific publications were excluded.
Figure 1.
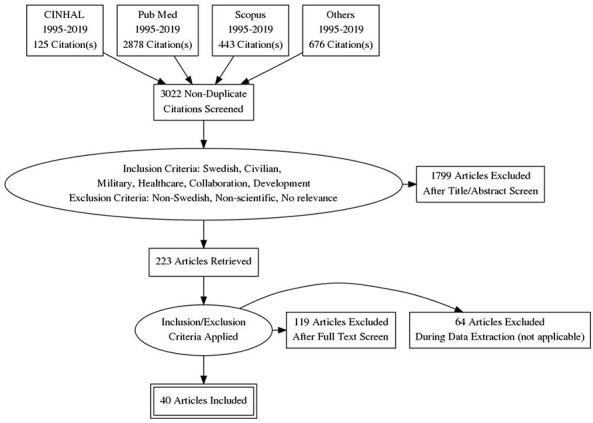
Flow diagram showing database outputs and selection of included studies for both objectives based on the PRISMA flow diagram.11
Results
Historically, the development of Swedish civilian and military healthcare has been closely associated and can be divided into four distinct periods: (1) war period (before 1814–1911), (2) peace and development period (1813–1911), (3) period of neutrality and international engagement (1912–1945), and (4) period of civilian-military collaboration (1946 to current).
Swedish Military Healthcare Before 1814: The War Period
During this period, Sweden was constantly involved in wars with all neighboring countries. The treatment of war injuries and of infectious disease was practiced by both monks and barbers. The monks’ influence on surgery declined gradually, allowing the barbers to practice surgery by performing different tasks such as cutting beard and hair, phlebotomy, tooth extractions, and drainage of abscesses in the civilian population.14,15 During the wars in the sixteenth to nineteenth centuries, there were increasing demands for amputation, abdominal procedures, and other surgical interventions. The military forces hired barbers for the care of the casualties.16 However, since the barbers found it risky to follow on military campaigns and often refused the task, they were often themselves forced to enlist.
Uppsala University recognized medicine as an academic specialty in the 1600s, and as a result the number of trained physicians gradually increased. In 1663, the newly founded Swedish Collegium Medicum received the task of opposing quacks and charlatanism within the medical profession. A few years later, they were given the responsibility of licensing medical and pharmacy graduates and, in 1685, supervision of surgical education.15 However, they had no authority to supervise the barbers’ skills and knowledge.
As a result of the plague epidemic (1710–1713) and several outbreaks of measles, the Serafimer hospital opened in Stockholm in 1752 to serve the whole country. The war with Russia in the late 1780s led to a new era in Swedish military healthcare, since infectious diseases and surgical conditions dominated the causes of death among soldiers.14,15 The barbers’ limited knowledge and lack of insight regarding field conditions resulted in a suggestion to set up temporary educational institutions for the training of field surgeons (1789–1808). As a result, the Karolinska Institute was formed in 1810, with the task of setting up a 2-year training program, after which the participants could work as interns in the field. They were also allowed to continue their medical studies after the war. The same year the Collegium Medicum was divided into civilian and military divisions,16 a garrison hospital was built, and two new professors were installed: one in medicine and the other in the surgery.14–16
Swedish Military Healthcare Between 1814 and 1911: Peace and Development Period
At the beginning of the nineteenth century, the Swedish economy deteriorated, due to internal social issues, though there were no concerns about external threats. After several years of wars, the new foreign policy known as the Policy of 1812 resulted in a long period of peace and development after 1814. Collegium Medicum was modernized in 1813, and a new medical organization, “Sundhetskollegium,” consisting of four divisions, civilian healthcare, military healthcare, obstetric and vaccination care, and pharmaceutical division, was formed. In 1878, Medicinalstyrelsen replaced Sundhetskollegium and was gradually given a broader task for the supervision of other areas such as public health, veterinary care, dental care, forensic medicine, etc.14,16,17
With the birth of the Red Cross and the Geneva Convention, voluntary activities started in different countries, including Sweden. The official position of the Swedish Government was not to get involved in armed conflict. However, Swedish physicians and nurses actively participated through various help organizations in other armed conflicts such as the Danish-German War (1864), the Franco-German War (1870–1871), and the Boer War (1899–1902). The knowledge, as well as the experience they gained, was later used at home.18
According to the reigning Swedish policy, military healthcare and hospitals aimed to provide medical care for the Swedish army. Nevertheless, the introduction of more efficient weapons (eg, machine guns) which caused more severe injuries and greater numbers of casualties forced the armies in several countries, including Sweden, to build military hospitals and hire specialist doctors to manage trauma.16 Garrison hospitals in Linköping, Karlsborg, Sollefteå, Stockholm, Skövde, and Boden and the regiment hospital in Södermansland were built during this period. The size and the characteristics of these hospitals depended on the prevailing sociopolitical conditions. They were all eventually closed after WW2.14–16,18–20
Swedish Military Healthcare Between 1912 and 1945: Period of Neutrality and International Engagement
Its position as a neutral country during WWI and WWII gave Sweden an opportunity to develop social welfare and healthcare systems. The introduction of air raids into warfare, causing both military and civilian casualties, initiated the development of civil defense, that is, a more formalized approach to civilian-military cooperation. The first report recommending civilian-military collaboration in war was published in 1936, and a plan was delivered 1 year later. However, the partnership did not start until the end of WWII. In 1940, the first preparedness department was established within the Medicinalstyrelsen, and a link between civilian and military healthcare was established by creating a position as defense assistant. The task of the department was further developed to become the healthcare preparedness committee (SBN = Sjukvårdens beredskapsnämnd).17
Swedish volunteers continued their involvement, and considerable medical and nonmedical support was offered to victims of the war.21 Numerous voluntary physicians and nurses participated in the Balkan War (1912–1913) by joining the Swedish Red Cross. The most significant activity during the WW1 was the establishment of a Swedish hospital in Vienna (1917–1918) with around 400 beds. The Swedish contribution in the Finnish Civil War (1918) was the four-staffed ambulances from the Swedish Red Cross. In this war, another voluntary organization, “Swedish Red Star,” offered veterinary help. In 1937, 12 Swedish physicians, medical students, and nurses took part in the Second Italo-Ethiopian War (1935–1937). The Spanish Civil War gathered many participants through the Swedish Red Cross and other voluntary organizations such as the Swedish-Spanish Help Organization. A hospital was gradually built with 700 beds to offer medical care to both military and civilian casualties. During WWII, as many as 102 Swedish physicians worked within different units abroad. The establishment of war hospitals in Visby (1939–1945), Lärbo (1942–1945), Hemse (1939–1945), and Klinte (1939–1945) offered care for victims of the war, including many refugees. One of the most reported activities of a Swedish voluntary organization during WWII was the so-called white buses, which saved the lives of many refugees held in camps, by transferring them to Sweden.18,19,22
Although Sweden never got directly involved in any of these wars, the knowledge and experience gained by voluntary healthcare professionals could be used in civilian healthcare after their return. It also helped to organize better medical assistance in other conflicts such as in the Korean War, where through the Swedish Red Cross, 170 Swedish healthcare staff joined the American and South Korean medical teams to take care of the military personnel and casualties. The Swedish mission continued by offering healthcare services to the Korean civilian population. The Korean mission inspired many of the participants who also took part in later United Nations missions, such as in Congo.18
Swedish Military Healthcare Since 1945: Toward Civilian-Military Collaboration
Because of the growing risk of nuclear conflict during the Cold War, the Swedish defense policy was based on both national defense and involvement in international peacekeeping missions. However, the main aim was to defend the Swedish territory from invasion.
National Preparedness
Several years of discussions and investigations after WWII resulted in the creation of a medical disaster committee in 1965. Its main task was to increase Swedish preparedness for unexpected incidents and disasters by issuing recommendations and guidelines. Three years later, the National Board of Health and Welfare was established to cover all areas of health and social care in peace and war, which implied collaboration with the armed forces. This collaboration developed gradually from 1969 to reach its peak in 1980 with regular meetings, planning, and mutual projects.17
The national preparedness implied that most of the national resources would be immediately ready for use after a rapid mobilization. Several preparedness hospitals (civilian buildings that could be converted into hospitals) were created, where medical equipment, supplies, etc. were stored. Additionally, a civil defense system with the responsibility of protecting the civilian population during the war was created. Many shelters were built, extensive plans for the evacuation of the people from urban areas were made, and stockpiles of food, fuel, drugs, etc. were created. The program was estimated to involve 2.8 million people after a full mobilization in the early 1980s.14–17,23,24 The provision of medical care in this plan was the subject of several investigations. As an example, a government’s report proposed to give military medicine a position as a medical specialty of its own and to require such competence for holding certain positions within the military healthcare system. Also, the report proposed the establishment of research programs in the military to deal specifically with military medical issues. Finally, a small number of permanent employees were recruited as senior executives in military medicine to create career development opportunities, enhance recruitment of medical staff, and stimulate military healthcare.23,24
International Missions
From the late 1960s, the Cold War became less cold, and the risk for Swedish involvement in armed conflicts was considered less likely. Thus, Swedish preparedness was reduced significantly. Some of the 50+ field hospitals and naval combat hospitals that the Swedish Armed Forces (SAF) had in their possession were used in various international assignments. The remaining facilities were dismantled around the turn of the millennium due to the collapse of the Warsaw Pact and the Soviet Union. The reduced risk of large-scale armed conflicts on European soil led to a new era in Swedish military healthcare strategy and organization.14,23,24 The new defense policy aimed to build Sweden’s security abroad in coalition with forces from other nations. The result was Sweden’s participation in major peacekeeping operations such as the Bosnian War as part of the United Nations Protection Force (Former Yugoslavia) UNPROFOR, the war in Afghanistan as part of the International Security Assistance Force (ISAF), the Libyan Civil War, and the ongoing conflict in Mali.15,24,25 Simultaneously SAF was significantly reduced in size and went from conscript service to employ only professional staff.
International missions need risk assessment and preventive measures; thus, medical intelligence and preventive medicine had to be developed. New medical treatment facilities were built based on modular units to be used nationally or internationally during armed conflicts as well as in humanitarian missions. Most of the medical staff were hired part-time, combining both civilian and military careers. In addition to their civilian skills, that is, skills equivalent to advanced trauma life support (ATLS), they also needed basic military training, as well as military trauma-focused specialized training, for example, Battlefield Advanced Trauma Life Support (BATLS) and Definitive Surgical Trauma Care (DSTC).20,24,25 All soldiers were trained to use tourniquets as well as some medications such as fentanyl in the prehospital setting. In each group of eight soldiers, a “combat lifesaver” (CLS) was included, given 7 weeks of additional medical training and who carried more medical equipment. Registered nurses staffed military ambulances. Furthermore, physicians staffed ambulance helicopters, as well as light maneuver units (NATO Role 2LM), forward surgical teams (FST), and field hospitals (NATO Role 2). For hospital care following repatriation, the SAF signed an agreement with one of the university hospitals in the Stockholm region (NATO Role 4 hospital). Strategic evacuation (Stratevac) of injured Swedish soldiers was included in the contract, to be carried out by a civil aviation operator with the support of a medical team from the hospital. Admitted patients were to be transferred to their county hospitals, as soon as their medical condition permitted. The latter were responsible for further care, including rehabilitation, prosthetic care, psychological support, etc.24,25
A New Era and New Scenarios: Toward Civilian-Military Healthcare Collaboration
The political tension in Europe has increased during the last decade.25,26 Russia has upgraded and expanded its military forces. Conflicts in Georgia, Ukraine, and Syria have proved that nations are capable and willing to use military force to gain political goals. In Sweden, the reduction of in size of the SAF, including the military healthcare system, has impaired the capability to handle military casualties resulting from a possible armed attack on Sweden itself. This responsibility thus became the challenge for the civilian healthcare system. However, the civilian healthcare system has during the same period reduced the number of hospital beds by >50% due to strained finances and associated technological developments and has changed from stockpiling to same-day delivery of supplies. Thus, there is an obvious need for collaboration between the civilian and military healthcare systems.26,27 Consequently, the SAF and the National Board of Health and Welfare initiated the project “total defense’s healthcare system” in 2015.27 The project aimed to identify risks, vulnerabilities, and measures needed to provide the necessary medical care in the event of major incidents, disasters, and wars. Within the framework of the collaboration, the authorities have developed a concept for civilian-military coordination in planning, education, skills provision, and resources to increase the national capacity. Furthermore, there is the intention to develop national plans for trauma and emergency medical education, support and focus on research through the Knowledge Centers for Disaster Medicine, and the development of national guidelines for multi-professional exercises and training. The project report provides a basis for continued dialogue with relevant stakeholders such as the government, authorities, and healthcare professionals and initiates a new era in the development of Swedish military healthcare system.27
Discussion and Conclusion
Each of the four distinct periods of historical development in the Swedish military healthcare system was characterized by the changes necessary for transferring Sweden from an offensive to a defensive and collaborative nation, with national and international engagement, to finally achieve the conditions required for successful civilian-military collaboration and the concept of total defense healthcare.14–18,28 Although the partnership encompasses readiness and willingness to share resources and to adjust routines and guidelines, it also needs a culture of consensus and respect for each other’s limitations and capabilities.29 Although associated with challenges, interorganizational collaboration is an essential factor in effective crisis and disaster management. One of the main characteristics of the Swedish civilian disaster and crisis response system is its firm emphasis on shared and collaborative actions,30 a concept that has developed during a long period of peace, sociopolitical stability, and civil defense improvement. The first plan for civilian-military collaboration was published in the late 1930s, yet it took many years of partnership, discussion, and meetings until the beginning of the twenty-first century to harmonize such concert.17 A fruitful and fair healthcare collaboration encompasses all major nonmedical and medical elements of crisis management such as command, control, communication, information sharing, standard treatment guidelines, routines, etc.27,31,32
There are medical and nonmedical contact points and challenges for future Swedish civilian-military collaboration.24,26,27,31,32 These discouraging factors must be reviewed, and proper actions should be implemented to enhance civilian-military collaboration. Interactive training and education might be one way to stimulate a fruitful collaboration between civilian and military healthcare systems. The SAF has participated in joint simulation exercises with civilian healthcare. Such a partnership allows both systems to identify strengths and weaknesses in their networks and to use their resources favorably. It also increases their ability to understand each other’s limitations as well as capabilities and respect the areas of responsibilities. Besides organizational rapprochements, professional development can be achieved by mutual medical courses, simulation exercises, and linking military medicine and military healthcare staff to academia.24,27,32 The latter also provides a new opportunity for military medicine-related research activities.31,33 Defense funding of research in physiology, trauma, emergency medicine, public health, preventive medicine, and other areas of mutual interest not only increases the readiness of the military forces but also benefits the Swedish civilian healthcare system.31
From a Swedish perspective, military operational activity cannot be maintained without an integration between military and civilian healthcare philosophy.31,34 Having that in mind, the current Swedish approach to integration and collaborative work is logical for the proper use of resources, sharing knowledge, and determination of responsibilities and limitations. Such integration also has a profound impact on guidelines and procedures as well as the choice of equipment to support the most critically injured in the military context. Investing in all aspects of civilian healthcare development, including research and recognition of military medicine, as part of integration policy, is an essential step that needs plans, time, and policy discussion and constitutes the foundation for a total defense healthcare system.31,34 In defining military medicine as “a specialty consisting of all forms of medicine, such as military emergency care, military traumatology, military occupational and environmental medicine, veteran care, medical intelligence, as well as medical leadership and administration,” the primary task of military medicine remains to maintain the combat readiness of the troops.
Consequently, besides surgical procedures as an essential part of military medicine, combat-related injuries also require prehospital care as well as transport to a qualified medical facility, medical intelligence, preventive medicine, emergency and daily medical care, as well as rehabilitation.35–37 These areas constitute potential areas of collaboration between the civilian and military healthcare systems.24,27,31 Furthermore, medical intelligence follows the process of risk identification, assessment, and management, which is an essential part of disaster and major incident management.38
Despite earlier recommendations,22,23 military medicine has not yet been established as a specialty in Sweden. There are some common denominators between the tasks of the military and civilian healthcare systems. These denominators are mutually interdependent, but the successful accomplishment of any one of them depends upon the efficient performance of the others.27,31,33,34 The definition of military medicine and the military physician’s role in Sweden is imperative for further civilian-military collaboration. The collaboration within the total defense healthcare system will result in technical achievements, innovations, and medical advancements for the benefit of the whole nation.
In conclusion, recent global sociopolitical changes necessitate civilian-military healthcare collaboration. Although subject-related civilian-military healthcare partnerships have been reported earlier,39,40 the Swedish concept of healthcare systems’ integration and collaboration may be a more fruitful approach, which demands a long period of stability, peace, and a culture of collaboration and consensus.41
AK conceived the idea for the manuscript, undertook the literature review, and wrote the draft. All authors, contributed, studied and approved the final draft of the manuscript.
The views expressed are solely those of the authors and do not reflect the official policy or position of the Swedish Armed Forces, the Department of Defense, or the Swedish Government.
References
- 1. Van Way C, III: War and trauma: a history of military medicine. Mil Med 2016; 113(4): 260–3. [PMC free article] [PubMed] [Google Scholar]
- 2. Lim Meng K: Military Medicine through the Ages . Available at https://www.mindef.gov.sg/oms/content/dam/imindef_media_library/graphics/pointer/PDF/2017/MED50/MED50_A1.pdf; accessed January 2020.
- 3. Grissinger JW: The development of military medicine. Annal N Y Acad Med 1927; 3(5): 301–36. [PMC free article] [PubMed] [Google Scholar]
- 4. Zimble J: Military medicine: an operational definition. Mil Med 1996; 161(4): 183–8. [PubMed] [Google Scholar]
- 5. Fransson SG: Profiles in cardiology. Clin Cardiol 1997; 20: 974–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Uppsala Universitet Kort Historik—Personalgalleri. Available athttps://medfarm.uu.se/vetenskapsomradet/fakulteter-och-institutioner/kort-historia/; accessed January 2020.
- 7. Greitz T: Sven-Ivar Seldinger. Am J Neuro Radiol 1999; 20(6): 1180–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. International Parkinson and Movement Disorder Society Available at https://www.movementdisorders.org/MDS/About/Committees--Other-Groups/Special-Interest-Groups/Neurosurgery-Special-Interest-Group/Pioneer-Surgeon-Lars-Leksell.htm; accessed January 2020.
- 9. Thulesius O: Pacemakern-ett av medicinens stora framsteg-fyller 50 år. Lakartidningen 2008; 24: 1871–1872. Available at http://www.lakartidningen.se/Functions/OldArticleView.aspx?articleId=9719; accessed January 2020. [PubMed] [Google Scholar]
- 10. Medicinska Fakulteten-Lund Universitet Inge Edler och Helmuth Hertz. Available athttps://www.medicin.lu.se/om-fakulteten-institutionerna/fakultetens-historia/inge-edler-och-hellmuth-hertz;accessed January 2020.
- 11. Moldéus P, Berlin RG, Castagnoli N Jr, Carlssson E: P450=Losec. Correspondence. Gastroenterology 1991; 100(5): 1488–9. Available at https://www.gastrojournal.org/article/0016-5085(91)90834-8/pdf; accessed January 2020. [PubMed] [Google Scholar]
- 12. Anell A, Glenngard AH, Merkur S: Sweden health system review. Health Syst Transit 2012; 14(5): 1–159. [PubMed] [Google Scholar]
- 13. Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group : Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6(7): e1000097. doi: 10.1371/journal.pmed1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gustafsson RÅ: Traditionernas ok-Den svenska hälso-och sjukvårdens organisering i historie-sociologiskt perspektiv. ESSELTE STUDIUM AB. Gummessons Tryckeri AB, Falköping, 1987.
- 15. Gustafsson T: Medicin och krig—Svenska erfarenheter från sjukvårdsarbete i utländska konflikter. Socialmedicinsk tidskrift 2012; 1: 26–34. [Google Scholar]
- 16. Lindberg BS. Kirurgernas Historia. Om badare, barberare och fältskärer. Uppsala, Kph Trycksaksbolaget, 2017. [Google Scholar]
- 17. Socialstyrelsen : Den civila hälso-och sjukvårdens beredskapens utveckling- några återblickar. SoS 1999-00-014, SoS arkiv, 1998.
- 18. Bro T. Återställandets konst-Svenska frivilliga läkares erfarenheter av militärmedicine i utländska krig 1864–1964, Doctoral Dissertation Series. Lund, Lund University: Faculty of Medicine, 2017. [Google Scholar]
- 19. Swedish National Archives : Riksarkivet. Garnison och krigssjukhus i Sverige. Available at https://sok.riksarkivet.se/?postid=ArkisRef+SE%2fKrA%2f0351&s=Balder; accessed January 2020.
- 20. Andersson SO. Militär akutsjukvård I fält—när den övade verkligheten blir verklig, Dissertation No. 1411. Linköping University Medical, 2014. [Google Scholar]
- 21. Bro T: Två svenska läkare på var sin sida om fronten. Lakartidningen 2017; 114: EMA6. [Google Scholar]
- 22. The Swedish Red Cross : Röda Korset . Available at https://www.rodakorset.se/om-oss/vita-bussarna/; accessed January 2020.
- 23. Lagen.nu : Läkaren i totalförsvarets. SOU 1961:63 . Available at: https://lagen.nu/sou/1961:63; accessed January 2020.
- 24. Lundberg L, Molde Å, Örtenwall P. Hälso-och sjukvård under krig och väpnade konflikter In: Katastrofmedicin. Sten Lennquist [red.]. Stockholm, Liber AB, 2009. [Google Scholar]
- 25. Gellerfors M, Linde J: Svensk militärsjukvård i Afghanistan håller toppklass. Lakartidningen 2014; 111: CP16. [PubMed] [Google Scholar]
- 26. Khorram-Manesh A, Carlström E: Civil-militär samverkan behövs för att klara masskadelägen. Lakartidningen 2019; 116: FRZE. [PubMed] [Google Scholar]
- 27. Khorram-Manesh A, Lönroth H, Rotter P et al. : Non-medical aspects of civilian-military collaboration in management of major incidents. Eur J Trauma Emerg Surg 2017; 43(5): 595–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Socialstyrelsen (SoS) : Totalförsvaret Sjukvårdssystem . Available at https://www.socialstyrelsen.se/om-socialstyrelsen/pressrum/press/samarbete-om-totalforsvarets-sjukvardssystem/. Accessed January 2020.
- 29. Trimbur J: Consensus and differences in collaborative learning. Coll Engl 1989; 51(6): 602–16. [Google Scholar]
- 30. Strandh V: Sweden’s capacity to prepare and respond to a terrorist attack on rail-bound traffic-promising practices and obstacles to inter-organizational collaboration. JRACR 2015; 5(4): 215–25. [Google Scholar]
- 31. Khorram-Manesh A: Facilitators and constrainers of civilian-military collaboration: the Swedish perspectives. Eur J Trauma Emerg Surg 2018. doi: 10.1007/s00068-018-1058-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Khorram-Manesh A, Angthong C, Pangma A et al. : Hospital evacuation; learning from the past? Flooding of Bangkok 2011. BJMMR 2014; 4(1): 395–415. [Google Scholar]
- 33. Rasmussen TE: Why military medical research? Mil Med 2014; 179(1): 1–2. [DOI] [PubMed] [Google Scholar]
- 34. Hodgetts TJ: The future character of military medicine. JR Army Corps 2019; 158(3): 271–8. [DOI] [PubMed] [Google Scholar]
- 35. Bricknell MCM, Cameron E: International military medical engagement with the indigenous civilian health sector. JR Army Med Corps 2011; 157(Supp 4): 472–6. [Google Scholar]
- 36. Yanagawa Y, Oode Y, Adegawa Y et al. : Japanese civilian and us military interaction in the evacuation of casualties from Camp Fuji. BMJ Military Health Published Online First: 29 June 2019. doi: 10.1136/jramc-2019-001247. [DOI] [PubMed] [Google Scholar]
- 37. Tracy EJ: Combining military and civilian trauma systems. Top Emerg Med 2005; 27(3): 170–5. [Google Scholar]
- 38. European Union : Risk Assessment Guidelines (RAG)–europa.eu . Available at https://ec.europa.eu/consumers/consumer-safety/rag/#/screen/home; accessed January 2020.
- 39. Olsen GR: Civil-military cooperation in crisis management in Africa: American and European Union policies compared. J Int Relat Dev 2011; 14(3): 333–53. [Google Scholar]
- 40. Melkon J, Embrey J, Bader H, Mennes B. Civil-Military interaction during infantry operations In: Effective Civil-Military Interaction in Peace Operations. Edited by Lucius G, Rietjens S. Cham, Springer, 2016. [Google Scholar]
- 41. Licina D: The military sectors role in global health: historical context and future directions. Global Health Governance 2012, Volume VI, Issue 1 (FALL 2012). Available at http://www.ghgj.org; accessed Januray 2020. [Google Scholar]


