Abstract
Injuries sustained in motorcycle collisions can be organized into distinct patterns to improve recognition and treatment.
Lowside, highside, topside, and collision are the four main categories of motorcycle crash types.
Within those four crash types, mechanisms of injury include head-leading collisions, direct vertical impact, motorcycle radius, motorcycle thumb, fuel tank injures, limb entrapment, tyre-spoke injury, and crash modifying manoeuvre.
Cite this article: EFORT Open Rev 2020;5:544-548. DOI: 10.1302/2058-5241.5.190090
Keywords: motorcycle injury, trauma, patterns of injury, emergency medicine
Introduction
Though the incidence of motorcycle collisions (MCC) in the US has declined since 2007, motorcyclists are six times more likely to be involved in an accident than motorvehiclists.1 In addition, patients in MCC accidents have significant musculoskeletal morbidity, with 71.5% of patients requiring an orthopaedic consult.2 Therefore, it is imperative for our orthopaedic trauma surgeons to be able to easily recognize and treat the often-complex injuries associated with motorcycle traumas. Several classifications have been proposed in an attempt to organize such patterns based on the MCC specific mechanism of injury. The purpose of this article is to organize motorcycle trauma into recognizable injury mechanisms to better understand how these injuries occur.
Mechanisms of injury
For the purposes of this article, a motorcycle is defined as having an engine size greater than 150 cc. Through the review of the existing literature, we have identified distinct injury patterns with predictable mechanisms of injury. Though motorcycle trauma can be caused by several different mechanisms occurring in concert, we propose categorizing the injury patterns associated with motorcycle trauma into several distinct mechanism types which may facilitate recognition and treatment. A 2016 study which reviews motorcycle injury in the professional racing community classifies injury patterns into four broad groups: lowside, highside, topside, and collision (Table 1).3 These injury patterns can then be further broken down to describe how injuries relevant to the orthopaedic surgery community are sustained (Table 2).
Table 1.
Crash type
| Crash type | Description |
|---|---|
| Lowside | Rider falls to the lowside of the lean angle during a turn. |
| Highside | Rider falls to the opposite side of a turn while trying to correct, causing the motorcycle to flip over and the rider to be thrown from the motorcycle. |
| Topside | Motorcycle suddenly decelerates and rider flips over the handlebars. |
| Collision | Rider strikes or is struck by a stationary object and is subjected to blunt trauma and deceleration forces. |
Table 2.
Notable crash mechanisms
| Region of body | Notable mechanism(s) | Crash type |
|---|---|---|
| Head | Head-leading collisions | Topside/highside |
| Upper extremity: shoulder girdle | Direct vertical impact | Collision |
| Upper extremity: wrist | Motorcycle radius | Topside/highside |
| Upper extremity: hand | Motorcycle thumb | Collision |
| Pelvic ring | Fuel tank injuries | Collision |
| Lower extremity: femur, tibia, fibula | Limb entrapment | Lowside |
| Lower extremity: heel | Tyre-spoke injury | Lowside |
| Lower extremity: foot | Crash modifying hyperdorsiflexion manoeuvre | Lowside |
Lowside crash
During a lowside mechanism of injury, the low side of the motorcycle skids with the ipsilateral lower extremity often being trapped under the motorcycle and the ipsilateral upper extremity instinctively being placed down to brace for impact. This leads to a high prevalence of ipsilateral lower and upper extremity injuries with the contralateral side being relatively preserved.
Limb entrapment
Limb entrapment is a lowside crash mechanism that occurs when the lower extremity is caught between a fixed object and the motorcycle. This is an exceedingly common mechanism of injury. In fact, the lower extremities are the most common sites of orthopaedic injuries in MCC, with incidence in some studies ranging between 40% and 60%.4–7 The most common of these injuries are tibia fractures (20–30%) followed by ankle and foot injuries.4,7,8
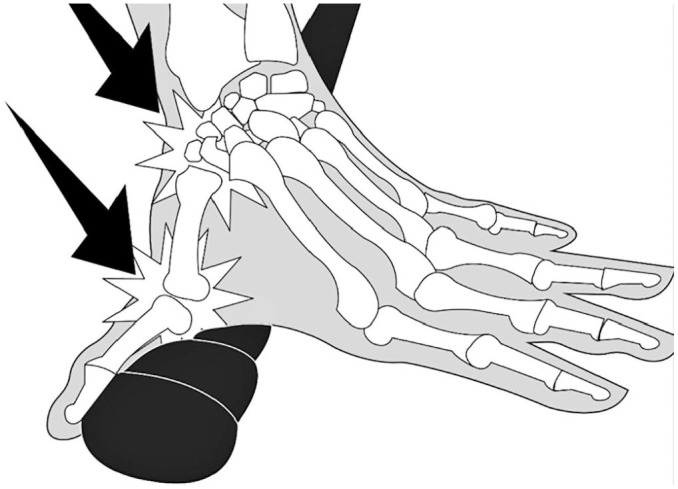
Crash modifying manoeuvres (Fig. 1)
Fig. 1.

Crash modifying manoeuvre.
Riders, in an attempt to recover from a pending lowside collision, may sustain lower extremity injuries described as ‘crash modifying manoeuvres’. These occur when a rider, in anticipation of a motorcycle losing tyre stability on a turn, will react to an impending crash by stretching out their leg in an attempt to right the motorcycle and catch themselves. The foot may impact first causing a hyperdorsiflexion, external rotation injury. Milder forms of these injuries can present as simple fracture dislocations of the foot and ankle with mangled extremities being seen with the more severe injuries.
Tyre-spoke injury (Fig. 2)
Fig. 2.
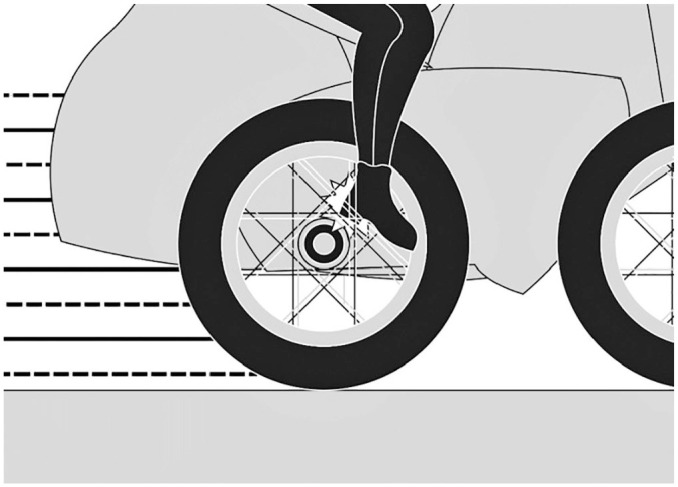
Tyre-spoke injury.
Another subset of the entrapment type injury is the ‘tyre-spoke injury’ which are often complex soft tissue injuries where the foot becomes caught within the spokes of the motorcycle tyre. These are associated with severe soft defects as well as injuries to the calcaneus and achilles.9 Tyre-spoke injuries have a high risk of amputation.
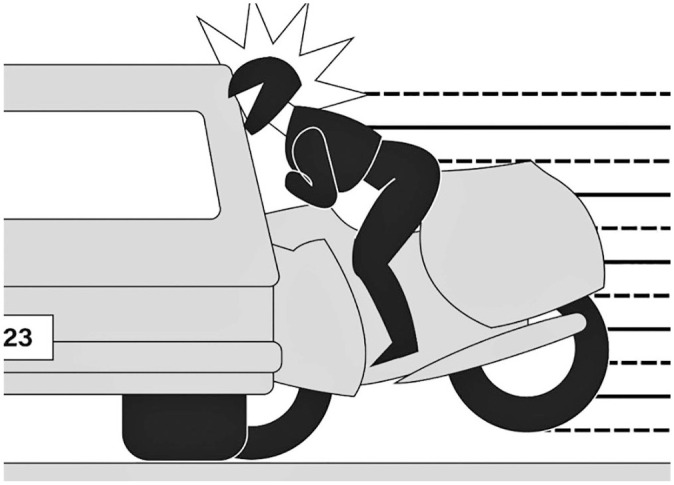
Topside/highside (Fig. 3)
Fig. 3.

Topside/highside collision.
Topside collisions describe riders being thrown over the handlebars of their motorcycle. Highside collisions describe riders falling away, opposite the side that their motorcycle is falling. These two crash mechanisms can generate similar injuries. In both cases the rider is thrown violently from the motorcycle. The distinction is whether the rider is thrown off the side or towards the front.
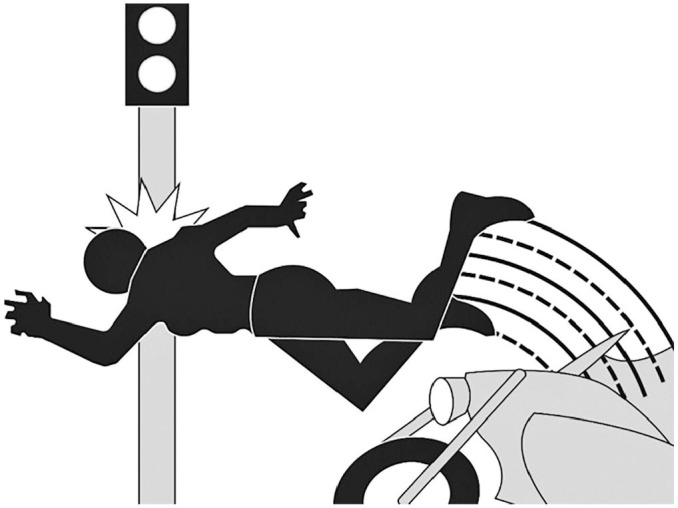
Head-leading collisions (Fig. 4)
Fig. 4.
Head-leading collision.
Head-leading implies a head-first collision in which the longitudinal body axis is aligned approximately parallel with the collision velocity,10 and often occurs after the rider is ejected from the motorcycle. This mechanism may be recognized by signs of frontal head trauma. Otherwise eyewitness account and helmet damage may suggest such an injury pattern. Head injuries are seen in 10–50% of motorcycle collisions and are the most common cause of fatality.4,8,10–14 Common injuries sustained from these mechanisms include facial soft tissue injuries and fractures, depressed skull fractures, linear fractures of the vault, and cerebral cortical contusions.15 As the head hyperextends, forces are transmitted through the cervical spine and cause injuries to structures at the junction of the head and neck, such as to the inferior temporal bone, basilar skull and cervical spine. In addition, patients may demonstrate traumatic brain injuries. The highest likelihood of traumatic brain injury (TBI) is associated with fractures of the zygoma, orbit and mandible, so recognition of these types of fracture should raise concern for TBI.15,16 Motorcyclists with head-leading injury should also have high suspicion of cervical injury as there is a strong correlation between head trauma and cervical spine injuries. Cervical spine injuries occur in 3% to 8% of patients with head injuries,17 -20 and are primarily concentrated in the upper third of the cervical spine.21
Crumple zone effect
It is important to note that the more distal upper extremity injuries are often associated with lower mortality which may be attributable to a ‘crumple zone effect’.22 When a patient is thrown from the motorcycle, they instinctively extend their arms in front of them to catch and brace themselves prior to impact. The distal portion of the upper extremity impacts the object first, absorbing the energy of the collision and potentially mitigating more severe proximal trauma. The most common injuries from the crumple zone effect are distal radius fractures, which are called ‘motorcycle radius’ injuries.23
Collision
The collision injury mechanism is the cause of direct impact with a fixed object, another motorcycle, or vehicle.
Fuel tank injuries (Fig. 5)
Fig. 5.
Fuel tank injury.
Fuel tank injury occurs when a motorcycle comes to an abrupt stop, and the momentum of the driver creates high peak loads between the rider’s pelvis and the motorcycle fuel tank. In one study, 85% of the pelvic injuries sustained by the patient were due to this type of mechanism.24 The injuries most commonly associated with this injury mechanism include pelvic fractures and bladder injuries. Bladder injuries tend to be found with more mild impact injuries, whereas fractures to the anterior and posterior portions of the pelvis suggest a higher velocity at the time of impact. The fracture characteristics of these injuries often resemble Anterior Posterior Compression types 2 and 3 pelvic fractures.25 Typically, a routine anteroposterior (AP) pelvis radiograph is part of the initial trauma workup as the incidence of these pelvic ring injuries is as high as 13%,4,8 with one study demonstrating 13% mortality.8
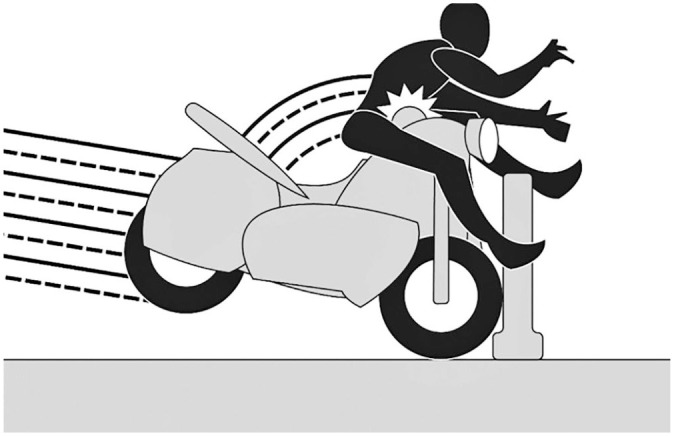
Direct vertical impact (Fig. 6)
Fig. 6.
Direct vertical impact collision.
Direct vertical impact injury commonly occurs when a motorcyclist strikes their shoulder against a fixed road sign or pole while traveling at high speed.26 In regard to the upper extremity, about a third of motorcycle crashes result in an upper extremity injury, with shoulder girdle injuries being the most common.22 This mechanism may cause brachial plexus injury, clavicle fractures, scapula fractures, and scapulothoracic dissociation, with studies reporting these injuries are responsible for 15–20% of all upper extremity injuries in MCC.4,7,22 Forearm fractures are the second most common upper extremity injury accounting for 10–15% of upper extremity injuries.22,27 Distal upper extremity fractures are less common, with studies reporting hand and wrist fractures in 5–10% of upper extremity injuries.7,22,28
More distally, ‘motorcycle thumb’ (Fig. 7) injuries can be encountered. These injuries occur secondary to the handlebar during impact. During a collision, the rider braces themselves by locking their elbows and griping the handlebars. The resultant force is directed into the palm and metacarpal base. Though these are less critical injuries, the thumb carpometacarpal (CMC) joint is injured approximately 50% of the time and the thumb ulnar collateral ligament is injured 20% of the time.29
Fig. 7.
Motorcycle thumb.
Evaluation and treatment
At our institution, most motorcycle injuries present as a ‘Full Trauma’ response, activating the general surgery, emergency medicine, and orthopaedic departments to respond immediately. The initial evaluation of the trauma patient is typically presided over by the general surgery team on call. Report of the patient is given by the first responder to the general surgery and emergency medicine teams. A general surgeon begins the primary survey in line with the Advanced Trauma Life Support (ATLS) guidelines, while other general surgery team members place initial orders needed for the patient in the trauma bay. The general surgeon continues with his secondary survey and the emergency medicine team will often carry out a focused assessment with sonography in trauma (FAST) at this time. The orthopaedic surgery team present will re-evaluate the patient in an attempt to seek out injuries and will request X-rays of areas of concern to be performed if the patient is stable. A portable chest and pelvic X-ray are typically the only radiographs performed routinely in the trauma bay. Any urgent orthopaedic interventions, such as pelvic sheeting, are performed at this time. The patient is then taken for computed tomography (CT) scanning for head/neck as well as chest, abdomen, and pelvis imaging at the discretion of the general surgery team. The general surgery team will also routinely perform a tertiary exam 24 hours after initial presentation to ensure no injury is missed.
Conclusion
Motorcycle injuries create a significant burden within the orthopaedic scope of practice. It is imperative that orthopaedists be familiar and comfortable with the scope of injuries that may present with motorcycle trauma. Motorcycle patients, as with other trauma patients, are at a high risk of sustaining severe injuries and should be evaluated and triaged under ATLS guidelines. While we recognize the limitations of fitting every MCC with these mechanisms of injury, they facilitate the recognition of orthopaedic injuries in these patients. These mechanisms, however, should not be viewed as an alternative to trauma evaluation guidelines. Classifying motorcycle injuries into distinct patterns so as to better recognize and treat them is a viable approach to better caring for these often-complex poly-trauma MCC patients.
Acknowledgments
We would like to thank Joshua Finkel of New York University for creating the figures associated with this manuscript.
Footnotes
ICMJE Conflict of interest statement: The authors declare no conflict of interest relevant to this work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. US Department of Transportation, National Highway Traffic Safety Administration; Federal Highway Administration, Traffic Safety Facts, NHTSA’s National Center for Statistics and Analysis, August 2019. [Google Scholar]
- 2. Amin NH, Jakoi A, Katsman A, Harding SP, Tom JA, Cerynik DL. Incidence of orthopedic surgery intervention in a level I urban trauma center with motorcycle trauma. J Trauma 2011;71:948–951. [DOI] [PubMed] [Google Scholar]
- 3. Bedolla J, Santelli J, Sabra J, Cabanas JG, Ziebell C, Olvey S. Elite motorcycle racing: crash types and injury patterns in the MotoGP class. Am J Emerg Med 2016;34:1872–1875. [DOI] [PubMed] [Google Scholar]
- 4. Alicioğlu B, Yalniz E, Eşkin D, Yilmaz B. [Injuries associated with motorcycle accidents]. Acta Orthop Traumatol Turc 2008;42:106–111. [PubMed] [Google Scholar]
- 5. Eid HO, Barss P, Adam SH, et al. Factors affecting anatomical region of injury, severity, and mortality for road trauma in a high-income developing country: lessons for prevention. Injury 2009;40:703–707. [DOI] [PubMed] [Google Scholar]
- 6. Wick M, Müller EJ, Ekkernkamp A, Muhr G. The motorcyclist: easy rider or easy victim? An analysis of motorcycle accidents in Germany. Am J Emerg Med 1998;16:320–323. [DOI] [PubMed] [Google Scholar]
- 7. Batista F, Silveira LO, Castillo JJ, de Pontes JE, Villalobos LD. Epidemiological profile of extremity fractures in victims of motorcycle accidents. Acta Ortop Bras 2015;23:43–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ankarath S, Giannoudis PV, Barlow I, Bellamy MC, Matthews SJ, Smith RM. Injury patterns associated with mortality following motorcycle crashes. Injury 2002;33:473–477. [DOI] [PubMed] [Google Scholar]
- 9. Zhu YL, Li J, Ma WQ, Mei LB, Xu YQ. Motorcycle spoke injuries of the heel. Injury 2011;42:356–361. [DOI] [PubMed] [Google Scholar]
- 10. Kraus JF, Peek-Asa C, Cryer HG. Incidence, severity, and patterns of intrathoracic and intra-abdominal injuries in motorcycle crashes. J Trauma 2002;52:548–553. [DOI] [PubMed] [Google Scholar]
- 11. Lastfogel J, Soleimani T, Flores R, et al. Helmet use and injury patterns in motorcycle-related trauma. JAMA Surg 2016;151:88–90. [DOI] [PubMed] [Google Scholar]
- 12. MacLeod JBA, Digiacomo JC, Tinkoff G. An evidence-based review: helmet efficacy to reduce head injury and mortality in motorcycle crashes: EAST practice management guidelines. J Trauma 2010;69:1101–1111. [DOI] [PubMed] [Google Scholar]
- 13. Erhardt T, Rice T, Troszak L, Zhu M. Motorcycle helmet type and the risk of head injury and neck injury during motorcycle collisions in California. Accid Anal Prev 2016;86:23–28. [DOI] [PubMed] [Google Scholar]
- 14. Talving P, Teixeira PG, Barmparas G, et al. Motorcycle-related injuries: effect of age on type and severity of injuries and mortality. J Trauma 2010;68:441–446. [DOI] [PubMed] [Google Scholar]
- 15. Peter K, Krantz G. Head and neck injuries to motorcycle and moped riders: with special regard to the effect of protective helmets. Injury 1985;16:253–258. [DOI] [PubMed] [Google Scholar]
- 16. Bambach MR, Mattos GA. Head and spine injuries sustained by motorcyclists in head-leading collisions with fixed roadside objects. Traffic Inj Prev 2015;16:168–176 [DOI] [PubMed] [Google Scholar]
- 17. Holly LT, Kelly DF, Counelis GJ, Blinman T, McArthur DL, Cryer HG. Cervical spine trauma associated with moderate and severe head injury: incidence, risk factors, and injury characteristics. J Neurosurg 2002;96:285–291. [DOI] [PubMed] [Google Scholar]
- 18. Mulligan RP, Friedman JA, Mahabir RC. A nationwide review of the associations among cervical spine injuries, head injuries, and facial fractures. J Trauma 2010;68:587–592. [DOI] [PubMed] [Google Scholar]
- 19. Tian HL, Guo Y, Hu J, et al. Clinical characterization of comatose patients with cervical spine injury and traumatic brain injury. J Trauma 2009;67:1305–1310. [DOI] [PubMed] [Google Scholar]
- 20. Lam C, Lin MR, Chu SF, Tsai SH, Bai CH, Chiu WT. The effect of various types of motorcycle helmets on cervical spine injury in head injury patients: a multicenter study in Taiwan. Biomed Res Int 2015;2015:487985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lin M-R, Kraus JF. A review of risk factors and patterns of motorcycle injuries. Accid Anal Prev 2009;41:710–722. [DOI] [PubMed] [Google Scholar]
- 22. Paryavi E, Gilotra MN, Johnson AJ, Pensy RA, Eglseder WA, Abzug JM. Upper extremity injuries in motorcyclists: implications for mortality and need for rehabilitation services. J Trauma Acute Care Surg 2015;78:1021–1025. [DOI] [PubMed] [Google Scholar]
- 23. Zettas JP, Zettas P, Thanasophon B. Injury patterns in motorcycle accidents. J Trauma 1979;19:833–836. [DOI] [PubMed] [Google Scholar]
- 24. Meredith L, Baldock M, Fitzharris M, et al. Motorcycle fuel tanks and pelvic fractures: a motorcycle fuel tank syndrome. Traffic Inj Prev 2016;17:644–649. [DOI] [PubMed] [Google Scholar]
- 25. Rockwood CA, Green DP, Heckman JD, Bucholz RW. Rockwood and Green’s fractures in adults. Philadelphia, PA: Lippincott Williams & Wilkins, 2001. [Google Scholar]
- 26. Soldado F, Ghizoni MF, Bertelli J. Injury mechanisms in supraclavicular stretch injuries of the brachial plexus. Hand Surg Rehabil 2016;35:51–54. [DOI] [PubMed] [Google Scholar]
- 27. Kosola S, Salminen P, Laine T. Heading for a fall: moped and scooter accidents from 2002 to 2007. Scand J Surg 2009;98:175–179. [DOI] [PubMed] [Google Scholar]
- 28. Rubin G, Peleg K, Givon A, Rozen N. Upper extremity fractures among hospitalized road traffic accident adults. Am J Emerg Med 2015;33:250–253. [DOI] [PubMed] [Google Scholar]
- 29. Alexander C, Abzug JM, Johnson AJ, Pensy RA, Eglseder WA, Paryavi E. Motorcyclist’s thumb: carpometacarpal injuries of the thumb sustained in motorcycle crashes. J Hand Surg Eur Vol 2016;41:707–709. [DOI] [PubMed] [Google Scholar]


