Abstract
Background and aims
Diabetes is a frequent comorbidity in patients with Severe COVID-19 infection associated with a worse prognosis. Hypercoagulability with elevation in D-dimer levels has been demonstrated in patients with COVID-19. This study aims to study D-dimer levels in people with diabetes compared to those without diabetes among patients with COVID-19 infection.
Methods
In this observational study 98 moderate and severely ill patients with COVID-19 infection were included at a dedicated COVID hospital. The study group was divided into patients with diabetes and without diabetes. Peak D-dimer was measured in both the groups and compared using appropriate statistical tests.
Results
In our study peak D-dimer levels were 1509 ± 2420 ng/mL (Mean ± SD) in people with diabetes and 515 ± 624 ng/mL (Mean ± SD) in patients without diabetes. Patients with diabetes had higher D-dimer levels which were statistically significant.
Conclusions
This study shows COVID-19 patients with diabetes had significantly higher D-dimer levels. Therefore, it is possible that COVID-19 infection with diabetes is more likely to cause hypercoagulable state with a worse prognosis. However clinical implications of these findings will need to be seen in further studies.
Keywords: D-dimer, Diabetes, COVID-19
Highlights
-
•
Patients of COVID-19 with diabetes had more severe disease levels.
-
•
People with diabetes had higher D-dimer levels in COVID-19.
-
•
D-dimer is a valuable biomarker of severity of COVID-19 in patients of diabetes.
1. Introduction
The Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) first cases of which were reported in Wuhan district, China in December 2019 has caused a global outbreak of a novel disease [1]. The disease which is still spreading and has affected almost all countries was declared a pandemic by the World Health Organization on 11 Mar 2020. There are more than 27 million confirmed COVID-19 cases worldwide with more than 0.9 million deaths as of Aug 20 [2].
Risk factors like age, diabetes, cardiovascular disease, chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), malignancy, and stroke among others have been associated with severe disease and adverse outcomes [[3], [4], [5]]. Biomarkers like C-reactive protein, ferritin, lactate dehydrogenase, D-dimer, interleukin 6, and fibrinogen have been utilized to predict severe disease in patients with COVID-19 [[3], [4], [5]].
Diabetes mellitus has been one of the most consistent risk factors for severe disease in patients with COVID-19 and uncontrolled hyperglycemia has been associated with poor outcomes and mortality. This could be due to diabetes being associated with other risk factors like age, hypertension and obesity. This could be also due to people with diabetes having a dysregulated innate and adaptive immune response and their already having chronic low-grade inflammation which makes them more susceptible to cytokine storm. People with diabetes could also be at higher risk for thrombotic events as diabetes is associated with an imbalance between clotting factors and fibrinolysis [6].
D-dimer is a byproduct of fibrin degradation. It is widely recognized as a biomarker for thromboembolism and as a prognostic marker for critical patients. COVID-19 being a procoagulant state thus D-dimer has been studied as a biomarker for predicting disease severity.
Studies have shown people with diabetes especially as well as those with macrovascular and microvascular complications have higher levels of D-dimer. Since diabetes has been identified as a strong predictor of disease severity in COVID-19, it is yet to be seen if D-dimer values in people with diabetes are any different from those without diabetes before we can assume it to be one of the causes of severe disease in COVID-19 showing increased susceptibility to thromboembolic disease in Diabetes Mellitus. This study aims to study D-dimer levels in people with diabetes compared to those without diabetes among patients with COVID 19 infection.
2. Methods
2.1. Study design and patients
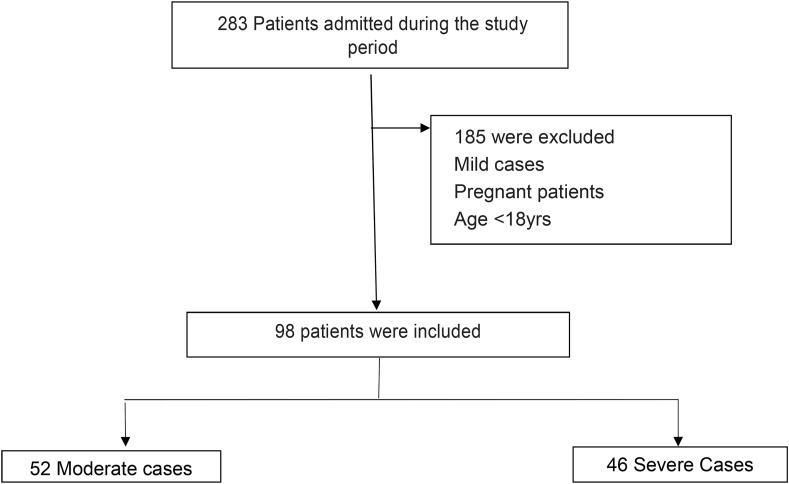
This cross-sectional study was conducted at a dedicated COVID hospital in North India from 12 July 2020 to 31 Aug 2020. Patients were triaged as per severity on basis of national guidelines-asymptomatic, Mild(Respiratory Rate <24/min, SpO2>94% at room air), Moderate(Respiratory rate:24–30/min, SpO2 90–94% at room air) and Severe(Respiratory rate>30/min SpO2<90%), ARDS and Septic Shock [7]. All laboratory-confirmed COVID-19 cases by RTPCR(Real Time Reverse Transcription Polymerse Chain Reaction) or RAT(Rapid Antigen Test) were admitted at this centre. Only Moderate and Severe patients of confirmed COVID 19 were included in this study. The estimation of D-dimer levels was done by chemiluminescent immunoassay at presentation and during the hospital stay every 48–72 hourly till discharge or death. Exclusion criteria were age <18yrs, patients with a pre-existing history of venous thromboembolism, or on anticoagulants, and pregnancy (see Fig 1 ). Written informed consent was taken. This study was approved by the Institutional Ethics Committee.
Fig. 1.
Flow chart showing enrolment of patients for the study.
2.2. Statistical analysis
Data was collected and analyzed with SPSS version 25. Continuous variables were expressed as means and standard deviation. Categorical variables were expressed as counts and percentages in both the People with Diabetes and People without Diabetes category. Chi-square test and Mann Whitney U tests were used to test for significant differences between the two groups. P values < 0.05 were considered statistically significant.
3. Results
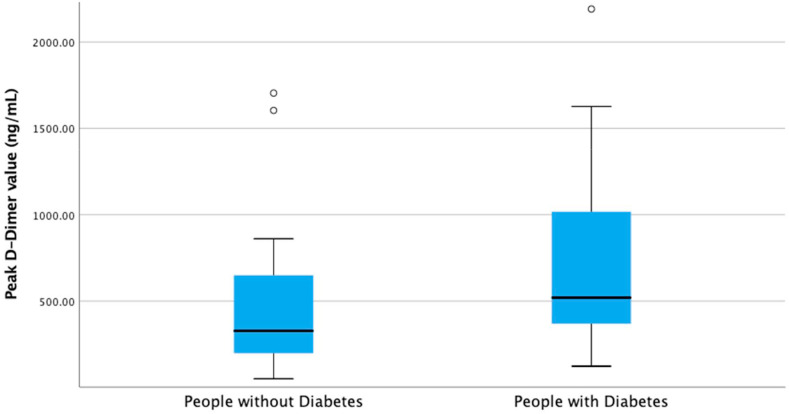
Among the 98 enrolled patients, 71% were males and 28.6% were females. Total 44% were with diabetes and the rest were without diabetes. The baseline characteristics of the two groups are comparable, except severe disease which was more in people with Diabetes shown in Table 1 . The Box-plots of peak D-dimer levels in people with diabetes and people without diabetes are shown in Fig. 2 . The relation between D-dimer levels in COVID-19 in people with diabetes and those without diabetes shows a significant difference as shown in Table 2 (P value = 0.002). In subgroup analysis, difference in D-dimer levels in patients with diabetes and those without diabetes with moderate disease was statistically significant (P value = 0.041). However, the difference between D-dimer levels in patients with diabetes and those without diabetes with severe disease was not statistically significant (P valve = 0.066) as shown in Table 3 .
Table 1.
Baseline characteristics.
| Characteristic | All patients (n = 98) | People with Diabetes (n = 45) | People without Diabetes (n = 53) | P value |
|---|---|---|---|---|
| Age, Mean ± SD -yr | 53 ± 13 | 57 ± 12 | 50 ± 14 | 0.19 |
| Sex-Male; no (%) | 70(71.4%) | 32 (71.1%) | 38(71.6%) | 0.949 |
| Hypertension; no (%) | 49 (50.0%) | 26(57.7%) | 23 (43.3%) | 0.839 |
| Severity | 0.048 | |||
| Moderate no (%) | 52 (53.0%) | 19 (42.2%) | 33 (62.2%) | |
| Severe no (%) | 46 (47.0%) | 26 (57.8%) | 20 (37.8%) |
Fig. 2.
Box-plots of Peak D-dimer levels in COVID-19 showing a significant difference between people with diabetes and people without diabetes.
Table 2.
Diabetes and peak D-dimer levels.
| All Patients (n = 98) | People with Diabetes (n = 45) | People without Diabetes (n = 53) | P value | |
|---|---|---|---|---|
| D -dimer Mean ± SD (ng/mL) | 972 ± 1764 | 1509 ± 2420 | 515 ± 624 | 0.002 |
| D-dimer Median (ng/mL) | 441 | 519 | 327 | |
| D-dimer interquartile range (ng/mL) | 482 | 706 | 468 |
Table 3.
Subgroup analysis of D-dimer values with disease severity.
| Disease severity | People with Diabetes | People without Diabetes | P value |
|---|---|---|---|
| Moderate disease, D -dimer Mean ± SD (ng/mL) | 1707 ± 2921 | 411 ± 392 | 0.041 |
| Severe disease, D -dimer Mean ± SD (ng/mL) | 1364 ± 2028 | 687 ± 671 | 0.066 |
4. Discussion
Our study was done on moderate and severely ill patients with COVID-19 infection. It demonstrated a significant relation of D-dimer levels with diabetes in patients with COVID-19. D-dimer levels were significantly higher in the group with diabetes as compared to the group without diabetes. All patients with diabetes received insulin therapy for diabetes in our hospital. All patients with moderate and severe COVID-19 received prophylactic or therapeutic anticoagulation as per national guidelines.
Diabetes is frequent comorbidity associated with severe disease and poor prognosis in COVID-19 infection [[8], [9], [10]]. In intensive care units the incidence of diabetes is two times higher than non- ICU patients with COVID-19 [11].In the study by Guan et all in Wuhan the primary composite endpoint of death, mechanical ventilation, and ICU admission was in 22% of the patients with diabetes as compared to 6% in patients without diabetes [12]. Analysis in Italy revealed that two-third of the patients with diabetes had a fatal outcome in COVID 19 infection [13].
D-dimer has been utilized in past as a marker of hypercoagulability. Studies in COVID-19 patients have demonstrated coagulation abnormalities with marked elevation in D-dimer levels in patients with severe disease. Recent studies have correlated D-dimer more than 2000 ng/mL was associated with increase fatality in COVID-19 [14]. Severe hypoxia in patients with ARDS can lead to activation of extrinsic coagulation pathway and increase blood viscosity leading to hypercoagulable state in COVID-19 infection [15].
In our study peak D-dimer levels were 1509 ± 2420 ng/mL (Mean ± SD) in patients with diabetes and 515 ± 624 ng/mL (Mean ± SD) in patients without diabetes. In subgroup analysis, COVID-19 patients with moderate disease had D-dimer levels were 1707 ± 2921 ng/mL (Mean ± SD) in patients with diabetes and 411 ± 392 ng/mL (Mean ± SD) in patients without diabetes. In COVID-19, patients with severe disease had D-dimer levels 1364 ± 2028 ng/mL (Mean ± SD) in patients with diabetes and 687 ± 871 ng/mL (Mean ± SD) in patients without diabetes, however this was statistically not significant. This shows that moderate disease has a statistically significant association with D-dimer levels, which means that the significant association of D-dimer with diabetes is not entirely due to greater number of severe patients in the diabetes group. The non-significant association of D-dimer in severe disease with diabetes could also be due to the smaller samples in the subgroup analysis. This could also be because the patients were triaged as per severity at admission, however peak D-dimer levels during entire course of hospital stay was utilized in statistical analysis. Further, glycaemic control was not considered while analysing the peak D-dimer values in diabetes which could possibly affect outcomes.
Patients with diabetes had more severe disease with higher D-dimer levels. Persistent hyperglycemia can lead to endothelial dysfunction and inflammation which can lead to thrombus formation [16]. Therefore, it is likely that severe SARS-CoV-2 infection with diabetes is more likely to cause coagulopathy and resultant poor outcome. However clinical implications of these findings are yet to be seen. Our study was limited in form of a single centre study. Our patients consisted of only moderate to severe patients with COVID-19 and all patients were started on anticoagulant therapy. Further studies will be required to validate the same and examining the clinical significance of these findings.
Acknowledgements
Nil.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that there is no conflict of interest.
References
- 1.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coronavirus COVID-19 (2019-nCoV) https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 [Internet]. [cited 2020 Sep 13]. Available from:
- 3.Wu C., Chen X., Cai Y., Xia J., Zhou X., Xu S. Risk factors associated with Acute respiratory distress Syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chow N., Fleming-Dutra K., Gierke R., Hall A., Hughes M., Pilishvili T. Preliminary estimates of the prevalence of selected underlying Health conditions among patients with coronavirus disease 2019. MMWR Morb Mortal Wkly Rep. 2020;69:382–386. doi: 10.15585/mmwr.mm6913e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA, J Am Med Assoc. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 6.Apicella M., Campopiano M.C., Mantuano M., Mazoni L., Coppelli A., Del Prato S. COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol [Internet] 2020;8(9):782–792. doi: 10.1016/S2213-8587(20)30238-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ministry of Health and Family Welfare . vol. 13. 2020. https://www.mohfw.gov.in/pdf/ClinicalManagementProtocolforCOVID19.pdf (Clinical management Protocol : COVID-19). [Google Scholar]
- 8.Muniyappa R., Section C.E., Branch O., Diseases K., Mellitus D. Perspective : COVID-19 pandemic , corona viruses , and diabetes mellitus ranganath muniyappa and sriram gubbi clinical endocrine section , diabetes , endocrinology , and obesity branch , national institute of diabetes and digestive and kidney diseases. N. Am J Physiol Metab. 2020:318. [Google Scholar]
- 9.Bin S.Y., Heo J.Y., Song M.S., Lee J., Kim E.H., Park S.J. Environmental contamination and viral shedding in MERS patients during MERS-CoV outbreak in South Korea. Clin Infect Dis. 2015;62:755–760. doi: 10.1093/cid/civ1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bornstein S.R., Dalan R., Hopkins D., Mingrone G., Boehm B.O. Endocrine and metabolic link to coronavirus infection. Nat Rev Endocrinol. 2020;16:297–298. doi: 10.1038/s41574-020-0353-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li B., Yang J., Zhao F., Zhi L., Wang X., Liu L. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109:531–538. doi: 10.1007/s00392-020-01626-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guan W., Ni Z., Hu Y., Liang W., Ou C., He J. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sardu C., Gambardella J., Morelli M.B., Wang X., Marfella R., Santulli G. Hypertension, thrombosis, kidney failure, and diabetes: is COVID-19 an endothelial disease? A comprehensive evaluation of clinical and basic evidence. J Clin Med. 2020;9:1417. doi: 10.3390/jcm9051417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang L., Yan X., Fan Q., Liu H., Liu X., Liu Z. D-dimer levels on admission to predict in-hospital mortality in patients with Covid-19. J Thromb Haemostasis. 2020;18:1324–1329. doi: 10.1111/jth.14859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gupta N., Zhao Y.Y., Evans C.E. The stimulation of thrombosis by hypoxia. Thromb Res. 2019;181:77–83. doi: 10.1016/j.thromres.2019.07.013. [DOI] [PubMed] [Google Scholar]
- 16.Domingueti C.P., Dusse L.M.S.A., Carvalho M.D.G., De Sousa L.P., Gomes K.B., Fernandes A.P. Diabetes mellitus: the linkage between oxidative stress, inflammation, hypercoagulability and vascular complications. J Diabet Complicat. 2016;30:738–745. doi: 10.1016/j.jdiacomp.2015.12.018. [DOI] [PubMed] [Google Scholar]