Abstract
Lesson 1: The loosening of federal government regulations enabled the rapid scaling of telehealth, as it enabled providers to be reimbursed for video visits at the same rate as in-person services.
Lesson 2: While resistance to change was the norm, the COVID-19 crisis motivated improvements to four major internal operational workflows (scheduling, appointment conversions, patient support and Virtual Rooming Assistants) for video visits, which were met with acceptance by both clinical and non-clinical staff.
Lesson 3: Leveraging prior intraorganizational relationships and active collaboration between different stakeholders, helped drive rapid operational change. An ongoing centralized communication and support strategy, ensured all stakeholders were informed and engaged during these uncertain times.
Lesson 4: Regular electronic health record (EHR) training and educational material increased end-user knowledge of video visits and helped ensure the visit was safe, medically effective and maintained patient-provider relationships.
Lesson 5: A clearly defined intake and evaluation process to filter out technologies that do not integrate with the patient portal or the EHR, ensures operational consistency and long-term sustainability.
Lesson 6: Personalized support to patients of different levels of technical literacy with using the preferred patient portal and application, was vital to its use, adoption and overall patient experience.
Keywords: Telehealth, COVID-19, Technology, Operations, Patient satisfaction, Video visit
1. Background
While telehealth promised benefits such as ease and convenience of patient care, prior to COVID-19, it was not readily scalable across health systems. This was largely due to the restrictive state and federal regulations as well as inconsistent practices by commercial payors which limited telehealth reimbursement to select patient populations in rural areas. The mainstream adoption of telehealth was further compounded by the challenges of integrating virtual care technology with the electronic health record.1
However, recognizing the need for continued patient care amid social distancing guidelines to slow the spread of COVID-19, in March 2020 the government introduced waivers under section 1135(b) (8) of the Social Security Act to vastly expand telehealth services.2 CMS subsequently relaxed COVID-19 telehealth reimbursement guidelines; they removed geographic restrictions, relaxed technological restrictions for both providers and patients, and reimbursed video visits for both new and return patients at the same rate as in-person visits for over 80 services.3 As commercial payors followed suit, this propelled the rapid adoption of telehealth. In response, many Academic Medical Centers (AMC) who had previously only piloted telehealth programs, were now tasked with rapidly converting and scaling thousands of in-person visits to video visits.
At Yale New Haven Health System (YNHHS) these external changes fueled a rapid cultural and institutional alignment, vital to scaling and implementing system-wide transformations. Notably, the increasing patient acuity and clinical financial losses as the pandemic progressed fueled a sense of urgency, requiring comprehensive stakeholder collaboration to mitigate risk by scaling virtual care. The ongoing pandemic challenged YNHHS System to: (1) rapidly roll out telehealth across the complex organization using pre-existing workflows which were previously untested on a large scale, and (2) to focus clinical and financial recovery efforts on sustaining and growing telehealth, given the future promises of virtual healthcare delivery.
2. Organizational context
Yale New Haven Health System is a hub and spoke academic medical center composed of five community hospitals. Yale New Haven Hospital is the main hospital and is affiliated with two distinct physician practice groups: (1) Yale Medicine (YM), the multispecialty clinical practice of Yale School of Medicine - a private institution of higher education and research. (2) North East Medical Group (NEMG) a non-profit multispecialty medical foundation.4 , 5
In 2019, Yale Medicine saw continued growth in ambulatory care as healthcare delivery continued to shift from inpatient to outpatient care. Ambulatory visit volume increased from 1,137,560 to 1,234,977, an 8.5% growth from the prior year. During that same time-period, the full-time physician workforce saw a modest decrease from 1299 to 1267 while the number of employed non-physician providers grew by 10% from 704 to 776.6
In 2019, Yale Medicine pursued several system-wide operational innovation projects. This included entering the second year of a three-year plan to expand the scheduling/access center to 16 out of 22 departments. This centralized scheduling structure would later prove to be a key element in the mass and rapid deployment of video visits.
3. Personnel content
The Telehealth program organizational structure is composed of the Executive Steering Committee, the Executive Planning Committee, the Operations team as well as several working groups. The Operations team, a multidisciplinary group of 17 employees from YNHHS and Yale Medicine, were essential to the organization-wide adoption of telehealth. The four members of the YM Telehealth team - a subset of the Operations team, all have multiple years of experience in healthcare operations and were largely responsible and accountable for scaling virtual visits throughout Yale Medicine. This team also includes the YNHHS Medical Director for Telehealth Services.
For 3-years leading up to the pandemic, the interorganizational telehealth team had been working together and had intact and well-defined roles; the team had completed the necessary five stage team development process.7 However, given the immediate needs of the COVID-19 response, re-defining the roles of the larger telehealth multidisciplinary team was crucial for the successful conversion of in-person visits to video visits. The unique challenges presented by COVID-19 prompted the team to quickly adapt to working under conditions of extreme stress and variation, while also assuming an equal distribution of social and task roles, features commonplace to effective crisis management in high reliability organizations.8 This systems thinking approach to understanding how the various stakeholders and entities within a complex health system are connected, was critical when scaling video visits during the pandemic amid much uncertainty.9
4. Problem
4.1. Problem 1. Efficiently and rapidly converting in-person visits to telehealth in an outpatient multi-specialty setting during COVID-19
Amidst new social distancing guidelines, YM Telehealth Leadership recognized the need to restructure the organization to continue to deliver safe and effective patient care. This involved supporting clinicians from different specialties to redesign and transition patient care to a virtual setting. While CMS telehealth reimbursement guidelines incentivized virtual care during this time, the question remained, on how best to scale video visits and support teaching across multiple specialties, especially since many physicians were traditionally resistant to telehealth.
Prior to COVID-19, the YM Telehealth team would identify two champions within each ambulatory specialty to spearhead telehealth adoption efforts: (1) An ‘Operational Lead’ who helps develop an operational video visit workflow that also aligns with the existing patient visit workflow and (2) A ‘Clinical Champion’, usually a physician expressing interest in piloting this new video visit workflow. However, many specialties were not able to fill these champion roles prior to COVID-19. Yet, through a limited number of individual provider telehealth pilots, the YM Telehealth team recognized the potential promises of video visits, from both a workflow and patient satisfaction perspective. However, even when the individual pilot was successful in a specialty, broader physician buy-in across the specialty was lacking and telehealth failed to gain traction across certain specialties, mainly due to financial misalignment. Reimbursement for outpatient virtual care was limited to coverage in the postoperative global period – i.e. only follow-up visits in select specialties such as surgery and oncology care.
Despite the limited number of video visits prior to the pandemic, the YM Telehealth team gained the opportunity to learn organizational best practices when redesigning and implementing telehealth operational workflows. For instance, given the importance of stakeholder collaboration when implementing these transformational projects, the YM Telehealth team together with the Operational Leads, participated in interactive management workshops focused on Accountability. It helped them problem-solve together on operational requirements for telehealth success such as educating patients, obtaining devices and ensuring provider punctuality. Moreover, these workshops helped build positive relationships between the Telehealth team and Operational Leads early on, which were vital to the later success of the program. Additionally, although there were few champions prior to the pandemic, this same process was later applied during the crisis to quickly identify such individuals from each specialty, pilot the video visit workflow and rapidly deploy telehealth across the entire specialty.
4.2. Problem 2. Rapidly scaling telehealth technology across different stakeholders during a public health pandemic
A second challenge was addressing the numerous technical barriers to scaling outpatient video visits system-wide during COVID-19. During the public health emergency, the Center for Medicare and Medicaid Services (CMS) released relaxed reimbursement guidelines and the HHS Office for Civil Rights (OCR) allowed HIPAA compliance waivers. Both these eliminated the penalty for using non-HIPAA compliant devices and applications (e.g., FaceTime, Zoom, Skype) to provide patient care.
While these applications were more convenient to end-users, System leadership and the YM Telehealth team recognized the potential risk of the government reimposing waivers at the end of the emergency. Furthermore, YNHHS converted to Epic in October 2011 and has since expanded service offerings integrated with the EHR, including the current patient portal – MyChart. To ensure the sustainability of telehealth after the pandemic, it was imperative to choose a patient portal such as MyChart that would continue to meet regulatory guidelines after the pandemic while also meeting billing, compliance, and operational guidelines that have already been built into Epic workflows. Therefore, in the context of limited time, resources and prior investments, both Epic and MyChart were chosen and quickly modified early in the pandemic, to strengthen bandwidth and support additional user needs. However, the question remained on how to widely deploy this technology among all stakeholders in this large healthcare system (see Fig. 1).
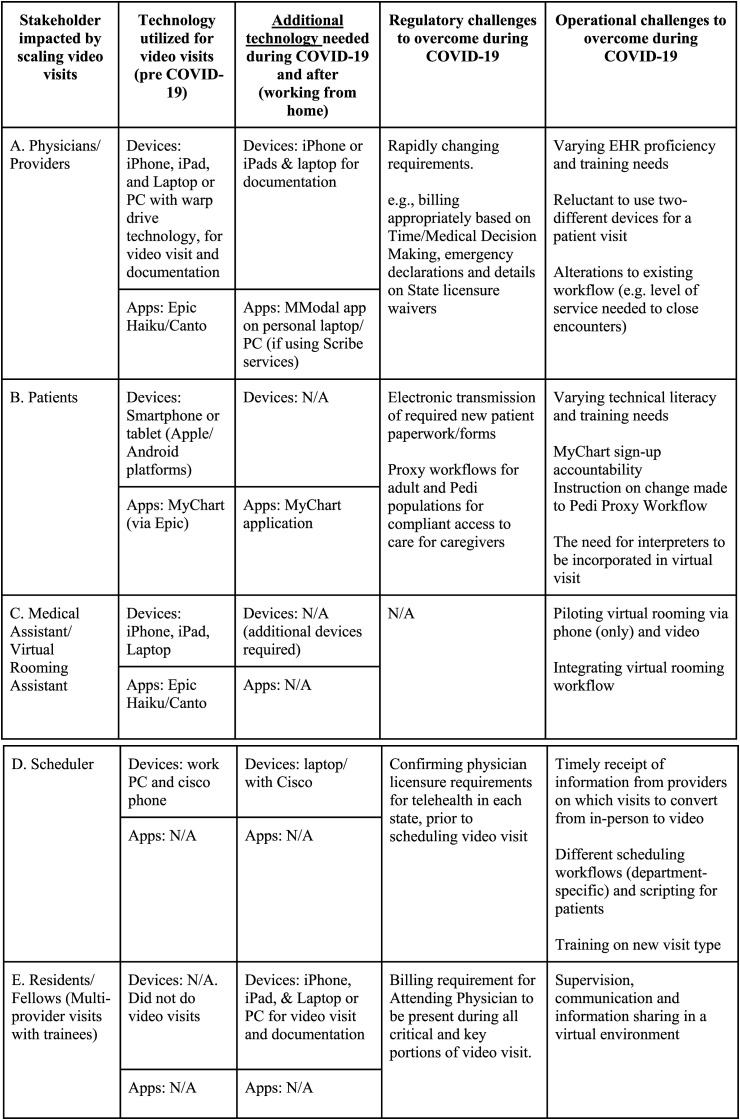
Fig. 1.
Technological considerations per stakeholder when operationalizing outpatient video visits during COVID-19. Source: Yale Medicine.
Several stakeholders-patients, physicians, providers, trainees (multi-provider visits), schedulers and Medical Assistants, were impacted by the COVID-19 ambulatory telehealth initiative at YM (see Fig. 1 ). Each stakeholder had unique technological, operational and regulatory considerations which needed to be addressed during COVID-19. These included ensuring technological compatibility with EHR, providing technical assistance and ensuring providers adhered to telehealth state licensure requirements based on where patients lived (Fig. 1).
Furthermore, the training and supervision of residents and fellows would require multi-provider video visit workflows. While prior CMS and ACGME guidelines required the physical presence of the training physician, they altered guidelines during the crisis permitting direct supervision to trainees via real-time audio/video technologies for the same key or critical portions of evaluations. Additional loosening of restrictions accommodated the primary care exception, allowing trainees to treat patients virtually without direct supervisory oversight. However, limitations remained on supervision for surgical or technical procedures via video based on clinical and technical skill of the trainee.10
Given these dynamic rules and regulations, the YM Telehealth team needed a strategy and plan to encourage all stakeholders, many of whom now worked from home due to social distancing guidelines, to use a pre-approved, standardized suite of technological services. Hence, the main question was, how to scale-up the preferred MyChart video visit technology across different stakeholders, and how to do so while overcoming dynamic IT and regulatory issues?
5. Solutions
We responded to the above system-wide challenges by partnering with operations, strategically scaling EHR-integrated technology and ensuring all stakeholders were informed and engaged through a centralized communication and training plan.
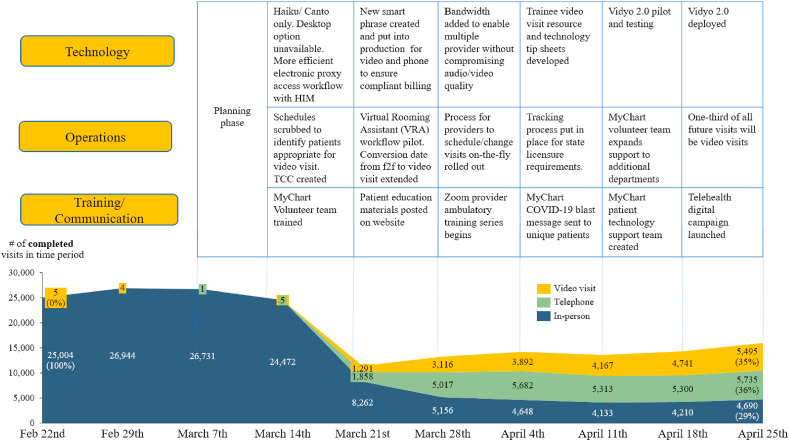
Fig. 2 illustrates the volume of YM video visits at both provider-based and office-based locations and weekly operational highlights while scaling telehealth during COVID-19. Prior to COVID-19, approximately 1–2 YM video visits were completed per day. However, during the height of the pandemic between March 7th to April 25th, this number grew rapidly and 22,728 YM video visits were completed, averaging at approximately 628 per weekday.
Fig. 2.
Timeline of operationalizing video visits at Yale Medicine during early COVID-19 (March–April 2020). Source: Yale Medicine Ambulatory Encounters Dashboard. NOTE: HIM = Health Information Management; f2f = face-to-face or in-person visit; TCC = Telehealth Conversion Center.
5.1. Strategic scaling of standardized EHR integrated technology
Given OCR changes, providers would not be penalized for using non HIPAA-compliant software.11 Yet, rules and regulations concerning privacy, compliance and HIPAA remain intact throughout the public health emergency. Therefore, it was important to select an EHR that permitted video visit technology that would be sustainable after the crisis, while capitalizing on prior investments and EHR workflows.
5.1.1. Why MyChart was the preferred technology platform
Additional considerations motivated the decision to pursue MyChart video visits as the preferred platform. They included the inherent benefits of the patient portal in increasing patient engagement, the automated ‘After Visit Summary’ in the MyChart patient's account and an interface for provider-patient communication, all within an EHR that met Connecticut state telehealth law requirements. Furthermore, interfaces like e-consent and other EHR tools, ensured the timely transmission of information to ensure valid and complete documentation. Providers who expressed difficulty with MyChart were encouraged to present requests for alternate technology, to then be assessed by the telehealth team for compliance; if a use case was appropriate, exceptions were made and guardrails put in place to ensure compliance with rapidly evolving telehealth rules.
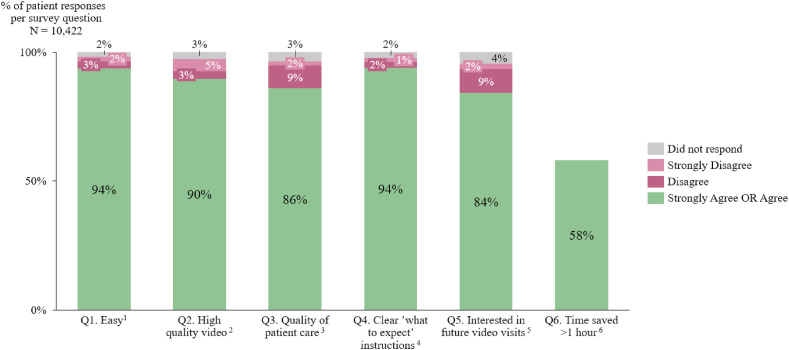
In a patient survey of first-time video visit users conducted in March and April (distributed via text after their initial video visit), patients were highly satisfied with the MyChart application and expressed interest in continuing to participate in video visits for future appointments (see Fig. 3 ). 58% of respondents saved more than 1-h of time (including travel, wait-time and time off from work). In total, approximately 15,738 h of patient-time was saved, averaging at 90-min per patient per appointment. Although this survey was conducted at the height of the pandemic and may have positively skewed patient perception of virtual care, these results nevertheless underscore the importance of understanding patient needs and preferences to drive wider adoption of telehealth.
Fig. 3.
Patient Satisfaction survey results for video visits conducted via the MyChart mobile application in March and April 2020 (N = 10,422).
Source: Rx Health (third-party vendor).
-
1.The MyChart App made it easy to have a video visit.
-
2.The video visit picture and audio quality were good.
-
3.My family member or I received the same quality of care during our video visit as an office visit.
-
4.My family member or I was satisfied with the video visit expectation instructions from the provider or provider's office.
-
5.My family member or I am interested in using video visits for future appointments.
-
6.How much time did you and/or your family member save by having a video visit? (this includes travel, wait, time off from work).
5.1.2. Use-cases for alternate technology for group sessions
As with all technological solutions, a single solution rarely solves all problems and needs of all clinical departments. One clear example of this was the need for video technology for multi-provider or group sessions. The first iteration of the preferred Vidyo technology within EHR, compromised video and audio quality when multiple patients joined one session. Therefore, the team compared various other options and chose Zoom as the alternative platform. The expectation was to rapidly approve this following a discussion with the department on their unique needs and workflows; departments discussed as to why the preferred system could not accomplish clinical care goals and how sessions may be completed outside the EHR. In these instances, new workflows were created to ensure the patient would receive and submit consent forms, as the typical process of obtaining consent was bypassed using alternative technology.
5.1.3. Vidyo connect 2.0
During the crisis, the platform used for video visits within the EHR was available for upgrade. The upgraded version (Vidyo 2.0) would allow for added flexibility with approved devices for video technology and satisfy the needs of many of the use cases requiring alternative technology. Once implemented in September 2020, it would allow for a smooth transition to a single platform for both individual or group video sessions, with opportunities to include care collaborators, additional conference features such as ad hoc consultants, a chat function, whiteboarding and interpreter services.
5.2. Partnering with operations and standardizing scheduling workflows
The system-wide adoption of Telehealth during COVID-19 required the scaling of four major internal operational workflows-patient scheduling, appointment conversions, patient support and Virtual Rooming Assistants (VRA). To minimize the operational drawbacks of an AMC with inherent complexity especially in a changing regulatory environment, the YM Telehealth team aimed to centralize and ensure consistency of these workflows across all specialties.
To accomplish this, the YM Telehealth team provided centralized support and oversight to the system. For instance, they created and advertised one e-mail address accessible to the core telehealth team, where providers and lead administrators could reach out with questions and feedback. Additionally, they closely collaborated with each operational entity to help define parameters for the conversion process, prepare training material for both clinical and non-clinical staff and obtain resources required for patient MyChart support.
5.2.1. Scheduling patients
Prior to the COVID-19, Yale Medicine had two main managed entities to handle scheduling workflows for outpatient clinics: (1) The access center which conducted centralized scheduling for multiple departments and (2) individual departments which self-scheduled. During the crisis, while the access center leveraged standardized workflows, departments with decentralized scheduling could not adapt as quickly.
The YM Telehealth team hoped to promote cooperation and resource-sharing as opposed to competition, to continue to provide high-quality patient care and access during the crisis. Therefore, based on the pre-existing centralized workflows and structure of the access center, a third managed entity-the Telehealth Conversion Center (TCC), was established early in the crisis to offer scheduling support to 22 decentralized Epic departments. By building on existing centralized workflows from the access center, the TCC could rapidly deploy scheduling workflows consistently and efficiently for multiple departments.
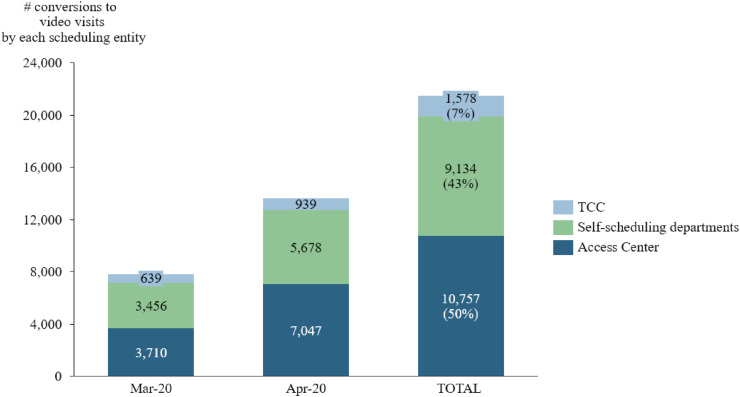
However, many individual departments chose to continue to self-schedule throughout the pandemic (defined as the self-scheduling departments in Fig. 4 ). Even then, their scheduling and conversion process was guided by ongoing interactions between the YM Telehealth team and Operational Leads, contributing to system-wide workflow and process consistency.
Fig. 4.
Volume of in-person appointments converted to video visits by each managed entity associated with Yale Medicine (March–April 2020). Source: EPIC BI Portal. Note: TCC = Telehealth Conversion Center.
5.2.2. Appointment conversions
Due to the seriousness of the pandemic, the State issued guidelines strongly recommending conversions to video visits whenever possible for the safety of patients and providers. Each department and physician had the autonomy to determine which patients could be offered a video visit or in-person visit either during the pandemic or later, depending on clinical necessity and patient acuity; each department decided these criteria based on their respective thresholds for clinical need.
The YM Telehealth team provided centralized operational guidance on the conversion process in Epic. Physicians were advised to notate patients eligible for video visits on their Epic schedule or to send a list of patient names to the schedulers. The schedulers would then convert the appointment and make patient contact. Detailed workflows for the exchange of this information were developed and implemented with rapid Plan-Do-Study-Act cycles.
5.2.3. Patient support
The YM Telehealth team recognized that helping patients of all levels of technological literacy to become comfortable with MyChart and troubleshooting technical issues, is essential to the use, adoption and success of this application.12 Two layers of support were offered during COVID-19: (1) MyChart support, whereby a dedicated group of scheduling staff and volunteer managerial staff were trained to call and assist patients prior to their scheduled visit, to help them sign up for MyChart, download the application to a smartphone or tablet and then test the internet connection. If a patient did not have the technology needed, they were offered the option to complete a telephone consult. (2) Technical troubleshooting support offered by dedicated IT personnel for issues such as setting up devices or re-setting passwords (MyChart, Apple or Android); patients were transferred to technical support by a YM staff member.
5.2.4. Virtual Rooming Assistants (VRA)
Recognizing the value-addition of multidisciplinary teams in virtual settings, as well as the opportunity to mirror the usual in-person clinical workflow in a virtual world, the VRA initiative was set up in late March. The YM Telehealth team partnered with YM Operations to pilot VRA workflows with Plan-Do-Study-Act cycles, prior to widely scaling across all specialties.
A VRA is usually a Medical Assistant (MA), Physician Assistant (PA) or nurse. The VRA can sign into Epic prior to the appointment to notate the patient has ‘arrived’ in the virtual waiting room, room the patient and then document vitals, History of Present Illness and Review of Systems on the EHR. The VRA can also directly notate on Epic that the patient is ‘ready for provider’ since before the VRA workflow this was done via alternative means of communication such as phone/e-mail/text. Furthermore, the VRA can provide real-time IT troubleshooting to prepare the patient for the visit, resulting in an efficient virtual clinic flow while allowing the provider to focus their time on clinical care. Positive physician and patient feedback underscore the success of this VRA workflow.
5.3. Frequent and ongoing communication, training and support
Given the need to keep diverse stakeholders informed in the context of a rapidly evolving regulatory and operations environment, the YM Telehealth team recognized the importance of clear and frequent communication. They distributed a weekly COVID-19 Telehealth Update to clinical and operational leaders throughout the system. The e-mail encompassed a weekly project tracker from all core teams supporting telehealth, an interactive dashboard displaying the volume of video visit conversions by managed entity and Epic department and most importantly, a list of ‘Need to Knows’ on the latest regulatory, operational and IT updates, which leadership then shared with their respective staff members. In hindsight, this centralized weekly communication established transparency and clarity, at a time of rapid change both within and outside the organization.
Additionally, educational material and intensive training was offered to keep providers and staff informed on both regulatory and operational changes. In mid-March, the YM Telehealth team widely shared pre-existing ‘Tip Sheets’ with instructions on how to successfully complete a video visit. They constantly requested feedback from providers as well as clinical and operational leads. This feedback highlighted that while the educational material gave providers a basic understanding of video visits, it did not lead to wider competence in using telehealth technologies; numerous providers had similar questions and many requested live trainings. In response, the YM Telehealth team modified the prior ‘Tip Sheets’ and recruited the help of an internal team specializing in employee trainings to deliver regular live trainings. They conducted hourly training sessions for providers via Zoom, with the same topic offered multiple times a week to accommodate uncertain schedules. Feedback from these were highly positive and in hindsight, provided much needed clarity on accessing and using telehealth during COVID-19.
6. Unresolved questions and lessons for the field
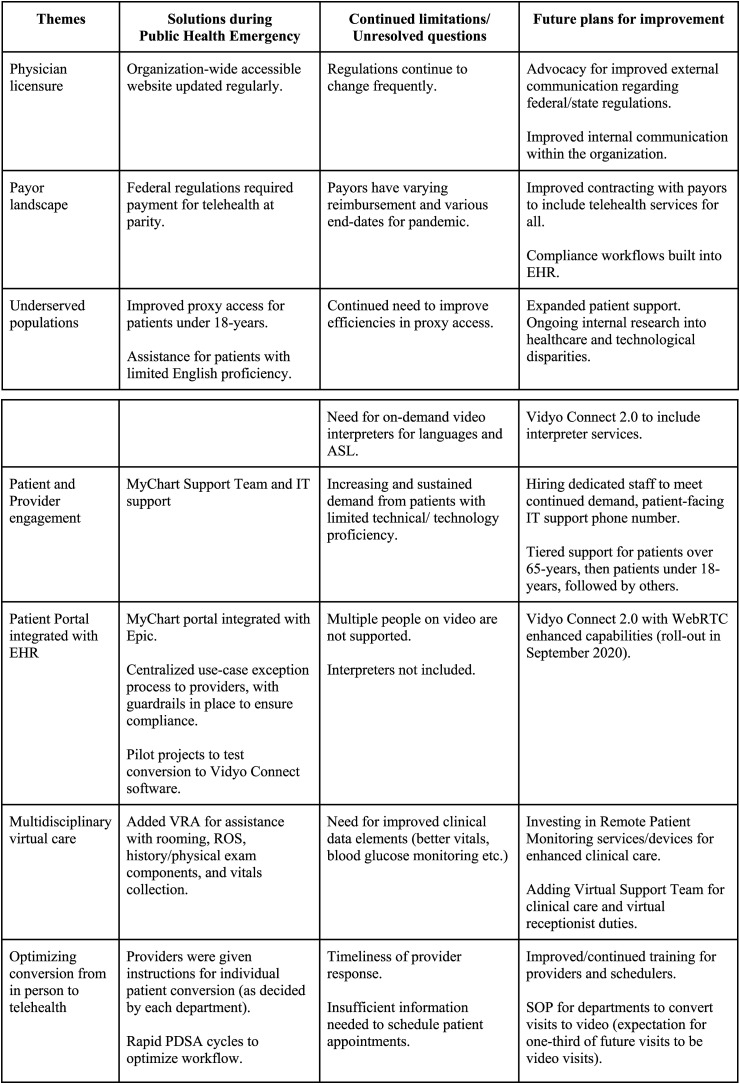
Overall, the COVID-19 telehealth initiative at YM was successfully implemented and scaled across all specialties. However, there remain important lessons learned, unresolved questions, and plans for improvement given the promising capabilities of virtual healthcare delivery in future (see Fig. 5 ).
Fig. 5.
Lessons learned from rapidly scaling Telehealth during COVID-19, continued limitations and future plans for improvement. Source: Yale Medicine. Note: VRA = Virtual Rooming Assistant; RTC = Real-Time Communication. PDSA = Plan-Do-Study-Act.
6.1. Future physician licensing issues
We found significant variability and therefore a critical need to track, manage and communicate current licensure requirements for each state during the public health emergency. We also needed to communicate and incorporate current licensure status for accurate scheduling.
6.2. Payor landscape unknown
Uncertainties on the reimbursement following the crisis, pose challenges for telehealth planning. Coordination between EHR and compliance is vital, with built-in automation where possible to assist providers to complete legal requirements and payor requests.
6.3. Underserved populations
This crisis has highlighted the growing healthcare disparities for underserved and vulnerable populations. Patients may lack devices, technology literacy, or access to reliable internet to complete the video successfully. Interpreter services and treating patients who are deaf or hard of hearing was also an important issue. Additional concerns for pediatric patients arose, as providers balanced patient privacy while encouraging parents and guardians to engage in treatment. System-wide efforts are underway to address each of these, including long-term research and investments in infrastructure, education, staffing, and technologies.
6.4. Patient and provider engagement
An important component of communication was the ability to manage and solve technological issues as they arose. Given how essential patient-facing support services are for the patient experience, engagement and willingness to use MyChart, operational plans are underway to create a larger and permanent group for MyChart support, as well as to create a direct patient-facing number for technical troubleshooting.
Together, these lessons suggest that while the implementation of telehealth was largely successful during COVID-19, in future, additional efforts must be dedicated to continuously improve patient/provider accessibility, technological literacy and satisfaction to ensure the long-term sustainability of telehealth.
Disclaimer
The views expressed in this article represent the authors' views and not necessarily the views or policies of their respective affiliated institutions.
Funding/support
None.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to thank Lynne Midolo and Dr. Howard Forman for their contributions to the development of this manuscript.
References
- 1.Toner M., Tompkins R.G. Invention, innovation, entrepreneurship in academic medical centers. Surgery. 2008;143:168–171. doi: 10.1016/j.surg.2007.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CMS . vols. 1–14. 2020. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet (Medicare Telemedicine Health Care Provider Fact Sheet, Centers Medicare Medicaid Serv). (accessed June 8, 2020) [Google Scholar]
- 3.CMS Physicians, Clinicians Other. CMS Flexibilities to Fight COVID-19. 2020. https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth- accessed June 8, 2020.
- 4.Academic Medical Centers — Strategies Mergers, Goals and Affiliations. https://www.beckershospitalreview.com/hospital-physician-relationships/academic-medical-centers-strategies-mergers-goals-and-affiliations.html (n.d.) (accessed June 8, 2020)
- 5.Barrett D.J. The evolving organizational structure of Academic Health Centers: the case of the University of Florida. Acad Med. 2008;83:804–808. doi: 10.1097/ACM.0b013e318181d054. [DOI] [PubMed] [Google Scholar]
- 6.Yale Medicine . 2020. Read the Yale Medicine 2019 Annual Report < Yale School of Medicine.https://medicine.yale.edu/news-article/22860/ accessed. [Google Scholar]
- 7.Tuckman B.W. Developmental sequence in small groups. Psychol Bull. 1965;63:384–399. doi: 10.1037/h0022100. [DOI] [PubMed] [Google Scholar]
- 8.Burke C.S., Georganta E., Marlow S. A bottom up perspective to understanding the dynamics of team roles in mission critical teams. Front Psychol. 2019;10 doi: 10.3389/fpsyg.2019.01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alabi G. Concepts for managing in turbulent times: received wisdom from Dr. Deming. Int J Manag Inf Syst. 2011;16:11. doi: 10.19030/ijmis.v16i1.6718. [DOI] [Google Scholar]
- 10.CMS, Hospitals Teaching. Teaching physicians and medical residents: CMS flexibilities to fight. COVID- 2020;19 [Google Scholar]
- 11.US Department of Health and Human Services . HHS Heal. Inf. Priv.; 2020. Notification of enforcement discretion for telehealth.https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html (accessed June 8, 2020) [Google Scholar]
- 12.Ramsey A., Lanzo E., Huston-Paterson H., Tomaszewski K., Trent M. Increasing patient portal usage: preliminary outcomes from the MyChart genius project. J Adolesc Health. 2018;62:29–35. doi: 10.1016/j.jadohealth.2017.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]