Abstract
The novel coronavirus 19 SARS-CoV2 caused a change in the practice of Otolaryngology around the globe. The high viral load in the nasal cavity, nasopharynx and airway subjects Otolaryngologists to a high risk of catching the virus during aerosol generating procedures. After the first outbreak wave has subsided, many teams are now discussing how our ‘new normal’ practice will look. We share our guidelines on restarting elective clinical work in order to create a safe environment for patients and staff in a Pediatric Otolaryngology outpatient clinic.
Keywords: COVID-19, SARS-CoV2, Clinical practice guidelines, Pediatric otolaryngology
1. Introduction
In December 2019 the first human infection with the new virus called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was described in Wuhan [1]. Since then it's resulting disease, termed coronavirus disease 2019 (COVID-19), has spread rapidly around the world, with the World Health Organization declaring a pandemic health emergency in March 2020 [2]. The highest viral load has been found in the nose and throat, which puts Otolaryngologists directly at risk of infection [3]. Several centers published guidelines of reorganization Otolaryngology departments for the first phase of the pandemic [[4], [5], [6]]. Most recently, the rate of new infections has slowly decreased in some parts of the world and a discussion about restarting outpatient clinics has begun. We describe our experience with reorganizing our outpatient Pediatric Otolaryngology clinic during the second phase of the pandemic, with the aim of creating a safe ‘new normal’ for healthcare workers and patients.
2. Main text
2.1. Team
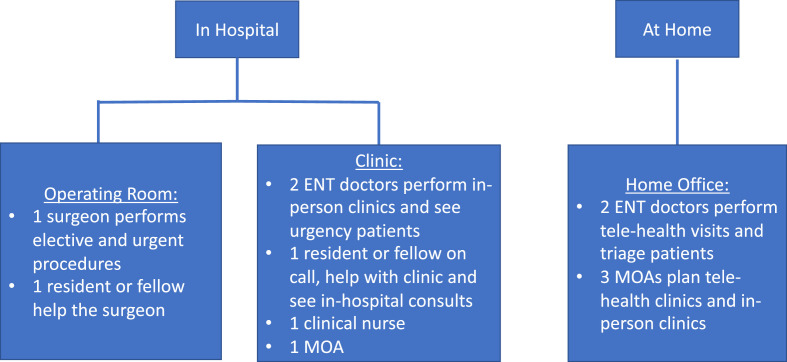
Our team consists of five Pediatric Otolaryngologists. For restarting elective clinics, a maximum of two physicians will run clinics simultaneously. One surgeon will be running an initially reduced elective operating list, with a plan to increase cases up to full operating capacity over four weeks. The rest of the physicians will work remotely from home performing telehealth clinics, with telehealth being shown to be helpful for the families despite some challenges [7]. One Resident and one Fellow are supporting the team, and are given a choice on whether they want to be involved in cases in clinics or operating rooms on case-by-case basis. Medical students are not undertaking placements as determined by the University. One medical office assistant (MOA) is physically in the clinic and assists the patients with their appointment. The other MOAs work remotely from home and schedule appointments by phone. One clinical nurse supports the physicians in the clinic (Fig. 1 ).
Fig. 1.
Team Division and responsibilities.
2.2. Clinic facilities
Patients are to spend as little time as possible in the waiting room. If patients need to wait in the common area, seats have been separated to maintain social distancing (2 m) and toys and magazines have been removed. The MOA is protected by a plexiglass shield on the desk and a mask during contact with patients. Each physician employs at least two different examination rooms, which allows cleaning in between patients without time wastage. The largest rooms of the clinic are used to facilitate social distancing. Aerosol generating procedures (e.g. nasal endoscopy) are performed in a negative pressure room which is designated for this purpose alone. The use of portable HEPA purifiers could be considered as recommended by Christopherson et al. [8]. Unnecessary equipment has been removed from the rooms. Only equipment required for each individual patient is to be out during a consultation, with all dirty and unused equipment removed at the end of each consultation. A filter on the suction should be considered. Thorough cleaning of surfaces with >70% alcohol wipes must be performed after every patient visit as it is known that the virus can remain on surfaces for hours to days [9].
2.3. Appointments
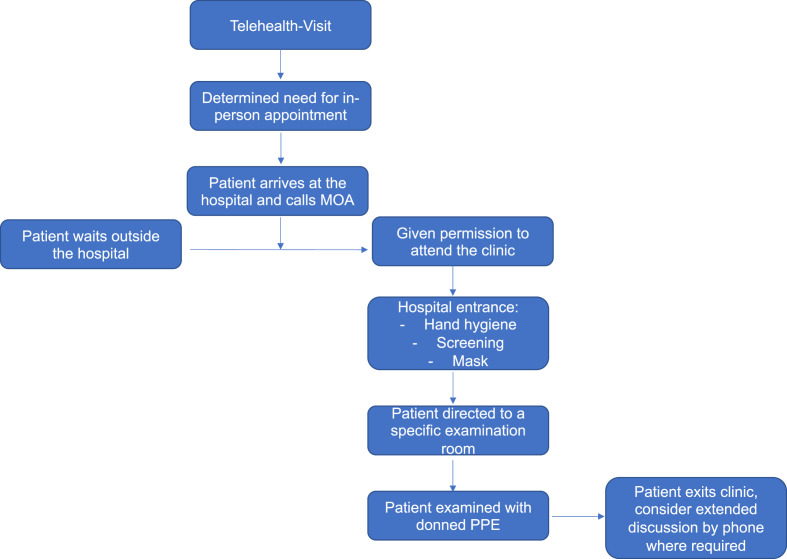
All patients are evaluated via a physician telehealth consultation to be triaged. Full history is taken and a provisional plan formulated, including whether in-person appointment is required, and to determine if a trans-nasal flexible fiberoptic-laryngoscopy (FFL) will be needed. If the patient needs to be seen in person, a clinic appointment will be scheduled and COVID-19 screening will be performed by phone. No COVID-19 testing will be required in asymptomatic patients. Only one parent will be allowed to accompany the child to the clinic. It is requested that face masks are worn. They are informed to call the MOA on their arrival to the hospital. If an empty examination room is available, they will be directed to come to the clinic to that specific room. If not, they will be asked to wait outside the hospital or in their car until they are contacted by the MOA. Hand-hygiene and screening will be performed at the outpatient buildings entrance. The patient in-person visit should be as short as possible, using notes from the telehealth consultation as an aid to direct the examination. Prolonged in-person communication should be minimized, with further extended discussions possible via phone where needed (Fig. 2 ). The patient volume is reduced by scheduling longer appointment intervals (e.g. 30 min) allowing time for personal protective equipment (PPE) donning and doffing, cleaning of consultation rooms and telehealth consultations between in-person appointments.
Fig. 2.
Flow-chart for our outpatient clinic appointments.
2.4. Examinations
For a normal Ear Nose Throat (ENT) examination, the physician is wearing contact and droplet protections (mask with a face shield or goggles, gown, gloves). For aerosol generating procedures we recommend using a N95 mask with goggles or PAPR (if available) as recommended by Howard, but local guidelines should be followed for PPE [10]. FFL should be performed by using a camera, screen and video capture equipment to maximize the distance between the patient and the physician and limit the time needed to scope. In view of the often difficult compliance in children during FFL, we recommend considering N95 masks even in asymptomatic patients. The use of a pre-prepared modified mask for the patient with a hole for the scope should also be considered to cover the nose and the mouth during the endoscopy depending on the age and the compliance of the patient. A significant reduction of aerosol spread has been shown [11]. The scope is wiped and stored in a covered box before transport for sterilization.
3. Discussion
The first phase of the pandemic changed the practices of Otolaryngologists all over the world to a largely emergency-driven service [4,5]. With reducing COVID-19 case numbers in many countries and lockdown measures being eased, Otolaryngologists are working towards restarting their elective clinics. Telehealth has been useful in recent weeks and will continue to play an important role in the future, especially with reduced ability to see as many patients face-to-face as previously [12]. Avoiding waiting time and crowding in the clinic, along with continued social distancing and basic precautions is paramount. Protection of healthcare-workers and patients must continue to be at the forefront of planning. Additionally, the training needs of residents and fellows must be addressed [13].
4. Conclusion
Our guidelines describe a thoughtful plan for restarting Pediatric Otolaryngology outpatient clinic for the next few months.
Sponsorships
None.
Funding source
None.
CRediT authorship contribution statement
Katharina Leitmeyer: Writing - original draft, originated idea, co-wrote and edited manuscript, final approval, accountability. Mark Felton: Writing - original draft, originated idea, co-wrote and edited manuscript, final approval, accountability. Neil K. Chadha: Writing - original draft, originated idea, co-wrote and edited manuscript, final approval, accountability.
Declaration of competing interest
None.
References
- 1.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020 Feb 28 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO). WHO Director-General's Opening Remarks at the Media Briefing on COVID-19: 11 March 2020. Published March 11, 2020.
- 3.Zou L., Ruan F., Huang M. SARS-CoV-2 viral load in upper respiratory specimen of infected patients. N. Engl. J. Med. 2020;382(12):1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leboulanger N., Sagardoy T., Akkari M. COVID-19 and ENT pediatric otolaryngology during the COVID-19 pandemic. Guidelines of the French association of pediatric otorhinolaryngology (AFOP) and French society of otorhinolaryngology (SFORL) Eur Ann Otorhinolaryngol Head Neck Dis. 2020 Apr 18 doi: 10.1016/j.anorl.2020.04.010. pii: S1879-7296(20)30100-30109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Givi B., Schiff B.A., Chinn S.B. Safety recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic. JAMA Otolaryngol Head and Neck Surg. 2020. Mar 31 doi: 10.1001/jamaoto.2020.0780. [DOI] [PubMed] [Google Scholar]
- 6.De Bernardi F., Turri-Zanoni M., Battaglia P., Castelnuovo P. How to reorganize an ear, nose and throat outpatient service during the COVID-19 outbreak: report from northern Italy. Laryngoscope. 2020 May 5 doi: 10.1002/lary.28716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sarah E., Maurrasse S.E., Rastatter J.C., Hoff S.R., Billings K.R., Valika T.S. Telemedicine during the COVID-19 pandemic: a pediatric otolaryngology perspective. Otolaryngol. Head Neck Surg. 2020 Sep;163(3):480–481. doi: 10.1177/0194599820931827. Epub 2020 May 26. [DOI] [PubMed] [Google Scholar]
- 8.Christopherson D.A., Yao W.C., Lu M., Vijayakumar R., Sedaghat A.R. High-efficiency particulate air filters in the era of COVID-19: function and efficacy. Otolaryngol. Head Neck Surg. 2020 Jul 14 doi: 10.1177/0194599820941838. 194599820941838. [DOI] [PubMed] [Google Scholar]
- 9.Van Doremalen N., Lloyd-Smith J.O., Munster V.J. Aerosol and surface stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020 Apr 16;382(16):1564–1567. doi: 10.1056/NEJMc2004973. Epub 2020 Mar 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Howard B.E. High-Risk aerosol-generating procedures in COVID 19: respiratory protective equipment considerations. Otolaryngol. Head Neck Surg. 2020 Jul;163(1):98–103. doi: 10.1177/0194599820927335. Epub 2020 May. [DOI] [PubMed] [Google Scholar]
- 11.Workman A.D., Welling D.B., Carter B.S., Curry W.T., Holbrook E.H., Gray S.T., Scangas G.A., Bleier B.S. Endonasal instrumentation and aerosolization risk in the era of COVID-19: simulation, literature review, and proposed mitigation strategies. Int Forum Allergy Rhinol. 2020 Apr 3 doi: 10.1002/alr.22577. [DOI] [PubMed] [Google Scholar]
- 12.Hagge D., Knopf A., Hofauer B. Telemedicine in the fight against SARS-COV-2-opportunities and possible applications in otorhinolaryngology : narrative review. HNO. 2020 Apr 16 doi: 10.1007/s00106-020-00864-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Comer B.T., Gupta N., Mowry S.E., Malekzadeh S. Otolaryngology education in the setting of COVID-19: current and future implications. Otolaryngol. Head Neck Surg. 2020 Apr 28 doi: 10.1177/0194599820923621. 194599820923621. [DOI] [PubMed] [Google Scholar]