Abstract
Background
There is an increasing trend toward regionalization of emergency general surgery, which burdens patients. The absence of a standardized, emergency general surgery transfer algorithm creates the potential for unnecessary transfers. The aim of this study was to evaluate clinical reasoning prompting emergency general surgery transfers and to initiate a discussion for optimal emergency general surgery use.
Methods
Consecutive emergency general surgery transfers (December 2018 to May 2019) to 2 tertiary centers were prospectively enrolled in an institutional review board–approved protocol. Clinical reasoning prompting transfer was obtained prospectively from the accepting/consulting surgeon. Patient outcomes were used to create an algorithm for emergency general surgery transfer.
Results
Two hundred emergency general surgery transfers (49% admissions, 51% consults) occurred with a median age of 59 (18 to 100) and body mass index of 30 (15 to 75). Insurance status was 25% private, 45% Medicare, 21% Medicaid, and 9% uninsured. Weekend transfers (Friday to Sunday) occurred in 45%, and 57% occurred overnight (6:00 pm to 6:00 am). Surgeon-to-surgeon communication occurred with 22% of admissions. Pretransfer notification occurred with 10% of consults. Common transfer reasons included no surgical coverage (20%), surgeon discomfort (24%), or hospital limitations (36%). A minority (36%) underwent surgery within 24 hours; 54% did not require surgery during the admission. Median length of stay was 6 (1 to 44) days.
Conclusion
Conditions prompting emergency general surgery transfers are heterogeneous in this rural state review. There remains an unmet need to standardize emergency general surgery transfer criteria, incorporating patient and hospital factors and surgeon availability. Well-defined requirements for communication with the accepting surgeon may prevent unnecessary transfers and maximize resource allocation.
Introduction
Emergency general surgery (EGS) accounts for more than 3 million hospital admissions in the United States annually.1 National trends indicate increasing regionalization of care for these patients, with nearly 85% of EGS admissions being treated in urban hospitals.1 , 2 While some have hypothesized a combination of explanations to account for these trends, including a shortage of rural general surgeons and an increasing concern surrounding malpractice, the true impetus remains unclear.1 , 2
There are arguments both in favor of and in opposition to the regionalization of EGS care in the United States.3 Proponents of regionalization argue that this model provides critical access to EGS care for communities who lack surgical coverage or the resources to care for the critically ill and that high-volume centers have shown better outcomes. Opponents argue that regionalization burdens patients and their families and places a strain on urban hospital systems, without providing a clear clinical benefit.4 Some have hypothesized that nearly 10% of EGS interhospital transfers are unnecessary and that outcomes for EGS transfer patients are worse when compared to nontransfer patients. Others argue that this difference in outcomes is small and that transfer patients represent a higher acuity population.2 , 5 , 6
Specific, standardized criteria guide transfers in other surgical fields, such as trauma and burn care, reducing subjectivity.7 , 8 There is currently an unmet need to similarly standardize criteria for interhospital transfer of EGS patients to tertiary referral centers. Standardizing the care paradigm in this patient population could potentially avert unnecessary patient transfer, ultimately mitigating burden on patient families and optimizing resource allocation across the health care system. Developing such criteria begins with gaining an understanding of the clinical reasoning prompting interhospital transfer in this patient population. Our study aimed to identify the reasons behind EGS interhospital transfers to tertiary care centers in a rural state. Using this data, we aimed to establish criteria for EGS transfers.
Methods
Under an institutional review board–approved protocol, consecutive patient transfers initiated from outlying hospitals in a rural state to the nontrauma EGS services at 2 tertiary referral centers between December 2018 and May 2019 were prospectively enrolled. Enrollment criteria included transfer patients who were directly admitted to the EGS service or transfer patients who received EGS service consultation within 48 hours of admission. The day and time of transfer, the specialty of the transferring provider, and the name of the transfer facility were collected for each patient.
For patients directly admitted to the EGS service, details surrounding the clinical reasoning for transfer were obtained directly from the accepting surgeon who discussed the patient with the transferring provider. Transfers were categorized as being due to an absence of surgical coverage at the referring facility, surgeon discomfort with the required procedure, hospital limitations (including inability to care for patient comorbidities, unavailability of required diagnostic modalities, or need for a specialty service such as interventional radiology or interventional endoscopy), continuity of care, or patient preference.
For consults to the EGS service, details regarding the clinical reasoning for surgical consultation, as well as the level of involvement of the consulting surgeon prior to patient transfer, were obtained from the consulting surgeon. Patient characteristics and outcomes were obtained through chart review.
Patients accepted for transfer by specialty services, such as trauma surgery, colorectal surgery, or surgical oncology, were not included. Specifically, patients with surgical diagnoses related to a traumatic injury, a known diagnosis of inflammatory bowel disease or malignancy, a necrotizing pancreatitis, hepatic pathologies, or conditions requiring biliary reconstruction were excluded. Consults for minor surgical issues unrelated to the admission diagnosis, such as gastrostomy tube placement, tracheostomy, incision and drainage of minor abscesses, etc, were also not included. Surgical intervention was considered emergency if it occurred within 1 hour of admission or surgical consultation, urgent if it occurred between 1 and 24 hours, or delayed if it occurred greater than 24 hours after admission or surgical consultation but during the same hospitalization.
Descriptive statistics were obtained. Statistical calculations were performed using R software (R Foundation for Statistical Computing, Vienna, Austria). Data were used to create an algorithm to standardize EGS transfer criteria to tertiary centers. The acute physiology and chronic health evaluation (APACHE II) score uses 12 commonly collected physiologic measurements, in combination with patient age and pre-existing comorbidities, to provide a prognostic indicator for patients presenting to the hospital.9 The scoring system was included in our algorithm as a potential tool to stratify illness severity for EGS patients prior to transfer.
Results
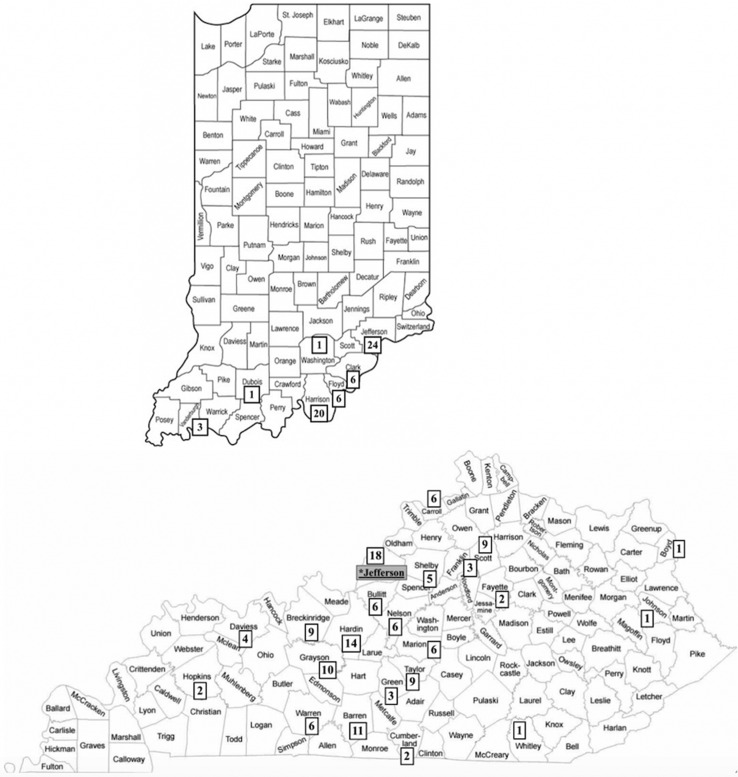
Two hundred patients transferred from 39 hospitals spanning 29 counties in Kentucky and southern Indiana were enrolled (Fig 1 ). Median age was 59 (range, 18 to 100) (Table I ). Median body mass index was 30 (range, 15 to 75). Half were direct admissions to the EGS service, and half were consultations for the EGS service after transfer. Nearly half of patients were enrolled in Medicare as their primary insurance. The remaining patients had private insurance (25%), Medicaid (21%), or were self-pay (9%). One-third of the patients were admitted to the intensive care unit. The remaining patients were admitted to either progressive care units (18%) or medical-surgical units (49%). The most common EGS diagnoses on admission related to small bowel (20%), pancreaticobiliary (19%), gastric/foregut (16%), and colonic (16%) pathologies.
Fig. 1.
Number of EGS transfers from referring Kentucky and Indiana counties. ∗Location of study tertiary referral center.
Table I.
Patient characteristics
| n (%) or median (range) | |
|---|---|
| EGS transfers | 200 |
| Surgery admissions | 98 (49%) |
| Surgery consults | 102 (51%) |
| Age (y) | 59 (18–100) |
| BMI (kg/m2) | 30 (15–75) |
| Insurance status | |
| Medicare | 91 (45%) |
| Private | 50 (25%) |
| Medicaid | 42 (21%) |
| Self-pay | 17 (9%) |
| Level of care on admission | |
| Intensive care unit | 66 (33%) |
| Progressive care unit | 35 (18%) |
| Medical-surgical floor | 99 (49%) |
| Transfer diagnosis | |
| Small bowel | 41 (20%) |
| Pancreaticobiliary | 38 (19%) |
| Gastric/foregut | 31 (16%) |
| Colonic | 31 (16%) |
| Skin and soft tissue infection | 24 (12%) |
| Hernia | 15 (7%) |
| Appendix | 4 (2%) |
| Other | 16 (8%) |
BMI, body mass index.
The day of transfer was split roughly evenly between weekday (Monday to Thursday) (55%) versus weekend (Friday to Sunday) (45%) transfers (Table II ). Transfers were slightly more frequent at night (1800 to 0600) (57%) versus during the day (0600 to 1800) (43%).
Table II.
EGS transfer details
| n (%) or median (range) | |
|---|---|
| Day of transfer | |
| Weekday (Monday to Thursday) | 111 (55%) |
| Weekend (Friday to Sunday) | 89 (45%) |
| Time of transfer | |
| Day (0600 to 1800) | 85 (43%) |
| Night (1800 to 0600) | 115 (57%) |
| Pretransfer communication | |
| Surgeon-to-surgeon (admissions only) | 22 (22%) |
| Admitting MD-to-surgeon (consults only) | 10 (10%) |
| Stated reason for transfer (admissions only, n = 98) | |
| Hospital limitations | 35 (36%) |
| Surgeon discomfort | 23 (24%) |
| Presence of comorbidities | 6/23 (26%) |
| Cirrhosis | 3 |
| Obesity | 2 |
| Advanced age | 1 |
| Complexity of diagnosis/surgical intervention | 17/23 (74%) |
| Complex foregut | 7 |
| Complex fistula | 3 |
| Recurrent abdominal wall hernia | 2 |
| Colonic perforation | 2 |
| Complex perirectal abscess/necrotizing fasciitis | 2 |
| Open cholecystectomy | 1 |
| No on-call surgeon | 20 (20%) |
| Continuity of care | 14 (14%) |
| Patient request | 6 (6%) |
Of the 98 direct surgical admissions, the most common stated reason for transfer was hospital limitations (36%). This was followed by surgeon discomfort with providing the care required for the patient (24%), the absence of an on-call surgeon (20%), continuity of care (14%), and patient request (6%). In cases of surgeon discomfort (23 total), most were due to a stated discomfort with the required procedure (17, 74%). This was most commonly related to complex foregut pathologies requiring advanced foregut laparoscopy. Patient comorbidities, including cirrhosis, obesity, and advanced age, were the cited reasons for surgeon discomfort for the remaining patients (6, 26%).
Communication occurred between a surgeon at the transferring facility and a surgeon at the accepting facility in 22% of direct surgical admissions. Communication between the admitting physician and the consulting surgeon occurred prior to patient transfer in 10% of surgical consults.
One-quarter of the patients required emergent surgical intervention (Table III ). The most common emergency procedures included partial colectomy, drainage/debridement of skin and soft tissue infections, small bowel resection, and repair of gastric perforation. Eleven percent required urgent surgical intervention. The most common urgent procedures included laparoscopic cholecystectomy, small bowel resection, and drainage/debridement of skin and soft tissue infections. However, most patients (54%) did not require surgical intervention during their hospital stay.
Table III.
Patient outcomes
| n (%) or median (range) | |
|---|---|
| Surgical intervention∗ | |
| Emergency (<1 h) | 49 (25%) |
| Partial colectomy | 11 |
| Drainage/debridement of skin and soft tissue | 8 |
| Small bowel resection | 6 |
| Repair of gastric perforation | 6 |
| Paraesophageal hernia repair/gastropexy | 4 |
| Repair of abdominal wall hernia | 4 |
| Appendectomy | 3 |
| Evacuation of intra-abdominal abscess | 3 |
| Adhesiolysis | 1 |
| Other | 3 |
| Urgent (<24 h) | 23 (11%) |
| Laparoscopic cholecystectomy | 5 |
| Small bowel resection | 4 |
| Drainage/debridement of skin and soft tissue | 4 |
| Evacuation of intraabdominal abscess | 2 |
| Open cholecystectomy | 2 |
| Paraesophageal hernia repair/gastropexy | 2 |
| Partial colectomy | 1 |
| Adhesiolysis | 1 |
| Other | 2 |
| Delayed (>24 h) | 20 (10%) |
| Drainage/debridement of skin and soft tissue | 6 |
| Laparoscopic cholecystectomy | 4 |
| Evacuation of intra-abdominal abscess | 2 |
| Open cholecystectomy | 2 |
| Small bowel resection | 1 |
| Adhesiolysis | 1 |
| Other | 4 |
| None | 108 (54%) |
| Not indicated | 55 |
| Conservative management | 48 |
| Palliative care | 5 |
| Length of stay (days) | 6 (1–44) |
| ≲4 d | 84 (42%) |
| 5–9 d | 61 (30%) |
| ≳10 d | 55 (28%) |
| Disposition | |
| Home | 139 (70%) |
| Subacute rehabilitation | 40 (20%) |
| Long-term acute care | 5 (2%) |
| Palliative care | 11 (6%) |
| Death | 5 (2%) |
Time to surgical intervention is listed in relation to admission time for surgical admissions and in relation to consultation time for surgical consultations.
Median length of stay was 6 (1–44) days. Most patients (70%) were discharged directly to their homes. Eleven (6%) patients were referred to palliative care, 7 of whom did not undergo any operative intervention before referral. Five (2%) died, all from complications related to their EGS diagnosis.
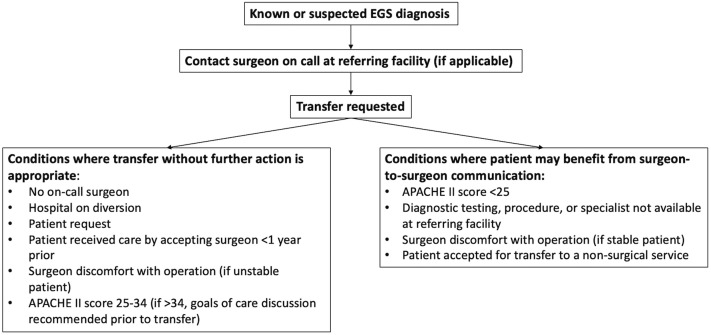
Using this data, we proposed an algorithm defining criteria for EGS transfer (Fig 2 ). This algorithm attempts to identify situations in which surgeon-to-surgeon communication might prevent unnecessary patient transfer by considering objective versus subjective reasons for transfer, as well as patient stability and comorbid status.
Fig. 2.
Proposed algorithm outlining criteria for EGS transfers to tertiary referral centers.
The algorithm recommends direct surgeon-to-surgeon communication before transfer when the stated reason for transfer is surgeon discomfort, provided the patient is considered stable by the referring facility and the patient’s APACHE II score is less than 25 (indicating an inpatient mortality rate of less than 40%).9 Additionally, when the need for diagnostic testing, specialty procedures (such as interventional radiology or endoscopic retrograde cholangiopancreatography), or care from a specialty service is the stated reason for transfer, direct surgeon-to-surgeon communication to determine the likelihood of the patient needing these resources is recommended. Direct communication with the surgeon at the transfer facility is also recommended when a patient with a surgical diagnosis is accepted for transfer to a nonsurgical service.
Our algorithm recommends transfer without additional consultation when there is an absence of surgical coverage or bed availability at the referring facility, the patient is an established patient at the transfer facility, or the patient requests the transfer. When the stated reason for transfer is surgeon discomfort and the patient is considered hemodynamically unstable by the referring physician or has an APACHE II score of 25 to 34 (predicted inpatient mortality rate of 55% to 75%), transfer without additional consultation is also recommended.9 For patients with APACHE II scores of 35 or higher (predicted inpatient mortality rate greater than 85%), our algorithm recommends a goal-of-care discussion prior to proceeding with transfer.
Discussion
Evaluation of national patient databases indicate an increase in the proportion of interhospital transfers among EGS admissions in the United States by 150% between 2002 and 2011.2 , 6 This practice burdens patients, who must travel long distances to obtain health care, as well as tertiary referral centers, who often suffer financially from caring for transferred patients.10 Our study is the first to prospectively delineate circumstances prompting transfer to tertiary centers for EGS diagnoses. Our results indicate that patients are most often transferred owing to limitations at the referring facility, followed closely by surgeon discomfort with the required procedures and an absence of surgical coverage at the referring facility. Adequate communication with the surgeon before transfer, in which the patient’s diagnosis, need for surgical intervention, and limitations at the referring facility are discussed, is rare. Additionally, greater than half of EGS transfer patients did not require surgical intervention, suggesting that interhospital transfer was, perhaps, unnecessary. Our proposed algorithm for EGS interhospital transfer focuses on enhancing communication with the accepting surgical service in order to avoid unnecessary interhospital transfers and to optimize use of health care resources.
Interhospital transfers are costly and use a significant amount of health care resources.10, 11, 12 Transfer patients generally have higher rates of comorbidities and a higher level of acuity, resulting in worse mortality and increased length of stay, compared to their directly admitted counterparts.2 , 5 , 6 , 13 , 14 As a result, tertiary referral centers oftentimes suffer a net financial loss in caring for these patients, particularly in the setting of value-based reimbursement models.10 Additionally, transfers over significant distances burden patients and their families during both the inpatient stay, as well as during the follow-up period.
The information available in national databases cannot explain why EGS transfers are on the rise.2 However, there are a number of proposed theories, including a critical shortage of rural general surgeons, an inability of smaller hospitals to provide postoperative care in the setting of extensive patient comorbidities and/or a need for critical care, and malpractice concerns for general surgeons in low-volume centers who lack training in more advanced surgical techniques.1 , 2 , 12 There is also a generalized notion that EGS transfers occur more frequently in the setting of less desirable patients who present at less desirable times, despite having uncomplicated surgical conditions. This notion is supported by Misercola et al, who found that insurance status does influence patient transfer.12 Furthermore, a declining mortality rate, a declining length of stay, and frequent discharge without surgical intervention among EGS transfers suggest that an increasing proportion of these transfers are not indicated.2 , 15
Our data indicate that reasons prompting transfer are multifactorial and often subjective, based on the surgeon’s comfort level with the indicated procedure and the surgeon’s belief in the referring facility’s ability to care for the patient. Despite the subjectivity of transfer indications, insurance status, day of the week, and time of day did not appear to play a significant role. Our findings are comparable to those found by Philip et al and Broman et al from the University of Wisconsin and Vanderbilt University, respectively.15 , 16 However, these were retrospective studies and did not include surgeon discomfort as a transfer reason.
An unexpected finding in our study was that half of transferred patients with EGS diagnoses were accepted for transfer by nonsurgical services and almost always bypassed any communication with the surgeon at the accepting facility. This method prevents any evaluation by the surgeon prior to transfer and results in a delay of resource mobilization when urgent or emergency surgical intervention is required, as occurred in 26% of the surgery consult cohort. In contrast, when no surgical intervention is required, which occurred in 70% of the surgery consult cohort, communication with the surgeon prior to patient transfer could potentially avoid the transfer altogether.
To understand the specific reasoning behind EGS transfers requires adequate communication between the referring and the accepting surgeons, which is frequently absent from the interhospital transfer process. Our algorithm to evaluate EGS transfers centers around filling this communication void. For patients who are unstable, patients with an increased mortality risk (as measured by the Apache II scoring system), and in situations where a surgeon is unavailable, the indication for transfer to a tertiary facility is generally well-established. However, for patients who are stable and with a low mortality risk, direct surgeon-to-surgeon communication could prevent interhospital transfers that are unlikely to provide additional benefit to the patient. Based on our data, this could specifically be of benefit when transfer is planned to a nonsurgical service or when a potential need for a specialty service, such as interventional radiology, is the indication for transfer.
When the referring facility lacks surgical coverage, telemedicine and image sharing platforms could provide an avenue through which enhanced communication could occur. This has been proven effective within the trauma referral system.17 With the increased use of such platforms as a result of the COVID-19 pandemic, streamlining this technology for broad, continued use is feasible. Particularly in rural states, this could provide a means of evaluation that could ultimately prevent unnecessary transfer when a surgeon is not available to review diagnostic imaging or to evaluate the patient in-person.
This study should be interpreted in light of several limitations. Data regarding clinical reasoning prompting transfer for the EGS consult cohort, specifically, was not available, as the consulting surgeon did not speak directly with the transferring facility in those situations. This comprises half of our patients, limiting our sample size for this metric. Because specialty services were not included in data collection, overlaps between diagnoses that could be managed by either an EGS or a specialty service could have been missed. However, the manner in which specialty services interact with the EGS service regarding transfers and consults at our institution likely limits this overlap. The APACHE II scoring system is not often calculated and likely not well known outside of the critical care community. While we recognize this as a limitation in our algorithm, there is not a widely accepted or widely available EGS-specific scoring system to assess illness severity and mortality risk.18 The APACHE II score combines both acute and chronic conditions into a simple calculation based on data that are collected on almost every patient seen in an emergency room. It is an easily translatable tool in applying objective metrics as a means of patient stratification. Finally, our algorithm was developed after evaluation of and in response to the data we collected. Because of this, we were unable to retrofit this algorithm to our cohort, due to its reliance on patient condition at presentation to the outside hospital and our limited access to this data. Prospective analysis of this algorithm is required.
In conclusion, EGS transfers burden patients and increase health care costs. Prior studies have concluded that many EGS transfers are unnecessary, but they have failed to identify the clinical reasoning prompting these transfers. Our study indicates that this process is frequently based on subjective reasoning and often without direct communication with the accepting surgeon. Our algorithm outlining criteria for EGS transfer addresses this void. Prospective application of this algorithm is needed to determine its effect on EGS transfer volume.
Conflicts of interest/Disclosures
All listed authors of this study have no conflicts of interest or disclosures.
Funding/Support
None.
References
- 1.Gale S.C., Shafi S., Dombrovskiy V.Y., Arumugam D., Crystal J.S. The public health burden of emergency general surgery in the United States: A 10-year analysis of the Nationwide Inpatient Sample--2001 to 2010. J Trauma Acute Care Surg. 2014;77:202–208. doi: 10.1097/TA.0000000000000362. [DOI] [PubMed] [Google Scholar]
- 2.Reinke C.E., Thomason M., Paton L., Schiffern L., Rozario N., Matthews B.D. Emergency general surgery transfers in the United States: a 10-year analysis. J Surg Res. 2017;219:128–135. doi: 10.1016/j.jss.2017.05.058. [DOI] [PubMed] [Google Scholar]
- 3.Santry H., Kao L.S., Shafi S., Lottenberg L., Crandall M. Pro-con debate on regionalization of emergency general surgery: controversy or common sense? Trauma Surg Acute Care Open. 2019;4 doi: 10.1136/tsaco-2019-000319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Urbach D.R. Pledging to eliminate low-volume surgery. N Engl J Med. 2015;373:1388–1390. doi: 10.1056/NEJMp1508472. [DOI] [PubMed] [Google Scholar]
- 5.Yelverton S., Rozario N., Matthews B.D., Reinke C.E. Interhospital transfer for emergency general surgery: An independent predictor of mortality. Am J Surg. 2018;216:787–792. doi: 10.1016/j.amjsurg.2018.07.055. [DOI] [PubMed] [Google Scholar]
- 6.Huntington C.R., Cox T.C., Blair L.J. Acuity, outcomes, and trends in the transfer of surgical patients: a national study. Surg Endosc. 2016;30:1301–1309. doi: 10.1007/s00464-015-4361-0. [DOI] [PubMed] [Google Scholar]
- 7.Sasser S.M., Hunt R.C., Faul M., and the Centers for Disease Control and Prevention (CDC) Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm Rep. 2012;61:1–20. [PubMed] [Google Scholar]
- 8.American Burn Association/American College of Surgeons Guidelines for the operation of burn centers. J Burn Care Res. 2007;28:134–141. doi: 10.1097/BCR.0b013e31802c8861. [DOI] [PubMed] [Google Scholar]
- 9.Knaus W.A., Draper E.A., Wagner D.P., Zimmerman J.E. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–829. [PubMed] [Google Scholar]
- 10.Keeven D.D., Harris C.T., Davenport D.L., Smalls B., Bernard A.C. Cost burden and mortality in rural emergency general surgery transfer patients. J Surg Res. 2019;234:60–64. doi: 10.1016/j.jss.2018.08.052. [DOI] [PubMed] [Google Scholar]
- 11.Keeven D.D., Davenport D.L., Bernard A.C. Escalation of mortality and resource utilization in emergency general surgery transfer patients. J Trauma Acute Care Surg. 2019;87:43–48. doi: 10.1097/TA.0000000000002291. [DOI] [PubMed] [Google Scholar]
- 12.Misercola B., Sihler K., Douglas M., Ranney S., Dreifus J. Transfer of acute care surgery patients in a rural state: a concerning trend. J Surg Res. 2016;206:168–174. doi: 10.1016/j.jss.2016.06.090. [DOI] [PubMed] [Google Scholar]
- 13.Santry H.P., Janjua S., Chang Y., Petrovick L., Velmahos G.C. Interhospital transfers of acute care surgery patients: should care for nontraumatic surgical emergencies be regionalized? World J Surg. 2011;35:2660–2667. doi: 10.1007/s00268-011-1292-3. [DOI] [PubMed] [Google Scholar]
- 14.Ingraham A., Wang X., Havlena J. Factors associated with the interhospital transfer of emergency general surgery patients. J Surg Res. 2019;240:191–200. doi: 10.1016/j.jss.2018.11.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Broman K.K., Poulose B.K., Phillips S.E. Unnecessary transfers for acute surgical care: Who and why? Am Surg. 2016;82:672–678. [PubMed] [Google Scholar]
- 16.Philip J.L., Saucke M.C., Schumacher J.R. Characteristics and timing of interhospital transfers of emergency general surgery patients. J Surg Res. 2019;233:8–19. doi: 10.1016/j.jss.2018.06.017. [DOI] [PubMed] [Google Scholar]
- 17.Rogers F.B., Ricci M., Caputo M. The use of telemedicine for real-time video consultation between trauma center and community hospital in a rural setting improves early trauma care: preliminary results. J Trauma. 2001;51:1037–1041. doi: 10.1097/00005373-200112000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Havens J.M., Columbus A.B., Seshadri A.J. Risk stratification tools in emergency general surgery. Trauma Surg Acute Care Open. 2018;3 doi: 10.1136/tsaco-2017-000160. [DOI] [PMC free article] [PubMed] [Google Scholar]