Abstract
Older adults frequently under-report depressive symptoms and often fail to access services after a disaster. To address unmet mental health needs, we developed a service delivery program (SMART-MH) that combines outreach, assessment, and therapy and implemented it in New York City after Hurricane Sandy. This study aimed to examine the feasibility, effectiveness, and patients’ engagement of our brief psychotherapy (“Engage”). We predicted that Engage would result in reductions of depression, and that the benefits would be comparable to those of a historical comparison group who received Engage in a controlled experimental setting. A total of 2,831 adults (age ≥ 60) impacted by Hurricane Sandy were screened for depression. Assessments and therapy were conducted in English, Spanish, Cantonese, and Russian. Depressed individuals (PHQ-9 ≥ 10) who were not in treatment were offered Engage therapy in their native language at local senior center/nutrition sites. Twelve percent of the participants reported depression (N = 333). Of these 333 participants, 201 (60%) were not receiving treatment and 143 agreed to receive Engage therapy. Linear mixed-effects model showed that depression severity decreased significantly over time. More than two thirds had a five-point reduction in PHQ-9 scores and post-treatment scores ≤9. Post-hoc comparison of standardized slopes of change found patterns of depression reductions equivalent to Engage provided in a controlled setting. Partnerships to integrate mental health care into community settings can increase detection of mental-health needs and access to services in patients’ native language. Brief reward exposure-based psychotherapy delivered in the community can provide comparable benefits to those achieved in research settings.
Keywords: Depression, Community-based interventions, Older adults
Older adults impacted by Superstorm Sandy with depression showed meaningful clinical reduction in depressive symptoms in response to a brief psychotherapy.
Implications.
Practice: Engage is a brief therapy for depression that may be useful for older adults with depression as it can be both offered in community settings and decrease depressive symptoms among a diverse older adult population.
Policy: Given the challenge of accessing care among post disaster victims, and vulnerable older adults, service delivery models that combine outreach, assessments, and streamlined therapy may increase access to care and improve mental health outcomes.
Research: Barriers to community implementation of evidence-based psychotherapies can be addressed by developing and testing streamlined approaches that match the skill set of practicing clinicians.
INTRODUCTION
According to the World Health Organization (WHO), the number of adults aged 60 years or older will rise from 900 million to 2 billion between 2015 and 2050 (moving from 12% to 22% of the total global population) [1]. In the USA, 15% of the population is 65 years of age, with older adults aged 85 years and older as the fastest growing subsample [2]. Nationally, 5.9% of the population suffers from depression [3] with higher rates found among older adults with chronic illness, needing emergency medical services or receiving aging support services [4–6].
Older adults with mental health needs do not receive the services they need; most older adults with anxiety and depressive disorders do not obtain treatment [7–9]. In the USA, most adults (73.3%) who receive treatment for depression are cared for in primary care settings, with a majority of patients (87%) receiving pharmacotherapy [9]. Older adults rarely receive psychotherapy for depression [9], even though they may prefer it to antidepressant treatment [10]. Untreated major depression in older adults is associated with increased rates of suicide [11], nonsuicidal mortality [12], risk of falling [13,14], and quality-adjusted life years [15]. Even mild depression takes a significant toll on quality of life among older adults [15]. Psychotherapy is as effective in decreasing symptoms of depression as it is in younger adults, and has been useful in improving functioning [16,17], and reducing mortality in the elderly [18].
Older adults are especially vulnerable to sudden changes in their environment caused by natural disasters given high rates of disability, medical conditions, and difficulty mobilizing [19]. Following Hurricane Sandy, studies suggested that older adults were among the most vulnerable and had the most difficulty navigating the complex bureaucracy surrounding government aid [20,21]. As a result, they were less likely than younger adults to receive disaster aid, had the least amount of communication with service providers, and the highest mortality rates [21]. Compared to younger adults, elders are more likely to present with symptoms of depression, Post-traumatic Stress Disorder, as well as general psychiatric morbidity following natural disasters [22]. Those older adults with prior depressive symptoms and depression diagnoses [23] and minority populations were found to be more likely to have depression and post-traumatic stress [24]. Elevated symptoms of mental health difficulties among individuals exposed to Hurricane Sandy remained years after the storm hurricane [25,26]. There was a decrease in depression rates reported among a sample interviewed 11–28 months after the storm when they were reinterviewed to 23–42 months after the storm; however, the decrease from 35.4% to 30.8% did not indicate a reduction of need in the community [27]. Thus, increasing the access of this population to mental health is crucial [23,28–30].
To address the unmet mental health needs of older adults, care should be integrated into other service delivery systems. Collaborative care [31,32] and the increase in community delivered therapies [33] can improve older adults’ access to psychosocial services in nonmental health sites. However, with the exception of collaborative care, few examples exist where mental health care is integrated and sustained into other settings that serve older adults.
Academic–community partnerships can develop science-informed mental health services that are integrated in nonmental health service settings and have the potential to overcome barriers and meet the mental health needs of diverse community older adults. In addition to limited availability, attitudes affect access to care among those who need services [34] and stigma remains a powerful deterent to accessing mental health services for older adults [35–37] especially for minority older adults [38,39]. Mental health services developed with a deployment focused model [19] where services are collaboratively constructed in the community setting are likely to be sustained and have favorable mental health outcomes. To improve treatment participation, our group has developed community-based mental health initiatives to provide psychoeducation, address barriers, and tailor mental health services to meet clients’ needs and personal goals. Based on a partnership model, a brief psychosocial intervention to improve engagement in mental health treatment, called Open Door [20,21], was implemented and improved the initiation of mental health services among homebound older adults [21]. To improve adherence to prescribed antidepressant therapy in primary care settings, we targeted barriers to care and helped older adults build a personalized adherence strategy [21]
To serve individuals impacted by disasters, mental health providers have brought services to impacted communities to reduce barriers to accessing and engaging in mental health care. REACH NOLA was a research-practice collaborative based on the principles of community participatory research to evaluate and address the unmet mental health needs in New Orleans. As part of this program, training on cognitive-behavioral therapy was provided to community therapists who found it useful, however less than a third of therapists were able to deliver CBT to a single client [22]. The investigators noted the need for effort at the outset and the importance of engaging administrators and therapists in community agencies to support the implementation. However, this approach may be insufficient to address the training and the caseload variability faced by community therapists [23]. Community–academic partnerships that can bring streamlined therapies to sites with unmet needs to serve the diverse, multilingual population can improve service delivery and have potential for sustainability.
To address the needs of New York City’s older adults outside of traditional service sectors (e.g., primary care, mental health clinics), a government–academic partnership demonstration project was funded by a New York State Block Grant. Funds were allocated by FEMA to identify community aging service and mental health needs and offer services based in the community. The SMART-MH (Sandy Mobilization, Assessment, Referral and Treatment for Mental Health) [28] was the first program to integrate community outreach activities to identify and serve the mental health needs of older adults living in NYC areas affected by Hurricane Sandy. Analysis of a subsample (N = 1,512) of the total sample (N = 2,813) indicated high rates of depression, especially in older adults younger than 75 years [28]. These findings indicated that mental health needs persist for months and even years after a disaster [24,29,30].
The aim of the current study was to examine the rates of client engagement and the impact of Engage therapy, delivered in four languages as part of the SMART-MH program. Engage is a neurobiologically informed psychotherapy [40], whose principal intervention is reward exposure [41,42]. We predicted that Engage would lead to clinically meaningful reductions in depression in this population. Additionally, we investigated whether Engage led to comparable depressive symptom change to that of a historical comparison group treated with Engage in a clinical trial [42]. We predicted that Engage will show a statistically indistinguishable rate of depressive symptom reduction among an ethnically diverse and multilingual population of older adults affected by Hurricane Sandy.
Method
Participants
All older adults (age ≥ 60 years) who resided within NYC Flood Zones 1 and 2 in New York City during Hurricane Sandy were eligible for participation. SMART-MH interdisciplinary and multilingual staff worked with community agency and congregate meal staff in impacted communities to conduct outreach activities to identify eligible older adults impacted by Hurricane Sandy. Participants were consented to participate in the New York City Department for the Aging (DFTA) needs assessment. Storm impact was determined based on a single self-report item where clients were asked to verify that they had been living in the flood zone during the hurricane. These questions enabled us to exclude individuals who were new to the area and not impacted.
From October 31, 2014, through July 7, 2016 (24–44 months after the storm), a total of 2,831 needs assessments were conducted by staff with older adults in four languages (Spanish, Russian, Cantonese, and English). Assessments and weekly PHQ-9 data were entered into the DFTA database and deidentified data were released to University Name for evaluation and outcome analyses after review by the University name (IRB # 1504016137).
Measures
The New York City Department for the Aging (DFTA) needs assessment includes the PHQ-9 to assess depressive symptoms and a score of 10 or above with the endorsement of at least one gateway symptom (depressed mood or anhedonia) indicated clinically significant depression consistent with screening guidelines [43]. We utilized relatively stringent criteria for “clinically significant improvement,” defined as (a) final PHQ-9score of less than 10; and (b) a five-point reduction on the PHQ-9 [44]. Clients who endorsed suicidal ideation at baseline assessment were administered the Suicide Risk Assessment [45] to evaluate risk level. Results were then reviewed by a senior licensed clinician and safety plans were implemented.
To assess participant’s perception of negative storm impact, an overall storm-related loss rating was reported by each participant using a scale of 1–10. Instrumental activities of daily living were assessed using three items from the Multi-level Assessment Inventory [46], assessing capacity to do housework, to buy groceries, and to get around without assistance. In addition, overall self-rated health was measured using the single health item from the SF-36 [47]. Results are reported in Table 1.
Table 1.
Characteristics of the total sample and Engage
| Total sample | Engage sample | |||
|---|---|---|---|---|
| N = 2,831 | N = 141 | |||
| Characteristics | N | %/mean | N | %/mean |
| Age | 2,831 | 74.4 | 141 | 74.75 |
| Female | 2,119 | 76.1 | 114 | 82.0 |
| Race: | ||||
| White not Hispanic | 843 | 29.8 | 59 | 41.8 |
| White Hispanic | 257 | 9.1 | 9 | 6.4 |
| Black or African American | 169 | 6.0 | 7 | 5.0 |
| Asian | 1,047 | 37.0 | 35 | 24.8 |
| Other | 515 | 18.2 | 31 | 21.9 |
| Ethnicity | ||||
| Hispanic/Latino | 279 | 9.9 | 11 | 7.8 |
| Not Hispanic/Latino | 1,785 | 63.1 | 91 | 64.5 |
| Refused to Answer or Missing | 767 | 27.1 | 39 | 27.7 |
| Language of assessment | ||||
| English | 1,544 | 54.6 | 98 | 69.5 |
| Spanish | 155 | 5.5 | 6 | 4.3 |
| Russian | 94 | 3.3 | 4 | 2.8 |
| Chinese | 1,032 | 36.5 | 33 | 23.4 |
| Has food stamps | ||||
| Yes | 1,177 | 42.1 | 57 | 40.4 |
| Education | ||||
| 8th grade or less | 810 | 29.0 | 28 | 20.0 |
| Some high school | 382 | 13.7 | 15 | 10.7 |
| Completed high school | 645 | 23.1 | 29 | 20.7 |
| Some college | 626 | 22.4 | 39 | 27.9 |
| Completed college or more | 315 | 11.3 | 29 | 20.7 |
| Assistance needed to get out (e.g., cane, walker) | 1,039 | 37.3 | 69 | 49.6 |
| Self-reported medical conditions | ||||
| Heart disease | 637 | 22.8 | 44 | 31.4 |
| Cancer | 151 | 5.4 | 10 | 7.1 |
| Diabetes | 715 | 25.5 | 39 | 28.1 |
| Hypertension | 1,414 | 50.4 | 79 | 56.0 |
| Other medical illness | 770 | 39.0 | 55 | 53.9 |
| Mean self-rated health | 2,761 | 2.83 | 137 | 2.34 |
| Activities of daily living | ||||
| Need at least some help to walk | 639 | 23.0 | 49 | 35.7 |
| Need at least some help to shop for groceries | 679 | 24.5 | 51 | 37.2 |
| Need at least some help to do housework | 782 | 28.3 | 59 | 43.7 |
Procedure
Individuals who reported mental health need (PHQ-9 ≥ 10) on the needs assessment and were not receiving mental health services at the time of the assessment were offered six free weekly 45-min sessions of Engage therapy in a nearby senior center. Weekly PHQ-9 screening questionnaires were administered by the therapist prior to each session to monitor treatment progress. Data were entered into the NYC Department for the Aging (DFTA) STARS database system [48]. Transfer of deidentified data was approved by the University Name IRB.
Treatment
Engage is a reward-based psychotherapy for late-life depression developed to match the skills of community clinicians and guided by neurobiological principals included in the Research Domain Criteria [49]. It is based on the premise that dysfunction in the positive valence systems is a critical mechanism in late-life depression, as depressed older adults suffer from anhedonia and do not engage in rewarding activities which activate this system [40,50]. Thus, Engage focuses on “reward exposure” as its principal intervention, with the aim of increasing patients’ engagement in rewarding activities, which could potentially reignite the reward system and as a result reduce depression. Engage is effective in reducing depressive symptoms and increasing behavioral activation in depressed older adults [42], with depression reduction rates comparable to Problem-Solving Psychotherapy, a gold-standard evidence-based psychotherapy [51]. In this study, SMART-MH therapists were licensed social workers or mental health counselors who were trained and supervised by a licensed clinical psychologist who codeveloped Engage (P.J.R).
Statistical analysis plan
A linear mixed-effects model investigated symptomatic change over time, as measured using the PHQ-9. Analysis was conducted using lme4 package in R [52]. The model included subject-specific random intercept and fixed effects for time. Due to differences in language of treatment delivery, as well as patients’ native language, we initially conducted our analyses with therapists ID’s as covariate (each therapist provided treatment in a different language), as well as with patients’ primary language (categorical variable English versus non-English) as a covariate. Both covariates were nonsignificant and thus removed from the final model. Additionally, we tested the effects of gender and age. Age was defined as a categorical variable based on our previous depression findings that “young-old” participants had higher depression. For these analyses, we used this definition which was also consistent with a mean split (elder older adults aged 75 years and over and younger older adults aged 74 years or under).
Second, Tukey post-hoc test was used to assess the significance of session-by-session reduction in symptoms (corrected for multiple comparisons). Third, a series of t-tests were conducted to compare standardized slopes of change in sessions 1 through 6 derived from mixed-linear models in the current sample with change trends in a previous pilot study which tested the efficacy of nine-session Engage provided within a controlled experimental setting at academic medical center.
Results
A total of 2,831 older adults were assessed over 18 months (Table 1) with 96.5% (2715/2813) completing a PHQ-9 screen. Only those participants with PHQ-9 screenings were included. Out of 2,715 participants with completed PHQ-9 screening, 12.3% (n = 333) endorsed clinically significant symptoms of depression (PHQ-9 ≥ 10), and of these, 26.6% endorsed suicidal ideation on the PHQ-9. Among those with depressive symptoms, 201 reported unmet needs for mental health services, and 70.1% (n = 141) agreed to receive Engage therapy. Seventy-seven percent of the patients (n = 109) completed the 6-session protocol; 5 clients completed 5 sessions and 27 clients completed 4 sessions or less. The average number of sessions was 5.35, with no differences between English and non-English speaking clients (5.3 and 5.5, respectively).
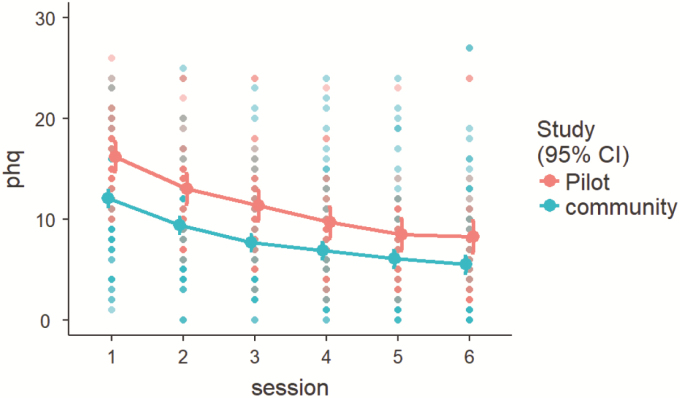
Overall, 68% of clients met the “significantly clinical improvement” criterion (i.e., reduction of five points on PHQ-9 and PHQ9 < 10). Mixed-effects model suggested that depressive symptoms reduced significantly over the course of six sessions (F [6,737] = 174.73; p < .0001; see Table 2 and Fig. 1). We tested the effects of loss due to the storm by including the number of storm stressors and patients’ rating of perceived loss in our mixed-effects model (trauma stressors were not included since only 9 patients reported experiencing one of those stressors). Since none of these effects were significant they were excluded from the final model. We conducted post-hoc Tukey test (corrected for multiple comparisons) to examine session-by-session changes in depression severity. We found significant reductions in depressive symptoms at each point from baseline to week 3 (Table 2). A series of t-tests comparing standardized slopes of change in the current sample compared to Engage therapy implemented in an open clinical trial, derived from linear mixed-effects models, were nonsignificant, indicating equivalent noninferior symptomatic reductions in the current sample and in the Engage open clinical trial (see Table 3 and Fig. 2).
Table 2.
Reduction in PHQ-9 over the course of Engage treatment
| Time | Mean (SD) | df | t value | p value |
|---|---|---|---|---|
| Baseline | 13.78 (342) | |||
| Session 1 | 11.92 (4.38) | 740 | 5.55 | <.0001 |
| Session 2 | 9.41 (4.30) | 742 | 8.26 | <.0001 |
| Session 3 | 7.87 (4.24) | 743 | 5.18 | <.0001 |
| Session 4 | 7.18 (4.23) | 740 | 2.33 | .22 |
| Session 5 | 6.39 (4.64) | 740 | 2.43 | .18 |
| Session 6 | 5.79 (5.08) | 740 | 1.67 | .63 |
t value indicates reduction in depressive symptoms from previous time point, derived from post-hoc comparisons of mixed-effects model; df = degrees of freedom.
Fig 1.
Mixed-effects model for reduction in PHQ-9 scores over the course of 6-session Engage therapy. Bars represent 95% confidence intervals.
Table 3.
Comparison of standardized slopes of change over time in PHQ-9 between Engage treatment provided in a controlled setting and Engage provided in the community
| Time | Engage pilot | Engage community | df | t | p |
|---|---|---|---|---|---|
| (Intercept) | 16.13 | 12.09 | |||
| Session 2 | −3.07 | −2.68 | 165 | 0.55 | .58 |
| Session 3 | −1.65 | −1.71 | 153 | 0.08 | .93 |
| Session 4 | −1.63 | −0.78 | 144 | 1.18 | .24 |
| Session 5 | −1.13 | −0.83 | 139 | 0.38 | .70 |
| Session 6 | −0.16 | −0.58 | 132 | 0.53 | .59 |
Standardized slopes (β’s) of change over time were retrieved from linear mixed-effects- models followed by post-hoc Tukey test for session-by-session change (corrected for multiple comparisons). Engage Community = sample presented in the current study. Engage pilot = Nine-session Engage treatment provided in a controlled setting. We present slope changes from session 1 through 6 for both samples for the purpose of comparison.
Fig 2.
Trajectories of change in PHQ-9 over time in the Pilot Engage sample and the Engage Community sample reported in this manuscript. Bars represent 95% confidence intervals.
Discussion
The principal finding of this study is that using a delivery model that includes outreach, assessment and brief, streamlined psychotherapy resulted in high levels of engagement among older adults with mental health need and clinically meaningful reductions in depressive symptoms. The delivery of brief, six-session version of Engage, a reward exposure-based therapy for late-life depression, was feasible and had clinical impact when delivered by master’s level clinicians to a diverse, multilingual group of older adults impacted by a natural disaster with depression. Despite the heterogeneity of the clinical population, diverse delivery settings, and potential barriers, as well as relatively short length of treatment, Engage led to session-by-session reductions in depression, which were equivalent to those found in a controlled experimental setting.
The high rate of clients’ engagement in Engage reflects the impact of strategies to improve access to mental health services. Our previous work demonstrated that when depressed older adults received a referral (phone number to call), without additional interventions, only 22% followed up to request services [21]. However, we have been able to improve treatment engagements using the Open Door approach that includes goal setting, barrier assessments, problem solving, and follow-up [21]. In an implementation of Open Door, 31 congregant meal sites in New York City were randomized to learn to implement depression screening (using the PHQ-9) and offer mental health referrals using the Open Door approach, or screening with the “usual” referral strategies. Sites using the Open Door strategy had a higher connection rate with either a primary care of mental health provider (73.6% vs. 32.4%) [53].
Our findings are consistent with other studies in primary care settings that examine the clinical impact of brief interventions on depression level. A telephone-supported depression self-care intervention lowered PHQ-9 depression scores from 12.2 to 7.9 among primary care patients with chronic physical conditions and depression [54]. A multisite treatment trial for late-life depression in older adults recruited from primary care clinics [55,56] resulted in a decrease in depression scores from 13.6 to 6.1 [57]. In a previous study, we found that Engage training was faster and led to lower therapist skills drift, compared to Problem-Solving Therapy [58]. Taken together, Engage may be a therapy that can improve the move to integrate nonpharmacologic mental health services into nonmental health settings.
Our findings should be considered in the context of the limitations imposed by service demonstration projects. Our study did not include a control condition and we cannot compare our outcomes to those individuals who did not receive Engage. In addition, unlike clinical trial designs, no independent assessments were conducted by trained raters to compare pre and post therapy symptom changes. Instead, depression severity was measured in a way more consistent with practice. Although we recognize that there may be a therapist bias in such assessments that inflate the therapy’s impact, there is an opportunity to track symptoms over time and evaluate the usefulness of therapy in real time.
In conclusion, the SMART-MH project demonstrated the feasibility and clinical impact of delivery of a brief psychotherapy for late-life depression offered in multiple languages in community settings. Additionally, our results suggest that a therapeutic response was not determined by patients’ age, gender, or storm-related experiences. Given these promising results, SMART-MH program has served as a prototype model for the new Geriatric Mental Health Initiative in New York City (https://www1.nyc.gov/site/dfta/services/thrivenyc-at-dfta.page). The model is being sustained by government support from the New York City Department for the Aging and University name is implementing mental health services in New York City in 16 congregant meal sites serving diverse older adults in New York City. While the SMART-MH program therapy was offered without charge, the sustained Geriatric Mental Health Initiative model will enhance sustainability by billing for services. Innovative strategies to improve care delivery can serve those individuals who are hard to reach with language and other barriers.
Acknowledgements:
We have to thank all the staff who worked on the SMART-MH project, the community partners who provided support, space, and trusted our staff, and the older adults who gave their time and experience post-storm. Data collection was funded by New York State SSBG grant awarded to the Aging in New York Fund, 501(c)(3) and the New York City Department for the Aging. Data analyses, interpretation and manuscript preparation were supported by the Weill Cornell ALACRITY (P50 MH113838, GSA), R01 MH102252 (GSA), and T32 MH019132 (GSA)s
Compliance with Ethical Standards
Conflicts of Interest: G.S.A. serves at the speakers’ bureaus of Takeda, Lundbeck, Otsuka, and Sunovion. No other authors report conflicts of interest.
Human Rights: Data analyses of deidentified data were conducted with the approval of the Weill Cornell Medical College IRB# 1504016137.
Informed consent: Consent for assessment and tracking was obtained by the New York City Department for the Aging. Deidentified data were provided to Weill Cornell.
Welfare of Animals: This article does not contain any studies with animals performed by any of the authors.
References
- 1. WHO. World Report on Ageing and Health. Geneva, Switzerland: World Health Organization; 2015. https://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf;jsessionid=51089ADDB69F9BA543FE4436CFEF976A?sequence=1. [Google Scholar]
- 2. Federal Interagency Forum on Aging-Related Statistics. Older Americans 2016: Key Indicators of Well-Being. Washington, DC; 2016. https://agingstats.gov/docs/LatestReport/Older-Americans-2016-Key-Indicators-of-WellBeing.pdf. [Google Scholar]
- 3. World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates. Geneva, Switzerland; 2017. https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf?sequence=1. [Google Scholar]
- 4. Shah MN, Jones CM, Richardson TM, Conwell Y, Katz P, Schneider SM. Prevalence of depression and cognitive impairment in older adult emergency medical services patients. Prehosp Emerg Care. 2011;15(1):4–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Walker S, Walker J, Richardson G, et al. Cost-effectiveness of combining systematic identification and treatment of co-morbid major depression for people with chronic diseases: the example of cancer. Psychol Med. 2013;44(7):1–10. [DOI] [PubMed] [Google Scholar]
- 6. Richardson TM, He H, Podgorski C, Tu X, Conwell Y. Screening depression aging services clients. Am J Geriatr Psychiatry. 2010;18(12):1116–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Barry LC, Abou JJ, Simen AA, Gill TM. Under-treatment of depression in older persons. J Affect Disord. 2012;136(3):789–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Byers AL, Arean PA, Yaffe K. Low use of mental health services among older Americans with mood and anxiety disorders. Psychiatr Serv. 2012;63(1):66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Olfson M, Blanco C, Marcus SC. Treatment of adult depression in the United States. JAMA Intern Med. 2016;176(10):1482–1491. [DOI] [PubMed] [Google Scholar]
- 10. Areán PA, Hegel MT, Reynolds CF. Treating depression in older medical patients with psychotherapy. J Clin Geropsychol. 2001;7(2):93–104. [Google Scholar]
- 11. Conwell Y, Duberstein PR, Hirsch JK, Conner KR, Eberly S, Caine ED. Health status and suicide in the second half of life. Int J Geriatr Psychiatry. 2010;25(4):371–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gallo JJ, Bogner HR, Morales KH, Post EP, Ten Have T, Bruce ML. Depression, cardiovascular disease, diabetes, and two-year mortality among older, primary-care patients. Am J Geriatr Psychiatry. 2005;13(9):748–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Byers AL, Sheeran T, Mlodzianowski AE, Meyers BS, Nassisi P, Bruce ML. Depression and risk for adverse falls in older home health care patients. Res Gerontol Nurs. 2008;1(4):245–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Eggermont LH, Penninx BW, Jones RN, Leveille SG. Depressive symptoms, chronic pain, and falls in older community-dwelling adults: the MOBILIZE Boston Study. J Am Geriatr Soc. 2012;60(2):230–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jia H, Lubetkin EI. Incremental decreases in quality-adjusted life years (QALY) associated with higher levels of depressive symptoms for U.S. Adults aged 65 years and older. Health Qual Life Outcomes. 2017;15(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Alexopoulos GS, Sirey JA, Banerjee S, et al. Two behavioral interventions for patients with major depression and severe COPD. Am J Geriatr Psychiatry. 2016;24(11):964–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Marino P, Sirey JA, Raue PJ, Alexopoulos GS. Impact of social support and self-efficacy on functioning in depressed older adults with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2008;3(4):713–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gallo JJ, Bogner HR, Morales KH, Post EP, Lin JY, Bruce ML. The effect of a primary care practice-based depression intervention on mortality in older adults: a randomized trial. Ann Intern Med. 2007;146(10):689–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Weisz J, Chu B, Polo A. Treatment dissemination and evidence-based practice: strengthening intervention through clinician-researcher collaboration. Clin Psychol Sci Pr. 2004;11(3):300–307. [Google Scholar]
- 20. Sirey JA, Greenfield A, DePasquale A, et al. Improving engagement in mental health treatment for home meal recipients with depression. Clin Interv Aging. 2013;8:1305–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sirey JA, Banerjee S, Marino P, et al. Improving mental health treatment initiation among depressed community dwelling older adults. Am J Geriatr Psychiatry. 2016;24(4):310–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ngo VK, Centanni A, Wong E, Wennerstrom A, Miranda J. Building capacity for cognitive behavioral therapy delivery for depression in disaster-impacted contexts. Ethn Dis. 2011;21(3suppl 1):S1–38. [PMC free article] [PubMed] [Google Scholar]
- 23. Arean P. Implementing evidence-based psychotherapies in settings serving older adults: challenges and solutions. Psychiatr Serv. 2012;63(6):605–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Norris FH, Perilla JL, Riad JK, Kaniasty K, Lavizzo EA. Stability and change in stress, resources, and psychological distress following natural disaster: findings from hurricane Andrew. Anxiety Stress Coping. 1999;12(4):363–396. [DOI] [PubMed] [Google Scholar]
- 25. Schwartz RM, Sison C, Kerath SM, et al. The impact of Hurricane Sandy on the mental health of New York area residents. Am J Disaster Med. 2015;10(4):339–346. [DOI] [PubMed] [Google Scholar]
- 26. Schwartz RM, Rothenberg P, Kerath SM, Liu B, Taioli E. The lasting mental health effects of hurricane sandy on residents of the rockaways. J Emerg Manag. 2016;14(4):269–279. [DOI] [PubMed] [Google Scholar]
- 27. Schwartz RM, Schwartz RM, Gillezeau CN, Liu B, Lieberman-Cribbin W, Taioli E. Longitudinal impact of hurricane sandy exposure on mental health symptoms. Int J Environ Res Public Health. 2017;14(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sirey JA, Berman J, Halkett A, et al. Storm impact and depression among older adults living in hurricane sandy–affected areas. Disaster Medicine and Public Health Preparedness. 2016;11(1):1–13. [DOI] [PubMed] [Google Scholar]
- 29. Norris FH, Friedman MJ, Watson PJ. 60,000 disaster victims speak: part II. Summary and implications of the disaster mental health research. Psychiatry. 2002;65(3):240–260. [DOI] [PubMed] [Google Scholar]
- 30. Kessler RC, Galea S, Gruber MJ, Sampson NA, Ursano RJ, Wessely S. Trends in mental illness and suicidality after Hurricane Katrina. Mol Psychiatry. 2008;13(4):374–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gilbody SM. IMPACT collaborative care programme reduces suicide ideation in depressed older adults. Evid Based Ment Health. 2007;10(2):51. [DOI] [PubMed] [Google Scholar]
- 32. Bruce ML, Pearson JL. Designing an intervention to prevent suicide: PROSPECT (Prevention of Suicide in Primary Care Elderly: collaborative Trial). Dialogues Clin Neurosci. 1999;1(2):100–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ciechanowski P, Wagner E, Schmaling K, et al. Community-integrated home-based depression treatment in older adults: a randomized controlled trial. JAMA. 2004;291(13):1569–1577. [DOI] [PubMed] [Google Scholar]
- 34. Andrade LH, Alonso J, Mneimneh Z, et al. Barriers to mental health treatment: results from the WHO World Mental Health surveys. Psychol Med. 2014;44(6):1303–1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sirey JA, Bruce ML, Alexopoulos GS, et al. Perceived stigma as a predictor of treatment discontinuation in young and older outpatients with depression. Am J Psychiatry. 2001;158(3):479–481. [DOI] [PubMed] [Google Scholar]
- 36. Sirey JA, Bruce ML, Alexopoulos GS, Perlick DA, Friedman SJ, Meyers BS. Stigma as a barrier to recovery: perceived stigma and patient-rated severity of illness as predictors of antidepressant drug adherence. Psychiatr Serv. 2001;52(12):1615–1620. [DOI] [PubMed] [Google Scholar]
- 37. Sirey JA, Franklin AJ, McKenzie SE, Ghosh S, Raue PJ. Race, stigma, and mental health referrals among clients of aging services who screened positive for depression. Psychiatr Serv. 2014;65(4):537–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Conner KO, Copeland VC, Grote NK, et al. Mental health treatment seeking among older adults with depression: the impact of stigma and race. Am J Geriatr Psychiatry. 2010;18(6):531–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sirey JA, Franklin AJ, McKenzie SE, Ghosh S, Raue PJ. Race, stigma and mental health recommendations among depressed older persons in aging services. Psychiatr Serv. 2014;65(4):537–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Alexopoulos GS, Arean P. A model for streamlining psychotherapy in the RDoC era: the example of ‘Engage’. Mol Psychiatry. 2014;19(1):14–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Alexopoulos GS, O'Neil R, Banerjee S, et al. “Engage” therapy: prediction of change of late-life major depression. J Affect Disord. 2017;221:192–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Alexopoulos GS, Raue PJ, Gunning F, et al. “Engage” therapy: behavioral activation and improvement of late-life major depression. Am J Geriatr Psychiatry. 2016;24(4):320–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. McMillan D, Gilbody S, Richards D. Defining successful treatment outcome in depression using the PHQ-9: a comparison of methods. J Affect Disord. 2010;127(1–3):122–129. [DOI] [PubMed] [Google Scholar]
- 45. Raue PJ, Brown EL, Meyers BS, Schulberg HC, Bruce ML. Does every allusion to possible suicide require the same response? J Fam Pract. 2006;55(7):605–612. [PubMed] [Google Scholar]
- 46. Lawton MP, Moss M, Fulcomer M, Kleban MH. A research and service oriented multilevel assessment instrument. J Gerontol. 1982;37(1):91–99. [DOI] [PubMed] [Google Scholar]
- 47. Ware JS, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). Medical Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 48. Corrado DM. Mayor’s Management Report. Department for the Aging; 2014:177–182. https://www1.nyc.gov/assets/operations/downloads/pdf/pmmr2014/2014_pmmr.pdf. [Google Scholar]
- 49. Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Med. 2013;11:126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Alexopoulos GS, Buckwalter K, Olin J, Martinez R, Wainscott C, Krishnan KR. Comorbidity of late life depression: an opportunity for research on mechanisms and treatment. Biol Psychiatry. 2002;52(6):543–558. [DOI] [PubMed] [Google Scholar]
- 51. Alexopoulos GS, Raue PJ, Kiosses DN, Seirup JK, Banerjee S, Arean PA. Comparing engage with PST in late-life major depression: a preliminary report. Am J Geriatr Psychiatry. 2015;23(5):506–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Bates D, et al. Fitting Linear Mixed-Effects Models Using lme4. Vol. arXiv:1406. 2014. [Google Scholar]
- 53. Berman J, Furst L.. Addressing the needs of depressed older New Yorkers: A public-private partnership: EASE-D and other interventions. Internal Report: NYC Department for the Aging; 2014. [Google Scholar]
- 54. McCusker J, Lambert SD, Cole MG, et al. Activation and self-efficacy in a randomized trial of a depression self-care intervention. Health Educ Behav. 2016;43(6):716–725. [DOI] [PubMed] [Google Scholar]
- 55. Unützer J, Katon W, Callahan CM, et al. Collaborative Care Management of Late-Life Depression in the Primary Care Setting: A Randomized Controlled Trial. JAMA. 2002;288(22):2836–2845. [DOI] [PubMed] [Google Scholar]
- 56. Unützer J, Katon W, Williams JW Jr, et al. Improving primary care for depression in late life: the design of a multicenter randomized trial. Med Care. 2001;39(8):785–799. [DOI] [PubMed] [Google Scholar]
- 57. Löwe B, Unützer J, Callahan CM, Perkins AJ, Kroenke K. Monitoring depression treatment outcomes with the patient health questionnaire-9. Med Care. 2004;42(12):1194–1201. [DOI] [PubMed] [Google Scholar]
- 58. Raue P. Therapist Fidelity to Engage vs. PST for late-life depression: time to competency and skill drift. In Mental Health Services Research Conference. 2018. Rockville, MD. [Google Scholar]