Condensed Abstract
Million Hearts and partners have been committed to raising national cardiac rehabilitation participation rates to a goal of 70%. Quality improvement tools, resources, and surveillance models have been developed in support. Efforts to enhance research programs and collaborative initiatives have created momentum to accelerate implementation of new care models.
Keywords: cardiac rehabilitation, enrollment barriers, quality improvement, alternative programs models
Million Hearts is a national initiative co-led by the Centers for Disease Control and Prevention (CDC) and the Centers for Medicare & Medicaid Services (CMS) with the goal of preventing one million heart attacks, strokes, and other acute cardiovascular events in a 5-yr period. The initiative is currently in its second 5-yr term, Million Hearts 2022 (2017–2021); the initial iteration spanned from 2012 through 2016.1 Although cardiac rehabilitation (CR) was not an initial focus of Million Hearts, it was identified as an important component of a comprehensive, evidence-based approach to secondary prevention. As such, the Million Hearts Cardiac Rehabilitation Leadership Summit was convened in November of 2015, bringing together healthcare leaders, healthcare insurers and insurance purchasers, and experts in CR with staff from CDC, CMS, and the National Institutes of Health (NIH), to discuss strategies to increase CR referral and participation.
Summit participants committed to a sustained, collective effort and a bold target of raising CR participation among eligible patients from its chronically low rate of ~20%2 to 70% by 2022. A critical output of the Summit was the ‘Million Hearts Cardiac Rehabilitation Road Map’.3 This publication catalyzed nationwide initiatives to improve CR utilization including a learning collaborative, quality improvement tools, a surveillance methodology and resultant analyses, funding to fill gaps in knowledge about CR delivery in diverse populations, and plans for a think tank to address new CR delivery models (Table 1).
Table 1 –
Timeline of Select Million Hearts-related Cardiac Rehabilitation Activities
| Date | Activity |
|---|---|
| November 2015 | Million Hearts Cardiac Rehabilitation Leadership Summit |
| February 2016 | Million Hearts Cardiac Rehabilitation Leadership Summit transitioned to quarterly Million Hearts Cardiac Rehabilitation Collaborative meetings |
| November 2016 | Publication of Ades P, et al., “Increasing Cardiac Rehabilitation Participation From 20% to 70%: A Road Map From the Million Hearts Cardiac Rehabilitation Collaborative” |
| January 2017 | Inclusion of a 70% cardiac rehabilitation participation target in Million Hearts 2022 |
| July 2018 | Million Hearts/AACVPR Cardiac Rehabilitation Change Package launched |
| July – September 2018 | Four NIH cardiac rehabilitation-related research grants awarded |
| September 2018 | CDC “Innovative State and Local Public Health Strategies to Prevent and Manage Diabetes and Heart Disease and Stroke” (CDC-RFA-DP18–1817) funding awarded |
| March 2019 | AHRQ task order funding awarded to increase cardiac rehabilitation use, which ultimately became TAKEheart |
| February 2019 | Million Hearts Outpatient Cardiac Rehabilitation Use Surveillance Methodology finalized |
| February 2019 – February 2020 | Million Hearts hosted three cardiac rehabilitation Twitter chats |
| January 2020 | Publication of Ritchey MD, et al., “Tracking Cardiac Rehabilitation Participation and Completion Among Medicare Beneficiaries to Inform the Efforts of a National Initiative” |
| May 2020 | CMS identifies cardiac rehabilitation as a high value service with zero cost-sharing for qualified health plans to include in value-based insurance plans |
| July 2020 | CR enrollment measure included in the HEDIS Measurement Year 2020 and Measurement Year 2021 Volume 2 |
| Q4 2020/Q1 2021 | Million Hearts Cardiac Rehabilitation Think Tank (planned) |
Abbreviations: AACVPR, American Association of Cardiovascular and Pulmonary Rehabilitation; AHRQ, Agency for Healthcare Research and Quality; CDC, Centers for Disease Control and Prevention; HEDIS, Healthcare Effectiveness Data and Information Set; NCQA, National Committee for Quality Assurance; NIH, National Institutes of Health.
As a direct result of the Million Hearts Cardiac Rehabilitation Leadership Summit and resultant Road Map, the target of achieving a 70% participation rate in CR for eligible patients was adopted as a focus for Million Hearts 2022. A clinical quality measure related to CR referral was subsequently added to the small set of measures supported by the initiative.4 The Summit transitioned into the Million Hearts Cardiac Rehabilitation Collaborative (CRC). The CRC is an open forum that convenes on a quarterly basis to advance progress towards the 70% CR participation target. Members of the CRC contribute to yearly action plans with defined goals and report on their successful implementation of priority activities. Membership of the CRC is diverse and has steadily grown over time (Supplemental Figure 1); it currently includes nearly 400 CR professionals, researchers, patient advocates, staff from state and local departments of health, federal agency representatives, payers, technology vendors, and others from almost 200 organizations.
To fill research gaps identified at the initial Summit, NIH provided funding for four research projects related to enhancing participation in CR, with funding exceeding $5.5 million from 2018–2020. Three projects relate to the use of new care models, including home-based and/or center- and home-based CR, otherwise known as hybrid CR5,6,7, and one explores approaches to improve participation rates among patients of lower socioeconomic status.8 Results from these trials are forthcoming.
To facilitate improvement in CR participation, Million Hearts collaborated with experts from the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR) to develop the Million Hearts/AACVPR Cardiac Rehabilitation Change Package (CRCP). Launched in 2018, this quality improvement tool offers a menu of evidence- and practice-based changes that hospitals and CR professionals can make to improve rates of referral, enrollment and participation, and adherence to CR. For each CR change strategy, the change package provides tested tools and resources that were gathered from numerous national organizations and twenty exemplar CR programs. The CRCP has been widely distributed to CR professionals through AACVPR annual meetings, state affiliate meetings, and a variety of webinars conducted for federal, state, and private sector stakeholders.
The Agency for Healthcare Research and Quality (AHRQ) is charged with disseminating and implementing patient-centered outcomes research findings and has an ongoing nomination process to find candidate projects. Earlier in 2018 AHRQ selected two Million Hearts-recommended strategies – automatic, opt-out electronic health record referrals for all CR-eligible patients and use of care coordinators or “liaisons” to educate patients about the benefits of CR and facilitate a referral process – for implementation in a new initiative. This 3-yr (2019–2022), $6 million initiative, entitled “TAKEheart,” aims to increase use of CR by eligible patients nationwide. It provides technical assistance, coaching, and support to 100 hospitals across the U.S. to implement automatic referrals with care coordination using tools and resources from the CRCP. Additionally, TAKEheart supports a broader Learning Community of up to 200 hospitals to explore additional strategies of interest, from the CRCP and top-performing CR programs, for increasing rates of CR referral, enrollment, and retention.9
In 2018, CDC released a notice of funding opportunity entitled “Innovative State and Local Public Health Strategies to Prevent and Manage Diabetes and Heart Disease and Stroke” (CDC-RFA-DP18–1817). This opportunity included the option to explore and test innovative ways to enhance referral, participation, and adherence related to CR in traditional center-based, as well as community- and home-based settings. Twelve out of twenty-five recipient health departments are addressing CR.
Although CR is underutilized, few analyses have been formally conducted. One of the most cited, by Suaya et al., assessed CR utilization in Medicare fee-for-service beneficiaries aged ≥65 yr with an index hospitalization in 1997. The authors reported that CR was used (≥1 session) by only 18.7% of eligible patients.2 Only a few additional estimates have been published regarding CR utilization.10,11 Recognizing the importance of providing updated participation estimates, as well as guidance on analyzing administrative and claims data, a team from CDC and CMS collaborated with national experts to develop a surveillance methodology for CR participation (attended ≥1 session), timely initiation (within 21 d), and completion (attended 36 sessions). Using that methodology, Medicare fee-for-service data were analyzed for beneficiaries aged ≥65 yr who had qualifying events in two complementary studies.12,13 The investigators found that overall participation (not directly comparable to Suaya) was 20.2% in 2013 and 24.4% in 2016, emphasizing a persistent gap in care.12,13 However, from 1997 to 2016, more substantial increases in participation were seen among patients grouped by their CR-qualifying diagnosis and/or procedure, i.e. among beneficiaries who had an acute myocardial infarction with coronary artery bypass graft (29.8% to 45.9%), coronary artery bypass graft alone (31.0% to 55.3%), and an acute myocardial infarction with percutaneous coronary intervention (20.9% to 32.5%).2,13
In 2018, new recommendations for CR performance measures were published by the American College of Cardiology/American Heart Association Task Force on Performance Measures.14 Shortly thereafter, Million Hearts was invited, along with members of the Task Force, to collaborate with the National Committee on Quality Assurance to develop CR enrollment measures for potential inclusion in the 2020 and 2021 Healthcare Effectiveness Data and Information Set (HEDIS). The Million Hearts CR surveillance methodology, data analyses, and translation materials have been integral contributions to measure development and review. After undergoing public comment in early 2020, a CR enrollment measure was included in 2020 and 2021 HEDIS, Volume 2. The opportunity for health insurance issuers to cover CR with zero cost sharing, as per the value-based insurance plan blueprint provided by CMS in the Final Payment Notice for 2021, may help to improve performance on this new measure.15
To continually raise awareness of the importance of CR and increase stakeholder engagement, Million Hearts created a CR webpage and CR Communications Toolkit. Key messages from these communications were amplified via three Million Hearts Twitter chats (#CardiacRehabChat) from February 2019 to February 2020 that generated a total of 13.7 million social media impressions. Over the years, Million Hearts partnered with AACVPR, health care systems, cardiologists, patient advocates, and federal agencies to further messaging via journal articles, blogs, implementation stories, and patient testimonials.
Future Efforts
Center-based CR, encompassing team-based care focused on integral standard core components, remains the current standard for comprehensive secondary prevention for eligible patients.16 However, there are a limited number of center-based CR programs in the United States. An analysis suggested that if all center-based CR programs were filled to capacity plus an additional 10%, only 45% of eligible patients in the nation could be accommodated.17 Moreover, given the presence of CR deserts in some parts of the United States (Figure 1), coupled with limited hours of operation, the time and cost of transportation and/or parking and the logistics of in-person attendance, new care delivery models that preserve the core components and appropriately reimburse for the sustained delivery of those services are warranted.
Figure 1.
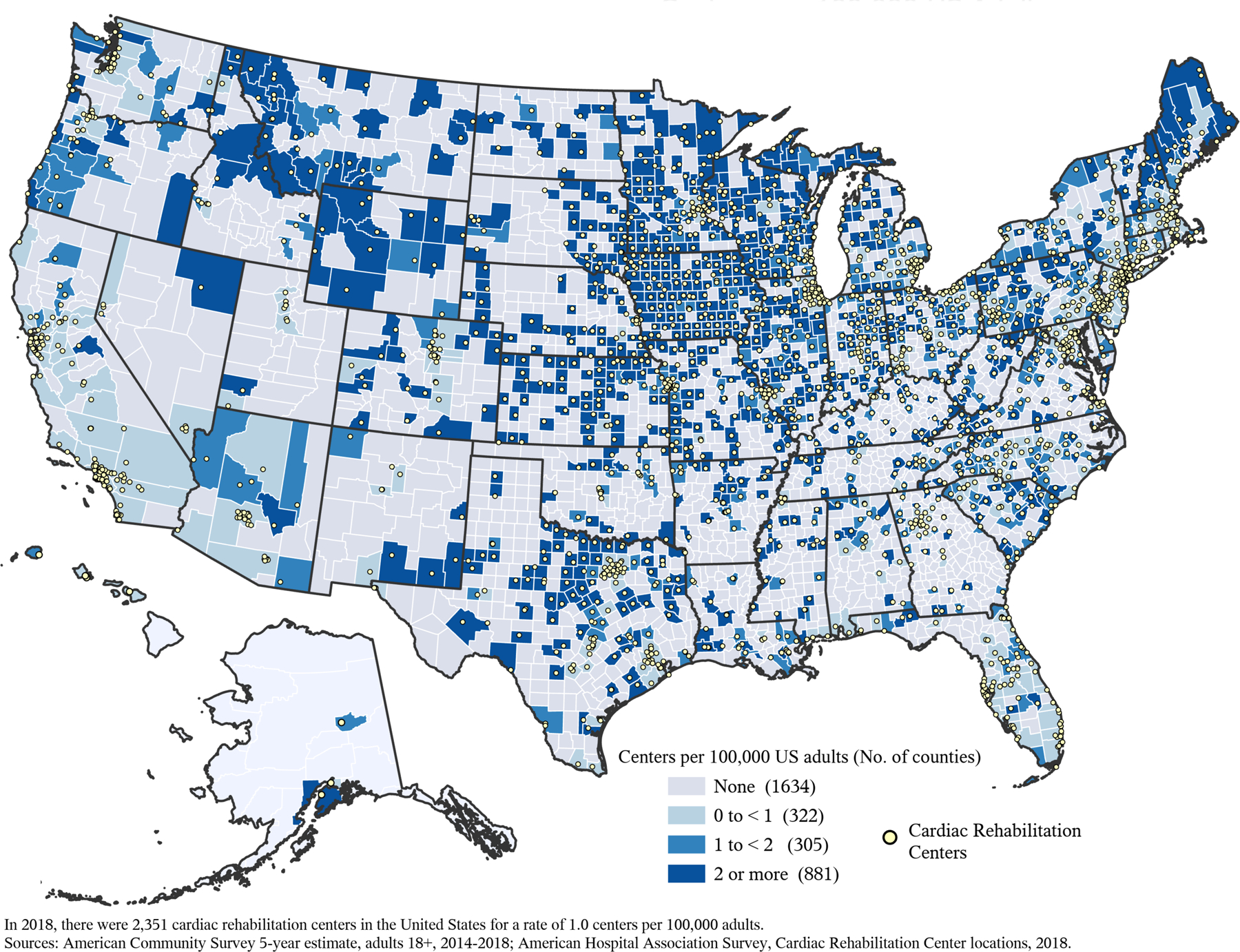
Number of Cardiac Rehabilitation Centers per 100,000 US Adults Aged 18 or older, by County, 2018
The significant challenges encountered in the delivery of traditional center-based CR during local or national emergencies, like the current pandemic, highlight the importance of closing the gaps in CR care and rapid implementation of new care models. In support of this need, Million Hearts has planned a ‘think tank’ to gather CR experts, implementation specialists, public health professionals, payers, and others. This think tank will be charged with reviewing current challenges and potential opportunities, exploring terminology (i.e. is the current vernacular of “home-based” or “hybrid” CR optimal), understanding needed facilitators for accelerating standards-based hybrid, home-based, or community-based programs, and drafting an 18-mo strategic plan with concrete actions needed to address this issue.
The field of CR is composed of professionals, researchers and patient advocates concerned about the delivery of quality care to eligible patients at risk for a secondary cardiovascular event. For decades, organizations like AACVPR have provided leadership in CR through accreditation, registry hosting, and professional development. Million Hearts is committed to focusing on the underutilization of CR, identifying system-, clinician-, and patient-level barriers to care, and highlighting the impact that social determinants of health have on utilization by disparate populations. Public health-clinical partnerships such as Million Hearts can integrate epidemiologic approaches and data analysis with research translation, convene diverse partners to identify and solve problems, and leverage public policy and public resources to catalyze utilization of CR and accelerate implementation of new care models to help achieve the national CR participation goal of 70%.
Supplementary Material
Figure 1A.
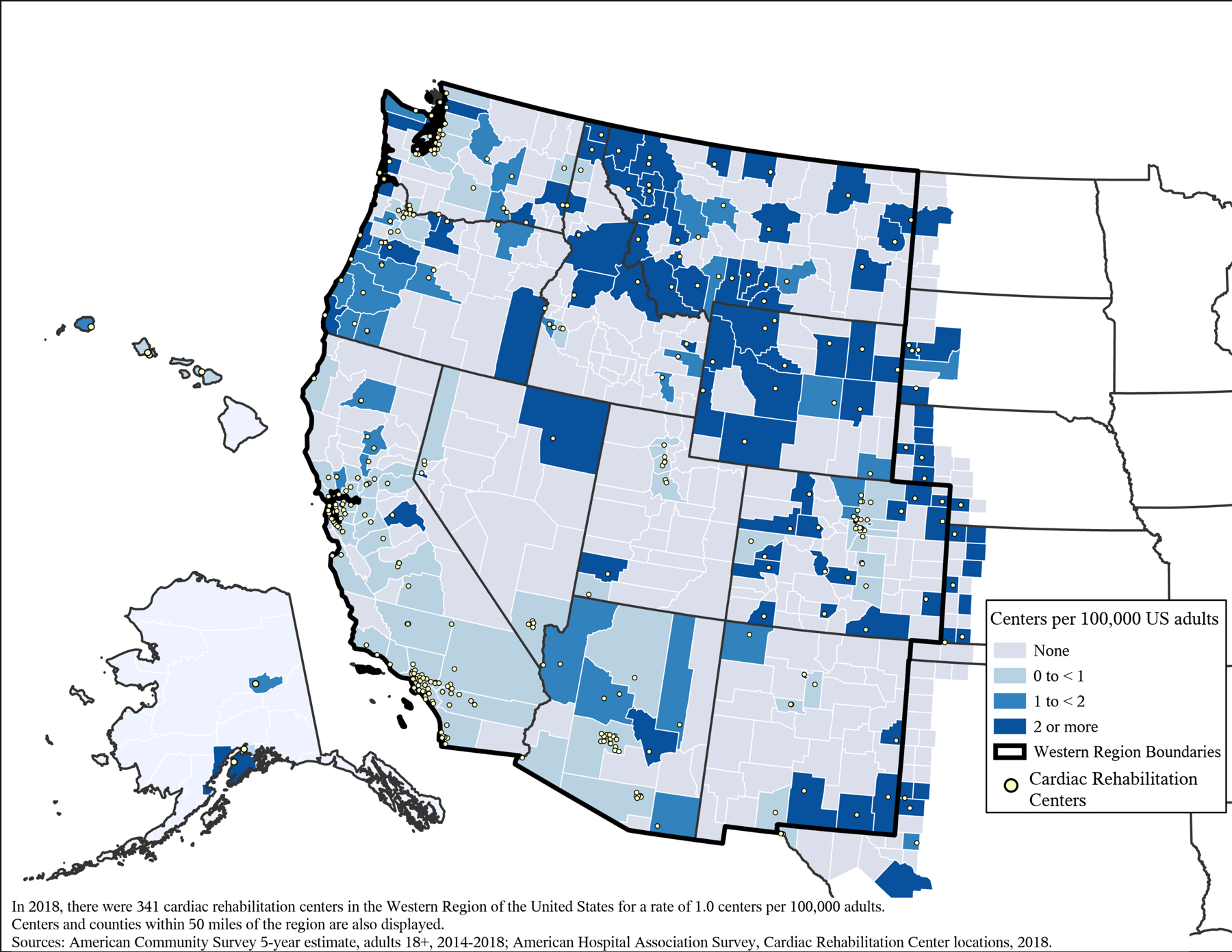
Number of Cardiac Rehabilitation Centers per 100,000 US Adults Aged 18 or older, by County, Western Region, 2018
Figure 1B.

Number of Cardiac Rehabilitation Centers per 100,000 US Adults Aged 18 or older, by County, Midwest Region, 2018
Figure 1C.

Number of Cardiac Rehabilitation Centers per 100,000 US Adults Aged 18 or older, by County, Northeast Region, 2018
Figure 1D.
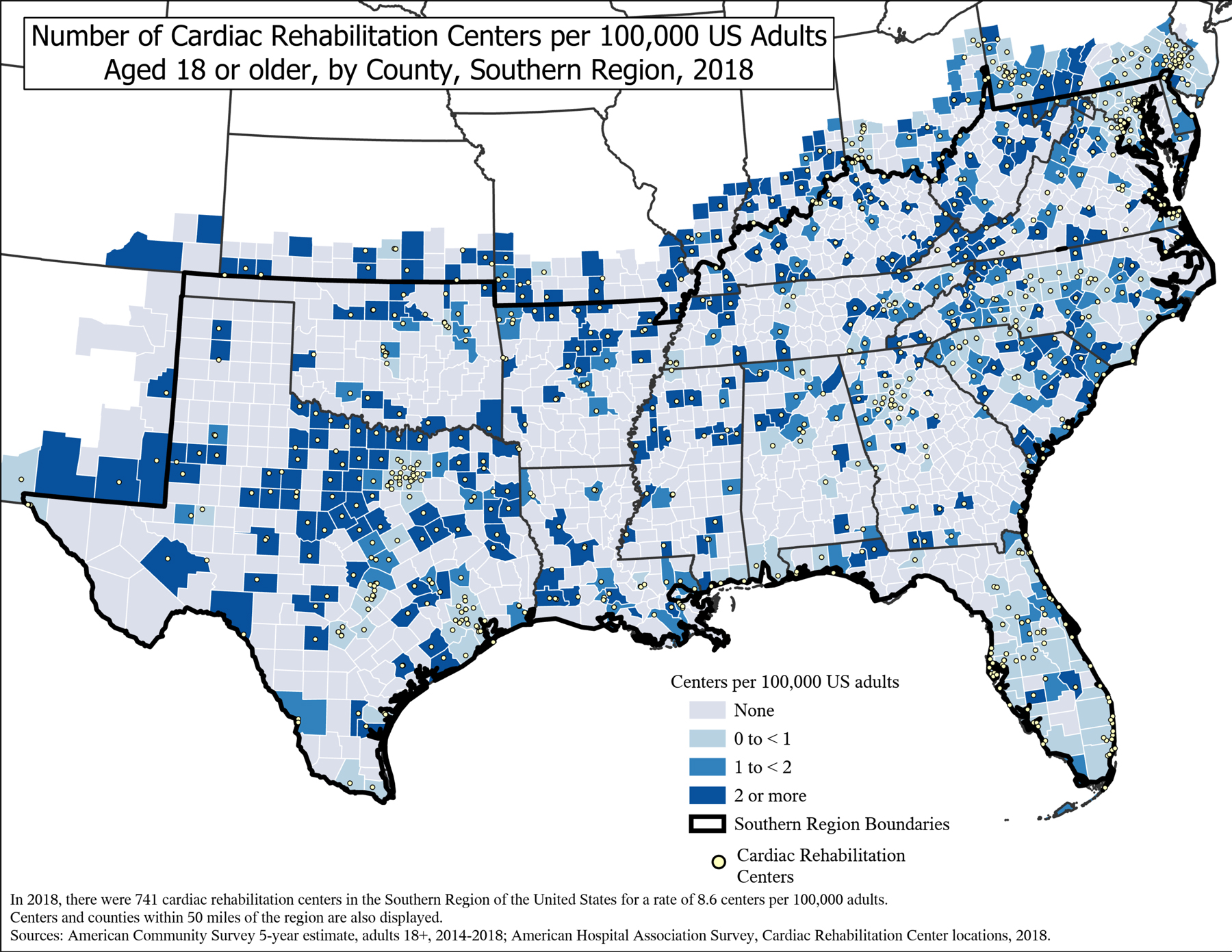
Number of Cardiac Rehabilitation Centers per 100,000 US Adults Aged 18 or older, by County, Southern Region, 2018
Acknowledgments
The authors would like to acknowledge Amir Mirsajedin and Linda Schieb from the Division for Heart Disease and Stroke Prevention, Centers for Disease Control and Prevention for providing the map depicting cardiac rehabilitation deserts.
Sources of Funding: Philip A. Ades, MD is currently receiving Federal salary support from two National Institutes of Health grants (NIGMS P20GM103644 and NHLBI R33HL143305). All other authors declare no sources of support.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily reflect the official position of the Centers for Disease Control and Prevention.
Footnotes
Conflicts of interest: None.
References
- 1.Wall HK, Ritchey MD, Gillespie C, Omura JD, Jamal A, and George MG. Vital Signs: Prevalence of Key Cardiovascular Disease Risk Factors for Million Hearts 2022 - United States, 2011–2016. MMWR Morb Mortal Wkly Rep. 2018;67(35):983–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, and Stason WB. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116(15):1653–1662. [DOI] [PubMed] [Google Scholar]
- 3.Ades PA, Keteyian SJ, Wright JS, et al. Increasing Cardiac Rehabilitation Participation From 20% to 70%: A Road Map From the Million Hearts Cardiac Rehabilitation Collaborative. Mayo Clin Proc. 2017;92(2):234–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Million Hearts. Clinical Quality Measure Alignment. Accessed https://millionhearts.hhs.gov/data-reports/measures.html on March 20, 2020.
- 5.National Institutes of Health Project Information, 1R01AG060499–01. Modified Application of Cardiac Rehabilitation (CR) For Older Adults (MACRO). Accessed on March 23, 2020 at https://projectreporter.nih.gov/project_info_description.cfm?aid=9597601&icde=41558292&ddparam=&ddvalue=&ddsub=&cr=2&csb=default&cs=ASC&pball=.
- 6.National Institutes of Health Project Information, 1R61HL143099–01. The Improving Attendance to Cardiac Rehabilitation (Iattend) Trial. Accessed on March 23, 2020 at https://projectreporter.nih.gov/project_info_details.cfm?aid=9588024.
- 7.National Institutes of Health Project Information, 1R61HL143324–01. Enhancing Cardiac and Pulmonary Rehabilitation Adherence Through Home-Based Rehabilitation And Behavioral Nudges: Era Nudge. Accessed March 23, 2020 at https://projectreporter.nih.gov/project_info_details.cfm?aid=9589299&icde=0.
- 8.National Institutes of Health Project Information, 1R61HL143305–01. Improving Participation in Cardiac Rehabilitation Among Lower-Socioeconomic Status Patients: Efficacy Of Early Case Management And Financial Incentives. Accessed March 23, 2020 at https://projectreporter.nih.gov/project_info_details.cfm?aid=9588856.
- 9.Agency for Healthcare Research and Quality. The TAKEheart Goal. Accessed on June 19, 2020 at https://takeheart.ahrq.gov/takeheart-initiative/takeheart-goal.
- 10.Bachmann JM, Duncan MS, Shah AS, et al. Association of Cardiac Rehabilitation With Decreased Hospitalizations and Mortality After Ventricular Assist Device Implantation. JACC Heart Fail. 2018;6(2):130–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beatty AL, Truong M, Schopfer DW, Shen H, Bachmann JM, and Whooley MA. Geographic Variation in Cardiac Rehabilitation Participation in Medicare and Veterans Affairs Populations: Opportunity for Improvement. Circulation. 2018;137(18):1899–1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McNeely J, Ritchey MD, Maresh S, et al. Regional Variation in the Availability and Utilization of Cardiac Rehabilitation Services Among Eligible Medicare Fee-for-Service Beneficiaries: Where are the Opportunities for Improvement? Circulation. 2018;134:A15035. [Google Scholar]
- 13.Ritchey MD, Maresh S, McNeely J, et al. Tracking Cardiac Rehabilitation Participation and Completion Among Medicare Beneficiaries to Inform the Efforts of a National Initiative. Circ Cardiovasc Qual Outcomes. 2020;13(1):e005902. doi: 10.1161/CIRCOUTCOMES.119.005902 Epub 2020 Jan 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thomas RJ, Balady G, Banka G, et al. 2018 ACC/AHA Clinical Performance and Quality Measures for Cardiac Rehabilitation: A Report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. J Am Coll Cardiol. 2018;71(16):1814–1837. [DOI] [PubMed] [Google Scholar]
- 15.Patient Protection and Affordable Care Act; HHS Notice of Benefit and Payment Parameters for 2021; Notice Requirement for Non-Federal Governmental Plans, 85 Fed. Reg. 29236 (May 14, 2020) (to be codified at 85 FR 29236).
- 16.Randal TJ, Beatty AL, Beckie TM, et al. Home-Based Cardiac Rehabilitation: A Scientific Statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. J Cardiopulm Rehabil Prev. 2019;39(4):208–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pack QR, Squires RW, Lopez-Jimenez F, et al. The current and potential capacity for cardiac rehabilitation utilization in the United States. J Cardiopulm Rehabil Prev. 2014;34(5):318–26. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


