Abstract
There have been recent reports of children presenting with severe multi-system hyperinflammatory syndrome resembling Kawasaki disease (KD) during current COVID-19 pandemic. Exact pathophysiology is unknown, however, most of the children have multi-organ dysfunction and respiratory system involvement is less common compared to adults. These patients have certain characteristic laboratory parameters different from those seen in children with KD. However, only limited literature is available at present for identification and management of such patients. We report a young girl who presented with fever, rash and other manifestations mimicking classic KD and fulfilling the case definitions for pediatric multi-system inflammatory syndrome. She had lymphopenia, thrombocytopenia and hyponatremia in the absence of macrophage activation syndrome, similar to that seen in patients reported from UK and Italy. Clinical manifestations resolved and laboratory parameters improved with intravenous immunoglobulin and corticosteroids. Early recognition is important to administer immunomodulatory therapy which may be life saving for these patients.
Keywords: COVID-19, Kawasaki disease, PIMS, MIS-C
Lay Summary
Several cases of a severe multi-system inflammatory syndrome have been reported in children during the current COVID-19 pandemic. Clinical manifestations may resemble Kawasaki disease (KD) which is the most common childhood vasculitis. A 7-year-old-girl presented with fever, rash and abdominal pain. Examination showed maculopapular rash over lower limbs, back, right ear, trunk and abdomen; erythema and swelling over bilateral upper eyelids; conjunctival injection; reddened lips and erythema over palms and soles. She had lymphopenia, thrombocytopenia, with elevated erythrocyte sedimentation rate, C-reactive protein (CRP), pro-brain natriuretic peptide and interleukin-6 (IL-6). Real-time polymerase chain reaction for severe acute respiratory syndrome coronavirus 2 was negative. Serology, however, could not be performed due to unavailability. Macrophage activation syndrome was ruled out with normal ferritin and triglyceride with raised fibrinogen level. Echocardiography showed normal coronary diameters. Child received meropenem, intravenous immunoglobulin, aspirin and methylprednisolone. She improved with resolution of fever, decrease in CRP, increase in platelet and lymphocyte count. Index child had features similar to those reported from UK and Italy: features of KD, abdominal pain, lymphopenia, thrombocytopenia, elevated IL-6 and myocardial dysfunction with no significant respiratory involvement. Pediatricians should be aware of such uncommon presentation in children to initiate early treatment with immunomodulatory therapy.
INTRODUCTION
Coronavirus disease 2019 (COVID-19) is now known to affect all age groups. The disease is, however, less severe in children and associated with decreased mortality compared with adults. Several cases of a severe multi-system inflammatory syndrome have been reported in children from UK during COVID-19 pandemic [1]. The constellation of findings has been described as pediatric multi-system inflammatory syndrome (PIMS) temporally related to COVID-19 [2, 3] or multi-system inflammatory syndrome in children and adolescents [4] as per case definitions by World Health Organization (WHO) [2], Royal College of Pediatrics and Child Health (RCPCH) [3] and Centers for Disease Control and Prevention (CDC) [4]. Clinical manifestations of PIMS may resemble Kawasaki disease (KD) which is the most common vasculitic disorder in children [5]. We report a young girl from COVID-19 treatment facility from North India with features of PIMS mimicking KD.
CASE PRESENTATION
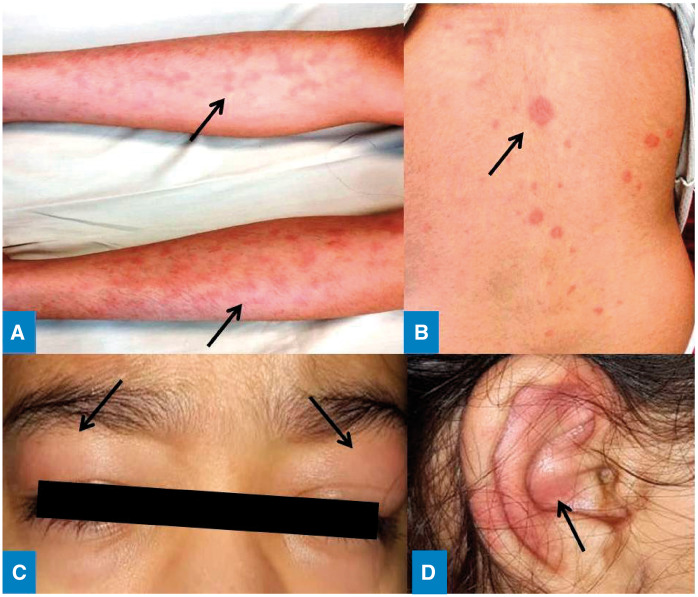
A 7-year-old-girl presented with fever for 5 days, non-pruritic rash over lower limbs and abdominal pain. She did not report history of contact with COVID-19 patient. She had received oral amoxicillin-clavulanate for 3 days without any improvement. Examination showed a febrile child with diffuse erythematous maculopapular rash over lower limbs (Fig. 1A), back (Fig. 1B), right ear (Fig. 1C), trunk and abdomen. Erythema and swelling over bilateral upper eye lids (Fig. 1D), conjunctival injection of eyes, reddened lips and erythema over palms and soles were also noted. However, there was no lymphadenopathy, redness of tongue or edema over hands and feet. Systemic examination was unremarkable. She had hemoglobin 116 g/l (normal: 115–155 g/l), lymphopenia (total leukocyte count 12.7 × 109/l, neutrophils 91%, lymphocytes 4%, monocytes 2%, eosinophils 3%) and thrombocytopenia (platelet count 117 × 109/l, normal: 170–450 × 109/l), with elevated inflammatory markers [erythrocyte sedimentation rate (ESR) 41 mm in first hour, C-reactive protein (CRP) 256.6 mg/l]. Pro-brain natriuretic peptide (NT-pro BNP: 2300 pg/ml, normal: <125 pg/ml) and interleukin-6 (IL-6: 684, normal: 0–7) level were elevated. She also had hyponatremia (serum sodium 128.7 mmol/l, normal: 136–146 mmol/l) and minimal right pleural effusion on ultrasonography. Chest X-ray, urine examination, renal and liver functions were normal. Procalcitonin was 1.1 ng/ml and blood culture was sterile. Work up for typhoid, dengue, malaria, scrub typhus and chikungunya was negative. Real-time polymerase chain reaction (RT-PCR) for severe acute respiratory syndrome coronavirus 2 (SARS CoV-2) was also negative. Macrophage activation syndrome (MAS) was ruled out with normal ferritin (89.97 ng/ml) and fasting triglyceride (134.9 mg/dl) with raised fibrinogen (507 mg/dl) level. Echocardiography showed left main coronary artery 2.8 mm (z-score −0.4), left anterior descending artery 1.5 mm (z-score −1.91), left circumflex artery 1.1 mm (z-score −2.41), right coronary artery 2.1 mm (z-score −1.21) with normal ejection fraction suggesting normal coronary artery diameters.
Fig 1.
Maculopapular rash over (A) bilateral lower limbs, (B) back, (C) erythema and swelling over bilateral upper eye lids and (D) right ear.
A diagnosis of PIMS mimicking classic KD was proffered. Child received meropenem, intravenous immunoglobulin (IVIG) at 2 g/kg body weight and aspirin (3 mg/kg body weight). In view of PIMS, methylprednisolone (15 mg/kg/day) was also administered for 3 days. Child showed improvement with resolution of fever, decrease in CRP (4.46 mg/l), rise in platelet (355 × 109/l) and lymphocyte count (total leukocyte count 10.2 × 109/l, neutrophils 72%, lymphocytes 26%) and serum sodium level (138.4 mmol/l). Oral prednisolone has been planned for 2 weeks.
DISCUSSION
Clinical manifestations in patients with KD occur as a result of cytokine cascade causing multi-system vasculitis involving medium sized arteries. A hyperinflammatory state is also reported in patients with COVID-19. Children with hyper-inflammatory syndrome are increasingly being reported during current COVID-19 pandemic. The first reported cohort of children with PIMS from UK had following sentinel features [1]: fulfilled criteria for classic or incomplete KD, no significant respiratory involvement in most of the children, thrombocytopenia (75%), negative SARS CoV-2 testing in all children and no identifiable micro-organism. Compared to the historic cohort of KD at Giovanni, Italy, children with KD diagnosed during COVID-19 pandemic had lymphopenia (80%), thrombocytopenia (80%), hyponatremia (80%) and a more severe disease course necessitating adjunctive steroids [6]. Serology for SARS CoV-2 antibodies revealed IgG positivity in 80% patients while PCR was positive in only 20% [6].
Index child fulfilled the criteria for classic KD [5] and PIMS (Table 1). However, presence of lymphopenia, thrombocytopenia, hyponatremia and myocardial dysfunction (raised NT-pro BNP) in absence of MAS strongly favours PIMS. RT-PCR for SARS-CoV2 was negative in our child. Serology, however, could not be performed due to unavailability. Treatment options for children with PIMS include IVIG, corticosteroids and Tocilizumab. Our child responded to IVIG and methylprednisolone with resolution of fever and decrease in CRP.
Table 1.
Comparison of various case definitions of PIMS with index child
| Characteristic | WHO preliminary case definition [2] | RCPCH case definition [3] | CDC case definition [4] | Index child |
|---|---|---|---|---|
| Age (years) | 0–19 | Child, age not defined | <21 | 7 |
| Fever duration | ≥3 days | Persistent, duration not defined | ≥24 h | 5 days |
| Muco-cutaneous manifestations | Rash, bilateral non-purulent conjunctivitis, muco-cutaneous inflammation signs involving oral cavity, hands or feet | Classic or incomplete KD | Classic or incomplete KD | Classic KD |
| Organ involvement | Myocardial dysfunction, pericarditis, valvulitis or coronary abnormalities (ECHO findings, elevated troponin, NT-pro BNP) | Single or multi-organ dysfunction (shock, cardiac, respiratory, renal, gastrointestinal or neurological) | Multi-organ dysfunction (cardiac, renal, respiratory, hematologic, gastrointestinal, dermatologic and neurological) | Myocardial (raised NT-pro BNP), hematologic (lymphopenia and thrombocytopenia) and gastrointestinal (abdominal pain) |
| Acute gastro-intestinal problem | Diarrhea, vomiting or abdominal pain | Diarrhea, vomiting or abdominal pain | Not included | Abdominal pain |
| Lab parameters | Elevated ESR, CRP or procalcitonin | Neutrophilia, lymphopenia, low albumin, elevated CRP, D-dimer, ferritn, IL-6, IL-10 and thrombocytopenia | Neutrophilia, lymphopenia, low albumin, Elevated ESR, CRP, procalcitonin, fibrinogen, D-dimer, ferritin, LDH and IL-6 | Neutrophilia, lymphopenia, thrombocytopenia, hyponatremia, elevated ESR, CRP and IL-6 |
| No other obvious microbial cause | Included | Included | Included | Work up for infective etiology and MAS negative |
| Evidence of COVID-19 | RT-PCR, antigen test or serology positive or likely contact with patient with COVID-19 | May be positive or negative | RT-PCR, antigen test or serology positive or COVID-19 exposure within 4 weeks prior to symptom onset | RT-PCR negative. Serology could not be done due to unavailability |
ECHO, echocardiography; LDH, lactate dehydrogenase.
PIMS is an emerging condition and limited information is currently available about etiology, risk factors, pathophysiology, disease course and long-term implications. Multi-disciplinary approach involving pediatric rheumatologists, pediatricians and pediatric intensivists is required to identify such presentations in children and to initiate early treatment with immunomodulatory therapy.
ACKNOWLEDGEMENT
The authors acknowledge Dr Vikram Lahoria, Consultant Dermatologist, Max Super Speciality Hospital, Mohali, Punjab, India, for his involvement in patient care.
REFERENCES
- 1. Riphagen S, Gomez X, Gonzales-Martinez C, et al. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet 2020;395:1607–08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Multisystem Inflammatory Syndrome in Children and Adolescents Temporally Related to COVID-19. World Health Organization. : https://www.who.int/news-room/commentaries/detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19 (29 May 2020, date last accessed).
- 3.Guidance—Paediatric Multisystem Inflammatory Syndrome Temporally Associated With COVID-19. Royal College of Paediatrics and Child Health. https://www.rcpch.ac.uk/resources/guidance-paediatric-multisystem-inflammatory-syndrome-temporally-associated-covid-19 (29 May 2020, date last accessed).
- 4.AAP News. CDC Details COVID-19-Related Inflammatory Syndrome in Children. https://www.aappublications.org/news/2020/05/14/covid19 inflammatory 051420 (29 May 2020, date last accessed).
- 5. Gupta A, Singh S.. Kawasaki disease for dermatologists. Indian Dermatol 2016;7:461–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Verdoni L, Mazza A, Gervasoni A, et al. An outbreak of severe Kawasaki like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet 2020;395:1771–8. [DOI] [PMC free article] [PubMed] [Google Scholar]