Brief overview of COVID-19 in Wuhan, China
COVID-19 has become a global health crisis since its initial outbreak in Wuhan, China in December 2019, now affecting >520 000 people worldwide. Across China, a total of 82 078 confirmed cases had been reported as of 27 March 2020, more than half of whom were from Wuhan (50 006 confirmed cases). As revealed by China CDC1 (data from 11 February 2020), the epidemic curve of onset of symptoms peaked on 23–26 January for the general population.
The basic reproductive number (R0) is estimated to be 2.0–4.0. It is noteworthy that the epidemic doubling time was 2.4 days between 20 January and 2 February,2 and the growth rate had considerably slowed down thanks to the rigorous quarantine and prevention measures issued by the government.
Unfortunately, 1716 health workers became infected, 63% of whom were in Wuhan.1 Of these, 14.6% of confirmed cases among health workers were classified as severe or critical and 5 deaths were noted. In a previous report from our hospital3, of the 138 COVID-19 patients, 57 (41.3%) were presumed to have acquired the infection in hospital, including 17 patients (12.3%) who were already hospitalized for other reasons and 40 health workers (29%). Patient-to-patient transmission was also presumed to have occurred. Furthermore, health worker infections seemed more overwhelming in general wards than in wards specific for patients admitted with COVID-19: 77.5% for the former and 22.5% for the latter. The above data warn that cross-infection in hospital poses a serious danger for both health workers and inpatients.
Poor awareness of personal protection at the early stage of the COVID-19 outbreak may partly explain the high incidence of infection of health workers in general wards. A Department of Cardiology may also encounter COVID-19 cases in clinical practice. Large pitfalls can exist when patients are asymptomatic on admission but presented due to cardiovascular symptoms. As such, early identification and proper protection measures are crucial to reduce possible transmission among health workers and inpatients.
Herein, we present the COVID-19 cases we have confronted in the department of Cardiology of Zhongnan Hospital, Wuhan University and share our experiences in containing the spread of COVID-19 in hospital.
Presentation of five COVID-19 cases in cardiology
Between 1 and 31 January 2020, of 417 inpatients and 116 health workers in our department, 4 patients (1 male, 3 female) and 1 nurse (female) were diagnosed with COVID-19. The 77-year-old male patient, who was initially admitted for acute myocardial infarction (AMI), was confirmed as COVID-19 (presumed to be hospital acquired) and died of respiratory and circulation failure 2 weeks later. In the other three patients, the outbreak occurred shortly after hospitalization but they showed no COVID-19-related symptoms, and were presumed to be already in the incubation period before admission. They eventually recovered and were discharged. The nurse probably became infected due to close contact with confirmed patients when providing nursing care under insufficient personal protection, since she had no other known exposure history. Details of these cases are given in Supplementary material online.
Practical strategies and suggestions against COVID-19 from cardiology
To contain possible transmissions in the cardiology ward, we have elaborated a detailed protection plan defining personal protection in different clinical settings on the basis of general control and prevention principles. Our major control and prevention measures are summarized in Table 1. Regarding the use of personal protection equipment (PPE), facial and eye protection, gown, and gloves are considered crucial since the main transmission routes of COVID-19 are respiratory droplets and contact. The PPE is classified into three levels according to exposure risk. For instance, a level-1 PPE is used for general medical contact with non-infected inpatients in cardiology, while a level-3 PPE is proposed when aerosol-generating procedures (i.e. cardiopulmonary resuscitation) or emergent cardiovascular interventions are performed for confirmed or highly suspected cases.
Table 1.
Practical protection and prevention measures developed in cardiology
| Key measures |
|
| PPE applied |
|
PPE, personal protection equipment.
Our measures are adapted from Regulation for Prevention and Control of Healthcare Associated Infection of Airborne Transmission Disease in Healthcare Facilities (People’s Republic of China, WS/T 511-2016).
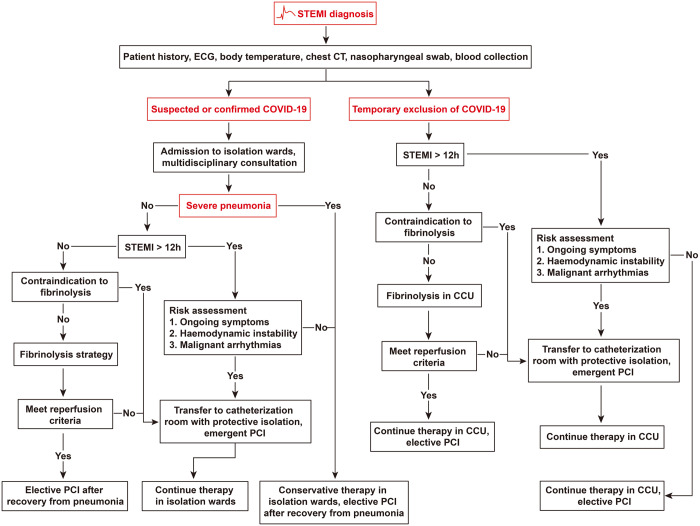
AMI is one of the most life-threatening cardiovascular emergencies. In response to the epidemic, a modified workflow for managing AMI patients was developed in our centre (Figure 1), which had undergone repeated discussions among local cardiologists before its implementation, by fully weighing the risk–benefit ratio from both the patients’ and health workers’ perspective.
Figure 1.
Workflow for the management of STEMI patients in the context of a COVID-19 outbreak. STEMI, ST-segment elevation myocardial infarction; CCU, coronary care unit; PCI, percutaneous coronary intervention.
Although primary percutaneous coronary intervention (PCI) or emergent PCI is an effective reperfusion strategy, especially for ST-segment elevation myocardial infarction (STEMI) cases, its role had to be relatively secondary in the context of the sudden COVID-19 outbreak. Increased exposure risks due to lack of negative pressure catheterization rooms and shortage of PPE and the significant increased difficulty in fine manipulation of guidewires under level-3 protection may all contribute to clinical decision-making. We recommend that fibrinolysis be preferred when both PCI and fibrinolysis can be selected. Once PCI is required, all staff engaged should be under level-3 protection, and thorough environmental disinfection must be given after each PCI.
Similarly, for patients with non-STEMI, PCI can be performed in the high-risk population group: ongoing ischaemic symptoms, haemodynamic instability, and malignant arrhythmias. An in-hospital multidisciplinary consultation (involving experts from cardiology, ICU, department of infectious disease, and emergency department) should be organized in cases of AMI or other cardiovascular emergencies complicated with COVID-19. However, we have to acknowledge that our changed treatment for AMI is not evidence based but is a compromise in the context of the COVID-19 pandemic. Further validations may be warranted to observe its potential impact on patient outcome.
Conclusion
Great care should also be taken by cardiologists since they may also confront COVID-19 cases. Prompt identification could be challenging when the patients are asymptomatic or still in an incubation period at admission, highlighting the importance of early proper protection measures in advance. Our practical strategies could be useful for cardiology departments worldwide in response to the COVID-19 outbreak.
References
References are available as Supplementary material at European HeartJournal online.
Supplementary Material
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.