Abstract
Background
Diabetes is a progressive disease, and thus, it is important to prevent diabetes at the prediabetes stage. Although the loss of muscle strength and prediabetes are associated, few studies have examined relative handgrip strength (RHGS), which can be an indicator of both muscle strength and adiposity. Therefore, our study aimed to examine the association between RHGS and prediabetes (HbA1c level >5.7%) stratified by sex due to sex differences in strength.
Methods
We analyzed data from the 2016–2018 Korean National Health and Nutrition Examination Survey. Prediabetes was defined using the HbA1c cut-off level of 5.7–6.4%, identified by the American Diabetes Association. RHGS was calculated as the maximal absolute handgrip strength of both hands divided by body mass index and was divided into sex-specific quartiles. Multiple logistic regression analysis was performed to determine the association between sex-specific RHGS and prediabetes.
Results
Among the total participants, 13,384 did not have diabetes. In men, the low and mid-low RHGS groups had increased odds of prediabetes (low group, odds ratio [OR]: 1.42, 95% confidence interval [CI]: 1.10–1.82; mid-low group, OR: 1.32, 95% CI: 1.04–1.67). However, no significant differences were observed between the corresponding female groups. Moreover, central obesity and lower RHGS were strongly associated with prediabetes in men (low group, OR: 2.40, 95% CI: 1.52–3.80; mid-low group, OR: 2.00, 95% CI: 1.26–3.17; mid-high group, OR: 1.76, 95% CI: 1.11–2.81), and a trend was observed (p = 0.0026).
Conclusion
RHGS could be a practical and inexpensive tool for predicting diabetes in men. Programs aimed at preventing diabetes need to include exercise routines for improving muscle strength, and further research through longitudinal studies is required to investigate the causality of RHGS on the risk of prediabetes.
Introduction
Diabetes is a non-communicable, progressive disease characterized by high blood glucose and elevated glycated hemoglobin (HbA1c) levels. According to the World Health Organization, 422 million people worldwide had diabetes in 2014 [1]. Compared to 1980, the age-specific prevalence of diabetes had doubled in men and was 60% higher in women in 2014 [2].
It is well known that obesity is a major risk factor for type 2 diabetes. One cohort study found that an increased body mass index (BMI) is associated with an increased risk of type 2 diabetes and that preventing obesity is linked to preventing diabetes [3]. Physical activity, which leads to energy expenditure, and skeletal muscle contraction can activate glucose metabolism and prevent obesity and diabetes [4] as well as strengthen muscles [5].
Some studies have shown that loss of muscle strength is associated with diabetes and that insulin resistance causes muscle protein loss [6, 7]. This is because skeletal muscle is the major site of insulin-mediated glucose uptake [8]. When muscle capacity decreases, insulin resistance increases, which can lead to diabetes progression. Previous studies found that patients with diabetes had low muscle strength [7, 9] and strengthening muscles via exercise has been reported to improve glycemic control in patients with diabetes [4, 10].
Handgrip strength is recommended as a simple and economical method for measuring muscle strength [11, 12], and absolute handgrip strength is the sum of the maximal measurement values of both hands [13]. Moreover, relative handgrip strength (RHGS), which considers BMI, can reflect both muscle strength and adiposity [11]. Thus, it is used as a more objective index than absolute handgrip strength.
It has been revealed that handgrip strength is a predictor of body protein loss and is linked to insulin resistance [14].One study of South Korean adults found an association between RHGS and diabetes diagnosed using fasting glucose levels [15]. Large population-based studies were also performed and found significant associations between RHGS and prediabetes [16, 17]. However, only a few studies have investigated the association between RHGS and prediabetes after adjusting for obesity.
We hypothesized that those with low RHGS were more likely to have an HbA1c level over 5.7% after adjusting for several health characteristics including obesity. Therefore, our study aimed to examine the association between RHGS and HbA1c levels, which reflect blood glucose levels [1], over a period of a few weeks. Moreover, due to sex differences in strengths [18], we investigated the differences in the prevalence of prediabetes according to RHGS between men and women.
Methods
Study population
This study used data from the Korea National Health and Nutrition Examination Survey (KNHANES). The KNHANES is a nationwide, population-based, cross-sectional survey assessing the health and nutritional status of the Korean population. It uses a stratified multistage cluster-sampling design to obtain a nationally representative sample. This survey has been conducted annually by the Korean Centers for Disease Control and Prevention since 1998. The data were not reviewed by an institutional review board on the basis of the Bioethics Act and Article 2 of its enforcement regulations. Furthermore, written consent was obtained from all participants before this survey. We conducted this study using the data from KNHANES Ⅶ (2016–2018).
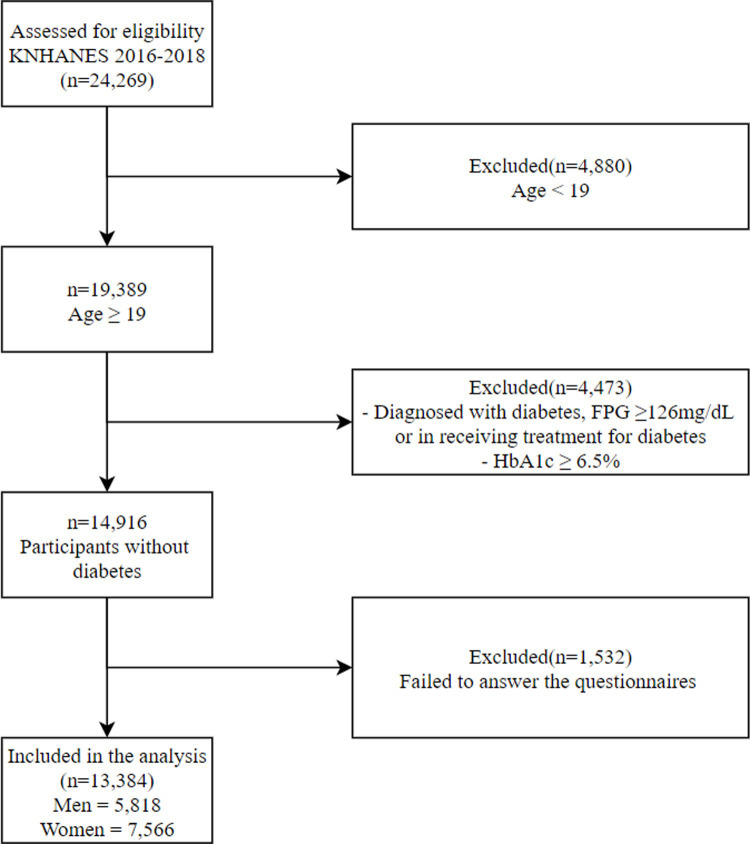
We excluded participants aged under 19 years (n = 4,880) and those who were diagnosed with diabetes mellitus (fasting plasma glucose levels over 126 mg/dL, HbA1c levels over 6.5%, or the use of medications for diabetes mellitus) (n = 4,473) among the total subjects (n = 24,269). Furthermore, we excluded those without data for the variables included in our study (n = 1,532). Finally, 13,384 survey participants (5,818 men, 7,566 women) were selected for this study (Fig 1).
Fig 1. Flow diagram of subject inclusion and exclusion criteria.
Abbreviations: KNHANES, Korea National Health and Nutrition Examination Survey; FPG, fasting plasma glucose.
Variables
The presence of prediabetes was the main outcome of this study, and we defined prediabetes using the HbA1c cut-off of 5.7–6.4%, identified by the American Diabetes Association [19]. We then separated our population into two groups: those with HbA1c levels more than and equal to or less than 5.7%; we defined participants who had HbA1c levels over 5.7% as those with prediabetes.
As the main independent variable, RHGS was calculated as the maximal absolute handgrip strength of both hands divided by BMI [11]. In the survey, handgrip strength was measured in the standing position in participants without disabilities in either hand. We considered sex-specific RHGS, because RHGS has been reported to differ according to sex [18]. We then divided sex-specific RHGS into quartiles and specified the 1st, 2nd, 3rd, and 4th quartiles as the low, mid-low, mid-high, and high groups, respectively.
Independent variables that may act as potential confounding variables included sociodemographic, economic, and health-related characteristics. Sociodemographic characteristics included age (19–29, 30–39, 40–49, 50–59, or ≥60 years), marital status (living with or without spouse), region (metropolitan or rural area), and educational level (middle school or less, high school, and college or over). Economic characteristics included occupation category and household income (low, mid-low, mid-high, or high). Health-related characteristics included smoking status, alcohol consumption status, aerobic exercise, BMI, waist circumference, and comorbidities.
Occupations were categorized according to the Korean version of the Standard Classification of Occupations (KSCO) based on the International Standard Classification of Occupations by the International Labor Organization. We re-categorized the classifications into four categories: white (office work), pink (sales and service), blue (agriculture, forestry, fishery, and armed forces occupation), and inoccupation. Lifetime smoking experience was classified as “yes” or “no” based on the response to the question: “Are you a current smoker?”. Drinking experience was classified as “yes” or “no” based on the response to the following question: “How often did you drink alcohol in the current year?”. Those who had consumed alcohol once or more within the current year were classified to have drinking experience. Those practicing aerobic exercise were defined as participants who performed moderate exercise for over 150 min, vigorous exercise for over 75 min, or a mixture of both (rating 1 min for moderate exercise and 2 min for vigorous exercise) for over 150 min per week regardless of working and exercising. BMI was classified into three groups as follows: underweight and normal range (≤22.9), overweight (23.0–24.9), and obese (≥25). Waist circumference (WC) was classified into two groups according to the cut-off point for central obesity for adults, recommended by the Korean Society for the Study of Obesity. The cut-off points are as follows: for men, ≥90 cm and for women, ≥85 cm. Comorbidities included hypertension, hyperlipidemia, stroke and myocardial infarction, and angina, and we calculated the number of comorbid diseases that each person had.
Statistical analysis
Independent variables were compared using the chi-squared test to identify the association between RHGS and HbA1c levels. After adjusting for sociodemographic, economic, and health-related variables, we used multiple logistic regression analysis to evaluate the association between RHGS and HbA1c levels. Multiple logistic regression is used for dichotomous single-outcome variables and when there is more than one independent variable [20]. The results were reported using odds ratios (ORs) and confidence intervals (CIs). Moreover, we performed subgroup analysis stratified by sex and multiple logistic regression analysis to examine the associations of sex-specific RHGS in subjects with HbA1c levels, age, smoking status, alcohol consumption, aerobic exercise, BMI, and WC. In the subgroup analysis, we tested the trends for significance after adjusting for sociodemographic, economic, and health-related variables to determine the OR trend related to prediabetes (≥5.7%) in each category. Differences were considered significant at p-values of <0.05 as well as at p-values for trends <0.05. All statistical analyses were performed using SAS software (version 9.4; SAS Institute, Cary, NC).
Results
For the purpose of this study, we analyzed each variable according to sex. Table 1 shows the general characteristics of the study population. Among the 13,384 participants, 1,643 men (28.2%) and 2,148 women (28.4%) met the criteria for prediabetes. According to RHGS, 572 (39.3%), 462 (31.8%), 367 (25.2%), and 242 (16.6%) men with prediabetes and 815 (43.1%), 584 (30.9%), 450 (23.8%), and 299 (15.8%) women with prediabetes were included in the low, mid-low, mid-high, and high RHGS groups, respectively.
Table 1. General characteristics of the study population.
| Variables | HbA1c | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | |||||||||||||
| TOTAL | ≥5.7% | <5.7% | P-value | TOTAL | ≥5.7% | <5.7% | P-value | |||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |||
| Total(n = 13,384) | 5,818 | 100.0 | 1,643 | 28.2 | 4,175 | 71.8 | 7,566 | 100.0 | 2,148 | 28.4 | 5,418 | 71.6 | ||
| Sex-specific RHGSa | <0.0001 | <0.0001 | ||||||||||||
| Q1 (low) | 1,455 | 25.0 | 572 | 39.3 | 883 | 60.7 | 1,892 | 25.0 | 815 | 43.1 | 1,077 | 56.9 | ||
| Q2 (mid-low) | 1,454 | 25.0 | 462 | 31.8 | 992 | 68.2 | 1,891 | 25.0 | 584 | 30.9 | 1,307 | 69.1 | ||
| Q3 (mid-high) | 1,455 | 25.0 | 367 | 25.2 | 1,088 | 74.8 | 1,891 | 25.0 | 450 | 23.8 | 1,441 | 76.2 | ||
| Q4 (high) | 1,454 | 25.0 | 242 | 16.6 | 1,212 | 83.4 | 1,892 | 25.0 | 299 | 15.8 | 1,593 | 84.2 | ||
| Age (years) | <0.0001 | <0.0001 | ||||||||||||
| 19–29 | 902 | 15.5 | 45 | 5.0 | 857 | 95.0 | 1,024 | 13.5 | 38 | 3.7 | 986 | 96.3 | ||
| 30–39 | 1,097 | 18.9 | 176 | 16.0 | 921 | 84.0 | 1,357 | 17.9 | 150 | 11.1 | 1,207 | 88.9 | ||
| 40–49 | 1,140 | 19.6 | 287 | 25.2 | 853 | 74.8 | 1,592 | 21.0 | 296 | 18.6 | 1,296 | 81.4 | ||
| 50–59 | 1,021 | 17.5 | 380 | 37.2 | 641 | 62.8 | 1,505 | 19.9 | 554 | 36.8 | 951 | 63.2 | ||
| ≥60 | 1,658 | 28.5 | 755 | 45.5 | 903 | 54.5 | 2,088 | 27.6 | 1,110 | 53.2 | 978 | 46.8 | ||
| Marital Status | <0.0001 | 0.0047 | ||||||||||||
| Living with spouse | 4,108 | 70.6 | 1,366 | 33.3 | 2,742 | 66.7 | 5,165 | 68.3 | 1,518 | 29.4 | 3,647 | 70.6 | ||
| Living without spouse | 1,710 | 29.4 | 277 | 16.2 | 1,433 | 83.8 | 2,401 | 31.7 | 630 | 26.2 | 1,771 | 73.8 | ||
| Region | 0.1971 | 0.9529 | ||||||||||||
| Metropolitan area | 2,766 | 47.5 | 759 | 27.4 | 2,007 | 72.6 | 3,618 | 47.8 | 1,026 | 28.4 | 2,592 | 71.6 | ||
| Rural | 3,052 | 52.5 | 884 | 29.0 | 2,168 | 71.0 | 3,948 | 52.2 | 1,122 | 28.4 | 2,826 | 71.6 | ||
| Occupational categoriesb | <0.0001 | <0.0001 | ||||||||||||
| White | 1,880 | 32.3 | 419 | 22.3 | 1,461 | 77.7 | 1,898 | 25.1 | 292 | 15.4 | 1,606 | 84.6 | ||
| Pink | 610 | 10.5 | 151 | 24.8 | 459 | 75.2 | 1,174 | 15.5 | 349 | 29.7 | 825 | 70.3 | ||
| Blue | 1,861 | 32.0 | 633 | 34.0 | 1,228 | 66.0 | 1,102 | 14.6 | 443 | 40.2 | 659 | 59.8 | ||
| Inoccupation | 1,467 | 25.2 | 440 | 30.0 | 1,027 | 70.0 | 3,392 | 44.8 | 1,064 | 31.4 | 2,328 | 68.6 | ||
| Educational level | <0.0001 | <0.0001 | ||||||||||||
| Middle school or less | 1,172 | 20.1 | 509 | 43.4 | 663 | 56.6 | 2,159 | 28.5 | 1,035 | 47.9 | 1,124 | 52.1 | ||
| High school | 2,016 | 34.7 | 531 | 26.3 | 1,485 | 73.7 | 2,438 | 32.2 | 610 | 25.0 | 1,828 | 75.0 | ||
| College or over | 2,630 | 45.2 | 603 | 22.9 | 2,027 | 77.1 | 2,969 | 39.2 | 503 | 16.9 | 2,466 | 83.1 | ||
| Household income | <0.0001 | <0.0001 | ||||||||||||
| Low | 798 | 13.7 | 291 | 36.5 | 507 | 63.5 | 1,220 | 16.1 | 520 | 42.6 | 700 | 57.4 | ||
| Mid-low | 1,346 | 23.1 | 422 | 31.4 | 924 | 68.6 | 1,826 | 24.1 | 560 | 30.7 | 1,266 | 69.3 | ||
| Mid-high | 1,728 | 29.7 | 440 | 25.5 | 1,288 | 74.5 | 2,177 | 28.8 | 554 | 25.4 | 1,623 | 74.6 | ||
| High | 1,946 | 33.4 | 490 | 25.2 | 1,456 | 74.8 | 2,343 | 31.0 | 514 | 21.9 | 1,829 | 78.1 | ||
| Smoking | <0.0001 | <0.0001 | ||||||||||||
| Yes | 4,339 | 74.6 | 1,354 | 31.2 | 2,985 | 68.8 | 859 | 11.4 | 167 | 19.4 | 692 | 80.6 | ||
| No | 1,479 | 25.4 | 289 | 19.5 | 1,190 | 80.5 | 6,707 | 88.6 | 1,981 | 29.5 | 4,726 | 70.5 | ||
| Alcohol consumption | <0.0001 | <0.0001 | ||||||||||||
| Yes | 4,952 | 85.1 | 1,317 | 26.6 | 3,635 | 73.4 | 5,237 | 69.2 | 1,254 | 23.9 | 3,983 | 76.1 | ||
| No | 866 | 14.9 | 326 | 37.6 | 540 | 62.4 | 2,329 | 30.8 | 894 | 38.4 | 1,435 | 61.6 | ||
| Practicing aerobic exercise | <0.0001 | <0.0001 | ||||||||||||
| Yes | 2,834 | 48.7 | 672 | 23.7 | 2,162 | 76.3 | 3,252 | 43.0 | 844 | 26.0 | 2,408 | 74.0 | ||
| No | 2,984 | 51.3 | 971 | 32.5 | 2,013 | 67.5 | 4,314 | 57.0 | 1,304 | 30.2 | 3,010 | 69.8 | ||
| Obesity Status (BMI)c | <0.0001 | <0.0001 | ||||||||||||
| Underweight & Normal range | 1,989 | 34.2 | 396 | 19.9 | 1,593 | 80.1 | 4,012 | 53.0 | 786 | 19.6 | 3,226 | 80.4 | ||
| Overweight | 1,532 | 26.3 | 416 | 27.2 | 1,116 | 72.8 | 1,548 | 20.5 | 511 | 33.0 | 1,037 | 67.0 | ||
| Obese | 2,297 | 39.5 | 831 | 36.2 | 1,466 | 63.8 | 2,006 | 26.5 | 851 | 42.4 | 1,155 | 57.6 | ||
| Waist circumferenced | <0.0001 | <0.0001 | ||||||||||||
| Men(≥90cm), Women(≥85cm) | 1,761 | 30.3 | 724 | 41.1 | 1,037 | 58.9 | 1,704 | 22.5 | 809 | 47.5 | 895 | 52.5 | ||
| Men(<90cm), Women(<85cm) | 4,057 | 69.7 | 919 | 22.7 | 3,138 | 77.3 | 5,862 | 77.5 | 1,339 | 22.8 | 4,523 | 77.2 | ||
| The number of chronic diseasese | <0.0001 | <0.0001 | ||||||||||||
| 0 | 4,227 | 72.7 | 925 | 21.9 | 3,302 | 78.1 | 5,649 | 74.7 | 1,135 | 20.1 | 4,514 | 79.9 | ||
| 1 | 1,076 | 18.5 | 469 | 43.6 | 607 | 56.4 | 1,283 | 17.0 | 623 | 48.6 | 660 | 51.4 | ||
| ≥2 | 515 | 8.9 | 249 | 48.3 | 266 | 51.7 | 634 | 8.4 | 390 | 61.5 | 244 | 38.5 | ||
a Relative Hand Grip Strength, categorized into sex-specific quartiles
Men: Q1(<2.78), Q2(2.78–3.22), Q3(3.22–3.66), Q4(>3.66).
Women: Q1(<1.67), Q2(1.67–2.00), Q3(2.00–2.33), Q4(>2.33).
bThree groups (white, pink, blue) based on the International Standard Classification Occupations codes. Inoccupation group includes housewives.
cBMI: Body mass index/obesity status defined by BMI based on the 2018 Clinical Practice Guidelines for Overweight and Obesity in Korea.
dCentral obesity is defined by waist circumference. The cut-off points for Korean adults were decided by the Korean Society for the Study of Obesity.
eChronic disease was defined as diagnosed diseases: hypertension, hyperlipidemia, stroke and myocardial infarction or angina. The number of chronic diseases is the sum of the number of diagnosed above diseases.
Table 2 presents the factors associated with prediabetes. In men, the low and mid-low RHGS groups showed increased odds for prediabetes (low group, OR: 1.42, 95% CI: 1.10–1.82; mid-low group, OR: 1.32, 95% CI: 1.04–1.67). However, no female group showed a significant association between RHGS and prediabetes. Participants who were over the age of 30; qualified as overweight, obese, or having central obesity; and had comorbidities showed significant associations with prediabetes among both sexes.
Table 2. Factors associated with prediabetes.
| Variables | HbA1c ≥5.7% | |||||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | |||||||
| OR | 95% CI | OR | 95% CI | |||||
| Sex-specific RHGSa | ||||||||
| Q1 (low) | 1.42 | (1.10 | - | 1.82) | 1.10 | (0.86 | - | 1.40) |
| Q2 (mid-low) | 1.32 | (1.04 | - | 1.67) | 0.95 | (0.76 | - | 1.19) |
| Q3 (mid-high) | 1.16 | (0.91 | - | 1.48) | 0.99 | (0.81 | - | 1.21) |
| Q4 (high) | 1.00 | 1.00 | ||||||
| Age (years) | ||||||||
| 19–29 | 1.00 | 1.00 | ||||||
| 30–39 | 3.36 | (2.23 | - | 5.07) | 2.85 | (1.88 | - | 4.33) |
| 40–49 | 5.85 | (3.90 | - | 8.76) | 5.63 | (3.73 | - | 8.50) |
| 50–59 | 9.46 | (6.24 | - | 14.35) | 12.93 | (8.42 | - | 19.85) |
| ≥60 | 11.47 | (7.38 | - | 17.82) | 20.17 | (12.83 | - | 31.69) |
| Marital status | ||||||||
| Living with spouse | 1.00 | 1.00 | ||||||
| Living without spouse | 0.98 | (0.79 | - | 1.20) | 1.02 | (0.86 | - | 1.21) |
| Region | ||||||||
| Metropolitan area | 1.00 | 1.00 | ||||||
| Rural | 0.87 | (0.75 | - | 1.02) | 0.87 | (0.76 | - | 1.01) |
| Occupational categoriesb | ||||||||
| White | 1.00 | 1.00 | ||||||
| Pink | 1.33 | (1.02 | - | 1.73) | 1.13 | (0.90 | - | 1.43) |
| Blue | 1.29 | (1.03 | - | 1.61) | 1.17 | (0.92 | - | 1.48) |
| Inoccupation | 1.09 | (0.85 | - | 1.39) | 0.98 | (0.81 | - | 1.18) |
| Educational level | ||||||||
| Middle school or less | 1.03 | (0.83 | - | 1.28) | 1.30 | (1.05 | - | 1.59) |
| High school | 0.93 | (0.73 | - | 1.19) | 1.30 | (1.01 | - | 1.66) |
| College or over | 1.00 | 1.00 | ||||||
| Household income | ||||||||
| Low | 1.10 | (0.84 | - | 1.44) | 1.14 | (0.90 | - | 1.46) |
| Mid-low | 1.09 | (0.90 | - | 1.33) | 1.11 | (0.91 | - | 1.36) |
| Mid-high | 0.92 | (0.76 | - | 1.11) | 1.13 | (0.95 | - | 1.35) |
| High | 1.00 | 1.00 | ||||||
| Smoking | ||||||||
| Yes | 1.39 | (1.16 | - | 1.66) | 0.87 | (0.70 | - | 1.09) |
| No | 1.00 | 1.00 | ||||||
| Alcohol consumption | ||||||||
| Yes | 0.80 | (0.64 | - | 0.99) | 0.85 | (0.74 | - | 0.98) |
| No | 1.00 | 1.00 | ||||||
| Practicing aerobic exercise | ||||||||
| Yes | 1.00 | 1.00 | ||||||
| No | 1.22 | (1.05 | - | 1.42) | 0.89 | (0.77 | - | 1.02) |
| Obesity status (BMI)c | ||||||||
| Underweight and normal weight | 1.00 | 1.00 | ||||||
| Overweight | 1.30 | (1.06 | - | 1.59) | 1.33 | (1.12 | - | 1.59) |
| Obese | 1.86 | (1.45 | - | 2.38) | 1.55 | (1.25 | - | 1.93) |
| Waist circumferenced | ||||||||
| Men (≥90 cm), Women (≥85 cm) | 1.66 | (1.36 | - | 2.02) | 1.62 | (1.33 | - | 1.97) |
| Men (<90 cm), Women (<85 cm) | 1.00 | 1.00 | ||||||
| Number of chronic diseasese | ||||||||
| 0 | 1.00 | 1.00 | ||||||
| 1 | 1.34 | (1.12 | - | 1.61) | 1.42 | (1.20 | - | 1.67) |
| ≥2 | 1.39 | (1.08 | - | 1.78) | 2.20 | (1.77 | - | 2.74) |
a Relative hand grip strength, categorized into sex-specific quartiles
Men: Q1(<2.78), Q2(2.78–3.22), Q3(3.22–3.66), Q4(>3.66).
Women: Q1(<1.67), Q2(1.67–2.00), Q3(2.00–2.33), Q4(>2.33).
bThree groups (white, pink, blue) based on the International Standard Classification Occupations codes Inoccupation group includes housewives.
cBMI: Body mass index; obesity status was defined by BMI based on the 2018 Clinical Practice Guidelines for Overweight and Obesity in Korea.
dCentral obesity is defined using waist circumference. The cut-off points for Korean adults were decided by the Korean Society for the Study of Obesity.
eChronic diseases were defined as diagnosed diseases: hypertension, hyperlipidemia, stroke and myocardial infarction or angina. The number of chronic diseases is the sum of the number of diagnosed mentioned above.
Table 3 shows the results of subgroup analysis stratified by independent variables. Men who smoked, consumed alcohol, or had obesity in the low and mid-low RHGS groups showed significant positive associations with prediabetes. These results were consistent with the main results in Table 2. Moreover, men with central obesity who had lower RHGS showed higher associations with prediabetes (low group, OR: 2.40, 95% CI: 1.52–3.80; mid-low group, OR: 2.00, 95% CI: 1.26–3.17; mid-high group, OR: 1.76, 95% CI: 1.11–2.81), and a trend was observed (p = 0.0026). There were no significant differences in men, and no trend was seen.
Table 3. Subgroup analysis stratified by independent variables*.
| Variables | HbA1c ≥5.7% | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex-specific RHGSa | ||||||||||||||
| Q1 (low) | Q2 (mid-low) | Q3 (mid-high) | Q4 (high) | P value for trend | ||||||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | ||||||||
| Male | ||||||||||||||
| Age (years) | ||||||||||||||
| 19–29 | 2.75 | (0.70 | - | 10.83) | 2.86 | (0.90 | - | 9.11) | 1.67 | (0.42 | - | 6.57) | 1.00 | 0.1143 |
| 30–39 | 2.06 | (1.13 | - | 3.75) | 1.79 | (1.02 | - | 3.14) | 1.43 | (0.83 | - | 2.46) | 1.00 | 0.0340 |
| 40–49 | 1.05 | (0.60 | - | 1.82) | 0.84 | (0.53 | - | 1.34) | 0.74 | (0.46 | - | 1.19) | 1.00 | 0.8438 |
| 50–59 | 1.62 | (0.97 | - | 2.72) | 1.81 | (1.13 | - | 2.89) | 1.51 | (0.97 | - | 2.35) | 1.00 | 0.0439 |
| ≥60 | 1.02 | (0.65 | - | 1.63) | 0.94 | (0.59 | - | 1.50) | 0.94 | (0.56 | - | 1.57) | 1.00 | 0.8427 |
| Smoking | ||||||||||||||
| Yes | 1.35 | (1.02 | - | 1.79) | 1.31 | (1.01 | - | 1.69) | 1.12 | (0.86 | - | 1.46) | 1.00 | 0.1243 |
| No | 1.64 | (0.91 | - | 2.94) | 1.36 | (0.77 | - | 2.40) | 1.22 | (0.71 | - | 2.10) | 1.00 | 0.2343 |
| Alcohol consumption | ||||||||||||||
| Yes | 1.50 | (1.14 | - | 1.97) | 1.43 | (1.10 | - | 1.86) | 1.22 | (0.94 | - | 1.58) | 1.00 | 0.0521 |
| No | 0.98 | (0.52 | - | 1.83) | 0.81 | (0.44 | - | 1.47) | 0.84 | (0.45 | - | 1.57) | 1.00 | 0.9467 |
| Practicing aerobic exercise | ||||||||||||||
| Yes | 1.81 | (1.23 | - | 2.67) | 1.88 | (1.32 | - | 2.68) | 1.49 | (1.02 | - | 2.16) | 1.00 | 0.0078 |
| No | 1.17 | (0.84 | - | 1.64) | 1.00 | (0.74 | - | 1.36) | 0.96 | (0.70 | - | 1.30) | 1.00 | 0.7596 |
| Obesity status (BMI)b | ||||||||||||||
| Underweight and Normal range | 1.06 | (0.65 | - | 1.74) | 0.92 | (0.60 | - | 1.41) | 1.10 | (0.73 | - | 1.64) | 1.00 | 0.6782 |
| Overweight | 0.91 | (0.58 | - | 1.43) | 1.11 | (0.72 | - | 1.71) | 1.07 | (0.71 | - | 1.61) | 1.00 | 0.4073 |
| Obese | 1.90 | (1.23 | - | 2.92) | 1.70 | (1.12 | - | 2.60) | 1.28 | (0.82 | - | 1.99) | 1.00 | 0.0034 |
| Waist circumferencec | ||||||||||||||
| Men(≥90cm), Women(≥85cm) | 2.40 | (1.52 | - | 3.80) | 2.00 | (1.26 | - | 3.17) | 1.76 | (1.11 | - | 2.81) | 1.00 | 0.0026 |
| Men(<90cm), Women(<85cm) | 1.01 | (0.74 | - | 1.38) | 1.14 | (0.85 | - | 1.52) | 1.03 | (0.77 | - | 1.36) | 1.00 | 0.4977 |
| Female | ||||||||||||||
| Age (years) | ||||||||||||||
| 19–29 | 0.63 | (0.31 | - | 2.00) | 1.38 | (0.51 | - | 3.74) | 0.20 | (0.01 | - | 0.75) | 1.00 | 0.9819 |
| 30–39 | 0.97 | (0.45 | - | 2.06) | 0.81 | (0.42 | - | 1.56) | 0.71 | (0.41 | - | 1.23) | 1.00 | 0.9816 |
| 40–49 | 1.42 | (0.89 | - | 2.25) | 0.76 | (0.49 | - | 1.19) | 0.83 | (0.57 | - | 1.22) | 1.00 | 0.3440 |
| 50–59 | 0.96 | (0.62 | - | 1.48) | 1.06 | (0.72 | - | 1.55) | 1.07 | (0.75 | - | 1.53) | 1.00 | 0.7479 |
| ≥60 | 1.09 | (0.64 | - | 1.86) | 0.89 | (0.53 | - | 1.51) | 1.21 | (0.73 | - | 2.02) | 1.00 | 0.9589 |
| Smoking | ||||||||||||||
| Yes | 1.48 | (0.72 | - | 3.03) | 0.86 | (0.42 | - | 1.74) | 0.80 | (0.44 | - | 1.47) | 1.00 | 0.6348 |
| No | 1.10 | (0.85 | - | 1.43) | 0.97 | (0.77 | - | 1.24) | 1.01 | (0.82 | - | 1.26) | 1.00 | 0.7534 |
| Alcohol consumption | ||||||||||||||
| Yes | 1.16 | (0.86 | - | 1.58) | 0.92 | (0.70 | - | 1.21) | 0.97 | (0.76 | - | 1.23) | 1.00 | 0.6670 |
| No | 1.03 | (0.70 | - | 1.51) | 0.99 | (0.67 | - | 1.47) | 0.99 | (0.67 | - | 1.47) | 1.00 | 0.9589 |
| Practicing aerobic exercise | ||||||||||||||
| Yes | 1.17 | (0.80 | - | 1.70) | 0.87 | (0.64 | - | 1.19) | 0.97 | (0.72 | - | 1.31) | 1.00 | 0.7674 |
| No | 1.07 | (0.77 | - | 1.49) | 1.01 | (0.74 | - | 1.39) | 0.98 | (0.74 | - | 1.29) | 1.00 | 0.8685 |
| Obesity status (BMI)b | ||||||||||||||
| Underweight and Normal range | 1.01 | (0.72 | - | 1.41) | 0.91 | (0.67 | - | 1.23) | 0.99 | (0.78 | - | 1.26) | 1.00 | 0.5765 |
| Overweight | 0.99 | (0.60 | - | 1.63) | 0.90 | (0.56 | - | 1.44) | 0.84 | (0.52 | - | 1.35) | 1.00 | 0.8835 |
| Obese | 1.03 | (0.55 | - | 1.95) | 0.82 | (0.44 | - | 1.54) | 0.84 | (0.44 | - | 1.61) | 1.00 | 0.3574 |
| Waist circumferencec | ||||||||||||||
| Men(≥90cm), Women(≥85cm) | 0.81 | (0.44 | - | 1.51) | 0.69 | (0.37 | - | 1.30) | 0.67 | (0.36 | - | 1.27) | 1.00 | 0.7709 |
| Men(<90cm), Women(<85cm) | 1.07 | (0.81 | - | 1.41) | 0.94 | (0.73 | - | 1.21) | 0.97 | (0.78 | - | 1.21) | 1.00 | 0.8557 |
*Adjusted for age, marital status, region, household income, job, educational status, smoking status, alcohol consumption, practicing aerobic exercise, BMI, waist circumference, and the number of chronic diseases.
a Relative Hand Grip Strength, categorized into sex-specific quartiles
Men: Q1(<2.78), Q2(2.78–3.22), Q3(3.22–3.66), Q4(>3.66) / Women: Q1(<1.67), Q2(1.67–2.00), Q3(2.00–2.33), Q4(>2.33).
bBMI: Body mass index; obesity status was defined by BMI based on the 2018 Clinical Practice Guidelines for Overweight and Obesity in Korea.
cCentral obesity is defined using waist circumference. The cut-off points for Korean adults were decided by the Korean Society for the Study of Obesity.
Discussion
This study found that RHGS was negatively associated with prediabetes in men but not in women. This result is similar to that of a previous study, which found a negative relationship between handgrip strength and prediabetes in healthy-weight American adults without diabetes [21]. However, low and mid-low RHGS showed significant associations with prediabetes only in men in this study. This means that men with low handgrip strength relative to their BMI or with high BMI relative to their handgrip strength were likely to have an HbA1c level over 5.7%.
It is well-known that poor health behaviors lead to diabetes. For example, cigarette smoking is associated with increased insulin resistance [22], and excessive alcohol consumption increases the likelihood of developing of many diseases, including diabetes [23]. Moreover, type 2 diabetes is related to a decrease in physical activity and an increase in obesity [4]. Based on these findings, the significant association with prediabetes in men alone may be explained by health-related characteristics. The male participants included in this study had worse health behaviors than female participants. Men tended to smoke more, drink more alcohol, and have a higher prevalence of obesity or central obesity than women. This tendency was similar in the subgroup analysis in this study, which showed the relationship between RHGS, prediabetes, and health-related characteristics. We found that men who smoked, drank alcohol, or were obese had significant associations with lower RHGS and prediabetes. This might be caused by sex-specific demographic and sociographic characteristics: in South Korea, the proportion of men who smoke and drink is higher than that of women [24], and similar patterns have been seen in other countries [25, 26]. Our study’s results were consistent with those reported previously [27].
The differences in hormones and glucose metabolism could also explain the different results between the sexes. Leptin is affected by sex hormones, and high levels of leptin are related to an increased risk of diabetes in men but not in women [28]. Additionally, testosterone impairs insulin-mediated glucose uptake and leads to impaired glycogen synthase expression [29]. In terms of glucose metabolism, some studies have revealed that men had a higher prevalence of impaired fasting glucose levels, while women had a higher prevalence of impaired 2-hour plasma glucose levels [30]. This finding might have affected our results as our definition of diabetes did not consider impaired 2-hour plasma glucose levels. For these reasons, men were more likely to show a significant association between RHGS and prediabetes than women.
In the subgroup analysis, the trends of association were significant in men aged 30–39 years and 50–59 years, those who regularly performed aerobic exercises, those with obesity, and those with central obesity. Furthermore, the association between RHGS and prediabetes was stronger in men who had central obesity. A large WC is a well-known indicator for predicting non-insulin-dependent diabetes [31], and this finding shows that low muscle strength and central obesity are more relevant to diabetes than central obesity alone.
Another findings comparing mentioned above, among men, no drinking experience and lower RHGS were negatively associated with prediabetes, but this association was not significant. However, alcohol consumption is expected to have stronger association with prediabetes than low handgrip in this population. In contrast, not practicing aerobic exercise and having lower RHGS were positively associated with prediabetes among men, but not significantly. Therefore, it can be assumed that low handgrip is a stronger factor than performance of aerobic exercise in this population.
We suspected a negative relationship between RHGS and prediabetes based on the results of some studies which reported an association between muscle strength and diabetes. First, diabetes leads to muscle weakness due to insulin resistance and glucose toxicity. Moreover, insulin resistance is associated with impaired mitochondrial function in muscles [32], which is related to attenuated muscle strength. In addition, intermuscular adipose tissue volume is inversely related with physical function [33] and is greater in those with diabetes [34]. Based on these findings, muscle strengthening is needed to prevent diabetes.
This study has several strengths. By excluding those with diabetes or an HbA1c level over 6.5%, we determined the relationship between handgrip strength and prediabetes. Moreover, this provides evidence for easy prediction of diabetes by assessing both handgrip strength and BMI. In addition, we reported WC as a confounder in this study, which showed a more positive relationship between low muscle strength and prediabetes than with BMI. WC could also be used as a measure for exploring further risk factors of diabetes. Finally, we used representative data collected by a reliable institution in South Korea [35].
However, there are several limitations to this study. First, we used cross-sectional data, and thus, we could only determine an association between RHGS and prediabetes; we could not examine causality between these two variables. Further explanatory studies are needed to infer causality. Second, the estimation of handgrip strength can change according to measurement position [36]. Thus, before applying handgrip strength as a predictor of diabetes, a standardized and accurate method for measuring handgrip strength should be used for all participants. Third, there may be other residual factors that were not included in this study. Fourth, data on insulin resistance and hormone levels were not collected which could have provided a statistical explanation for the results. Fifth, the health-related characteristics used in this study, such as smoking and drinking status, were measured through self-reported questionnaires. Lastly, we used South Korean population-based data, and thus, our results may not apply to other ethnic groups.
Conclusions
This study found a negative relationship between RHGS and prediabetes in men. Thus, an index combining handgrip strength and BMI would be a practical and inexpensive tool for predicting diabetes among men. In addition, central obesity showed a stronger relationship with low muscle strength and prediabetes than with BMI. Programs aimed at improving muscle strength or reducing WC would be beneficial as interventions for preventing diabetes. Further research such as longitudinal studies are required to investigate the causality of RHGS on prediabetes risk.
Acknowledgments
We would like to thank the Korean Centers for Disease Control, which conducted and provided data based on a nationwide survey. In addition, we would like to thank our colleagues at the Institute of Health Services Research of Yonsei University, who provided their advice on intellectual content.
Data Availability
Publicly available data are from the Korea National Health & Nutrition Examination Survey website (https://knhanes.cdc.go.kr/knhanes/eng/index.do).
Funding Statement
The authors received no specific funding for this work.
References
- 1.World Health Organization. Global report on diabetes. 2017.
- 2.Zhou B, Lu Y, Hajifathalian K, Bentham J, Di Cesare M, Danaei G, et al. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4· 4 million participants. The Lancet. 2016;387: 1513–1530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ford ES, Williamson DF, Liu S. Weight change and diabetes incidence: findings from a national cohort of US adults. American Journal of Epidemiology. 1997;146: 214–222 10.1093/oxfordjournals.aje.a009256 [DOI] [PubMed] [Google Scholar]
- 4.Sigal RJ, Kenny GP, Wasserman DH, Castaneda-Sceppa C. Physical activity/exercise and type 2 diabetes. Diabetes Care. 2004;27: 2518–2539 10.2337/diacare.27.10.2518 [DOI] [PubMed] [Google Scholar]
- 5.Gerdhem P, Ringsberg K, Åkesson K, Obrant K. Influence of muscle strength, physical activity and weight on bone mass in a population-based sample of 1004 elderly women. Osteoporosis International. 2003;14: 768–772 10.1007/s00198-003-1444-x [DOI] [PubMed] [Google Scholar]
- 6.Kalyani RR, Corriere M, Ferrucci L. Age-related and disease-related muscle loss: the effect of diabetes, obesity, and other diseases. The Lancet Diabetes & Endocrinology. 2014;2: 819–829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leenders M, Verdijk LB, van der Hoeven L, Adam JJ, Van Kranenburg J, Nilwik R, et al. Patients with type 2 diabetes show a greater decline in muscle mass, muscle strength, and functional capacity with aging. Journal of the American Medical Directors Association. 2013;14: 585–592 10.1016/j.jamda.2013.02.006 [DOI] [PubMed] [Google Scholar]
- 8.Karlsson HK, Zierath JR. Insulin signaling and glucose transport in insulin resistant human skeletal muscle. Cell biochemistry and biophysics. 2007;48: 103–113 10.1007/s12013-007-0030-9 [DOI] [PubMed] [Google Scholar]
- 9.Kelley DE, He J, Menshikova EV, Ritov VB. Dysfunction of mitochondria in human skeletal muscle in type 2 diabetes. Diabetes. 2002;51: 2944–2950 10.2337/diabetes.51.10.2944 [DOI] [PubMed] [Google Scholar]
- 10.Baldi J, Snowling N. Resistance training improves glycaemic control in obese type 2 diabetic men. International journal of sports medicine. 2003;24: 419–423 10.1055/s-2003-41173 [DOI] [PubMed] [Google Scholar]
- 11.Choquette S, Bouchard D, Doyon C, Sénéchal M, Brochu M, Dionne IJ. Relative strength as a determinant of mobility in elders 67–84 years of age. A nuage study: Nutrition as a determinant of successful aging. The Journal of Nutrition, Health & Aging. 2010;14: 190–195 [DOI] [PubMed] [Google Scholar]
- 12.Wind AE, Takken T, Helders PJ, Engelbert RH. Is grip strength a predictor for total muscle strength in healthy children, adolescents, and young adults? European Journal of Pediatrics. 2010;169: 281–287 10.1007/s00431-009-1010-4 [DOI] [PubMed] [Google Scholar]
- 13.Leyk D, Gorges W, Ridder D, Wunderlich M, Rüther T, Sievert A, et al. Hand-grip strength of young men, women and highly trained female athletes. European Journal of Applied Physiology. 2007;99: 415–421 10.1007/s00421-006-0351-1 [DOI] [PubMed] [Google Scholar]
- 14.Windsor J, Hill G. Grip strength: a measure of the proportion of protein loss in surgical patients. British Journal of Surgery. 1988;75: 880–882 10.1002/bjs.1800750917 [DOI] [PubMed] [Google Scholar]
- 15.Choi EY. The association of relative handgrip strength with type 2 diabetes among Koreans aged 20 years or more. Korean Society for Health Promotion and Disease Prevention. 2019;19: 77–83 [Google Scholar]
- 16.Manda CM, Hokimoto T, Okura T, Isoda H, Shimano H, Wagatsuma Y. Handgrip strength predicts new prediabetes cases among adults: A prospective cohort study. Preventive Medicine Reports. 2020;17: 101056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hu S, Gu Y, Lu Z, Zhang Q, Liu L, Meng G, et al. Relationship between grip strength and prediabetes in a large-scale adult population. American journal of preventive medicine. 2019;56: 844–851 10.1016/j.amepre.2019.01.013 [DOI] [PubMed] [Google Scholar]
- 18.Sağiroğlu İ, Kurt C, Ömürlü İK, Çatikkaş F. Does hand grip strength change with gender? The traditional method vs. the allometric normalisation method. European Journal of Physical Education and Sport Science. 2017: [Google Scholar]
- 19.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37: S81–S90 10.2337/dc14-S081 [DOI] [PubMed] [Google Scholar]
- 20.Hosmer DW Jr, Lemeshow S, Sturdivant RX. Applied logistic regression: John Wiley & Sons; 2013. [Google Scholar]
- 21.Mainous AG, Tanner RJ, Anton SD, Jo A. Low grip strength and prediabetes in normal-weight adults. The Journal of the American Board of Family Medicine. 2016;29: 280–282 10.3122/jabfm.2016.02.150262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eliasson B. Cigarette smoking and diabetes. Progress in cardiovascular diseases. 2003;45: 405–413 10.1053/pcad.2003.00103 [DOI] [PubMed] [Google Scholar]
- 23.Fernández-Solà J. Cardiovascular risks and benefits of moderate and heavy alcohol consumption. Nature Reviews Cardiology. 2015;12: 576–587 10.1038/nrcardio.2015.91 [DOI] [PubMed] [Google Scholar]
- 24.Korea Centers for Disease Control & Prevention. Major results of Korea National Health and Nutrition Examination Survey. Available: https://knhanes.cdc.go.kr/knhanes/eng/index.do. Accessed April 3rd 2020.
- 25.Reitsma MB, Fullman N, Ng M, Salama JS, Abajobir A, Abate KH, et al. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: a systematic analysis from the Global Burden of Disease Study 2015. The Lancet. 2017;389: 1885–1906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Griswold MG, Fullman N, Hawley C, Arian N, Zimsen SR, Tymeson HD, et al. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2018;392: 1015–1035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Song X, Qiu M, Wang H, Tong W, Ju L, Gu L, et al. Gender-related affecting factors of prediabetes on its 10-year outcome. BMJ Open Diabetes Research and Care. 2016;4: e000169 10.1136/bmjdrc-2015-000169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen GC, Qin LQ, Ye JK. Leptin levels and risk of type 2 diabetes: gender‐specific meta‐analysis. Obesity Reviews. 2014;15: 134–142 10.1111/obr.12088 [DOI] [PubMed] [Google Scholar]
- 29.Rincon J, Holmäng A, Wahlström EO, Lönnroth P, Björntorp P, Zierath JR, et al. Mechanisms behind insulin resistance in rat skeletal muscle after oophorectomy and additional testosterone treatment. Diabetes. 1996;45: 615–621 10.2337/diab.45.5.615 [DOI] [PubMed] [Google Scholar]
- 30.Mauvais-Jarvis F. Gender differences in glucose homeostasis and diabetes. Physiology & behavior. 2018;187: 20–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wei M, Gaskill SP, Haffner SM, Stern MP. Waist circumference as the best predictor of noninsulin dependent diabetes mellitus (NIDDM) compared to body mass index, waist/hip ratio and other anthropometric measurements in Mexican Americans—a 7‐year prospective study. Obesity Research. 1997;5: 16–23 10.1002/j.1550-8528.1997.tb00278.x [DOI] [PubMed] [Google Scholar]
- 32.Martins AR, Nachbar RT, Gorjao R, Vinolo MA, Festuccia WT, Lambertucci RH, et al. Mechanisms underlying skeletal muscle insulin resistance induced by fatty acids: importance of the mitochondrial function. Lipids in Health and Disease. 2012;11: 30 10.1186/1476-511X-11-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tuttle LJ, Sinacore DR, Mueller MJ. Intermuscular adipose tissue is muscle specific and associated with poor functional performance. Journal of Aging Research. 2012;2012: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tuttle LJ, Sinacore DR, Cade WT, Mueller MJ. Lower physical activity is associated with higher intermuscular adipose tissue in people with type 2 diabetes and peripheral neuropathy. Physical Therapy. 2011;91: 923–930 10.2522/ptj.20100329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kweon S, Kim Y, Jang M-j, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea national health and nutrition examination survey (KNHANES). International Journal of Epidemiology. 2014;43: 69–77 10.1093/ije/dyt228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boadella JM, Kuijer PP, Sluiter JK, Frings-Dresen MH. Effect of self-selected handgrip position on maximal handgrip strength. Archives of Physical Medicine and Rehabilitation. 2005;86: 328–331 10.1016/j.apmr.2004.05.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Publicly available data are from the Korea National Health & Nutrition Examination Survey website (https://knhanes.cdc.go.kr/knhanes/eng/index.do).