Over the past few months, more than 80 000 Americans with COVID-19 have been treated with convalescent plasma, under an expanded access programme. The programme was discontinued on Aug 23, 2020, after the US Food and Drug Administration (FDA) authorised the emergency use of convalescent plasma in hospitalised patients with COVID-19. “This product may be effective in treating COVID-19”, stated the FDA. “The known and potential benefits...outweigh the known and potential risks.” The agency had good reason to sound so cautious. Convalescent plasma remains unproven. A tiny fraction of the thousands of Americans to have received the treatment did so as part of a randomised clinical trial.
“It is definitely disappointing that we were not able to put many of these patients into randomised trials”, said Michelle Gong, director of Critical Care Research at Montefiore Medical Center (New York City, NY, USA). “We have to give the same urgency to research on COVID-19 as we do to the clinical need.” Still, running randomised trials at the same time as dealing with large numbers of critically ill patients is no small task. It may be beyond the capabilities of some institutions. “A lot of the smaller, community hospitals in the USA are not equipped for research, and the worst time to learn is during a pandemic”, concedes Gong. But for those that do possess the requisite baseline capacity, there are established techniques and adaptations for conducting research in the midst of an infectious disease outbreak.
“We have clarity on what is needed to succeed”, confirms John-Arne Rottingen, chair of the international steering committee for WHO's Solidarity trial for COVID-19 therapeutics. Previous pandemics have seen an excess of small, uncoordinated studies with differing designs and inconclusive results. Setting up the studies often took so long that the pandemic had more or less blown over by the time the investigators were ready to start running the trial. “When the pandemic hits, you have to act quickly”, said Rottingen. He added that the trials that provide meaningful clinical value are those with patient populations measured in the thousands. “That is the only way that you can really demonstrate clear effects on outcomes such as the need for ventilation or mortality”, stressed Rottingen.
Solidarity involves more than 10 000 patients across 27 countries. It is evaluating the antimalarial drug hydroxychloroquine, the HIV drug combination lopinavir–ritonavir, and the antiviral medication remdesivir, all of which are compared with the standard-of-care. The hydroxychloroquine and lopinavir–ritonavir groups were discontinued after the interim results indicated that the treatments did not reduce mortality in hospitalised patients with COVID-19. The groups involving remdesivir and lopinavir–ritonavir plus interferon beta-1a are ongoing.
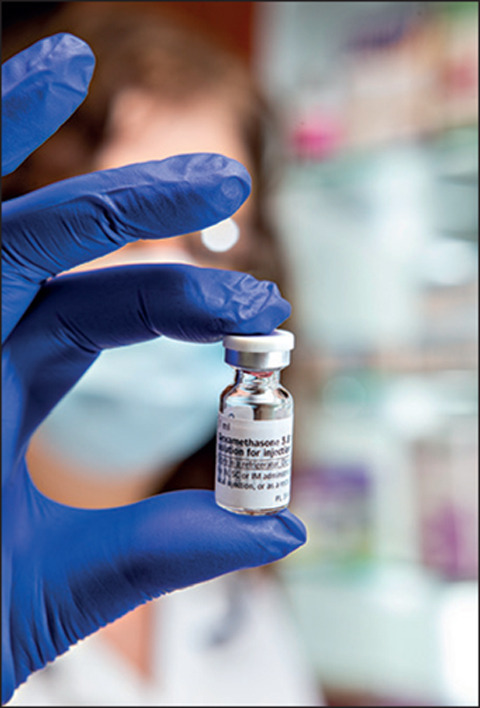
The RECOVERY trial is led by Peter Horby and Martin Landray at Oxford University and involves 176 NHS acute hospitals across the UK. It has thus far recruited more than 12 000 patients. On Sept 14, 2020, the investigators announced plans to evaluate the monoclonal antibody REGN-COV2. The treatment has been specifically designed to target COVID-19. Aside from REGN-COV2, RECOVERY has either evaluated, or is in the process of evaluating, six therapies. “We compared hydroxychloroquine with the standard-of-care for hospitalised patients; it does not work. We compared lopinavir–ritonavir with the standard-of-care; it also does not work. And we compared dexamethasone with the standard-of-care; we found that it works quite well in severely ill patients”, said Landray. He added that all three results went against the orthodoxy.
“Hydroxychloroquine and lopinavir–ritonavir were stipulated either as first-line or second-line treatment in most clinical guidelines, while dexamethasone was mostly not recommended or contraindicated”, said Landray. All of which amply demonstrates the value of pragmatic, randomised trials. “Patients all over the world are receiving drugs to treat severe COVID-19, which are raising false expectations and could even be hazardous; then you have those drugs that may be beneficial, but no one has conclusively proved it, so an awful lot of patients are missing out”, points out Landray.
The USA was slower to establish large-scale clinical trials for COVID-19 than Europe. “We are doing better now”, said Gong. “The National Institutes of Health (NIH) and the scientific community have come together to pool their resources.” The ACTIV initiative is a public–private partnership established by the NIH with the stated aim of developing a “coordinated research strategy for prioritising and speeding development of the most promising treatments and vaccines”. In August, it launched randomised trials to evaluate monoclonal antibody treatments for hospitalised COVID-19 patients as well as patients with mild and moderate disease.
© 2020 TEK IMAGE/Science Photo Library
“One problem we have had in the USA is the kind of mixed messages about COVID-19 that have emerged from social media and news cycles; it has made it more difficult for patients to make decisions about their treatment”, said Gong. “We do not have the kind of unified health-care system that the UK has, and I think the lack of coordination set us back a bit, particularly at the start of the pandemic.”
In early April, 2020, the Chief Medical Officers (CMOs) of England, Scotland, Wales, and Northern Ireland co-authored a letter urging clinicians to enrol COVID-19 patients in national priority clinical trials. “We strongly discourage the use of off-licence treatments outside of a trial, where participation in a trial is possible”, they wrote. Last month, the four CMOs suggested that UK hospitals aim to recruit 60% of eligible patients with COVID-19 into clinical trials. “It is a huge benefit to have a leadership that can send this kind of powerful message to every single hospital in the country”, said Gong. “But the really crucial thing is to have institutions that have a strong willingness to collaborate.”
Landray emphasises the importance of simplification. For the RECOVERY trial, the consent form consists of just two pages of explanation and one page for the signature. “The clinical community and the traditional research community has to forge a partnership. When we planned these trials, we put ourselves in the position of the doctor at the bedside in the middle of a pandemic”, said Landray. “Any barrier to entering a patient had to be completely justified. We wanted to get the trial running as quickly as possible and enrol as many patients as we could.”
Each centre involved in clinical research has to figure out how to accommodate the requirements of infection control. It might be better to have patients provide electronic signatures rather than handling a paper consent form, for example. “You can wipe down an iPad”, notes Gong. At Montefiore Medical Center, hospital-based clinicians have taken care of things like screening and enrolment, while coordinators outside the institution have managed tasks that can be performed remotely, such as data entry and query resolution. The institution had the advantage of a lengthy history of critical care research. “We understand the intricacies and sensitivities involved in working with conditions with high rates of mortality and morbidity”, Gong told The Lancet Respiratory Medicine.
“We need answers we can make use of in the real-world, and that means trials need to be designed pragmatically”, said Rottingen. If investigators involved in large pragmatic trials want to study new drugs, as distinct from repurposed ones, they need more data collection than would normally be possible in such a trial. One option is to combine the pragmatic trial approach with additional data collection. “All the participating centres recruit under the same randomisation protocol, but some of them do the more detailed data collection related to safety and efficacy that will be necessary for regulatory approval”, explains Rottingen. Solidarity and RECOVERY can be conceived of as both single, large-scale, randomised trials and as trial platforms. “The emerging concept is to establish a framework in which both phase 2 and 3 data collection can be done”, concluded Rottingen.
Then there is the question of how to publicise your findings. “It takes time to write your manuscript, go through peer review, and deal with the corrections and revisions”, said Landray. “In a pandemic like this one, when you have thousands of patients presenting to hospitals every week, one in four of whom will die, and there is no information on whether any treatments will save lives, you cannot afford to wait around. You have to get your results into the public domain as rapidly as possible.” The investigators at RECOVERY decided to reveal their findings through press releases. Within 4 h of the publication of the release detailing the results of the dexamethasone trial, the UK CMOs had recommended that the drug be installed as standard-of-care for hospitalised patients. The European Medicines Agency, NIH, and WHO have all followed suit.
Landray believes that the adaptations necessitated by the COVID-19 pandemic should prompt a re-examination of how clinical trials in general are run. He argues for a change in the way investigators approach research. “The methods we are using to deliver answers in RECOVERY are exactly the sort of methods that could answer all kinds of important questions that have nothing to do with COVID-19”, said Landray. “We have ended up with an overly complicated trial system which has lost sight of the one key question: if I give this drug to my patient will he or she do better or worse than if I do not give them the drug?”
© 2020 Lewis Houghton/Science Photo Library