Abstract
PURPOSE
Locally advanced cervical cancer may present with uncontrollable vaginal bleeding in up to 70% of cases. Pelvic vessel embolization has been used as an urgent maneuver for achieving fast hemostatic control. This report describes outcomes of selective pelvic vessel embolization in patients with severe bleeding due to a locally advanced cervical cancer.
METHODS
In this retrospective study, technical aspects, clinical variables, and bleeding-related morbidity were described. The frequency of recurrent disease and the vital status at 1 year of follow-up were determined. Analysis was performed with statistical software R, version 3.6.2. The setting was Instituto Nacional de Cancerología- Bogotá, Colombia, between January 2009 and July 2017.
RESULTS
A total of 47 patients were included. Median age was 44 years (range, 26-70 years). The pre-embolization median hemoglobin level was 7.9 g/dL (range, 5.0-11.3 g/dL). Blood transfusions were administered to 41 women (87.2%). Bleeding control was achieved in 95.7% of cases in the first 24 hours after the embolization. There were no major complications. In 17 cases (36.2%), minor complications were reported; the most common was pelvic pain. In 17.1% of cases, a second embolization was required. After 12 months of follow-up, 27.7% of patients were alive without disease, 44.7% were alive with disease, and 25.5% of them have died of cervical cancer progression.
CONCLUSION
Selective pelvic vessel embolization is a useful alternative in patients with locally advanced cervical cancer and life-threatening bleeding. Its impact on recurrent disease and death due to oncologic cause is not clear.
INTRODUCTION
According to GLOBOCAN 2018, the burden of cervical cancer in Latin America is high, with an incidence of 14.6 and a mortality rate of 7.1 per 100,000 women.1 In Colombia, cervical cancer is the second most frequently occurring gynecologic cancer after breast carcinoma; its annual incidence and mortality are 12.7 and of 5.7 per 100,000 women, respectively.1 At diagnosis, more than two-thirds of patients present with advanced disease (International Federation of Gynecology and Obstetrics [FIGO] 2009 stage IB2-IVA).2 In this scenario, approximately 6% of patients will die of unstoppable cervicovaginal bleeding.3
Context
Key Objective
To determine if emergency embolization of pelvic vessels can be used to treat uncontrollable bleeding in locally advanced cervical cancer.
Knowledge Generated
The success rate of first embolization in bleeding control is 95.7%. Some patients had transient pelvic pain after the procedure (31.9%); no major complications or deaths were reported in this case series.
Relevance
In countries with a high prevalence of cervical cancer and limited resources, as in Latin American countries, arterial embolization is a lifesaving strategy for uncontrollable tumoral bleeding with low morbidity.
Ligation of the hypogastric artery is one method to stop bleeding due to cervical cancer, with a reported 85% decrease in blood flow from the bleeding area.4 However, due to the frequent recurrence of revascularization hemorrhage, it has been shown that hypogastric artery ligation alone is not enough and might require concomitant ligation of the infundibulopelvic, round, and uterosacral ligaments. On the other hand, in these patients, surgical management can add intraoperative or anesthetic complications to the patient’s already critical condition.4
Arterial embolization was brought to our attention as an important tool in the control of massive hemorrhage due to gynecologic neoplasms, because it provides an exact visualization of the bleeding vessel and allows minimally invasive direct therapy to achieve hemostasis. This procedure, compared with surgical ligation, lowers the number of blood transfusions and surgical complications in almost all cases.5,6
At Instituto Nacional de Cancerología, in Bogotá, Colombia, this procedure is offered to patients with cervical cancer and associated vaginal bleeding after conventional vaginal packing has failed and blood transfusion has been required. The objective of this study was to describe the technique and the clinical results of a consecutive series of patients in whom selective embolization of pelvic vessels was used to control massive vaginal bleeding secondary to cervical cancer.
METHODS
Descriptive, retrospective research was conducted including all patients with a confirmed histopathological diagnosis of locally advanced cervical cancer (according to FIGO 2009: IB2, IIA2, IIB, IIIA, IIIB, and IVA), complicated with uncontrolled vaginal bleeding, who underwent embolization of pelvic vessels at the Instituto Nacional de Cancerología during the period from January 2009 to July 2017.
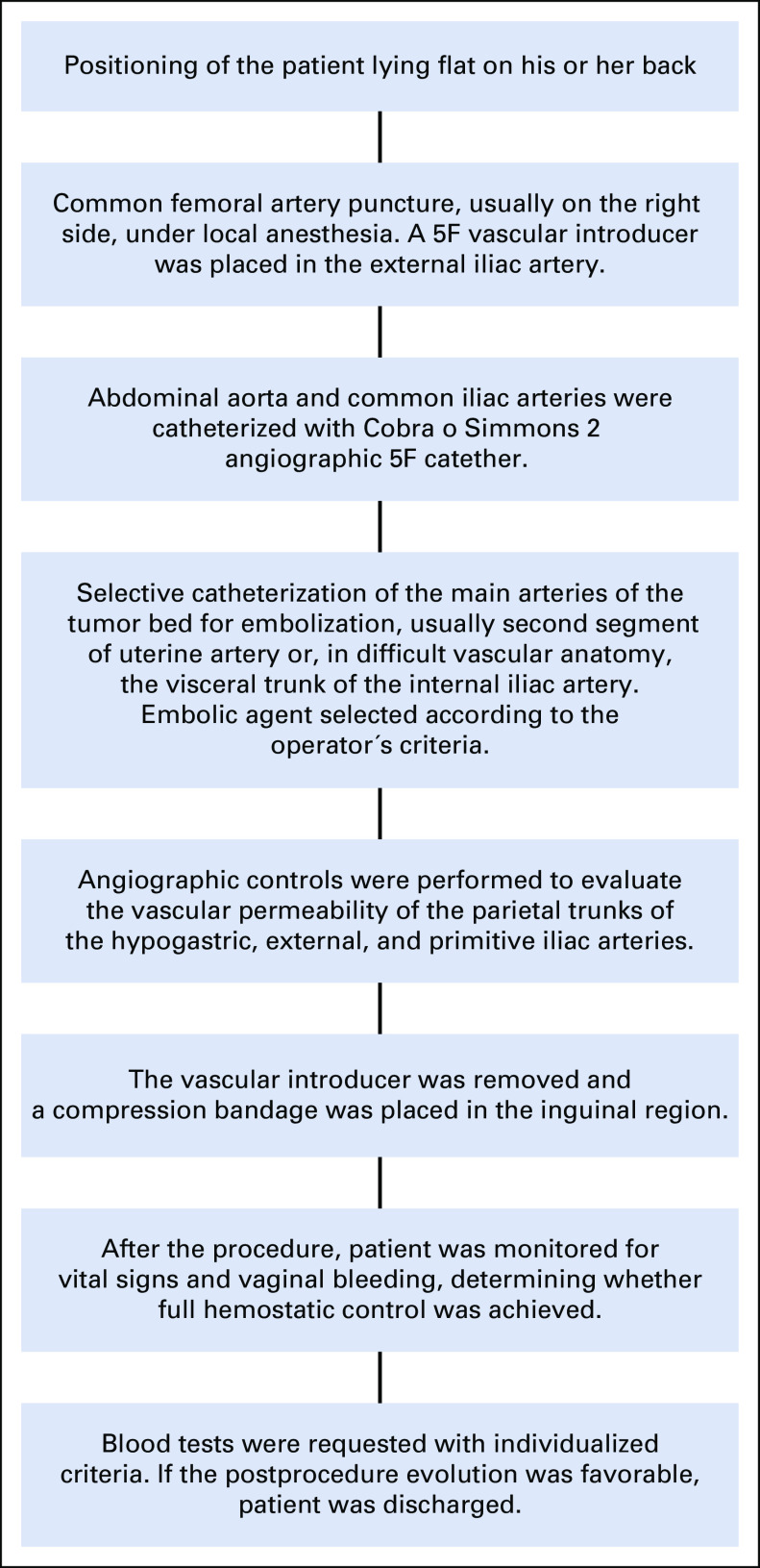
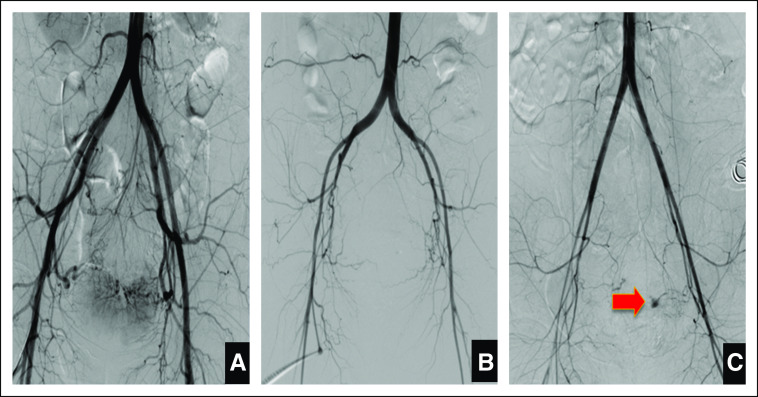
The procedure was conducted in our institution by an expert interventional radiologist, as described in Figure 1. Conventional angiographic acquisitions of the abdominal aorta, aortoiliac bifurcation, and the internal iliac arteries were conducted to evaluate the tumor’s main blood supply and surrounding circulation. We proceeded with selective catheterization of the main tumors arteries to introduce the embolizing agent. Subsequently, angiographic controls were conducted to evaluate the vascular permeability of the posterior hypogastric branches and external and primitive iliac arteries (Fig 2).
FIG 1.
Procedure of embolization of pelvic vessels.
FIG 2.
Aortograms. (A) A moderately vascularized mass is seen in the central pelvic region, with arterial contributions derived from uterine arteries. (B) There is a generalized decrease in the caliber of the pelvic vessels and external iliac arteries, related to hemorrhagic shock in a patient with cervical neoplasia without evidence of active bleeding prior to embolization. (C) Similar to (B), there is a marked decrease in the caliber of all visualized arteries, with contrast accumulation dependent on the left uterine artery. This is a pseudoaneurysm (red arrow) with active bleeding due to tumor infiltration and rupture of the vascular wall.
A review of the medical records was performed by two researchers. The inclusion criterion was selective pelvic vessel embolization due to uncontrollable bleeding cervical cancer leading to secondary anemia (hemoglobin concentration, < 12 g/dL), with clinical signs of orthostatic hypotension. Cases of procedures performed at another institution or patients with incomplete data on the technique and associated morbidity were excluded. The following characteristics of the population were collected: age, FIGO stage, status of cancer treatment at the time of embolization, variables related to hemorrhagic morbidity (eg, preprocedure hemoglobin level, prior bleeding management, need for transfusion, readmission due to bleeding), and the embolization technique (eg, embolizing agent, occluded blood vessel, among others).
Postembolization complications were classified on the basis of the Society of Interventional Radiology Classification System into minor and major complications.7 In addition, status of disease (ie, alive without disease, alive with disease, death) at 12 months was described.
A univariate analysis was conducted. Categorical variables were expressed in absolute numbers or frequencies and percentage. Normal distribution was verified for continuous variables by the Shapiro-Wilk test. The data were then expressed in median and range (difference of minimum and maximum values). R, version 3.6.2, was used for the database analysis. This project was approved by local institutional review board. The informed consent of a patient was obtained for the publication of images; the confidentiality of her data was guaranteed.
RESULTS
A total of 52 patients with locally advanced cervical cancer were scheduled to undergo embolization of pelvic vessels. Four cases in which information about complications related to the procedure was unavailable and one patient who received embolization outside the institution were excluded. For the final analysis, 47 patients were included.
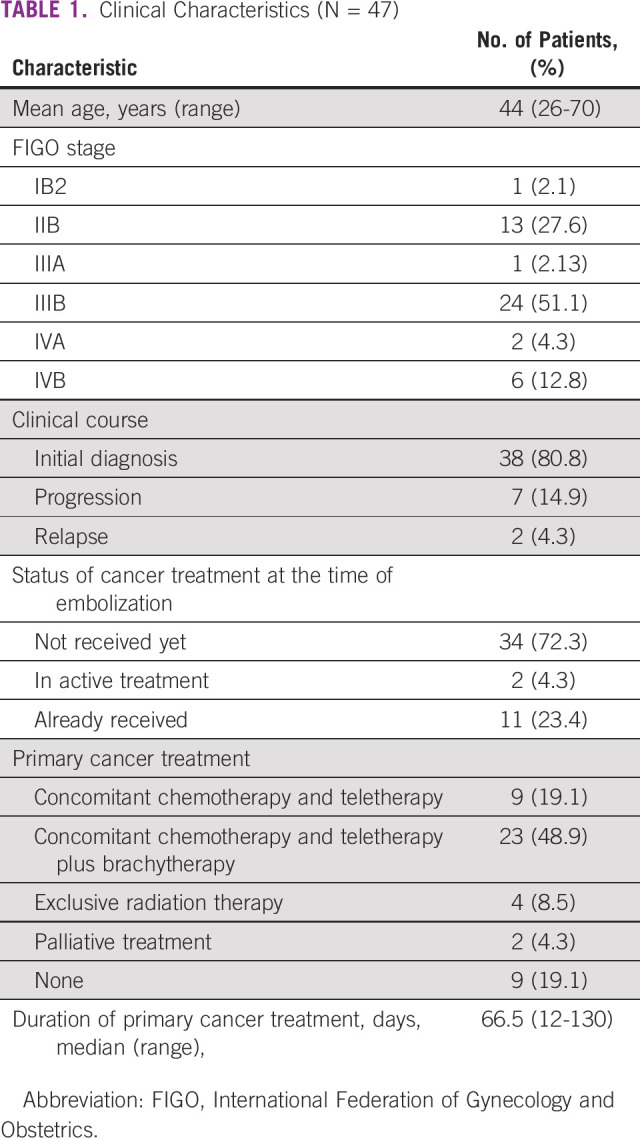
Median age was 44 years (range, 26-70 years). More than half the patients (51.1%) were diagnosed with stage IIIB cancer. The majority of women underwent embolization at the time of initial diagnosis (n = 38; 80.8%), and 34 patients (72.3%) had not started oncologic treatment at embolization. The main prescribed treatment modality in this population was concurrent chemoradiotherapy (Table 1).
TABLE 1.
Clinical Characteristics (N = 47)
All patients’ main complaint was vaginal bleeding. In 37 cases (78.7%), a prior vaginal packing was performed without success. In the remaining 10 cases, primary embolization was indicated because of massive bleeding. Forty-one women (87.2%) received blood transfusions, with a median of 3 units of packed red blood cells (range, 1-8 units). The pretransfusion median hemoglobin level was 7.9 g/dL (range, 5-11.3 g/dL). None of the patients required surgical ligation of hypogastric arteries after embolization.
Uterine artery embolization was performed in 34 cases (72.4%) and hypogastric artery embolization in 13 (27.6%), according to radiologist decision. Forty-two patients (89.3%) underwent bilateral selective and five (10.7%) underwent unilateral selective embolization. The embolic agents used were calibrated particles in 35 cases (74.5%) and other agents in 12 cases (25.5%). These other agents were Spongostan gelatin sponges (Ferrosan, Copenhagen, Denmark) in 5 cases; Gelfoam (Pharmacia & Upjohn Company, New York, NY) in four cases; and Gelfoam (Pharmacia & Upjohn Company, New York, NY) plus silk in three cases.
The bleeding control after embolization was achieved in 95.7% of cases in the first 24 hours. Two patients (4.3%) required new vaginal packaging with hemostatic solution (Monsel’s solution) on the tumor and bleeding control was achieved in both between 24 and 48 hours after the procedure.
There were no major complications related to embolization. In 17 cases (36.1%), minor complications were reported; pelvic pain was the most common complication (31.9% of the total population). One patient had fever, leukocytosis, and nausea, considered to be postembolization syndrome. All patients received opioid analgesics and acetaminophen according to medical criteria, achieving analgesic response in the first 48 hours after the procedure, and were discharged within this period, with the same analgesic treatment (Table 2).
TABLE 2.
Technical Aspects of Embolization and Morbidity (N = 47)
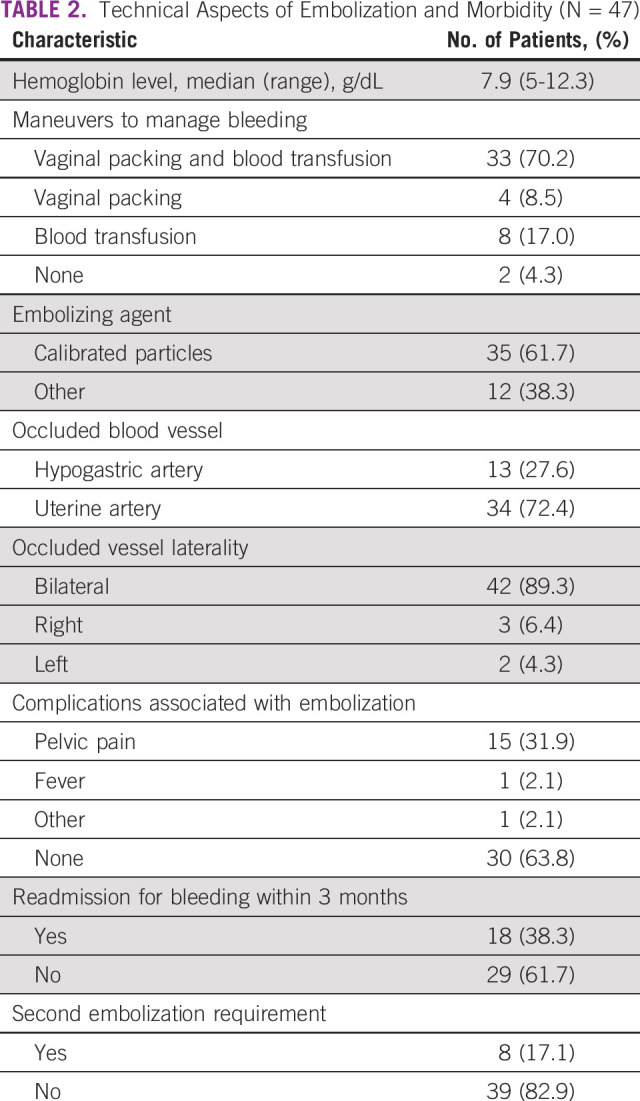
During follow-up, 18 patients (38.3%) had bleeding episodes in the first 3 months after the procedure. Of these, only 8 (17.1%) required a second embolization for uncontrollable bleeding and secondary anemia (median hemoglobin level, 6.7 g/dL; range, 6.2-8.9 g/dL) despite vaginal packing. The median number of transfusions in this group was 2 units of packed red blood cells (range, 1-5 units). There were no major nor minor complications. In all patients, hemostatic control was achieved within the first 24 hours.
Finally, the vital status was described at 12 months- follow-up and showing that 44.7% of the patients were alive with disease (n = 21 cases), 27.6% were alive without disease (n = 13 cases), and 25.5% died of disease (n = 12 cases). Information about oncologic outcome was not retrievable for one patient.
DISCUSSION
We have presented data from 47 cases of pelvic vessel embolization in patients with locally advanced cervical cancer and uncontrollable vaginal bleeding, in whom control was achieved in 95.7% of cases in the first 24 hours, with minor morbidity reported, and no major complications.
Approximately 85% of cases of cervical cancer occur in developing countries. This is especially due to limited access to health services, screening, and treatment of preinvasive lesions.8 In our study, > 70% of our patients had not yet received treatment when they presented with a hemorrhagic episode. The median time in months from initial diagnosis to embolization was 2.5 months (range, 0-40.2 months).
In locally advanced stages of cervical cancer, fragility of tumoral neoformation vessels results in frequent hemorrhagic morbidity. Massive vaginal bleeding in patients with cervical cancer progresses rapidly and could lead to death from hemorrhagic shock in a few hours.9 This complication can be managed with quite simple measures such as vaginal packing and administration of hemoderivatives. When this fails to control hemorrhage, surgical ligation of the hypogastric artery or with arterial embolization are the only remaining alternatives.3 In this series, most patients presented with vaginal bleeding and moderate anemia, and although more than one-third of the patients received blood transfusion and/or vaginal tamponade as initial management, it was necessary to perform a pelvic vessel embolization procedure as additional therapy.
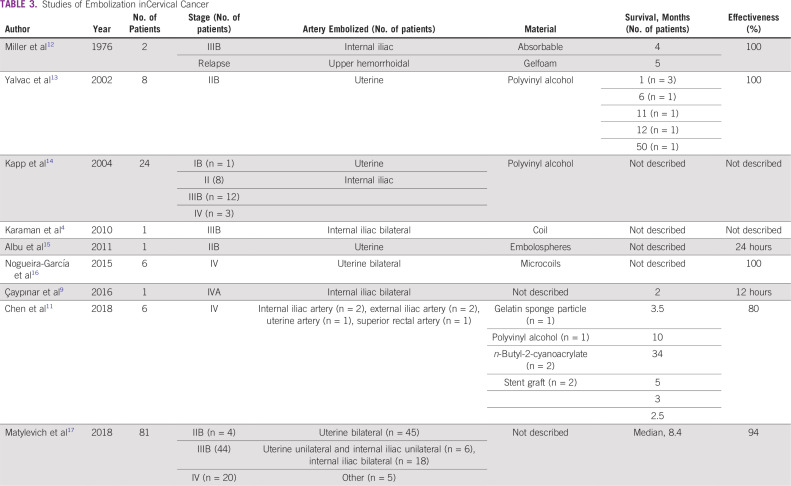
Even though surgical methods have high efficacy in the control of massive bleeding, arterial embolization has become a feasible therapy in untreatable hemorrhage that does not respond to initial management in gynecologic and obstetric conditions involving massive and uncontrollable bleeding.10,11 Its first reported use was in patients with gynecologic malignancies in the mid-1970s; transcatheter arterial embolization of the internal iliac arteries was first described by Ring11a in 1972 and 1973. Miller et al in 197612 performed selective gelatin sponge embolization to control bleeding in two patients with gynecologic cancer. There are multiple studies that have shown the role of selective pelvic-vessels embolization in cervical cancer (Table 3).4,9,11-17
TABLE 3.
Studies of Embolization inCervical Cancer
The procedure is performed if an interventional radiologist is available. The treatment has an efficacy of 69%-100% in the first 24 hours.15 Similarly, bleeding control 24 hours after embolization was successful in 95.7% of patients in our study. The procedure decreases the need for transfusion and the incidence of new bleeding episodes compared with surgical ligation. It also improves the patient’s general condition to continue oncologic therapy.18
Different reports rate overall complication rates for obstetric and gynecologic cases between 6% and 9%.19 Complications described are related to the angiographic procedure (eg, groin puncture site hematoma, catheter-induced vessel dissection, contrast medium–associated allergy or nephrotoxic effect) and complications secondary to embolization such as postembolization syndrome (ie, pain, fever, nausea, and leukocytosis) in up to 50% of patients. Other infrequent complications are uterine, bladder, or rectal necrosis; abscess and sepsis; ischemia of adjacent tissue; and sexual dysfunction.20 No major complications were reported in our patients. Minor complications were reported in 17 women. The risks of such complications are reduced by knowledge of the vascular anatomy and meticulous attention to embolization technique.
Finally, an interesting aspect that has been discussed is the oncologic outcome of this procedure. The role of tumor oxygenation and its impact on treatment is well known. Tumor hypoxia is an adverse factor in this neoplasm and is related to poor outcome regardless of management modality.21
In addition, tumor hypoxia has also been observed to promote genetic changes associated with metastatic disease. Embolization could be related to a state of chronic hypoxia by occluding the main vessels supplying the tumor and, thus, its sensitivity to kill cells could be affected.22 In our study, 34 patients (72.3%) had not received oncologic treatment at the time of embolization. They had been recommended to undergo embolization before a massive vaginal bleeding that put their life at risk. Because of the type of study, the oncologic impact of the procedure is unknown. However, Kapp et al14 evaluated 24 patients with cervical cancer who underwent bilateral embolization before definitive radiotherapy compared with 230 patients who did not undergo embolization. With a median follow-up of 49.5 months, the authors reported a trend toward poorer disease-specific survival and pelvic control in patients who had undergone embolization, even though no impact on radiocurability could be demonstrated in multivariate analysis after controlling for the major tumor characteristics and hemoglobin level during the treatment.14 Additional evidence on this aspect is necessary.
A strength of this study is that, to our knowledge, it is the largest published series about pelvic vessels embolization in locally advanced cervical cancer in Latin America. Taking into account that cervical cancer is a high-prevalence disease in countries with low resources, it can be proposed as a lifesaving strategy for uncontrollable vaginal bleeding with less morbidity compared with traditional surgical treatment. Among the study limitations, we can mention the low number of patients included, the retrospective nature of the study, a heterogeneous population with different stages of the disease, the lack of evaluation of the oncologic impact of the procedure, and its external validity, because not all the cancer centers in developing countries have an interventional radiology service.
Cancer control needs not only the integration of prevention, screening, and a high-quality diagnosis and treatment structure but also the full range of other services, including rehabilitation, survivorship, and palliative care.23 Selective pelvic-vessel embolization as a hemostatic strategy in this study was a useful tool in patients with locally advanced cervical cancer with life-threatening bleeding. Embolization achieved adequate early hemostatic control in most patients with low morbidity and no deaths. The methodology used in this study did not allow us to determine the oncologic impact of this technique.
AUTHOR CONTRIBUTIONS
Conception and design: Julián Beltrán, Abel Merchán, Jorge Egurrola, Fernando Heredia, René Pareja
Administrative support: René Pareja
Provision of study material or patients: Julián Beltrán, Abel Merchán, Jorge Egurrola
Collection and assembly of data: Adriana Alméciga, Juliana Rodriguez, Julián Beltrán, Abel Merchán, Javier Burbano, Fernando Heredia
Data analysis and interpretation: James Sáenz, Jorge Egurrola, Lina Trujillo, Fernando Heredia
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/site/misc/authors.html.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Juliana Rodriguez
Honoraria: Johnson & Johnson
Travel, Accommodations, Expenses: AstraZeneca
Abel Merchán
Travel, Accommodations, Expenses: AstraZeneca, Johnson & Johnson
No other potential conflicts of interest were reported.
REFERENCES
- 1. doi: 10.3322/caac.21492. Bray F, Ferlay J, Soerjomataram I, et al: Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394-424, 2018 [Erratum: CA Cancer J Clin 70:313, 2020] [DOI] [PubMed] [Google Scholar]
- 2.Shrivastava S, Mahantshetty U, Engineer R, et al. Treatment and outcome in cancer cervix patients treated between 1979 and 1994: A single institutional experience. J Cancer Res Ther. 2013;9:672–679. doi: 10.4103/0973-1482.126480. [DOI] [PubMed] [Google Scholar]
- 3. Eleje GU, Eke AC, Igberase GO, et al: Palliative interventions for controlling vaginal bleeding in advanced cervical cancer. Cochrane Database Syst Rev 3:CD011000, 2019. [DOI] [PMC free article] [PubMed]
- 4.Karaman B, Oren NC, Andic C, et al. Transcatheter embolization for the treatment of both vaginal and lower intestinal bleeding due to advanced pelvic malignancy. Eurasian J Med. 2010;42:153–156. doi: 10.5152/eajm.2010.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pisco JM, Martins JM, Correia MG. Internal iliac artery: Embolization to control hemorrhage from pelvic neoplasms. Radiology. 1989;172:337–339. doi: 10.1148/radiology.172.2.2748811. [DOI] [PubMed] [Google Scholar]
- 6.Yamashita Y, Harada M, Yamamoto H, et al. Transcatheter arterial embolization of obstetric and gynaecological bleeding: Efficacy and clinical outcome. Br J Radiol. 1994;67:530–534. doi: 10.1259/0007-1285-67-798-530. [DOI] [PubMed] [Google Scholar]
- 7.Sacks D, McClenny TE, Cardella JF, et al. Society of Interventional Radiology clinical practice guidelines. J Vasc Interv Radiol. 2003;14:S199–S202. doi: 10.1097/01.rvi.0000094584.83406.3e. [DOI] [PubMed] [Google Scholar]
- 8.Murillo R, Herrero R, Sierra MS, et al. Cervical cancer in Central and South America: Burden of disease and status of disease control. Cancer Epidemiol. 2016;44(suppl 1):S121–S130. doi: 10.1016/j.canep.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 9.Çaypınar SS, Güraslan H, Şentürk B, et al. Salvage therapy in acute life-threatening vaginal bleeding of cervical cancer: Hypogastric artery embolization. Taiwan J Obstet Gynecol. 2016;55:607–608. doi: 10.1016/j.tjog.2015.01.005. [DOI] [PubMed] [Google Scholar]
- 10.Wu CC, Lee MH. Transcatheter arterial embolotherapy: A therapeutic alternative in obstetrics and gynecologic emergencies. Semin Intervent Radiol. 2006;23:240–248. doi: 10.1055/s-2006-948761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen CS, Park S, Shin JH, et al. Endovascular treatment for the control of active vaginal bleeding from uterine cervical cancer treated with radiotherapy. Acta Radiol. 2018;59:1336–1342. doi: 10.1177/0284185118758133. [DOI] [PubMed] [Google Scholar]
- 11a.Ring EJ, Athanasoulis C, Waltman AC, et al. Arteriographic management of hemorrhage following pelvic fracture. Radiology. 1973;109:65–70. doi: 10.1148/109.1.65. [DOI] [PubMed] [Google Scholar]
- 12.Miller FJ, Jr, Mortel R, Mann WJ, et al. Selective arterial embolization for control of hemorrhage in pelvic malignancy: Femoral and brachial catheter approaches. AJR Am J Roentgenol. 1976;126:1028–1032. doi: 10.2214/ajr.126.5.1028. [DOI] [PubMed] [Google Scholar]
- 13.Yalvac S, Kayikcioglu F, Boran N, et al. Embolization of uterine artery in terminal stage cervical cancers. Cancer Invest. 2002;20:754–758. doi: 10.1081/cnv-120003543. [DOI] [PubMed] [Google Scholar]
- 14.Kapp KS, Poschauko J, Tauss J, et al. Analysis of the prognostic impact of tumor embolization before definitive radiotherapy for cervical carcinoma. Int J Radiat Oncol Biol Phys. 2005;62:1399–1404. doi: 10.1016/j.ijrobp.2004.12.037. [DOI] [PubMed] [Google Scholar]
- 15.Albu S, Grigoriu C, Vasiliu C, et al. The role of uterine artery embolization in cervical cancer - single case report. Maedica (Buchar) 2011;6:137–140. [PMC free article] [PubMed] [Google Scholar]
- 16.Nogueira-García J, Moreno-Selva R, Ruiz-Sánchez ME, et al. Uterine artery embolization as palliative treatment in cervical cancer. Ginecol Obstet Mex. 2015;83:289–293. [Article in Spanish] [PubMed] [Google Scholar]
- 17.Matylevich OP, Akinfeev VV, Randall TC, et al. The Belarus experience of pelvic artery embolisation in patients with advanced and recurrent cervical cancer presenting with haemorrhage. Eur Oncol Haematol. 2018;14:45. [Google Scholar]
- 18.Field K, Ryan MJ, Saadeh FA, et al. Selective arterial embolisation for intractable vaginal haemorrhage in genital tract malignancies. Eur J Gynaecol Oncol. 2016;37:736–740. [PubMed] [Google Scholar]
- 19.Carrillo TC. Uterine artery embolization in the management of symptomatic uterine fibroids: An overview of complications and follow-up. Semin Intervent Radiol. 2008;25:378–386. doi: 10.1055/s-0028-1102997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Katz MD, Sugay SB, Walker DK, et al. Beyond hemostasis: Spectrum of gynecologic and obstetric indications for transcatheter embolization. Radiographics. 2012;32:1713–1731. doi: 10.1148/rg.326125524. [DOI] [PubMed] [Google Scholar]
- 21.Lyng H, Malinen E. Hypoxia in cervical cancer: From biology to imaging. Clin Transl Imaging. 2017;5:373–388. doi: 10.1007/s40336-017-0238-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murland SL. Tumour oxygenation: The importance of hypoxia, anemia, and angiogenesis in radiation therapy. Can J Med Radiat Technol. 2005;36:21–33. [Google Scholar]
- 23.Strasser-Weippl K, Chavarri-Guerra Y, Villarreal-Garza C, et al. Progress and remaining challenges for cancer control in Latin America and the Caribbean. Lancet Oncol. 2015;16:1405–1438. doi: 10.1016/S1470-2045(15)00218-1. [DOI] [PubMed] [Google Scholar]