Abstract
Objective
Human papilloma virus (HPV) preventive measures are underutilized globally; consequently, international university students (IUS) are at increased risk for HPV infection and sequelae (e.g., cancer). The study aim was to explore IS HPV knowledge and preventive behaviors.
Participants
81 undergraduate and graduate IUS at a southeastern university.
Methods
Exploratory sequential mixed methods guided by the Health Belief Model.
Results
Integrated qualitative/quantitative data revealed four themes mapped to relevant HBM constructs: Perceived susceptibility to HPV; Perceived benefits/Perceived barriers to HPV prevention; Cues to Action; and Likelihood of Engaging in Health-Promoting Behavior. Over half could identify intercourse as a primary transmission mode yet believed they were not at risk for HPV/sequelae. Only a quarter had received any dose of HPV vaccine and/or a Pap smear.
Conclusions
IUS students represent an important catch-up population for HPV vaccination and screening. Results can be used to design and tailor interventions for this vulnerable population.
Keywords: Human Papilloma Virus, Cancers, Knowledge, Prevention, Behaviors
Introduction
International university students (IUS), comprising nearly 4% of total US undergraduate- and graduate-level enrollment, are at particular risk for contracting Human Papilloma Virus (HPV). While HPV is a group of over 200 related viruses, in common usage the term HPV refers to sexually transmitted infections (STIs) caused by select, high-risk strains of HPV.1 Fourteen million people are newly infected annually, making HPV the most common STI in the United States (US).2, 3 In fact, HPV is so common that most sexually active men and women will be infected with at least one type at some point in their lives. HPV is also responsible for serious sequelae. It is the primary causative organism in cancers of the anus and cervix (90%), vagina and vulva (70%), penis (60%), and oropharynx (70%).4, 5 Approximately 39,800 HPV-associated cancers occur in the US annually; women are 1.4 times more likely to be diagnosed as compared to men.6
The risk for HPV-associated cancers can be reduced significantly through appropriate screening (e.g., Papanicolaou test, also known as a Pap smear) and HPV vaccination (in the US, Gardasil®9), which protects against HPV types commonly associated with disease.7 The World Health Organization (WHO) and US Food and Drug Administration (FDA) recommends HPV vaccines for boys and girls aged 9 through 26, as approximately 50% of all new HPV infections are among youth between the ages of 15 and 24.7, 8 HPV vaccines have been found to provide up to 100% protection against some HPV types that can cause cancer,7, 9, 10 yet uptake of the vaccine in the US has been slow. While improving, recent estimates indicate half of US adolescents are not fully immunized against HPV;11 vaccination rates amongst US university students have also been suboptimal, especially for males.12 This is, in part, due to 1) limited understanding regarding HPV infection and sequelae; 2) an underestimation of personal risk; and 3) lack of knowledge about protective practices and behaviors.13
In addition to these factors, IUS entering the US university system have specific challenges that increase their risk of HPV infection. For example, it is likely the experiences of culture shock, language difficulties, poor social integration, and the absence of family and friends may result in feelings of isolation associated with increased engagement in sexual behaviors, elevating the risk of HPV exposure.15, 16 While previous studies have demonstrated lower levels of HPV awareness and knowledge among college students in other countries,17, 18 little work has evaluated the experiences of IUS in the US. A better understanding of these experiences will facilitate the development of culturally appropriate interventions designed to increase HPV knowledge and uptake of preventive measures.
Purpose
Preventive and detective measures have improved HPV-related cancer morbidity and mortality. However, knowledge regarding these topics remains limited among specific population groups, increasing the risk of infection and long-term sequelae. The purpose of this study was to engage with IUS to 1) examine knowledge of HPV and its associated sequelae; and 2) explore attitudes toward preventive practices.
Theoretical Framework
This theory-driven study was guided by the Health Belief Model (HBM). It posits individuals will engage in preventive health behavior if they 1) believe themselves threatened by an illness or condition; and 2) believe that the benefits of taking preventive action outweigh the barriers to or costs of said action.19 Relevant study concepts include perceived susceptibility, perceived benefits/barriers, and cues to action, resulting in likelihood of engaging in health-promoting behaviors. The HBM is one of the most widely used frameworks for explaining and predicting health-related behaviors, including in the context of HPV.20–22
Methods
Study design and instrumentation
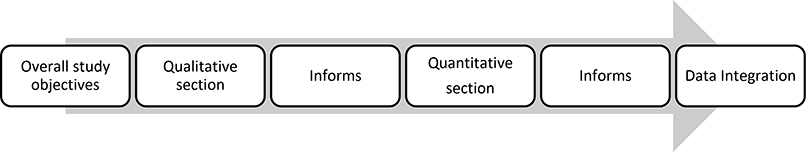
This study used a mixed-method, exploratory sequential design (Figure 1); reporting of study conduct was guided by the HBM and Mixed Methods Appraisal Tool to ensure rigor, accuracy, and transparency.23 Data included semi-structured interviews, focus group discussions, and quantitative surveys.
Figure 1:
Exploratory Sequential Mixed Methods Study Design
Interview and focus group guides were developed by FIRST AUTHOR, a female Nigerian nurse researcher and former US IUS, using information from the Cervical Cancer Free Coalition National Surveys and Health Information National Trends Survey.24, 25 The guides included open-ended questions (e.g., What do you know about Human Papilloma Virus? Tell me about cervical cancer.) as well as exploratory probes to encourage more detailed reflection. After conducting the initial 5 interviews and one focus group, the first two authors made minor edits (e.g., addition of new probes, reordering questions) to the interview and focus group guides prior to conducting the remaining interviews and focus group. The quantitative survey was then developed and refined using concepts gleaned from the qualitative interviews and focus groups. It included 42 questions divided into four sections: 1) participant demographics; 2) specific knowledge regarding HPV, associated cancers, and preventive measures; 3) attitudes toward these same topics; and 4) preventive measures practice. Rigor of the qualitative questions and face validity of the survey were confirmed by SECOND AUTHOR, a pediatric nurse practitioner and researcher with a background in pediatric primary care delivery (including HPV preventive services) and the conduct of qualitative and mixed-methods studies. THIRD AUTHOR, a nurse researcher, contributed expertise in qualitative data analysis, integration of quantitative and qualitative data, and interpretation of results.
Study setting and sampling
The study setting was a public R1 research university located in the southeast US. Of the approximately 34,000 students located on the main campus, there were approximately 1800 IUS at the time of study conduct. Inclusion criteria included participants who: 1) were 18 years or older; 2) self-reported as an IUS; and 3) had spent at least a semester in the US. University IRB approval was obtained prior to initiating any study activities.
Participant recruitment and data collection
Qualitative phase
Participants were recruited from various IUS groups and via snowballing. The study purpose was explained to potential participants and written consent was obtained prior to data collection. Participants could choose participation in a focus group or to be interviewed one-on-one. Interviews and focus group discussions were audiotaped, with interviews lasting between 17 and 55 minutes and focus groups between 1 to 2 hours. Afterward, all participants completed a demographic questionnaire containing information about their age, sex, country of citizenship, length of stay in the US, program of study, level of study, and years in the program. To maintain confidentiality, the participants were identified by the research identification number.
Quantitative phase
Participants for this phase were solicited through internet-based sites, including the international student bimonthly newsletter, the international student Facebook site, and IUS associations and countries sites. Survey data were collected and managed using Research Electronic Data Capture (REDCap), a secure, web-based application designed for research studies.26 Students who opted to participate clicked on an embedded REDCap link; no identifying information was collected beyond demographics detailed in the qualitative phase description.
Data analysis
To enhance rigor and encourage reflexivity, the authors conferred regularly to discuss how their professional backgrounds and personal experiences influenced all phases of the research, including data collection, analysis, interpretation, and integration of results.
Qualitative data analysis
NVivo software was used for qualitative data management. Analysis was accomplished using Braun and Clarke’s six-step Thematic Analysis approach.27 The data analysis process began with the transcription of six interviews by the first author. After comparison with audio recording to ensure fidelity, these transcripts were read by the first two authors several times to familiarize themselves with the data. They then met to discuss initial thoughts, assumptions, and understandings of key concepts, and to flesh out initial codes. The coding schema developed from this exercise was then used to code the remaining transcribed interview and focus group data; these codes were then collapsed into categories, then emergent themes. They met again to reconcile the minor differences in interpretation and finalize and name the themes.
Quantitative data analysis and data integration
Quantitative data were analyzed using SAS software version 9.4. Basic descriptive statistics (e.g., frequency, percentages, and means) were generated to describe participant demographics, knowledge, attitude toward, and uptake of HPV preventive measures. After iterative readings of the qualitative data, all authors considered the relevance of the theoretical framework constructs with the finalized themes, discussed the relationships between the themes and how they informed the quantitative results, and determined how to best integrate and report results for enhanced understanding.
Results
A total of 81 IUS from 12 countries (China, Ghana, South Korea, India, Senegal, United Arab Emirates, Nigeria, Lesotho, Saudi Arabia, Sri Lanka, Vietnam, and Somalia) took part in the study. Twenty-seven consented to participate in the exploratory qualitative phase; of these, 17 were interviewed one-on-one and 10 took part in the two focus group discussions (3 and 7 persons per group). Fifty-four IUS completed the online survey. Demographic characteristics of all participants are shown in Table 1. Themes are organized by HBM theoretical constructs;19 quantitative results are integrated within discussion of each theme. All qualitative participant names are pseudonyms.
Table 1.
Demographic Characteristics of the Quantitative Survey and Qualitative Samples
| Online Survey Sample (N=54) | Interview and Focus Group Sample (N=27) | |
|---|---|---|
|
|
||
| Mean or Percentage (%) | Mean or Percentage (%) | |
| Age | 28.4 | 27.8 |
| Sex | ||
| Female | 35 (64.8%) | 14 (51.9%) |
| Male | 19 (35.2%) | 13 (48.2%) |
| Number of years in US | 2.54 | 3.18 |
| Level of study | ||
| Undergraduate | 12 (22.2%) | 6 (22.2%) |
| Graduate | 42 (77.8%) | 21 (77.8%) |
“I think is quite hard for me to get it”: Perceived susceptibility to HPV
Over two-thirds (36/54) of the survey participants had heard of HPV infection, with 62% correctly identifying sexual intercourse as a primary mode of transmission. However, very few qualitative participants could correctly identify behaviors associated with an increased risk of contracting HPV, such as having multiple sex partners (5/27, 19%) or having sex without condom (4/27, 15%).
Most survey participants (38/54, 70%) perceived they were not at risk for contracting HPV or believed that they were not at risk of developing any HPV-related cancers (39/54, 74%). Qualitative participants provided several reasons to support why they believed that they were not at risk for HPV and HPV related cancers, including being in monogamous relationships, having a healthy lifestyle (eating fruits and vegetables, exercising and personal hygiene), having no family history of cancer, and the perceived rarity of HPV-related cancer. Zhang, a 21-year-old Chinese male noted, “I don’t think I have a chance to get it because my lifestyle is very healthy…. I eat very healthy, less junk food, and I exercise and I have a good mood...I think is quite hard for me to get it.” Achila, a 26 year old female from Sri Lanka added, “I don’t think I have any chance of getting the virus…I know I don’t have the infection and I only have one sexual relationship with my husband.”
A few of the qualitative participants (4/27, 15%) shared that the belief in their home countries is that you cannot be at risk of any disease that has not occurred in your family. Krish, a 30-year-old Indian male stated, “I am not at risk because the cancers you mentioned are not very usual cancers that I have heard…I don’t think there is anybody around me that have had cancer, so compared to others disease like heart disease or diabetics.”
Several qualitative participants (6/27, 22%) relayed beliefs about perceived vulnerability to HPV infections based on sexual orientation or gender. For example, Dino, a 40 year-old female from Lesotho felt HPV-related cancer was only a concern for homosexuals and risk did not pertain to her, as she was heterosexual: “People that I know that have died of anal cancer are from the gay community.” Male participants in particular considered HPV to be a “more dangerous” problem for women:
I still don’t know if it affects both men and women, so I don’t know my chances of getting it. If is a woman thing, obviously, my chances are zero. But if it affects both men and women, my chances are low. (Saeed, 21 year-old United Arabian Male)
and prevention their responsibility:
They have talked about being hygienic…females generally should be able to take care of themselves down there, at the cervix, should be able to ensure that all these things are at least being prevented. (Emy, 28 year-old Nigerian male)
Some qualitative participants (5/27, 18.5%) stated that the risk of contracting HPV was increased by living in the United States; these reasons included beliefs that HPV was more common in the US, US culture promotes HPV infection, or environment or food could be an exposure risk. A particular concern was that public spaces might harbor the virus:
It is likely for people to get HPV because we don’t see it…We go to our departments, to public places to use the bathrooms. We don’t even know what we can pick from there, so anytime you use the bathroom, you may pick something. (Wang, 23, Chinese male).
Another participant corroborated:
The chances are very high. Anyone can get it. You can get from the hospital, from the street, from the bank. You can be outside, [a] mosquito will strike you and transfer the disease from [an] animal or from another person to you…I think we should try to be in clean environment. (Ahmad, 41, Saudi male).
“The earlier you know, the better your chances”: Perceived benefits/Perceived barriers to HPV prevention
Even though a large number (20/27, 74.1%) of participants lacked HPV knowledge and held erroneous beliefs regarding susceptibility, they understood the benefits of preventative behaviors. Long, a 29 year-old Vietnamese female noted:
It is important for people to know about how to prevent themselves from getting exposure to cancer. I think the most important one is the fact that people should know when things are going wrong with their bodies. Like breast cancer for example, the earlier you know, the better your chances. All these cancers generally, the earlier you know, the better your chances. So is better to go for check up to find out on time.
Mei, a 29 year-old Chinese female added:
I believe is very effective [HPV vaccine] and if it can prevent a certain type of cancer, why should we not do it, I mean, everyone should do it especially for underdeveloped countries or those countries that have lack of information.
However, 7 qualitative participants related specific barriers to accessing appropriate preventive care, including fear of the disease, stigma against sexually transmitted infection, and shyness. Khan, a 27-year-old Indian male related: “You know HPV is sexually transmitted, and clearly nobody wants other people to know that they have STD because of the stigma. So, I think the stigma will make people not to want to know.”
Another frequently encountered barrier was navigating a new health care system, which often differed greatly from their countries of origin. For example, for some qualitative participants (10/27, 37%) the need to book an appointment before seeing a provider was not readily understood, as in their home countries health care providers operate on a walk-in basis. Yang, a 20-year-old male from China observed:
You just go to the hospital and tell the staff that you want to see the doctor, although you may have to wait for several hours before you can see the doctor that day.
Knowing who needed preventive services, and where to access them, were other common challenges. While almost all the survey participants had heard of HPV vaccines (38/53, 71.7%) very few had an understanding of vaccine specifics. Only four qualitative participants were able to specify the recommended age range for HPV vaccination, while majority said it is for children. One 28-year-old Chinese female participant stated, “Actually, I am considering to take HPV vaccine…I don’t know for sure because I am already above the age for taking the vaccine”. Only 11 (20%) survey participants knew that the vaccine is recommended for both males and females. In regard to where to obtain screening, Subira, a 27-year old Indian female was unsure:
I don’t think I can do pap smear anywhere because is for cancer, is probably gonna be in some really good and big hospital. I don’t think you can do it at the health center. Yea, I don’t know.
Cost was another barrier. For HPV preventive services, almost 30% of the survey participants believed the vaccine (16/54) and pap smear (11/54) to be cost prohibitive. Most qualitative participants (23/27, 85.2%) felt US health services were very expensive and insurance did not relieve the financial burden. Yang, a 28-year-old Chinese female agreed:
I go to the hospital when sick but to be honest, I never go to the clinic because the bill is very expensive.
And not knowing the cost of services before accessing them was perceived as problematic and dishonest:
When you go to the hospital, you don’t have an idea of what you will be paying. Even though they tell you that when your bill comes, your insurance will cover the illness or some of the treatment. But when you get the bill, the number don’t add up correctly to me…People like to say numbers don’t lie, but eeeee, numbers lie in US…For me, I avoid going to hospital. (Ahmed, 26, Somalian male).
Conversely, when participants understood their insurance benefits, they felt they would be able to access preventive services; over half of the qualitative participants (14/27, 51.8%) noted that they would take up preventive measures if their insurance fully covered the cost. Kwole, a 35-year-old Senegalese female stated:
I will like to take both the vaccine and the pap smear, if my insurance will cover it completely. And I also most think international students will want to take HPV vaccine and pap smear, if their insurance covers the full cost.
“The nurse sat me down”: Cues to Action
Only a few qualitative participants (4/27, 15%) participants noted that physical symptoms – “feeling sick” - would motivate them to take up preventive measures. Main cues to action identified included health provider’s recommendation, education about HPV risks and prevention, and institutional mandates. Among the survey participants, over 70% stated they would receive HPV vaccine or Pap smear based on a provider’s recommendation. Helen, a 30-year-old Ghanaian female elaborated:
If a nurse should tell me that is time for me to do it, I will do the test. If you give me information about the test, I will just keep the information. Maybe when I go for another check-up, like the way I did in the UK and the nurse persuaded me, she stressed that I should do it. Definitely, I will go.
Participants wanted more HPV information, stating more education would motivate them to take up preventive measures. Among the survey participants, over 40% said they would receive HPV vaccine and Pap smear with more education on HPV and cervical cancer. Sally, a 26-year-old Sri Lankan female related:
If the student knows about the virus…If they have the picture in their head, I mean if they have that clear idea in their head, they will go for the vaccine and pap smear.
Three out of the four qualitative participants who had actually received the vaccine specifically stated that they thought the vaccine was compulsory, since it was on the University IS immunization. A similar pattern was noted with Pap smear screening. Only three of the thirteen female qualitative participants had received a Pap smear; they were required to do so as part of prenatal care.
“Prevention is better than cure”: Likelihood of Engaging in Health-Promoting Behavior
As noted previously, the majority of qualitative participants expressed willingness to be vaccinated (19/27, 70%) and belief it would protect them against HPV and its associated cancers. However, over 70% of all study participants – both qualitative and quantitative - had not received the HPV vaccine. Some qualitative participants alluded to God’s will as a mitigating factor in their intention to seek preventive services. One participant stated, “That is the life. You do not know what God prepares for you. Personally, I will be happy in both cases because, God will give me the health; God will give me the disease.”
Many quantitative participants attributed noncompliance to cost (16/54, 30%) and not knowing about the vaccine (10/54, 18%); however, several gave no reason for not being immunized (13/54, 24%). Of the quantitative participants (14/54, 26%) who had received HPV vaccine, 9 received the vaccine in their home country, 4 in the US, and 1 could not remember. Of these, six received the complete three-dose series, 4 received two doses, and one received one. For the qualitative participants, only 4 of the 27 had received at least one dose of the HPV vaccine; 3 received the vaccine in their home country and 1 in the US. Only one completed all three doses of the vaccine. A similar pattern was noted regarding Pap smear screening, with only three of the thirteen female qualitative participants ever having receive a Pap smear. Among female quantitative participants, 68.5% had never had a Pap smear, with 40.0% not providing any reason for not screening and 22.8% not knowing about the Pap smear.
Discussion
A heightened and appropriate sense of vulnerability to HPV and its sequelae is critical for effective IUS sexual health promotion and cancer prevention; however, these participants overwhelmingly reported they were not at risk for contracting HPV, nor were they concerned about developing any HPV-related cancers. Individuals who do not perceive that they are vulnerable may have a false sense of safety, which in turn may lead to more risky sexual behaviors.12 While it was encouraging some participants perceived that they were vulnerable to HPV infection and cancers, the narratives demonstrated they lacked evidence-based knowledge regarding HPV risk factors. For example, participants talked about contracting HPV from food exposed to HPV and use of public toilet, others that HPV sequelae were dependent on sexual orientation. These erroneous beliefs contributed to both over- and under-estimation of their HPV risk.
Results also demonstrated gendered differences regarding HPV risk and preventive practices. Given that the spotlight has been on female-specific HPV-related disease (e.g., cervical cancer), more publicity focused on male-specific HPV-related disease is needed to increase awareness of male vulnerability to HPV and sequelae. Public health messaging should emphasize that both genders are equally susceptible to HPV infection.29 Preventive measures should include instructions on the use of both male (e.g. condoms) and female-controlled preventive measures (e.g. female condoms)30 to allow individuals to take charge of their sexual health.
Similar to fatalism findings amongst African Americans, some participants felt that HPV and the development of cancer to be inevitable, which may explain in part the low degree of HPV preventive measures uptake. Health care provider strategies could include incorporating culturally specific information on cancer prevention, treatment, and outcomes and addressing erroneous beliefs about risk.31
While IUS may encounter similar barriers identified in other studies among college students,32–34 understanding IUS specific barriers is important for clinicians when designing HPV interventions for this population. Barriers to HPV vaccination and Pap smear uptake among this group included lack of understanding about the US health care system, as well as time constraints. Many colleges have campus clinics available on-site, improving the convenience of health care for students.33 However, convenience does not guarantee access. Access is a complex issue and facilitating health care access should focus on helping people to negotiate and utilize health care resources appropriately in order to preserve or improve their health.35 Additionally, if the main reason for being in the US is to complete an educational program in a timely fashion, IUS may not prioritize the need for preventive health services, especially if they lack understanding of their risks. However, the most salient barrier for these study participants was cost. Even though IUS are required to have health insurance, students who have health insurance without vaccine coverage may need to pay some out-of-pocket costs to be vaccinated at college health centers. With the cost ranging from $130 to $170 per dose (not including administration charges), the 3-dose HPV series is one of the most expensive vaccines;36 effective HPV programs will address this primary barrier, at it is not unique to IUS.
Similar to reports from other studies,32,33 these IUS said health care providers’ recommendations were an important influence on HPV preventive measures decision-making. University and college campus clinics have a role to play in providing targeted sexual education to reduce IUS risky behaviors. There is also opportunity to provide catch-up vaccination for under-immunized, age-eligible international students to protect both the short and long-term health of this population.37 A pilot study to improve HPV vaccination for college-aged males at a student health center in Utah found that providers reported missed opportunities for recommending the HPV vaccine during routine patient encounters.37 Future interventions should target university and college health center health care providers, raising their awareness of the need to recommend HPV preventive services to IUS.37,38
Practice implications
As these IUS had suboptimal knowledge of HPV and related cancers and experienced specific access barriers, it was not surprising that more than two-thirds of the participants had not received the HPV vaccination or (for the females) had a Pap smear. To address these knowledge gaps and increase uptake of HPV preventive measures, evidence-based and theory-driven interventions should: 1) provide accurate information on HPV transmission modes, risk factors, and risk reductions; 2) target sites where IUS are likely to encounter the information early on their arrival to the US; 3) address costs and how to negotiate the US health care system; and 4) include one-on-one HPV preventive measures counseling by nurses and other health care professionals.
Limitations
This study had several strengths. Using a mixed method approach provided an in-depth understanding of IUS perceptions of HPV and preventive practices, a university population with unique challenges and cultural lens that may differ from US born college students. However, this study is not without limitations. Results are not generalizable to all IUS because of the small sample and participants’ self-selection. Additionally, as the study explored the sensitive topic of sexual behaviors, it is possible participants may have withheld particular experiences or opinions due to concerns about social desirability.
Conclusion
The use of the HBM allowed a comprehensive understanding of the unique challenges and potential points of intervention for IUS at risk for HPV. A multi-pronged approach focusing on awareness, knowledge, health care provider recommendations, and alleviating barriers hold the potential to improve HPV preventive practices and decrease associated sequelae.
Acknowledgements
Research reported in this publication was supported in part by NHLBI of the National Institutes of Health under award number K23 HL133596-01A1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Chigozie A. Nkwonta, University of South Carolina College of Nursing, Columbia, South Carolina.
Robin M. Dawson, University of South Carolina College of Nursing, Columbia, South Carolina..
Adebola Adegboyega, University of Cincinnati College of Nursing, Cincinnati, Ohio.
References
- 1.National Cancer Institutes. Human Papilloma Virus (HPV) Vaccines. Available at https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-vaccine-fact-sheet. Accessed May 21, 2019.
- 2.Centers for Disease Control and Prevention (CDC). Human Papilloma Virus. 2018;. Available at https://www.cdc.gov/std/hpv/stdfact-hpv.htm. Accessed September 17, 2018
- 3.Centers for Disease Control and Preventions. (CDC) Genital HPV Infection - Fact Sheet. 2018; https://www.cdc.gov/std/hpv/stdfact-hpv.htm. Accessed september 17, 2018.
- 4.Bosch FX, Broker TR, Forman D, et al. Comprehensive control of human papillomavirus infections and related diseases. Vaccine. 2013;31:H1–H31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Martel C, Ferlay J, Franceschi S, et al. Global burden of cancers attributable to infections in 2008: a review and synthetic analysis. The lancet oncology. 2012;13(6):607–615. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC). HPV- Associated Cancer Statistics. Available at https://www.cdc.gov/cancer/hpv/statistics/index.htm. Accessed May 21, 2019
- 7.World Health Organization (WHO). WHO reccomendations for routine immunization-summary tables. Available at https://www.who.int/immunization/policy/immunization_tables/en/. Accessed May 21, 2019
- 8.Centers for Disease Control and Prevention (CDC). FDA licensure of quadrivalent human papillomavirus vaccine (HPV4, Gardasil) for use in males and guidance from the Advisory Committee on Immunization Practices (ACIP). MMWR Morbidity and mortality weekly report. 2010;59(20):630. [PubMed] [Google Scholar]
- 9.Chatterjee A The next generation of HPV vaccines: nonavalent vaccine V503 on the horizon. Expert review of vaccines. 2014;13(11):1279–1290. [DOI] [PubMed] [Google Scholar]
- 10.Heard I, Tondeur L, Arowas L, et al. Effectiveness of human papillomavirus vaccination on prevalence of vaccine genotypes in young sexually active women in France. The Journal of infectious diseases. 2016;215(5):757–763. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention (CDC). HPV Vaccination Coverage Data. Avaiable at https://www.cdc.gov/hpv/hcp/vacc-coverage/index.html. Accessed May 21, 2019.
- 12.Thompson EL, Vamos CA, Vázquez-Otero C, Logan R, Griner S, Daley EM. Trends and predictors of HPV vaccination among US College women and men. Preventive medicine. 2016;86:92–98. [DOI] [PubMed] [Google Scholar]
- 13.Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA pediatrics. 2014;168(1):76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wei M, Heppner PP, Mallen MJ, Ku T-Y, Liao KY-H, Wu T-F. Acculturative stress, perfectionism, years in the United States, and depression among Chinese international students. Journal of Counseling Psychology. 2007;54(4):385. [Google Scholar]
- 15.Yeh CJ, Inose M. International students’ reported English fluency, social support satisfaction, and social connectedness as predictors of acculturative stress. Counselling Psychology Quarterly. 2003;16(1):15–28. [Google Scholar]
- 16.Sherman S, Nailer E, Minshall C, Coombes R, Cooper J, Redman C. Awareness and knowledge of HPV and cervical cancer in female students: A survey (with a cautionary note). Journal of Obstetrics and Gynaecology. 2016;36(1):76–80. [DOI] [PubMed] [Google Scholar]
- 17.Sherman SM, Lane EL. Awareness of risk factors for breast, lung and cervical cancer in a UK student population. Journal of Cancer Education. 2015;30(4):660–663. [DOI] [PubMed] [Google Scholar]
- 18.Rosenstock IM. Historical origins of the health belief model. Health education monographs. 1974;2(4):328–335. [DOI] [PubMed] [Google Scholar]
- 19.Donadiki E, Jiménez-García R, Hernández-Barrera V, et al. Health Belief Model applied to noncompliance with HPV vaccine among female university students. Public health. 2014;128(3):268–273. [DOI] [PubMed] [Google Scholar]
- 20.Gerend MA, Shepherd JE. Predicting human papillomavirus vaccine uptake in young adult women: comparing the health belief model and theory of planned behavior. Annals of Behavioral Medicine. 2012;44(2):171–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lambert CLC, Azuero A, Enah CC, McMillan SC. A psychometric examination of an instrument to measure the dimensions of Champion’s Health Belief Model Scales for cervical cancer screening in women living with HIV. Applied Nursing Research. 2017;33:78–84. [DOI] [PubMed] [Google Scholar]
- 22.Hong QN, Pluye P, Fàbregues S, et al. Mixed methods appraisal tool (MMAT), version 2018. IC Canadian Intellectual Property Office, Canada. 2018. [Google Scholar]
- 23.Hong QN, FÀBregues S, Bartlett G, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Education for Information. 2018(Preprint):1–7. [Google Scholar]
- 24.Cervical Cancer Free Coalition. National Surveys. Available at http://www.cervicalcancerfreecoalition.org/resources/national-surveys/2016.
- 25.National Cancer Institute. Health Information National Trends Survey (HINTS. 2015; https://hints.cancer.gov/.
- 26.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saldaña J The coding manual for qualitative researchers. Sage; 2015. [Google Scholar]
- 28.Bendik MK, Mayo RM, Parker VG. Knowledge, perceptions, and motivations related to HPV vaccination among college women. Journal of Cancer Education. 2011;26(3):459–464. [DOI] [PubMed] [Google Scholar]
- 29.Gillison ML, Chaturvedi AK, Lowy DR. HPV prophylactic vaccines and the potential prevention of noncervical cancers in both men and women. Cancer. 2008;113(S10):3036–3046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Branković I, Verdonk P, Klinge I. Applying a gender lens on human papillomavirus infection: cervical cancer screening, HPV DNA testing, and HPV vaccination. International journal for equity in health. 2013;12(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Passmore SR, Williams-Parry KF, Casper E, & Thomas SB (2017). Message Received: African American Women and Breast Cancer Screening. Health Promotion Practice, 18(5), 726–733. 10.1177/1524839917696714 [DOI] [PubMed] [Google Scholar]
- 32.Barnard M, George P, Perryman ML, Wolff LA. Human papillomavirus (HPV) vaccine knowledge, attitudes, and uptake in college students: Implications from the Precaution Adoption Process Model. PloS one. 2017;12(8):e0182266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Navalpakam A, Dany M, Hussein IH. Behavioral perceptions of Oakland university female college students towards human papillomavirus vaccination. PloS one. 2016;11(5):e0155955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hirth JM, Batuuka DN, Gross TT, Cofie L, Berenson AB. Human papillomavirus vaccine motivators and barriers among community college students: Considerations for development of a successful vaccination program. Vaccine. 2018;36(8):1032–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pitts MJ, Stanley SJ, Kim S. College males’ enduring and novel health beliefs about the HPV vaccine. Health communication. 2017;32(8):995–1003. [DOI] [PubMed] [Google Scholar]
- 36.Gulliford M, Figueroa-Munoz J, Morgan M, et al. What does ‘access to health care’ mean? Journal of health services research & policy. 2002;7(3):186–188. [DOI] [PubMed] [Google Scholar]
- 37.Gilmer LS. Human papillomavirus vaccine update. Primary Care: Clinics in Office Practice. 2015;42(1):17–32. [DOI] [PubMed] [Google Scholar]
- 38.Martin S, Warner EL, Kirchhoff AC, Mooney R, Martel L, Kepka D. An electronic medical record alert intervention to improve HPV Vaccination Among Eligible Male College Students at a University Student Health Center. Journal of community health. 2018;43(4):756–760. [DOI] [PubMed] [Google Scholar]
- 39.Barnett KS, Shoben AB, McRee A-L, Reiter PL, Paskett ED, Katz ML. Human papillomavirus vaccine and Pap tests on college campuses: How do historically black colleges and universities (HBCUs) measure up? Journal of American College Health. 2016;64(8):613–618. [DOI] [PubMed] [Google Scholar]