Abstract
Objective:
To evaluate characteristics associated with adverse outcomes in low-risk nulliparous women randomized to elective labor induction at 39 weeks of gestation or expectant management.
Methods:
We conducted a secondary analysis of women randomized during the 38th week to induction at 39 weeks or expectant management. Deliveries before 39 weeks, not adherent to study protocol or with fetal anomalies were excluded. A composite of adverse outcomes (perinatal death or severe neonatal complications), 3rd or 4th degree lacerations, and postpartum hemorrhage were evaluated. Log binomial regression models estimated relative risks (RR) and 95% confidence intervals (CI) for associations of outcomes with patient characteristics including randomly assigned treatment group. Interactions between patient characteristics and treatment group were tested.
Results:
Of 6,096 women with outcome data, 5,007 (82.1%) met criteria for inclusion in this analysis. Frequency of the perinatal composite was 252 (5.0%), 166 (3.3%) for 3rd or 4th degree perineal laceration, and 237 (4.7%) for postpartum hemorrhage. In multivariable analysis, intended labor induction at 39 weeks was associated with a reduced perinatal composite outcome (4.1% vs. 6.0%; aRR 0.71; 95% CI 0.55-0.90) while increasing BMI was associated with an increased perinatal composite outcome (aRR 1.04 per unit increase; 95% CI 1.02-1.05). Decreased risk of 3rd or 4th degree perineal laceration was observed with increasing BMI ( aRR 0.96 per unit increase; 95% CI 0.93-0.98) and in black compared with white women (1.2% vs. 3.9%; aRR 0.34; 95% CI 0.19-0.60). Increased risk of postpartum hemorrhage was observed in Hispanic compared with white women (6.3% vs. 4.0%; aRR 1.64; 95% CI 1.18-2.29). Patient characteristics associated with adverse outcomes were similar between treatment groups (p for interaction > 0.05).
Conclusion:
Compared with expectant management, intended induction at 39 weeks was associated with reduced risk of adverse perinatal outcome. Patient characteristics associated with adverse outcomes were few and similar between groups.
Clinical Trial Registration:
Précis:
Characteristics associated with adverse outcomes were few and similar between induction and expectant management, and induction at 39 weeks was associated with reduced adverse perinatal outcomes.
Introduction:
The ARRIVE trial (a randomized trial of elective induction versus expectant management) tested the hypothesis that elective induction of labor at 39 weeks compared with expectant management among low-risk nulliparous women reduces the risk of a composite of perinatal mortality and severe neonatal morbidity. The primary perinatal outcome in the ARRIVE trial was not significantly different between the induction of labor and expectant management groups (RR 0.80; 95% CI 0.64-1.00), whereas the major secondary outcome of cesarean delivery was significantly less common in the induction of labor group (RR 0.84; 95% CI 0.76-0.93)1.
In the wake of the ARRIVE trial, it is theorized that outcomes with induction of labor at 39 weeks’gestation and expectant management may be different in certain subgroups of low-risk women. Characteristics such as maternal age, maternal weight, or Bishop score could be used to better identify which low-risk women at 39 weeks are at greatest risk of adverse outcomes, and therefore might preferentially benefit from labor induction or from expectant management. Our objective in this secondary analysis was to evaluate the association between patient characteristics and maternal and perinatal adverse outcomes among women who underwent intended elective labor induction at 39 weeks or expectant management. We also wanted to determine whether a multivariable model could be developed to predict outcome based on characteristics.
Methods:
We performed a secondary analysis of the ARRIVE trial of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. Women eligible for enrollment in the initial trial were low-risk nulliparous women with a live non-anomalous singleton fetus in a vertex presentation, and who had no contraindication to vaginal delivery, no planned cesarean delivery or indication for induction prior to 40 weeks 5 days. Eligible, consenting women were randomized between 38 weeks 0 days and 38 weeks 6 days to either induction of labor or expectant management. Women in the induction group were assigned to undergo induction of labor at 39 weeks 0 days to 39 weeks 4 days and women in the expectant management group were asked to forego elective delivery before 40 weeks 5 days and to have delivery initiated no later than 42 weeks 2 days. Full descriptions of the eligibility criteria and study procedures of the initial trial are published elsewhere 1. The study protocol was reviewed and approved by all participating institutions’ review boards. Written informed consent was obtained from all participants before randomization.
To estimate the associations between patient characteristics and adverse outcomes for women for whom these associations would be relevant in an actual clinical setting, the current analysis excluded women in the trial whose labor, induction or cesarean section began before 39 weeks 0 days, even if the actual delivery was at 39 weeks 0 days or later. Because an inclusion criterion for the trial was non-anomalous fetuses, and this secondary analysis evaluated a perinatal outcome, the 12 enrolled pregnancies with anomalies detected after randomization were also excluded from this analysis. Women whose management and delivery were not compliant with the intended intervention were also excluded. Therefore women assigned to induction were excluded if their delivery began after 39 weeks 4 days unless the delay was due to a newly developed medical indication (e.g., awaiting resolution of active herpes) and women assigned to expectant management were excluded if an induction without a medical indication was initiated before 40 weeks 5 days. Women in either group were excluded if they had an elective cesarean without labor.
Outcomes evaluated included a composite of perinatal mortality and severe perinatal morbidity, 3rd or 4th degree perineal lacerations, and postpartum hemorrhage. The perinatal composite outcome for this analysis was the same as the primary outcome of the parent trial, defined as one or more of the following: perinatal death, the need for respiratory support within 72 hours after birth, Apgar score of 3 or less at 5 minutes, hypoxic–ischemic encephalopathy, seizure, infection (confirmed sepsis or pneumonia), meconium aspiration syndrome, birth trauma (bone fracture, neurologic injury, or retinal hemorrhage), intracranial or subgaleal hemorrhage, or hypotension requiring vasopressor support. Postpartum hemorrhage was defined as any of the following: use of two or more uterotonics (methergine, prostaglandin F2-alpha, prostaglandin E1) other than oxytocin, blood transfusion, or other surgical interventions for bleeding such as uterine compression sutures (B-Lynch stitch), uterine artery ligation, vascular embolization, hypogastric artery ligation, uterine balloon or packing, curettage, or non-elective hysterectomy.
In addition to treatment group, eleven baseline maternal characteristics that could be identified prior to induction or expectant management undertaken at 39 weeks were evaluated: maternal age, self-reported race-ethnicity, body mass index (BMI) at randomization, marital status, employment status, insurance type, smoking, drinking, previous pregnancy loss (<20 weeks), assisted conception history, and modified Bishop score at randomization.
We compared differences in study outcomes by treatment group and patient characteristics using the χ2 test for categorical variables and the Wilcoxon rank sum test for continuous variables. Log-binomial multivariable regression models were used to estimate the relative risks (RR) and 95% confidence intervals (CI). Only those patient characteristics that showed a significant association with outcome in univariate analysis (p<0.05) were included in the multivariable models. Backwards selection was used to retain significant characteristics. To account for patient clustering within a hospital, random effects for hospital were included in the final models. Interactions were then assessed between each patient characteristic and treatment group, with interactions retained if p<0.05. Area under the curve (AUC) was estimated for each final model with and without random effects for hospital. AUC values from the receiver-operating characteristic (ROC) curves used to characterize the classification ability of the models were as follows: 0.5 was considered no better than chance, >0.5 to <0.7 poor, ≥0.7 to <0.8 acceptable, ≥0.8 to <0.9 excellent, ≥0.9 outstanding2. All statistical analyses were performed using SAS 9.4 and all tests were two-sided with p<0.05 considered statistically significant. No imputation for missing data was performed.
Results:
Of the 6,106 women enrolled in the ARRIVE trial, 6,096 (99.8%) had delivery data. Of these, 5,007 (82.1%) achieved 39 weeks’ gestation, had no fetal anomalies and adhered to the study protocol. (Figure 1). The maternal characteristics for those included in the analysis and those excluded because they were not delivered per protocol are presented in Appendix 1.
Figure 1.
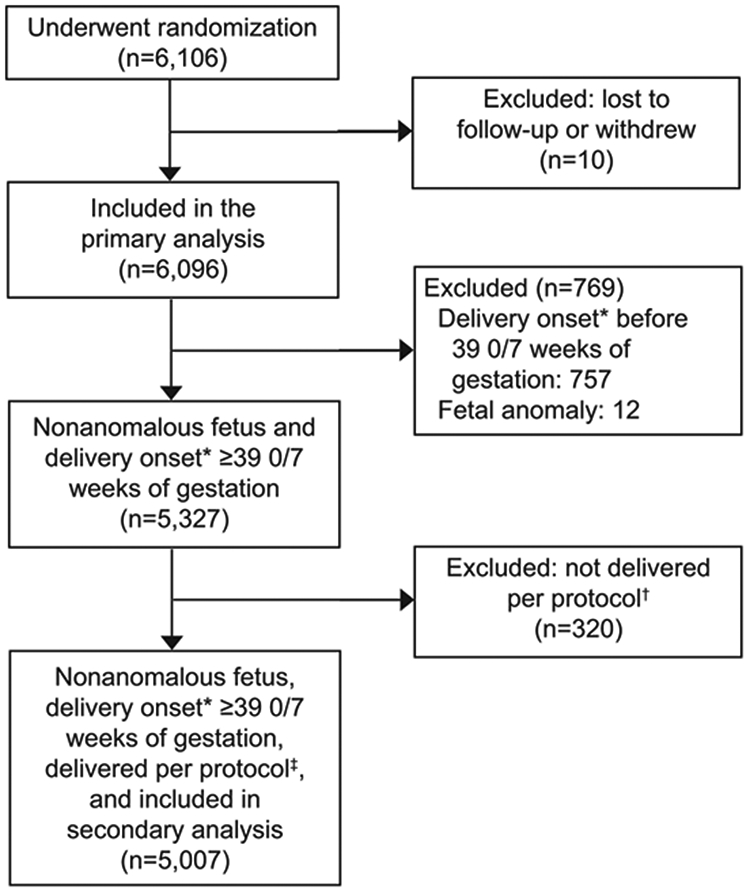
Flowchart of eligibility determination for inclusion in this secondary analysis. *Onset defined as when the process of delivery started. †Women assigned to induction were excluded if their delivery began after 39 0/4 weeks of gestation unless the delay was due to a newly developed medical indication (eg, awaiting resolution of active herpes) and women assigned to expectant management were excluded if an induction without a medical indication was initiated before 40 5/7 weeks of gestation. Women in either group were excluded if they had an elective cesarean delivery without labor. ‡Among those in the intended induction group who achieved 39 weeks of gestation with a nonanomalous fetus (n=2,505), delivery per protocol included electively induced labor (n=2,150), spontaneous labor (n=285), or medically indicated delivery (n=65) from 39 0/7 to 39 4/7 weeks of gestation, or delivery delayed past 39 4/7 weeks of gestation because of a newly developed medical indication (ie, active herpes) (n=5). Among those in the intended expectant management group who achieved 39 weeks of gestation with a nonanomalous fetus (n=2,502), delivery per protocol included induction from 40 5/7 to 42 2/7 weeks of gestation (n=440), or spontaneous labor (n=1,552), or medically indicated delivery (n=510) from 39 0/7 to 42 2/7 weeks of gestation.
Overall, the perinatal composite occurred in 252 (5.0%) newborns, 166 (3.3%) women had a 3rd or 4th degree perineal laceration, and 237 (4.7%) deliveries were complicated by postpartum hemorrhage. The perinatal composite outcome occurred in 103 (4.1%) women in the induction of labor group compared with 149 (6.0%) women in the expectant management group (p=0.003). Conversely, frequencies of 3rd or 4th degree perineal laceration and postpartum hemorrhage were similar between women in the induction of labor and expectant management groups (laceration: 3.5% vs. 3.2%, p=0.53; postpartum hemorrhage: 4.7% vs. 4.8%, p=0.94). Outcomes were similar between those included in the analysis and those excluded because they were not delivered per protocol (perinatal composite 5.0% vs. 5.3%, p=0.82; 3rd or 4th degree perineal laceration 3.3% vs. 2.8%, p=0.62; postpartum hemorrhage 4.7% vs. 3.8%, p=0.42).
The final unadjusted and multivariable models showing the characteristics significantly associated with each outcome are presented in Table 1. Intended elective induction of labor at 39 weeks was associated with a reduced risk of the perinatal composite outcome (4.1% vs. 6.0%; aRR 0.71; 95% CI 0.55-0.90) and BMI (per unit increase) was associated with an increased risk of the perinatal composite outcome (aRR 1.04; 95% CI 1.02-1.05). A decreased risk of 3rd or 4th degree perineal laceration was observed with increasing BMI (per unit increase) (aRR 0.96; 95% CI 0.93-0.98), and in black women (vs. white women) (1.2% vs. 3.9%; aRR 0.34; 95% CI 0.19-0.60). A higher risk of 3rd or 4th degree perineal laceration was observed in Asian women in the unadjusted model, but not in the adjusted model. Hispanic women (vs. white women) were at an increased risk for postpartum hemorrhage (6.3% vs. 4.0%; aRR 1.64; 95% CI 1.18-2.29). Patient characteristics associated with adverse outcomes were similar between treatment groups (p for interaction > 0.05; treatment group by BMI interaction for the perinatal outcome p=0.32; treatment group by BMI interaction for 3rd or 4th degree perineal lacerations p=0.35; treatment group by race and ethnicity interaction for 3rd or 4th degree perineal lacerations ranged from p=0.47 to p=0.88; treatment group by race and ethnicity interaction for postpartum hemorrhage ranged from p=0.09 to p=0.53).
Table 1.
Characteristics significantly associated with adverse outcomes
| Exposure | N (%) | uRR (95% CI) | Model 1 aRR (95% CI) |
Model 2 aRR (95% CI) |
|---|---|---|---|---|
| Perinatal Composite* | ||||
| Treatment group | ||||
| Intended elective induction of labor | 103 (4.1) | 0.69 (0.54-0.88) | 0.69 (0.54-0.88) | 0.71 (0.55-0.90) |
| Expectant management | 149 (6.0) | referent | referent | |
| Per unit increase in BMI, kg/m2 | 1.03 (1.01-1.05) | 1.03 (1.01-1.05) | 1.04 (1.02-1.05) | |
| 3rd or 4th degree perineal laceration† | ||||
| Per unit increase in BMI, kg/m2 | 0.95 (0.92-0.98) | 0.96 (0.93-0.98) | 0.96 (0.93-0.98) | |
| Race-ethnicity | ||||
| Non-Hispanic black | 14 (1.2) | 0.31 (0.18-0.54) | 0.34 (0.19-0.60) | 0.34 (0.19-0.60) |
| Non-Hispanic Asian | 11 (7.3) | 1.87 (1.02-3.42) | 1.71 (0.93-3.14) | 1.75 (0.94-3.25) |
| Hispanic | 50 (3.7) | 0.96 (0.68-1.35) | 1.01 (0.72-1.43) | 1.01 (0.70-1.45) |
| Other or unknown | 4 (3.1) | 0.80 (0.30-2.15) | 0.86 (0.32-2.30) | 0.88 (0.33-2.37) |
| Non-Hispanic white | 87 (3.9) | referent | referent | referent |
| Postpartum hemorrhage‡ | ||||
| Race-ethnicity | ||||
| Non-Hispanic black | 51 (4.4) | 1.11 (0.79-1.55) | n/a | 1.17 (0.80-1.70) |
| Non-Hispanic Asian | 9 (6.0) | 1.49 (0.77-2.91) | n/a | 1.44 (0.73-2.84) |
| Hispanic | 84 (6.3) | 1.57 (1.17-2.10) | n/a | 1.64 (1.18-2.29) |
| Other or unknown | 4 (3.1) | 0.78 (0.29-2.10) | n/a | 0.78 (0.29-2.09) |
| Non-Hispanic white | 89 (4.0) | referent | n/a | referent |
uRR, unadjusted relative risk; aRR, adjusted relative risk; CI, confidence interval; BMI, body mass index, n/a, not applicable
Perinatal composite model 1 included treatment group and BMI; model 2 included treatment group, BMI, and random effects for hospital
3rd or 4th degree perinatal laceration model 1 included BMI and race-ethnicity; model 2 included BMI, race-ethnicity, and random effects for hospital
Postpartum hemorrhage model 1 is not applicable because race-ethnicity was the only variable found to be associated with postpartum hemorrhage which is presented as the uRR; model 2 included race-ethnicity and random effects for hospital
As demonstrated by the AUC values of the ROC curves, the final multivariable models (without the random effects of hospital) were poor at predicting adverse outcomes [AUC for the perinatal composite 0.58 (95% CI 0.55-0.62); AUC for 3rd or 4th degree laceration 0.64 (95% CI 0.60-0.68); AUC for postpartum hemorrhage 0.56 (95% CI 0.52-0.59)]. The AUCs remained weak when the random effects of hospital were added to the models [perinatal composite 0.70 (95% CI 0.67-0.73); 3rd or 4th degree laceration 0.67 (95% CI 0.63-0.71); postpartum hemorrhage 0.67 (95% CI 0.63-0.71)].
Discussion:
We found that few baseline patient variables were significantly associated with adverse outcomes in low-risk nulliparous women who achieved 39 weeks’ gestation. In this secondary analysis of the ARRIVE trial, women were included only if the delivery process had not started by 39 weeks and subsequently were managed consistently with their randomly assigned approach to delivery (i.e., intended 39-week labor induction or expectant management). Such a cohort composition is necessary if the results are to provide insight into the fundamental questions at hand: for women at 39 weeks of gestation who have the choice to undergo immediate labor induction or expectant management, are there particular individual characteristics that could provide insight into whether they may be at particular risk of adverse outcomes and is pursuit of one strategy better than the other? The patient characteristics selected were those that could be identified prior to induction or expectant management, and thus potentially inform patient counseling. In multivariable analysis, few factors remained associated with the adverse outcomes. Notably, for all of the outcomes evaluated, no characteristics or groups of characteristics could be used to identify a subgroup of women who were more likely to benefit from expectant management versus labor induction.
Induction at 39 weeks in this analysis was associated with a reduction in the perinatal composite outcome compared with expectant managment. This finding has been reported in several earlier observational studies.3-7 and reflects a key difference between the parent trial and this secondary analysis. In the trial, women were randomized as early as 38 week 0 days and women who delivered before 39 weeks in both groups would be likely to have similar outcomes. In the current study, only women who reached 39 weeks were analyzed, given that it would be analytically not possible to determine factors associated with adverse outcomes after 39 weeks for women who were no longer pregnant at that gestational age. Correspondingly, this analysis reveals that among women who are at 39 weeks of gestation—the only group of women for whom the decision to proceed with induction or expectant management is truly actionable—intended elective induction of labor is associated with a lowering of the adverse perinatal composite outcome.
The results of the multivariable analysis demonstrating an increased risk of the perinatal composite outcome with increasing BMI are consistent with other studies8,9. Other studies also have described a decreased risk of 3rd or 4th degree perineal laceration with increasing BMI and in black women10,11. The association with an increased risk of postpartum hemorrhage in Hispanic women has been previously noted as well10. Nevertheless, our analysis demonstrated that characteristics associated with adverse outcomes were few, had relatively weak associations, and were poorly predictive; moreover, none of these associations varied significantly by treatment group.
The strengths of our analysis arise from the large and robust study from which it is derived (which included 41 community and academic geographically diverse centers), which had strict inclusion criteria, prospectively collected data, and reliable and detailed, clinically relevant outcomes. Limitations of our study are those inherent to any observational study, as well as the generalizability of the findings.
In summary, intended labor induction at 39 weeks was associated with a reduction in the perinatal composite outcome. Our analysis demonstrated that few maternal characteristics were associated with adverse outcomes after 39 weeks, and none could reliably predict which women were most likely to have these adverse outcomes. Furthermore, while induction of labor at 39 weeks was associated with a reduction in the perinatal composite outcome, no characteristics identified a subgroup of women who would prefentially benefit from undergoing expectant management. Such information may be useful to women and their obstetric providers as they consider their choices regarding timing of delivery.
Supplementary Material
Acknowledgements:
The authors thank Lindsay Doherty, M.S. for data and study management and Vinay Bhandaru, M.S. for statistical programming.
Funding: Supported by grants (HD40512, HD36801, HD27869, HD34208, HD68268, HD40485, HD40500, HD53097, HD40560, HD40545, HD27915, HD40544, HD34116, HD68282, HD87192, HD68258, HD87230) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the National Center for Advancing Translational Sciences (UL1TR001873). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Dr. Rouse, Associate Editor (Obstetrics) of Obstetrics & Gynecology, was not involved in the review or decision to publish this article.
Financial Disclosure
Robert M. Silver disclosed receiving funds as a consultant for Gestavision. Gail Mallett reports that money was paid to her institution from the George Washington University Biostatistics Center. Edward K. Chien disclosed that money was paid to his institution from Alydia Health and Gestvision. Both were industry sponsored research projects without overlap with this study. Ronald S. Gibbs disclosed that money was paid to him from Gestavision for consultation and ACI/Novavax for serving on the DSMB for a clinical trial of RSV vaccine. Geeta K. Swamy received funds from GlaxoSmithKline, Pfizer, and SAOL. The other authors did not report any potential conflicts of interest.
Contributor Information
Yasser Y. El-Sayed, Departments of Obstetrics and Gynecology of Stanford University, Stanford, CA
Madeline Murguia Rice, George Washington University Biostatistics Center, Washington, DC
William A. Grobman, Northwestern University, Chicago, IL
Uma M. Reddy, Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, MD
Alan T.N. Tita, University of Alabama at Birmingham, Birmingham, AL
Robert M. Silver, University of Utah Health Sciences Center, Salt Lake City, UT
Gail Mallett, Northwestern University, Chicago, IL
Kim Hill, University of Utah Health Sciences Center, Salt Lake City, UT
Elizabeth A. Thom, George Washington University Biostatistics Center, Washington, DC
Ronald J. Wapner, Columbia University, New York, NY
Dwight J. Rouse, Brown University, Providence, RI
George R. Saade, University of Texas Medical Branch, Galveston, TX
John M. Thorp, Jr, University of North Carolina at Chapel Hill, Chapel Hill, NC
Suneet P. Chauhan, University of Texas Health Science Center at Houston-Children’s Memorial Hermann Hospital, Houston, TX
Edward K. Chien, MetroHealth Medical Center-Case Western Reserve University, Cleveland, OH
Brian M. Casey, University of Texas Southwestern Medical Center, Dallas, TX
Ronald S. Gibbs, University of Colorado School of Medicine, Anschutz Medical Campus, Aurora, CO
Sindhu K. Srinivas, University of Pennsylvania, Philadelphia, PA
Geeta K. Swamy, Duke University, Durham, NC
Hyagriv N. Simhan, University of Pittsburgh, Pittsburgh, PA
George A. Macones, Washington University, Saint Louis, MO
References:
- 1.Grobman WA, Rice MM, Reddy UM, Tita AT, Silver RM, Mallett G, et al. Labor induction versus expectant management in low-risk nulliparous women. New England Journal of Medicine. 2018;379:513–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hosmer DW, Lemeshow S, Sturdivant RX. Applied Logistic Regression, 3rd Ed. Chapter 5, John Wiley and Sons, Hoboken, NJ: (2013). [Google Scholar]
- 3.Cheng YW, Kaimal AJ, Snowden JM, Nicholson JM, Caughey AB. Induction of labor compared to expectant management in low-risk women and associated perinatal outcomes. American journal of obstetrics and gynecology. 2012;207:502. e1–. e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Darney BG, Snowden JM, Cheng YW, Jacob L, Nicholson JM, Kaimal A, et al. Elective induction of labor at term compared with expectant management: maternal and neonatal outcomes. Obstetrics and gynecology. 2013;122:761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gibson KS, Waters TP, Bailit JL. Maternal and neonatal outcomes in electively induced low-risk term pregnancies. American journal of obstetrics and gynecology. 2014;211(3):249. e1–. e16. [DOI] [PubMed] [Google Scholar]
- 6.Osmundson S, Ou-Yang RJ, Grobman WA. Elective induction compared with expectant management in nulliparous women with an unfavorable cervix. Obstetrics & Gynecology. 2011;117(3):583–7. [DOI] [PubMed] [Google Scholar]
- 7.Stock SJ, Ferguson E, Duffy A, Ford I, Chalmers J, Norman JE. Outcomes of elective induction of labour compared with expectant management: population based study. BMJ. 2012;344:e2838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aune D, Saugstad OD, Henriksen T, Tonstad S. Maternal body mass index and the risk of fetal death, stillbirth, and infant death: a systematic review and meta-analysis. Jama. 2014;311(15):1536–46. [DOI] [PubMed] [Google Scholar]
- 9.Scott-Pillai R, Spence D, Cardwell C, Hunter A, Holmes V. The impact of body mass index on maternal and neonatal outcomes: a retrospective study in a UK obstetric population, 2004–2011. BJOG: An International Journal of Obstetrics & Gynaecology. 2013;120(8):932–9. [DOI] [PubMed] [Google Scholar]
- 10.Grobman WA, Bailit JL, Rice MM, Wapner RJ, Reddy UM, Varner MW et al. Racial and ethnic disparities in maternal morbidity and obstetric care. Obstetrics and gynecology. 2015;125(6):1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blomberg M Maternal body mass index and risk of obstetric anal sphincter injury. BioMed research international. 2014;2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


