Abstract
Background.
We compared the utility of existing and modified versions of high resolution manometry for diagnosing defecatory disorders (DD).
Methods.
In 64 healthy and 136 constipated women, we compared left lateral (LL) and seated manometry, analyzed with existing (Manoview™) and new methods, for discriminating between constipated patients with normal and prolonged rectal balloon expulsion time (BET). In both positions, the rectoanal gradient (RAG), and for the new analysis, the pressure topography pattern during evacuation, were used to discriminate between constipated patients without and with DD.
Key Results.
The BET was prolonged, suggestive of a DD, in 52 patients (38%). During evacuation, rectoanal pressures and the RAG were greater in the seated than the LL position (P≤.001). In the seated position, the BET was associated with the pattern (P=.0001), being prolonged in respectively 45%, 15%, 53%, and 0% of patients with minimal change, anal relaxation, paradoxical contraction, and transmission. Within each pattern, the RAG was greater (ie, less negative, P<.0001) in patients with a normal than a prolonged BET. Compared to the Manoview™ RAG in the LL position, the integrated analysis (ie, pattern and new RAG) in the LL position (P<.01) and the seated Manoview™ gradient (P=.02) were each more effective for discriminating between constipated patients without and with DD.
Conclusions & Inferences.
Anorectal HRM ideally should be performed in the more-physiological seated position, and analyzed by a two-tier approach which incorporates the overall pattern followed by the rectoanal gradient. These findings reinforce the utility of manometry for diagnosing DD.
Keywords: Anorectal test, High resolution manometry, Defecatory disorder, Constipation, Diagnostic utility
Graphical Abstract
Introduction
Among constipated patients, anorectal tests, typically anorectal manometry and the rectal balloon expulsion test (BET) or defecography with barium or magnetic resonance imaging, are necessary to diagnose defecatory disorders (DD).1–4 Overall, the results of these tests are correlated with each other.5, 6 However, among individual patients, different tests often provide different answers, which confounds the diagnosis of DD. High resolution manometry (HRM) is the initial and arguably the most widely used test to diagnose DD.7 In addition to assessing rectoanal functions during defecation, HRM may also hint at structural abnormalities (eg, rectal prolapse and large rectoceles).8, 9 However recent studies have concluded that “anal manometry is of limited utility for diagnosing DD because even in asymptomatic people, the rectoanal pressure gradient (rectal – anal pressure) during evacuation is negative”10 and overlaps considerably between healthy people and DD patients.7, 10–12 No studies have evaluated the more clinically relevant question, that is, the utility of the gradient for distinguishing between constipated patients with and without DD.
Perhaps the utility of HRM for diagnosing DD is limited because HRM is performed in the left lateral (LL) position and/or because the method for analyzing rectoanal pressures during evacuation is suboptimal. In three studies, of which two only included healthy people, rectal, and to a lesser extent anal pressures measured with conventional or non-HRM, during evacuation were greater and dyssynergia was less prevalent in the seated than in the LL position.13–15 However, rectoanal dyssynergia in the seated position did not predict a prolonged BET, which reflects pelvic floor dysfunction, in healthy people.14 Among constipated patients, the agreement between rectoanal pressures measured with solid-state manometry, not HRM, and the BET was numerically better in the seated than the LL position.16 An abstract reported that 27% of patients with dyssynergia during HRM in the left lateral position had a normal pattern in the seated position.17 However, none of these studies evaluated the diagnostic utility of HRM in healthy controls or patients. A statistical comparison of the diagnostic utility of solid state manometry in the seated and LL positions was not performed. Indeed, a 2019 consensus document recommends that manometry “should be performed in the left lateral position”.18
During evacuation, the default ManoScan™ (Medtronic Inc, Minneapolis, MN) software algorithm for analyzing HRM identifies the highest rectoanal gradient (RAG) over a consecutive period of 2 seconds during the 20 second maneuver. (We use a duration of 3 seconds, which is arguably more representative of evacuation than the default Manoview™ option of 2 seconds). The RAG is calculated by subtracting the anal from the rectal pressure. The rectal pressure is measured by the same sensor throughout evacuation. By contrast, the sensor with the highest anal pressure at each instant (at 10 Hz) is used to summarize anal pressure. This method has several limitations. First, because the highest, and not the lowest, anal pressure is used to calculate the gradient, the gradient is generally not the highest pressure difference between the rectum and the anal canal. Perhaps this explains, at least in part, why the RAG during evacuation is negative in most asymptomatic people.12 Second, the specific sensor that is used to measure anal pressure often moves over the 20 second evacuation period. Third, the highest anal pressure measurement is prone to artifact, for example due to catheter impingement.19 Finally, while the RAG is a useful metric, it ignores the underlying pressure topography pattern that is evident by careful inspection and is used to classify esophageal motility disorders (e.g. subtypes of achalasia).20
Addressing these limitations, we aimed to 1) compare rectoanal pressures measured in the LL and seated positions, 2) compare the utility of LL and seated HRM, and 3) compare rectoanal pressures measured with the existing and a new approach, in order to discriminate among healthy controls, constipated patients without DD, and constipated patients with DD.
Methods
Design
All participants consented to participate in these studies, which were approved by the Mayo Clinic Institutional Review Board and performed between January 2011 and April 2018. After two sodium phosphate enemas (Fleet; C.B. Fleet), rectoanal pressures were measured at rest, during squeeze, and simulated evacuation with high-resolution anorectal manometry in the LL and seated positions in 64 healthy and 136 constipated women. The rectal balloon expulsion test was performed in the seated position.
Subjects
All participants, aged 18 years or older, had a clinical interview and physical examination. Neither healthy controls nor patients had clinically systemic disease (eg, cardiovascular or neurological) or were taking medications (eg, opioids) that have major effects on gastrointestinal motility. Controls did not have a functional bowel disorder by Rome 3 criteria, documented grade 3 or 4 obstetric anorectal laceration, or any previous anorectal surgery.21 Patients had symptoms of chronic constipation for at least 1 year and had failed treatment with over-the-counter laxatives.
Procedures
Anorectal Manometry
Rectoanal pressures were measured with HRM catheters (Manoscan™; 4.2 mm diameter; currently Medtronic Inc). Pressures were measured for 20 seconds at rest, during squeeze (voluntary contraction of the anal sphincter, 3 attempts), simulated evacuation with an empty rectal balloon, and a Valsalva maneuver.22 Rectal sensory thresholds for first sensation, urge and discomfort were recorded. This procedure was performed in the LL and subsequently seated positions while seated on the commode. During seated HRM, the catheter was externally enclosed within a plastic clip (Mayo Clinic and Medtronic Inc) to limit displacement.
All studies were analyzed with the commercially-available version of the software (Manoview AR v3.0; Medtronic Inc)22 and separately with a new method.
Rectal balloon expulsion time
Participants had up to 3 minutes to expel a 4-cm-long balloon filled with 50 ml water from the rectum in privacy while seated on a commode.6, 23 The BET was noted and the balloon was removed if participants could not expel the balloon within 3 minutes. Normal values for the BET depend on the type of balloon.23, 24 With a Foley catheter, the upper limit of normal BET (nBET) is 2 minutes. Consistent with data from our and other centers with balloons similar to that used in this study, a BET greater than 60 seconds was considered to be prolonged (ie, abnormal) for the analysis.23, 24
New analysis
For the new analysis, the American Standard Code for Information Interchange (ASCII) datasets for each study were exported to Microsoft Excel (Microsoft Inc). The catheter comprises two rectal balloon sensors (sensors 1 and 2). Sensor 2 is 3.4 cm oral to the uppermost of 10 sensors, which are numbered 3–12 in this paper. Sensors 3–12 are separated by 6 mm (they span 5.4 cm). Because the most distal sensors, i.e. 12, and often 11, are outside the body, they were not used for this assessment.
The new analysis comprised the following steps:
Identifying the anal canal by manometry. Sensors 3–4 and 7–10 are typically in the rectum and anal canal respectively. Sensors 5 and 6 may be located either in the rectum or anal canal. In a prior study, sensors that recorded pressures which were 20 mmHg greater than rectal pressure were considered to be in the anal canal.25 At rest, the rectal pressure is approximately 10 mmHg. Hence, in this study, sensors that recorded a resting pressure of 30 mmHg or greater were considered to be in the functional anal canal.
Duration. The rectoanal pressures were averaged over 1.5 seconds immediately before evacuation and between 5 to 15 seconds after the onset of evacuation. During the first 5 seconds of evacuation, the anal pressure often increases, even in healthy people; hence these pressures were not analyzed (unpublished observations).
Identification of patterns. Based on the change in rectal and anal pressures during evacuation, four patterns were identified (Figure 1). Anal relaxation was defined as a reduction in pressure in four or more consecutive anal sensors. The thresholds for relaxation were 5 mmHg or greater in sensors 5–7, 9, and 10 and 10 mmHg in sensor 8. Conversely, paradoxical contraction was defined by an increase in anal pressure in two or more consecutive sensors. The threshold change was 10 mm Hg in sensors 5, 7, 8, 9, and 10 and 15 mm Hg in sensor 6. Guiding the selection of these thresholds, approximately one-third (ie, sensors 5, 6, and 10) or two-thirds (ie, sensors 7–9) of healthy people with a nBET had anal relaxation as defined by these criteria (unpublished data). Conversely, only approximately 10% of healthy people had paradoxical contraction. Participants who had anal relaxation in some sensors and paradoxical contraction in other sensors were included in the latter category because anal contraction impedes evacuation. Those who did not have criteria for either pattern were categorized as minimal change. Transmission, which is visually evident, is characterized by transmission of rectal pressures throughout the anal canal, suggestive of a common cavity. To identify this pattern, we analyzed the linear regression of rectal and anal pressures during evacuation versus location (sensors 3 to 10) in each patient. Two parameters in this regression, the square root of R2, which is the slope, and the root mean square (RMS) error, which represents the closeness of fit between the observed and the fitted data, were used to define transmission. When pressures decline from the rectum (sensor 3) to the distal anal canal (sensor 10), the √R2 is high. A low root mean square (RMS) error suggests a close fit between the observed and the fitted data. A √R2/RMS error ≥2 was used to define transmission.
The rectoanal gradient (ie, rectal – anal pressure) was calculated over ten seconds (ie, between 5 – 15 seconds of evacuation). The rectal pressure was derived by identifying the greater value of pressures measured by sensors 1 and 2 at each instant. Thereafter, these values were averaged over the 10 seconds. The anal pressure was derived by averaging the pressures recorded by sensors 8, 9, and 10 over 10 seconds.
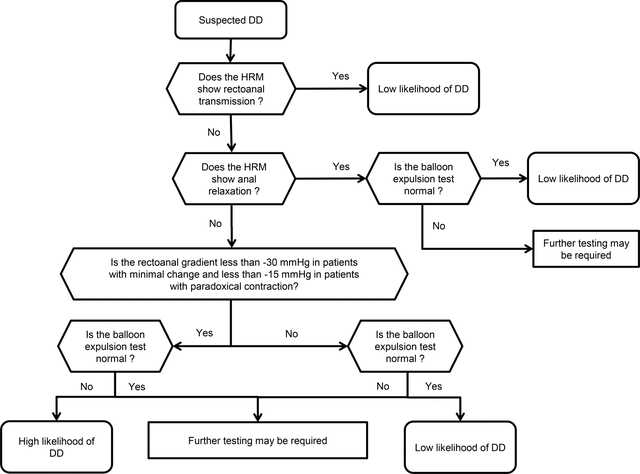
Figure 1.
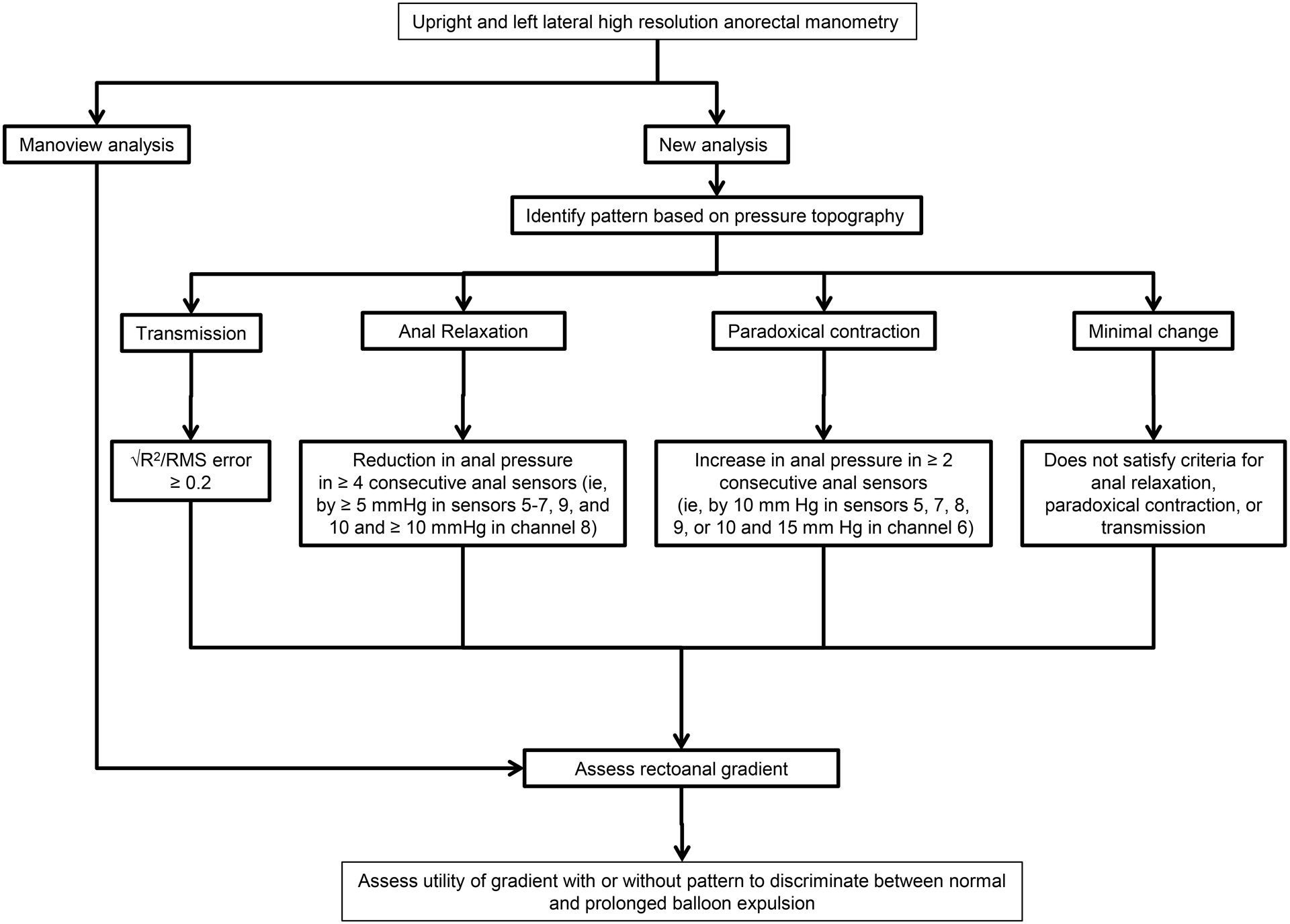
Analysis of rectoanal pressures during evacuation. Rectoanal pressures were measured with left lateral and seated HRM and analyzed with the Manoview™ analysis and a new method. The new analysis comprises two steps i.e., characterization of the rectoanal pressure profiles into 4 patterns followed by an assessment of the rectoanal gradient to discriminate between constipated patients with a normal and a prolonged balloon expulsion test.
The differences between the existing and the new methods are described in Table 1.
Table 1.
Definitions of Rectoanal Parameters Evaluated with Manoview and New Analysis
| Parameter | Manoview™ | New analysis |
|---|---|---|
| Rectal pressure at rest | Difference between the anal pressures expressed as “absolute reference” and “rectal reference” values at rest | Highest instantaneous pressure averaged over 1.5 seconds before evacuation |
| Anal pressure at rest | Average of the maximum anal pressure (eSleeve) for 20 seconds | Average of anal pressures recorded by sensors 8,9,10 during 1.5 seconds before evacuation |
| Rectal pressure during evacuation | Rectal pressures during the 3 second epoch when rectoanal gradient is the most positive | Highest instantaneous pressure in sensors 1 and 2 were averaged over 10 s (ie, from 5 – 15 seconds) during evacuation |
| Anal pressure during evacuation | Average of the maximum anal pressure during the 3 second epoch when RAG is least negative or most positive | Average of anal pressures in sensors 8,9,10 over 10 s (ie, from 5 – 15 seconds) during evacuation |
| Rectal pressure increment during evacuation | Rectal pressure change (evacuation – rest) | Rectal pressure change (evacuation – rest) |
| Change in anal pressure during evacuation | Anal pressure change (evacuation – rest) | Anal pressure change (evacuation – rest) |
| Rectoanal gradient during evacuation | (Rectal – anal pressure) during evacuation | (Rectal – anal pressure) during evacuation |
Statistical Analysis
The paired and unpaired t tests were used to compare the outcome variables (rectal and anal pressures and the RAG) between the LL and seated positions in healthy people and constipated patients and between constipated patients with a nBET and a prolonged BET (pBET). For each abnormal rectoanal parameter, likelihood ratios (LR) were used express the likelihood (sensitivity/[1-specificity]) of a DD relative to constipation without DD in patients with constipation with pBET versus constipation with nBET.26 Among constipated patients, the pre- and based on the LR, the post-test probabilities of having disease were computed. Categorical variables were compared with the chi square test. Receiver operating characteristic (ROC) curves that were derived from logistic regression models were used to compare the utility of the RAG computed with the Manoview™ analysis and the new analysis and the addition of rectoanal pressure patterns, assessed in the LL and seated positions, for discriminating between constipated patients with nBET and pBET, which suggests a DD. Similar comparisons, albeit incorporating the BET as a continuous rather than a dichotomized variable were performed with univariate and multiple Cox proportional regression models. Unless stated otherwise, the data are summarized as the Mean (SD). All analyses used JMP software (version 9.4, SAS Cary, NC). Comparison between models used the model partial chi-square statistics in the case of nested models, and used “DeLong and Delong” in the case of non-nested models.27
Results
Demographic Features and Clinical Characteristics
The mean age and BMI were not significantly different among 64 controls with a nBET (35 [13] y, 26 [5] kg/m2), 84 constipated patients with nBET (42 [17] y, 25 [5] kg/m2) and 52 constipated patients with pBET (41 [14] y, 24 [5] kg/m2). Among 84 patients with nBET, 41 (49%) had symptoms of functional constipation and 40 (48%) had symptoms of constipation-predominant IBS. The remaining 3 patients had chronic constipation but did not satisfy Rome criteria because they were taking laxatives. Among 52 patients with a BET longer than 60 seconds, 35 (67%) had symptoms of functional constipation and 17 (33%) had constipation-predominant IBS; the BET was longer than 180 seconds in 44 of 52 (85%) of participants.
Table 2 compares the proportion of patients with specific bowel symptoms in each of four groups, which are categorized by BET and HRM results, separately for seated and LL HRM. These proportions were not significantly different among groups.
Table 2.
Comparison of bowel symptoms among different groups
| Left lateral position | Seated position | P-value for left lateral position | P-value for seated position | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Normal HRM | Abnormal HRM† | Normal HRM | Abnormal HRM† | |||||||
| Normal BET n (%) |
Prolonged BET n (%) |
Normal BET n (%) |
Prolonged BET n (%) |
Normal BET n (%) |
Prolonged BET n (%) |
Normal BET n (%) |
Prolonged BET n (%) |
|||
| Total patients (N) | 17 | 1 | 67 | 51 | 32 | 4 | 52 | 48 | ||
| Symptoms | ||||||||||
| <3 bowel movements | 5 (29) | 0 (0) | 28 (42) | 33 (65) | 15 (47) | 3 (75) | 18 (35) | 30 (63) | 0.27 | 0.27 |
| Incomplete evacuation | 12 (71) | 1 (100) | 50 (75) | 40 (78) | 24 (75) | 3 (75) | 38 (73) | 38 (79) | 0.27 | 0.22 |
| Straining | 12 (71) | 1 (100) | 60 (90) | 44 (86) | 27 (84) | 4 (100) | 45 (87) | 41 (85) | 0.27 | 0.27 |
| Hard stools | 11 (65) | 1 (100) | 47 (70) | 38 (75) | 22 (69) | 4 (100) | 36 (69) | 35 (73) | 0.27 | 0.27 |
| Anal blockage | 11 (65) | 1 (100) | 45 (67) | 37 (73) | 20 (63) | 3 (75) | 36 (69) | 35 (73) | 0.27 | 0.27 |
| Anal digitation | 5 (29) | 0 (0) | 27 (40) | 26 (51) | 12 (38) | 0 (0) | 20 (38) | 26 (54) | 0.27 | 0.27 |
Abnormal HRM includes patients with paradoxical contraction or the minimal change pattern
Effects of Position
With a few exceptions, rectal and anal pressures at rest and during evacuation were generally greater in the seated than the LL position in healthy controls and in constipated patients (Table 3). Compared to the LL position, the rectal pressure at rest (P<.0001) and during evacuation (P<.0001) and the anal pressure at rest (P≤.0003) and during simulated evacuation (P≤ .0006), and the RAG during evacuation were greater in the seated position in controls and patients.
Table 3.
Comparison of Rectoanal Pressures in the Left Lateral and Seated Positions
| Healthy controls (n=64) | Constipation (n=136) | |||||||
|---|---|---|---|---|---|---|---|---|
| Rectoanal parameters† | Left lateral position | Seated position | P-value‡ | Left lateral position | Seated position |
P-value‡ | P-value left lateral -Controls vs constipation | P-value Seated -Controls vs constipation |
| Anal pressure - rest, Manoview™ | 85 (24) | 97 (27) | .0003 | 90 (28) | 105 (34) | <.0001 | .20 | .07 |
| Anal pressure - squeeze, Manoview™ | 203 (58) | 192 (52) | .01 | 183 (67) | 159 (68) | <.0001 | .02 | .0001 |
| Anal pressure - Valsalva, Manoview™ | 127 (43) | 128 (41) | .74 | 125 (44) | 133 (48) | .004 | .72 | .47 |
| Rectal pressure - rest, Manoview™ | 4 (7) | 32 (20) | <.0001 | 6 (8) | 28 (16) | <.0001 | .16 | .15 |
| Rectal pressure - rest, new analysis | 7 (6) | 33 (20) | <.0001 | 8 (11) | 30 (17) | <.0001 | .25 | .34 |
| Rectal pressure – evacuation, Manoview™ | 33 (20) | 66 (40) | <.0001 | 33 (28) | 62 (36) | <.0001 | .94 | .39 |
| Rectal pressure – evacuation, new analysis | 33 (18) | 63 (34) | <.0001 | 32 (26) | 58 (29) | <.0001 | .91 | .30 |
| Rectal pressure increment – evacuation, Manoview™ | 29 (19) | 34 (30) | .03 | 27 (26) | 33 (28) | .02 | .46 | .58 |
| Rectal pressure increment – evacuation, new analysis | 26 (17) | 30 (21) | .05 | 24 (22) | 28 (21) | .02 | .58 | .43 |
| Anal pressure – evacuation, Manoview™ | 73 (22) | 83 (25) | .0006 | 83 (27) | 97 (34) | <.0001 | .002 | .001 |
| Anal pressure - evacuation, new analysis | 65 (22) | 67 (21) | .44 | 74 (28) | 81 (31) | .005 | .007 | .0002 |
| Change in anal pressures– evacuation, Manoview™ | −12 (31) | −13 (32) | .66 | −4 (26) | −4 (29) | .60 | .07 | .04 |
| Change in anal pressures - evacuation, new analysis | −2 (17) | −12 (19) | .0002 | 6 (18) | 2 (20) | .02 | .001 | <.0001 |
| Rectoanal gradient- evacuation, Manoview™ | −39 (25) | −17 (42) | <.0001 | −51 (33) | −35 (46) | <.0001 | .006 | .004 |
| Rectoanal gradient- evacuation, new analysis | −32 (28) | −4 (39) | <.0001 | −42 (32) | −23 (41) | <.0001 | .03 | .001 |
| Rectal threshold - first sensation, ml | 45 (14) | 46 (17) | .71 | 49 (20) | 54 (23) | .02 | .21 | .05 |
| Rectal threshold - desire to defecate, ml | 70 (17) | 67 (20) | .51 | 84 (32) | 87 (34) | .45 | .002 | .0001 |
| Rectal threshold - urge to defecate, ml | 117 (29) | 123 (46) | .42 | 123 (45) | 125 (46) | .83 | .39 | .90 |
Values are in mmHg unless stated otherwise
Left lateral vs seated position
Anal pressures during squeeze were lower in the seated than the LL position in healthy women (P=.01) and in constipated patients (P<.0001). The threshold for the first sensation was greater, only in patients, in the seated than the LL position (P= 0.02).
Discriminant Utility of Rectoanal Pressures
Compared to constipated women with nBET, in constipated women with pBET, the (i) anal pressure at rest and during evacuation was greater in both positions (P ≤ .05), and (ii) the rectal pressure (P=.06 for LL and P=.003 for seated positions) and pressure increment (P≤.01 for both positions) during evacuation was also lower (Table 4). The RAG was greater (ie, less negative, P<.0001) in patients with nBET than pBET. In the seated position, the rectal threshold volume for urgency was greater in constipated women with pBET than nBET (P=.03).
Table 4.
Comparison of Rectoanal Sensorimotor Functions in Constipated Patients with Normal and Prolonged Rectal Balloon Expulsion Time.
| Left lateral position | Seated position | |||||
|---|---|---|---|---|---|---|
| Rectoanal parameters† | Constipation and normal BET (n=84) |
Constipation and prolonged BET (n=52) |
P-value‡ | Constipation and normal BET (n=84) |
Constipation and prolonged BET (n=52) |
P-value‡ |
| Rectoanal parameters | ||||||
| Anal pressure - rest, Manoview™ analysis | 85 (28) | 96 (27) | .03 | 98 (34) | 116 (31) | .002 |
| Anal pressure - squeeze, Manoview™ analysis | 194 (66) | 182 (67) | .31 | 189 (65) | 198 (59) | .37 |
| Anal pressure - Valsalva, Manoview™ analysis | 119 (43) | 132 (42) | .08 | 123 (49) | 150 (42) | .001 |
| Rectal pressure - rest, Manoview™ analysis | 7 (9) | 5 (8) | .08 | 27 (14) | 29 (17) | .43 |
| Rectal pressure - rest, new analysis | 8 (12) | 8 (9) | .88 | 31 (19) | 27 (13) | .12 |
| Rectal pressure – evacuation, Manoview™ analysis | 36 (27) | 27 (28) | .06 | 67 (33) | 50 (30) | .003 |
| Rectal pressure – evacuation, new analysis | 36 (27) | 26 (23) | .02 | 64 (30) | 48 (25) | .0009 |
| Rectal pressure increment – evacuation, Manoview™ analysis | 32 (27) | 20 (24) | .008 | 38 (29) | 24 (23) | .001 |
| Rectal pressure increment – evacuation, new analysis | 28 (23) | 18 (19) | .006 | 32 (21) | 21 (18) | .0008 |
| Anal pressure – evacuation, Manoview™ analysis | 78 (27) | 93 (26) | .002 | 86 (29) | 115 (34) | <.0001 |
| Anal pressure - evacuation, new analysis | 68 (27) | 84 (27) | .0007 | 70 (25) | 98 (33) | <.0001 |
| Change in anal pressures– evacuation, Manoview™ analysis | −5 (31) | −1 (15) | .29 | −7 (35) | −1 (17) | .11 |
| Change in anal pressures - evacuation, new analysis | 3 (19) | 12 (16) | .007 | −3 (21) | 9 (17) | .0006 |
| Rectoanal gradient- evacuation, Manoview™ analysis | −42 (30) | −65 (33) | <.0001 | −19 (35) | −64 (43) | <.0001 |
| Rectoanal gradient- evacuation, new analysis | −32 (29) | −59 (32) | <.0001 | −7 (31) | −50 (40) | <.0001 |
| Rectal threshold - first sensation, ml | 46 (20) | 52 (19) | .12 | 51 (24) | 57 (22) | .14 |
| Rectal threshold - desire to defecate, ml | 82 (32) | 88 (33) | .40 | 82 (30) | 94 (37) | .07 |
| Rectal threshold - urge to defecate, ml | 117 (43) | 132 (46) | .11 | 116 (43) | 137 (53) | .03 |
Values are in mmHg unless stated otherwise
For constipated patients with normal versus prolonged BET
Supplemental table 1 compares the diagnostic utility of various rectoanal parameters, agnostic to the underlying patterns, for discriminating between constipated patients with nBET and pBET. There are 3 salient observations. First, the RAG was the most useful of all parameters for discriminating between constipated patients with nBET and pBET. Second, for several parameters, the LR for discriminating between constipated patients with nBET and pBET were numerically greater, suggestive of greater diagnostic utility, with the new than the Manoview™ analysis. For example, for the gradient the LR for the new and Manoview™ analysis were respectively 6.2 and 3.1 in the LL and 7.8 and 4.8 in the seated position. Third, the diagnostic utility was different in the LL and seated positions. For example, the RAG measured with the new technique had a LR of 6.2 in the LL and 7.8 in the seated position for discriminating between constipated patients with nBET and pBET. Expressed differently, among all constipated women, the pre-test probability of having a DD was 38% (ie, 52 of 136 patients). Among constipated women with a more negative Manoview or new RAG in the LL position, the incremental probability of a DD was 21% and 35%. Hence, the post-test probability of a DD in women with an abnormal Manoview™ or new gradient was 59% and 73% respectively; in the seated positions, the corresponding values were 68% and 77%.
Rectoanal Patterns
As defined (Supplemental table 1), during evacuation, the anal pressure declined in anal relaxation (AR) and increased in paradoxical contraction (PC) (Table 5, Figure 2). Transmission is characterized by transmission of pressure changes from the rectum to the anus while the minimal change (MC) pattern does not satisfy the criteria for any other pattern.
Table 5.
Rectoanal pressures analyzed with the new method in constipated patients with normal and prolonged BET †
| Pattern† | Balloon expulsion time | N (%) | Rectal pressure change during evacuation‡ (mmHg) | Anal pressure change during evacuation‡ (mmHg) | Rectoanal gradient during evacuation (mmHg) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Left lateral position | Seated position |
Left lateral position |
Seated position |
Left lateral position |
Seated position |
Left lateral position | Seated position |
||
| Minimal change | Normal | 43 (60%) | 36 (55%) | 20 (12, 29) | 24 (18, 34) | 3 (−4, 6) | 0 (−7, 14) | −32 (−48, −3) | −6 (−33, 11) |
| Prolonged | 29 (40%) | 30 (45%) | 8 (2, 14)* | 10 (6, 21)* | 2 (−1, 8) | 3 (−3, 8) | −54 (−69, −38)** | −49 (−68, −18)*** | |
| Anal Relaxation | Normal | 14 (93%) | 23 (85%) | 19 (12, 24) | 22 (17, 32) | −13 (−24, −3) | −17 (−22, −7) | −46 (−60, −37) | −15 (−32, 12) |
| Prolonged | 1 (7%) | 4 (15%) | NA | 16 (12, 21) | NA | −3 (−8, 9) | NA | −37 (−45, −32)*** | |
| Paradoxical contraction | Normal | 24 (52%) | 16 (47%) | 32 (14, 65) | 45 (30, 56) | 16 (10, 24) | 12 (0, 28) | −29 (−61, −19) | 1 (−16, 14) |
| Prolonged | 22 (48%) | 18 (53%) | 21 (7, 40) | 23 (12, 38)* | 19 (11 , 26) | 17 (8, 20) | −76 (−94, −58)*** | −57 (−104, −36)*** | |
| Transmission | Normal | 3 (100%) | 9 (100%) | 44 (26, 59) | 72 (56, 74) | 0 (−20, 1) | −12 (−49, 42) | 9 (2, 42) | 16 (12, 39) |
| Prolonged | 0 | 0 | NA | NA | NA | NA | NA | NA | |
Values are median (interquartile range),
(maneuver-baseline),
P < 0.05,
P ≤ 0.01,
P ≤ 0.001 for normal versus prolonged BET in the same position. NA – Not applicable because either there were no patients or only 1 patient in that category
Figure 2.
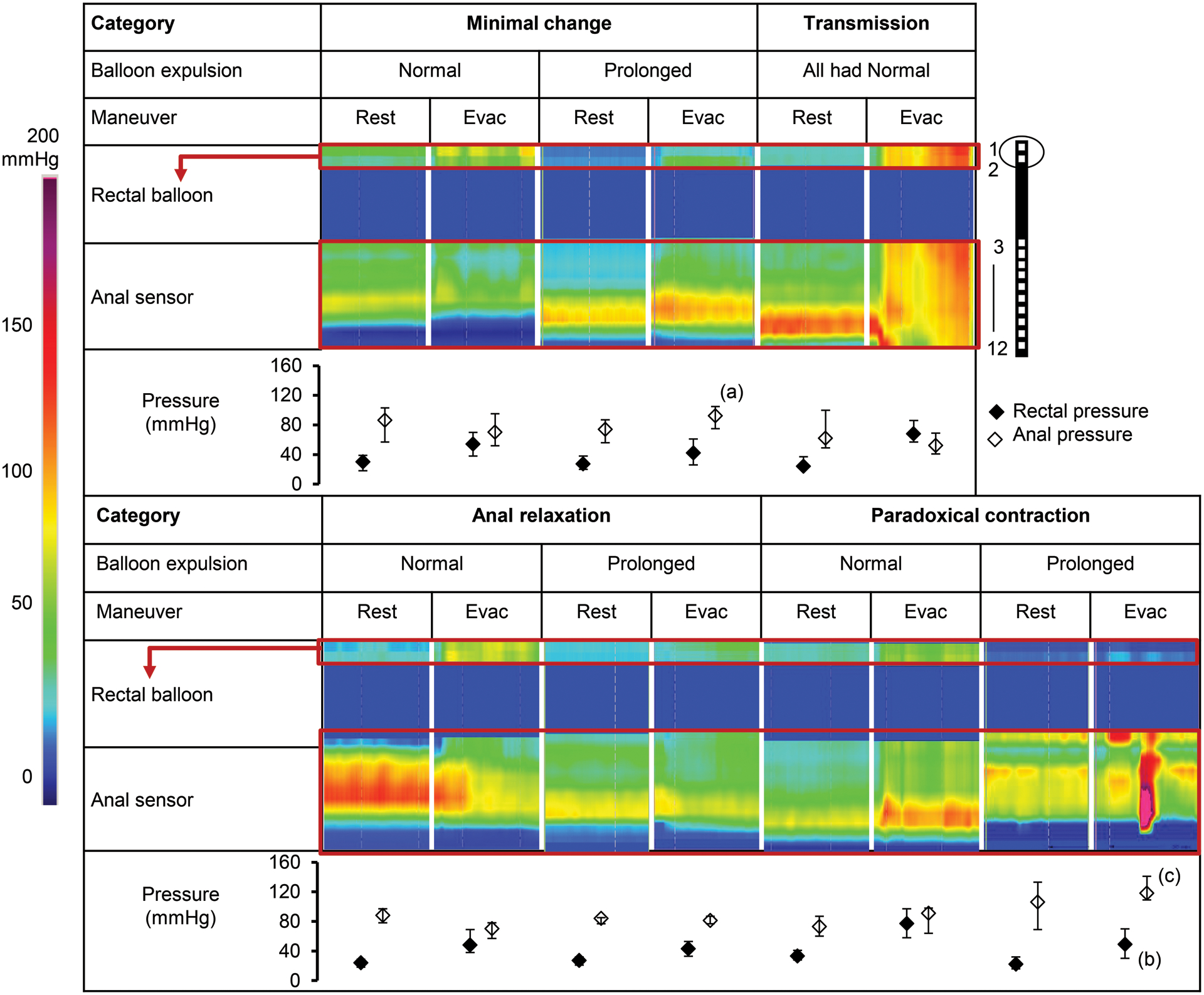
Representative images and summary data (median and inter-quartile values) of rectoanal pressures at rest and during evacuation in the seated position in the four patterns. Rectoanal pressures were measured by a 12-sensor catheter depicted in the cartoon on the top right. The rectoanal gradients are provided in Table 5. Observe the caudal transmission of pressure from the rectal balloon throughout the anal canal in the transmission pattern. a P < 0.05, b P ≤ 0.01, c P ≤ 0.001 for comparison of rectal or anal pressure during evacuation in patients with normal versus prolonged BET in the same pattern.
In the LL position, 33 (52%) heathy women had MC, 19 (30%) had AR, and 12 (18%) had PC. In the seated position, 32 (50%) had MC, 26 (41%) had AR and 6 (9%) had PC. Table 5 provides the distribution of these patterns in constipated patients. Forty nine percent of patients had the same pattern in both positions (Supplemental figure 1). The remainder had different patterns in the LL and seated positions.
Among constipated patients, these patterns were associated with pBET in the LL (P=.005) and seated positions (P=.0001). In both positions, all patients with transmission had nBET (Table 5). In the LL position, only 7% with AR but 40% of patients with MC and 48% with PC had pBET. In the seated position, 15% (AR), 53% (PC), and 45% (MC) of patients had pBET.
Integrated Assessment of Rectoanal Pressures and Patterns
In contrast to Supplemental table 1, Table 5, Supplemental table 2, and Figure 3 consider an integrated assessment of rectoanal pressures and patterns to answer related but different questions. In Figure 2, observe that the difference between rectal and anal pressures, which reflects the RAG, was wider in patients with pBET than nBET. In each pattern, the RAG was significantly lower (ie, more negative) in patients with pBET than nBET (Table 5). Among patients with the MC pattern in the seated position, the median (range) of values for the gradient in patients with nBET and pBET were −6 (−33, −11) and −49 (−68, −18) mmHg respectively. For example, among patients with the MC pattern, a RAG less than −30 mm Hg was 65% sensitive and 82% specific for discriminating between nBET and pBET while a gradient less than −50 mmHg had a sensitivity of 65% and a specificity of 81% in the LL position. In patients with PC, a RAG less than −15 mm Hg was 75% sensitive and 77% specific in the seated position while a gradient less than −50 mm Hg had a sensitivity of 67% and a specificity of 78% in the LL position.
Figure 3.
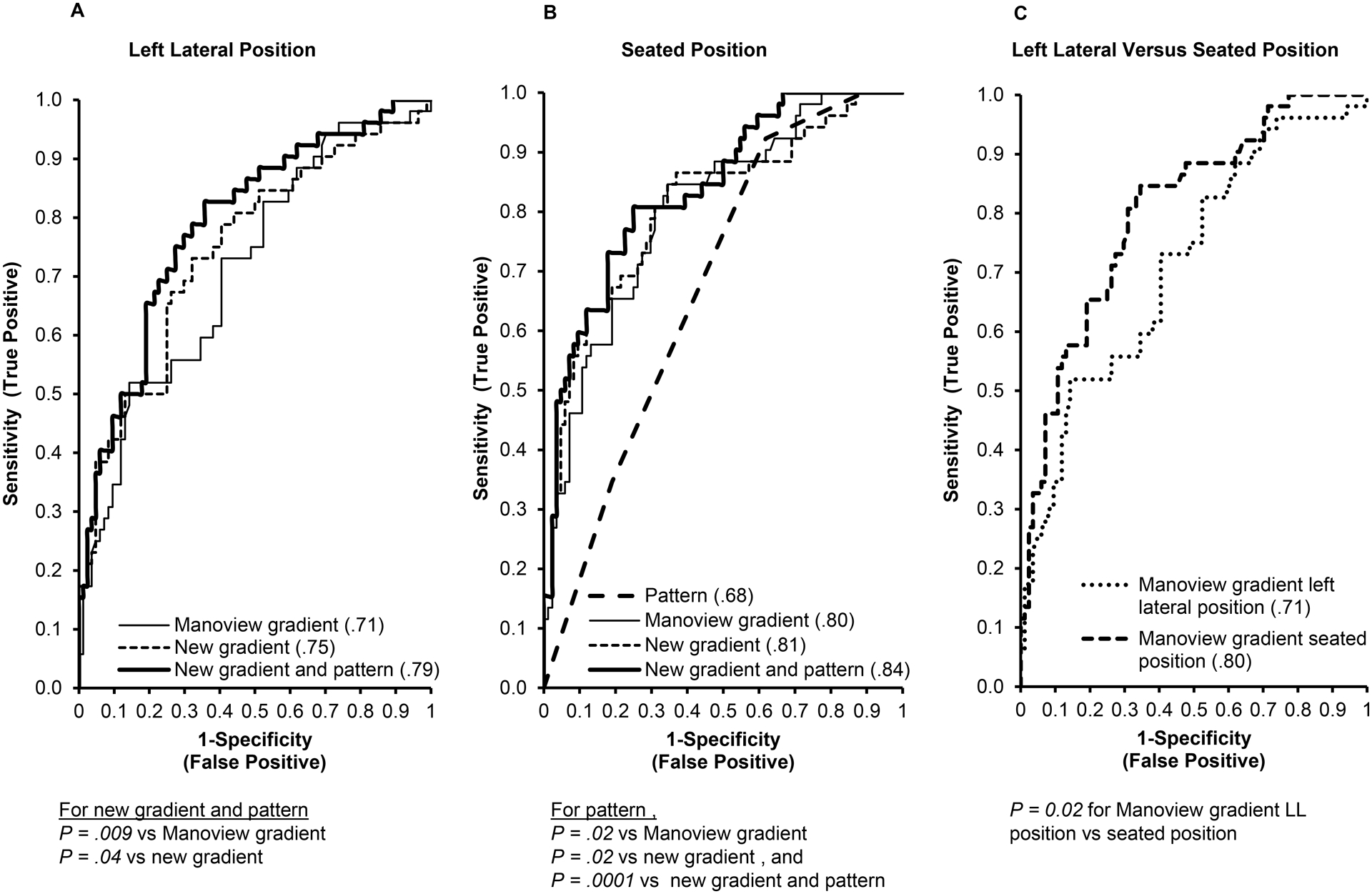
Discriminating between constipated patients with normal and prolonged BET. The AUC values for the corresponding ROC curve are provided in parentheses. In the LL position (A), the AUC for pattern and new gradient was greater than the AUC for the Manoview™ (P = .009) and new (P = .04) gradients. In the seated position (B), the AUCs for Manoview™ gradient (P = .02), new gradient (P = .02), and pattern plus gradient (P = .0001) were greater than the pattern alone. The AUC for the Manoview™ gradient in the seated position was greater (P = .02) than the AUC for the corresponding gradient in the LL position (C).
In the Cox proportional regression models, a higher (ie, more positive) gradient was associated with a shorter (ie, more normal) BET in the LL and seated positions (Supplemental table 2). The pattern was also associated with the BET (P=.0001). Compared to the reference group (ie, MC pattern), AR was associated with a shorter BET in the LL and seated positions. The transmission pattern predicted a shorter BET only in the seated position. Finally, in the combined model that incorporated the gradient and the pattern, the gradient and AR independently predicted a shorter BET in the LL and seated positions.
The ROC curves, which were derived from the logistic regression models, compared the effects of position and the method of analysis for discriminating between constipated patients with nBET and pBET. In the LL position, the combined analysis (ie, pattern and new RAG, AUC=0.79) was more effective than the Manoview™ (P=.009) and separately the new (P=.04) gradients for discriminating between constipated patients with nBET and pBET (Figure 3A). In the seated position, the combination (ie, pattern and new gradient) was not different from the Manoview™ gradient alone (Figure 3B). Finally, the Manoview™ gradient in the seated position was more effective (P=0.02) than the corresponding LL gradient for discriminating between nBET and pBET (Figure 3C).
Discussion
We modified the process for conducting and analyzing anorectal HRM and compared the existing and new approaches for discriminating between constipated patients with nBET and pBET. We studied 200 participants (i.e. 64 controls and 136 constipated patients); 38% of patients had a DD. There are 4 key observations. First, extending previous studies,13–15 the rectal pressure, and to a lesser extent, anal pressure at rest and during evacuation were greater in the seated position than in the LL position, which affords a more physiological assessment of defecation. Second, with the Manoview™ analysis, the seated gradient was more useful than the LL gradient for discriminating between patients with nBET and pBET, which underscores the benefits of conducting HRM in the seated position. Hence, HRM should ideally be performed in the seated position. Third, by contrast to the Manoview™ analysis, which only relies on rectoanal pressures during evacuation, the new analysis employs a two-step system that incorporates the pattern (ie, rectoanal pressure topography) and the RAG during evacuation to determine the likelihood of a DD. Four, exemplifying the advantages of the new analysis, the combined assessment of new gradient and pattern was significantly more effective than the Manoview™ analysis alone in the LL position for differentiating between constipated patients with nBET and pBET. While the Rao criteria were developed with non-high resolution manometry, the new classification in this study was developed with HRM.28 The Ratuapli classification system, which was based on HRM, is very useful for understanding the pathogenesis of DD but cannot be readily used for interpreting HRM studies in clinical practice11. The integrated assessment of patterns and the rectoanal gradient in the current classification provide a more robust and user-friendly approach for quantifying the likelihood of a DD that can be implemented in clinical practice. The differences in AUC values between techniques for discriminating between constipated patients without and with DD are statistically significant but misleadingly small. Indeed, because an AUC value of 0.5 is no better than chance, it is only the area above the diagonal of the AUC curve (ie, values that are greater than 0.5) that truly counts. Hence an increase in the AUC from 0.71 (ie, for Manoview gradient in the LL position) to 0.84 (ie, for the new gradient and pattern in the upright position) is a difference of 0.13 units, which represents a fractional improvement of 0.26 (ie, 0.13/0.5), that is, 26% of the total improvement possible. This AUC of 0.84 for discriminating between constipated patients with nBET and pBET is numerically greater than the AUC of 0.64 for discriminating between healthy controls and all constipated patients (ie, with and without DD) LL HRM in a prior study.10 Expressed differently, in this study, at a specificity of 80%, the new analysis (ie, combination of RAG and pattern) was 73% sensitive for discriminating between constipated patients with nBET and pBET versus a sensitivity of 46% at a specificity of 80% for discriminating between controls and functional constipation patients in the prior study.10
New analysis
Overcoming the limitations of the Manoview™ analysis detailed earlier, the new analysis uses the same anal sensors to estimate the RAG in all patients and for a longer duration (ie, between 5–15 seconds after the onset of evacuation). The new analysis also employs a two-tiered approach that incorporates the overall pattern and the RAG. [The RAG is not directly used to define the patterns.] These two parameters are derived from the raw data that can be extracted from the program. Identifying the pattern is useful because the proportion of patients who have pBET differs among the patterns. For example, in the seated position, the proportion of patients with pBET ranges from 0% in patients with anal transmission, 15% with AR, 53% with PC, and 45% with MC. In the LL position, only 7% of patients with AR and none with transmission had pBET. Transmission is an uncommon pattern characterized by rectoanal pressurization, which implies that the anal canal is at least partly open. Hence, among patients with transmission or AR, the pattern alone is perhaps sufficient to exclude pelvic floor dysfunction. With other patterns (e.g. MC), the pattern alone is not useful for predicting the risk of pBET. However, within every pattern, the RAG is useful for discriminating between patients with nBET and pBET. The threshold for the RAG that separates patients with nBETs and pBETs differs among the patterns.
Clinical implications
The new analysis is not complex but requires 15–20 minutes, which may be challenging in clinical practice. By comparison, implementing seated HRM with the Manoview™ analysis may be simpler and offers a discriminant utility (ie, AUC of 0.80) that is comparable to the most effective approach (ie, seated HRM with new analysis of gradient and pattern), which has an AUC of 0.84, for discriminating between constipated patients with nBET and pBET. Anecdotally, catheter damage was comparable for left lateral HRM and seated HRM with a clip to prevent catheter displacement. Since false-positive or negative anorectal test results are inevitable,6 the Rome criteria recommend that at least two abnormal tests be used to diagnose DD.1 Currently, the utility of LL HRM for diagnosing DD is limited by the considerable overlap in the RAG between healthy people and DD.7, 12 By comparison, the HRM performed in the seated position with or without the new analysis is more useful for diagnosing DD.
The algorithm in Figure 4 incorporates these findings to integrate HRM and the BET for predicting a DD. In both positions, transmission and AR are generally associated with a nBET. In such patients, when the BET is also normal, further testing (eg, defecography) is probably unnecessary unless warranted, for example, when the clinical features suggest a significant rectocele. Among patients with MC or PC, the value of the RAG relative to the threshold specified in Figure 4 is useful for estimating the likelihood of a DD. When the gradient is greater (ie, less negative) than those thresholds and the BET is normal, the likelihood of a DD is probably low and additional tests seem unnecessary. When the gradient is lower (ie, more negative) than the thresholds shown in Figure 4 and the BET is prolonged, the likelihood of a DD is probably high and additional tests seem unnecessary. Intermediate scenarios likely warrant further testing. By enhancing the utility of HRM for diagnosing DD, we anticipate that these findings will reduce the need for barium defecography, which entails radiation exposure and is not available at many centers.
Figure 4.
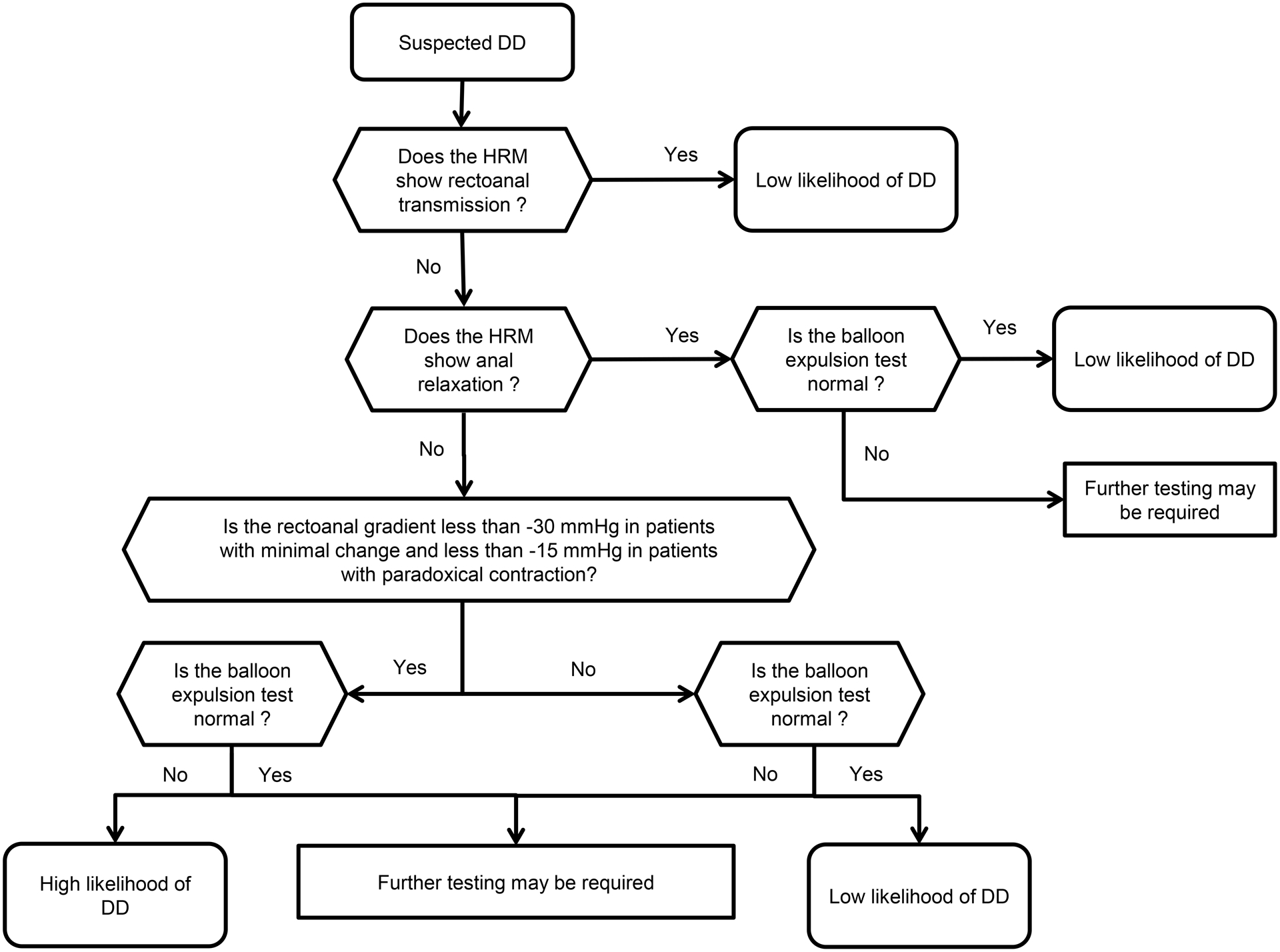
Algorithm for diagnosing defecatory disorders in the upright position. Among patients with transmission or AR, in whom the risk of a DD is low, a normal BET effectively excludes a DD. In the other patterns, the rectoanal gradient is useful for estimating the likelihood of a DD and guiding the need for further tests. By substituting the values for the rectoanal gradient (ie, −50 instead of −30mmHg in patients with minimal change and −50 instead of −15mmHg in patients with paradoxical contraction), this algorithm can be used in the left lateral position.
Limitations
These observations need to be confirmed with the same technique and with other HRM catheters.12 Absent a gold-standard diagnostic test for DD, this study relied on the BET, and relied on a cutoff of 60 seconds, which is relatively sensitive and specific for identifying pelvic floor dysfunction and widely used in clinical practice.1, 23, 24 However, defecography may demonstrate a DD in some patients with nBET and vice versa.5, 6 Hence, future studies should compare the diagnostic utility of LL and seated HRM and the existing and new analyses for DD diagnosed by abnormal defecography. These studies should also evaluate whether the patterns predict the response to pelvic floor retraining by biofeedback therapy.
Conclusions
Seated HRM, and to a lesser extent, LL HRM analyzed with a different approach, are more useful than conventional LL HRM for discriminating between constipated patients with nBET and pBET.
Supplementary Material
Comparison of pressure patterns in the left lateral and seated positions. The colors inside the circle denote the pattern in the seated position. The colors of the symbols represent the pattern in the left lateral position. Symbols on and inside the circle perimeter represent a normal BET; symbols on the perimeter had the same pattern in both positions while symbols inside the perimeter had different patterns in the left lateral and seated positions. Participants with a prolonged BET are shown outside the circle.
Study highlights.
What is known
Anorectal high resolution manometry (HRM) is widely used to diagnose defecatory disorders in constipated patients.
However, HRM in the left lateral position is of limited utility for diagnosing defecatory disorders.
Among healthy people and constipated patients, rectoanal pressures are greater in the seated than the left lateral (LL) position.
What is new here
Compared to LL manometry and the existing analysis, seated manometry and a new method to analyze rectoanal pressures are each more effective for diagnosing DD in constipated patients.
Instead of the left lateral position, anorectal HRM ideally should be performed in the more physiological seated position, and analyzed by a two-tier approach which incorporates the overall pattern followed by the rectoanal gradient.
Financial support:
This study was supported by USPHS NIH Grant R01 DK78924.
Abbreviations
- AR
anal relaxation
- BET
balloon expulsion time
- BMI
body mass index
- DD
defecatory disorder
- HR
Hazards ratio
- HRM
high-resolution manometry
- IBS
irritable bowel syndrome
- LL
left lateral
- MC
minimal change
- PC
paradoxical contraction
- ROC
Receiver operating characteristic
Footnotes
Potential competing interests: Dr. Bharucha holds a patent jointly with Medtronic Inc for the anorectal manometry catheter fixation device used in this study and a patent for another anorectal manometry catheter. Other authors do not have any conflicts of interest.
References
- 1.Rao SS, Bharucha AE, Chiarioni G, et al. Functional Anorectal Disorders. Gastroenterology 2016;25:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carrington EV, Scott SM, Bharucha A, et al. Expert consensus document: Advances in the evaluation of anorectal function. Nature Reviews Gastroenterology & Hepatology 2018;15:309–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bharucha AE, Wald A. Chronic Constipation. Mayo Clinic Proceedings 2019;94:2340–2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bharucha AE, Lacy BE. Chronic Constipation: Mechanisms, Evaluation and Management. Gastroenterology 2020;158:1232–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Palit S, Thin N, Knowles CH, et al. Diagnostic disagreement between tests of evacuatory function: a prospective study of 100 constipated patients. Neurogastroenterology and Motility 2016;28:1589–98. [DOI] [PubMed] [Google Scholar]
- 6.Prichard DO, Lee T, Parthasarathy G, et al. High-resolution Anorectal Manometry for Identifying Defecatory Disorders and Rectal Structural Abnormalities in Women. Clinical Gastroenterology & Hepatology 2017;15:412–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Basilisco G, Bharucha AE. High-resolution anorectal manometry: An expensive hobby or worth every penny? Neurogastroenterology & Motility 2017;29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heinrich H, Sauter M, Fox M, et al. Assessment of Obstructive Defecation by High-Resolution Anorectal Manometry Compared With Magnetic Resonance Defecography. Clinical Gastroenterology & Hepatology 2015;13:1310–1317.e1. [DOI] [PubMed] [Google Scholar]
- 9.Prichard D, Harvey DM, Fletcher JG, et al. Relationship Among Anal Sphincter Injury, Patulous Anal Canal, and Anal Pressures in Patients With Anorectal Disorders. Clinical Gastroenterology and Hepatology 2015;13:1793–1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grossi U, Carrington EV, Bharucha AE, et al. Diagnostic accuracy study of anorectal manometry for diagnosis of dyssynergic defecation. Gut 2016;65:447–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ratuapli S, Bharucha AE, Noelting J, et al. Phenotypic Identification and Classification of Functional Defecatory Disorders Using High Resolution Anorectal Manometry Gastroenterology 2013;144:314–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee TH, Bharucha AE. How to Perform and Interpret a High-resolution Anorectal Manometry Test. Journal of neurogastroenterology and motility 2016;22:46–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnson GP, Pemberton JH, Ness J, et al. Transducer manometry and the effect of body position on anal canal pressures. Diseases of the Colon & Rectum 1990;33:469–75. [DOI] [PubMed] [Google Scholar]
- 14.Rao SSC, Kavlock R, Rao S. Influence of body position and stool characteristics on defecation in humans. American Journal of Gastroenterology 2006;101:2790–2796. [DOI] [PubMed] [Google Scholar]
- 15.Wu GJ, Chen JDZ. Anorectal manometry-Should it be performed in a seated position? A reply to the Letter. Neurogastroenterology & Motility 2019;31:e13504. [DOI] [PubMed] [Google Scholar]
- 16.Wu GJ, Xu F, Lin L, et al. Anorectal manometry: Should it be performed in a seated position? Neurogastroenterology & Motility 2017;29:05. [DOI] [PubMed] [Google Scholar]
- 17.Rao SS, Leelasinjaroen P, Amieva-Balmori M, et al. 771 Characterization of Dyssynergia Phenotypes With High Resolution Anorectal Manometry (HRAM). Gastroenterology 2016;150:S158–S159. [Google Scholar]
- 18.Carrington EV, Heinrich H, Knowles CH, et al. The international anorectal physiology working group (IAPWG) recommendations: Standardized testing protocol and the London classification for disorders of anorectal function. Neurogastroenterol Motil 2020;32:e13679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Babaei A, Szabo A, Yorio SD, et al. Pressure exposure and catheter impingement affect the recorded pressure in the Manoscan 360TM system. Neurogastroenterology & Motility 2018;09:09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pandolfino JE, Fox MR, Bredenoord AJ, et al. High-resolution manometry in clinical practice: utilizing pressure topography to classify oesophageal motility abnormalities. Neurogastroenterology & Motility 2009;21:796–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Longstreth GF, Thompson WG, Chey WD, et al. Functional bowel disorders. Gastroenterology 2006;130:1480–91. [DOI] [PubMed] [Google Scholar]
- 22.Oblizajek NR, Gandhi S, Sharma M, et al. Anorectal pressures measured with high-resolution manometry in healthy people—Normal values and asymptomatic pelvic floor dysfunction. Neurogastroenterology and Motility : the official journal of the European Gastrointestinal Motility Society 2019:e13597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ratuapli S, Bharucha AE, Harvey D, et al. Comparison of rectal balloon expulsion test in seated and left lateral positions. Neurogastroenterology and Motility 2013;25:e813–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mazor Y, Prott G, Jones M, et al. Anorectal physiology in health: A randomized trial to determine the optimum catheter for the balloon expulsion test. Neurogastroenterology & Motility 2019;31:e13552. [DOI] [PubMed] [Google Scholar]
- 25.Vollebregt PF, Rasijeff AMP, Pares D, et al. Functional anal canal length measurement using high-resolution anorectal manometry to investigate anal sphincter dysfunction in patients with fecal incontinence or constipation. Neurogastroenterol Motil 2019;31:e13532. [DOI] [PubMed] [Google Scholar]
- 26.McGee S Simplifying likelihood ratios. Journal of General Internal Medicine 2002;17:646–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988;44:837–45. [PubMed] [Google Scholar]
- 28.Rao SS, Mudipalli RS, Stessman M, et al. Investigation of the utility of colorectal function tests and Rome II criteria in dyssynergic defecation (Anismus). Neurogastroenterology & Motility 2004;16:589–96. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Comparison of pressure patterns in the left lateral and seated positions. The colors inside the circle denote the pattern in the seated position. The colors of the symbols represent the pattern in the left lateral position. Symbols on and inside the circle perimeter represent a normal BET; symbols on the perimeter had the same pattern in both positions while symbols inside the perimeter had different patterns in the left lateral and seated positions. Participants with a prolonged BET are shown outside the circle.


