Abstract
Objective:
To first review and critically discuss published evidence on psychosocial stressors, stress, and asthma in adolescents, and then discuss potential future directions in this field.
Data Sources:
National Library of Medicine (Pubmed).
Study Selections:
A literature search was conducted for human studies on stressors or stress and asthma between 2000 and 2020. Studies that were published in English, contained a full text, and included adolescents were considered for inclusion in this review.
Results:
Compared with the available body of evidence in children and adults, relatively few studies have published in adolescents. Current evidence suggests that exposure to stressors (at the individual, family, and community levels) or stress (acute and chronic) are associated with asthma and worse asthma outcomes, but such evidence must be cautiously interpreted due to limitations in the design or analytical approach of published studies.
Conclusion:
Future large studies with a prospective design should determine whether and how stressors or stress cause or worsen asthma in adolescents. At present, clinicians should assess exposure to stressors (e.g., violence or abuse) and screen for anxiety and depressive disorders when caring for adolescents with asthma, providing referrals to social workers or mental health professionals when appropriate. Public health policies are needed to reduce psychosocial stressors such as gun violence and racism in adolescents.
Keywords: violence, stress, asthma, adolescents
INTRODUCTION
Asthma is the most common chronic disease in children and adolescents. In the United States, the estimated prevalence of asthma is higher in adolescents aged 12 to 17 years (9.9%) than in younger children (3.8% to 8.1%) or adults (7.6%) (1). Adolescents with asthma account for a substantial proportion of emergency department (ED) visits (2) and school absences among youth with asthma (3).
Adolescence is a challenging life stage because of the occurrence of physical and psychological changes in a short period of time (4). Adolescents start to develop autonomy and personal decision-making (5), while seeking independence from their parents and strengthening relationships with their peers (6). Cognitively, adolescents move from concrete thinking to abstract, multidimensional, hypothetical and planned thinking (7). All these changes make handling a chronic disease like asthma a challenge, as evidenced by their poor understanding of the disease and poor adherence to treatment (8–11). Moreover, adolescents start facing or perceiving an increased amount of stressors that may be prove difficult to handle (12).
Psychosocial stressors include poverty, exposure to violence, racism and discrimination. Such stressors can affect adolescents at the individual, family, and community levels. Stressors may be acute, when they are time limited or transient, or chronic, when they cannot be resolved and pervade an individual’s life leading to changes in identity or social roles (13). Both psychosocial stressors and (acute severe or chronic) stress have been associated with increased asthma prevalence and worse asthma outcomes in multiple studies in children and adults (14), with fewer studies focusing on the vulnerable adolescent population. The mechanisms underlying the link between stressors or stress and asthma are insufficiently understood but likely include direct and indirect effects (14). Stress may directly affect epigenetic regulation of gene expression, immune responses, and the neuroendocrine, autonomic and immune systems (15, 16). For example, acute stress can activate the hypothalamic-pituitary-adrenocortical (HPA) axis and sympathetic and adrenomedullary systems, disrupting their normal balance and increasing the circulating levels of cortisol, epinephrine and norepinephrine, which can have anti-inflammatory and bronchodilator effects (17). However, after prolonged or chronic exposure to stress, the effector receptors can be downregulated and an imbalance between glucocorticoids and catecholamines can take place, establishing a pro-inflammatory environment with a hyporesponsive HPA axis (16, 18) and reduced response to therapies such as short-acting bronchodilators (16, 19, 20) (see Figure 1). Chronic stress may thus enhance airway inflammation in response to environmental and infectious exposures, leading to asthma exacerbations (16, 21, 22).
Figure 1.
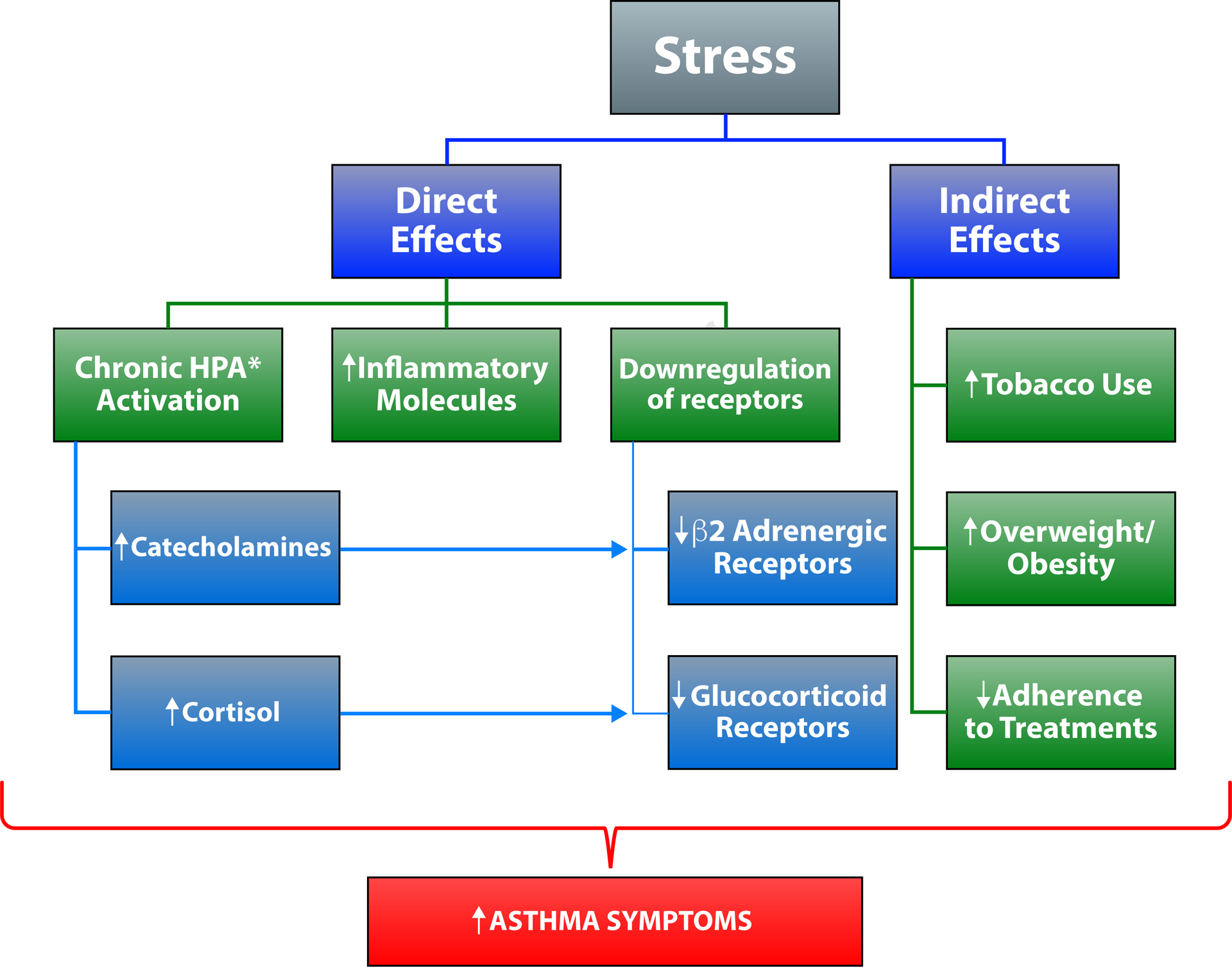
Proposed pathways for the effects of stress on asthma.
Footnote: *Hypothalamic pituitary adrenal axis.
Stress or stressors could also affect asthma through indirect mechanisms, including tobacco use, overweight or obesity due a poor diet and limited physical activity, and reduced adherence to treatment (see Figure 1). Moreover, stress or stressors may interact with other risk factors for asthma, such as indoor and outdoor pollutants. A more detailed discussion of the possible direct and indirect mechanisms underlying the link between stress and asthma is beyond the scope of this manuscript, and thus the reader is referred to recent reviews of that topic (14–16, 23).
In this review, we will first summarize and critically review the available epidemiologic evidence on psychosocial stressors and stress on asthma in adolescents, focusing on stressors at the individual, family and community levels (see Figure 2). We will then discuss what is needed to advance our knowledge of whether and how stressors or stress affect asthma during adolescence.
Figure 2.
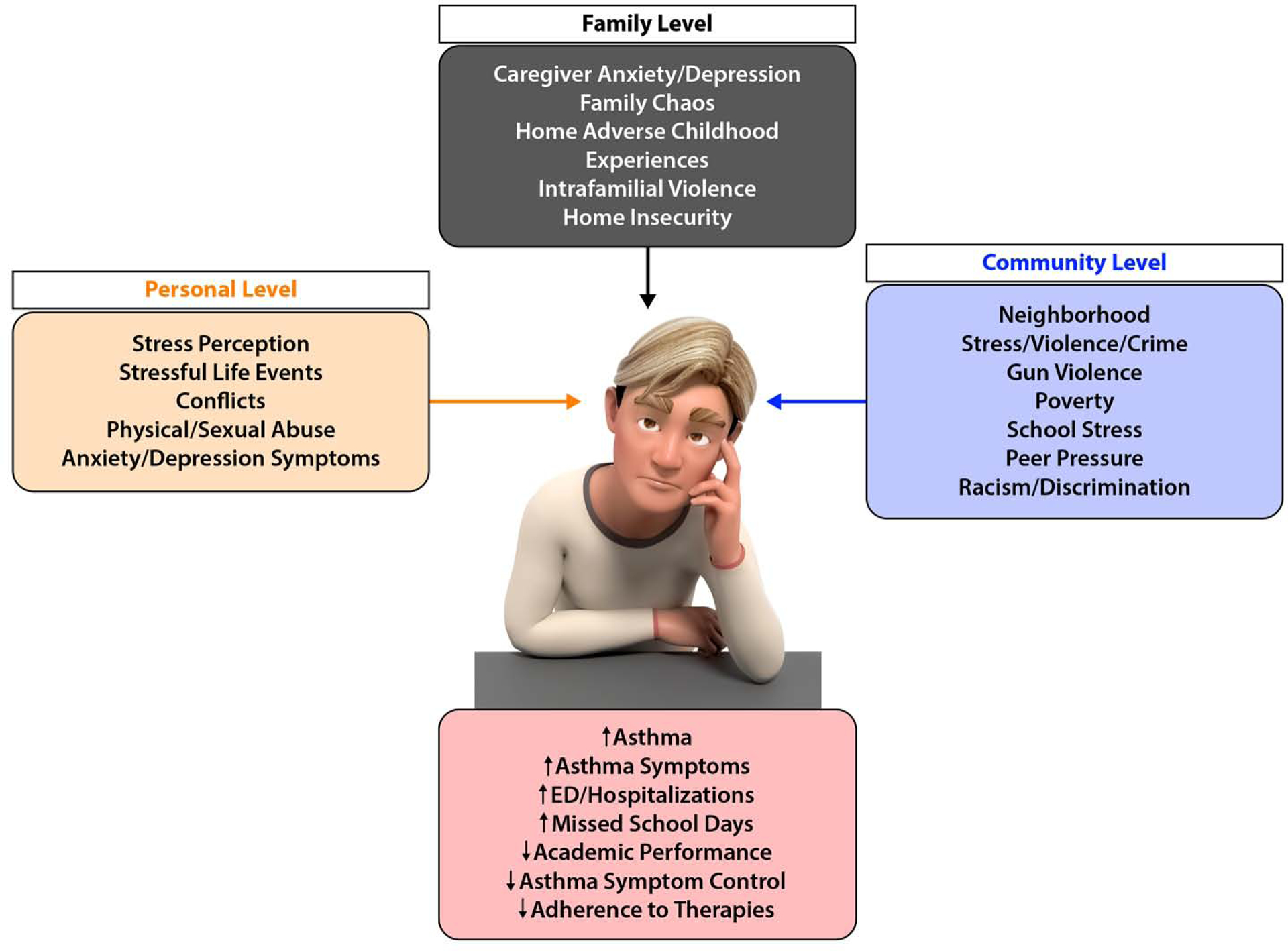
Psychosocial stressors at the personal, family and community levels.
PSYCHOSOCIAL STRESSORS, STRESS, AND ASTHMA
Individual-level stressors
Adolescents are often exposed to stressful situations. A prospective study assessed stressful life events between ages 15 and 16 years and both asthma at age 16 years and incident asthma (between ages 18 and 29 years) in 318 (25.5%) of 1,246 subjects enrolled in a birth cohort study (24). Among 16-year-old adolescents without a diagnosis of asthma, males who had been highly exposed to stressful life events in the prior year had higher odds of having concurrent asthma at age 16 years than those who were not highly exposed (odds ratio [OR]=3.26, 95% confidence interval [CI]=0.88 to 12.15), and this association was essentially unchanged after adjustment for emotional support (24). Similar but non-significant results were obtained for high exposure to stressful life events and incident asthma between ages 18 and 29 years in males. Although promising, those findings must be cautiously interpreted due to potential selection bias, no evidence of a significant interaction between sex and life events on incident asthma, and limited statistical power.
In adolescents with asthma, perceived stress has been associated with asthma symptoms. A prospective study of 20 low-income Hispanic adolescents with asthma utilized a real-time data capturing strategy via smartphone to survey asthma symptoms in children at set intervals during the day and after inhaler use (25). In that study, stressful situations such as disagreements with parents, teasing, or arguing was associated with worsening asthma symptoms in the hours following the stressful events. Moreover, more severe asthma symptoms were reported by the participants when they were outdoors, perhaps due to exposure to pollutants. Similar findings were reported in a study of 61 children ages 10 to 20 years (38 of whom had asthma), which showed that fractional exhaled nitric oxide (FeNO) increased ~45 minutes after an acute stressor (a family conflict discussion), but only in children with asthma and low socioeconomic status (SES) (26). In that study, the acute stressor was not significantly associated with pulmonary function. In a separate cross-sectional study of 806 children and adults with asthma, 510 (63.3%) reported having at least one non-respiratory symptom (most commonly, anxiety, headache, and palpitations) preceding an asthma attack, particularly among those with moderate to severe asthma (27). Although the studies discussed above were limited by cross-sectional design (26, 27), small sample size (25, 26), or lack of adjustment for confounders such as pollutants (25, 27), the notion that repeated acute stressful situations may exacerbate airway inflammation and trigger asthma symptoms deserves further investigation.
Chronic stress may also worsen asthma by reducing response to short-acting bronchodilators. In a cross-sectional study of three ethnically diverse cohorts of children and adolescents, high levels of chronic stress were significantly associated with reduced bronchodilator response (BDR) (20). In that study, a meta-analysis of genotypic data from 2,741 children and adolescents with asthma from seven different cohorts showed that a single nucleotide polymorphism (rs34548976) in the gene for adenylate cyclase activating polypeptide 1 receptor type 1 (ADCYAP1R1) was associated with reduced BDR (20). In a cohort of Puerto Rican children and adolescents, SNP rs34548976 was shown to be associated with reduced BDR only in subjects with high levels of chronic stress, but this SNP-by-stress interaction could not be replicated in other cohorts, as they had no data on chronic stress. Of note, SNP rs34548976 was also associated with reduced expression of the gene for the β2-adrenergic receptor (ADRB2) in CD4+ lymphocytes from children and adults with asthma. Taken together, those results suggest that chronic stress could lead to down-regulation of ADRB2 through persistent secretion of catecholamines in genetically susceptible individuals. Although promising, those findings need to be examined in future prospective studies.
Exposure to violence can lead to both acute and chronic stress in adolescents. In a cross sectional study of Puerto Ricans aged 6 to 14 years (a high-risk group for asthma), each 1-point increment in a scale for lifetime exposure to violence was associated with 10% excess odds of asthma after adjusting for potential confounders (95% CI for OR=1.0 to 1.12) (28). Interestingly, exposure to violence remained significantly associated with asthma after adjusting for chronic stress (29), which may be explained by the effects of risk factors correlated with violence (e.g., outdoor pollutants, healthcare quality) or unmeasured pre- or peri-natal stress. Future well-designed longitudinal studies should further assess these results.
Physical or sexual abuse during childhood or adolescence has been linked to asthma (30, 31). In a cross-sectional study of Puerto Rican children and adolescents, a history of physical or sexual abuse in the prior year was associated with asthma, medication use for asthma, and healthcare utilization for asthma (32). A subsequent 16-year prospective study of 28,456 African American women aged 21 to 69 years showed that self-reported physical abuse during childhood was significantly associated with an increased risk of new-onset asthma, particularly among those who reportedly felt in danger inside their home during childhood (33). In a separate study of Australian young adults, emotional abuse between birth and age 14 years was significantly associated with asthma by age 21 years, even after adjusting for cigarette smoking and other forms of childhood maltreatment (34). However, no dose-response was shown for this association. Despite limitations such as cross-sectional design, retrospective assessment of abuse, or lack of data on potential confounders, findings from these reports merit further examination in prospective studies.
Anxiety disorders or anxiety symptoms can be markers or a consequence of chronic stress. Moreover, anxiety disorders or symptoms may cause or be caused by asthma. In a meta-analysis of data from cross-sectional studies in over 7,000 children and adolescents, the pooled prevalence of anxiety disorders in youth with asthma was as high as 22.7%, which is up to thrice as high as that reported in healthy individuals (35). A database-driven analysis of one-year information in >65,000 subjects with asthma (aged 6 to 21 years) in Massachusetts showed that anxiety and/or depression was associated with 1.2 times to 1.8 times higher rates of ED visits for asthma (95% CI for the relative risk (RR) for anxiety=1.1 to 1.35 and 95% CI for the RR for anxiety and depression=1.6 to 2.0) (36). Consistent with some of those findings, a one-year study of 86 inner-city Black adolescents with persistent asthma showed that probable anxiety at baseline was significantly associated with ED visits for asthma and persistent uncontrolled asthma, but not with lung function or FeNO. Of note, however, 22% of the participants in that study were lost to follow up (37). In a separate study, adolescents with asthma were more likely to report depressive symptoms, cigarette smoking and cocaine use than those without asthma, and adolescents with asthma and suicidal ideations were also more likely to report substance abuse (38). A major limitation of the studies referenced above (35–38) is lack of data on medication use or medication adherence, as poorly controlled asthma may be more likely to lead to anxiety or depression than well-controlled asthma. Indeed, such hypothesis is supported by findings from a cross-sectional study of a convenience sample of 140 children and adolescents with and without asthma, which found no significant difference in anxiety or depression between subjects with mostly well-controlled asthma (on inhaled corticosteroids) and controls (39).
Finally, psychosocial interventions to educate youth on how to deal with stressful situations may reduce asthma symptoms, particularly in economically disadvantaged individuals. In a cross-sectional study of 308 children and adolescents with asthma, those who practiced “shift and persist” had improved asthma symptoms only if they had low SES or experienced more unfair treatment than their peers (40). Further prospective studies are needed to explore the cost-effectiveness and impact of psychological interventions targeted to caregivers (41) or adolescents to improve asthma.
Family-level stressors
Family structure and functionality could affect an adolescent’s health, growth, and wellbeing. Caregivers of children with asthma have more depression and anxiety symptoms than those of healthy children (42), and depressive symptoms can affect the overall health, employment, and SES of caregivers, which may in turn affect asthma outcomes in their children (43, 44). In a cross-sectional study of 223 primarily Hispanic children and adolescents with uncontrolled asthma, depressive symptoms in the parent and her/his child were associated with worse asthma severity or control, activity limitations, and emotional triggers of asthma (45). Moreover, family chaos (measured by assessing commotion, disorganization and routine in the household (46)), was associated with worse asthma control (even after adjusting for depressive symptoms in parent and child) and was a mediator of the association between parent/child depressive symptoms and worse asthma outcomes (45).
Adverse experiences in an individual’s household can be highly stressful and have a long-lasting impact on an adolescent. A cross-sectional study of six home adverse childhood experiences (ACE) and lifetime asthma prevalence in 92,472 children and adolescents (0 to 17 years old) in the United States showed that home ACE were significantly associated with increased odds of lifetime asthma, with a dose-response relationship going from 1 ACE (OR=1.28, 95% CI=1.12 to 1.43) to 4 ACE (OR=1.73, 95% CI=1.27 to 2.36) (47). However, inconsistent results with no clear dose-response relationship were reported in a subgroup analysis of adolescents (aged 12 to 17 years). In that study, home ACE included living with a parent or guardian who was divorced or separated, who died, who served time in jail or prison, who was mentally ill or suicidal or severely depressed, who had a problem with substance use, or who partook in domestic violence. In an exploratory analysis, Hispanic children and adolescents were shown to be at higher risk of lifetime asthma when exposed to home ACE than children in other racial or ethnic groups (47). Limited evidence suggests that intrafamilial violence is linked to all asthma (48, 49) or non-atopic asthma (50) in pre-school (48, 49) and school-aged (50) children, but little is known about intrafamilial violence and asthma in adolescents.
Homelessness is a severe stressor, and asthma prevalence in homeless children and adolescents has been reported to be 2 to 3 times higher than that in their housed peers (51, 52). A database-driven analysis of subjects with asthma in New York showed that homeless children and adolescents had asthma hospitalization rates that were 31 times higher than those in non-homeless youth, and that homelessness was associated with greater risk of need for ventilatory support for asthma among subjects aged 5 years and older (53). Because of its design, that study could not assess whether the observed associations were mediated or confounded by risk factors correlated with homelessness (e.g., healthcare access, substance abuse, post-traumatic stress disorder, or depression)(52).
Community-level stressors
In engaging with their communities, adolescents face potentially adverse situations while attending school, interacting with their peers, and perceiving or becoming aware of neighborhood or community stressors such as violence, poverty, discrimination, and racism. In a cross-sectional study of a convenience sample of 61 primarily African American adolescents with asthma, high cumulative stress (accounting for poverty, neighborhood stress, school stress, peer pressure and caregiver-adolescent conflict) was associated with worse quality of life, worse asthma control, and ED visits for asthma (54). Moreover, adolescents with well-controlled asthma were less likely to live in poverty and had lower levels of neighborhood stress, school-related stress, and peer-pressure than those with poorly controlled asthma. Findings from that study must be cautiously interpreted because of its cross-sectional design, small sample size, and non-adjustment for confounders such as obesity, healthcare access, and pollutants.
A link between community violence and asthma has been reported in pre-adolescent children and adults. Such link may be explained by violence-related stress or risk factors correlated with community violence (55–57). In a cross-sectional analysis of data from a convenience sample of 156 children and adolescents with asthma, living in disadvantaged neighborhoods was associated with daily and nocturnal asthma symptoms, as well as marginally lower peak expiratory flow rates (58). In a separate retrospective analysis of data for 4,638 ED visits and hospitalizations for asthma among children and adolescents in Cincinnati (OH), crime rates in a child’s census tract were significantly associated with increased asthma utilization rates, even after accounting for poverty, unemployment, substandard housing, and traffic exposure (59). Of interest, violent crime rates in the child’s census tract were more strongly and significantly correlated with healthcare utilization for asthma than all-crime rates in the child’s census tract. Interpretation of the findings of the studies above is limited by their cross-sectional design and lack of data on potential confounders.
Gun violence has become increasingly common in the United States (60). Whether this severe form of violence affects asthma in adolescents has just recently been explored. In a cross-sectional study of 466 Puerto Rican children and adolescents, lifetime exposure to gun violence (defined as having heard gunshots more than once) was significantly associated with 1.8 times increased odds of asthma, even after accounting for SES, traffic-related air pollution, prematurity, and other confounders (95% CI for OR=1.1 to 2.7) (61). This association was stronger in children who were exposed to gun violence and reported being afraid to leave their home. In a separate analysis of that cohort, the global proportion of African ancestry in Puerto Rican children and adolescents was associated with both asthma and higher total IgE among participants exposed to gun violence, but not in those unexposed (62). These findings should be explored in prospective studies with comprehensive data on potential confounders and mediators of the association between gun violence and asthma.
Racism or discrimination can negatively affect an adolescent’s self-esteem, mental health, or academic achievement (63). A cross-sectional study of two cohorts of minority youth (ages 8 to 21 years) showed that reported discrimination was associated with increased odds of asthma (OR=1.78, 95% CI=1.33 to 2.39) and poor asthma control (OR=1.97, 95% CI=1.42 to 2.76) in African Americans, even after accounting for SES and other confounders (64). Among Mexican Americans in that study, reported discrimination was only associated with asthma among those of low SES. In a separate analysis of one of those cohorts, reported discrimination was also associated with increased bronchodilator response in African American youth, particularly in those with elevated plasma TNF-alpha levels (65). Consistent with negative effects of discrimination on asthma, a study that followed 121 Canadian youth with asthma over a period of 2 years reported that targeted rejection (a form of discrimination) was associated with lower mRNA for glucocorticoid receptor and β2-adrenergic receptor in whole blood, even after accounting for body mass index and other confounders (but not for medication use) (66).
Coping mechanisms such as family support may ameliorate detrimental effects of community stressors on asthma. For example, a cross-sectional study of a convenience sample of 308 subjects ages 9 to 17 years showed that, among those living in a neighborhood deemed dangerous or disorderly, participants who had better family relationships had fewer asthma symptoms and activity limitations but a higher FEV1 than those lacking such relationships, accounting for use of inhaled corticosteroids, ethnicity, and other confounders (67). In that study, living in neighborhoods deemed dangerous or disorderly was associated with increased T helper 1 and T helper 2 cytokine production and decreased glucocorticoid sensitivity. Although that study utilized a novel approach to define disordered or dangerous neighborhoods by using Google Street View images, comprehensive tools to more accurately define disadvantaged neighborhoods are needed.
CONCLUSION
In contrast to the body of published evidence for children and adults, relatively few studies have focused on stressors or stress and asthma in adolescents. Despite limitations related to study design (e.g., small sample size, cross-sectional nature, potential selection bias, lack of objective measures of lung function or atopy) or data analysis (e.g., non-adjustment for confounders such as medication use, asthma severity, obesity, or air pollution), current evidence suggests that adolescents exposed to stressors (at the individual, family, or community levels) and those who experience stress/anxiety or are depressed are at increased risk of asthma or worse asthma outcomes.
Future large studies with a prospective or longitudinal design should determine whether and how stressors or stress cause or worsen asthma in adolescents, defined and assessed not only through questionnaires but also by objective measures of pulmonary function, airway responsiveness, and atopy. Moreover, such studies should assess factors that could confound or mediate the relation between stressors or stress and asthma (e.g., vaping, smoking, diet, treatment adherence), while also considering biologically plausible interactions (e.g., with obesity, diet, or pollutants). This, coupled with biomarkers of omics and immune responses, are needed to better understand the relative contributions of direct vs. indirect effects of stress or stressors on asthma phenotypes, as well as potential causal mechanisms.
Evidence from studies in adolescents and young adults support conducing randomized clinical trials of behavioral interventions or coping mechanisms to reduce the effects of certain psychosocial stressors on asthma outcomes in adolescents with asthma. Such evidence also supports well-designed clinical trials of antidepressants as an adjuvant therapy in adolescents with asthma, particularly poorly controlled asthma.
Given available evidence, clinicians should assess exposure to stressors (e.g., violence or abuse) and screen for anxiety and depressive disorders when caring for adolescents with asthma, providing referrals to social workers or mental health professionals, as appropriate. Finally, public health policies are needed to reduce psychosocial stressors such as gun violence and racism in adolescents.
KEY MESSAGES.
Current evidence suggests that exposure to stressors (at the individual, family, and community levels) or stress (acute and chronic) are associated with asthma and worse asthma outcomes.
Future large studies with a prospective or longitudinal design should determine whether and how stressors or stress cause or worsen asthma in adolescents.
Clinicians should assess exposure to stressors (e.g., violence or abuse) and screen for anxiety and depressive disorders when caring for adolescents with asthma, providing referrals to social workers or mental health professionals when appropriate.
Public health policies are needed to reduce psychosocial stressors such as gun violence and racism in adolescents.
Funding:
This work was supported by grants HL117191, HL119952, and MD011764 from the U.S National Institutes of Health (NIH). Dr. Landeo-Gutierrez is supported by training grant T32 HL129949 from the U.S. NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures of Interest:
Dr. Celedón has received research materials from Merck and GSK (inhaled steroids) and Pharmavite (vitamin D and placebo capsules), in order to provide medications free of cost to participants in NIH-funded studies, unrelated to the current work. The other authors have no conflicts of interest to declare.
REFERENCES
- 1.Centers for Disease Control and Prevention. Summary health statistics: National Health Interview Survey 2018. FastStats - Asthma CDC at <https://www.cdc.gov/nchs/fastats/asthma.htm>.
- 2.QuickStats: Percentage* of All Emergency Department (ED) Visits† Made by Patients with Asthma,§ by Sex and Age Group - National Hospital Ambulatory Medical Care Survey, United States 2014–2015. MMWR Morb Mortal Wkly Rep 2018;67:167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hsu J, Qin X, Beavers SF, Mirabelli MC. Asthma-Related School Absenteeism, Morbidity, and Modifiable Factors. Am J Prev Med 2016;51:23–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alderman EM, Breuner CC, COMMITTEE ON ADOLESCENCE. Unique needs of the adolescent. Pediatrics 2019;144: [DOI] [PubMed] [Google Scholar]
- 5.Carswell J Chapter 2 Normal physical growth and development In: Katzman DK, editorStafford D, translator. Neinstein’s Adolescent And Young Adult Health Care: A Practical Guide (adolescent Health Care A Practical Guide), 6th ed Philadelphia, PA: Lww; 2016. p. 134. [Google Scholar]
- 6.Goldstein MA, editor. The massgeneral hospital for children adolescent medicine handbook. Cham: Springer International Publishing; 2017. doi: 10.1007/978-3-319-45778-9. [DOI] [Google Scholar]
- 7.Cognitive Steinberg L. and affective development in adolescenc e. Trends Cogn Sci (Regul Ed) 2005;9:69–74. [DOI] [PubMed] [Google Scholar]
- 8.Naimi DR, Freedman TG, Ginsburg KR, Bogen D, Rand CS, Apter AJ. Adolescents and asthma: why bother with our meds? J Allergy Clin Immunol 2009;123:1335–1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Engelkes M, Janssens HM, de Jongste JC, Sturkenboom MCJM, Verhamme KMC. Prescription patterns, adherence and characteristics of non-adherence in children with asthma in primary care. Pediatr Allergy Immunol 2016;27:201–208. [DOI] [PubMed] [Google Scholar]
- 10.De Simoni A, Horne R, Fleming L, Bush A, Griffiths C. What do adolescents with asthma really think about adherence to inhalers? Insights from a qualitative analysis of a UK online forum. BMJ Open 2017;7:e015245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bollinger ME, Mudd KE, Boldt A, Hsu VD, Tsoukleris MG, Butz AM. Prescription fill patterns in underserved children with asthma receiving subspecialty care. Ann Allergy Asthma Immunol 2013;111:185–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grant KE, Compas BE, Stuhlmacher AF, Thurm AE, McMahon SD, Halpert JA. Stressors and child and adolescent psychopathology: Moving from markers to mechanisms of risk. Psychol Bull 2003;129:447–466. [DOI] [PubMed] [Google Scholar]
- 13.Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull 2004;130:601–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Landeo-Gutierrez J, Forno E, Miller GE, Celedón JC. Exposure to violence, psychosocial stress, and asthma. Am J Respir Crit Care Med 2020;201:917–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosenberg SL, Miller GE, Brehm JM, Celedón JC. Stress and asthma: novel insights on genetic, epigenetic, and immunologic mechanisms. J Allergy Clin Immunol 2014;134:1009–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen E, Miller GE. Stress and inflammation in exacerbations of asthma. Brain Behav Immun 2007;21:993–999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chrousos GP. The hypothalamic-pituitary-adrenal axis and immune-mediated inflammation. N Engl J Med 1995;332:1351–1362. [DOI] [PubMed] [Google Scholar]
- 18.Forsythe P, Ebeling C, Gordon JR, Befus AD, Vliagoftis H. Opposing effects of short- and long-term stress on airway inflammation. Am J Respir Crit Care Med 2004;169:220–226. [DOI] [PubMed] [Google Scholar]
- 19.Miller GE, Chen E. Life stress and diminished expression of genes encoding glucocorticoid receptor and beta2-adrenergic receptor in children with asthma. Proc Natl Acad Sci USA 2006;103:5496–5501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brehm JM, Ramratnam SK, Tse SM, Croteau-Chonka DC, Pino-Yanes M, Rosas-Salazar C, Litonjua AA, Raby BA, Boutaoui N, Han Y-Y, Chen W, Forno E, Marsland AL, Nugent NR, Eng C, Colón-Semidey A, Alvarez M, Acosta-Pérez E, Spear ML, Martinez FD, Avila L, Weiss ST, Soto-Quiros M, Ober C, Nicolae DL, Barnes KC, Lemanske RF, Strunk RC, Liu A, et al. Stress and Bronchodilator Response in Children with Asthma. Am J Respir Crit Care Med 2015;192:47–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clougherty JE, Rossi CA, Lawrence J, Long MS, Diaz EA, Lim RH, McEwen B, Koutrakis P, Godleski JJ. Chronic social stress and susceptibility to concentrated ambient fine particles in rats. Environ Health Perspect 2010;118:769–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Islam T, Urman R, Gauderman WJ, Milam J, Lurmann F, Shankardass K, Avol E, Gilliland F, McConnell R. Parental stress increases the detrimental effect of traffic exposure on children’s lung function. Am J Respir Crit Care Med 2011;184:822–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ohno I Neuropsychiatry phenotype in asthma: Psychological stress-induced alterations of the neuroendocrine-immune system in allergic airway inflammation. Allergol Int 2017;66S:S2–S8. [DOI] [PubMed] [Google Scholar]
- 24.Oren E, Gerald L, Stern DA, Martinez FD, Wright AL. Self-Reported Stressful Life Events During Adolescence and Subsequent Asthma: A Longitudinal Study. J Allergy Clin Immunol Pract 2017;5:427–434.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dunton G, Dzubur E, Li M, Huh J, Intille S, McConnell R. Momentary assessment of psychosocial stressors, context, and asthma symptoms in hispanic adolescents. Behav Modif 2016;40:257–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen E, Strunk RC, Bacharier LB, Chan M, Miller GE. Socioeconomic status associated with exhaled nitric oxide responses to acute stress in children with asthma. Brain Behav Immun 2010;24:444–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liccardi G, Baldi G, Berra A, Carpentieri E, Cutajar M, D’Amato M, Del Donno M, Del Prato B, Folletti I, Gani F, Gargano D, Giannattasio D, Giovannini M, Infantino A, Lombardi C, Lo Schiavo M, Madonna F, Maniscalco M, Meriggi A, Milanese M, Montera C, Pio A, Russo M, Salzillo A, Scavalli P, Scichilone N, Sposato B, Stanziola A, Starace A, et al. Non respiratory symptoms in asthma as possible predictors of exacerbations. J Allergy Clin Immunol Pract 2015;3:798–800.e2. [DOI] [PubMed] [Google Scholar]
- 28.Chen W, Boutaoui N, Brehm JM, Han Y-Y, Schmitz C, Cressley A, Acosta-Pérez E, Alvarez M, Colón-Semidey A, Baccarelli AA, Weeks DE, Kolls JK, Canino G, Celedón JC. ADCYAP1R1 and asthma in Puerto Rican children. Am J Respir Crit Care Med 2013;187:584–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Landeo-Gutierrez J, Marsland AL, Acosta-Pérez E, Canino G, Celedón JC. Exposure to violence, chronic stress, asthma, and bronchodilator response in Puerto Rican children. Ann Allergy Asthma Immunol 2020;doi: 10.1016/j.anai.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Romans S, Belaise C, Martin J, Morris E, Raffi A. Childhood abuse and later medical disorders in women. An epidemiological study. Psychother Psychosom 2002;71:141–150. [DOI] [PubMed] [Google Scholar]
- 31.Scott KM, Von Korff M, Alonso J, Angermeyer MC, Benjet C, Bruffaerts R, de Girolamo G, Haro JM, Kessler RC, Kovess V, Ono Y, Ormel J, Posada-Villa J. Childhood adversity, early-onset depressive/anxiety disorders, and adult-onset asthma. Psychosom Med 2008;70:1035–1043. [DOI] [PubMed] [Google Scholar]
- 32.Cohen RT, Canino GJ, Bird HR, Celedón JC. Violence, abuse, and asthma in Puerto Rican children. Am J Respir Crit Care Med 2008;178:453–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Coogan PF, Wise LA, O’Connor GT, Brown TA, Palmer JR, Rosenberg L. Abuse during childhood and adolescence and risk of adult-onset asthma in African American women. J Allergy Clin Immunol 2013;131:1058–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Abajobir AA, Kisely S, Williams G, Strathearn L, Suresh S, Najman JM. The association between substantiated childhood maltreatment, asthma and lung function: A prospective investigation. J Psychosom Res 2017;101:58–65. [DOI] [PubMed] [Google Scholar]
- 35.Dudeney J, Sharpe L, Jaffe A, Jones EB, Hunt C. Anxiety in youth with asthma: A meta-analysis. Pediatr Pulmonol 2017;52:1121–1129. [DOI] [PubMed] [Google Scholar]
- 36.Bardach NS, Neel C, Kleinman LC, McCulloch CE, Thombley R, Zima BT, Grupp-Phelan J, Coker TR, Cabana MD. Depression, anxiety, and emergency department use for asthma. Pediatrics 2019;144: [DOI] [PubMed] [Google Scholar]
- 37.Shams MR, Bruce AC, Fitzpatrick AM. Anxiety Contributes to Poorer Asthma Outcomes in Inner-City Black Adolescents. J Allergy Clin Immunol Pract 2018;6:227–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bender BG. Depression symptoms and substance abuse in adolescents with asthma. Ann Allergy Asthma Immunol 2007;99:319–324. [DOI] [PubMed] [Google Scholar]
- 39.Letitre SL, de Groot EP, Draaisma E, Brand PLP. Anxiety, depression and self-esteem in children with well-controlled asthma: case-control study. Arch Dis Child 2014;99:744–748. [DOI] [PubMed] [Google Scholar]
- 40.Lam PH, Miller GE, Chiang JJ, Levine CS, Le V, Shalowitz MU, Story RE, Chen E. One size does not fit all: Links between shift-and-persist and asthma in youth are moderated by perceived social status and experience of unfair treatment. Dev Psychopathol 2018;30:1699–1714. [DOI] [PubMed] [Google Scholar]
- 41.Teach SJ, Shelef DQ, Fousheé N, Horn IB, Yadav K, Wang Y, Rand CS, Streisand R. Randomized clinical trial of parental psychosocial stress management to improve asthma outcomes. J Asthma 2019;1–12.doi: 10.1080/02770903.2019.1665063. [DOI] [PubMed] [Google Scholar]
- 42.Easter G, Sharpe L, Hunt CJ. Systematic Review and Meta-Analysis of Anxious and Depressive Symptoms in Caregivers of Children With Asthma. J Pediatr Psychol 2015;40:623–632. [DOI] [PubMed] [Google Scholar]
- 43.Wood BL, Brown ES, Lehman HK, Khan DA, Lee MJ, Miller BD. The effects of caregiver depression on childhood asthma: Pathways and mechanisms. Ann Allergy Asthma Immunol 2018;121:421–427. [DOI] [PubMed] [Google Scholar]
- 44.Johnson DA, Meltzer LJ, Zhang T, Lu M, Cassidy-Bushrow AE, Stokes-Buzzelli S, Duffy E, McKinnon B, Mahajan P, Redline S, Joseph CL. The influence of psychosocial stressors and socioeconomic status on sleep among caregivers of teenagers with asthma, the Puff City study. Sleep Health 2018;4:141–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Weinstein SM, Pugach O, Rosales G, Mosnaim GS, Walton SM, Martin MA. Family chaos and asthma control. Pediatrics 2019;144: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bazzoli GJ, Shortell SM, Dubbs N, Chan C, Kralovec P. A taxonomy of health networks and systems: bringing order out of chaos. Health Serv Res 1999;33:1683–1717. [PMC free article] [PubMed] [Google Scholar]
- 47.Wing R, Gjelsvik A, Nocera M, McQuaid EL. Association between adverse childhood experiences in the home and pediatric asthma. Ann Allergy Asthma Immunol 2015;114:379–384. [DOI] [PubMed] [Google Scholar]
- 48.Suglia SF, Enlow MB, Kullowatz A, Wright RJ. Maternal intimate partner violence and increased asthma incidence in children: buffering effects of supportive caregiving. Arch Pediatr Adolesc Med 2009;163:244–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Suglia SF, Duarte CS, Sandel MT, Wright RJ. Social and environmental stressors in the home and childhood asthma. J Epidemiol Community Health 2010;64:636–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bonfim CB, dos Santos DN, Barreto ML. The association of intrafamilial violence against children with symptoms of atopic and non-atopic asthma: A cross-sectional study in Salvador, Brazil. Child Abuse Negl 2015;50:244–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Prevalence Asthma & Access to Care Among Homeless High School Students – Institute for Children, Poverty & Homelessness. at <https://www.icphusa.org/reports/asthma-prevalence-access-to-care-among-homeless-high-school-students/>.
- 52.Grant R, Shapiro A, Joseph S, Goldsmith S, Rigual-Lynch L, Redlener I. The health of homeless children revisited. Adv Pediatr 2007;54:173–187. [DOI] [PubMed] [Google Scholar]
- 53.Sakai-Bizmark R, Chang R-KR, Mena LA, Webber EJ, Marr EH, Kwong KY. Asthma hospitalizations among homeless children in new york state. Pediatrics 2019;144: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Miadich SA, Everhart RS, Greenlee J, Winter MA. The impact of cumulative stress on asthma outcomes among urban adolescents. J Adolesc 2020;80:254–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Apter AJ, Garcia LA, Boyd RC, Wang X, Bogen DK, Ten Have T. Exposure to community violence is associated with asthma hospitalizations and emergency department visits. J Allergy Clin Immunol 2010;126:552–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wright RJ, Mitchell H, Visness CM, Cohen S, Stout J, Evans R, Gold DR. Community violence and asthma morbidity: the Inner-City Asthma Study. Am J Public Health 2004;94:625–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sternthal MJ, Jun HJ, Earls F, Wright RJ. Community violence and urban childhood asthma: a multilevel analysis. Eur Respir J 2010;36:1400–1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tobin ET, Zilioli S, Imami L, Saleh DJ, Kane HS, Slatcher RB. Neighborhood stress, depressive symptoms, and asthma morbidity in youth. J Pediatr Psychol 2016;41:952–960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Beck AF, Huang B, Ryan PH, Sandel MT, Chen C, Kahn RS. Areas with High Rates of Police-Reported Violent Crime Have Higher Rates of Childhood Asthma Morbidity. J Pediatr 2016;173:175–182.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fowler KA, Dahlberg LL, Haileyesus T, Annest JL. Firearm injuries in the United States. Prev Med 2015;79:5–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ramratnam SK, Han Y-Y, Rosas-Salazar C, Forno E, Brehm JM, Rosser F, Marsland AL, Colón-Semidey A, Alvarez M, Miller GE, Acosta-Pérez E, Canino G, Celedón JC. Exposure to gun violence and asthma among children in Puerto Rico. Respir Med 2015;109:975–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rosas-Salazar C, Han Y-Y, Brehm JM, Forno E, Acosta-Pérez E, Cloutier MM, Alvarez M, Colón-Semidey A, Canino G, Celedón JC. Gun Violence, African Ancestry, and Asthma: A Case-Control Study in Puerto Rican Children. Chest 2016;149:1436–1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Benner AD, Wang Y, Shen Y, Boyle AE, Polk R, Cheng Y-P. Racial/ethnic discrimination and well-being during adolescence: A meta-analytic review. Am Psychol 2018;73:855–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Thakur N, Barcelo NE, Borrell LN, Singh S, Eng C, Davis A, Meade K, LeNoir MA, Avila PC, Farber HJ, Serebrisky D, Brigino-Buenaventura E, Rodriguez-Cintron W, Thyne S, Rodriguez-Santana JR, Sen S, Bibbins-Domingo K, Burchard EG. Perceived discrimination associated with asthma and related outcomes in minority youth: the GALA II and SAGE II studies. Chest 2017;151:804–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Carlson S, Borrell LN, Eng C, Nguyen M, Thyne S, LeNoir MA, Burke-Harris N, Burchard EG, Thakur N. Self-reported racial/ethnic discrimination and bronchodilator response in African American youth with asthma. PLoS One 2017;12:e0179091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Murphy MLM, Slavich GM, Chen E, Miller GE. Targeted rejection predicts decreased anti-inflammatory gene expression and increased symptom severity in youth with asthma. Psychol Sci 2015;26:111–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chen E, Hayen R, Le V, Austin MK, Shalowitz MU, Story RE, Miller GE. Neighborhood social conditions, family relationships, and childhood asthma. Pediatrics 2019;144 (2): e20183300. [DOI] [PMC free article] [PubMed] [Google Scholar]


