Abstract
Background
Professional interpretation improves healthcare quality and outcomes for limited English proficient (LEP) patients, yet interpreter use remains low even when interpretation is available remotely. We analyzed the effect of remote interpretation (telephone or video) on pediatric emergency provider attitudes and behaviors around professional interpretation.
Methods
A cross-sectional questionnaire of pediatric emergency providers was conducted as part of a randomized trial of telephone versus video interpretation with Spanish speaking LEP families. Providers recalled lapses of professional interpretation for medical communication (use of an ad hoc or no interpreter), if they had delayed or deferred communication due to the need for professional interpretation, and were asked about their satisfaction with the interpretation modality. Bivariate and multivariate analysis of professional interpreter use and communication behaviors were analyzed by self-report of study group assignment.
Results
One-third of providers reported lapses of professional interpretation and many reported less frequent (46%) and deferred communication (35%) due to the need for interpretation. There was no significant difference in these outcomes between telephone and video assignment. Interpreter skill and technical difficulties were similar between groups. Providers assigned to telephone, compared to video, were more likely to be dissatisfied (p<0.001) and to report that interpretation was ineffective (p=0.002).
Conclusion
Despite access to interpretation, providers caring for patients enrolled in a study of professional interpreter modalities reported frequent lapses in professional interpretation and deferring or delaying communication because an interpreter was needed. Addressing barriers to remote interpreter use will improve quality of care and health equity for LEP patients.
Keywords: Limited English Proficient, Interpreter, Emergency, Pediatrics
Background
Individuals who are limited English proficient (LEP) comprise 8.6% of the United States population1 and have an increased risk of medical errors and adverse events resulting in harm.2 The use of professional interpretation can mitigate this inequity and improve the quality of care for LEP patients.3,4 However, despite federal mandates for language access,5 professional interpreter use remains low.3,6–10 Even when interpreters are readily available, lapses in professional interpretation can occur if providers choose to “get by” with ad hoc interpreters (family members or hospital staff), who have high rates of making clinically important errors in interpretation,11 or to forego interpretation completely.12
Pediatric emergency department (ED) providers practice in a unique environment in which they interact with a patient and family multiple discrete times over the course of the patient’s care, while simultaneously assessing and managing other patients of varying acuity and facing frequent interruptions.13 Time constraints, clinical urgency, and competing demands, the natural environment of the pediatric ED, are all factors that impact a provider’s approach to communication with an LEP patient,14 including decisions around when to communicate with the patient and whether or not to use professional interpretation.10
Remote interpreter modalities (telephone and video interpretation) are widely used methods to increase access to professional interpretation.15 In a pragmatic randomized clinical trial (RCT) of remote interpreter modalities in the pediatric ED, LEP families assigned to receive video interpretation, compared to phone interpretation, were less likely to report lapses in professional interpretation (use of an ad hoc or no interpreter) and more likely to be able to recall their child’s diagnosis, despite similar parent report of communication and interpreter quality.16 Embedded in this RCT, we surveyed providers of enrolled patients to assess provider attitudes and behaviors related to the use of remote interpreter modalities in order to better understand the role of interpretation type on the factors that drive provider decision making around communication with LEP patients and families. We analyzed the effect of remote interpreter modality (telephone and video) on provider report of the following: 1) medical communication without professional interpretation, 2) changes in communication behaviors (such as delaying communication or communicating less frequently) due to the need for interpretation, and 3) provider assessment of difficulties/barriers with these remote modalities. We hypothesized that providers assigned to use video interpretation would be less likely to report lapses in professional interpretation and have lower rates of dissatisfaction and technical difficulties with the remote modality.
Methods
Design, Setting, and Participants
We conducted a cross-sectional questionnaire-based study embedded in an RCT of remote interpreter modalities in the pediatric ED.16 The ED-based pragmatic RCT enrolled Spanish-speaking LEP parents or guardians and their child (ages up to 18 years). The study was conducted between February and October 2014 in a large academic pediatric ED with 39,000 ED patient visits that year. The need for professional interpretation was assessed prior to rooming with the question “What is your preferred language for care?”. Hospital policy requires that providers use professional interpretation for all medical communication with LEP patients and families and ad hoc interpreter use is actively discouraged. In the ED, an in-person Spanish interpreter was present during hours of peak volume, five mobile video interpretation units were available with interpretation provided through InDemand Interpreting™ (Seattle WA), and each patient room had dual-handset speaker-enabled telephones with one-touch dialing for telephone interpretation services provided through Pacific Interpreters™ (LanguageLine Solutions, Monterey CA). In order to communicate directly in a nonnative language, providers are required to receive certification of proficient bilingual language skills after completing the telephone-based Clinical Cultural and Linguistic Assessment (ALTA Language Services, Atlanta, GA); providers with this certification have this indicated clearly on their hospital name badge.
Randomization to telephone or video interpretation occurred by day throughout the ED. Providers were asked to use that day’s randomly assigned remote interpreter modality (telephone or video) with all Spanish-speaking LEP families until the family was approached for enrollment and, if the family enrolled, to continue to do so over the course of the ED visit. However, providers retained discretion over how to communicate, and at times chose to use the non-assigned interpreter modality with enrolled families. Providers could use their preferred professional interpretation modality with families who declined or were ineligible to participate.
For this study, physicians (attendings, pediatric emergency medicine fellows, and residents training in pediatrics, emergency medicine, and family medicine) and nurse practitioners were eligible to complete a questionnaire if they were assigned to care for an enrolled patient during an ED shift. Eligible providers completed an online questionnaire about their communication with that patient and family. This study was approved by our Institutional Review Board.
Data Collection and Coding
Eligible providers received an email during their ED shift identifying any patient they were caring for who had agreed to enroll in the study. Providers received a second email on the following business day with a link to complete the follow-up questionnaire. Questionnaires were anonymous and were not linked to the enrolled patient. All data were collected through the University of Washington’s Catalyst Web Tools.
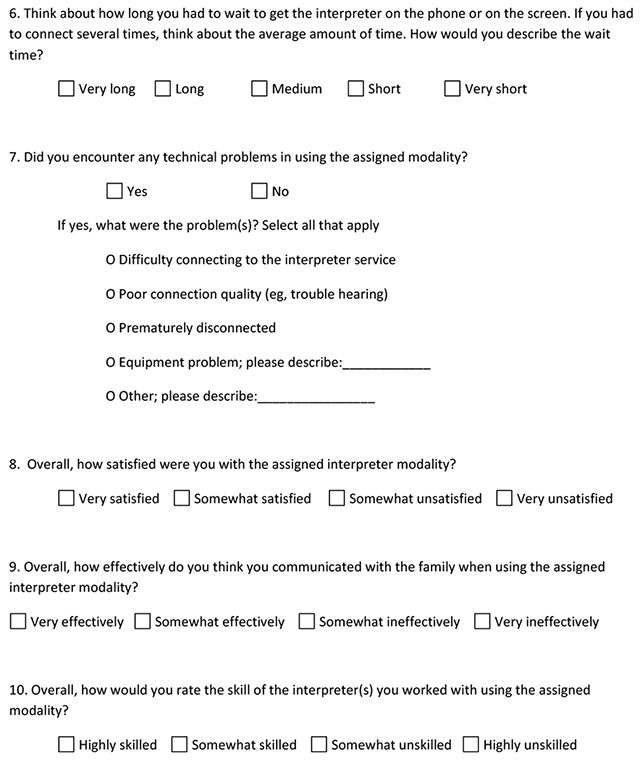
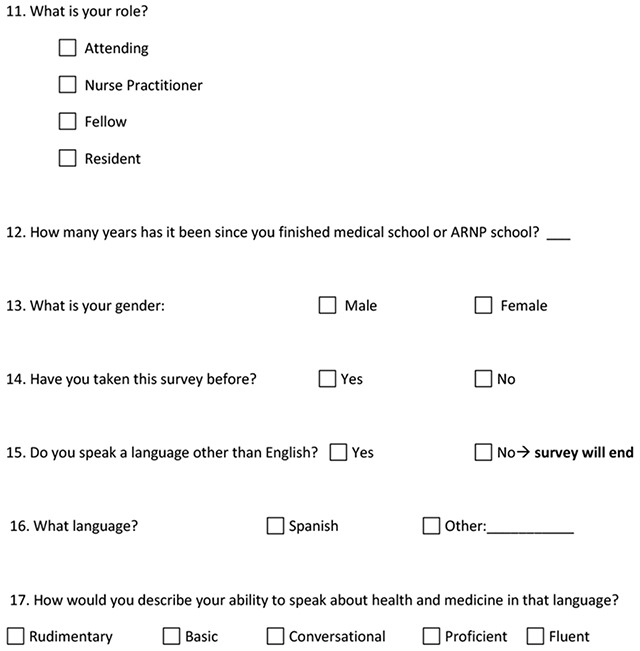
Providers completed an online 17-item questionnaire (Appendix 1). Demographic information was collected, including gender, provider role, and years of practice. Participants were asked if they spoke any language other than English and were asked to rate their medical proficiency in that language on a 5-point Likert scale. Participants indicated if they had previously completed the survey for a prior patient enrolled in the RCT.
The remaining questions sought to assess provider communication patterns and experiences when providing care to the patient enrolled in the RCT. Study questions were developed and pilot-tested with ED providers prior to study initiation. Providers were asked to recall if and how they communicated with the patient and family during two key time periods: 1) initial history-taking, and 2) discussion of diagnoses, plans, and discharge instructions. Response options included: telephone interpreter; video interpreter; in-person professional interpreter; in English without an interpreter present; in Spanish without an interpreter present; or through a friend, family member, or patient who spoke English. A lapse of professional interpretation was considered to have occurred if the provider reported communicating in English or Spanish without an interpreter present or if they used ad hoc interpretation (interpretation through a friend, family member, or patient who spoke English). However, if a provider reported being proficient or fluent in medical Spanish, it was not categorized as a lapse of professional interpretation when they spoke directly to the patient and caregivers in Spanish. Provider report of any medical communication (history-taking and/or discussion of diagnosis, plan, and discharge instructions) was coded as occurring with professional interpretation or with a lapse in professional interpretation. Providers were also asked if, due to the need for interpretation, they had delayed communication with the family at any point and if, due to the need for interpretation, they had communicated less with the family than they would have otherwise. Participants were asked to recall to which interpreter modality the patient had been randomly assigned and to use a 4-point Likert scale to indicate how often they used the assigned modality when communicating with the family. If the participant did not know the assigned modality or reported never using the assigned modality during the patient encounter, the survey concluded. Participants who reported knowing and using the assigned interpreter modality were asked to identify interpretation delays and technical problems and to rate their satisfaction with the interpreter modality.
Data Analysis
Chi-square, Fisher exact test, and two-tailed t-tests were used for bivariate analysis of differences between assigned interpreter modality groups in provider characteristics, communication behaviors, and professional interpreter use and experience. Multivariate analysis of professional interpreter use and communication behaviors were analyzed by study group assignment using logistic regression. We controlled for potential a priori identified confounders: provider role, self-reported Spanish proficiency and prior survey completion.
Results
The RCT took place over 25 weeks, during which 336 Spanish-speaking families were screened for eligibility and 249 consented to enrollment. During that period, 162 physicians and nurse practitioners cared for at least one enrolled patient and 495 survey links were sent to these providers following enrollment (Figure 1). One-third of eligible providers (33%) initiated surveys. Half were first time participants (51%). Three in every four providers (77%) reported an assigned modality with video (n=65) or telephone (n=58) interpretation and that they had used the assigned modality; these providers were included in all analyses. Provider characteristics were similar across the two self-reported assigned study groups (Table 1). Eighteen providers (11%) were not able to recall the assigned modality and 19 providers (12%; 10 telephone, 9 video) knew the assigned modality but reported that they never used it.
Figure 1.
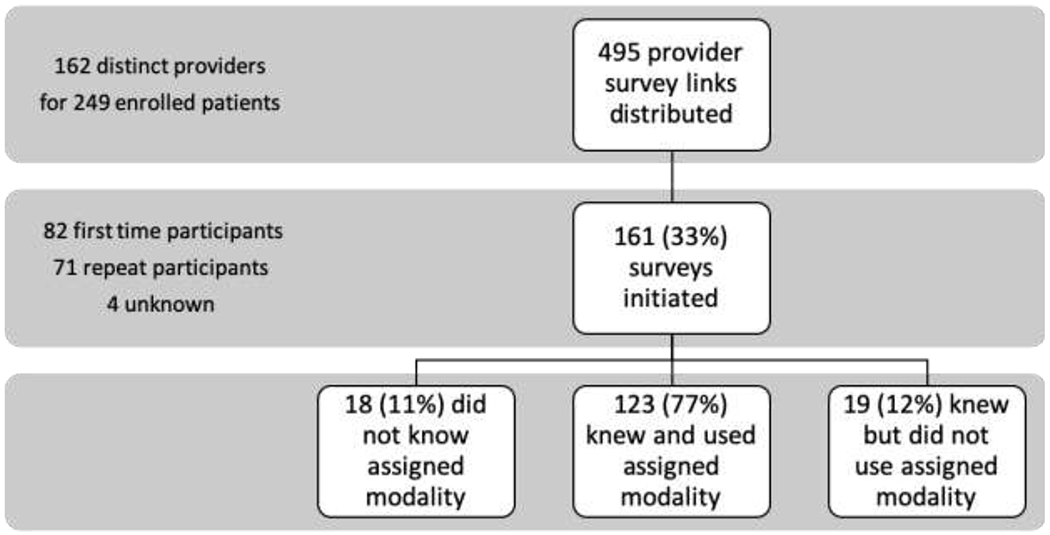
Provider Enrollment and Survey Participation
Table 1:
Characteristics of Participating Providers
| Overall (n = 161) | Telephone Arm (n = 68)a | Video Arm (n = 74)a | P value | |
|---|---|---|---|---|
| Role | ||||
| Attending | 51.6% (80/155) | 53.7% (36/67) | 51.4% (38/74) | .33 |
| ARNP | 7.7% (12/155) | 9.0% (6/67) | 8.1% (6/74) | |
| Fellow | 6.5% (10/155) | 4.5% (3/67) | 5.4% (4/74) | |
| Resident | 34.2% (53/155) | 32.8% (22/67) | 35.1% (26/74) | |
| Female | 62.6% (97/155) | 66.2% (45/68) | 61.6% (45/73) | .51 |
| Years of practice, mean (SD) | 8.3 (8.2) n=154 | 8.5 (8.3) n=66 | 8.1 (8.2) n=74 | .76 |
| Self-reported Spanish proficiency | ||||
| Rudimentary | 8.3% (2/24) | 28.6% (2/7) | 0 | |
| Basic | 33.3% (8/24) | 57.1% (4/7) | 16.7% (2/12) | .009 |
| Conversational | 29.2% (7/24) | 0 | 50% (6/12) | |
| Proficient | 20.9% (5/24) | 0 | 25% (3/12) | |
| Fluent | 8.3% (2/24) | 14.3% (1/7) | 8.3% (1/12) | |
| Taken survey before | 46.4% (71/153) | 44.8% (30/67) | 48.0% (35/73) | .71 |
ARNP = Advanced Registered Nurse Practitioner; SD = Standard Deviation
Denominators vary due to missing data from skipped survey questions
Sample sizes for Telephone Arm plus Video Arm do not add to Overall, as there were respondents who did not know the patient’s assigned modality
One-third of providers (32.7%) reported lapses in professional interpretation for some medical communication (history taking and/or discussion of diagnosis, plan, and discharge instructions) with an enrolled LEP family (Table 2). Providers who used professional interpretation reported using the assigned modality 93% of the time. There were no significant self-reported differences in lapses of professional interpretation or changes in communication behaviors between providers who reported being assigned to telephone versus video interpretation (p > 0.2). Lapses in professional interpretation for any medical communication (history taking and/or discussion of diagnosis, plan, and discharge instructions) were similar between providers who reported caring for patients assigned to telephone and video interpretation (31.3% vs 26.0%, p=0.5), but were more commonly reported by those providers who were not able to recall the patient’s assigned interpretation modality (p = 0.004). Attendings who took the patient history were more likely to report a lapse in professional interpretation relative to other medical providers (37% vs 21.2%, p = 0.04); there was no statistically significant difference in professional interpretation lapse by provider type for discussions of diagnosis, plan, and discharge.
Table 2:
Self-reported Medical Communication with LEP Patients Enrolled in RCT table
| Overall (n =161) | Telephone Arm (n = 68) | Video Arm (n = 74) | Assigned Arm Unknown (n=18) | P valuea | |
|---|---|---|---|---|---|
| Medical Communication without Professional Interpretationb | |||||
| Anyc,d | 32.7% (50/153) | 31.3% (20/64) | 26.0% (19/73) | 68.8% (11/16) | .004 |
| History Takinge | 25.7% (36/140) | 20.3% (12/59) | 22.1% (15/68) | 69.2% (9/13) | .001 |
| Discussionf | 27.2% (37/136) | 26.8% (15/56) | 22.7% (15/66) | 50% (7/14) | .11 |
| Medical Communication Behaviors Due to the Need for Professional Interpretation | |||||
| Delayed communicationg | 34.6% (54/156) | 41.2% (28/68) | 31.9% (23/72) | 18.8% (3/16) | .19 |
| Communicated lessh | 45.6% (73/160) | 51.5% (35/68) | 43.2% (32/74) | 33.3% (6/18) | .33 |
Denominators vary due to missing data from skipped survey questions
Compares telephone vs video vs unknown
Among providers without self-reported proficiency or fluency in Spanish
“Any” refers to a positive response to “history taking” or “discussion”
p = 0.50 for chi-square analysis comparing Telephone vs Video arms only
p = 0.83 for chi-square analysis comparing Telephone vs Video arms only
p = 0.60 for chi-square analysis comparing Telephone vs Video arms only
p = 0.26 for chi-square analysis comparing Telephone vs Video arms only
p = 0.33 for chi-square analysis comparing Telephone vs Video arms only
Nearly half of providers (45.6%) reported less communication with LEP patients due to the need for professional interpretation. One-third of providers (34.6%) reported delayed communication with LEP patients due to the need for professional interpretation (Table 2). In-person interpretation was reported by six providers, and the rate of delayed communication was not significantly changed when these responses were excluded from analysis. There were no statistically significant differences in communication frequency and delays when analyzed by dichotomized provider type (attending vs not attending).
Table 3 shows the results of regression analysis. When adjusting for provider role, self-reported provider Spanish proficiency, and prior survey completion, there was no significant difference in self-report of medical communication without professional interpretation or medical communication behaviors between providers who reported being assigned to telephone and video interpretation. Not being able to recall the patient’s assigned interpretation modality was associated with 12.7-fold increased odds of reporting a lapse in professional interpretation when taking a medical history (95% CI 2.11-76.4).
Table 3:
Self-Reported Provider Communication by Assigned Interpretation Modality
| Unadjusted OR (95% CI) | Adjusted OR (95% CI)a | |
|---|---|---|
| Medical Communication without Professional Interpretationb | ||
| Anyc | ||
| Telephone | reference | reference |
| Video | 0.77 (0.37, 1.63) | 0.84 (0.38, 1.86) |
| Unknown assignment | 4.84 (1.48, 15.8) | 3.62 (0.89, 14.7) |
| History Taking | ||
| Telephone | reference | reference |
| Video | 1.11 (0.47, 2.61) | 1.38 (0.53, 3.57) |
| Unknown assignment | 8.81 (2.31, 33.6) | 12.7 (2.11, 76.4) |
| Discussion | ||
| Telephone | reference | reference |
| Video | 0.80 (0.35, 1.84) | 0.87 (0.36, 2.13) |
| Unknown assignment | 2.73 (0.82, 9.10) | 2.71 (0.64, 11.5) |
| Medical Communication Behaviors Due to the Need for Professional Interpretation | ||
| Delayed communication | ||
| Telephone | reference | reference |
| Video | 0.67 (0.34, 1.34) | 0.61 (0.30, 1.28) |
| Unknown assignment | 0.33 (0.09, 1.27) | 0.38 (0.07, 2.03) |
| Communicated less | ||
| Telephone | reference | reference |
| Video | 0.72 (0.37, 1.39) | 0.67 (0.33, 1.37) |
| Unknown assignment | 0.47 (0.16, 1.40) | 0.33 (0.09, 1.32) |
OR = Odds Ratio; CI = Confidence Interval
Adjusted for provider role, self-reported Spanish proficiency, and prior survey completion
Among providers without self-reported proficiency or fluency in Spanish
“Any” refers to a positive response to “history taking” or “discussion”
Providers who reported caring for patients assigned to telephone interpretation were more likely to feel unsatisfied or very unsatisfied with the assigned modality relative to those caring for patients assigned to video interpretation (p<0.001; Table 4). Providers who reported being in the telephone arm were also more likely to report that communication was ineffective (p=0.002) and that there was a long wait time for professional interpretation (p=0.02). Provider report of the skill of interpretation was similar between the two groups (p=0.30), as was report of technical difficulties with the interpretation modality (Table 5).
Table 4:
Provider Ratings of Professional Interpretation Modalities
| Telephone Arm (n = 58) | Video Arm (n = 66) | P-value | |
|---|---|---|---|
| Satisfaction | |||
| Very unsatisfied | 13.8% (8/58) | 0 | <.001 |
| Somewhat unsatisfied | 22.4% (13/58) | 15.2% (10/66) | |
| Somewhat satisfied | 60.3% (35/58) | 43.9% (29/66) | |
| Very satisfied | 3.5% (2/58) | 40.9% (27/66) | |
| Effectiveness of communication | |||
| Very ineffective | 5.2% (3/58) | 0 | .002 |
| Somewhat ineffective | 24.1% (14/58) | 7.7% (5/65) | |
| Somewhat effective | 50% (29/58) | 46.2% (30/65) | |
| Very effective | 20.7% (12/58) | 46.2% (30/65) | |
| Perceived skill of interpreter | |||
| Highly unskilled | 1.7% (1/58) | 0 | .30 |
| Somewhat unskilled | 1.7% (1/58) | 3.0% (2/66) | |
| Somewhat skilled | 43.1% (25/58) | 30.3% (20/66) | |
| Highly skilled | 53.5% (31/58) | 66.7% (44/66) | |
| Perceived wait time to interpretation | |||
| Very long | 3.5% (2/58) | 1.5% (1/65) | .02 |
| Long | 15.5% (9/58) | 1.5% (1/65) | |
| Medium | 37.9% (22/58) | 35.4% (23/65) | |
| Short | 32.8% (19/58) | 35.4% (23/65) | |
| Very short | 10.3% (6/58) | 26.2% (17/65) | |
Table 5.
Provider Report of Technical Difficulties with Professional Interpretations
| Telephone Arm (n = 57) | Video Arm (n = 65) | P value | |
|---|---|---|---|
| No difficulty | 57.9% (33/57) | 55.4% (36/65) | .78 |
| Difficulty connecting | 14% (8/57) | 16.9% (11/65) | .71 |
| Poor connection quality | 33.3% (19/57) | 30.8% (20/65) | .45 |
| Prematurely disconnected | 8.8% (5/57) | 12.3% (8/65) | .56 |
| Other equipment problem | 5.3% (3/57) | 3.1% (2/65) | .49 |
| Other | 15.8% (9/57) | 12.3% (8/65) | .45 |
Discussion
In this sample of pediatric emergency providers caring for LEP Spanish-speaking families enrolled in an RCT of remote interpreter modalities, one-third of respondents reported that they did not use professional interpretation for the entirety of medical communication. Providers also reported high rates of altering their communication behaviors due to the need for professional interpretation, by communicating with these LEP families less promptly and less frequently. We found no differences in these findings between those providers who reported caring for patients assigned to video and telephone interpretation. Although there were no differences in reports of technical difficulties between the two remote modalities, provider satisfaction, frequency of perceived short wait time, and perceived effectiveness of interpretation was significantly higher in the video interpretation group.
The rate of self-reported lapses in professional interpretation across all groups was high, although lower than the rate of lapse reported by parents16 and observed in video subanalysis9 from this same RCT, indicating recall and social desirability bias. While providers recalled that most LEP visits included interpretation, the high reported rate of episodic lapses in professional interpretation in critical tasks such as obtaining medical history and discussing the treatment plan is concerning, particularly within a cohort of providers who were aware of the ongoing study of professional interpretation. Our findings highlight that providers may consciously decide to “get by” without interpretation during portions of the visit, despite ready access to professional interpretation. Further, though providers reporting to be in the telephone arm reported longer wait times for interpretation, few providers reported long or very long wait times. Perceived effectiveness and skill of interpretation was high. Thus, even in the setting of interpretation perceived to be readily accessible and highly functional and effective, interpreter use remained suboptimal.
Pediatric ED providers also reported frequently delaying and deferring communication with LEP families due to the need for professional interpretation. This finding suggests that pediatric ED providers, who interact with patients and caregivers in a fragmented pattern for reassessments and as results are available, may provide a different standard of care for following up with, updating, and checking in on LEP patients and families compared with English proficient ED patients. Communication with English proficient patients in the emergency department is already brief and may be inadequate.17,18 Each communication encounter with a patient and caregiver offers the provider a chance to give updates, reinforce existing assessments and plans of care, assess patient and caregiver knowledge and understanding, offer the patient and caregiver an opportunity to ask questions, and to concurrently re-evaluate the patient; our results reveal providers acknowledge a clear disparity in communication and care for LEP families. LEP patients have higher rates of return visits for admission19 and of escalation to intensive care after admission, even when controlling for patient acuity and complexity.10 With infrequent, limited communication, particularly if there are lapses in professional interpretation, there may be fewer opportunities for bidirectional communication with the patient and caregiver during the ED visit, which may deny caregivers the opportunity to ask for clarification, add previously omitted details, or give updates on the patients status, thereby impacting ongoing plan of care, disposition planning and patient outcomes.
Although perception of interpreter skill and frequency of technical difficulties was similar between the two groups, providers reported higher satisfaction with and more effective communication through video compared to telephone interpretation. Although we did not find a difference in lapses in professional interpretation reported by providers in this study, our findings, which are reliant on self-report, are limited to the two specific time points designated in the questionnaire (history taking and discussion of diagnosis and discharge). Further, we do not know the assigned group of those providers who were unable to recall this information. Parents assigned to the telephone group in the RCT reported higher lapses in professional interpretation,16 which may be explained by the lower provider satisfaction with telephone interpretation. Additionally, the higher perceived effectiveness of communication by providers who reported being assigned to video interpretation may be due to the added ability of video interpreters to view and incorporate nonverbal cues and is reflected in the improved diagnosis recall by LEP caregivers receiving video interpretation.16 Providers who reported being assigned to video interpretation also reported lower wait times when connecting to remote interpretation, which can be essential to an ED provider who is moving between multiple patient care activities. These benefits of video interpretation should be the focus of future studies aimed at improving medical communication and health outcomes for LEP communities.
Providers who were unable to recall the interpreter modality to which their patient was randomly assigned were more likely to report lapses in professional interpretation. There are several potential explanations for this finding. First, providers may have been unaware that the patient they cared for was enrolled in the RCT and their much lower use of professional interpretation may therefore more closely reflect usual practice. Alternatively, these providers may have known that their patient was enrolled, but in the context of a busy ED shift, reverted to their usual practice and did not display artificially elevated rates of interpreter use due to the Hawthorne effect. It may be that these providers may also have been less influenced by social desirability bias. Another potential explanation is that these providers may not have clearly recalled the encounter and may therefore have been reporting on their usual practices, rather than those pertaining to the specific enrolled family. It is also interesting to note that providers who did not know the assigned study arm were less likely to report delayed or deferred communication due to the need for interpretation (although the difference did not achieve statistical significance). This finding supports the notion that these providers defaulted to communicating with them without interpretation, and therefore without modifying their communication patterns around the need for interpretation.
This was a questionnaire study and is limited by self-report, recall, and social-desirability bias,20 which are inherent to this study design; we are additionally limited by low response rate. We were reliant on self-report of the assigned remote interpretation modality for our analysis; however, since we did not find significant differences in provider behaviors between the two groups, this is unlikely to substantially influence our findings. Similarly, at the time of this study few providers had obtained official certification of bilingual language proficiency, and so we relied on self-report of proficiency so as to protect respondent anonymity. In order to maintain anonymity, provider responses were not linked to patient data, and so we cannot determine the assigned modality for those providers who were unable to recall this information. Without linking to patient data, we are also unable to associate provider responses with patient or caregiver characteristics, caregiver survey responses, or emergency department metrics16, and are unable to determine how long after the ED visit providers responded to the survey. Finally, this study took place in a single center and may not be generalizable. However, this study took place in a center with a strong institutional culture for the use of professional interpretation, and so the findings may in fact underestimate national practices.
Conclusion
There are well documented disparities in health outcomes for LEP patients, including an increased risk for serious medical errors and physical harm21–23 and professional interpretation has been demonstrated to be associated with improved quality of healthcare.3 Despite ready access to effective interpretation, providers caring for patients enrolled in a study of remote professional interpreter modalities reported frequent lapses in professional interpretation and frequently deferring or delaying communication because an interpreter was needed. Providers reported higher satisfaction with video compared to telephone interpretation. Future efforts directed towards increasing professional interpretation should focus on continuing to identify and decrease barriers to interpreter use and to promoting provider behavior change around communication through professional interpreters. These interventions will be essential to making progress in addressing healthcare disparities for patients and families with limited English proficiency.
Acknowledgements
We thank the Seattle Children’s Hospital Emergency Department Research Team and staff and patients for their participation and contributions. We are grateful to the Seattle Children’s Hospital Department of Interpreter Services, and in particular to Juan Kraus, to whose memory this work is dedicated.
Funding This work was funded by the Seattle Children’s Research Institute Center for Child Health, Behavior and Development and the Seattle Children’s Hospital Center for Diversity and Health Equity. K.C.L. was supported by National Institute of Child Health and Human Development Grant K23 HD078507 (PI, K. C. Lion). Funding sources had no role in the study design, collection, analysis, and interpretation of data, in writing the manuscript, or in submitting the article for publication.
Appendix 1. Provider Questionnaire
For the following questions, please consider your experience with the last family you cared for who was enrolled in the interpreter modality study.
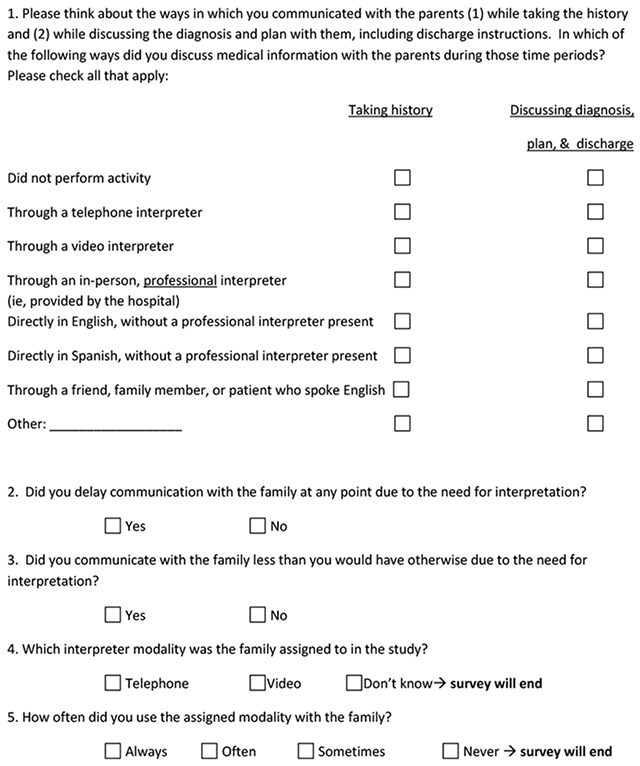
For the following questions, please consider only your experience with the enrolled family using the interpreter modality assigned by the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest The authors have no conflicts of interest to disclose.
References
- 1.Language Use in the United States:2011. US Census Bureau;2013. [Google Scholar]
- 2.Improving Patient Safety Systems for Patients with Limited English Proficiency. Rockville, MD: Agency for Healthcare Research and Quality;2012. [Google Scholar]
- 3.Flores G The impact of medical interpreter services on the quality of health care: a systematic review. Medical care research and review : MCRR. 2005;62(3):255–299. [DOI] [PubMed] [Google Scholar]
- 4.Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health services research. 2007;42(2):727–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen AH, Youdelman MK, Brooks J. The legal framework for language access in healthcare settings: Title VI and beyond. Journal of general internal medicine. 2007;22 Suppl 2:362–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramirez D, Engel KG, Tang TS. Language interpreter utilization in the emergency department setting: a clinical review. Journal of health care for the poor and underserved. 2008;19(2):352–362. [DOI] [PubMed] [Google Scholar]
- 7.Kuo DZ, O’Connor KG, Flores G, Minkovitz CS. Pediatricians’ use of language services for families with limited English proficiency. Pediatrics. 2007;119(4):e920–927. [DOI] [PubMed] [Google Scholar]
- 8.Lee KC, Winickoff JP, Kim MK, et al. Resident physicians’ use of professional and nonprofessional interpreters: a national survey. Jama. 2006;296(9):1050–1053. [DOI] [PubMed] [Google Scholar]
- 9.Gutman CK, Cousins L, Gritton J, et al. Professional Interpreter Use and Discharge Communication in the Pediatric Emergency Department. Academic pediatrics. 2018;18(8):935–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hartford EA, Anderson AP, Klein EJ, Caglar D, Carlin K, Lion KC. The Use and Impact of Professional Interpretation in a Pediatric Emergency Department. Academic pediatrics. 2019;19(8):956–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flores G, Laws MB, Mayo SJ, et al. Errors in medical interpretation and their potential clinical consequences in pediatric encounters. Pediatrics. 2003;111(1):6–14. [DOI] [PubMed] [Google Scholar]
- 12.Diamond LC, Schenker Y, Curry L, Bradley EH, Fernandez A. Getting by: underuse of interpreters by resident physicians. Journal of general internal medicine. 2009;24(2):256–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jeanmonod R, Boyd M, Loewenthal M, Triner W. The nature of emergency department interruptions and their impact on patient satisfaction. Emergency medicine journal : EMJ 2010;27(5):376–379. [DOI] [PubMed] [Google Scholar]
- 14.Hsieh E Not just “getting by”: factors influencing providers’ choice of interpreters. Journal of general internal medicine. 2015;30(1):75–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Masland MC, Lou C, Snowden L. Use of communication technologies to cost-effectively increase the availability of interpretation services in healthcare settings. Telemedicine journal and e-health : the official journal of the American Telemedicine Association. 2010;16(6):739–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lion KC, Brown JC, Ebel BE, et al. Effect of Telephone vs Video Interpretation on Parent Comprehension, Communication, and Utilization in the Pediatric Emergency Department: A Randomized Clinical Trial. JAMA pediatrics. 2015;169(12):1117–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rhodes KV, Vieth T, He T, et al. Resuscitating the physician-patient relationship: emergency department communication in an academic medical center. Annals of emergency medicine. 2004;44(3):262–267. [DOI] [PubMed] [Google Scholar]
- 18.Musso MW, Perret JN, Sanders T, et al. Patients’ comprehension of their emergency department encounter: a pilot study using physician observers. Annals of emergency medicine. 2015;65(2):151–155.e154. [DOI] [PubMed] [Google Scholar]
- 19.Samuels-Kalow ME, Stack AM, Amico K, Porter SC. Parental Language and Return Visits to the Emergency Department After Discharge. Pediatric emergency care. 2017;33(6):402–404. [DOI] [PubMed] [Google Scholar]
- 20.Althubaiti A Information bias in health research: definition, pitfalls, and adjustment methods. Journal of multidisciplinary healthcare. 2016;9:211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured: findings from a national sample. Medical care. 2002;40(1):52–59. [DOI] [PubMed] [Google Scholar]
- 22.Lion KC, Rafton SA, Shafii J, et al. Association between language, serious adverse events, and length of stay among hospitalized children. Hospital pediatrics. 2013;3(3):219–225. [DOI] [PubMed] [Google Scholar]
- 23.Cohen AL, Rivara F, Marcuse EK, McPhillips H, Davis R. Are language barriers associated with serious medical events in hospitalized pediatric patients? Pediatrics. 2005;116(3):575–579. [DOI] [PubMed] [Google Scholar]


