Abstract
Violence is a public health concern linked with mental health problems among adolescents, and risk behavior increases the likelihood of violence exposure. Family cohesion may attenuate the negative effects of risk behavior. The purpose of this study was to examine family cohesion as a moderator in the relation between risk behavior (substance use and delinquency) and violence exposure, and to explore longitudinal associations among cohesion, violence exposure, and subsequent mental health outcomes (PTSD and depression). Data were drawn from the National Survey of Adolescents-Replication, a nationally representative sample of 3,604 adolescents, with data collected via structured phone interviews at three waves spanning a two-year period. Hypotheses were tested using longitudinal structural equation modeling. Findings revealed that high family cohesion attenuated the relation between risk behavior and subsequent violence exposure. Wave 2 violence exposure was associated with more Wave 3 mental health problems, but high family cohesion was related to fewer subsequent symptoms. Follow-up analyses revealed that family cohesion moderated the relation between risk behavior and experiencing, but not witnessing, violence. Several demographic associations were observed. Although risk behavior increases exposure to violence, and in turn, mental health problems, family cohesion may serve as a protective factor, attenuating the link between risk behavior and subsequent negative consequences. This effect emerged even when accounting for demographic and socioeconomic covariates. Interventions with adolescents should target family relationships as a protective factor to reduce risk of violence exposure and mental health problems, particularly for adolescents who are engaging in high-risk behaviors.
Keywords: trauma, family cohesion, PTSD, depression, risk behavior, substance use
Violence exposure remains a major public health concern among adolescents. It is estimated that 50-70% of adolescents have experienced violence in their lifetime (Finkelhor, Turner, Shattuck, & Hamby, 2013; Kilpatrick et al., 2000). Adolescents who are victimized—particularly those who experience multiple victimizations—are at greater risk of experiencing mental health difficulties, including depression and posttraumatic stress disorder (PTSD; Finkelhor, Ormrod, & Turner, 2007a; Kilpatrick et al., 2003). Consistent with the lifestyle and routine activities theory (Riley, 1987), engaging in risk behaviors, such as delinquency and substance use, increases the likelihood that adolescents will experience violence (Begle et al., 2011). Protective factors within the family context may shield adolescents from the risk of these behaviors, but few studies have examined the buffering role of family factors, such as cohesion, in preventing adolescent violence exposure. In a nationally representative sample of adolescents aged 12-17, the current study examined family cohesion as a protective factor in the longitudinal relation between risk behaviors and violence exposure, and examined family cohesion and violence exposure as longitudinal predictors of subsequent mental health outcomes.
Violence Exposure Among Adolescents
Adolescents’ exposure to violence can include sexual abuse and assault, physical abuse and assault, and witnessing domestic or community violence. These incidents can include violence perpetrated by either peers or adults, family members or non-family members, and known individuals or strangers. The most common form of violence exposure for adolescents is witnessing violence in the home or community, with prevalence estimates around 40% (Finkelhor et al., 2013; Kilpatrick et al., 2000; Zinzow, Ruggiero, Resnick, et al., 2009). Physical assault is estimated to occur among 22 to 55% of adolescents, with rates varying based on the definition and measurement of the assault (Finkelhor et al., 2013; Kilpatrick et al., 2000). About one-quarter of adolescents are estimated to have experienced any type of maltreatment by a caregiver, such as physical or sexual abuse. One in ten adolescents have experienced sexual assault by someone other than a caregiver (Finkelhor et al., 2013). Each of these forms of violence, both experienced and witnessed, can result in mental health difficulties, including PTSD and depression (Kilpatrick et al., 2003). There is some debate regarding whether directly experienced or witnessed violence is more strongly associated with negative outcomes, with some studies showing differential effects between the two types (Margolin, Vickerman, Oliver, & Gordis, 2010) and others demonstrating similar outcomes for both (Sternberg, Baradaran, Abbott, Lamb, & Guterman, 2006). Overall, however, it is clear that experiencing multiple incidents of violence can be particularly detrimental for adolescent well-being.
Adolescents who experience one traumatic event are also at high risk of re-victimization (Benedini, Fagan, & Gibson, 2016), leaving them vulnerable to the cumulative effects of polyvictimization (Adams et al., 2016). In addition to increasing the risk of further re-victimization (Finkelhor, Ormrod, & Turner, 2007b), polyvictimization is associated with a greater number and severity of PTSD and depressive symptoms (Cloitre et al., 2009; Mustanski, Andrews, & Puckett, 2016; Suliman et al., 2009), suggesting a need to identify avenues to bolster violence prevention efforts and reduce negative mental health outcomes for adolescents.
Violence Exposure and Risk Behavior
According to Jessor and Jessor’s (1977) problem behavior theory, adolesent risk behavior can be defined as a constellation of behaviors that co-occur and may lead to negative health consequences. This theory has been tested and validated across multiple populations and developmental stages (Chun & Mobley, 2010; Monahan, Rhew, Hawkins, & Brown, 2014; Racz, McMahon, & Luthar, 2011), with evidence demonstrating that a range of risk behaviors—including delinquency, rule-breaking, alcohol use, cigarette use, and other substance use—are aspects of a broader underlying construct of risk-taking (O’Connor, Dolphin, Fitzgerald, & Dooley, 2016). Certain behaviors become more normative across adolescent development, and the frequency with which adolescents engage in these risk behaviors across development is not always linear (Chen & Jacobson, 2012). Several heritable and contextual risk factors may explain individual differences in engagement in high-risk behavior across adolescence. For example, at the individual level, sensation-seeking, cognitive abilities, and poor response inhibition are linked to risk-taking (Meyers & Dick, 2010; Nigg et al., 2006). Examples of contextual risk factors include authoritarian parenting, childhood maltreatment and early stressors, and deviant peer relationships (Monahan et al., 2014; Whitesell, Bachand, Peel, & Brown, 2013). Consistent with the concept of developmental equifinality, numerous combinations of risk factors may lead to increased engagement in risk behaviors, and across these varied risk factors, risk-taking behavior has been consistently associated with a range of negative outcomes across development (McGue & Iacono, 2008). Given the heterogeneity in risk behaviors across development, an examination of risk behavior engagement and its longitudinal associations with family processes and violence exposure outcomes in a nationally representative adolescent sample is needed.
Associations have been consistently found between adolescent violence exposure and risk behaviors, including substance use and delinquency (e.g., Homma, Wang, Saewyc, & Kishor, 2012; Moreland et al., 2018; Wright et al., 2013). Previous data from the National Survey of Adolescents-Replication, a nationally representative sample of adolescents aged 12-17, examined the temporal order of this association and demonstrated that the effects may be bidirectional, particularly for boys (Begle et al., 2011). The lifestyle and routine activities theory (Riley, 1987) states that adolescents are more likely to experience or witness violence when they are spending time in community settings where violence is more likely to be committed (Janssen, Dekovic, & Bruinsma, 2014). Consistent with this theory, Begle et al. (2011) found that adolescent boys who experienced victimization subsequently engaged in more risk behavior, and engagement in risk behavior increased the likelihood of experiencing subsequent victimization. Similarly, studies with other samples have documented reciprocal effects between violence exposure and risk behavior (e.g., Mrug & Windle, 2009; Smith & Ecob, 2007). Violence exposure is theorized to increase risk behaviors, including substance use, in part through coping and self-medication (Begle et al., 2011; Brady & Donenberg, 2006). In turn, risk behaviors may increase the likelihood of victimization or re-victimization. Though the relation between risk behavior and violence exposure is likely reciprocal, the current study focuses on risk behavior predicting subsequent (re)victimization in order to identify potential targets to reduce the negative effects of risk behavior on adolescents and, ultimately, to inform the prevention of violence exposure.
Several mechanisms may explain the relation between risk behavior and subsequent violence exposure. Biologically, the use of substances such as alcohol and prescription drugs may lead to impaired decision-making, leaving adolescents more vulnerable to violence (Logan, Walker, Cole, & Leukefeld, 2002). Cigarette use, though not necessarily linked with impairment in decision-making, may be related to violence exposure due to its correlation with other areas of risk, including use of other substances, high impulsivity, and executive functioning deficits (Crane, Hawes, & Weinberger, 2013). Indeed, consistent with problem behavior theory (Jessor & Jessor, 1977), studies examining latent factors of risk behavior have shown that cigarette use loads onto a unitary underlying construct along with other aspects of substance use and delinquent behaviors (Racz et al., 2011). Engagement in substance use (including cigarette use) and delinquency also tend to co-occur with deviant peer affiliation, another risk factor for violence exposure (Vézina et al., 2011). Importantly, these findings suggest that one of the mechanisms by which adolescents are likely to be victimized or re-victimized is through their increased engagement in risk behaviors, including substance use and delinquency. Therefore, identifying protective factors that can mitigate the negative outcomes of risk behavior, including the link between risk behavior and violent victimization—or re-victimization—is an essential aspect of violence exposure prevention.
Family Cohesion as a Protective Factor for Adolescents
The family system is the environment most proximal to adolescents and is among the most influential factors in adolescent adjustment (Bronfenbrenner, 1979). A growing body of research demonstrates that family cohesion, defined as emotional bonding and supportiveness among family members (Maynard & Olson, 1987), serves as a protective factor for adolescents. A number of studies have demonstrated direct effects of family support, broadly defined, on adolescent risk behavior (e.g., Goodrum, Armistead, Tully, Cook, & Skinner, 2017; Tyler & Johnson, 2006). In fact, in a study examining competing theories of the relation between parenting and sexual risk behavior among African American youth, parental support emerged as the most influential aspect of parenting (Simons, Sutton, Simons, Gibbons, & Murry, 2016). In addition to reducing risk behavior, family support and other family-level factors may directly predict fewer victimization experiences for adolescents, such as witnessing community violence (Gorman-Smith, Henry, & Tolan, 2004) and experiencing multiple victimization (Romano, Bell, & Billette, 2011).
Beyond its direct effects, some studies have examined family cohesion as a buffer for adolescents who have experienced traumatic stress. For example, Deane and colleagues (2018) found that family cohesion and support protected adolescents against the negative effects of PTSD on subsequent aggression; youth from highly cohesive families were less likely to exhibit aggressive behavior in the face of PTSD symptoms. Similarly, among a diverse sample of adolescents, those who witnessed violence were less likely to exhibit subsequent violent behavior if they perceived their families as supportive (Brookmeyer, Henrich, & Schwab-Stone, 2005), and in the National Survey of Adolescents-Replication (NSA-R), family cohesion was found to reduce the impact of witnessing community violence on subsequent delinquency (Barr et al., 2011). Family support is thought to be protective for youth by providing a secure and positive relational context in which adolescents can gain a healthy working model of relationships (Simons et al., 2016). Additionally, a warm and supportive family environment bolsters the effectiveness of other parenting practices such as monitoring and behavioral control.
Although research has documented the buffering role of family cohesion in the link between traumatic stress and adolescent outcomes, less is known about how family cohesion may be a protective factor in preventing trauma exposure for adolescents engaging in high-risk behavior. Previous studies have documented that family cohesion directly reduces adolescent risk behavior, but even for those engaged in high-risk activities, it is possible that cohesion may attenuate the negative effects of those behaviors, including (re)victimization. However, the moderating role of cohesion in protecting adolescents against the risky effects of externalizing behaviors on violence exposure has not been adequately explored.
Current Study
The purpose of the current study was to examine longitudinal associations among adolescent risk behavior, family cohesion, violence exposure, and mental health outcomes in the NSA-R, a nationally representative sample of 3,614 adolescents. Specifically, we examined family cohesion as a moderator in the relation between risk behavior and subsequent violence exposure, including sexual abuse and assault, physically abusive punishment, physical assault, and exposure to domestic and community violence. We hypothesized that family cohesion would serve as a protective factor that would attenuate the longitudinal relation between (wave 1) risk behavior and subsequent (wave 2) violence exposure experiences. Based on the potential differential effects of witnessed versus directly experienced violence (Margolin et al., 2010), we conducted post-hoc analyses to determine whether the effects of family cohesion differed for witnessing versus directly experiencing violence. We also investigated (wave 2) violence exposure and family cohesion as predictors of subsequent (wave 3) PTSD and depression, hypothesizing that more types of violence exposure and less family cohesion would each be longitudinally associated with more mental health problems. The roles of demographic and socioeconomic factors were also explored. Given prior research demonstrating higher trauma exposure among racial/ethnic minority individuals and those from lower socioeconomic status (SES) backgrounds (Hatch & Dohrenwend, 2007), we anticipated that adolescents of color (including Black, Latinx, Native American) and those from lower income homes, lower parental education families, or less safe neighborhoods would report more traumatic experiences than their White or higher SES counterparts, respectively.
Method
Participants and Procedures
Data for the current study were drawn from the National Survey of Adolescents – Replication (NSA-R), a longitudinal epidemiological study of adolescents aged 12-17 (N = 3,604). The primary aims of the NSA-R study were to assess prevalence of traumatic events, such as physically abusive punishment, physical assault, sexual abuse and assault, and exposure to community and domestic violence, among adolescents; and to identify the mental health correlates of these exposures. Data were collected at three waves, each one year apart, between 2005 and 2010. All study procedures were approved by the Institutional Review Board of the Medical University of South Carolina. Detailed descriptions of the procedures and sampling methods can be found in Wolitzky-Taylor et al. (2008) and Zinzow et al. (2009). Of the 6,694 families in which parents completed an interview identifying at least one eligible adolescent, 1,268 (18.9%) parents refused participation for their adolescents, 188 (2.8%) adolescents refused to participate after parental consent, 199 (1.8%) interviews were initiated but not completed, and 1,505 (22.5%) eligible adolescents could not be located during the field period for interviews. The remaining 3,614 families, in which both parent and adolescent interviews were completed at Wave 1, included a national probability sample (n = 2,459) as well as an oversample of urban-dwelling adolescents (n = 1,155). A total of 2,511 (69.5% of Wave 1) adolescents completed Wave 2 assessments, and 1,653 (45.7% of Wave I) completed Wave 3 assessments. For the current study, 10 participants were excluded because they fell outside of the 12 to 17 age range, resulting in a final sample size of n = 3,604.
Demographic characteristics of the sample are described in Table 1. The average age of adolescents was 14.51 (SD = 1.70, range = 12-17) at Wave 1, 15.72 (SD = 1.76, range = 12-20) at Wave 2, and 16.76 (SD = 1.77, range = 13-21) at Wave 3. Attrition analyses are detailed in Zinzow et al. (2009) and revealed that completers were more likely to be older by 0.1 years, report lower household income, be female, have a female (vs. male) parent participating in the interview, and report living in a large city or town. Completers and non-completers did not differ on household size, race/ethnicity, parent marital status, parent employment status, or parent education. The significant differences described above were very small and unlikely to be clinically meaningful (Zinzow et al., 2009). Less than 2% of raw data was missing on any Wave 1 variable. At Wave 2, less than 30% of raw data was missing on any variable. Due to high attrition, Wave 3 variables had the most missing raw data, with between 53% and 68% missing data. However, this level of missing data was mitigated by the use of full information likelihood estimation (FIML) in Mplus 8. With this estimation approach, less than 1% of data was missing for all Wave 1 and Wave 2 variables, and less than 35% was missing for Wave 3 variables.
Table 1.
Descriptive Statistics for All Study Variables (N = 3604, Weighted)
| Percentage | Mean | Standard Deviation | Range | ||
|---|---|---|---|---|---|
| Min | Max | ||||
| Child Age at Wave 1 | 14.51 | 1.70 | 12 | 17 | |
| Child Age at Wave 2 | 15.72 | 1.76 | 12 | 20 | |
| Child Age at Wave 3 | 16.76 | 1.77 | 13 | 21 | |
| Child Gender | |||||
| Male | 51.3% | ||||
| Female | 48.7% | ||||
| Child Race/Ethnicity | |||||
| White/Caucasian | 65% | ||||
| Black/African American | 16% | ||||
| Hispanic/Latino | 11% | ||||
| Asian/Pacific Islander | 3% | ||||
| Native American/Alaska Native | 2% | ||||
| Not Reported | 3% | ||||
| Community Setting | |||||
| Urban | 29% | ||||
| Suburban | 50% | ||||
| Rural | 21% | ||||
| Household Income | |||||
| Less than $20,000 | 13% | ||||
| $20,000 to $50,000 | 32% | ||||
| More than $50,000 | 55% | ||||
| Parental Education Level | |||||
| 8th grade or less | 1.3% | ||||
| Some high school | 5.7% | ||||
| High school | 27.2% | ||||
| Some college | 28.3% | ||||
| Four year college | 21.2% | ||||
| Some graduate school | 2.5% | ||||
| Graduate degree | 13.8% | ||||
| Neighborhood Safety | 2.26 | 1.20 | 1 | 4 | |
| Family Cohesion | 2.52 | 0.37 | 1 | 3 | |
| Violence Exposure1 | Wave 1 | Wave 2 | Wave 3 | ||
| Sexual Abuse/Assault | 7.5% | 2.1% | 2.3% | ||
| Physical Assault | 15.6% | 5.3% | 3.2% | ||
| Physically Abusive Punishment | 12.3% | 2.9% | 1.6% | ||
| Witnessed Domestic Violence | 8.9% | 1.2% | 1.0% | ||
| Witnessed Community Violence | 37.8% | 18.2% | 13.2% | ||
| Mean Violence Exposure Count | .83 | .30 | |||
| Risk Behaviors | Wave 1 | ||||
| Cigarette Use | 25% | ||||
| Alcohol Use | 30.8% | ||||
| Prescription Drug Use | 6.7% | ||||
| Club Drug Use | 3.0% | ||||
| Delinquent Behaviors | 20.8% | ||||
| Mental Health Outcomes2 | Wave 1 | Wave 2 | Wave 3 | ||
| Posttraumatic Stress Disorder | 8.1% | 7.5% | 7.6% | ||
| Major Depressive Disorder | 14% | 10.1% | 10.3% | ||
Note. Data are weighted according to 2005 U.S. Census estimates.
Wave 2 and Wave 3 violence exposure rates reflect new incidents of violence occurring between the prior and current wave (i.e., past year).
Wave 2 and Wave 3 mental health outcomes reflect meeting diagnostic criteria in the time since the prior wave (i.e., past year).
Measures
Demographic and socioeconomic factors.
Demographic variables were measured using standard questions from the U.S. Census Bureau (1988). Adolescent-level demographics included age, gender, and race/ethnicity. Race/ethnicity was analyzed as five dummy-coded variables reflecting non-Hispanic White, Black/African American, Asian/Pacific Islander, Native American, and Hispanic/Latino. Family-level demographics, reported by parents, included community setting (i.e., urban, suburban, or rural), parental education level, household income (measured on a 3-point ordinal scale from <$20,000, $20,000-50,000, and >$50,000), and neighborhood safety. Neighborhood safety was measured using one item (“How concerned are you about your [age]-year-old’s safety in your neighborhood?”) with ordinal response options ranging from 1 = Not at all concerned to 4 = Very concerned.
Risk behaviors.
Consistent with previous NSA-R research (e.g., Begle et al., 2011), Wave 1 risk behavior was measured as a latent factor composed of five binary (yes/no) variables reflecting cigarette use, alcohol use, prescription drug use, club drug use, and delinquency. The final latent variable for risk behavior, while comprised of five binary indicators, was a continuous variable reflecting the common variance across each of the types of risk behavior included. Sample substance use items included, “Have you ever tried cigarette smoking, even one or two puffs?” and “Have you ever, even once, had a full drink of beer, wine, liquor, or any alcoholic beverage?” A drink of alcohol was defined as one can of beer, one 4-ounce glass of wine, or one shot of liquor. For prescription drug use, adolescents were asked a series of questions assessing the use of specific prescription drugs, and these questions were combined into a dichotomous variable indicating the use of any prescription drugs for non-medical reasons. Similarly, for club drug use, a series of questions about specific club drugs were combined into one dichotomous variable. Delinquency was measured with a series of items adapted from the National Youth Survey (Elliott, 1994), which assessed whether adolescents had ever engaged in certain behaviors, including physically attacking someone, selling drugs, breaking into a house to steal, attempting to steal a motor vehicle, and being sent to jail or juvenile detention. These items were combined into a single dichotomous variable reflecting ever engaging in one or more delinquent behaviors.
Family cohesion.
Family cohesion at Wave 2 was assessed using six items related to adolescents’ perceptions of support and relationship quality among family members. This measure was developed for the NSA-R study (Kilpatrick et al., 2000). Response options were on a 3-point Likert-type scale ranging from 1 = Not at all to 3 = Very much. Sample items include, “How close do family members usually feel to each other? Would you say they feel very close, somewhat close, or not close?” and “How hard is it for family members to ask each other for help? Would you say it is very hard, somewhat hard, or not hard?” Items were averaged to create a scale score, with possible scores ranging from 1 to 3 and higher scores indicating more family cohesion. The scale showed adequate reliability, with Cronbach’s alpha = 0.71 in this sample.
Violence exposure.
Violence exposure at all three waves was measured as a count variable consisting of five different types of victimization experiences, including sexual abuse/assault, physically abusive punishment, physical assault, exposure to community violence, and exposure to domestic violence. Each violence exposure variable was assessed using a series of questions from a modified version of the violence assessment in the original National Survey of Adolescents study (Kilpatrick et al., 2000). Each type of violence exposure was coded dichotomously (0 or 1) according to whether the adolescent had experienced that form of violence ever (at Wave 1) or since the last interview (at Waves 2 and 3). Dichotomous scores for all five violence exposure types were summed to create a count variable, and the count variable had a possible range of 0 to 5. For the exploratory post-hoc analyses examining separate models for directly experienced vs. witnessed violence, two count variables were created. The count variable for directly experienced violence was a sum of the dichotomous variables for physically abusive punishment, physical assault, and sexual abuse/assault (range 0-3). The count variable for witnessed violence was a sum of the dichotomous variables for witnessing community violence and witnessing domestic violence (range 0-2).
Mental health outcomes.
Posttraumatic stress disorder.
PTSD was assessed using the PTSD module from the original NSA survey (Kilpatrick et al., 2000) and National Women’s Survey (Resnick et al., 1993; Kilpatrick, Resnick, Saunders, & Best, 1989), which is a structured diagnostic interview of DSM-IV PTSD symptoms. This measure has been validated against the PTSD module of the Structured Clinical Interview for the DSM (SCID; Spitzer, Williams, & Gibbon, 1987) and demonstrates good psychometric properties. Based on symptoms reported, PTSD was coded dichotomously (0 or 1) as present (i.e., meets diagnostic criteria) or not present ever (Wave 1) or since the prior interview (Waves 2 and 3). Coding was based on meeting symptom threshold criteria, and the functional impairment criterion was not considered in this coding.
Depression.
The presence of a major depressive episode (MDE) was assessed using the Depression module of the original NSA survey (Kilpatrick et al., 2000), a structured interview measuring DSM-IV MDE diagnostic criteria using a yes/no response to assess symptom presence. This measure has demonstrated good psychometric properties (Kilpatrick et al., 2003; Boscarino et al., 2004) and has been validated against the Brief Symptom Inventory-18. Scores were coded dichotomously (0 or 1) based on the presence or absence of a MDE ever (Wave 1) or since the previous interview (Waves 2 and 3). For the purpose of this study, the functional impairment criterion was not considered, and the presence of a MDE was based on meeting symptom threshold criteria.
Data Analytic Plan
Data were weighted according to 2005 U.S. Census estimates to approximate national distributions of urban vs. suburban vs. rural setting, age, and sex. All analyses were conducted in Mplus 8.0 using a longitudinal structural equation modeling framework. First, a confirmatory factor analysis evaluating a latent factor of risk behavior at Wave 1 was tested. Next, a measurement model was specified including the risk behavior factor and all other variables (Wave 1 and 2 violence exposure; Wave 2 family cohesion; depression and PTSD at all waves; and demographic covariates). A structural main effects model was then tested to evaluate longitudinal relations among risk behavior, family cohesion, and violence exposure. To evaluate the moderating role of family cohesion, a model including a latent interaction between risk behavior and family cohesion predicting violence exposure was specified. Finally, Wave 3 depression and PTSD were added to the model to assess longitudinal predictors of mental health outcomes. Measurement models and main effects models were tested using weighted least square mean and variance adjusted (WLSMV) estimation to accommodate the ordinal outcome variables. Models with the latent interaction term were tested using maximum likelihood estimation with robust standard errors (MLR). Model fit was evaluated using chi-square (smaller, nonsignificant values indicate better model fit), CFI (>.95 indicates good fit), TLI (>.95 indicates good fit), and RMSEA (<.08 indicates good fit). Thresholds for fit indices follow the convention of Hu and Bentler (1999).
Results
Descriptive Results
Descriptive results, including means, standard deviations, and frequencies, of all study variables are presented in Table 1. Bivariate correlations among primary study variables are presented in Table 2. Detailed descriptive data regarding rates of violence exposure are further discussed in Zinzow et al. (2009). In this nationally representative sample, the average number of different types of violence experienced by adolescents at Wave 1 was 0.83. Between Wave 1 and Wave 2, adolescents on average experienced 0.30 different types of violence exposure. The most commonly reported form of victimization across waves was exposure to community violence.
Table 2.
Bivariate Correlations among Primary Study Variables (N = 3604, Weighted)
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age1 | -- | ||||||||||||||
| 2. Cigarette Use1 | .33** | -- | |||||||||||||
| 3. Alcohol Use1 | .47** | .51** | -- | ||||||||||||
| 4. Rx Drug Use1 | .18** | .33** | .30** | -- | |||||||||||
| 5. Club Drug Use1 | .15** | .27** | .24** | .40** | -- | ||||||||||
| 6. Delinquency1 | .20** | .35** | .29** | .25** | .24** | -- | |||||||||
| 7. Family Cohesion2 | −.04 | −.15** | −.12** | −.08** | −.06* | −.12** | -- | ||||||||
| 8. Victimization1 | .21** | .35** | .33** | .26** | .22** | .41** | −.22** | ||||||||
| 9. Victimization2 | .08** | .16** | .19** | .14** | .17** | .27** | −.20** | .40** | -- | ||||||
| 10. Victimization3 | .03 | .18** | .14** | .08* | .13** | .23** | −.16** | .27** | .42** | -- | |||||
| 11. PTSD1 | .12** | .17** | .17** | .18** | .09** | .18** | −.12** | .33** | .24** | .20** | -- | ||||
| 12. MDD1 | .15** | .23** | .23** | .21** | .12** | .18** | −.16** | .35** | .25** | .17** | .53** | -- | |||
| 13. PTSD2 | .07** | .11** | .09** | .11** | .06* | .09** | −.20** | .24** | .31** | .22** | .32** | .33** | -- | ||
| 14. MDD2 | .09** | .16** | .12** | .14** | .09** | .09** | −.25** | .21** | .29** | .19** | .33** | .36** | .53** | -- | |
| 15. PTSD3 | .03 | .12** | .09** | .10** | .06* | .10** | −.16** | .22** | .17** | .24** | .27** | .26** | .31** | .34** | -- |
| 16. MDD3 | .01 | .13** | .08** | .06* | .04 | .09** | −.14** | .20** | .15** | .22** | .26** | .25** | .32** | .36** | .63** |
Note.
p < .05;
p < .001.
Subscripts indicate timepoint: Wave 1, Wave 2, or Wave 3. Data are weighted according to 2005 U.S. Census Estimates.
At the bivariate level, all primary study variables were correlated with one another in the expected direction. Risk behaviors were positively intercorrelated with one another. Family cohesion was significantly negatively correlated with risk behaviors, violence exposure, and mental health outcomes. Violence exposure was positively associated with risk behaviors and mental health outcomes. PTSD and MDD were positively correlated with one another. Compared to younger adolescents, older adolescents reported significantly more substance use, delinquency, violence exposure at waves 1 and 2, and mental health problems at waves 1 and 2. No effects of age were observed for family cohesion or any wave 3 variables.
Primary Results
Several demographic variables, including adolescent gender, race/ethnicity, household income, parental education, community setting (urban, suburban, or rural), and neighborhood safety, were covaried in all models. First, using the weighted least square mean and variance adjusted (WLSMV) estimator, a confirmatory factor analysis testing a latent factor of adolescent risk behavior at Wave 1 revealed good model fit (χ2 (5, N = 3604) = 15.483, p = 0.009, CFI = 1.00, RMSEA = 0.02 [0.01, 0.04]). Each of the five binary observed indicators (cigarette use, alcohol use, prescription drug use, club drug use, and delinquency) loaded onto the risk behavior factor significantly with a loading > 0.6. Given the wide age range of the sample, measurement invariance was confirmed using a multiple group analysis between younger (12-14) and older (15-17) adolescents. These age groupings were selected based on previously established developmental stages of adolescence, with age 12 to 14 comprising early adolescence and age 15 to 17 considered middle adolescence (Eccles, 1999; Spano, 2004). Before testing the structural models, a measurement model was evaluated using WLSMV estimation. The measurement model included the risk behavior latent factor, family cohesion, violence exposure at Waves 1 and 2, mental health outcomes at all three waves, and all covariates. Results revealed good model fit (χ2 (85, N = 3604) = 658.866, p < 0.001, CFI = 0.95, RMSEA = 0.04 [0.04, 0.05]), with variables intercorrelated in the expected direction. Factor loadings for the risk behavior latent factor were significant and ranged from 0.69 to 0.87.
Next, a series of longitudinal structural equation models was specified to examine relations among risk behavior, family cohesion, violence exposure, and mental health outcomes across time. Across all models, missing data was handled using full information maximum likelihood (FIML) estimation under the missing at random (MAR) assumption in Mplus 8.0, an accepted method for handling missing data in structural equation models (Enders, 2001).
Model 1: Main effects.
First, using WLSMV estimation, a main effects model was specified with paths from risk behavior at Wave 1 to family cohesion and violence exposure at Wave 2; from family cohesion to violence exposure at Wave 2; and violence exposure from Wave 1 to Wave 2. Figure 1 displays results of the main effects model. This model adequately fit the data (χ2 (62, N = 3232) = 509.17, p < .001, CFI = .92, TLI = .85, RMSEA = 0.05 [0.04, 0.05]). As expected, violence exposure at Wave 2 was significantly predicted by more risk behaviors at Wave 1 (β = 0.14, p < .001), lower family cohesion at Wave 2 (β = −0.15, p < .001), and prior levels of violence exposure at Wave 1 (β = 0.34, p < .001). Higher levels of Wave 1 risk behavior were correlated with less Wave 2 family cohesion (r = −0.22, p < .001), and risk behavior was correlated with concurrent violence exposure at Wave 1 (r = .48, p < .001). As a sensitivity analysis to confirm the relation between risk behavior and violence exposure across adolescence, age was examined as a moderator in the relation between Wave 1 risk behavior to Wave 2 victimization. This analysis revealed that the latent interaction between risk behavior and age was nonsignificant in predicting violence exposure (β = −0.02, n.s.), suggesting that the effect of risk behavior on subsequent violence exposure did not significantly vary by age.
Figure 1.
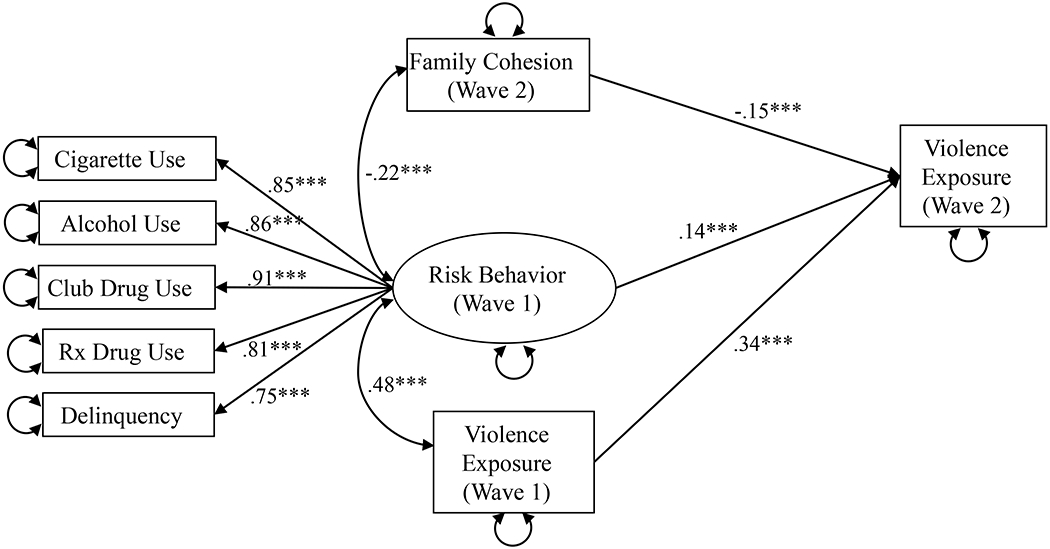
Structural regression model testing main effects among risk behavior, family cohesion, and victimization.
Note. *p < .05; **p < .01; ***p < .001. Standardized path coefficients displayed. Solid lines indicate significant paths. Dashed lines indicate nonsignificant paths. Covariates are not depicted; all primary variables were regressed on child age, gender, race/ethnicity, household income, parental education, urban vs. suburban vs. rural setting, and neighborhood safety.
Several demographic effects were detected in the main effects model. Compared to their White counterparts, Black/African American adolescents engaged in fewer risk behaviors (β = −0.06, p = .005) and Native American adolescents engaged in more (β = 0.07, p = .001). Girls (β = −0.06, p = .007), younger adolescents (β = .55, p < .001), adolescents from higher income homes (β = −.05, p = .043), and adolescents whose parents attained higher education levels (β = −0.06, p = .011) reported less risk-taking than their counterparts. At Wave 1, Native American (β = 0.05, p = .001), Hispanic/Latino (β = 0.04, p = .023), and Black adolescents (β = 0.06, p = .001) were more likely to be victimized than other racial/ethnic groups, but this effect was not observed for Native American adolescents at Wave 2. Older youth reported more violence exposure at Wave 1 (β = 0.22, p < .001), but less at Wave 2 (β = −0.06, p = .023). Household income was significantly related to violence exposure and family cohesion; adolescents from lower income homes reported more violence exposure (β = −0.07, p = .001) and less cohesion (β = −0.10, p < .001).
Model 2: Moderating effect of family cohesion.
To test the moderating effect of family cohesion in the relation between risk behavior and subsequent violence exposure, a model was specified with a latent variable interaction between risk behavior and family cohesion. Maximum likelihood estimation with robust standard errors (MLR) was used to test the interaction between risk behavior and family cohesion. As with the prior model, demographic variables were covaried in the model. Traditional model fit indices (e.g., CFI, TLI, RMSEA, SRMR) are not available because they have not been developed for latent variable interaction models (Maslowsky, Jager, & Hemken, 2015). Consistent with hypotheses, the interaction between family cohesion and risk behavior was significantly related to violence exposure at Wave 2 (β = −0.09, p = .004). The interaction was probed using simple slopes at low (1.5 SD below mean), medium (mean), and high (1.5 SD above mean) levels of family cohesion. Family cohesion significantly attenuated the association between risk behaviors and subsequent violence exposure. Specifically, at low (B = 0.46, p = .001) and medium (B = 0.40, p = .001) levels of cohesion, risk behavior significantly predicted more violence exposure. At high levels of cohesion, the relation between risk behavior and violence exposure was significantly reduced, though still significant (B = 0.33, p < .001). Figure 2 displays a graph of the moderation effect.
Figure 2.
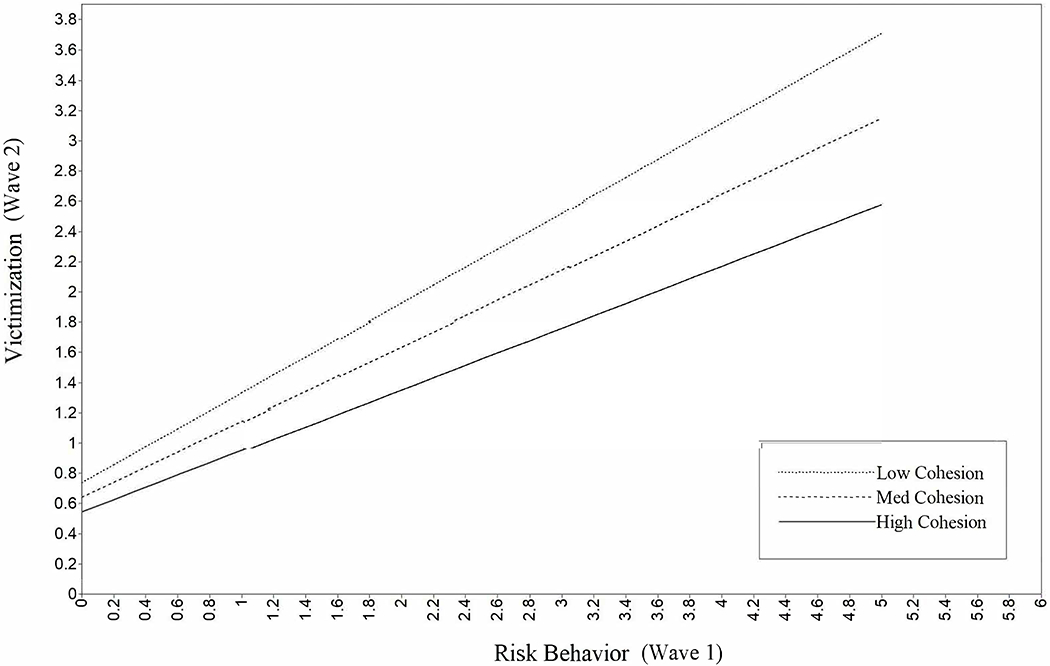
Graph displaying family cohesion as a moderator in the relation between adolescent risk behavior and victimization.
Model 3: Mental health outcomes.
To examine longitudinal predictors of mental health outcomes at Wave 3, a final model using MLR estimation was specified predicting PTSD and MDD at Wave 3. A structural regression model was specified with the latent interaction term between risk behavior and family cohesion, and the addition of paths from violence exposure and family cohesion at Wave 2 to subsequent mental health outcomes at Wave 3. All variables were regressed on demographic covariates. Results of the final model, including standardized parameter estimates, are displayed in Figure 3. PTSD and MDD at Wave 3 were significantly related to prior levels of PTSD and MDD at Waves 1 and 2 and lower levels of family cohesion at Wave 2. PTSD and MDD were both related to more violence exposure at Wave 2. MDD and PTSD were positively concurrently correlated with one another. Relations among risk behaviors, family cohesion, and violence exposure were consistent with the prior models.
Figure 3.
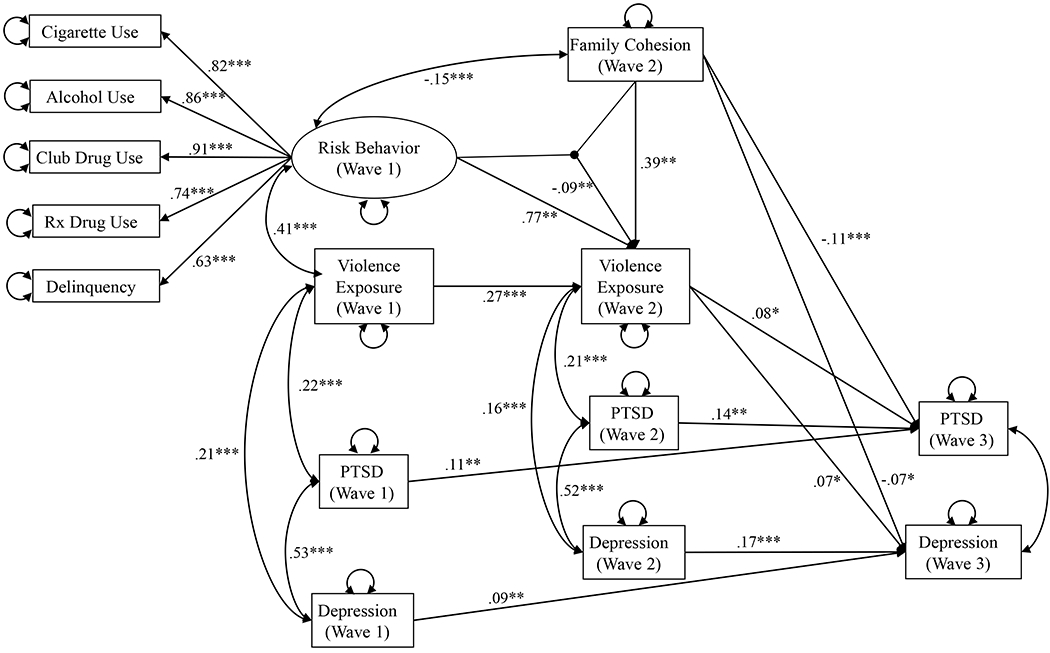
Final structural regression model testing latent interaction between risk behavior and family cohesion in predicting victimization, and longitudinal relations predicting subsequent mental health outcomes.
Note. *p < .05; **p < .01; ***p < .001. Standardized path coefficients displayed. Covariates are not depicted; all primary variables were regressed on child age, gender, race/ethnicity, household income, parental education, urban vs. suburban vs. rural setting, and neighborhood safety.
Girls were more likely to exhibit PTSD (β = .07, p = .007) and depression (β = .11, p < .001) at Wave 3, and Asian adolescents were less likely than their White counterparts to report mental health symptoms (PTSD β = −0.03, p = .013; MDD β = −0.03, p < .001). Adolescents living in suburban areas were more likely to report MDD at Wave 3 (β = .07, p = .013). Older adolescents (β = .61, p < .001) and Native American adolescents (β = .07, p = .001) reported more risk behavior than younger and White adolescents, respectively. Household income was significantly positively correlated with family cohesion (β = .10, p < .001), and neighborhood safety was negatively related to family cohesion (β = −0.05, p = .022). Compared to White adolescents, Black/African American adolescents reported higher rates of violence exposure at Wave 1 (β = 0.08, p = .001) and Wave 2 (β = .07, p = .006), and Asian adolescents reported lower rates at Wave 2 (β = −0.09, p = .004). Consistent with the main effects model, older adolescents were more likely to have experienced victimization at Wave 1 (β = .20, p < .001), but less likely at Wave 2 (β = −0.09, p = .002).
Exploratory analyses evaluating directly experienced vs. witnessed violence.
To assess whether effects differed according to directly experienced or witnessed violence, two additional models were tested examining these aspects of violence exposure separately. In the first model, violence exposure was conceptualized as a count variable of direct experiences of violent victimization, including sexual abuse/assault, physically abusive punishment, and physical assault. In the second model, violence exposure was conceptualized as witnessing violence (community-based and domestic). Results revealed that family cohesion moderated the relation between risk behaviors and direct experiences of violence (β = −0.14, p = .001), but not witnessing violence (β = −0.04, n.s.). Witnessing violence was directly positively predicted by risk behaviors (β = 0.16, p = .010), but not by family cohesion or the risk behavior by family cohesion interaction.
Demographic variables were differentially related to direct victimization versus witnessed violence. At Wave 1, Black/African American adolescents were the only racial/ethnic group that reported higher rates of both direct experiences of victimization (β = 0.05, p = .047) and witnessing violence (β = 0.08, p = .005). Hispanic/Latino adolescents and those from lower income homes were more likely to witness, but not directly experience, violence. No demographic variables were significantly related to experiencing victimization between Waves 1 and 2. Asian adolescents and adolescents in rural settings were less likely to witness violence between Waves 1 and 2.
Discussion
The purpose of the current study was to examine the buffering role of family cohesion in the relation between adolescent risk behavior and subsequent violence exposure, and to examine family cohesion and violence exposure as longitudinal predictors of PTSD and depression. Findings revealed that high family cohesion significantly attenuated the longitudinal relation between risk behaviors and violence exposure. Further, family cohesion directly predicted reduced risk of PTSD and depression, even when accounting for the effect of sociodemographic variables, prior levels of symptoms, and violence exposure. Violence exposure at Wave 2 predicted subsequent PTSD, but unexpectedly, not depression. Results highlight the central role of families in protecting adolescents against risk behavior and maladaptive effects of violence exposure.
Consistent with hypotheses and previous literature (Gorman-Smith et al., 2004), family cohesion was found to have a protective effect for adolescents. After accounting for demographic and contextual variables and the direct relation between risk behaviors on subsequent cohesion, family cohesion appeared to buffer adolescents against the negative effects of engaging in risk behaviors on experiencing victimization. Adolescents who engaged in risky behaviors were less likely to experience violence in the context of a cohesive, supportive family environment. Explanations of this finding may relate to families’ level of communication and parental monitoring. In highly cohesive families, parents may have more knowledge of their children’s whereabouts and can monitor safety more closely, even when adolescents are engaging in risky behaviors; previous literature suggests that parental monitoring can reduce risk of victimization (Janssen et al., 2014). Further, parental support may enhance the effectiveness of other parenting practices, such as monitoring and behavioral control (Lippold, Greenberg, Graham, & Feinberg, 2014). Further, adolescents who perceive their families as cohesive may be more likely to turn to family members for guidance and support, which may in turn reduce the risk of experiencing violence. Consistent with previous research identifying attachment theory as an important explanation for the protective role of family support (Simons et al., 2016), family cohesion may serve as a buffer by providing adolescents with healthy models of relationships and in turn equipping them with knowledge and tools to seek and maintain healthy relationships with peers. Additionally, highly cohesive families may engage in more communication about risk and safety compared to families low in cohesion. Given reciprocal relations between risk behavior and violence exposure (Mrug & Windle, 2009; Smith & Ecob, 2007) and between family support and adolescent functioning (Elkins, Fite, Moore, Lochman, & Wells, 2014), it is also important to note that the protective effect of family cohesion likely operates in the context of bidirectional relations among these processes over time. For example, early violence exposure may reduce subsequent family cohesion via adolescents’ increased engagement in risk behaviors, and these risk behaviors may subsequently increase the likelihood of further violence exposure and other negative outcomes. It is also possible that family cohesion functions as a mediator in the longitudinal reciprocal relation between risk behavior and violence exposure. Future research should explore these possible alternative paths.
Exploratory post-hoc analyses revealed that the moderating effect of family cohesion in the association between risk behavior and subsequent violence exposure differed for violence that was directly experienced versus witnessed. Though both direct and indirect experiences of violence are related to substance use, there may be unique types of associations across forms of victimization (e.g., Wright et al., 2013). As described in the lifestyle and routine activities theory (Riley, 1987), which states that youth are at higher risk of being exposed to violence or trauma when they are spending time with peers or in community settings in which violence is more likely to occur, witnessing violence in the community may be more strongly predicted by risk behaviors, such as substance use and delinquency, given the overlap in the time spent in the community. For example, in the current study, correlations between risk behaviors (substance use and delinquency) and witnessed community violence were stronger than those between risk behavior and directly experienced violence. Perceived support and closeness with family members may protect risk-taking adolescents from certain forms of violence exposure, such as those experienced in interpersonal relationships including sexual or physical assault, but not from exposure to violence in the community. Alternatively, it is also possible that because the witnessed violence variable included exposure to domestic violence, the role of the perpetrator is influencing the pattern of findings. For youth who have witnessed domestic violence, the measurement of family cohesion may reflect the adolescent’s relationship with the offending caregiver in the domestic violence incident. Sousa et al. (2011) noted that family support may serve as a more important protective factor when considering relationships with non-offending caregivers versus offending caregivers. Family cohesion may not be as effective a buffer when considering closeness between the adolescent and an offending caregiver.
As expected based on prior research (e.g., Kilpatrick et al., 2003), violence exposure predicted subsequent PTSD and depression. Adolescents who experienced new incidents of physically abusive punishment, physical assault, sexual abuse/assault, or witnessed violence between Waves 1 and 2 were more likely to report mental health symptoms at Wave 3. A higher number of violence incidents longitudinally predicted PTSD and depression, over and above the effect of prior levels of symptoms. This finding is consistent with prior research demonstrating a cumulative impact of polyvictimization (e.g., Adams et al., 2016; Suliman et al., 2009).
Within a multivariate model accounting for the role of demographic variables, violence exposure, and prior levels of symptoms, family cohesion remained a significant predictor of subsequent mental health outcomes. Consistent with a large body of evidence, adolescents who are victimized are at risk of experiencing posttraumatic stress and depression; however, family cohesion serves as a protective factor and is associated with fewer mental health concerns across time, with small but statistically and clinically significant effect sizes. This finding is similar to results of previous studies indicating inverse relations between family support and mental health symptoms (DiClemente et al., 2018; Guassi Moreira & Telzer, 2015) and highlights the potential benefits of supportive family relationships for reducing or preventing mental health difficulties.
Several sociodemographic variables emerged as significant correlates of risk behavior, family cohesion, violence exposure, and mental health symptoms. Findings suggest that ethnic minority adolescents and adolescents from lower socioeconomic backgrounds face higher risk for violence exposure than White adolescents and those from higher SES families, respectively. Consistent with previous literature (e.g., Estrada-Martínez, Caldwell, Schulz, Diez-Roux, & Pedraza, 2013), being from a lower income family, having parents with lower educational attainment, and living in a neighborhood that parents perceive as unsafe are each potential risk factors that were related to more violence exposure, less family cohesion, and/or more risk behaviors. This pattern of findings is consistent with the family stress theory (Conger et al., 2002), suggesting that socioeconomic strain affects youth outcomes indirectly via caregivers’ distress and compromised parenting and family relationships. Notably, racial and ethnic differences were still observed even when accounting for the effect of socioeconomic indicators. For example, Black/African American adolescents exhibited fewer risk behaviors but more violence exposure experiences than their White counterparts, and were the only racial group that experienced higher rates of both directly experienced and witnessed violence compared to White adolescents. Hispanic/Latino and Native American adolescents also experienced more victimization compared to White adolescents. These findings highlight racial and ethnic differences that exist beyond socioeconomic context, and may reflect risk factors related to racial discrimination and structural inequities (Kaufman & Cooper, 2001).
Limitations and Future Directions
Findings should be interpreted in light of study limitations. First, a primary limitation of this study is the reliance on adolescent report for most variables. Although previous research recommends examining adolescents’ self-reports of their own functioning and family environment (Jensen et al., 1999; Klein, Dougherty, & Olino, 2005; Schulte et al., 2017), findings may reflect common reporter variance and future research should triangulate findings from multiple reporters in order to bolster these conclusions. Second, family cohesion was only assessed at Wave 2 in the larger NSA-R study, precluding the possibility of examining baseline cohesion as an exogenous variable in the model. Third, our statistical modeling approach assumes an underlying linear trajectory for risk behaviors, though evidence suggests that changes in these behaviors may not be linear across adolescent development (Chen & Jacobson, 2012); future research should account for nonlinear growth in risk behaviors across time and should consider developmental timing of violence exposure incidents. An additional limitation is the high attrition observed across waves, with 46% completing all three waves; though attrition analyses revealed few meaningful differences between completers and non-completers, findings must be considered in the context of this limitation. Also, other family processes such as parenting practices were not assessed in the larger NSA-R study; future research should examine multiple aspects of the family environment across timepoints to determine the most impactful intervention targets for family-level prevention and intervention efforts. Further, though sociodemographic variables emerged as relevant correlates of cohesion, violence exposure, risk behavior, and mental health symptoms, the assessment of cultural and contextual variables was limited in this study. For example, previous research has demonstrated the role of adolescents’ own perceptions of their neighborhood safety in predicting adolescent risk behavior (e.g., Leventhal & Brooks-Gunn, 2000). Perceived racial discrimination has also been identified as a risk factor for trauma-related mental health symptoms among people of color—an association which may be explained by both higher rates of exposure to stressful life events as well as higher vulnerability to experiencing symptoms as a result of these events (Kirkinis, Pieterse, Martin, Agiliga, & Brownell, 2018). Thus, beyond racial identification, adolescents’ perceptions of racism and discrimination may be an important stressor to examine in relation to racial/ethnic differences in violence exposure and mental health outcomes. Future research should investigate these contextual variables from adolescents’ perspectives and explore relations with violence exposure and mental health. Finally, these findings should be replicated with assessment tools that reflect the changes made in DSM-5.
Conclusions and Clinical Implications
Despite its limitations, the current study represents an important contribution in identifying risk and protective factors for violence exposure and mental health outcomes. Findings underscore the protective role of family cohesion for adolescents. This study is the first to demonstrate family cohesion as a buffer attenuating the longitudinal risky effects of substance use and delinquency on subsequent violence exposure within an epidemiological sample. Using a nationally representative sample facilitates generalization of the findings across adolescents from a wide range of socioeconomic, racial/ethnic, and geographic backgrounds. The longitudinal design of this study also allows for the exploration of long-term (one- to two-year) outcomes, further highlighting the potentially detrimental over-time effects of violence, as well as the long-term benefits of cohesion. Findings point to family relationships and cohesion as potential targets for prevention and intervention efforts to reduce the risk of adolescent violence exposure and mental health problems, particularly for adolescents who are engaging in high risk behaviors. Family-based interventions, such as Risk Reduction through Family Therapy (RRFT; Danielson et al., 2010), targeting the family context to reduce risk behavior among trauma-exposed adolescents may be enhanced by intervening on cohesion within the family environment, to reduce the chance of further re-victimization. Prevention efforts among adolescents who have not experienced trauma should also consider ways to bolster supportive relationships within families, to prevent trauma exposure and reduce risk for mental health symptoms.
Acknowledgements:
This study was supported by the National Institute of Child Health and Human Development (R01 HD046830; PI: Kilpatrick) and the National Institute of Mental Health (T32 MH18869, PIs: Danielson & Kilpatrick).
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- Adams ZW, Moreland A, Cohen JR, Lee RC, Hanson RF, Danielson CK, … Briggs EC (2016). Polyvictimization: Latent profiles and mental health outcomes in a clinical sample of adolescents. Psychology of Violence, 6(1), 145–155. 10.1037/a0039713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barr SC, Hanson R, Begle AM, Kilpatrick DG, Saunders B, Resnick H, & Amstadter A (2011). Examining the Moderating Role of Family Cohesion on the Relationship Between Witnessed Community Violence and Delinquency in a National Sample of Adolescents. Journal of Interpersonal Violence, 27(2), 239–262. 10.1177/0886260511416477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begle AM, Hanson RF, Danielson CK, McCart MR, Ruggiero KJ, Amstadter AB, … Kilpatrick DG (2011). Longitudinal pathways of victimization, substance use, and delinquency: Findings from the National Survey of Adolescents. Addictive Behaviors, 36(7), 682–689. 10.1016/j.addbeh.2010.12.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benedini KM, Fagan AA, & Gibson CL (2016). The cycle of victimization: The relationship between childhood maltreatment and adolescent peer victimization. Child Abuse and Neglect, 59, 111–121. 10.1016/j.chiabu.2016.08.003 [DOI] [PubMed] [Google Scholar]
- Brady SS, & Donenberg GR (2006). Mechanisms linking violence exposure to health risk behavior in adolescence: Motivation to cope and sensation seeking. Journal of the American Academy of Child and Adolescent Psychiatry, 45(6), 673–680. 10.1097/01.chi.0000215328.35928.a9 [DOI] [PubMed] [Google Scholar]
- Brookmeyer KA, Henrich CC, & Schwab-Stone M (2005). Adolescents who witness community violence: can parent support and prosocial cognitions protect them from committing violence? Child Development, 76(4), 917–929. [DOI] [PubMed] [Google Scholar]
- Chen P, & Jacobson KC (2012). Developmental trajectories of substance use from early adolescence to young adulthood: Gender and racial/ethnic differences. Journal of Adolescent Health. 10.1016/j.jadohealth.2011.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chun H, & Mobley M (2010). Gender and grade-level comparisons in the structure of problem behaviors among adolescents. Journal of Adolescence. 10.1016/j.adolescence.2009.03.010 [DOI] [PubMed] [Google Scholar]
- Cloitre M, Stolbach BC, Herman JL, Van Der Kolk B, Pynoos R, Wang J, & Petkova E (2009). A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. Journal of Traumatic Stress, 22(5), 399–408. 10.1002/jts.20444 [DOI] [PubMed] [Google Scholar]
- Conger R, Wallace L, Sun Y, Simons RL, McLoyd VC, & Brody GH (2002). Economic pressure in African American families: A replication and extension of the family stress model. Developmental Psychology, 38(2), 179–193. 10.1037//0012-1649.38.2.179 [DOI] [PubMed] [Google Scholar]
- Crane CA, Hawes SW, & Weinberger AH (2013). Intimate Partner Violence Victimization and Cigarette Smoking: A Meta-Analytic Review. Trauma, Violence, and Abuse, 14(4), 305–315. 10.1177/1524838013495962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielson CK, McCart MR, de Arellano MA, Macdonald A, Doherty LS, & Resnick HS (2010). Risk reduction for substance use and trauma-related psychopathology in adolescent sexual assault victims: Findings from an open trial. Child Maltreatment, 15(3), 261–268. 10.1177/1077559510367939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deane K, Richards M, Mozley M, Scott D, Rice C, & Garbarino J (2018). Posttraumatic Stress, Family Functioning, and Externalizing in Adolescents Exposed to Violence: A Moderated Mediation Model. Journal of Clinical Child and Adolescent Psychology, 47(supl), S176–S189. 10.1080/15374416.2016.1197836 [DOI] [PubMed] [Google Scholar]
- DiClemente CM, Rice CM, Quimby D, Richards MEL, Grimes CT, Morency MM, … Pica JA (2018). Resilience in EIrban African American Adolescents: The Protective Enhancing Effects of Neighborhood, Family, and School Cohesion Following Violence Exposure. The Journal of Early Adolescence, 38(9), 1286–1321. 10.1177/0272431616675974 [DOI] [Google Scholar]
- Eccles JS (1999). Children Ages 6 to 14. The Future of Children, 9(2), 30–44. [PubMed] [Google Scholar]
- Elkins SR, Fite PJ, Moore TM, Lochman JE, & Wells KC (2014). Bidirectional effects of parenting and youth substance use during the transition to middle and high school. Psychology of Addictive Behaviors, 28(2), 475–486. 10.1037/a0036824 [DOI] [PubMed] [Google Scholar]
- Elliott DS (1994). Serious violent offenders: Onset, developmental course, and termination. Criminology, 32(1), 1–21. 10.1111/j.1745-9125.1994.tb01144.x [DOI] [Google Scholar]
- Enders CK (2001). The performance of the full information maximum likelihood estimator in multiple regression models with missing data. Educational and Psychological Measurement, 61(5), 713–740. [Google Scholar]
- Estrada-Martínez LM, Caldwell CEL, Schulz AJ, Diez-Roux AV, & Pedraza S (2013). Families, neighborhood socio-demographic factors, and violent behaviors among Latino, white, and black adolescents. Youth and Society, 45(2), 221–242. 10.1177/0044118X11411933 [DOI] [Google Scholar]
- Finkelhor D, Ormrod RK, & Turner HA (2007a). Polyvictimization and trauma in a national longitudinal cohort. Development and Psychopathology, 19(1), 149–166. 10.1017/S0954579407070083 [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Ormrod RK, & Turner HA (2007b). Re-victimization patterns in a national longitudinal sample of children and youth. Child Abuse and Neglect, 57(5), 479–502. 10.1016/j.chiabu.2006.03.012 [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Turner HA, Shattuck A, & Hamby SL (2013). Violence, crime, and abuse exposure in a national sample of children and youth an update. JAMA Pediatrics, 167(1), 614–621. 10.1001/jamapediatrics.2013.42 [DOI] [PubMed] [Google Scholar]
- Goodrum NM, Armistead LP, Tully EC, Cook SL, & Skinner D (2017). Parenting and youth sexual risk in context: The role of community factors. Journal of Adolescence, 57, 1–12. 10.1016/j.adolescence.2017.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorman-Smith D, Henry DB, & Tolan PH (2004). Exposure to community violence and violence perpetration: The protective effects of family functionin. Journal of Clinical Child & Adolescent Psychology, 33(3), 439–449. 10.1207/s15374424jccp3303_2 [DOI] [PubMed] [Google Scholar]
- Guassi Moreira JF, & Telzer EH (2015). Changes in family cohesion and links to depression during thecollege transition. Journal of Adolescence, 43, 72–82. 10.1016/j.adolescence.2015.05.012 [DOI] [PubMed] [Google Scholar]
- Hatch SL, & Dohrenwend BP (2007). Distribution of traumatic and other stressful life events by race/ethnicity, gender, SES and age: A review of the research. American Journal of Community Psychology, 40(3–4), 313–332. 10.1007/s10464-007-9134-z [DOI] [PubMed] [Google Scholar]
- Homma Y, Wang N, Saewyc E, & Kishor N (2012). The relationship between sexual abuse and risky sexual behavior among adolescent boys: A meta-analysis. Journal of Adolescent Health, 57(1), 18–24. 10.1016/j.jadohealth.2011.12.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Janssen HJ, Deković M, & Bruinsma GJN (2014). Parenting and time adolescents spend in criminogenic settings: A between-and within-person analysis. British Journal of Criminology, 54(A), 551–567. 10.1093/bjc/azu032 [DOI] [Google Scholar]
- Jensen PS, Rubio-Stipec M, Canino G, Bird HR, Dulcan MK, Schwab-Stone ME, & Lahey BB (1999). Parent and child contributions to diagnosis of mental disorder: Are both informants always necessary? Journal of the American Academy of Child and Adolescent Psychiatry, 38(12), 1569–1579. 10.1097/00004583-199912000-00019 [DOI] [PubMed] [Google Scholar]
- Kaufman JS, & Cooper RS (2001). Commentary: Considerations for Use of Racial/Ethnic Classification in Etiologic Research. American Journal of Epidemiology, 154(4), 291–298. 10.1093/aje/154.4.291 [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Aciemo R, Saunders B, Resnick HS, Best CL, & Schnurr PP (2000). Risk factors for adolescent substance abuse and dependence: Data from a national sample. Journal of Consulting and Clinical Psychology, 68(1), 19–30. 10.1037/0022-006X.68.1.19 [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, & Best CL (2003). Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the National Survey of Adolescents. Journal of Consulting and Clinical Psychology, 71(4), 692–700. 10.1037/0022-006X.71.4.692 [DOI] [PubMed] [Google Scholar]
- Kirkinis K, Pieterse AL, Martin C, Agiliga A, & Brownell A (2018, August 30). Racism, racial discrimination, and trauma: a systematic review of the social science literature. Ethnicity and Health, pp. 1–21. 10.1080/13557858.2018.1514453 [DOI] [PubMed] [Google Scholar]
- Klein DN, Dougherty LR, & Olino TM (2005). Toward guidelines for evidence-based assessment of depression in children and adolescents. Journal of Clinical Child and Adolescent Psychology, 34(3), 412–432. 10.1207/s15374424jccp3403_3 [DOI] [PubMed] [Google Scholar]
- Leventhal T, & Brooks-Gunn J (2000). The neighborhoods they live in: The effects of neighborhood residence on child and adolescent outcomes. Psychological Bulletin, 126(2), 309–337. 10.1037//0033-2909.126.2.309 [DOI] [PubMed] [Google Scholar]
- Lippold MA, Greenberg MT, Graham JW, & Feinberg ME (2014). Unpacking the Effect of Parental Monitoring on Early Adolescent Problem Behavior: Mediation by Parental Knowledge and Moderation by Parent–Youth Warmth. Journal of Family Issues. 10.1177/0192513X13484120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan T, Walker R, Cole J, & Leukefeld C (2002). Victimization and Substance Abuse among Women: Contributing Factors, Interventions, and Implications. Review of General Psychology, 6(4), 325–397. 10.1037/1089-2680.6.4.325 [DOI] [Google Scholar]
- Margolin G, Vickerman KA, Oliver PH, & Gordis EB (2010). Violence exposure in multiple interpersonal domains: Cumulative and differential effects. Journal of Adolescent Health, 47(2), 198–205. 10.1016/j.jadohealth.2010.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslowsky J, Jager J, & Hemken D (2015). Estimating and interpreting latent variable interactions: A tutorial for applying the latent moderated structural equations method. International Journal of Behavioral Development, 39(1), 87–96. 10.1177/0165025414552301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maynard PE, & Olson DH (1987). Circumplex model of family systems: A treatment tool in family counseling. Journal of Counseling and Development, 65, 502–504. [Google Scholar]
- McGue M, & Iacono WG (2008). The adolescent origins of substance use disorders. International Journal of Methods in Psychiatric Research, 17(SUPPL. 1), S30–S38. 10.1002/mpr.242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyers JL, & Dick DM (2010). Genetic and Environmental Risk Factors for Adolescent-Onset Substance Use Disorders. Child and Adolescent Psychiatric Clinics of North America, 19(3), 465–477. 10.1016/j.chc.2010.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monahan KC, Rhew IC, Hawkins JD, & Brown EC (2014). Adolescent pathways to co-occurring problem behavior: The effects of peer delinquency and peer substance use. Journal of Research on Adolescence, 24(4), 630–645. 10.1111/jora.12053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreland AD, Walsh K, Hartley C, Hanson R, Danielson CK, Saunders B, & Kilpatrick DG (2018). Investigating Longitudinal Associations Between Sexual Assault, Substance Use, and Delinquency Among Female Adolescents: Results From a Nationally Representative Sample. Journal of Adolescent Health, 63(3), 320–326. 10.1016/j.jadohealth.2018.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mrug S, & Windle M (2009). Bidirectional influences of violence exposure and adjustment in early adolescence: Externalizing behaviors and school connectedness. Journal of Abnormal Child Psychology, 37(5), 611–623. 10.1007/s10802-009-9304-6 [DOI] [PubMed] [Google Scholar]
- Mustanski B, Andrews R, & Puckett JA (2016). The effects of cumulative victimization on mental health among lesbian, gay, bisexual, and transgender adolescents and young adults. American Journal of Public Health, 106(3), 527–533. 10.2105/AJPH.2015.302976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg JT, Wong MM, Martel MM, Jester JM, Puttler LT, Glass JM, … Zucker RA (2006). Poor response inhibition as a predictor of problem drinking and illicit drug use in adolescents at risk for alcoholism and other substance use disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 45(4), 468–475. 10.1097/01.chi.0000199028.76452.a9 [DOI] [PubMed] [Google Scholar]
- O’Connor KL, Dolphin L, Fitzgerald A, & Dooley B (2016). Modeling problem behaviors in a nationally representative sample of adolescents. Journal of Adolescence, 50, 6–15. 10.1016/j.adolescence.2016.03.010 [DOI] [PubMed] [Google Scholar]
- Racz SJ, McMahon RJ, & Luthar SS (2011). Risky Behavior in Affluent Youth: Examining the Co-occurrence and Consequences of Multiple Problem Behaviors. Journal of Child and Family Studies, 20(1), 120–128. 10.1007/s10826-010-9385-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley D (1987). Time and crime: The link between teenager lifestyle and delinquency. Journal of Quantitative Criminology, 3(4), 339–354. 10.1007/BF01066835 [DOI] [Google Scholar]
- Romano E, Bell T, & Billette JM (2011). Prevalence and correlates of multiple victimization in a nation-wide adolescent sample. Child Abuse and Neglect, 35(7), 468–479. 10.1016/j.chiabu.2011.03.005 [DOI] [PubMed] [Google Scholar]
- Schulte MT, Armistead L, Marelich WD, Payne DL, Goodrum NM, & Murphy DA (2017). Maternal Parenting Stress and Child Perception of Family Functioning Among Families Affected by HIV. Journal of the Association of Nurses in AIDS Care, 28(5), 784–794. 10.1016/j.jana.2017.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons LG, Sutton TE, Simons RL, Gibbons FX, & Murry VMB (2016). Mechanisms That Link Parenting Practices to Adolescents’ Risky Sexual Behavior: A Test of Six Competing Theories. Journal of Youth and Adolescence, 45(2), 255–270. 10.1007/s10964-015-0409-7 [DOI] [PubMed] [Google Scholar]
- Smith DJ, & Ecob R (2007). An investigation into causal links between victimization and offending in adolescents. British Journal of Sociology, 58(4), 633–659. 10.1111/j.1468-4446.2007.00169.x [DOI] [PubMed] [Google Scholar]
- Sousa C, Herrenkohl TI, Moylan CA, Tajima EA, Klika JB, Herrenkohl RC, & Russo MJ (2011). Longitudinal study on the effects of child abuse and children’s exposure to domestic violence, parent-child attachments, and antisocial behavior in adolescence. Journal of Interpersonal Violence, 26(1), 111–136. 10.1177/0886260510362883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spano S (2004). Stages of Adolescent Development. Youth Upstate Center of Excellence. [Google Scholar]
- Sternberg KJ, Baradaran LP, Abbott CB, Lamb ME, & Guterman E (2006). Type of violence, age, and gender differences in the effects of family violence on children’s behavior problems: A mega-analysis. Developmental Review, 26(1), 89–112. 10.1016/j.dr.2005.12.001 [DOI] [Google Scholar]
- Suliman S, Mkabile SG, Fincham DS, Ahmed R, Stein DJ, & Seedat S (2009). Cumulative effect of multiple trauma on symptoms of posttraumatic stress disorder, anxiety, and depression in adolescents. Comprehensive Psychiatry, 50(2), 121–127. 10.1016/j.comppsych.2008.06.006 [DOI] [PubMed] [Google Scholar]
- Tyler KA, & Johnson KA (2006). A Longitudinal Study of the Effects of Early Abuse on Later Victimization Among High-Risk Adolescents. Violence and Victims, 21(3), 287–306. 10.1891/vivi.21.3.287 [DOI] [PubMed] [Google Scholar]
- Vézina J, Hébert M, Poulin F, Lavoie F, Vitaro F, & Tremblay RE (2011). Risky lifestyle as a mediator of the relationship between deviant peer affiliation and dating violence victimization among adolescent girls. Journal of Youth and Adolescence, 40(7), 814–824. 10.1007/s10964-010-9602-x [DOI] [PubMed] [Google Scholar]
- Whitesell M, Bachand A, Peel J, & Brown M (2013). Familial, Social, and Individual Factors Contributing to Risk for Adolescent Substance Use. Journal of Addiction, 2013, 1–9. 10.1155/2013/579310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolitzky-Taylor KB, Ruggiero KJ, Danielson CK, Resnick HS, Hanson RF, Smith DW, … Kilpatrick DG (2008). Prevalence and correlates of dating violence in a national sample of adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 47(7), 755–762. 10.1097/CHI.0b013e318172ef5f [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright EM, Fagan AA, & Pinchevsky GM (2013). The effects of exposure to violence and victimization across life domains on adolescent substance use. Child Abuse and Neglect, 37(11), 899–909. 10.1016/j.chiabu.2013.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinzow HM, Ruggiero KJ, Hanson RF, Smith DW, Saunders BE, & Kilpatrick DG (2009). Witnessed community and parental violence in relation to substance use and delinquency in a national sample of adolescents. Journal of Traumatic Stress, 22(6), 525–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinzow HM, Ruggiero KJ, Resnick H, Hanson R, Smith D, Saunders B, & Kilpatrick D (2009). Prevalence and mental health correlates of witnessed parental and community violence in a national sample of adolescents. Journal of Child Psychology and Psychiatry, 50(4), 441–450. 10.1111/j.1469-7610.2008.02004.x [DOI] [PMC free article] [PubMed] [Google Scholar]


