Abstract
INTRODUCTION:
Most of the neonatal and maternal deaths occur within the first 48 hours post-delivery. Hence, this time period is very crucial for the survival of newborns and mothers both. As per maternal and child health program guidelines in India, it is clearly mentioned that all the government health facilities should discharge the mother and baby only after 48 hours of delivery in case of normal delivery and after 7 days in case of delivery conducted by cesarean sections.
AIM:
The aim of the study was to find the various factors responsible for early maternity discharge (<48 h) of normal vaginal deliveries (NVDs) conducted at government health facilities.
MATERIAL AND METHODS:
The study was conducted in a rural block of Haryana, North India, from May to June, 2015. Postnatal women with NVD within 6 months of duration from initiation of the study were included after taking proper informed consent. A questionnaire was developed by the investigators to interview the women. The questionnaire consists of 26 items which included the socio-demographic details and questions on various factors affecting postnatal stay at the health facility.
RESULTS:
A total of 40 postnatal women consented and participated in the study. Their mean age was 23.46 ± 5.63 years. Majority of them (24, 60.0%) were having their first child. Out of them, 12 delivered at primary health centers (PHCs), 18 at community health centers, and the rest at the district hospital. A total of 24 (60%) of them were discharged early (<48 h) as per laid guidelines. It was observed that primiparity, delivery at PHC, normal birth weight of baby, and term deliveries were significantly associated with early discharge. Among those who had NVD and stayed beyond 48 h, most of them mentioned that the round-the-clock availability of doctors/nurses was the main reason for their staying at the health facility.
CONCLUSION:
The proportion of postpartum women discharged early is high and alarming. There is a need for essential counseling to be imparted to the mothers by doctors/nurses at all the health facilities for staying till 48 hours and by health workers during the antenatal period of the importance of the stay at the facility post delivery.
Keywords: Child health, early discharge, maternal health, newborn, PNC
Introduction
It is estimated that more than 500,000 women die each year as a result of pregnancy- and childbirth-related complications globally.[1] Most of the deaths are reported due to obstetric complications during the first 48 h after childbirth.[2] As per the World Health Organization, postpartum period or postnatal period is defined as the period immediately following birth of the baby and extending for about 6 weeks. This period represents a critical phase in determining the health and survival of the mother and her newborn. Most of the maternal and infant deaths occur in the 1st month after birth: “Almost half of postnatal maternal deaths occur within the first 24 h, and 66% occur during the 1st week. In 2013, 2.8 million newborns died in their 1st month of life – 1 million of these newborns died on the 1st day.”[3]
The hospital stay of the mother and her healthy term infant should be adequate enough to identify early health problems and to ensure that family is able to take care of the infant at home.[3] As per the guidelines of the American Academy of Pediatrics, early discharge is referred to as a postpartum hospital stay of <48 h.[1,3] Many health conditions related to transition from intrauterine to an extra uterine environment usually become apparent during the first 12 h after birth. The World Health Organization (WHO) also recommends that “healthy women and newborns should have a stay of at minimum of 24 h at a health facility and not discharged early”. It also recommends that discharge is acceptable only if a mother's bleeding is controlled, mother and baby do not have signs of infection or other diseases, and the baby is breastfeeding well.”[1]
Improving maternal and child health and their survival had remained the top priority for the National Rural Health Mission for achievement of the national health goals and Sustainable Development Goals 4 and 5 in India.[4]
Despite the national guidelines and interventions, 45%–67% of mothers in India and 27%–35% of mothers in the state of Haryana were reported to have been discharged within 48 h from the hospital/health facility after delivery.[5,6]
In view of the above context, the current study was conducted with the aim to find the proportion of early discharges among the women with uncomplicated pregnancies delivering at government health facilities and the factors associated with them.
Material and Methods
Study design and study population
An exploratory community-based cross-sectional study was conducted from May to June, 2015 in a rural block of Panchkula district of Haryana, North India. All the women who had a normal vaginal delivery (NVD) at any government health facility in the Raipur Rani community development block within the past 6 months from initiation of the study were included through convenient sampling. The list and records of all these women were obtained from the subcenters, primary health centers (PHCs), and the community health center (CHC) in the block. Women who had undergone a cesarean section or those who delivered at home were excluded. Furthermore, women requiring prolonged stay due to any of the obstetric complications or problems in newborns were also excluded. A final of 40 postnatal women fulfilling the eligibility criteria were included.
Data collection
A semi-structured questionnaire, developed by the investigators, was used to interview the postnatal women who had been discharged home after delivery. All the interviews were conducted by one of the investigators in the local language. Clinical and discharge records of the women were also seen to get information on various parameters. The women were called at the nearest Aanganwadi centers or subcenters for the interview, and the interview was conducted in a separate room maintaining confidentiality and secrecy.
The study questionnaire consisted of three sections. The first section consisted of the details on sociodemographic characteristics of the mother. The second section contained information on the clinical details of the infant and mother at the time of birth and during the stay at the facility such as birth weight, any complications in infant or mother, time of initiation of breastfeeding, and total duration of stay at the health facility. The third section consisted of questions on various potential causes which might have affected the duration of stay at the facility. The questionnaire was pilot tested on five women for suitability of the contents which were not included in the analysis, and appropriate changes in the questionnaire were made based on the findings of the pilot study.
Statistical analysis
Bivariate analysis using the Chi-square and Fisher's exact tests was performed to determine the factors significantly associated with early discharge. P < 0.05 was considered statistically significant.
Ethical considerations
Approval was obtained from the Institute Ethics Committee (IEC), PGIMER, Chandigarh, and permission was obtained from Senior Medical Officer, CHC, Raipur Rani block, before initiation of the study. Written informed consent from all the participants was obtained. Confidentiality of the participants and of the data collected was ensured by the investigators.
Results
A total of 40 women out of 46 eligible women contacted by the study investigator consented and participated in the study giving a response rate of 92.4%. Table 1 describes the sociodemographic characteristics of the studied population. The mean age of the women was 23.46 ± 5.23 years ranging from 18 to 32 years. Most of the women (60%) were primigravida, Hindu (75.0%) by religion, educated up to Class 5th(35.0%), and housewives (65%). Majority delivered at CHC (45%), followed by PHC (30%). The total monthly income of the family was < INR 5000/- in 20% of the women with maximum families (66.7%) having income in the range of INR 5000–10,000. Most of the women (88.6%) delivered at term (>37 weeks of gestation) with birth weight of baby more than 2.5 kg (75.0%) [Table 1].
Table 1.
Sociodemographic and other characteristics of studied women (n=40)
| Variables | n (%) |
|---|---|
| Mean age±SD (years) | 23.46±5.23 |
| Age groups (years) | |
| 18-24 | 28 (70.0) |
| 25-32 | 12 (30.0) |
| Birth order | |
| 1 | 24 (60.0) |
| 2-4 | 15 (37.5) |
| >4 | 1 (2.5) |
| Education of women | |
| Illiterate | 10 (25.0) |
| Up to primary (5th) | 8 (20.0) |
| Up to middle (8th) | 10 (25.0) |
| Up to high school (10th) | 7 (17.0) |
| Up to 10+2 or graduate | 5 (8.0) |
| Religion | |
| Hindu | 30 (75.0) |
| Muslim | 6 (15.0) |
| Sikh | 4 (10.0) |
| Occupation | |
| Housewife | 26 (65.0) |
| Agricultural laborer | 10 (25.0) |
| Private job/work | 4 (10.0) |
| Husband’s occupation | |
| Laborer | 24 (60.0) |
| Business | 10 (25.0) |
| Government/private job | 6 (15.0) |
| Total family income per month (INR) | |
| <5000 | 8 (20.0) |
| 5000-10,000 | 17 (42.5) |
| 10,001-15,000 | 7 (17.5) |
| 15001-20,000 | 4 (10.0) |
| >20,000 | 4 (10.0) |
| BPL family | |
| Yes | 24 (60.0) |
| No | 16 (40.0) |
| Period of gestation (weeks) | |
| <37 | 6 (15.0) |
| ≥37 | 34 (85.0) |
| History of abortion/stillbirth | |
| Yes | 8 (20.0) |
| No | 32 (80.0) |
| Place of delivery | |
| PHC | 12 (30.0) |
| CHC | 18 (45.0) |
| DH | 10 (25.0) |
| Mode of delivery | |
| NVD | 32 (80.0) |
| NVD with episiotomy | 8 (20.0) |
| Birth weight of newborn (in kgs) | |
| <2.5 | 10 (25.0) |
| >2.5 | 30 (75.0) |
PHC=Primary health center, CHC=Community health center, DH=District hospital, NVD=Normal vaginal delivery, BPL=Below the poverty line, SD=Standard deviation, INR=Indian national rupees
With respect to type of health facility where the women delivered and total duration of stay, PHC has the maximum proportion of early discharges where all the 12 women were discharged before 48 h, and 4 (33.3%) out of them were even discharged before 24 h. District hospital has the least proportion of early discharges where only 30.0% of the women were discharged before 48 h [Table 2].
Table 2.
Place of delivery of the postnatal women and duration of stay at the facility (n=40)
| Type of health facility | Duration of stay <24 h, n (%) | Duration of stay >24 h but <48 h, n (%) | Total early discharges, n (%) |
|---|---|---|---|
| PHC (n=12) | 4 (33.3) | 8 (66.7) | 12 (100.0) |
| CHC (n=18) | 1 (5.6) | 8 (44.4) | 9 (50.0) |
| DH (n=10) | 0 (0.0) | 3 (30.0) | 3 (30.0) |
PHC=Primary health center, CHC=Community health center, DH=District hospital
Hence, out of the 40 postnatal women, 24 (60.0%) had a total duration of stay <48 h, who were discharged early [Figure 1].
Figure 1.
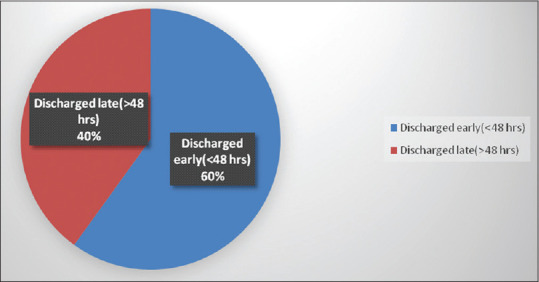
Proportion of early discharge versus late discharge (n = 40)
On bivariate analysis, variables found to be significantly associated with early maternity discharge were primiparity, delivery at primary healthcare level, term delivery and the normal birth weight of the baby [Table 3].
Table 3.
Factors associated with early discharge
| Variables | Discharged early (n=24), n (%) | Discharged late (n=16), n (%) | P |
|---|---|---|---|
| Age groups (years) | |||
| 18-25 | 18 (64.3) | 10 (35.7) | 0.39 |
| 25-32 | 6 (50.0) | 6 (50.0) | |
| Birth order (parity) | |||
| Primipara | 18 (75.0) | 6 (25.0) | 0.04* |
| Multipara | 6 (37.5) | 10 (62.5) | |
| Education of the mother | |||
| Illiterate | 7 (70.0) | 3 (30.0) | 0.71 |
| Literate | 17 (56.6) | 13 (43.4) | |
| Place of delivery | |||
| Primary care level (PHC) | 12 (100.0) | 0 (0.0) | 0.0009* |
| Secondary care level (CHC, SDH/DH) | 12 (30.0) | 16 (70.0) | |
| Mode of delivery | |||
| NVD | 20 (75.0) | 12 (25.0) | 0.52 |
| NVD with episiotomy | 4 (50.0) | 4 (50.0) | |
| Period of gestation (weeks) | |||
| <37 (preterm) | 1 (33.3) | 5 (66.7) | 0.02* |
| ≥37 (term) | 23 (67.6) | 11 (32.4) | |
| Birth weight of the baby (kg) | |||
| <2.5 | 2 (20.0) | 8 (80.0) | 0.003* |
| ≥2.5 | 22 (73.3) | 8 (26.7) |
*Statistically significant. PHC=Primary health center, CHC=Community health center, SDH/DH=Sub-district hospital/district hospital, NVD=Normal vaginal delivery
Factors related to healthy practices for newborn among the postnatal women are summarized in Table 4.
Table 4.
Factors related to healthy practices for newborn among the postnatal women (n=40)
| Factors | Yes, n (%) | No, n (%) |
|---|---|---|
| Was breastfeeding initiated at health facility before discharge? | 28 (70) | 12 (30) |
| Did the child pass urine and stool both before discharge? | 21 (52.5) | 19 (47.5) |
| Was the child bathed within 24 h? | 4 (10) | 36 (90) |
| Was the child immunized with BCG, OPV, and hepatitis B before discharge? | 24 (60) | 16 (40) |
| Did the mother or child have any problem within 7 days following discharge requiring OPD visit or hospitalization? | 16 (40) | 24 (60) |
OPD=Outpatient department, BCG=Bacillus Guerin, OPV=Oral polio vaccine
With regard to different probable factors affecting stay at the health facility post-delivery, around 52.0% of the participants stated that they were asked or advised to stay at the health facility for at least 48 h by the treating doctors or nurses. However, only 12.5% of the women were given the explanation for their stay for the recommended duration by the doctor or nurse. Around 60% of the interviewed women were not satisfied with the condition of the health facility to stay due to various reasons. Eighty percent of the respondents stated that their attendants including the female attendants were not provided a proper place to stay at the health facility. Further, around 52% of the women stated that they were discharged by the doctor [Table 5].
Table 5.
Responses to questions affecting stay at the health facility by the postnatal women (n=40)
| Questions | n (%) of respondents replying (yes) |
|---|---|
| Were you asked or advised by the doctor/nurse to stay at the health facility till 48 h after delivery? | 21 (52.5) |
| Were you explained the reason to stay till 48 h? | 5 (12.5) |
| Whether you were satisfied with the condition of the health facility to stay? | 16 (40.0) |
| Whether your attendant had proper place to stay at the facility? | 8 (20.0) |
| Did the doctor/nurse himself/herself discharge you before 48 h? | 21 (52.5) |
Discussion
Our study showed that women from a rural block of North India are not staying sufficiently enough at government health facilities post-delivery. Women who were primigravida, illiterate, delivering at PHCs, and had delivered after 37 weeks (at term) of gestation were most likely to be discharged within 48 h from the hospital/health facility post-delivery. This may be due to the fact that majority of the mothers, or their family members took the decision on early discharge without knowing the scientific reason for the 48-h stay in NVD cases. It was also observed that health workers were reluctant to implement the timely discharge, particularly in case of uncomplicated NVD cases. Our study found that mothers of younger age groups were more likely to be discharged early than older age group although the association was not statistically significant (P > 0.05). From literature review, it is found that other than age groups, multiple factors are responsible for early discharge from the health facility.[7,8] A study conducted in Maharashtra by Nipte et al. has similar findings where mothers of young age group were likely to be discharged early.[9] Contrary to this, a study conducted in the United States reported that mothers aged older than 35 years were likely to be discharged early.[10]
Early maternity discharge in NVD cases (uncomplicated) can reduce the window of opportunity for detecting potential complications.[11,12] It also reduced the chance for the counseling of mothers on puerperal care, especially where the ANC services are inadequate. The Government of India has launched multiple schemes and programs for reduction of maternal and infant mortality such as Janani Suraksha Yojana (JSY) and Janani Shishu Suraksha Karyakaram (JSSK) by leveraging on increase in institutional deliveries and for the delayed maternity discharge (for at least 48 h in hospitals after delivery).[13,14] Through these initiatives taken by the government, the number of institutional deliveries has increased significantly.[15,16]
Our findings of very high proportion of early maternal discharge in NVD cases are not encouraging at all and is a matter of concern. The factors may be multiple – this may be due to high caseload and lack of adequate space for hospitalization in the wards. Hence, infrastructural expansion in terms of providing more beds and making the hospital stay more comfortable at PHC levels becomes critical. The absence or unavailability of doctors and other health-care workers round-the-clock at the health facilities was emerged as one of the reasons for early maternity discharge, which has to be looked upon carefully and corrected at earest. Lack of counseling efforts from health workers during the stay at the health facility also emerged as an important factor for early maternity discharge. Health-care providers are needed to be trained accordingly to ensure strict implementation of JSY and JSSK schemes for the prevention of early discharge which could be the key to reduce early maternity discharge from the government health facilities in case of in uncomplicated NVD cases.
Conclusion
We conclude that mothers who were primipara, and delivered at PHC, uncomplicated cases such as term deliveries and normal birth weight of the baby, and those who requested for discharge were actually discharged before 48 h, i.e., prematurely from the hospitals.
Lack of counseling efforts by the care providers, doctors and nurses, during the stay at the health facility emerged as an important factor for early maternity discharge.
Recommendations
Awareness generation among various stakeholders, including proper ANC counseling to the mothers, their relatives, and significant others regarding the importance of the first 48 h institutional stay, is the need of the hour. Sensitization of health-care workers may play a vital role to prevent early maternity discharge of uncomplicated NVD cases from hospitals. In addition, qualitative studies for understanding the sociocultural grounds for early discharge are needed.
Limitations of this study
(1) Small sample size is one of the limitations; further study with larger sample size will give us better insight into the problems at block, district and state level. (2) Stakeholder analysis could give us an overall view of this problem.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We do acknowledge all the postnatal mothers for participating and giving their opinions in this study.
References
- 1.WHO Technical Consultation on Postpartum Care WHO Technical Consultation on Postpartum and Postnatal Care NCBI Bookshelf. [Last accessed on 2020 Jan 13]. Available from: https://wwwncbinlmnihgov/books/NBK310595/
- 2.Li XF1, Fortney JA, Kotelchuck M, Glover LH. The postpartum period: The key to maternal mortality. Int J Gynaecol Obstet. 1996;54:1–10. doi: 10.1016/0020-7292(96)02667-7. [DOI] [PubMed] [Google Scholar]
- 3.The Lancet Every Newborn Series – Healthy Newborn Network. [Last accessed on 2020 Jan 13]. Available from: https://wwwhealthynewbornnetworkorg/resource/the-lancet-every-newborn-series/
- 4.Sustainable Development Goals: Sustainable Development Knowledge Platform. [Last accessed on 2020 Jan 13]. Available from: https://sustainabledevelopmentunorg/menu=1300 .
- 5.Is Quality of Care During Childbirth Consistent from Admission to Discharge. A Qualitative Study of Delivery Care in Uttar Pradesh, India. [Last accessed on 2020 Jan 13]. Available from: https://journalsplosorg/plosone/articleid=101371/journalpone 0204607 . [DOI] [PMC free article] [PubMed]
- 6.National Family Health Survey. [Last accessed on 2020 Jan 13]. Available from: http://rchiipsorg/nfhs/haryanashtml .
- 7.Firoz T, Chou D, von Dadelszen P, Agrawal P, Vanderkruik R, Tunçalp O, et al. Measuring maternal health: Focus on maternal morbidity. Bull World Health Organ. 2013;91:794–6. doi: 10.2471/BLT.13.117564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maternal Mortality: Who, when, where, and Why – Science Direct. [Last accessed on 2020 Jan 13]. Available from: https://www.sciencedirect.com/science/article/pii/S014067360669380X .
- 9.Determinants of Early Discharge of Mothers from Hospitals after Delivery in Beed Block of Beed District, Maharashtra, India 2014 Clinical Epidemiology and Global Health. [Last accessed on 2020 Jan 13]. Available from: https://cegh.net/article/S2213-3984(15)00088-3/fulltext .
- 10.Merenstein & Gardner's Handbook of Neonatal Intensive Care E-Book - Sandra Lee Gardner, Brian S. Carter, Mary I Enzman-Hines, Jacinto A. Hernandez - Google Books. [Last accessed on 2020 Jan 13]. Available from: https://books.google.co.in/books?id=idpiCAAAQBAJ&pg=PA462&lpg=PA462&dq=United+States+reported+that+mothers+aged+older+than+35+years+were+likely+to+be+discharged+early&source=bl&ots=zKWG1nNSCj&sig=ACfU3U1LSr0DtQovxky0J2rmPEChuoMMpQ&hl=en&sa=X&ved=2ahUKEwimkZS744DnAhXmwzgGHc7pBO0Q6AEwDHoECAoQAQ#v=onepage&q=United%20States%20reported%20that%20mothers%20aged%20older%20than%2035%20 years%20were%20likely%20to%20be%20discharged%20early&f=false .
- 11.Vaginal Delivery: How does Early Hospital Discharge Affect Mother and Child Outcomes. A Systematic Literature Review. [Last accessed on 2020 Jan 13]. Available from: https://wwwncbinlmnihgov/pmc/articles/PMC5588709/ [DOI] [PMC free article] [PubMed]
- 12.Neiger R. Long-term effects of pregnancy complications on maternal health: A Review. J Clin Med. 2017;6 doi: 10.3390/jcm6080076. pii: E76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Janani Suraksha Yojana (JSY) National Health Portal of India. [Last accessed on 2020 Jan 13]. Available from: https://wwwnhpgovin/janani-suraksha-yojana-jsy-_pg .
- 14.Janani Shishu Suraksha Karyakaram (JSSK) National Health Portal of India. [Last accessed on 2020 Jan 13]. Available from: https://wwwnhpgovin/janani-shishu-suraksha-karyakaram-jssk_pg .
- 15.Salve HR, Charlette L, Kankaria A, Rai SK, Krishnan A, Kant S. Improving access to institutional delivery through Janani Shishu Suraksha Karyakram: Evidence from rural Haryana, North India. Indian J Community Med. 2017;42:73–76. doi: 10.4103/0970-0218.205223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gupta SK, Pal DK, Tiwari R, Garg R, Shrivastava AK, Sarawagi R, et al. Impact of Janani Suraksha Yojana on institutional delivery rate and maternal morbidity and mortality: An observational study in India. J Health Popul Nutr. 2012;30:464–71. doi: 10.3329/jhpn.v30i4.13416. [DOI] [PMC free article] [PubMed] [Google Scholar]


