Abstract
It has been suggested that abdominal obesity might be a better cardiovascular diseases (CVDs) discriminator than overall obesity. The most appropriate obesity measures for estimating CVD events in Kurdish populations have not been well-recognized. The objective of the present study was, therefore, to determine the cutoff points of BMI, waist circumference (WC), waist-to-hip ratio (WHR), and waist to height ratio (WHtR) as the diagnostic cut-offs to discriminate the prevalent cardiovascular diseases. The data collected from Ravansar Non-Communicable Disease (RaNCD) cohort, the first Kurdish population-based study, was analyzed. The information related to BMI, WC, WHR and WHtR of 10,065 adult participants in the age range of 35–65 was analyzed in this study. Receiver operating characteristic (ROC) analyses were conducted to evaluate the optimum cut-off values and to predict the incidence of cardiac events. The results showed that WHtR had the largest areas under the ROC curve for cardiac events in both male and female participants, and this was followed by WHR, WC, and BMI. The optimal cut-off values for determining the cardiac events in the Kurdish population were BMI = 27.02 kg/m2 for men and BMI = 27.60 kg/m2 for women, WC = 96.05 cm in men and 99.5 cm for women, WHRs = 0.96 in both sexes, and WHtR = 0.56 for men and 0.65 for women. The current study, therefore, showed that WHtR might serve as a better index of prevalent cardiac event than BMI, WHR and WC.
Subject terms: Heart development, Heart development, Nutrition, Nutrition
Introduction
Obesity, especially central obesity, is defined as fat accumulation around the abdominal area. While obesity is increasing worldwide, it is associated with the risk of cardiovascular diseases (CVDs)1,2. Among Iranian adults, 34.8% are overweight and 18.8% are obese3. The most common cause of mortality in both developed and developing countries is related to CVDs, imposing many costs on the health care systems4. Central obesity has adverse effects on cardio-metabolic indices, including insulin resistance, hypertension and dyslipidemia5,6. At present, obesity is identified as a major changeable risk factor7.
To identify obesity (i.e., extra body fat accumulation) and the risk of obesity-related complications, several methods such as body mass index (BMI), waist circumference (WC), and waist to hip ratio (WHR) are routinely applied8,9. Although BMI has been widely used to screen overweight and obese individuals, this index cannot predict abdominal obesity (i.e., central obesity). Also, it has different age, sex and ethnic-specific standards, making it less practical for parents and non-professional use5. Similarly, WC can reflect fat distribution in the abdominal area, but it may vary based on height, sex and race differences10. WHR is another simple index; however, this index cannot change with the increase or decrease in both WC or hip circumference1. It should be noted that bioelectrical impedance analysis (BIA) is a safe, inexpensive, and non-invasive method for the evaluation of body compositions such as central obesity and body fat accumulation9,11,12; however, BIA results are influenced by factors such as ethnicity, environment, phase of the menstrual cycle, dehydration, and underlying medical conditions. So, in large epidemiological studies, more straightforward techniques such as BMI, WC and WHR are regularly used instead of BIA to measure the body fat13.
Recently, a new index named waist-height ratio (WHtR) has also gained popularity; it has been used widely for screening the risk of cardiometabolic disorders14. This index can provide more accurate information about the obesity status, by considering height, sex and race differences15. A recent review has introduced a global boundary value of WHtR < 0.5, which can be helpful in the prevention of CVDs and type 2 diabetes (T2D)16.
On the other hand, the most frequently utilized cutoff values of the mentioned indices are mainly based on European and American population data5,8,17, which might not be accurately applied in other groups. So, it is necessary to find appropriate cutoff values of each anthropometric index for the early detection and management of CVD risks in other countries and different ethnicity groups18.
To the best of our knowledge, there has been no study on the cutoff points of WHtR and other anthropometric indices for the Kurdish population. Therefore, given the obesity rate in Iran, this cross-sectional study was designed to determine the cutoff points of WHtR for the CVDs risk among Kurdish provinces in the West of Iran.
Methods
Study design and population
Study design
This study was conducted, for the first time, in the Iranian Kurdish cities, or Eastern Kurdistan, an unofficial name representing those parts of the northwestern Iran inhabited by Kurds and surrounded by Iraq and Turkey. This study was carried out using the baseline data obtained from Ravansar Non-Communicable Disease (RaNCD) cohort study. RaNCD has been a population-based ongoing study since 2014, aiming to investigate the non-communicable diseases among 10,065 Kurdish participants (4775 men and 5290 women) in the age range of 35–65 years in Ravansar city, Kermanshah Province, West of Iran. An expert cardiologist screened all of the patients to check the eligibility of conducting the study and pregnant women were excluded because of the high abdominal circumference. An informed consent was obtained from all subjects. This study was part of the Prospective Epidemiological Research Studies in Iran (PERSIAN) mega cohort study approved by the ethics committees at the Ministry of Health and Medical Education, the Digestive Diseases Research Institute, Tehran University of Medical Sciences, Iran. The details of the RaNCD cohort study protocol have been introduced in the previous studies19,20. Also, all experiments were performed in accordance with relevant guidelines and regulations. A written informed consent was obtained from each study participant at the beginning of the measurement.
Data collection
Data collection and measurements performed by well-trained interviewers in the study site in Ravansar. We used demographic data, anthropometric indices, blood pressure, and biochemical analyses for this study. Participants’ demographic and lifestyle information, including smoking and alcohol consumption history, was collected via face-to-face interviews using a standard questionnaire.
Anthropometry
Height was measured by the automatic stadiometer BSM 370 (Biospace Co., Seoul, Korea) with a precision of 0.1 cm while the person was in the standing position without shoes. Weight measurements were performed by InBody 770 device (Inbody Co, Seoul, Korea), we asked all participants to wear the least clothing and without shoes. Height and weight measurement performed only once. BMI was calculated based on the following formula: weight21/(Height) (Meter) (meter). WC and HC measured by using non-stretched and flexible tape in standing position three times, and their average was reported. Waist circumference (WC) assessed by measuring the distance around the narrowest area of the waist between the lowest rib and iliac crest and above the umbilicus using a no stretchable tape measure. HC measured at the maximum diameter of the hips. WHR was determined by dividing WC (cm) to HC (cm), also WC (cm) divided by height (cm) was considered as WHtR. The measurement of the anthropometric indices performed by a trained examiner based on the protocol of the RaNCD cohort study.
Blood pressure
After 4–5 min of rest, Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured by conventional sphygmomanometry and auscultation of the Korotkoff sounds in sitting position from both arms of all participants two times. The interval between the two measurements was 10 min and the mean of them was recorded as the final blood pressure19.
Biochemical analysis
After 12 h of fasting, venous blood samples were obtained from all of the participants. Total cholesterol20, high-density lipoproteins (HDL), and triglyceride (TG) concentration were measured by enzymatic kits (Pars Azmun, Iran). The Friedewald equation was used to calculate low-density lipoprotein (LDL-C) levels25. Fasting blood glucose (FBS) was measured using the hexokinase method26.
Cardiac events
In the current study, we considered the history of CVD, including angina and/or heart failure and/or history of myocardial infarction and/or stroke as cardiac events diagnosed based on participants self-reported and/or medication history examination during a single visit by physicians at the RaNCD cohort health examination center.
Metabolic syndrome
In our study, the metabolic syndrome (MetS) is defined using the harmonizing metabolic syndrome by the IDF/AHA/NHBLI standard. Any 3 of the 5 following risk factors were considered as a diagnosis indicator of MetS. This criterion included central obesity (waist circumference ≥ 93 cm for Iranian adults) as a national or regional cut point for WC. Other components included: (1) triglycerides ≥ 150 mg/dl, (2) HDL cholesterol ≤ 40 mg/dl for men or 50 mg/dl for women, (3) systolic/diastolic blood pressure ≥ 130/85 mmHg or receiving drug treatment, and (4) fasting plasma glucose ≥ 100 mg/dl21.
Statistical analysis
All data analyzed by the SPSS (version 18; SPSS Inc., Chicago, IL) and STATA (version 13, Stata Corp, College Station, TX) software, and P values < 0.05 were considered as significant. Quantitative data were reported as mean ± standard deviation and quality values were expressed as frequency (%). Pearson correlation coefficient was used to determine the relationship between WHtR with lipid profiles and anthropometric indices. Binary logistic regression in the unadjusted model was used to assess the cardiac events between anthropometric indices and CVD risk factors. By the receiver operating characteristic (ROC) analysis and considering the best combination of sensitivity and specificity, we determined the best cut-off points for anthropometric indices. Likelihood ratios, positive and negative predictive values with 95% confidence intervals were assessed in each cut-off point level for the diagnosis of cardiac events. Besides, the ROC curve comparison tests were used to identify the best anthropometric indices for detecting the best cardiac events predictor. Among semi-parametric, parametric, and non-parametric approaches to estimate the area under the ROC curves, the parametric method appeared the least appropriate for analyzing. Two methods commonly used for establishing the “optimal” cut-point, the point on the ROC curve closest to (0,1) and the Youden index, J. Both have sound intuitive interpretations and are generalizable to weighted sensitivity and specificity hence we used this method22. To determine the binary state variable, we use the cardiac events.
Results
Descriptive analysis
The general characteristics of the study population were stratified by sex (Table 1). A total of 10,065 participated in the study (5290 women and 4775 men); the mean age was 48.1 ± 8.25 years and the mean o BMI was 26.34 kg/m2 in men and 28.56 kg/m2 in women. The mean WC was 96.16 cm in men and 98.27 cm in women. In the men group 13.2% were drinkers and 22.5% were current smokers, while just 0.1% and 2% of the participant women were drinkers and current smokers, respectively. Men had higher values of TG, DBP and SBP. There was a marginal difference in LDL (P = 0.005), and slight differences were found for other lipid concentrations between men and women.
Table 1.
General characteristics of the studied population.
| Variable | Total (n = 10,065) | Men (n = 4775) | Women (n = 5290) | P* |
|---|---|---|---|---|
| Age (years) | 48.1 ± 8.25 | 47.82 ± 8.05 | 48.36 ± 8.41 | < 0.001 |
| Weight21 | 72.9 ± 13.64 | 76.58 ± 13.43 | 69.6 ± 12.95 | 0.035 |
| Height (cm) | 162.76 ± 9.3 | 170.33 ± 6.3 | 155.97 ± 5.56 | < 0.001 |
| BMI (kg/m2) | 27.51 ± 4.63 | 26.34 ± 4.06 | 28.56 ± 4.86 | < 0.001 |
| WC (cm) | 97.27 ± 10.81 | 96.16 ± 9.99 | 98.27 ± 11.4 | < 0.001 |
| WHR | 0.94 ± 0.05 | 0.94 ± 0.05 | 0.94 ± 0.06 | < 0.001 |
| WHtR | 0.59 ± 0.07 | 0.56 ± 0.05 | 0.63 ± 0.07 | < 0.001 |
| SBP (mm/Hg) | 109.67 ± 17.16 | 111.02 ± 16.78 | 108.45 ± 17.41 | < 0.001 |
| DBP (mm/Hg) | 70.66 ± 9.99 | 71.45 ± 9.86 | 69.94 ± 10.04 | 0.155 |
| TG (mg/dl) | 137.69 ± 84.32 | 145.95 ± 89.26 | 130.25 ± 78.87 | < 0.001 |
| HDL (mg/dl) | 46.42 ± 11.33 | 42.8 ± 10.07 | 49.68 ± 11.42 | < 0.001 |
| LDL (mg/dl) | 102.08 ± 25.43 | 101.08 ± 24.65 | 102.99 ± 26.09 | 0.005 |
| TC (mg/dl) | 185.51 ± 38.02 | 181.65 ± 36.47 | 189 ± 39.05 | 0.001 |
| FBS (mg/dl) | 97.06 ± 30.21 | 97.13 ± 30.98 | 96.99 ± 29.49 | 0.942 |
| Diabetic, N(%) | 819 (8.19) | 378 (7.9) | 441 (8.3) | 0.499 |
| Metabolic syndrome, N(%) | 4194 (41.7) | 1837 (38.5) | 2357 (44.6) | < 0.001 |
BMI body mass index, WC waist circumference, WHR waist to hip ratio, WHtR waist to height ratio, SBP systolic blood pressure, DBP diastolic blood pressure, TG triglyceride, HDL high density lipoprotein, LDL low density lipoprotein, TC Total cholesterol, FBS fasting blood sugar.
*P value was obtained student T test and Chi square.
Discrimination analysis
The area under the curve (AUCs) of the anthropometric indices and cardiac events are shown in Table 2. The AUCs for WHtR were meaningfully higher than those for BMI, WHR and WC. Furthermore, the cut-off values of the various anthropometric indices calculated by ROC analysis for cardiac events are presented in Table 2. The optimal BMI cut-off value for the prediction of obesity-related cardiac events was 27.50 kg/m2 in the whole study population. The optimal WC and WHtR cut-off values were 97.15 cm and 0.56, respectively. The area under the ROC curve of WHtR (AUC = 0.69, 95% CI 0.67–0.70) was higher than other anthropometric indices. The AUC for BMI was the lowest among other anthropometric indices AUC = 0.58 (95% CI 0.54–0.59) (Table 2) (Fig. 1). WC showed the highest sensitivity (68%) for prevalent cardiac events, while the sensitivity of BMI (41%) was the lowest. Furthermore, the highest and lowest specificities were revealed for BMI and WC (71%, 43%). The optimal cut-off value of WC in the males was > 96 cm, which was lower than that in the females, i.e. 99 cm; on the other hand, the optimal cut-off for WHtR was > 0.66 in the females, 0.56 in males. Both parameters were found to be better than BMI. The best cut-off value for BMI was > 27.02 kg/m2 in the males, while it was > 27.60 kg/m2 in the females. WHtR showed the highest likelihood ratios (3.2, 1.4) in men and women, receptively. The LR+ (positive Likelihood Ratio) for WHtR was 3.2 in male, 1.4 in females, subjects were 3.2 (2.6–3.9) and 1.4 (1.3–1.6) times more likely to have cardiac events, respectively (Table 2) (Figs. 1, 2).
Table 2.
Area under the receiver operating characteristic curve (and 95% confidence interval) and optimal cut-off values of diagnostic measures of anthropometric indices against CVD stratified by sex.
| Variables | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|
| WHtR | WC (cm) | BMI (kg/m2) | WHR | WHtR | WC (cm) | BMI (kg/m2) | WHR | |
| AUC (95% CI) | 0.74 (0.71–0.76) | 0.58 (0.56–0.61) | 0.57 (0.55–0.59) | 0.59 (0.56–0.62) | 0.67 (0.64–0.69) | 0.57 (0.55–0.59) | 0.56 (0.54–0.58) | 0.59 (0.57–0.61) |
| Cut-off | 0.56 | 96.05 | 27.02 | 0.96 | 0.65 | 99.5 | 27.60 | 0.96 |
| Sen (%) (95% CI) | 36.6 (30.0–43.6) | 28.3 (22.2–35.0) | 25.9 (20.0–32.4) | 59.5 (52.5–66.3) | 59.9 (53.8–65.7) | 35.1 (29.5–41.0) | 47.3 (41.3–53.4) | 50.9 (44.9–56.9) |
| Spc (%) (95% CI) | 88.5 (87.5–89.4) | 78.2 (76.9–79.4) | 79.1(77.9–80.3) | 57.5 (56.1–58.9) | 58.3 (56.9–59.6) | 68.0 (66.7–69.3) | 59.4 (58.0–60.8) | 56.1(54.7–57.5) |
| LR + (95% CI) | 3.2 (2.6–3.9) | 1.3 (1.0–1.6) | 1.2 (0.9–1.5) | 1.4(1.2–1.6) | 1.4 (1.3–1.6) | 1.1(0.9–0.3) | 1.2 (1.0–1.3) | 1.1(1.0–1.3) |
| LR-(95% CI) | 0.7 (0.7–0.8) | 0.9 (0.8–1.0) | 0.9 (0.8–1.0) | 0.7 (0.6–0.8) | 0.7 (0.6–0.8) | 0.9 (0.8–1.0) | 0.9 (0.7–0.9) | 0.8 (0.7–0.9) |
| PPV(95% CI) | 12.5 (9.9–15.4) | 5.49 (4.2–7.0) | 5.2 (3.9–6.8) | 5.9 (4.9–7.0) | 7.4 (6.3–8.6) | 5.7 (4.7–6.9) | 6.1(5.1–7.2) | 6.1 (5.1–7.1) |
| NPV(95% CI) | 96.9 (96.3–97.4) | 96.1(95.4–96.7) | 96.0 (95.3–96.6) | 96.9(96.2–97.6) | 96.3 (95.6–96.9) | 95.0 (94.2–95.6) | 95.3 (94.5–96.0) | 95.4 (94.5–96.1) |
| Corrected classified | 60 | 51 | 36 | 25 | 45 | 52 | 59 | 33 |
AUC area under the ROC curve, Sen sensitivity, Spc specificity, LR likelihood ratios, WC waist circumference, BMI body mass index, WHR waist to hip ratio, WHtR waist to height ratio.
There are no significant difference among AUCs (df = 3) = 130, P = < 0.001, (df = 3) = 336, P = < 0.001 in men and women respectively. Data are AUC (95% confidence interval).
Figure 1.
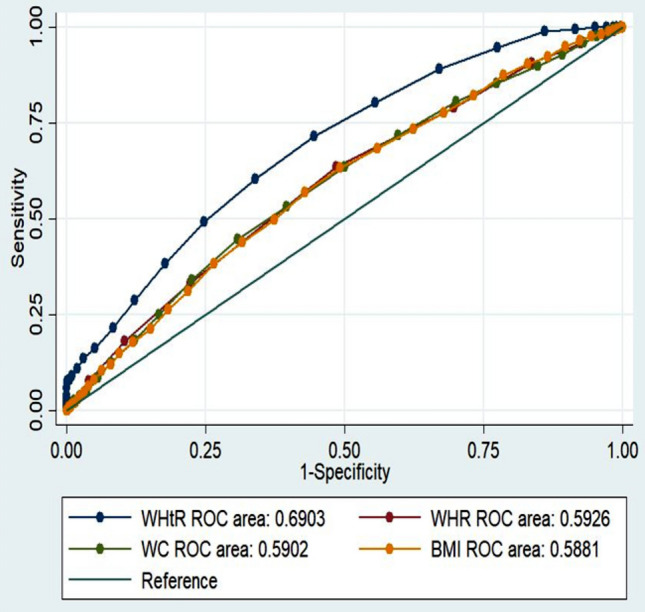
Comparison of AUC of the anthropometric indices for diagnosis of prevalent cardiac event in total.
Figure 2.
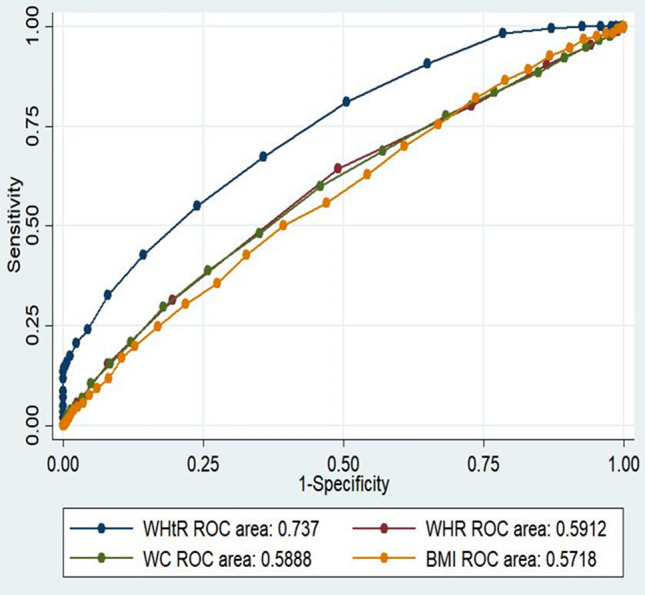
Comparison of AUC of the anthropometric indices for diagnosis of prevalent cardiac event in men.
One analysis assessed the accuracy of the anthropometric index in defining the CVD events. The percentage of individuals classified on the basis of each of the anthropometric indices for the general population was 55% by WHtR, 51% by WC, 49% by BMI and 30% by WHR. In the general population, ROC analysis displayed that WHtR could be a better predictor of CVD events than other anthropometric indices. More importantly, in women, the percentage of individuals classified for WC and BMI was greater than that based on WHtR (Table 2) (Figs. 2, 3).
Figure 3.
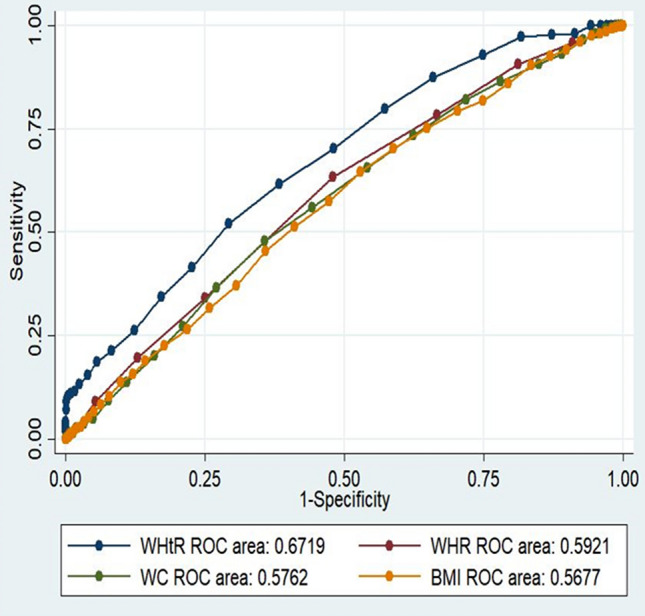
Comparison of AUC of the anthropometric indices for diagnosis of prevalent cardiac event in women.
The AUCs and ROC analysis of the anthropometric indices and MetS can be seen in Table 3. The AUCs for WC were meaningfully higher than those for BMI, WHtR and WHR. The area under the ROC curve of WC (AUC = 0.77, 95% CI 0.76–0.78) was higher than other anthropometric indices for MetS. The optimal cut-off value of WC in the males was > 94.8 cm, which was lower than that in the females, i.e., 98.7 cm; on the other hand, the optimal cut-off for WHtR was > 0.66 in males, and this was 0.56 in females. The optimal BMI cut-off value for MetS prediction was 27.6 kg/m2 in the whole study population. The best cut-off value for BMI was > 27 kg/m2 in males, while it was > 28.2 kg/m2 in the females. The percentage of individuals classified based on each of the anthropometric indices against MetS for the men and women was 71.9% and 68.5, respectively. According to WHtR, it was 70.9 and 57.9%, for WC, the percentages were 61.5 and 58.3% and finally, regarding BMI, 61.5 and 55.7% were obtained by WHR for males and females, respectively.
Table 3.
Area under the receiver operating characteristic curve (and 95% confidence interval) and optimal cut-off values of diagnostic measures of anthropometric indices against Metabolic syndrome stratified by sex.
| Variables | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|
| WHtR | WC (cm) | BMI (kg/m2) | WHR | WHtR | WC (cm) | BMI (kg/m2) | WHR | |
| AUC (95% CI) | 0.74(0.73–0.75) | 0.77(0.76–0.78) | 74.1(73.0–75.8) | 0.71(0.70–0.72) | 0.62 (0.60–0.63) | 62.5 (60.0–64.1) | 62.3 (60.8–63.8) | 0.53 (0.52–0.54) |
| Cut-off | 0.66 | 94.8 | 27 | 0.94 | 0.56 | 98.7 | 28.2 | 0.95 |
| Sen (%) (95% CI) | 73.5 (71.2–74.4) | 87.1(85.9–88.3) | 62.6 (60.1–64.8) | 70.4 (68.4–73.5) | 73.4 (69.4–77.5) | 57.0 (55.2–59.0) | 62.2 (60.1–64.2) | 71.8 (70.3–73.5) |
| Spc (%) (95% CI) | 69.2 (68.5–77.6) | 61.5 (69.0–52.1) | 70.3 (68.5–43.1) | 61.3 (58.3–64.3) | 65.3 (63.6–67.1) | 58.1(56.1–59.1) | 56.4 (54.8–58.3) | 42.7 (37.3–45.3) |
| LR + (95% CI) | 2.29 (2.17–2.32) | 2.3 (2.16–2.39) | 2.10 (1.91–2.21) | 1.81 (1.41–2.11) | 2.0 (1.84–2.17) | 1.40 (1.34–1.55) | 1.40 (1.21–1.59) | 1.2 (1.02–1.41) |
| LR-(95% CI) | 0.5 (0.48–0.55) | 0.22 (0.14–0.26) | 0.53 (0.49–0.57) | 0.48 (0.40–0.52) | 0.41 (0.32–0.49) | 0.8 (0.72–0.91) | 0.70 (0.68–0.72) | 0.65 (0.50–0.73) |
| PPV(95% CI) | 60.1(56.0–64.0) | 64.1 (61.1–67.0) | 63.4 (60.4–66.7) | 48.6 (46.9–50.3) | 53.7 (51.6–55.8) | 53.6 (51.2–56.0) | 53.6 (51.5–55.7) | 46.2 (44.8–47.6) |
| NPV(95% CI) | 64.7 (63.2–66.1) | 68.8 (67.3–70.3) | 68.3 (66.7–69.7) | 83.9 (82.0–85.8) | 62.2 (60.5–64.0) | 59.7 (58.1–61.3) | 61.7 (59.9–63.4) | 83.4 (78.6–87.5) |
| Corrected classified | 71.9 | 70.9 | 67.3 | 61.5 | 68.2 | 57.9 | 58.3 | 55.7 |
AUC area under the ROC curve, Sen sensitivity, Spc specificity, LR likelihood ratios, PPV positive predictive value, NPV negative predictive value, WC waist circumference, BMI body mass index, WHR waist to hip ratio, WHtR waist to height ratio.
There is no significant difference among AUCs (df = 3) = 130, P = < 0.001, (df = 3) = 336, P = < 0.001 in men and women respectively. Data are AUC (95% confidence interval).
Discussion
This study was intended to compare the anthropometric indices as the predictors of CVD to determine the best diagnostic parameter for cardiac events. Although BMI and WC are widely used, some studies have proposed that WHtR might be a more useful index to assess the adiposity and CVD risk5,8,16. The results of the current study indicated that WHtR might be the most accurate measure for detecting CVDs risk, among other anthropometric measurements. The present study, for the first time, revealed the precision, but not the accuracy of using WHtR for defining the cardiac events among Kurdish adults.
Epidemiological evidence shows that obesity could increase the risk of diabetes, CVD, all causing morbidity and mortality23. The most serious type of obesity is abdominal obesity, which increases the cardiometabolic risk24. There is no specific cutoff point to indicate the individuals at the risk of CVD in different populations18. The World Health Organization25 has proposed that the BMI cutoffs at which significant cardiometabolic risk is developed varies from 26.0 to 31.0 kg/m2, depending on the country, and there has been no prior study specifying the cutoff points for the Asian population, especially in the Iranian subjects with different ethnic or cultural backgrounds25. Previous studies have recommended that different BMI cut‐off points must be renewed among race/ethnic populations for better sensitivity and specificity26. The results of the present ROC analysis indicated that the BMI cut-off value for diagnosing cardiac events in men was 27.02 kg/m2 and 27.60 kg/m2 in women. Our results are in line with a longitudinal study conducted in the Iranian population to determine the cutoff values of the anthropometric variables in order to predict CVDs. Hadaegh et al.27 highlighted that the BMI cut-off point to predict various CVD risk factors in the Iranian population was 29.2 and 29.5 in men and women, respectively. Also, in other studies, it has been shown that the BMI cut-off point considered to predict various CVD risk factors in the Asian population was 23 kg/m2 in men and women18,28. The cut-off values obtained by our study for the Iranians were higher than those suggested for Asians and Caucasians: a finding consistent with several28,29 but not all previous studies.
WC ignores the effect of height on the cardiometabolic risk; so, some studies have highlighted that WC might be a better indicator of CVD risk than BMI in many race-ethnicity groups30,31 and abdominal fat accumulation; the high WC has been proved as a more reliable predictor of the risk of CVD in comparison with the overall obesity. In the western population, the WC cut-off value for defining the abdominal obesity is 102 cm for males and 88 cm for females32. There are still no clear WC cutpoints for the western Asians population33,34. Our results suggest that a WC of 96.05 cm in men and 99.5 cm in women should be considered as the cut-off points for CVD events prediction in the Kurdish adults. However, due to the low accuracy of this cut-point, it is not currently recommended. These results, therefore, indicated the inconsistency in WC thresholds in terms of sex, race and even country of origin29.
On the other hand, the specific cut-off point of a particular country cannot be generalized to all Asian Populations. The optimal WC cutoffs for predicting the cardiometabolic risk may differ among various Asian countries33; it is highly recommended that optimal WC cutoffs for abdominal obesity be attained across sexs or races. More recently, in a nationwide study of Iranian subjects, the means of WCs among women and men were 91 and 89 cm, respectively35. A higher WC in the Iranian women, as compared to other nations, might be attributed to their inactive life styles, genetic features, low smoking and high fertility rates36.
In line with the previous studies, as stated above, WC and BMI have some limitations in predicting the cardiovascular risk factors. It has been proposed that WHtR may be a simple anthropometric index for estimating the cardiometabolic risks in comparison to other anthropometric indices37. The results of our ROC analysis demonstrated that in both males and females, WHtR could be a better predictor of CVD events than WC, WHR and BMI; on the other hand, in another study, in the Australian population, it was found that WHtR was not better than WC or BMI in forecasting the CVD mortality38. In our study, the WHtR cut-off values considered to identify CVD events were 0.56 in men and 0.65 in women. These results were in close agreement with the findings of the previous studies carried out in the Iranian population27,39. Furthermore, the cut-off value of 0.5 for WHtR has been proposed as a better predictor of the CVD risk for both sexes in the European populations40. This is in agreement with our results, demonstrating that WHtR ≥ 0.5 is usually more sensitive (based on the ROC analysis) than WC ≥ 96 cm in women, and WC ≥ 96 cm in men, for the screening and diagnose of the CVD events8,15. Therefore, WHtR may have better efficacy than other anthropometric indices as a quantity of obesity to screen for CVD risk factors. WC has appeared as the second best anthropometric indicator for the screening of the CVD events. The greater AUC for WHtR in different population groups supports its use as a reliable screening tool for adiposity. Furthermore, the WHtR index overcomes some of the limitations of WC as it is adjusted for height. This is because, against other indices of abdominal adiposity, a world-wide cut-off points has been recommended for WHtR in numerous studies, apart from the necessity for age-, sex- and ethnic-specific cut-off standards1,14,37. While WHtR may be superior to BMI and WC in its discriminating power for the CVD events, as compared with WC, WHtR improved the discrimination of CVD by 9%. However, due to poor corrected classification, all of the indices in our study did not perform well enough to diagnose the CVD events. A value of 100% would suggest perfect discrimination, whereas 50% might show discrimination no superior than chance. In fact, most anthropometric measures are only expected to evaluate the cardiovascular risk factors with 60–70% accuracy8,14,15,17,32, as observed in our study; therefore, they should be regarded as the first‐stage, or population‐based, screening measures.
It seems that the effects of WC and BMI might be mediated by insulin resistance and other mechanisms such as inflammatory response. On the other hand, the application of WC to evaluate the CVD risk factors also lends support to the idea, although mistakenly, that risk stratification is not susceptible to individual height. The results of our ROC analyses demonstrated that WHtR was better than BMI and WC in predicting the CVD events in both sexes; interestingly, it was the best predictor in men. However, in women, the percentage of individuals correctly classified based on BMI and WC was greater based on WHtR. This could be related to the fact that BMI and WC might reflect the total body fat better than WHtR in women41. Furthermore, we examined anthropometric indices with cardiac events alone and with drugs-related CDV. All of the above were calculated as cardiac events and a sensitivity analysis excluding those participants having drugs-related CVD was conducted; the results did not change significantly.
Moreover, our results showed that women in the current survey were of a shorter height, as compared to European and Caucasian populations, which would cause the higher amount of body fat, as compared to the controls of the same ethnic group42,43. This evidence might possibly explain why WHtR and BMI are less sensitive tools for identifying CVD events in the short subjects.
Our results study showed that WHtR, as well as BMI and WC, could be useful for predicting MetS, which was consist with the study conducted by Rajput et al.44 Based on our AUC analysis, BMI, WC and WHtR were predictive of high metabolic risks in males (0.740, 0.770, and 0.740, respectively), whereas WHtR, BMI and WC were equally predictive of high MetS risks (0.62) in females. Liu et al.45 in their study of Chinese population, based on the ROC analyses of BMI, WC and WHtR values, indicated that the presence of multiple metabolic risk factors could be equally predicted, and the AUC values of BMI, WC and WHtR did not differ in men and women (0.702, 0.671 and 0.674, respectively). The appropriate cut-off values for BMI, WC and WHtR were 22.9 and 23.3 kg/m2, 91.3 cm and 87.1 cm, and 0.51 and 0.53 in men and women, respectively. Zeng et al. revealed that the ideal cut-off values to define obesity in Chinese adults were nearly 24.0 and 23.0 kg/m2 for BMI, 85.0 and 75.0 cm for WC, and 0.50 and 0.48 for WHtR in men and women, respectively. Ashwell et al. also stated that WC improved the identification of harmful CVD risk outcomes by 3%, as compared with BMI, and WHtR, enhancing the diagnosis by 4 to 5%. Additionally, WHtR was a robust prognosticator in comparison to WC CVD and37. In our cohort study, the best WHtR cutoff values for predicting MetS, according to WHtR, were 0.66 for men and 0.56 for women. The prevalence of MetS would be different based on various anthropometric indices46,47 and the criteria of MetS require more investigation to get a reliable and specific marker in order to classify MetS. Since obesity is the primary cause of the metabolic syndrome, it is essential to use the most reliable index to diagnose it. Furthermore, WHtR is reported as a simple and favorable index to identify MetS; some studies have also shown that the WHtR of more than 0.5 as the cut-off point can recognize people with a higher risk of MetS47. On the other hand, WHtR provides a universal cutoff value equally applicable in both sexes and different ages48. Such advantages have been summarized in the following public health motto: “Keep your waist circumference to less than half of your height”40.
The notable strength of the current study was the availability of the comprehensive data related to more than 10.000 subjects. However, there are some limitations; first, the data concerning diet and physical activity were not taken into account in the analysis because of the scarcity of such information. Secondly, we had to use the CVD events as the dependent variables to test WHtR and it was necessary to extend these findings, which were stratified by cardiovascular disease risk factors. The other limitation is that anthropometric measurements were measured once, while two measurements are usually needed; in some cases, three repeats are even required. Furthermore, it must be emphasized that for the cut-off point drawn from this study, based on the study of Kurdish people in the western part of Iran, additional studies are still needed to conclude that our results could be applied to other populations. Additionally, the lack of body composition analysis and skinfold thickness values to measure adiposity was another limitation in our study.
Conclusion
WHtR is a simple and effective index to predict the presence of the CVD events in the Kurdish population; so, it might be a better predictor than WC and BMI. Indeed, we could conclude that a WHtR of > 0.56 is better for the diagnosis of a population with CVD events. Our analyses highlighted the variability of the optimal cutoff points for different anthropometric indices among men and women; it is necessary to organize them to determine the optimum cut points in different Asian countries, especially in the Iranian women. Further studies are also required to determine the precise cut-off points to extend these findings for cardiovascular disease risk factors. Finally, we recommend that BMI = 27.02 kg/m2 in men and 27.60 kg/m2 in women, WC of 96.05 cm in men and 99.5 cm in women, WHRs of 0.96 in both, and WHtR of 0.56 in men and 0.65 in women would define the CVD events in the Kurdish population. Furthermore, the present study showed the precision but not the accuracy of using WHtR for defining the cardiac events among Kurdish adults for the first time. So, these anthropometric indices may be used as a noninvasive approach that could be useful as a prescreening tool rather than a diagnostic one.
Author contributions
Y.P, F.N, S.M and B.H.: provided the conception and design of the study, acquisition of data, analysis, and interpretation of data, drafting the article, revising it critically for important intellectual content, and final approval of the version to be submitted; J.M and S.S: drafting of the manuscript; Y.P. MA.J, M.M: supplied the design of the study, analysis, and interpretation; M.A.J, S.S.: supplied the acquisition of data and all of Authors’: provided the revised the article critically for important intellectual content and gave final approval of the version1 to be submitted.
Funding
RaNCD is part of the PERSIAN national cohort, and we would like to thank Prof. Reza Malekzadeh, the Deputy of Research and Technology at the Ministry of Health and Medical Education of Iran and Director of the PERSIAN cohort, as well as Dr. Hossein Poustchi, the Executive Director of the PERSIAN cohort, for all their support during the design and implementation of the RaNCD cohort. This study was supported by the Ministry of Health and Medical Education of Iran and Kermanshah University of Medical Sciences (Grant No. 92472).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Vikram NK, et al. Waist-to-height ratio compared to standard obesity measures as predictor of cardiometabolic risk factors in Asian Indians in North India. Metab. Syndr. Relat. Disord. 2016;14:492–499. doi: 10.1089/met.2016.0041. [DOI] [PubMed] [Google Scholar]
- 2.Moludi J, et al. Metabolic endotoxemia and cardiovascular disease: A systematic review about potential roles of prebiotics and probiotics. Clin. Exp. Pharmacol. P. 2020;47(6):927–939. doi: 10.1111/1440-1681.13250. [DOI] [PubMed] [Google Scholar]
- 3.Hajian-Tilaki KO, Heidari B. Prevalence of obesity, central obesity and the associated factors in urban population aged 20–70 years, in the north of Iran: a population-based study and regression approach. Obes. Rev. 2007;8:3–10. doi: 10.1111/j.1467-789X.2006.00235.x. [DOI] [PubMed] [Google Scholar]
- 4.Jokinen E. Obesity and cardiovascular disease. Minerva Pediatr. 2015;67:25–32. [PubMed] [Google Scholar]
- 5.Gupta N, et al. Improved utilization of waist‐to‐height ratio in cardiometabolic risk counselling in children: Application of DMAIC strategy. J. Eval. Clin. Pract. 2019;25(2):300–305. doi: 10.1111/jep.13055. [DOI] [PubMed] [Google Scholar]
- 6.Miralles CSW, et al. Waist-to-height ratio (WHtR) and triglyceride to HDL-c ratio (TG/HDL-c) as predictors of cardiometabolic risk. Nutr. Hosp. 2015;31:2115–2121. doi: 10.3305/nh.2015.31.5.7773. [DOI] [PubMed] [Google Scholar]
- 7.Pearson TA, et al. AHA guidelines for primary prevention of cardiovascular disease and stroke: 2002 update: consensus panel guide to comprehensive risk reduction for adult patients without coronary or other atherosclerotic vascular diseases. Circulation. 2002;106:388–391. doi: 10.1161/01.cir.0000020190.45892.75. [DOI] [PubMed] [Google Scholar]
- 8.Ashwell M, Gibson S. Waist-to-height ratio as an indicator of ‘early health risk’: simpler and more predictive than using a ‘matrix’ based on BMI and waist circumference. BMJ Open. 2016;6:e010159. doi: 10.1136/bmjopen-2015-010159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beechy L, Galpern J, Petrone A, Das SK. Assessment tools in obesity—psychological measures, diet, activity, and body composition. Physiol. Behav. 2012;107:154–171. doi: 10.1016/j.physbeh.2012.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guan X, et al. Associations between metabolic risk factors and body mass index, waist circumference, waist-to-height ratio and waist-to-hip ratio in a Chinese rural population. J. Diabetes Investig. 2016;7:601–606. doi: 10.1111/jdi.12442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Teigen LM, Kuchnia AJ, Mourtzakis M, Earthman CP. The use of technology for estimating body composition: strengths and weaknesses of common modalities in a clinical setting. Nutr. Clin. Pract. 2017;32:20–29. doi: 10.1177/0884533616676264. [DOI] [PubMed] [Google Scholar]
- 12.Gonzalez MC, Heymsfield SB. Bioelectrical impedance analysis for diagnosing sarcopenia and cachexia: what are we really estimating? J. Cachexia Sarcopenia Muscle. 2017;8:187–189. doi: 10.1002/jcsm.12159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Diaz E, Villar J, Immink M, Gonzales T. Bioimpedance or anthropometry? Eur. J. Clin. Nutr. 1989;43:129–137. [PubMed] [Google Scholar]
- 14.Yang H, Xin Z, Feng J-P, Yang JK. Waist-to-height ratio is better than body mass index and waist circumference as a screening criterion for metabolic syndrome in Han Chinese adults. Medicine. 2017;96:e8192. doi: 10.1097/MD.0000000000008192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Correa MM, Thume E, De Oliveira ERA, Tomasi E. Performance of the waist-to-height ratio in identifying obesity and predicting non-communicable diseases in the elderly population: a systematic literature review. Arch. Gerontol. Geriatr. 2016;65:174–182. doi: 10.1016/j.archger.2016.03.021. [DOI] [PubMed] [Google Scholar]
- 16.Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr. Res. Rev. 2010;23:247–269. doi: 10.1017/S0954422410000144. [DOI] [PubMed] [Google Scholar]
- 17.Corrêa MM, Tomasi E, Thumé E, Oliveira ERA, Facchini LA. Waist-to-height ratio as an anthropometric marker of overweight in elderly Brazilians. Cad. Saude Publ. 2017;33:e00195315. doi: 10.1590/0102-311X00195315. [DOI] [PubMed] [Google Scholar]
- 18.Misra A, et al. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. JAPI. 2009;57:163–170. [PubMed] [Google Scholar]
- 19.Pasdar Y, et al. Cohort profile: Ravansar non-communicable disease cohort study: the first cohort study in a Kurdish population. Int. J. Epidemiol. 2019;48:682. doi: 10.1093/ije/dyy296. [DOI] [PubMed] [Google Scholar]
- 20.Poustchi H, et al. Prospective epidemiological research studies in Iran (the PERSIAN Cohort Study): rationale, objectives, and design. Am. J. Epidemiol. 2017;187:647–655. doi: 10.1093/aje/kwx314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alberti K, et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 22.Detilleux J, Arendt J, Lomba F, Leroy P. Methods for estimating areas under receiver-operating characteristic curves: illustration with somatic-cell scores in subclinical intramammary infections. Prev. Vet. Med. 1999;41:75–88. doi: 10.1016/s0167-5877(99)00054-9. [DOI] [PubMed] [Google Scholar]
- 23.Ford ES. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. Diabetes Care. 2005;28:1769–1778. doi: 10.2337/diacare.28.7.1769. [DOI] [PubMed] [Google Scholar]
- 24.Després J-P, et al. Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk. Arterioscler. Thromb. Vasc. Biol. 2008;28:1039–1049. doi: 10.1161/ATVBAHA.107.159228. [DOI] [PubMed] [Google Scholar]
- 25.Who EC. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet (London, England) 2004;363:157. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 26.Kuczmarski RJ, Flegal KM, Campbell SM, Johnson CL. Increasing prevalence of overweight among US adults: the National Health and Nutrition Examination Surveys, 1960 to 1991. JAMA. 1994;272:205–211. doi: 10.1001/jama.272.3.205. [DOI] [PubMed] [Google Scholar]
- 27.Hadaegh F, et al. Appropriate cutoff values of anthropometric variables to predict cardiovascular outcomes: 7.6 years follow-up in an Iranian population. Int. J. Obes. 2009;33:1437. doi: 10.1038/ijo.2009.180. [DOI] [PubMed] [Google Scholar]
- 28.Temcharoen P, et al. The optimal cut-off points of body mass index which reflect the risk factors of cardiovascular disease in the urban Thai male population. J. Med. Assoc. Thail. Chotmaihet Thangphaet. 2009;92:S68–S74. [PubMed] [Google Scholar]
- 29.Misra A, Wasir JS, Vikram NK. Waist circumference criteria for the diagnosis of abdominal obesity are not applicable uniformly to all populations and ethnic groups. Nutrition. 2005;21:969–976. doi: 10.1016/j.nut.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 30.Savva S, et al. Waist circumference and waist-to-height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. Int. J. Obes. 2000;24:1453. doi: 10.1038/sj.ijo.0801401. [DOI] [PubMed] [Google Scholar]
- 31.Lee CMY, Huxley RR, Wildman RP, Woodward M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J. Clin. Epidemiol. 2008;61:646–653. doi: 10.1016/j.jclinepi.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 32.Aschner P, et al. Determination of the cutoff point for waist circumference that establishes the presence of abdominal obesity in Latin American men and women. Diabetes Res. Clin. Pract. 2011;93:243–247. doi: 10.1016/j.diabres.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 33.Zeng Q, et al. Optimal cut-off values of BMI, waist circumference and waist: height ratio for defining obesity in Chinese adults. Br. J. Nutr. 2014;112:1735–1744. doi: 10.1017/S0007114514002657. [DOI] [PubMed] [Google Scholar]
- 34.Misra A, et al. Waist circumference cutoff points and action levels for Asian Indians for identification of abdominal obesity. Int. J. Obes. 2006;30:106. doi: 10.1038/sj.ijo.0803111. [DOI] [PubMed] [Google Scholar]
- 35.Delavari A, Forouzanfar MH, Alikhani S, Sharifian A, Kelishadi R. First nationwide study of the prevalence of the metabolic syndrome and optimal cutoff points of waist circumference in the Middle East: the national survey of risk factors for noncommunicable diseases of Iran. Diabetes Care. 2009;32:1092–1097. doi: 10.2337/dc08-1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Janghorbani M, et al. First nationwide survey of prevalence of overweight, underweight, and abdominal obesity in Iranian adults. Obesity. 2007;15:2797–2808. doi: 10.1038/oby.2007.332. [DOI] [PubMed] [Google Scholar]
- 37.Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes. Rev. 2012;13:275–286. doi: 10.1111/j.1467-789X.2011.00952.x. [DOI] [PubMed] [Google Scholar]
- 38.Welborn T, Dhaliwal S. Preferred clinical measures of central obesity for predicting mortality. Eur. J. Clin. Nutr. 2007;61:1373. doi: 10.1038/sj.ejcn.1602656. [DOI] [PubMed] [Google Scholar]
- 39.Hsieh SD, Yoshinaga H. Waist/height ratio as a simple and useful predictor of coronary heart disease risk factors in women. Intern. Med. 1995;34:1147–1152. doi: 10.2169/internalmedicine.34.1147. [DOI] [PubMed] [Google Scholar]
- 40.Ashwell M, Hsieh SD. Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. Int. J. Food Sci. Nutr. 2005;56:303–307. doi: 10.1080/09637480500195066. [DOI] [PubMed] [Google Scholar]
- 41.Pouliot M-C, et al. Waist circumference and abdominal sagittal diameter: best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women. Am. J. Cardiol. 1994;73:460–468. doi: 10.1016/0002-9149(94)90676-9. [DOI] [PubMed] [Google Scholar]
- 42.Lara-Esqueda A, et al. The body mass index is a less-sensitive tool for detecting cases with obesity-associated co-morbidities in short stature subjects. Int. J. Obes. 2004;28:1443. doi: 10.1038/sj.ijo.0802705. [DOI] [PubMed] [Google Scholar]
- 43.López-Alvarenga JC, Montesinos-Cabrera RA, Velázquez-Alva C, González-Barranco J. Short stature is related to high body fat composition despite body mass index in a Mexican population. Arch. Med. Res. 2003;34:137–140. doi: 10.1016/S0188-4409(03)00002-X. [DOI] [PubMed] [Google Scholar]
- 44.Rajput R, et al. Waist height ratio: a universal screening tool for prediction of metabolic syndrome in urban and rural population of Haryana. Indian J. Endocrinol. Metab. 2014;18:394–399. doi: 10.4103/2230-8210.131201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liu Y, Tong G, Tong W, Lu L, Qin X. Can body mass index, waist circumference, waist-hip ratio and waist-height ratio predict the presence of multiple metabolic risk factors in Chinese subjects? BMC Publ. Health. 2011;11:35. doi: 10.1186/1471-2458-11-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hsieh SD, Muto T. Metabolic syndrome in Japanese men and women with special reference to the anthropometric criteria for the assessment of obesity: proposal to use the waist-to-height ratio. Prev. Med. 2006;42:135–139. doi: 10.1016/j.ypmed.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 47.Alberti KGMM, Zimmet P, Shaw J. Metabolic syndrome—a new world-wide definition. A consensus statement from the international diabetes federation. Diabetic Med. 2006;23:469–480. doi: 10.1111/j.1464-5491.2006.01858.x. [DOI] [PubMed] [Google Scholar]
- 48.Savva SC, Lamnisos D, Kafatos AG. Predicting cardiometabolic risk: waist-to-height ratio or BMI. A meta-analysis. Diabetes Metab. Syndr. Obes. Targets Ther. 2013;6:403. doi: 10.2147/DMSO.S34220. [DOI] [PMC free article] [PubMed] [Google Scholar]


