Abstract
Cardiac rehabilitation (CR) is an evidence-based intervention that uses patient education, health behavior modification, and exercise training to improve secondary prevention outcomes in patients with cardiovascular disease. CR programs reduce morbidity and mortality rates in adults with ischemic heart disease, heart failure, or cardiac surgery but are significantly underused, with only a minority of eligible patients participating in CR in the United States. New delivery strategies are urgently needed to improve participation. One potential strategy is home-based CR (HBCR). In contrast to center-based CR services, which are provided in a medically supervised facility, HBCR relies on remote coaching with indirect exercise supervision and is provided mostly or entirely outside of the traditional center-based setting. Although HBCR has been successfully deployed in the United Kingdom, Canada, and other countries, most US healthcare organizations have little to no experience with such programs. The purpose of this scientific statement is to identify the core components, efficacy, strengths, limitations, evidence gaps, and research necessary to guide the future delivery of HBCR in the United States. Previous randomized trials have generated low-to moderate-strength evidence that HBCR and center-based CR can achieve similar improvements in 3- to 12-month clinical outcomes. Although HBCR appears to hold promise in expanding the use of CR to eligible patients, additional research and demonstration projects are needed to clarify, strengthen, and extend the HBCR evidence base for key subgroups, including older adults, women, underrepresented minority groups, and other higher-risk and understudied groups. In the interim, we conclude that HBCR may be a reasonable option for selected clinically stable low- to moderate-risk patients who are eligible for CR but cannot attend a traditional center-based CR program.
Keywords: cardiac rehabilitation, behavior therapy, exercise, patient education
Cardiac rehabilitation (CR) services are an integral component in the continuum of care for patients with cardiovascular disease (CVD).1,2 A Class IA recommendation, referral to CR is 1 of 9 performance measures for secondary prevention established by the American Heart Association and American College of Cardiology3 after myocardial infarction (MI),4,5 percutaneous coronary intervention,6 or coronary artery bypass graft surgery7 or in the setting of stable angina8 or symptomatic peripheral arterial disease (ie, intermittent claudication).9 Referral to CR is also recommended after heart valve surgery10 or cardiac transplantation11 or in the setting of chronic heart failure (HF) with reduced ejection fraction.12 Referral to CR after MI is part of the “defect-free care” performance measure that is included by the Centers for Medicare & Medicaid Services in the consensus core set of cardiovascular performance measures.13,14 The safety and effectiveness of the traditional medically supervised, center-based CR (CBCR) model are well established, and CBCR is effective in reducing hospital readmissions, secondary events, and mortality in patients with CVD.1,2,15–21
Unfortunately, the impact of CBCR in the United States has been substantially limited by significant underuse among eligible patients. Data from several registries and databases indicate that although referral to CBCR is generally improving, patient participation remains low across most demographic groups.22 Between 2007 and 2011, only 16.3% of Medicare patients and 10.3% of veterans participated in CR after hospitalization for MI, percutaneous coronary intervention, or coronary artery bypass graft surgery.22 Participation is especially low for Medicare beneficiaries, veterans, women, older adults, and individuals from underserved populations, including those from underserved minority groups, those of lower socioeconomic status, and those who are uninsured or underinsured.
It is clear that new CR delivery strategies are urgently needed for the >80% of eligible patients in the United States who do not participate in CR.23,24 One potential approach is alternative site- or home-based CR (HBCR), which can be carried out in a variety of settings, including the home or other non clinical settings such as community centers, health clubs, and parks. In concept, HBCR could help overcome some of the barriers that CBCR programs face, including geographic, logistical, and other access-related barriers. Although home-based exercise training is commonly recommended by CBCR staff for their patients on days when they are not physically present in the CBCR center, “stand-alone” HBCR programs are still in their infancy. However, the European guidelines on CVD prevention stat ethat “home-based rehabilitation with and without telemonitoring holds promise for increasing participation and supporting behavioral change.”25 In addition, Cochrane collabrative reviews of CR have combined randomized studies of CBCR and HBCR trials, and a recent comparison of CBCR and HBCR has concluded that there is low- to moderate-strength evidence that HBCR and CBCR have similar effects on quality of life and cost among patients with recent MI or coronary revascularization.15,26–28
The use of HBCR, either alone or in combination with CBCR (ie, a hybrid approach to CR), represents a possible alternative that may improve the delivery of CR to eligible patients. HBCR has been incorporated into the healthcare systems of several countries, including Australia, Canada, and the United Kingdom. The British Heart Foundation recently reported that in the United Kingdom >50% of eligible patients are now participating in CR after a cardiac event or procedure.29 Table 1 lists potential advantages and disadvantages of HBCR, including the possibility that HBCR could help to overcome some of the logistical barriers (eg, transportation and scheduling barriers) that patients in CBCR programs face. In addition, HBCR has the potential to expand the breadth and depth of educational, counseling, and monitoring options for patients because HBCR services can potentially be used 24 hours a day, 7 days a week, whereas most CBCR programs are usually limited to the 3 to 4 hours of weekly in-person contact between CBCR patients and staff. Because most patients with CVD spend >5000 waking hours each year independent of medical providers,30 it is critically important to arm them with behavioral change strategies that can be implemented in their home, work, or community environments. Unfortunately, HBCR faces substantial challenges to implementation in the United States, most notably a lack of reimbursement by the Centers for Medicare & Medicaid Services and other third-party payers. Of interest, in a recent study of CR-eligible patients, when given the option to receive CR through a home-based or a center-based approach, nearly half preferred a home-based approach.31
Table 1.
Potential Advantages and Disadvantages of HBCR Compared With CBCR
| Potential Advantages | Potential Disadvantages |
|---|---|
| Reduced enrollment delays | Lack of reimbursement |
| Expanded capacity/access | Less intensive exercise training |
| Individually tailored programs | Less social support |
| Flexible, convenient scheduling | Less patient accountability |
| Minimal travel/transportation barriers | Lack of published standards for HBCR |
| Greater privacy while receiving CR services | Less face-to-face monitoring and communication |
| Integration with regular home routine | Safety concerns for patients at higher risk |
CBCR indicates center-based cardiac rehabilitation; CR, cardiac rehabilitation; and HBCR, home-based cardiac rehabilitation
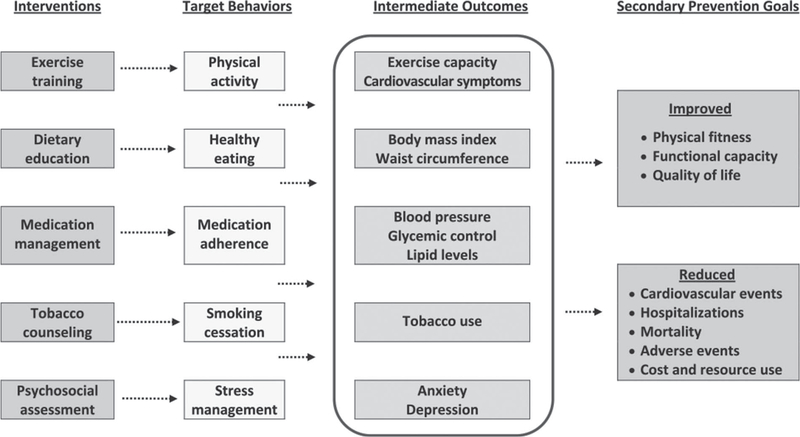
Both CBCR and HBCR include a number of elements that overlap with usual care, including management of lipids, blood pressure, diabetes mellitus, and cardioprotective medications (such as antiplatelet agents, β-blockers, angiotensin inhibitors, and statins). However, both types of CR are differentiated from usual care by their systematic, multidisciplinary, and team-based approach to patient-centered care that includes behavioral counseling and patient activation, which are promoted through multiple, individualized interactions with patients over time. CR services empower patients to meet the goals of increased physical activity, improved dietary habits, optimal adherence to prescribed medications, smoking cessation, and optimal psychosocial well-being, thereby helping them to reduce their risk of future CVD events (Figure 1).
Figure 1.
Target health behaviors for cardiac rehabilitation
The purpose of this scientific statement is to identify the core components, efficacy, strengths, limitations, evidence gaps, and research necessary to guide the future delivery and potential reimbursement of HBCR in the United States. Such work has been previously carried out for CBCR32 but not for HBCR, defined herein as systematic, comprehensive, and personalized services that involve medical evaluation, prescribed exercise, cardiovascular risk factor modification, patient education, and behavioral activation/counseling that are delivered mostly or entirely outside of the traditional CBCR setting. This is in contrast to traditional CR services that are implemented in a medical facility and require direct in-person observation of patients.
EVIDENCE FROM PUBLISHED STUDIES COMPARING HBCR AND CBCR
The writing group carried out a systematic review of published studies of HBCR compared with CBCR to assess the comparative effectiveness and potential benefits of HBCR and to explore implementation strategies for developing HBCR programs.
SEARCH STRATEGY AND DATA SOURCES
Comprehensive literature searches of Embase, CINAHL, PsychINFO, PubMed, Web of Science, and the Cochrane Library databases were conducted for peer-reviewed articles published from January 1980 to January 2017. Examples of heading search terms were CR, secondary prevention, and HBCR.
STUDY SELECTION
Previous meta-analyses and systematic reviews of randomized trials have demonstrated that CBCR improves morbidity, mortality, and health-related quality of life (HRQOL) in patients with an MI or those who have undergone coronary revascularization. For this review, 4 members of the writing group (T.M. Beckie, T.M. Brown, D.W.K., and R.J.T.) oversaw the literature search process and identified 23 studies that used randomized, experimental designs that directly compared the outcomes of HBCR and CBCR. These studies served as the primary scientific basis from which the writing group formulated this scientific statement. Meta-analyses, systematic reviews, qualitative studies, published letters, editorials, and case reports were excluded. Studies comparing HBCR with usual care were also excluded. Patient populations included adults with MI, stable angina, or HF and those having undergone coronary revascularization. Studies were included if they evaluated ≥1 of the following health outcomes: mortality, morbidity (reinfarction, revascularization, or cardiac-related hospitalization), exercise capacity, modifiable cardiovascular risk factors (eg, smoking, lipids, blood pressure, blood glucose, exercise capacity), HRQOL, adverse events, health services use, cost, or intervention adherence.
DATA EXTRACTION
Supplemental Table 1 presents the categories of information extracted from the 23 studies reviewed: design, participants and intervention details, length of follow-up, adherence, and health outcomes. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement and recommendations were used to guide the development and completion of this systematic review.33 We evaluated study risk of bias using the CONSORT (Consolidated Standards for Reporting Trials) statement criteria (eg, allocation concealment, dropouts and withdrawals, outcome blinding, and use of intention-to-treat analysis).34
Five of the 23 studies were conducted in the United States35–39; 3 were conducted in the United Kingdom28,40,41; 2 were conducted in Norway,42,43 Turkey,44,45 and Canada,46,47; and 1 was conducted in Denmark,48 Poland,49 Iran,50 Australia,51 Taiwan,52 Italy,53 and the Netherlands.54 Given the differences in healthcare systems and costs in the various countries, it is a limitation that we do not have specific analyses for studies from each of the various countries. However, to address this point, we have mentioned the results of the US studies separately in the sections related to cost and healthcare use, the issues that may be particularly affected by the country in which the studies were performed. Five studies were published in the year 2000 or earlier; 9 were published between 2001 and 2010; and 7 were published in 2011 and later. Trial sample sizes ranged from 20 to 525 patients (total sample, 2951) with follow-up ranging from very soon after intervention (eg, 6, 8, 12, or 24 weeks) to 6 years later. Although most studies included patients with uncomplicated MI or after coronary revascularization, 4 studies exclusively studied patients with HF.36,44,45,49 The duration (range, 1–6 months) and frequency (1–5 sessions per week) of the HBCR and CBCR interventions reported in the studies varied significantly, making direct comparisons challenging. Fourteen studies evaluated comprehensive programs (eg, exercise training in addition to education or psychological management), and 7 studies implemented an exercise-only intervention.38,39,42,44,45,50,52,55 One study evaluated a hybrid program that started with identical interventions in both HBCR and CBCR participants for the first 4 weeks, but from weeks 6 to 24, HBCR participants could participate in either HBCR or CBCR exercise sessions.35 Other HBCR interventions began with 2 to 8 supervised sessions in the CBCR facility followed by HBCR exercises.27,42,47,53–55
CORE COMPONENTS OF HBCR INTERVENTIONS
The American Heart Association and the American Association of Cardiovascular and Pulmonary Rehabilitation have previously defined the core components of CBCR known to optimize cardiovascular risk reduction, to enhance healthy behaviors, and to reduce cardiovascular morbidity and mortality.32 The 5 core components are patient assessment, exercise training, dietary counseling, risk factor management (smoking, lipids, blood pressure, weight, diabetes mellitus), and psychosocial intervention. These same 5 components were used in the interventions incorporated into the HBCR studies we reviewed (Supplemental Table 2). We have adjusted these components slightly, as described in the Core Components of HBCR Interventions section below and shown in Figure 2, to include medication adherence to emphasize the patient’s role in the medical control of lipids, blood pressure, diabetes mellitus, or body weight. We believe it is critical for both providers and patients to design HBCR programs to include important and effective risk-modifying health behaviors that patients can directly control(physical activity, healthy eating, medication adherence, smoking, and stress management).
Figure 2.
Structure, process, and outcome metrics for home-based cardiac rehabilitation.
PATIENT ASSESSMENT
All studies we reviewed included an initial baseline evaluation of participants. Details of those assessments varied but generally followed the recommendations for patient assessment that were outlined by Balady et al32 and included a participant’s medical history, physical examination, and testing. The medical history encompasses cardiovascular events, procedures and surgery, left ventricular function, comorbid conditions (eg, mental health and substance abuse), current symptoms (eg, chest pain, shortness of breath, lower extrmity edema), and lifestyle habits (dietary, physical activity, tobacco and alcohol habits). The physical examination includes a full cardiovascular-focused examination. Testing includes the assessment of physical fitness (usually measured by maximal exercise capacity or distance on a 6-minute walk test) and other components that help to assess cardiovascular health, including a 12-lead ECG, blood pressure, resting heart rate, lipid levels, body mass index, waist circumference, waist-to-hip ratio, blood glucose, glycosylated hemoglobin, psychosocial factors (eg, marital status, social support, anxiety, and depressive symptoms), frailty (eg, neuromuscular status, balance, and cognition function), sleep-related health, and patient-reported quality of life.
EXERCISE TRAINING
All interventions in the studies we reviewed, whether HBCR or CBCR, included an exercise training component. CBCR exercise sessions ranged in intensity (50%–95% of peak heart rate, heart rate reserve, or exercise capacity), modality (cycle ergometer, treadmill walking, circuit training, cross-country skiing, hall games), and duration (20–80 minutes per session, including warm-up and cool-down exercises). In some cases, intensity or modality was not reported.51,55,56 Most CBCR programs were supervised, group based, or monitored by electrocardiographic telemetry. The majority of HBCR exercise protocols involved walking with variable support via telephone calls or home visits from a physical therapist, exercise physiologist, or nurse. One HBCR program provided 4 weeks (12 sessions) of supervised CBCR exercise sessions with electrocardiographic monitoring,35 and another provided 12 onsite visits or telephone calls, depending on patient preference.37 Three studies provided heart rate monitors,45,53,54 and 2 others provided remote electrocardiographic telemetry monitoring.39,49
The provision of home exercise equipment is a potentially important component of HBCR that has not been thoroughly evaluated by the existing studies. In the hybrid CBCR/HBCR intervention tested in the HF-ACTION study (Heart Failure: A Controlled Trial Investigating Outcomes of Exercise Training), the provision of home exercise treadmills or stationary cycles plus a heart rate monitor during the HBCR portion of the intervention was associated with modest adherence in the intervention group.57 However, HF-ACTION did not include an intervention group that was not supplied with home equipment. Indeed, it does not appear that any study formally tested the effect of supplying exercise equipment on adherence/retention in HBCR. Although most patients can achieve recommended levels of physical activity with brisk walking or jogging, some patients may be unable to walk briskly or jog because of comorbid conditions or logistical barriers (eg, lack of access to a safe walking surface or gym). Evolving data suggest that the inclusion of other training modalities beyond brisk walking or jogging can result in additional health benefits. However, the use of such equipment in HBCR represents an area for additional study.
DIETARY/WEIGHT MANAGEMENT
Although details about the frequency and content of dietary/weight management services were generally not clearly described in the publications reviewed, most CBCR programs provided dietary counseling through education sessions35,37,39–41,43,47,48,51,53,54 or with input from a dietitian.46,56 Dietary information was conveyed in HBCR programs via the telephone,40,46 weekly educational and counseling meetings,35,37,43 home visits,41 dietary counseling sessions and practice cooking sessions,48 educational materials,39 or a web portal or smartphone.51
PSYCHOLOGICAL SUPPORT/MANAGEMENT
Although not always described clearly, several of the studies we reviewed offered psychological support or stress management in both the CBCR and HBCR arms.35,40,41,46.49,51,54,56 Only 1 study made any reference to a theoretical foundation for its behavior change interventions.35 Kraal and colleagues54 specifically described using principles of goal setting and motivational interviewing in both HBCR and CBCR interventions.
MEDICATION ADHERENCE
Although medication adherence was not a reported outcome of any of the studies reviewed, several interventions included some form of education on medications35,37,39,40,51,58 or provided access to a pharmacist.56
RISK FACTOR MANAGEMENT
Although the studies we reviewed focused on improving cardiovascular risk factor control in study participants, the methods incorporated into the studies to achieve improved risk factor control generally involved multicomponent strategies to improve lifestyle habits and adherence to prescribed medications. Smoking cessation strategies are particularly important components of CR services, and several studies outside the CR setting support the use of home-based and mobile health delivery models of smoking cessation.59 Although the HBCR studies included in this statement did not include adjustment of medication therapy for CVD risk factor management, close coordination of care between the CR staff and the patient’s physician is critically important as the need arises for adjustments in preventive medications. In addition, several components of HBCR and CBCR exert an important effect on CVD risk factor control, including counseling to optimize exercise training, dietary therapy, stress management, and medication adherence. Three studies explicitly reported providing education on signs and symptoms of coronary heart disease and HF.36,49,51 Two studies offered support group sessions for patients and families in the HBCR study arms.35,53
EFFECTS OF HBCR COMPARED WITH CBCR
The overall effectiveness of HBCR compared with CBCR is generally difficult to attribute to a single particular component, particularly in those studies that included bundled interventions comprising exercise training, dietary counseling, weight management, psychological support, and blood pressure and lipid management. Which components were most influential or how particular program or setting characteristics influenced patients and health outcomes is difficult to ascertain because of the diversity of patient characteristics, the length and intensity of programs, and the mechanisms of delivery. It has been reported that lifestyle changes that occur during CBCR can deteriorate when CBCR interventions are withdrawn.60 It is possible that the higher degree of self-monitoring/management and unsupervised exercise inherent in HBCR programs compared with CBCR may make the transition from active intervention to lifelong disease self-management more seamless, but this needs further investigation. In addition, the generalizability of findings from these studies is very limited for nonwhite ethnic minorities, individuals in lower socioeconomic groups, individuals who are uninsured or underinsured, older adults, and women because these groups were significantly underrepresented in the studies reviewed.
SAFETY
Given the fact that severe cardiovascular events are rare even in CBCR studies including a mix of lower- and higher-risk patients,61,62 studies of HBCR are currently underpowered to assess the risk of severe cardiovascular events, particularly in higher-risk patients. Given that limitation, the safety assessments were similar in the studies we reviewed of HBCR versus CBCR, at least in the low- to moderate-risk patients included in most studies. An emphasis on safety was mostly apparent in earlier studies,38 studies involving higher-intensity training,42 and those that enrolled older patients.53 Furthermore, the challenge of typical clinical concerns (eg, monitoring glucose levels in diabetes mellitus, hemodynamic changes, falls, impaired cognition, anxiety) was not mentioned in the studies we reviewed. In a time when patients with CVD are more likely to be older and frail, to have more comorbidities, and to be at greater cardiovascular risk, assumptions about the clinical safety and efficacy of HBCR for these patients merit greater scrutiny.
MORTALITY
Several studies reported all-cause mortality data for up to 12 months after the intervention and revealed no statistically significant differences between CBCR and HBCR.38,40,43,44,48,49,56,58 However, a 12-month follow-up may be too short to show a significant impact on mortality, and the relatively small sample sizes of the studies limited their power to detect a true difference in outcomes. Moreover, the lower-risk status of patients enrolled in most studies further weakens the statistical power to detect true differences between the groups. It is difficult to ascertain from published studies whether there are trends over time in the comparative effectiveness of HBCR and CBCR, especially taking into consideration temporal trends in secondary prevention efforts in clinical practice (usual care) settings. Among the studies that examined morbidity data beyond 1 year, Smith and colleagues63 reported no significant between-group differences in clinical events at the 6-year follow-up. A total of 46 of 74 patients participating in CBCR (62%) experienced a rehospitalization during the follow-up period compared with 35 of 70 patients participating in 53 HBCR(50%),and the median time to first rehospitalization was similar for both groups (4.49 years). However, the total number of rehospitalizations was higher in patients participating in CBCR (n=79) compared with patients participating in HBCR (n=42). Two studies reported no difference in revascularization or recurrent MI events between HBCR and CBCR programs.41,56
EXERCISE CAPACITY
Most studies comparing outcomes in individuals participating in HBCR and CBCR reported data on exercise capacity, including gas exchange in most cases.35–39,41–50,52–56,63–68 The majority of these studies reported data on changes in peak oxygen uptake among these clinical trial participan ts.35,37,42–49,52,54,63–66,68,69 In almost all of these studies, the improvement in peak oxygen uptake observed in those individuals assigned to HBCR was similar to that in patients assigned to CBCR. These data are limited by an overall low completion rate and by the fact that many participants did not undergo follow-up cardiopulmonary exercise testing on completion of the intervention. However, in at least 20 of the studies we reviewed, the effect of HBCR on improvements in exercise capacity (ie, peak oxygen uptake) appears to be similar to that observed from CBCR.
In addition to using peak oxygen uptake to assess exercise capacity, some studies have examined other measures of exercise capacity. Improvement in the distance achieved on an incremental shuttle walk test was evaluated in 2 studies and was similar in those HBCR participants and CBCR participants.36,41,55 The improvement in distance achieved on a 6-minute walk test was analyzed in 2 studies and was found to be similar in those participating in HBCR and patients participating in CBCR.45,48 Improvements in the peak metabolic equivalent tasks achieved on an exercise test,38,56,70 peak exercise duration,44 and work capacity on a cycle ergometer53 were also similar in those assigned to HBCR and those assigned to CBCR. In general,50 the magnitude of improvement in exercise capacity across all studies appeared to be similar in HBCR and CBCR settings.
MODIFIABLE RISK FACTORS
Multiple studies have examined the differential effect that HBCR and CBCR have on participant weight, blood pressure, lipid values, and tobacco use. Collectively, changes in these modifiable risk factors were similar in HBCR and CBCR among participants selected for these clinical trials. Outcomes for weight were specifically reported in 5 of these studies,37,46,48,51,63 and in all 5 studies, there was no difference in the change in weight between the HBCR and CBCR participants. Similarly, blood pressure changes were specifically reported in 8 of these studies.35,37,41,48,50,51,56,70 Most of these studies reported a similar effect on blood pressure in HBCR and CBCR participants. The effects on lipids were reported in 7 of these clinical trials.35,37,41,43,48,59,51 Although there were some isolated differences in the response of individual lipid parameters in HBCR versus CBCR, the remainder of the studies reported similar changes between HBCR and CBCR.35,37,41,43,48 Several studies found no difference in tobacco use/smoking behaviors between CBCR and HBCR interventions.37,40,48,56
HEALTH-RELATED QUALITY OF LIFE
Our review included 10 studies comparing the impact of HBCR and CBCR on HRQOL from a previous Cochrane review26 and 3 other studies that have been published since that review (Supplemental Table 3). Collectively, the 13 studies measured HRQOL using generic measures (EuroQol-5D, EuroQol-5D Index, Nottingham Health Profile, Short Form-36, and Sickness Impact Profile) and 1 disease-specific instrument (MacNew). Although comparisons across studies are not possible given the use of different measurement instruments and different follow-up periods, most studies reported improvements in overall HRQOL scores or subscale scores from baseline to follow-up for both HBCR and CBCR. However, 2 studies using the EuroQol-5D showed no changes in either HBCR or CBCR.41,56
WITHDRAWALS AND ADHERENCE
An important potential benefit of HBCR is that its flexibility may help improve the low levels of CR participation and adherence that have been reported in many CBCR studies. In general, the studies included in our review report that patient adherence strategies for HBCR appear to be comparable to those observed in CBCR. A recent Cochrane review by Taylor et al27 was not able to pool adherence data results because of substantial variation in the way that adherence was reported. However, 7 of the studies in that report, and in the studies that we reviewed, found no evidence of a significant difference in the level of adherence between HBCR and CBCR. Three other studies showed a higher level of adherence with HBCR than with CBCR. In addition, the rate with which patients attended all prescribed CR sessions (ie, completion or graduation rates) was slightly higher among the HBCR participants compared with CBCR participants (relative risk, 1.04 [95% CI, 1.01–1.05]; P= 0.009). Longer-term adherence after the initial phase of HBCR or CBCR, a critically important issue, was not reported in any of the studies reviewed. In addition, it is unclear how much the use of HBCR might improve the CR participation gap that currently exists. A recent study from the Veterans Health Administration found that patients offered referral to HBCR or facility-based CR were 4 times more likely to participate than those offered referral to facility-based programs alone,22,71 and a study from Kaiser Permanente in Colorado found that 41% of eligible patients participated in their HBCR program.72 However, another study from Toronto, ON, Canada, reported that only 10% of eligible patients receiving CR elected to participate in HBCR, despite it being covered by the local insurance provider.73
HBCR SESSIONS AND DOSE
Although the typical full dose of early outpatient (phase 2) CBCR in the United States is generally accepted as 36 sessions 60 to 90 minutes in length over a period of 12 to 36 weeks, the ideal dose of HBCR early after a qualifying event is not well defined. The typical HBCR intervention dose in the studies reviewed for this statement included 3 to 5 sessions of exercise training per week over a period of 8 to 12 weeks. Additional sessions of HBCR have included progressive exercise training, lifestyle counseling, and psychosocial counseling. The studies we reviewed did not include maintenance phases of HBCR longer than 36 weeks, although it is probable that the use of such longer-term options is likely to help improve longer-term adherence to the therapies initiated in the earlier postevent phase of HBCR.
COSTS AND HEALTHCARE USE
Costs were reported in 5 studies and in 1 study from the United States (Supplemental Table 4).35,41,53,55,56,60,74 Differences in the costs, currencies, and dates included in analyses limit the ability to directly compare these studies. Of the 2 studies reporting statistical comparisons of costs, 1 study found no significant difference in costs.70 Another found that HBCR cost £41 more than CBCR, but there was no significant difference in costs when patient travel costs were included.41 Of the 3 studies reporting statistical comparisons of the use of non-CR healthcare services (eg, medications, outpatient care, inpatient care), 2 reports found no significant difference in use between HBCR and CBCR,41,70 and 1 study reported fewer medical visits and hospitalizations with HBCR.53 Quality-adjusted life-years were reported in 2 studies, and both found no significant difference in quality-adjusted life-years between HBCR and CBCR.41,70 One study from the United States included limited cost data and suggested that costs may be lower for HBCR compared with CBCR.35
RISK OF BIAS
The risk of bias in many of the studies included in this review has previously been evaluated in an abridged Cochrane review.26,27 However, the studies reviewed generally lack sufficient detail to accurately assess their methodological quality and thus judge their risk of bias. Determining selection bias was difficult because most reports provided few details on random allocation sequence generation and concealment. Two studies revealed evidence of nonequivalence in baseline participant characteristics.36,46 Only 8 of 21 studies reported masking the study outcome assessments.36,40,41,46,47,52,53,56 Because protocol adherence was not addressed in the studies reviewed, it is impossible to determine the extent to which interventions were implemented with fidelity. Although most studies appeared to conduct intent-to-treat analyses, for many, this was difficult to ascertain without CONSORT diagrams. Several studies failed to conduct intention-to-treat analyses, a factor that would tend to result in overestimation of treatment effects.40,42,50–52 Reporting of loss to follow-up or dropouts was very diverse across studies according to intervention arm. Similarly, the dose (intensity, duration, and frequency) of the interventions for HBCR and for CBCR varied significantly in the studies reviewed, making precise interpretation of the results challenging. This is particularly difficult when interventions were individualized to patient needs or health status. There was evidence of crossover between interventions in 1 study47 and potential mixing of groups in another.54 The HBCR programs tended to use lower intensity and, in some cases, lower frequency of intervention compared with the CBCR programs. As noted in the Cochrane review of HBCR that included most of the articles we reviewed, low-quality reporting in the published studies makes it difficult to assess degree of bias, including publication bias (ie, that positive studies are more likely to be published than negative studies).
KEY FACTORS ASSOCIATED WITH SUCCESSFUL IMPLEMENTATION OF HBCR
Several delivery models for HBCR have been shown to address the challenges of implementing HBCR. Table 2 lists examples of specific implementation strategies shown to help improve CR participation. A frequently studied example for HBCR is the Heart Manual Program from the United Kingdom. Originally described in 1992, this 6-week self-management program includes health education, exercise training, and stress management, with telephone or in-person guidance from a trained facilitator.40 Another model that has been used in Canada involves 6 months of home-based exercise training with phone calls from a provider every 2 weeks to monitor progress, to assess adherence, to revise exercise prescription, and to provide support and education46 Costs of the home-based programs in the United Kingdom and Canada are covered by the national healthcare systems of each country. However, such programs are generally not covered by third-party payers in the United States. One exception is the MULTIFIT home-based program implemented at Kaiser Permanente Northern California.77 This nurse-based case management system starts during hospitalization for acute MI or revascularization and is followed over the subsequent 6 months by up to 12 nurse-initiated telephone contacts, up to 4 outpatient visits with a nurse case manager, and computer-generated progress reports based on patient questionnaires. Various hybrid approaches have also been tried.37,47,51 These typically include a combination of ≥1 facility-based sessions, usually focused on fitness assessment and exercise training, plus a number of home-based sessions, usually focused on the implementation of preventive therapies with the aid of patient education and motivational interviewing techniques.
Table 2.
Twelve Strategies to Facilitate Increased Referral to, Enrollment in, and Long-Term Participation in CR Programs
| 1. Achieve strong endorsement of outpatient CR by referring physicians and hospital administration by incorporating it into the hospital discharge plan |
| 2. Automatically refer all eligible patients to outpatient CR at the time of hospital discharge |
| 3. Use hospital-based liaisons to provide CR information and education to inpatients before discharge |
| 4. Develop a brief (5–10 min) promotional video about the value of outpatient CR that can be shown to all inpatients during hospital convalescence |
| 5. Provide patients with contact information for outpatient CR programs in close proximity to their home |
| 6. Schedule CR enrollment appointments via the patient’s preferred communication mode (telephone call, text message, email, or regular mail) |
| 7. Provide the option of an HBCR program at the time of hospital discharge for low- to moderate-risk patients |
| 8. Consider system-, provider-, and patient-level financial incentives for referral to, enrollment in, and completion of early outpatient exercise-based CR sessions |
| 9. Target specific patient subsets least likely to enroll in and complete CR (eg, racial/ethnic minorities, women, older adults, rural residents, and economically disadvantaged individuals) via a network of diversity liaisons |
| 10. Develop a series of integrated practice units, staffed by allied health professionals, that can provide counseling via in-person visits or through web-based and mobile applications, telephonic coaching, handheld computer technologies, or the internet |
| 11. Establish medication dosing and adherence as a quality assurance initiative in CR |
| 12. Offer serial assessments to track ongoing efforts for cardiovascular risk reduction, including physical activity/fitness |
CR indicates cardiac rehabilitation/secondary prevention programs; and HBCR, home-based cardiac rehabilitation.
PATIENT-LEVEL FACTORS
Patient motivation, self-efficacy, and engagement are the most important predictors of healthy long-term lifestyle changes and adherence to prescribed drug therapies. Howevr, the likelihood of success increases when counseling messages are tailored to an individual patient’s goals and readiness to make specific changes.78 The 6-stage Transtheoretical Stages of Change Model79 can be used to evaluate a patient’s stage of readiness to change a lifestyle habit before being counseled to change a specific behavior. For example, providing perception alteration or a critical analysis of the pros and cons of changing behavior may be required for the precontemplator and contemplator, respectively. Similarly, the preparation, action, maintenance, and relapse stages may be sequentially addressed by exploring alternative action plans, providing specific instructions (step-by-step guides), offering positive personal feedback, and halting recidivism. Although most people believe that a single behavior change is preferred at any given time, multiple simultaneous changes may be easier to adopt and sustain because they quickly yield perceptible benefits.80
Successful approaches to behavioral activation include the provider conveying understanding, acceptance, and interest in the patient as an individual; expressing empathy for unhealthy lifestyle practices; helping the patient understand and accept the need for change; identifying the patienťs stage of readiness to change; encouraging patients to hear themselves express why they want to change; and helping patients to identify, understand, and work through the barriers, challenges, and opportunities that influence their health-related behaviors (eg, job-related stressors, financial challenges).81 Additional steps involve helping patients overcome inertia and gain momentum with small serial successes over time, which should be viewed as an ally to successful lifestyle modification and a tool for dealing with inevitable recidivism.82,83 Clinicians should be aware of time-related challenges for patients and ensure the availability of convenient hours of operation for “real-time” (synchronous) HBCR, as well as for asynchronous HBCR. Technological advancements, including physical activity tracking, web-based and mobile applications, handheld computer technologies, the internet, and various wearable devices,84 may be helpful in this regard. Clinicians should also discuss other practical issues with patients who participate in HBCR, including their access to exercise equipment and facilities, availability of support systems (including family members and friends), and relevant comorbidities (eg, balance in older adults).
The core of effective counseling is a patient-centered approach in which providers work with their patients to create and implement an action plan to achieve their self-determined goals, resulting from questions carefully posed by the provider.85 The underlying power of this therapeutic approach, known as motivational interviewing, is that patients, with support from others, convince themselves to change behavior rather than rely exclusively on suggestions or advice from others.82,83,86 Specific strategies to circumvent or attenuate common CR barriers and to enhance patient referral, participation, and adherence to secondary prevention therapies, which clearly improve patient outcomes,87 are summarized in Table 2.24,75,88
PROVIDER-LEVEL FACTORS
The referring provider has 3 vital roles in the implementation of CR: referring eligible patients, encouraging patient participation, and communicating the importance of long-term lifestyle changes. CR is not intended to provide a short-term therapy but rather to help patients make essential lifestyle changes (eg, walking for 30 min/d) that will influence the long-term course of their disease. Greater emphasis on personal accountability on the part of the patient, adherence to prescribed cardioprotective medications, and ongoing engagement in health care reduce the potential for recidivism. Finally, the antedated mentality that CR is a time-limited intervention delivered in a supervised medical setting must be expanded to help empower patients to continue with their secondary prevention treatment plan in the longer term wherever they live, work, worship, or play.
SYSTEM-LEVEL FACTORS
Endorsement of HBCR and reimbursement at the health system level are by far the most critical factors influencing the success or failure of HBCR programs. Some countries, including the United Kingdom, Canada, and Australia, have national healthcare coverage policies that endorse and cover either CBCR or HBCR for patients with various cardiac conditions. In the United States, insurance carriers, including the Centers for Medicare & Medicaid Services, have coverage policies that endorse and cover up to 36 sessions of CBCR; however, coverage does not generally include HBCR except when it is provided as part of home health services for homebound patients (ie, those who are unable to leave home without considerable and taxing effort) who have a specific need that requires the skills of a licensed nurse or physical therapist.88a Although some patients who undergo coronary artery bypass graft surgery meet these requirements, many patients eligible for CR do not. Clearly, the lack of endorsement and reimbursement for HBCR is a major limiting factor to HBCR implementation in the United States.
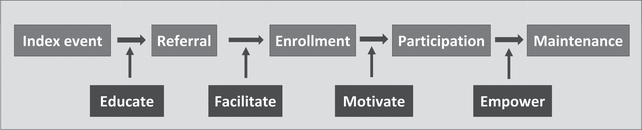
Specific strategies designed to circumvent or attenuate common barriers to referral, participation, and adherence are summarized in Figure 3.24,75,88
Figure 3.
Key opportunities to increase patient engagement in cardiac rehabilitation.
PRACTICAL CONSIDERATIONS
Roles and Competencies of Personnel
Traditional CBCR is implemented with the knowledge, skills, and certifications of a multidisciplinary team of healthcare professionals. In the studies reviewed, nurses and exercise physiologists supervised most HBCR programs. In this scenario, it is feasible to triage medical problems that arise to appropriate physicians, dietitians, pharmacists, psychologists, and related specialty programs (eg, smoking cessation clinics).
Durable Medical Equipment
Although exercise training can be achieved with activities that do not require specialized exercise equipment, home-based exercise equipment can be an important part of HBCR programs if available to patients. Such equipment includes treadmills, elliptical trainers, exercise pedalers, or stationary bicycles for aerobic training; pedometers or accelerometers for activity tracking; and resistance bands for strengthening. Heart rate monitors can help patients maintain fidelity to exercise prescriptions but often require out-of-pocket payments that are not feasible for many patients. Other items such as blood pressure monitors, bathroom scales, glucometers, and pill organizers can also be used as an important part of the patient’s follow-up care.
Patient Educational Materials
Numerous educational resources are available for patients enrolled in HBCR programs (Table 3). These materials should be used and adapted according to patient needs, health literacy, and learning abilities/limitations. Some examples are:
UK Heart Manual: Originally developed in 1992, the UK Heart Manual (NHS Lothian) is perhaps the most extensively studied self-management book for patients recovering from acute MI or coronary revascularization. It must be facilitated by specially trained healthcare professionals, who work with patients and their caregivers.89
American Heart Association/MULTIFIT: The American Heart Association has published a book and DVD titled An Active Partnership for the Health of Your Heart90 based on the MULTIFIT program that was originally developed as an intensive case management system by DeBusk et al.77 The book includes 12 chapters focused on relevant self-management skills and secondary prevention topics such as eating well, exercising, losing weight, reducing stress, quitting smoking, and taking medications.
Henry Ford Health System: The Henry Ford Health System has helped to pioneer a telemedicine-based HBCR program that is covered by both Blue Cross Blue Shield of Michigan and the Health Alliance Plan of Michigan for CR programs in Michigan that comply with statewide telemedicine statutes. A total of 28 educational audio-PDFs are freely available to patients and the public.91
University Health Network Toronto Rehabilitation Institute: The Cardiovascular Prevention and Rehabilitation Program at the University Health Network Toronto Rehabilitation Institute has published a comprehensive education workbook for secondary prevention in patients with CVD.92 It includes 22 chapters focused on secondary prevention topics and provides specific tools for helping patients with goal setting, exercise, healthy eating, and risk factor management.
National Heart Foundation of Australia/Australian Cardiac Rehabilitation Association: In 2015, the National Heart Foundation of Australia and Australian Cardiac Rehabilitation Association published a comprehensive book, My Heart, My Life, that includes extensive educational materials and tools for patients recovering from acute MI or coronary revascularization.93
Promising Practices in the Veterans Health Administration: The US Department of Veterans Affairs has developed home-based rehabilitation programs for qualified individuals.93a,94,95
Table 3.
Selected Electronic Patient Education Resources
| Website | Brief Description |
|---|---|
| https://www.cdc.gov/heartdisease | Written materials and podcasts for reliable health and safety information |
| https://www.heart.org | Educational materials for engaging patients with interactive tools |
| https://www.cardiosmart.org | Educational materials, risk calculators, and mobile applications for medication reminders |
| http://www.aacvpr.org | Educational resources for patients |
| https://mendedhearts.org | A support organization for cardiac patients |
| https://www.goredforwomen.org | Patient education in English and Spanish |
| https://womenheart.org | A support organization for women with heart disease |
| http://www.pcna.net | Downloadable patient education booklets; education also provided in Spanish |
| http://www.theheartmanual.com | UK Heart Manual |
| https://www.henryford.com/services/cardiology/cardiac-rehab/home-based-cardiac-rehabilitation | Patient education across a variety of cardiovascular disease–related topics using audio PDFs |
| https://www.cardiaccollege.ca | Patient education and a downloadable guide for living with cardiovascular disease |
| https://www.heartfoundation.org.au | My Heart, My Life |
CHALLENGES AND POTENTIAL SOLUTIONS IN HBCR
In theory, HBCR can help improve delivery of CR to eligible patients by overcoming common barriers that impede a patient’s participation in CBCR, including transportation challenges, competing time demands, and the lack of CBCR near a patient’s home. These and other barriers to CBCR have been described previously.23,24,96 However, challenges also exist that can limit patient participation in HBCR. Some of those challenges are unique to HBCR, and others are common to both HBCR and CBCR. This section summarizes several challenges for HBCR interventions that have been noted in the studies reviewed for this document and in other studies.
SAFETY
Challenges
One theoretical advantage of CBCR over HBCR is that CBCR provides participants with exercise training under in-person, continuous supervision by trained medical professionals. However, this emphasis on electrocardiographic monitoring may also have unintended consequences such as making patients concerned that exercise might be harmful or requires close supervision or suggesting that the need to exercise ends after completion of supervised CR. The studies we reviewed had low power to assess the safety of the HBCR interventions. Higher-risk patients were generally excluded, such as patients with HF and New York Heart Association functional class III to IV symptoms, a reduced ejection fraction (<40%), meaningful dysrhythmia, Canadian Cardiovascular Class 3 or higher angina pectoris, older age (eg, >75 years), a significant physical limitation, or a markedly reduced peak functional capacity (eg, <2 metabolic equivalent tasks).
Potential Solutions
Several studies have shown that with the use of appropriate screening and monitoring procedures in higher-risk patients, HBCR can be feasible and safe, including in patients with stable HF.36,45,49 A recent study by Dougherty et al97 specifically enrolled patients at risk for sudden cardiac arrest who were treated with an implantable cardioverter-defibrillator in a home-based walking program (compared with usual care) and showed that implantable cardioverter-defibrillator shocks were infrequent (exercise group, 4; usual care group, 8), with no statistically significant difference in frequency between the 2 study groups.
The HF-ACTION study is the largest study to assess the safety of exercise training provided initially in a CBCR but later outside a CBCR program. Patients with stable, chronic HF and New York Heart Association class II to IV symptoms (n= 2331) were enrolled. In this study, participants were prescribed 36 CBCR sessions followed by ≥9 months of HBCR. A heart rate monitor (chest/wrist heart rate monitor/watch and daily exercise records were used to guide and monitor exercise intensity at home. No significant difference was reported between the exercise and usual care groups for the overall rate of hospitalization (1.9% versus 3.2%, respectively) or death (0.4% versus 0.4%, respectively) during or within 3 hours after exercise.57 Furthermore, the investigators identified 1053 patients from the HF ACTION trial who had an implantable cardioverter-defibrillator at baseline and were randomized to the above exercise intervention versus control. Study participants had a median ejection fraction of 24% at baseline.98 During 2.2 years of follow-up, 20% of the 546 patients in the exercise group experienced a shock versus 22% of the 507 patients receiving usual care. Exercise training was not associated with the occurrence of implantable cardioverter-defibrillator shock (hazard ratio, 0.9 [95% CI, 0.7–1.2]).
Finally, indirect support for the safety of HBCR can be found in studies of CBCR (including both lower- and higher-risk patients) that have reported that serious CVD events occur rarely: ≈1 event per 50 000 patient-hours.62,99 A study by Pavy et al62 evaluated 25 420 patients undergoing CR at 65 different facilities. During 42 419 exercise stress tests and 743 471 patient-hours of exercise training, 20 severe cardiac events in 17 patients occurred. The event rate was 1 per 49 565 patient-hours of exercise training; the cardiac arrest rate was 1.3 per million patient-hours of exercise. No fatal complications or emergency defibrillations were reported.
COST/REIMBURSEMENT
Challenges
As pointed out earlier in this document, although CBCR services are reimbursed by third-party payers in the United States, HBCR is generally not covered. In addition, the increased use of HBCR compared with CBCR may not necessarily lead to cost savings for a healthcare organization because the costs to deliver CBCR and HBCR appear to be similar according to the available studies reviewed in this statement (Supplemental Table 4).
Potential Solutions
Although third-party payers and healthcare systems genrally do not provide reimbursement for HBCR, some do (ie, Kaiser Permanente of Northern California, Blue Cross Blue Shield of Michigan, Health Alliance Plan in Michigan, Veterans Affairs). Until the Centers for Medicare & Medicaid Services and other third-party payers find sufficient evidence to warrant adoption of policies that provide reimbursement for HBCR services, an alternative approach is to directly contract with employers or third-party payers to cover the costs of HBCR. One promising strategy that was initiated at the Henry Ford Hospital in Michigan is to provide HBCR in a manner that meets the state’s statutes for telemedicine, which then becomes a service covered by some third-party payers if correctly billed for such. A helpful reference that provides information about telemedicine policies in each state (and how they may or may not apply to HBCR coverage) can be found online.100 Another option to cover the costs of HBCR is to bill patients directly for HBCR services, but this option is likely to limit the acceptance and use of HBCR unless the costs to deliver HBCR are greatly reduced.
PARTICIPATION AND ADHERENCE
Challenges
Just as with CBCR, patient participation can be a significant challenge in HBCR. Some individuals may lack motivation for or interest in participating in HBCR, whereas others do not understand its importance or benefits. As with CBCR, it can be a challenge to help patients understand that the principles and strategies of HBCR are helpful in optimizing cardiovascular health in the shorter and longer term.
Potential Solutions
One potential advantage of HBCR compared with CBCR is that HBCR offers more convenience and flexibility for patients, which should help improve participation and adherence rates compared with CBCR. However, as noted previously, participation and adherence rates in HBCR, reported in a relatively small number of studies included in this review, were similar or only slightly better for HBCR compared with CBCR. In real clinical practice, adherence to home-based programs could be even higher if patients actually choose (versus being randomly assigned to) this model of care. Access to a health coach for HBCR participants has the potential to be a cost-effective strategy for sustaining adherence to the health behavior changes required for shorter- and longer-term cardiovascular benefits.101 Finally, evidence-based strategies that improve participation in CBCR (ie, systematic referral and enrollment strategies, participation incentives)76 are also likely to be successful in improving participation in HBCR.
EFFECTIVE COMMUNICATION, COUNSELING, SOCIAL SUPPORT, AND EDUCATION
Challenges
Communication, counseling, and education involving CR staff and patients are vitally important during the course of any CR program. In CBCR settings, such activities are typically delivered in face-to-face encounters. For HBCR settings, such communications are typically carried out by telephone, text messaging, synchronized video conferencing, or internet-based strategies. One study of cognitive behavioral therapy in patients with depression found that telephone-based counseling resulted in lower attrition rates and similar improvements in depression after 18 weeks of therapy compared with face-to-face counseling.102 However, at 6 months, patients who received face-to-face counseling were more likely to maintain their improvements than those in the telephone-based group. Social support and group-based dynamics that promote positive social support to participants are important components of CBCR but potentially may be challenging to establish in the HBCR setting.
Potential Solutions
The studies we reviewed reported similar lifestyle change effectiveness for the HBCR methods and CBCR methods used in the studies. Other studies support the efficacy of telephone- or internet-based lifestyle counseling, education, and group-based social support when evidence-based behavioral change techniques are used.103–105 Access to a health coach for HBCR participants has potential to improve communication, social support, and education, which can help sustain adherence to the health behavior changes required for cardiovascular health.101
STANDARDIZATION OF INTERVENTIONS
Challenges
Guidelines and standards of care have been well defined for CBCR, including core components,32 core competencies,106 clinical practice guidelines,107 performance measures,108,109 and certification (program and individual).110 However, such guidelines and standards have not been established specifically for HBCR. Although evidence-based treatment strategies can and should be personalized according to patient needs and preferences, standards of practice are still important for defining appropriate parameters of care. A lack of such guidance could potentially lead to inappropriate variation in the quality and impact of HBCR interventions. Furthermore, as noted, the dose of HBCR interventions varied in the studies we reviewed, making it difficult to identify a precise dose of therapy or intensity of prescribed exercise that should be recommended to patients. Finally, identifying guidelines and standards for longer-term maintenance of HBCR services is challenging given the limited data on the longer-term maintenance in the studies we reviewed.
Potential Solutions
The principles and protocols used in many of the HBCR studies we reviewed are similar to those used in CBCR studies, suggesting that the standards and guidelines for CBCR can generally be applied to HBCR. For example, in HBCR studies, the duration and frequency of exercise training are typically titrated upward, to ≥30 minutes and 3 to 5 sessions per week, respectively. Although any amount of physical activity will help a previously sedentary patient improve his or her clinical outcomes, national guidelines recommend at least 150 minutes of moderate (eg, walking) or 75 minutes of vigorous (eg, running) physical activity (≈500 metabolic equivalent-minutes) per week.111 Exercise intensity has been most often guided by heart rate response, set between 60% and 80% of achieved peak heart rate or at resting heart rate plus 60% to 80% of heart rate reserve (peak minus rest), with adjustment based on ratings of perceived exertion set between “somewhat hard” and “hard” (12–14 on the Borg Rating of Perceived Exertion scale112). Two HBCR studies42,43 involved high-intensity interval training, with exercise intensity set to as high as 95% of achieved peak heart rate. Furthermore, electronic tools, including text messaging, smartphone applications, and wearable sensors, can potentially help produce “mass customization” (ie, largescale standardization and personalization) of HBCR, helping patients to follow personalized recommendations for exercise training, dietary therapy, behavioral activation, stress management, and medication adherence. The length of the initial postevent phase of HBCR therapy, according to published studies of HBCR, can be up to 12 weeks, but longer-term adherence strategies of known effectiveness should also be studied in future studies of HBCR (and for studies of CBCR).
IMPACT ON CLINICAL EVENTS
Challenges
Although the impact on clinical CVD events has been reported for CBCR in both the shorter term (immediately after the intervention) and longer term (follow-up after the intervention), studies that address the impact of HBCR on longer-term clinical events are lacking.
Potential Solutions
Although it might be reasonable to assume that HBCR interventions, if successful in applying secondary preventive therapies of known efficacy, would result in longer-term improvements in clinical outcomes, further studies on the longer-term impact of HBCR on clinical outcomes are needed.
CONSIDERATIONS FOR QUALITY METRICS FOR HBCR
Although it is not the purpose of this document to propose quality metrics for HBCR, a brief review of quality metrics mentioned in the HBCR studies reviewed for this document may serve as a helpful guide. First, a primary emphasis of HBCR interventions has been to optimize participation (Figure 3). Although HBCR is not suggested to be a substitute for CBCR, it may represent a positive alternative strategy that targets secondary prevention and improved health outcomes for those who are not able to participate in CBCR. Second, we believe that it is important to separate the core components of HBCR (physical activity, healthy eating, medication adherence, smoking cessation, and stress management) from the clinical outcomes that these behavioral changes can achieve (changes in blood pressure, exercise capacity, body weight, lipid levels, and depressive symptoms; Figure 2).
Quality metrics to be considered for HBCR could include the following:
HBCR referral, enrollment, participation, and maintenance
Health behaviors: physical activity, dietary habits, stress management, medication adherence, and tobacco use
Cardiovascular risk factors: exercise capacity, blood pressure, lipid levels, glycemic control, tobacco use, and body weight/composition
Functional capacity, quality of life, and anxiety/depressive symptoms
Secondary prevention: readmission to hospital, recurrent cardiovascular events, and mortality rates
TECHNOLOGY TOOLS AND HBCR
Technology-facilitated HBCR has the potential to expand the reach of CR, to promote patient engagement, and to enable patient-provider communication. Many technology tools can play a role in the delivery of HBCR, including websites, mobile phone applications, text messaging, and sensors for physical activity, heart rate, ECG, and other health measures.113 Three studies directly included in this review prominently included technology use in their interventions.39,49,51 The devices included wearable heart rate monitors; a mobile telemonitoring system that recorded ECGs and transmitted data via a mobile phone; and smartphone applications, website tools, and text messaging communications. In each case, adherence, exercise capacity, and HRQOL with HBCR was equal to or better than with CBCR.
Other studies included in this review reported more limited information about the use of technology in HBCR interventions, including heart rate monitors, ambulatory electrocardiographic monitoring, and transtelephonic electrocardiographic monitoring. Although most studies did not report technical details, 2 studies reported that no arrhythmia or ischemia events were noted.35,38,42,53,55 All of these interventions included both technology and provider-facilitated HBCR, and many interventions reported additional features beyond the technology itself such as training on the use of the technology and the use of technology as a tool for patient-provider communication. However, these studies were unable to draw conclusions about the long-term impact on important patient-centered outcomes, including cardiovascular events. Additionally, because none of these studies directly compared HBCR with technology tools and HBCR without technology tools, we cannot conclude whether the effects of the interventions were the result of the delivery of HBCR or the inclusion of technology in the interventions.
Technology tools incorporated into HBCR delivery models have the potential to expand the reach of CR by improving uptake and adherence compared with CBCR approaches. More research is needed to assess whether technology-aided HBCR has a lasting favorable impact on program enrollment, adherence, and outcomes.
AREAS FOR FUTURE WORK
SPECIFIC POPULATION GROUPS
Although much work has been accomplished in HBCR, a number of key questions remain that will guide future research in this important area. Specifically, most published studies on HBCR have not included sufficient numbers of women to draw conclusions about the effects of HBCR in women or about specific sex differences in response to HBCR. Similarly, little is known about the efficacy of HBCR among those of diverse races and ethnicities because these participants have been underrepresented in existing studies. Furthermore, we identified no studies that explored the use of HBCR in patients with lower socioeconomic status, for whom HBCR may reduce important financial and logistical barriers to CR and provide significant benefits. Finally, studies are needed that assess the impact of HBCR in diverse age groups, especially in older adults, who often have unique needs and more numerous and daunting barriers to participation in any intervention, including HBCR. Therefore, more studies are needed that include more women, diverse racial/ethnic groups, socioeconomically disadvantaged groups, and diverse age groups to determine whether HBCR-type programs are generalizable to more diverse populations.
HIGHER-RISK POPULATIONS
Studies on HBCR reviewed in this document were derived predominantly from study populations that were carefully selected for low to moderate risk, high motivation, or sufficient ability to use telehealth devices and supports. The future of HBCR requires that the utility of HBCR be better established for a wider spectrum of eligible patients, including those who have more complicated conditions (eg, older adults; those with multiple morbidities; obese individuals; those who are cognitively challenged, frail, or socioeconomically challenged; ethnic minorities; rural residents; those with peripheral arterial disease) in whom HBCR may not achieve similar levels of safety or efficacy. Basic concepts of CR frequency, formatting, education, training intensity, and behavior modification techniques must be honed for home-based care that meets the varying needs (and limitations) of these patients.
HYBRID MODELS OF CR
Although most studies to date have compared CBCR and HBCR, few have assessed a model that is perhaps more compelling: a hybrid model in which patients participate in a mixture of CBCR and HBCR activities.113a In theory, such a model could help strengthen the impact of CR services by offering the best of both worlds to eligible patients. As the search continues for CR services of the highest value (ie, with high-quality outcomes per unit cost), hybrid models of CR may be more attractive than traditional CBCR models. Some centers have implemented and promoted such hybrid models,114,115 but additional research is needed to assess cardiovascular and other outcomes in both simple and hybrid versions of HBCR compared with traditional CBCR.
Other important areas for future research investigation include the analysis and integration of technology applications and their impact on patient participation and compliance in the setting of HBCR, as well as a comparison of patient satisfaction with and adherence to HBCR versus CBCR models.
STAFFING AND PROGRAMMING NEEDS
Critical issues of format (eg, staffing ratios, program personnel, intervention frequency and intensity), cost-efficiency, safety, supervision, and outcome metrics for home-based programs must be standardized for home-based models with subsequent uniform implementation.
CLINICAL OUTCOMES
Additional research is needed to assess the impact of HBCR on clinical and behavioral outcomes in both the shorter and longer term (eg, beyond 12 months). Such data, tested in patients receiving contemporary drug therapies or coronary interventions, are critically important if HBCR is to achieve the same status as CBCR as a Class I indication in clinical practice guidelines for patients with CVD and if HBCR is to be considered an evidence-based alternative or addition to CBCR.
EXERCISE EQUIPMENT AND TRAINING MODALITIES
Additional research is needed to assess whether the use of a simplified HBCR program (eg, one that is tailored to a patient’s needs, limitations, and living environment, incorporating activities such as brisk walking or jogging for cardiovascular exercise and calisthenics or elastic bands for strength training) produces exercise-related improvements in participants that are similar to those seen with a more comprehensive HBCR program that provides specialized exercise equipment such as that typically provided in a CBCR program or that could be provided to patients as part of an HBCR program (eg, an elliptical trainer, exercise bicycle, or similar equipment for cardiovascular exercise training; elastic bands or hand or machine weights for strength training). Furthermore, additional research is needed to assess the safety and impact of high-intensity interval training in a home-based setting for various patient subgroups.
CONCLUSIONS AND SUGGESTIONS FOR CLINICALS, HEALTHCARE ORGANIZATIONS, THIRD-PARTY PAYERS, AND POLICYMAKERS
With a growing realization that CR services are both life-saving and underused, there is a stark need to find new methods to augment the delivery of CR services to the >80% of eligible patients who do not participate in traditional programs. The focus of this scientific statement, HBCR, may provide such a method. The decades-old science behind CBCR is sizable and convincing but limited by patient-, provider-, and system-based barriers to participation. Although the science behind HBCR is relatively new and less developed, its findings are generally consistent with those reported for CBCR.
Available evidence suggests that HBCR may provide an alternative option for CR services for stable low- to moderate-risk patients with CVD who lack available CBCR services. Shorter-term improvements in functional capacity, HRQOL, and CVD risk factor control are similar in HBCR and CBCR, and longer-term studies on the impact of HBCR on clinical events are still lacking. Adherence to CR therapy appears to be better in HBCR compared with CBCR, a result of the greater flexibility and convenience for patients who use HBCR services. However, a lack of reimbursement by most third-party payers represents a challenge to HBCR implementation. Additional safety data are needed for HBCR, particularly in higher-risk groups.
The core components of HBCR are similar to those that have been recommended for CBCR: patient assessment, exercise training, dietary counseling, and risk factor control (eg, lipid abnormalities, hypertension, obesity, diabetes mellitus) through optimal adherence to medication, behavioral activation (eg, smoking cessation, healthy eating habits, physical activity), and psychosocial interventions. The primary difference between HBCR and CBCR is that CBCR programs require direct face-to-face observation of patients, whereas HBCR programs do not.
Evidence-based standards and guidelines for practice for CBCR have been widely disseminated and can be readily adapted to HBCR on the basis of results from the HBCR studies cited in this statement. Quality metrics for HBCR, when developed, should focus on key structure, process, and outcome metrics.
Technology tools are advancing at a rapid pace and will help improve communication between patients and providrs, improve the efficiency of patient monitoring for safety and effectiveness, and expand the reach of CR professionals beyond the typical reach of CBCR services and into a more home-based setting.
Further study is recommended to assess the impact of HBCR services in more diverse and higher-risk groups of patients and to assess the impact of hybrid models of CR, including components from both CBCR and HBCR. Such information will help inform reimbursement policies from third-party insurance providers, a critically important step in the implementation of HBCR services.
Suggestions for healthcare providers include the following:
Given the large body of evidence showing its benefits, CBCR should be recommended to all patients eligible for CR.
To potentially reduce the gap in CR participation that exists today, HBCR may be an alternative option to recommend for selected clinically stable low- to moderate-risk patients who cannot attend CBCR.
HBCR services should be designed and tested using effective processes of care for CVD secondary prevention.
- Healthcare organizations must develop and support the following:
- Efforts to maximize CR referral and entry through systematic approaches such as automatic referral systems and patient liaisons.
- High-quality programs of CBCR and HBCR that optimize delivery of CR services to their patients by using evidence-based standards and guidelines, strategies to maximize patient adherence in both the shorter and longer term, and outcome tracking methods that help promote continuous quality improvement.
- Testing and implementation of evidence-based hybrid approaches to CR that combine the positive and complementary aspects of both CBCR and HBCR to personalize and optimize CR services for each patient and to promote long-term adherence and favorable behavioral change.
CR professionals must work with other healthcare professionals and policymakers to implement additional research and demonstration projects to expand the evidence base for HBCR and to inform HBCR-related policy decisions.
Supplementary Material
Writing Group Disclosures
| Writing Group Member | Employment | Research Grant | Other Research Support | Speakers’ Bureau/Honoraria | Expert Witness | Ownership Interest | Consultant/Advisory Board | Other |
|---|---|---|---|---|---|---|---|---|
| Randal J. Thomas | Mayo Clinic | None | None | None | None | None | None | None |
| Mary A. Whooley | University of California, San Francisco Department of Medical Affairs Medical Center | Patient-Centered Outcomes Research Institute*; Veterans Health Administration Quality Enhancement Research Initiative* | None | None | None | None | None | None |
| Alexis L. Beatty | VA Puget Sound Health Care System, University of Washington | Alpha Phi Foundation†; John L. Locke Jr. Charitable Trust†; Seattle Institute for Biomedical and Clinical Research†; Veterans Affairs Health Services Research and Development†; (all research grants related to cardiac rehabilitation) | None | None | None | None | None | Veterans Affairs Health Services Research and Development Career Development Award (principal investigator)† |
| Theresa M. Beckie | University of South Florida | None | None | None | None | None | None | None |
| LaPrincess C. Brewer | Mayo Clinic College of Medicine | None | None | None | None | None | None | None |
| Todd M. Brown | University of Alabama at Birmingham | None | None | None | None | None | None | None |
| Daniel E. Forman | University of Pittsburgh Medical Center | None | None | None | None | None | None | None |
| Barry A. Franklin | William Beaumont Hospital | None | None | None | None | None | None | None |
| Steven J. Keteyian | Henry Ford Hospital | None | None | None | None | Nimble Heart, Inc* | None | None |
| Dalane W. Kitzman | Wake Forest University School of Medicine | NIH (funded clinical study)† | None | None | None | None | None | None |
| Judith G. Regensteiner | University of Colorado Denver School of Medicine Center for Women’s Health Research | None | None | None | None | None | None | None |
| Bonnie K. Sanderson | Auburn University | None | None | None | None | None | None | None |
This table represents the relationships of writing group members that may be perceived as actual or reasonably perceived conflicts of interest as reported on the Disclosure Questionnaire, which all members of the writing group are required to complete and submit. A relationship is considered to be “significant” if (a) the person receives $10 000 or more during any 12-month period, or 5% or more of the person’s gross income; or (b) the person owns 5% or more of the voting stock or share of the entity, or owns $10 000 or more of the fair market value of the entity. A relationship is considered to be “modest” if it is less than “significant” under the preceding definition.
Modest.
Significant.
Reviewer Disclosures
| Reviewer | Employment | Research Grant | Other Research Support | Speakers’ Bureau/Honoraria | Expert Witness | Ownership Interest | Consultant/Advisory Board | Other |
|---|---|---|---|---|---|---|---|---|
| Gary J. Balady | Boston Medical Center | None | None | None | None | None | None | None |
| Vera A. Bittner | University of Alabama at Birmingham | None | None | None | None | None | None | None |
| Richard Josephson | University Hospitals of Cleveland, Case Western Reserve University | None | None | None | None | None | None | None |
| Paul I. Oh | Toronto Rehabilitation Institute/University Health Network (Canada) | None | None | None | None | None | None | None |
| Quinn R. Pack | Baystate Medical Center | NHLBI (K23 from the NIH to study the role of the hospital in improving cardiac rehabilitation use. All money goes directly to my institution and is paid to me only through regular salary rather than commission or otherwise)* | None | None | None | None | None | None |
| Nanette K. Wenger | Emory University | None | None | None | None | None | None | None |
This table represents the relationships of reviewers that may be perceived as actual or reasonably perceived conflicts of interest as reported on the Disclosure Questionnaire, which all reviewers are required to complete and submit. A relationship is considered to be “significant” if (a) the person receives $10 000 or more during any 12-month period, or 5% or more of the person’s gross income; or (b) the person owns 5% or more of the voting stock or share of the entity, or owns $10 000 or more of the fair market value of the entity. A relationship is considered to be “modest” if it is less than “significant” under the preceding definition.
Modest.
Footnotes
ARTICLE INFORMATION
The American Heart Association, the American Association of Cardiovascular and Pulmonary Rehabilitation, and the American College of Cardiology make every effort to avoid any actual or potential conflicts of interest that may arise as a result of an outside relationship or a personal, professional, or business interest of a member of the writing panel. Specifically, all members of the writing group are required to complete and submit a Disclosure Questionnaire showing all such relationships that might be perceived as real or potential conflicts of interest.
REFERENCES
- 1.Dalal HM, Doherty P, Taylor RS. Cardiac rehabilitation. BMJ. 2015;351:h5000 10.1136/bmj.h5000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wenger NK. Current status of cardiac rehabilitation. J Am Coll Cardiol. 2008;51:1619–1631. 10.1016/j.jacc.2008.01.030 [DOI] [PubMed] [Google Scholar]
- 3.Drozda J Jr, Messer JV, Spertus J, Abramowitz B, Alexander K, Beam CT, Bonow RO, Burkiewicz JS, Crouch M, Goff DC Jr, Hellman R, James T 3rd, King ML, Machado EA Jr, Ortiz E, O’Toole M, Persell SD, Pines JM, Rybicki FJ, Sadwin LB, Sikkema JD, Smith PK, Torcson PJ, Wong JB. ACCF/AHA/AMA-PCPI 2011 performance measures for adults with coronary artery disease and hypertension: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures and the American Medical Association–Physician Consortium for Performance Improvement [published correction appears in Circulation. 2011;124:e39]. Circulation. 2011;124:248–270. 10.1161/CIR.0b013e31821d9ef2 [DOI] [PubMed] [Google Scholar]
- 4.Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr, Chavey WE 2nd, Fesmire FM, Hochman JS, Levin TN, Lincoff AM, Peterson ED, Theroux P, Wenger NK, Wright RS. 2012 ACCF/AHA focused update incorporated into the ACCF/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines [published correction appears in Circulation. 2013;127:e863–e864]. Circulation. 2013;127:e663–e828. 10.1161/CIR.0b013e31828478ac [DOI] [PubMed] [Google Scholar]
- 5.O’Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines [published correction appears in Circulation. 2013;128:e481]. Circulation. 2013;127:e362–e425. 10.1161/CIR.0b013e3182742cf6 [DOI] [PubMed] [Google Scholar]
- 6.Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Nallamothu BK, Ting HH. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions [published correction appears in Circulation. 2012;125:e412]. Circulation. 2011;124:e574–e651. 10.1161/CIR.0b013e31823ba622 [DOI] [PubMed] [Google Scholar]
- 7.Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, Cigarroa JE, Disesa VJ, Hiratzka LF, Hutter AM Jr, Jessen ME, Keeley EC, Lahey SJ, Lange RA, London MJ, Mack MJ, Patel MR, Puskas JD, Sabik JF, Selnes O, Shahian DM, Trost JC, Winniford MD. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;124:e652–e735.: 10.1161/CIR.0b013e31823c074e [DOI] [PubMed] [Google Scholar]
- 8.Smith SC Jr, Allen J, Blair SN, Bonow RO, Brass LM, Fonarow GC, Grundy SM, Hiratzka L, Jones D, Krumholz HM, Mosca L, Pasternak RC, Pearson T, Pfeffer MA, Taubert KA. AHA/ACC guideline sfo rsecondary preventio nfo rpatient swit hcoronary and other atherosclerotic vascular disease: 2006 update [published correction appears in Circulation. 2006;113:e847]. Circulation. 2006;113:2363–2372. 10.1161/CIRCULATIONAHA.106.174516 [DOI] [PubMed] [Google Scholar]
- 9.Gerhard-Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, Drachman DE, Fleisher LA, Fowkes FG, Hamburg NM, Kinlay S, Lookstein R, Misra S, Mureebe L, Olin J, Patel RA, Regensteiner JG, Schanzer A, Shishehbor MH, Stewart KJ, Treat-Jacobson D, Walsh ME. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published correction appears in Circulation. 2017;135:e790]. Circulation. 2017;135:e686–e725. 10.1161/CIR.0000000000000470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Butchart EG, Gohlke-Bärwolf C, Antunes MJ, Tornos P, De Caterina R, Cormier B, Prendergast B, Iung B, Bjornstad H, Leport C, Hall R, Vahanian A; Working Groups on Valvular Heart Disease, Thrombosis, and Cardiac Rehabilitation and Exercise Physiology, European Society of Cardiology. Recommendations for the management of patients after heart valve surgery. Eur Heart J. 2005;26:2463–2471. 10.1093/eurheartj/ehi426 [DOI] [PubMed] [Google Scholar]
- 11.Nytrøen K, Gullestad L. Effect of exercise in heart transplant recipients. Am J Transplant. 2013;13:527 10.1111/ajt.12046 [DOI] [PubMed] [Google Scholar]
- 12.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;128:1810–1852. 10.1161/CIR.0b013e31829e8807 [DOI] [PubMed] [Google Scholar]
- 13.ACTION Registry-GWTG: defect free care for acute myocardial infarction: specification and testing overview. http://www.ncdr.com/WebNCDR/docs/default-source/ncdr-general-documents/defect-free-care-10_4_13.pdf?sfvrsn=2 Accessed April 24, 2017.
- 14.Consensus core set: cardiovascular measures, version 1.0. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-As-sessment-Instruments/QualityMeasures/Downloads/Cardiovas-cular-Measures.pdf Accessed April 24, 2017.
- 15.Anderson L, Oldridge N, Thompson DR, Zwisler AD, Rees K, Martin N, Taylor RS. Exercise-based cardiac rehabilitation for coronary heart disease: Cochrane Systematic Review and Meta-Analysis. J Am Coll Cardiol. 2016;67:1–12. 10.1016/j.jacc.2015.10.044 [DOI] [PubMed] [Google Scholar]
- 16.Dunlay SM, Pack QR, Thomas RJ, Killian JM, Roger VL. Participation in cardiac rehabilitation, readmissions, and death after acute myocardial infarction. Am J Med. 2014;127:538–546. 10.1016/j.amjmed.2014.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shah ND, Dunlay SM, Ting HH, Montori VM, Thomas RJ, Wagie AE, Roger VL. Long-term medication adherence after myocardial infarction: experience of a community. Am J Med. 2009;122:961.e7–961.e13. 10.1016/j.amjmed.2008.12.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, Stason WB. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116:1653–1662. 10.1161/CIRCULATIONAHA.107.701466 [DOI] [PubMed] [Google Scholar]
- 19.Zeng W, Stason WB, Fournier S, Razavi M, Ritter G, Strickler GK, Bhalotra SM, Shepard DS. Benefits and costs of intensive lifestyle modification programs for symptomatic coronary disease in Medicare beneficiaries. Am Heart J. 2013;165:785–792. 10.1016/j.ahj.2013.01.018 [DOI] [PubMed] [Google Scholar]
- 20.Lawler PR, Filion KB, Eisenberg MJ. Efficacy of exercise-based cardiac rehabilitation post-myocardial infarction: a systematic review and meta-analysis of randomized controlled trials. Am Heart J. 2011;162:571–584.e2. 10.1016/j.ahj.2011.07.017 [DOI] [PubMed] [Google Scholar]
- 21.Taylor RS, Sagar VA, Davies EJ, Briscoe S, Coats AJ, Dalal H, Lough F, Rees K, Singh S. Exercise-based rehabilitation for heart failure. Cochrane Database Syst Rev. 2014:CD003331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beatty AL, Truong M, Schopfer DW, Shen H, Bachmann JM, Whooley MA. Geographic variation in cardiac rehabilitation participation in Medicare and Veterans Affairs populations: opportunity for improvement. Circulation. 2018;137:1899–1908. 10.1161/CIRCULATIONAHA.117.029471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arena R, Williams M, Forman DE, Cahalin LP, Coke L, Myers J, Hamm L, Kris-Etherton P, Humphrey R, Bittner V, Lavie CJ; on behalf of the American Heart Association Exercise, Cardiac Rehabilitation and Prevention Committee of the Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Council on Nutrition, Physical Activity and Metabolism. Increasing referral and participation rates to outpatient cardiac rehabilitation: the valuable role of healthcare professionals in the inpatient and home health settings: a science advisory from the American Heart Association. Circulation. 2012;125:1321–1329.. 10.1161/CIR.0b013e318246b1e5 [DOI] [PubMed] [Google Scholar]
- 24.Balady GJ, Ades PA, Bittner VA, Franklin BA, Gordon NF, Thomas RJ, Tomaselli GF, Yancy CW. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation. 2011;124:2951–2960.. 10.1161/CIR.0b013e31823b21e2 [DOI] [PubMed] [Google Scholar]
- 25.Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corrà U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FDR, Løchen ML, Löllgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, van der Worp HB, van Dis I, Binno Verschuren WMM; ESC Scientific Document Group. 2016 European guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37:2315–2381. 10.1093/eurheartj/ehw106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buckingham SA, Taylor RS, Jolly K, Zawada A, Dean SG, Cowie A, Norton RJ, Dalal HM. Home-based versus centre-based cardiac rehabilitation: abridged Cochrane Systematic Review and Meta-Analysis. Open Heart. 2016;3:e000463 10.1136/openhrt-2016-000463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taylor RS, Dalal H, Jolly K, Zawada A, Dean SG, Cowie A, Norton RJ. Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst Rev. 2015:CD007130. [DOI] [PubMed] [Google Scholar]
- 28.Dalal HM, Zawada A, Jolly K, Moxham T, Taylor RS. Home based versus centre based cardiac rehabilitation: Cochrane Systematic Review and Meta-Analysis. BMJ. 2010;340:b5631 10.1136/bmj.b5631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.British Heart Foundation. National Audit of Cardiac Rehabilitation (NACR) Annual Statistical Report 2017. https://www.bhf.org.uk/publications/statistics/national-audit-of-cardiac-rehabilitation-annual-statistical-report-2017 Accessed January 27, 2017.
- 30.Asch DA, Muller RW, Volpp KG. Automated hovering in health care–watching over the 5000 hours. N Engl J Med. 2012;367:1–3.. 10.1056/NEJMp1203869 [DOI] [PubMed] [Google Scholar]
- 31.Tang LH, Kikkenborg Berg S, Christensen J, Lawaetz J, Doherty P, Taylor RS, Langberg H, Zwisler AD. Patients’ preference for exercise setting and its influence on the health benefits gained from exercise-based cardiac rehabilitation. Int J Cardiol. 2017;232:33–39. 10.1016/j.ijcard.2017.01.126 [DOI] [PubMed] [Google Scholar]
- 32.Balady GJ, Williams MA, Ades PA, Bittner V, Comoss P, Foody JM, Franklin B, Sanderson B, Southard D. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2007;115:2675–2682. 10.1161/CIRCULATIONAHA.106.180945 [DOI] [PubMed] [Google Scholar]
- 33.Moher D, Liberati, Tetzlaff J, Altman DG; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269, W64. [DOI] [PubMed] [Google Scholar]
- 34.Schulz KF, Altman DG, Moher D; CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010;152:726–732. 10.7326/0003-4819-152-11-201006010-00232 [DOI] [PubMed] [Google Scholar]
- 35.Carlson JJ, Johnson JA, Franklin BA, VanderLaan RL. Program participation, exercise adherence, cardiovascular outcomes, and program cost of traditional versus modified cardiac rehabilitation. Am J Cardiol. 2000;86:17–23. [DOI] [PubMed] [Google Scholar]
- 36.Cowie A, Thow MK, Granat MH, Mitchell SL. Effects of home versus hospital-based exercise training in chronic heart failure. Int J Cardiol. 2012;158:296–298. 10.1016/j.ijcard.2012.04.117 [DOI] [PubMed] [Google Scholar]
- 37.Gordon NF, English CD, Contractor AS, Salmon RD, Leighton RF, Franklin BA, Haskell WL. Effectiveness of three models for comprehensive cardiovascular disease risk reduction. Am J Cardiol. 2002;89:1263–1268. [DOI] [PubMed] [Google Scholar]
- 38.Miller NH, Haskell WL, Berra K, DeBusk RF. Home versus group exercise training for increasing functional capacity after myocardial infarction. Circulation. 1984;70:645–649. [DOI] [PubMed] [Google Scholar]
- 39.Sparks KE, Shaw DK, Eddy D, Hanigosky P, Vantrese J. Alternatives for cardiac rehabilitation patients unable to return to a hospital-basedprogram. Heart Lung. 1993;22:298–303. [PubMed] [Google Scholar]
- 40.Bell JM. A Comparison of a Multi-Disciplinary Home Based Cardiac Rehabilitation Programme With Comprehensive Conventional Rehabilitation in Post-Myocardial Infarction Patients [dissertation].London, UK:UniversityofLondon; 1998. [Google Scholar]
- 41.Jolly K, Taylor R, Lip GY, Greenfield S, Raftery J, Mant J, Lane D, Jones M, Lee KW, Stevens A. The Birmingham Rehabilitation Uptake Maximisation Study (BRUM): home-based compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence. Health Technol Assess. 2007;11:1–118. [DOI] [PubMed] [Google Scholar]
- 42.Aamot IL, Forbord SH, Gustad K, Løckra V, Stensen A, Berg AT, Dalen H, Karlsen T, Støylen A. Home-based versus hospital-based high-intensity interval training in cardiac rehabilitation: a randomized study. Eur J Prev Cardiol. 2014;21:1070–1078.. 10.1177/2047487313488299 [DOI] [PubMed] [Google Scholar]
- 43.Moholdt T, Bekken Vold M, Grimsmo J, Slørdahl SA, Wisløff U. Home-based aerobic interval training improves peak oxygen uptake equal to residential cardiac rehabilitation: a randomized, controlled trial. PLoS One. 2012;7:e41199 10.1371/journal.pone.0041199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Daskapan A, Arikan H, Caglar N, Tunali N, Ataman S. Compparison of supervised exercise training and home-based exercise training in chronic heart failure. Saudi Med J. 2005;26:842–847. [PubMed] [Google Scholar]
- 45.Karapolat H, Demir E, Bozkaya YT, Eyigor S, Nalbantgil S, Durmaz B, Zoghi M. Comparison of hospital-based versus home-based exercise training in patients with heart failure: effects on functional capacity, quality of life, psychological symptoms, and hemodynamic parameters. Clin Res Cardiol. 2009;98:635–642. 10.1007/s00392-009-0049-6 [DOI] [PubMed] [Google Scholar]
- 46.Arthur HM, Smith KM, Kodis J, McKelvie R. A controlled trial of hospital versus home-based exercise in cardiac patients. Med Sci Sports Exerc. 2002;34:1544–1550. 10.1249/01.MSS.0000030847.23854.CB [DOI] [PubMed] [Google Scholar]
- 47.Grace SL, Midence L, Oh P, Brister S, Chessex C, Stewart DE, Arthur HM. Cardiac rehabilitation program adherence and functional capacity among women: a randomized controlled trial. Mayo Clin Proc. 2016;91:140–148. 10.1016/j.mayocp.2015.10.021 [DOI] [PubMed] [Google Scholar]
- 48.Oerkild B, Frederiksen M, Hansen JF, Simonsen L, Skovgaard LT, Prescott E. Home-based cardiac rehabilitation is as effective as centre-based cardiac rehabilitation among elderly with coronary heart disease: results from a randomised clinical trial. Age Ageing. 2011;40:78–85. 10.1093/ageing/afq122 [DOI] [PubMed] [Google Scholar]
- 49.Piotrowicz E, Baranowski R, Bilinska M, Stepnowska M, Piotrowska M, Wójcik A, Korewicki J, Chojnowska L, Malek LA, Klopotowski M, Piotrowski W, Piotrowicz R. A new model of home-based telemonitored cardiac rehabilitation in patients with heart failure: effectiveness, quality of life, and adherence. Eur J Heart Fail. 2010;12:164–171. 10.1093/eurjhf/hfp181 [DOI] [PubMed] [Google Scholar]
- 50.Kassaian MMM, Noohi F, Eftekharzadeh M, Arya A, Roshanall F, Momtahen M. Comparing effects of supervised versus home-based cardiac rehabilitation. Iranian Heart J. 2000;1:95–100. [Google Scholar]
- 51.Varnfield M, Karunanithi M, Lee CK, Honeyman E, Arnold D, Ding H, Smith C, Walters DL. Smartphone-based home care model improved use of cardiac rehabilitation in postmyocardial infarction patients: results from a randomised controlled trial. Heart. 2014;100:1770–1779. 10.1136/heartjnl-2014-305783 [DOI] [PubMed] [Google Scholar]
- 52.Wu SK, Lin YW, Chen CL, Tsai SW. Cardiac rehabilitation vs. home exercise after coronary artery bypass graft surgery: a comparison of heart rate recovery. Am J Phys Med Rehabil. 2006;85:711–717. 10.1097/01.phm.0000228597.64057.66 [DOI] [PubMed] [Google Scholar]
- 53.Marchionni N, Fattirolli F, Fumagalli S, Oldridge N, Del Lungo F, Morosi L, Burgisser C, Masotti G. Improved exercise tolerance and quality of life with cardiac rehabilitation of older patients after myocardial infarction: results of a randomized, controlled trial. Circulation. 2003;107:2201–2206. 10.1161/01.CIR.0000066322.21016.4A [DOI] [PubMed] [Google Scholar]
- 54.Kraal JJ, Peek N, Van den Akker-Van Marle ME, Kemps HM. Effects of home-based training with telemonitoring guidance in low to moderate risk patients entering cardiac rehabilitation: short-term results of the FIT@Home study. Eur J Prev Cardiol. 2014;21(Suppl):26–31. 10.1177/2047487314552606 [DOI] [PubMed] [Google Scholar]
- 55.Cowie A, Thow MK, Granat MH, Mitchell SL. A comparison of home and hospital-based exercise training in heart failure: immediate and long-term effects upon physical activity level. Eur J Cardiovasc Prev Rehabil. 2011;18:158–166. 10.1177/1741826710389389 [DOI] [PubMed] [Google Scholar]
- 56.Dalal HM, Evans PH, Campbell JL, Taylor RS, Watt A, Read KL, Mourant AJ, Wingham J, Thompson DR, Pereira G, ray DJ Home-based versus hospital-based rehabilitation after myocardial infarction: a randomized trial with preference arms– Cornwall Heart Attack Rehabilitation Management Study (CHARMS). Int J Cardiol. 2007;119:202–211. 10.1016/j.ijcard.2006.11.018 [DOI] [PubMed] [Google Scholar]
- 57.O’Connor CM, Whellan DJ, Lee KL, Keteyian SJ, Cooper LS, Ellis SJ, Leifer ES, Kraus WE, Kitzman DW, Blumenthal JA, Rendall DS, Miller NH, Fleg JL, Schulman KA, McKelvie RS, Zannad F, Piña IL; HF-ACTION Investigators. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA. 2009;301:1439–1450.. 10.1001/jama.2009.454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jolly K, Lip GY, Taylor RS, Raftery J, Mant J, Lane D, Greenfield S, Stevens A. The Birmingham Rehabilitation Uptake Maximisation study (BRUM): a randomised controlled trial comparing home-based with centre-based cardiac rehabilitation. Heart. 2009;95:36–42. 10.1136/hrt.2007.127209 [DOI] [PubMed] [Google Scholar]
- 59.Whittaker R, McRobbie H, Bullen C, Rodgers A, Gu Y. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev. 2016;4:CD006611 10.1002/14651858.CD006611.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gupta R, Sanderson BK, Bittner V. Outcomes at one-year follow-up of women and men with coronary artery disease discharged from cardiac rehabilitation: what benefits are maintained? J Cardiopulm Rehabil Prev. 2007;27:11–18; quiz 19. [DOI] [PubMed] [Google Scholar]
- 61.Haskell WL. The efficacy and safety of exercise programs in cardiac rehabilitation. Med Sci Sports Exerc. 1994;26:815–823. [PubMed] [Google Scholar]
- 62.Pavy B, Iliou MC, Meurin P, Tabet JY, Corone S; Functional Evaluation and Cardiac Rehabilitation Working Group of the French Society of Cardiology. Safety of exercise training for cardiac patients: results of the French registry of complications during cardiac rehabilitation. Arch Intern Med. 2006;166:2329–2334.. 10.1001/archinte.166.21.2329 [DOI] [PubMed] [Google Scholar]
- 63.Smith KM, McKelvie RS, Thorpe KE, Arthur HM. Six-year follow-up of a randomised controlled trial examining hospital versus home-based exercise training after coronary artery bypass graft surgery. Heart. 2011;97:1169–1174. 10.1136/hrt.2010.202036 [DOI] [PubMed] [Google Scholar]
- 64.Aamot IL, Karlsen T, Dalen H, Støylen A. Long-term exercise adherence after high-intensity interval training in cardiac rehabilitation: a randomized study. Physiother Res Int. 2016;21:54–64.. 10.1002/pri.1619 [DOI] [PubMed] [Google Scholar]
- 65.Andraos C, Arthur HM, Oh P, Chessex C, Brister S, Grace SL. Women’s preferences for cardiac rehabilitation program model: a randomized controlled trial. Eur J Prev Cardiol. 2015;22:1513–1522.. 10.1177/2047487314559275 [DOI] [PubMed] [Google Scholar]
- 66.Midence L, Arthur HM, Oh P, Stewart DE, Grace SL. Women’s health behaviours and psychosocial well-being by cardiac rehabilitation program model: a randomized controlled trial. Can J Cardiol. 2016;32:956–962. 10.1016/j.cjca.2015.10.007 [DOI] [PubMed] [Google Scholar]
- 67.Miller NH, Warren D, Myers D. Home-based cardiac rehabilitation and lifestyle modification: the MULTIFIT model. J Cardiovasc Nurs. 1996;11:76–87. [DOI] [PubMed] [Google Scholar]
- 68.Piotrowicz E, Zieliński T, Bodalski R, Rywik T, Dobraszkiewicz-Wasilewska B, Sobieszczańska-Małek M, Stepnowska M, Przybylski A, Browarek A, Szumowski Ł, Piotrowski W, Piotrowicz R. Home-based telemonitored Nordic walking training is well accepted, safe, effective and has high adherence among heart failure patients, including those with cardiovascular implantable electronic devices: a randomised controlled study. Eur J Prev Cardiol. 2015;22:1368–1377. 10.1177/2047487314551537 [DOI] [PubMed] [Google Scholar]
- 69.Piotrowicz E, Stepnowska M, Leszczyńska-Iwanicka K, Piotrowska D, Kowalska M, Tylka J, Piotrowski W, Piotrowicz R. Quality of life in heart failure patients undergoing home-based telerehabilitation versus outpatient rehabilitation: a randomized controlled study. Eur J Cardiovasc Nurs. 2015;14:256–263. 10.1177/1474515114537023 [DOI] [PubMed] [Google Scholar]
- 70.Taylor RS, Watt A, Dalal HM, Evans PH, Campbell JL, Read KL, Mourant AJ, Wingham J, Thompson DR, Pereira Gray DJ. Home-based cardiac rehabilitation versus hospital-based rehabilitation: a cost effectiveness analysis. Int J Cardiol. 2007;119:196–201. 10.1016/j.ijcard.2006.07.218 [DOI] [PubMed] [Google Scholar]
- 71.Schopfer DW, Krishnamurthi N, Shen H, Duvernoy CS, Forman DE, Whooley MA. Association of Veterans Health Administration home-based programs with access to and participation in cardiac rehabilitation. JAMA Intern Med. 2018;178:715–717. 10.1001/jamainternmed.2017.8039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ratchford AM, Hamman RF, Regensteiner JG, Magid DJ, Gallagher SB, Merenich JA. Attendance and graduation patterns in a group-model health maintenance organization alternative cardiac rehabilitation program. J Cardiopulm Rehabil. 2004;24:150–156. [DOI] [PubMed] [Google Scholar]
- 73.Brual J, Gravely S, Suskin N, Stewart DE, Grace SL. The role of clinical and geographic factors in the use of hospital versus home-based cardiac rehabilitation. Int J Rehabil Res. 2012;35:220–226. 10.1097/MRR.0b013e328353e375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cowie A, Moseley O. Home- versus hospital-based exercise training in heart failure: an economic analysis. Br J Cardiol. 2014;21:76. [Google Scholar]
- 75.Higgins RO, Murphy BM, Goble AJ, Le Grande MR, Elliott PC, Worcester MU. Cardiac rehabilitation program attendance after coronary artery bypass surgery: overcoming the barriers. Med J Aust. 2008;188:712–714. [DOI] [PubMed] [Google Scholar]
- 76.Ades PA, Keteyian SJ, Wright JS, Hamm LF, Lui K, Newlin K, Shepard DS, Thomas RJ. Increasing cardiac rehabilitation participation from 20% to 70%: a road map from the Million Hearts Cardiac Rehabilitation Collaborative. Mayo Clin Proc. 2017;92:234–242. 10.1016/j.mayocp.2016.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.DeBusk RF, Miller NH, Superko HR, Dennis CA, Thomas RJ, Lew HT, Berger WE 3rd, Heller RS, Rompf J, Gee D, Kraemer HC, Bandura A, Ghandour G, Clark M, Shah RV, Fisher L, Taylor CB. A case-management system for coronary risk factor modification after acute myocardial infarction. Ann Intern Med. 1994;120:721–729. [DOI] [PubMed] [Google Scholar]
- 78.Collins CA, Butryn ML, Jennings EG. Use of readiness for change in cardiac rehabilitation programs In: Kraus WE, Keteyian SJ, eds. Contemporary Cardiology: Cardiac Rehabilitation. Totowa, NJ: Humana Press, Inc; 2007:67–76. [Google Scholar]
- 79.Prochaska JO, Di Clemente CC. Transtheoretical therapy: toward a more integrative model of change. Psychother Theory Res Pract. 1982;19:276–288. [Google Scholar]
- 80.Hyman DJ, Pavlik VN, Taylor WC, Goodrick GK, Moye L. Simultaneous vs sequential counseling for multiple behavior change. Arch Intern Med. 2007;167:1152–1158. 10.1001/archinte.167.11.1152 [DOI] [PubMed] [Google Scholar]
- 81.Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, CruzFlores S, Davey-Smith G, Dennison-Himmelfarb CR, Lauer MS, Lockwood DW, Rosal M, Yancy CW; on behalf of the American Heart Association Council on Quality of Care and Outcomes Research, Council on Epidemiology and Prevention, Council on Cardiovascular and Stroke Nursing, Council on Lifestyle and Cardiometabolic Health, and Stroke Council. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132:873–898. 10.1161/CIR.0000000000000228 [DOI] [PubMed] [Google Scholar]
- 82.Britt E, Hudson SM, Blampied NM. Motivational interviewing in health settings: a review. Patient Educ Couns. 2004;53:147–155.. 10.1016/S0738-3991(03)00141-1 [DOI] [PubMed] [Google Scholar]
- 83.Bundy C. Changing behaviour: using motivational interviewing techniques. J R Soc Med. 2004;97(Suppl):43–47. [PMC free article] [PubMed] [Google Scholar]
- 84.Sandesara PB, Lambert CT, Gordon NF, Fletcher GF, Franklin BA, Wenger NK, Sperling L. Cardiac rehabilitation and risk reduction: time to “rebrand and reinvigorate.” J Am Coll Cardiol. 2015;65:389–395. 10.1016/j.jacc.2014.10.059 [DOI] [PubMed] [Google Scholar]
- 85.Epstein RM, Franks P, Fiscella K, Shields CG, Meldrum SC, Kravitz RL, Duberstein PR. Measuring patient-centered communication in patient-physician consultations: theoretical and practical issues. Soc Sci Med. 2005;61:1516–1528. 10.1016/j.socscimed.2005.02.001 [DOI] [PubMed] [Google Scholar]
- 86.Spring B, Ockene JK, Gidding SS, Mozaffarian D, Moore S, Rosal MC, Brown MD, Vafiadis DK, Cohen DL, Burke LE, D Lloyd-Jones; on behalf of the American Heart Association Behavior Change Committee of the Council on Epidemiology and Prevention, Council on Lifestyle and Cardiometabolic Health, Council for High Blood Pressure Research, and Council on Cardiovascular and Stroke Nursing. Better population health through behavior change in adults: a call to action. Circulation. 2013;128:2169–2176. 10.1161/01.cir.0000435173.25936.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Horwitz RI, Horwitz SM. Adherence to treatment and health outcomes. Arch Intern Med. 1993;153:1863–1868. [PubMed] [Google Scholar]
- 88.Franklin BA, Brinks J. Cardiac rehabilitation: underrecognized/underutilized. Curr Treat Options Cardiovasc Med. 2015;17:62 10.1007/s11936-015-0422-x [DOI] [PubMed] [Google Scholar]
- 88a.Feinberg JL, Russell D, Mola A, Trachtenberg M, Bick I, Lipman TH, Bowles KH. A mixed methods evaluation of the feasibility and acceptability of an adapted cardiac rehabilitation program for home care patients. Geriatr Nurs. 2018;39:191–198. [DOI] [PubMed] [Google Scholar]
- 89.Lothian NHS. The Heart Manual. http://www.theheartmanual.com Accessed January 27, 2017.
- 90.American Heart Association. An Active Partnership for the Health of Your Heart. Yardley, PA: StayWell Co Inc; 2015. [Google Scholar]
- 91.Henry Ford Health System. Home based cardiac rehabilitation. http://www.henryford.com/services/cardiology/cardiac-rehab/home-based-cardiac-rehabilitation Accessed March 5, 2017.
- 92.Health e-University. Cardiac college. http://www.cardiaccollege.ca Accessed January 27, 2017.
- 93.Heart Foundation website. https://heartfoundation.org.au/ Accessed January 27, 2017.
- 93a.Krishnamurthi N, Schopfer DW, Ahi T, Bettencourt M, Piros K, Ringer R, Shen H, Kehler JP, Whooley MA. Predictors of patient participation and completion of home-based cardiac rehabilitation in the Veterans Health Administration for patients with coronary heart disease. Am J Cardiol. 2019;123:19–24. [DOI] [PubMed] [Google Scholar]
- 94.Rohrbach G, Schopfer DW, Krishnamurthi N, Pabst M, Bettencourt M, Loomis J, Whooley MA. The design and implementation of a home-based cardiac rehabilitation program. Fed Pract. 2017;34:34–39. [PMC free article] [PubMed] [Google Scholar]
- 95.Wakefield B, Drwal K, Scherubel M, Klobucar T, Johnson S, Kaboli P. Feasibility an deffectiveness of remote, telephone-based delivery of cardiac rehabilitation. Telemed J E Health.2014;20:32–38. 10.1089/tmj.2013.0079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Dunlay SM, Witt BJ, Allison TG, Hayes SN, Weston SA, Koepsell E, Roger VL. Barriers to participation in cardiac rehabilitation. Am Heart J. 2009;158:852–859. 10.1016/j.ahj.2009.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dougherty CM, Glenny RW, Burr RL, Flo GL, Kudenchuk PJ. Prospective randomized trial of moderately strenuous aerobic exercise after an implantable cardioverter defibrillator. Circulation. 2015;131:1835–1842. 10.1161/CIRCULATIONAHA.114.014444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Piccini JP, Hellkamp AS, Whellan DJ, Ellis SJ, Keteyian SJ, Kraus WE, Hernandez AF, Daubert JP, Piña lL, O’Connor CM; HF-ACTION Investigators. Exercise training and implantable cardioverter-defibrillator shocks in patients with heart failure: results from HF-ACTION (Heart Failure and A Controlled Trial Investigating Outcomes of Exercise TraiNing). JACC Heart Fai. 2013;1:142–148. 10.1016/j.jchf.2013.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Franklin BA, Bonzheim K, Gordon S, Timmis GC. Safety of medically supervised outpatient cardiac rehabilitation exercise therapy: a 16-year follow-up. Chest. 1998;114:902–906. [DOI] [PubMed] [Google Scholar]
- 100.Center for Connected Health Policy. Current state laws & reimbursement policies. http://cchpca.org/state-laws-and-reimbursement-policies Accessed January 27, 2017.
- 101.Lawson KL, Jonk Y, O’Connor H, Riise KS, Eisenberg DM, Kreitzer MJ. The impact of telephonic health coaching on health outcomes in a high-risk population. Glob Adv Health Me. 2013;2:40–47. 10.7453/gahmj.2013.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Mohr DC, Ho J, Duffecy J, Reifler D, Sokol L, Burns MN, Jin L, Siddique J. Effect of telephone-administered vs face-to-face cognitive behavioral therapy on adherence to therapy and depression outcomes among primary carepatients: a randomized trial. JAMA. 2012;307:2278–2285. 10.1001/jama.2012.5588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Opdenacker J, Boen F. Effectiveness of face-to-face versus telephone support in increasing physical activity and mental health among university employees. J Phys Act Healt. 2008;5:830–843. [DOI] [PubMed] [Google Scholar]
- 104.Perri MG, Limacher MC, Durning PE, Janicke DM, Lutes LD, Bobroff LB, Dale MS, Daniels MJ, Radcliff TA, Martin AD. Extended-care programs for weight management in rural communities: the Treatment of Obesity in Underserved Rural Settings (TOURS) randomized trial. Arch Intern Med. 2008;168:2347–2354. 10.1001/archinte.168.21.2347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Strom JL, Egede LE. The impact of social support on outcomes in adult patients with type 2 diabetes: a systematic review. Curr Diab Rep. 2012;12:769–781. 10.1007/s11892-012-0317-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hamm LF, Sanderson BK, Ades PA, Berra K, Kaminsky LA, Roitman JL, Williams MA. Core competencies for cardiac rehabilitation/secondary prevention professionals: 2010 update: position statement of the American Association of Cardiovascular and Pulmonary Rehabilitation. J Cardiopulm Rehabil Prev. 2011;31:2–10. 10.1097/HCR.0b013e318203999d [DOI] [PubMed] [Google Scholar]
- 107.American Association of Cardiovascular and Pulmonary Rehabilitation. Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs. 5th ed. Champaign, IL: Human Kinetics; 1999. [Google Scholar]
- 108.Thomas RJ, King M, Lui K, Oldridge N, Piña IL, Spertus J. AACVPR/ACC/AHA 2007 performance measures on cardiac rehabilitation for referral to and delivery of cardiac rehabilitation/secondary prevention services. Circulation. 2007;116:1611–1642. 10.1161/CIRCULATIONAHA.107.185734 [DOI] [PubMed] [Google Scholar]
- 109.Thomas RJ, King M, Lui K, Oldridge N, Pina IL, Spertus J. AACVPR/ACCF/AHA 2010 update: performance measures on cardiac rehabilitation for referral to cardiac rehabilitation/secondary prevention services: a report of the American Association of Cardiovascular and Pulmonary Rehabilitation and the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures (Writing Committee to Develop Clinical Performance Measures for Cardiac Rehabilitation). Circulation. 2010;122:1342–1350. 10.1161/CIR.0b013e3181f5185b [DOI] [PubMed] [Google Scholar]
- 110.Thomas RJ, Balady G, Banka G, Beckie TM, Chiu J, Gokak S, Ho PM, Keteyian SJ, King M, Lui K, Pack Q, Sanderson BK, Wang TY. 2018 ACC/AHA clinical performance and quality measures for cardiac rehabilitation: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. Circ Cardiovasc Qual Outcomes. 2018;11:e000037 10.1161/HCQ.0000000000000037 [DOI] [PubMed] [Google Scholar]
- 111.Health.Gov. 2008. Physical activity guidelines for Americans. https://health.gov/paguidelines/guidelines/summary.aspx Accessed August 2,2017.
- 112.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–381. [PubMed] [Google Scholar]
- 113.Lear SA. The delivery of cardiac rehabilitation using communications technologies: the “virtual” cardiac rehabilitation program. Can J Cardiol. 2018;34(10S2):S278–S283. [DOI] [PubMed] [Google Scholar]
- 113a.Gabelhouse J, Eves N, Grace SL,Reid RC,Caperchione CM. Traditional versus hybrid outpatient cardiac rehabilitation: a comparison of patient outcomes. J Cardiopulm Rehabil Prev. 201838:231–238. 10.1097/HCR.0000000000000253 [DOI] [PubMed] [Google Scholar]
- 114.Franklin BA. An alternative approach to the delivery of cardiac rehabilitation services: a “hybrid” model for patient care. J Cardiopulm Rehabil. 2004;24:383–386. [DOI] [PubMed] [Google Scholar]
- 115.Hamm LF, Kavanagh T, Campbell RB, Mertens DJ, Beyene J, Kennedy J, Shephard RJ. Timeline for peak improvements during 52 weeks of outpatient cardiac rehabilitation.J Cardiopulm Rehabil. 2004;24:374–380; quiz 381. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.