Abstract
Head and neck reconstructive surgery involving tissue flaps is often complex requiring the development of an individualized anesthetic plan. The following case report describes the anesthetic management of an 87-year-old man considered at high risk for postoperative delirium due to advanced age and blindness undergoing general anesthesia for resection of squamous cell carcinoma of the right side of the nose and reconstructive surgery with a scalping forehead flap. Ultrasound-guided local anesthetic maxillary and supraorbital nerve blocks were successfully used perioperatively to reduce the need for alternative analgesics associated with higher risks of complications such as postoperative nausea, vomiting, and delirium.
Keywords: Ultrasound-guided maxillary nerve block, Supraorbital nerve block, Perioperative analgesia, Geriatric anesthesia, Scalping forehead flap, Postoperative delirium, General anesthesia
Multimodal approaches to managing acute postoperative pain following oral and maxillofacial surgery commonly incorporate a combination of acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), opioid agonists, and local anesthesia.1,2 However, NSAIDs and opioids can be associated with several potential complications, which may preclude their use. Potential drawbacks of NSAIDs include higher risks of serious cardiovascular, gastrointestinal, respiratory, and renal complications. For opioid agonists, the analgesic effect and risk of side effects are dose dependent. Potential complications associated with opioid use include sedation, dizziness, nausea, vomiting, constipation, dependence, tolerance, delayed gastric emptying, respiratory depression, and delirium. Consideration for using the lowest effective dose necessary is critical when adding opioids into an anesthetic management plan.
Postoperative delirium is a major risk factor for flap loss and complications following reconstruction with tissue flaps.3 As such, the prevention of postoperative delirium is essential to a good surgical outcome. Postoperative delirium is multifactorial4 with common risk factors that include dementia, stroke, Parkinson's disease, advanced age, sensory impairment, cerebrovascular disorders, sensory disorders, and pain.5–8
Postoperative nausea and vomiting (PONV) is another potential complication of particular importance as it can impair the patient's appetite,9,10 leading to delays in discharge and healing. Retching and vomiting can inadvertently lead to damage of the surgical sites as well. Anesthetic risk factors for PONV include the use of volatile anesthetics, prolonged duration of anesthesia, and opioid administration.11,12 Prevention of PONV is another important consideration for optimizing postoperative recovery.
In head and neck surgery, extensive use of opioids is common for intraoperative analgesia.1 In such cases, the risks of postoperative delirium and PONV increase accordingly.13 A conventional anesthetic plan that utilizes NSAIDs and opioids for managing postoperative analgesia for head and neck surgery, particularly for reconstruction with tissue flaps, may be suboptimal due to the potential side effects and complications. Therefore, consideration of alternative approaches that minimize the risks of delirium and PONV are likely warranted. In our hospital, extensive use of opioids for postoperative analgesia is generally avoided. This case report describes the successful anesthetic management utilizing ultrasound-guided a maxillary nerve block (MNB) and supraorbital nerve blocks (SNBs) for a geriatric patient undergoing a scalping forehead flap procedure and discusses the advantages of perioperative trigeminal nerve blockade. The following case report was approved by our institutional research ethics committee, and the patient provided informed consent prior to publication.
CASE PRESENTATION
An 87-year-old man (height 152 cm; weight 55 kg; body mass index 23 kg/m2) with squamous cell carcinoma of the right side of the nose underwent resection of the lesion and soft tissue reconstruction using a scalping forehead flap (Figures 1 and 2). The patient's medical history was significant for well-controlled diabetes mellitus type II (HbA1c 6.1%) and hypertension. He also had a history of a minor left thalamic stroke (asymptomatic) and blindness secondary to bilateral retinal detachment that occurred 13 years previously. The patient had no history of previous surgery, nor any allergies. The patient's medications included insulin degludec/insulin aspart (70/30; 16 units/d) and amlodipine. The preoperative tests (electrocardiography, pulmonary function test, and basic metabolic panel) and physical examination yielded no remarkable results.
Figure 1.
Surgical defect and planned soft tissue flap. Perioperative view of the resected nasal lesion and planned reconstruction with a left forehead rotational soft tissue flap.
Figure 2.
Completed soft tissue flap. Perioperative view of the completed reconstruction with the pedicle flap sutured in place.
The patient was deemed high risk for postoperative delirium due to his advanced age and blindness. As such, the developed anesthetic plan included general anesthesia in combination with regional local anesthetic blocks for perioperative analgesia to avoid the use of opioids. Ultrasound-guided right MNB and bilateral SNBs were utilized to provide anesthesia of the surgical sites (the upper right aspect of the maxilla and both sides of the forehead).
Standard anesthetic monitoring consisting of an electrocardiogram, a sphygmomanometer, capnography, and a pulse oximeter was instituted upon entry to the operating room. After intravenous (IV) access was obtained with a 20-gauge peripheral IV catheter, general anesthesia was induced with an IV bolus of propofol (60 mg) and maintained with desflurane (4%) and oxygen/air (50/50%; 2 L/min). Muscle relaxation was achieved with rocuronium (50 mg). A continuous infusion of remifentanil (0.05–0.2 mcg/kg/min) was administered from induction until intubation. The patient was mask ventilated and orally intubated with an 8.0-ETT without difficulty. After securing the airway, a right MNB was performed with 6 mL of 0.375% ropivacaine plain (22.5 mg) administered at the right lateral pterygoid plate via a suprazygomatic approach under ultrasound guidance (SonoSite SII, Fujifilm, Tokyo, Japan) (Figures 3 and 4).13,14 The ultrasound probe was placed just caudal to the zygomatic arch, and a 22-G needle was advanced to the lateral pterygoid plate. The needle insertion point for the right MNB was the angle formed by the superior edge of the zygomatic arch and the posterior orbital rim. Bilateral SNBs were performed with 2 mL (4 mL total) of 0.375 % ropivacaine plain (15 mg) under ultrasound guidance (Figure 5). The injection point was slightly cranial to the supraorbital notch, which was palpable as a bony landmark. The patient's heart rate and blood pressure remained stable (±20% of baseline) intraoperatively. The surgical procedure was completed in 3 hours and 16 minutes, blood loss was minimal, and the patient was extubated without difficulty while spontaneously breathing and fully awake. Acetaminophen (1000 mg) and tramadol (200 mg) were administered intravenously in the operating room after conclusion of the surgical procedure for additional postoperative analgesia. The immediate postoperative course was uneventful with no episodes of delirium or PONV. Notably antiemetics were not administered intra- or postoperatively. The patient had no complaints of pain, required no additional rescue analgesics throughout his stay until discharge on postoperative day 37, and had no postoperative complications.
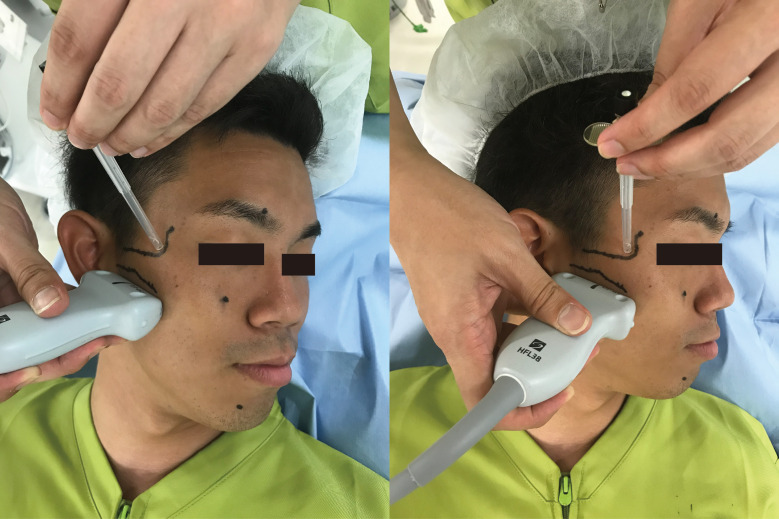
Figure 3.
Ultrasound-guided maxillary nerve block via a suprazygomatic approach. Ultrasound probe placed just caudal to the zygomatic arch and a 22-G block needle inserted at the angle formed by the superior edge of the zygomatic arch and the posterior orbital rim.
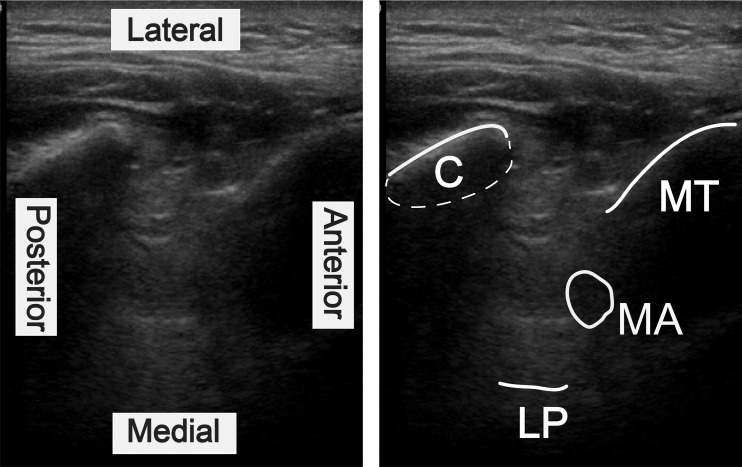
Figure 4.
Ultrasound visualization of the temporal fossa. The maxillary artery was observed in the temporal fossa, allowing avoidance of arterial injury. C, coronoid; LP, lateral plate of the pterygoid process; MT, maxillary tuberosity; MA, maxillary artery.
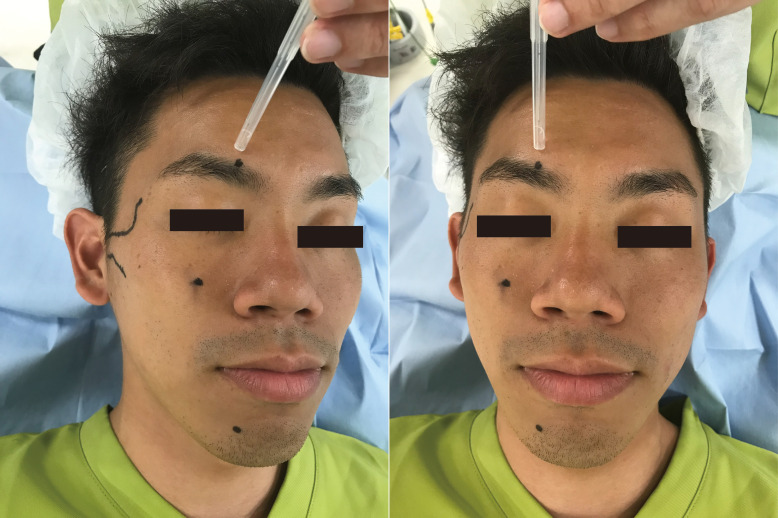
Figure 5.
Supraorbital nerve block approach. Needle insertion point was slightly cranial to the supraorbital notch, which was palpable as a bony landmark. Local anesthetic injected subcutaneously.
DISCUSSION
In this case, because the patient was elderly and had a visual impairment, the risk of developing delirium after general anesthesia was expected to be high. Therefore, ropivacaine, a long-acting local anesthetic, was utilized for nerve blocks to provide excellent perioperative anesthesia and analgesia without need for NSAIDs or potent opioids.
Nerve blocks administered in combination with a long-acting local anesthetic such as ropivacaine are superior to local anesthesia infiltration in terms of providing an increased duration of action coupled with an increased distribution or area of local anesthetic coverage. Although peripheral nerve blocks with lidocaine can effectively control surgical pain, the duration would be substantially shorter than blocks performed with ropivacaine, which can last for an extended period. Ropivacaine is effective as a plain local anesthetic as it inherently causes some degree of vasoconstriction negating the need for additional vasoconstrictors.
In this case, ropivacaine plain was utilized primarily due to its prolonged duration of action compared with lidocaine. The absence of epinephrine was also beneficial in preventing excessive cardiovascular stimulation. Ropivacaine can be used intraoperatively for an extended time with little cardiovascular fluctuation due to noxious surgical stimulation.
In our experience, an MNB with ropivacaine can provide sufficient analgesia for 12 to 24 hours.14,15 The use of local anesthesia permits avoidance of other more problematic analgesics (opioids and NSAIDs), leading to fewer instances of delirium, PONV, and other complications. Satisfactory analgesic effects have been obtained in other cases in our hospital while simultaneously reducing the risks of delirium and PONV (Table 1). Acute pain can be sufficiently controlled with the use of a long-acting local anesthetic for nerve blocks, producing negligible postoperative pain as was seen with this patient.
Table 1.
Additional Cases Utilizing Ultrasound-Guided Nerve Blocks in Our Hospital*
|
Sex |
Disease |
Operative Method |
Nerve Block |
Age |
Height (cm) |
Weight (kg) |
BM |
| Female | Postoperative maxillary cyst | Cyst resection | MNB | 70 | 148 | 40 | 18 |
| Male | Zygomatic fracture | Open reduction and internal fixation | MNB | 84 | 160 | 61 | 23 |
| Female | Zygomatic fracture | Open reduction and internal fixation | MNB | 75 | 152 | 51 | 21 |
| Male | Post-jaw deformities | Plate removal | MNB, IANB | 22 | 172 | 54 | 18 |
| Male | Zygomatic fracture | Open reduction and internal fixation | MNB | 72 | 165 | 72 | 26 |
| Female | Impacted third molar teeth | Teeth extraction | MNB, IANB | 22 | 156 | 52 | 21 |
| Female | Jaw deformities | Mandibular and maxillary surgery | NMB, IANB | 22 | 156 | 42 | 17 |
MNB, maxillary nerve block; IANB, inferior alveolar nerve block.
Table 1.
(Extended)
|
ASA-PS |
Operation Time |
Anesthesia Time |
Initial Opioid for Anesthesia Induction (Yes/No) |
Additional Opioids Given Intraoperatively (Yes/No) |
Opioid Requirement in Ward by POD2 (Yes/No) |
Postoperative Delirium (Yes/No) |
| 2 | 1:51 | 3:05 | No | Yes | No | No |
| 2 | 4:13 | 5:24 | No | Yes | No | No |
| 2 | 4:00 | 5:11 | No | No | No | No |
| 1 | 2:55 | 4:06 | No | No | No | No |
| 2 | 3:26 | 4:50 | No | No | No | No |
| 1 | 2:47 | 3:49 | No | No | No | No |
| 1 | 8:49 | 10:24 | No | Yes | No | No |
Administering local anesthetics under ultrasound guidance provides several benefits. Ultrasound-guided local anesthetic delivery can help avoid inadvertent intravascular injection. The local anesthetic solution can also be visualized during injection surrounding the target nerves. It is also possible to identify deep maxillofacial structures, such as the maxillary artery or maxillary tuberosity. The needle location can be easily visualized during insertion, allowing adjustments to anatomical positional relationships in real time, further enabling safe and accurate local anesthetic delivery. Ultrasonography can be useful for a variety of local anesthetic injections including inferior alveolar nerve blocks (IANBs).16
In the present case, not only was perioperative pain management satisfactory, but there were also no complications related to the local anesthetic blocks. The success rates of ultrasound-guided suprazygomatic MNB and IANBs are 100% in our experience (Table 1).14 Because ultrasound-guided MNBs and IANBs were introduced to our hospital, we have performed these techniques for all patients undergoing oral and maxillofacial surgery procedures. We have found MNBs to be quite effective for surgical procedures involving zygomatic fractures or maxillary cystectomies, as well as in orthognathic surgeries when combined with IANBs. Performance of these nerve blocks via ultrasound guidance can provide effective perioperative analgesia while minimizing the risk of adverse events for at-risk patient populations, such as the extremes of age, patients with significant medical comorbidities, and those at high risk of postoperative delirium.
CONCLUSION
This case report presents the successful use of an ultrasound-guided right MNB and bilateral SNBs with ropivacaine to provide safe and reliable analgesia for a patient at high risk of postoperative delirium. These blocks were effective and reduced the need for additional analgesics (opioids and NSAIDs) likely to cause complications in this patient.
ACKNOWLEDGMENTS
The datasets are available from the corresponding author on reasonable request.
YK, KM, and KH wrote the paper and were involved in the anesthetic management of this case. All authors read and approved the final manuscript. The authors declare that they have no competing interests.
Permission was obtained from the patient to report this case. The Ethics Committee of Asahi General Hospital approved of this case report.
REFERENCES
- 1.Đanić P, Salarić I, Macan D. New findings on local tramadol use in oral surgery. Acta Stomatol Croat. 2017;51:336–344. doi: 10.15644/asc51/4/9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bennett JD. Preoperative preparation and planning of the oral and maxillofacial surgery patient. Oral Maxillofac Surg Clin North Am. 2017;29:131–140. doi: 10.1016/j.coms.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Yang R, Lubek JE, Dyalram D, Liu X, Ord RA. Head and neck cancer surgery in an elderly patient population: a retrospective review. Int J Oral Maxillofac Surg. 2014;43:1413–1417. doi: 10.1016/j.ijom.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 4.Elie M, Cole MG, Primeau FJ, Bellavance F. Delirium risk factors in elderly hospitalized patients. J Gen Intern Med. 1998;13:204–212. doi: 10.1046/j.1525-1497.1998.00047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fick DM, Agostini JV, Inouye SK. Delirium superimposed on dementia: a systematic review. J Am Geriatr Soc. 2002;50:1723–1732. doi: 10.1046/j.1532-5415.2002.50468.x. [DOI] [PubMed] [Google Scholar]
- 6.Lundström M, Edlund A, Bucht G, Karlsson S, Gustafson Y. Dementia after delirium in patients with femoral neck fractures. J Am Geriatr Soc. 2003;51:1002–1006. doi: 10.1046/j.1365-2389.2003.51315.x. [DOI] [PubMed] [Google Scholar]
- 7.Inouye SK, Robinson T, Blaum C, et al. American Geriatrics Society Expert Panel on Postoperative Delirium in Older Adults. Postoperative delirium in older adults: best practice statement from the American Geriatrics Society. J Am Coll Surg. 2015;220:136–148.e1. doi: 10.1016/j.jamcollsurg.2014.10.019. [DOI] [PubMed] [Google Scholar]
- 8.Ahmed S, Leurent B, Sampson EL. Risk factors for incident delirium among older people in acute hospital medical units: a systematic review and meta-analysis. Age Ageing. 2014;43:326–333. doi: 10.1093/ageing/afu022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.White PF, O'Hara JF, Roberson CR, Wender RH, Candiotti KA; POST-OP Study Group. The impact of current antiemetic practices on patient outcomes: a prospective study on high-risk patients. Anesth Analg. 2008;107:452–458. doi: 10.1213/ane.0b013e31817b842c. [DOI] [PubMed] [Google Scholar]
- 10.Manahan MA, Basdag B, Kalmar CL, et al. Risk of severe and refractory postoperative nausea and vomiting in patients undergoing diep flap breast reconstruction. Microsurgery. 2014;34:112–121. doi: 10.1002/micr.22155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Apfel CC, Heidrich FM, Jukar-Rao S, et al. Evidence-based analysis of risk factors for postoperative nausea and vomiting. Br J Anaesth. 2012;109:742–753. doi: 10.1093/bja/aes276. [DOI] [PubMed] [Google Scholar]
- 12.Koivuranta M, Läärä E, Snåre L, Alahuhta S. A survey of postoperative nausea and vomiting. Anaesthesia. 1997;52:443–449. doi: 10.1111/j.1365-2044.1997.117-az0113.x. [DOI] [PubMed] [Google Scholar]
- 13.Marcantonio ER, Juarez G, Goldman L, et al. The relationship of postoperative delirium with psychoactive medications. JAMA. 1994;272:1518–1522. [PubMed] [Google Scholar]
- 14.Kumita S, Murouchi T, Arakawa J. Ultrasound-guided maxillary and inferior alveolar nerve blocks for postoperative analgesia in gnathoplasty. Asian J Anesthesiol. 2017;55:89–90. doi: 10.1016/j.aja.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 15.Sola C, Raux O, Savath L, Macq C, Capdevila X, Dadure C. Ultrasound guidance characteristics and efficiency of suprazygomatic maxillary nerve blocks in infants: a descriptive prospective study. Paediatr Anaesth. 2012;22:841–846. doi: 10.1111/j.1460-9592.2012.03861.x. [DOI] [PubMed] [Google Scholar]
- 16.Kojima Y, Murouchi T, Akiba M, Oka T. Ultrasound-guided inferior alveolar nerve block for postoperative analgesia after mandibular sequestrectomy: a single-center retrospective study. J Clin Anesth. 2019;60:39–40. doi: 10.1016/j.jclinane.2019.08.026. [DOI] [PubMed] [Google Scholar]