Abstract
Rationale: Racial disparities in health and healthcare in the United States are well documented and are increasingly recognized in acute critical illnesses such as sepsis and acute respiratory failure.
Objectives: Using a large, representative, U.S. nationwide database, we examined the hypothesis that black and Hispanic patients with severe acute respiratory failure have higher mortality rates when compared with non-Hispanic whites.
Methods: This retrospective analysis used discharge data from the Agency for Healthcare Research and Quality, Nationwide Inpatient Sample, Healthcare Cost and Utilization Project, for the years 2008–2012. We identified hospitalizations with acute respiratory failure using a combination of International Classification of Diseases, Ninth Revision, Clinical Modification, codes. A logistic regression model was fitted to compare in-hospital mortality rates by race.
Measurements and Main Results: After adjusting for sex, age, race, disease severity, type of hospital, and median household income for patient ZIP code, blacks had a greater odds ratio of in-hospital death when compared with non-Hispanic whites (odds ratio [OR], 1.13; 95% confidence interval [CI], 1.11–1.14; P < 0.001), and Hispanics also had a greater odds ratio of in-hospital death when compared with non-Hispanic whites (OR, 1.17; 95% CI, 1.15–1.19; P < 0.001), and so did Asian and Pacific Islanders (OR, 1.15; 95% CI, 1.12–1.18; P < 0.001) and Native Americans (OR, 1.08; 95% CI, 1.00–1.15; P < 0.001) when compared with non-Hispanic whites (OR, 1.0).
Conclusions: Blacks, Hispanics, and other racial minorities in the United States were observed to exhibit significantly higher in-hospital sepsis-related respiratory failure associated mortality when compared with non-Hispanic whites.
Keywords: respiratory failure, health disparities, race, ethnicity, mortality
Acute respiratory failure (ARF) is a frequent complication of hospitalization and the most common reason for admission to intensive care units (1). Common causes include acute asthma exacerbation, acute exacerbation of chronic obstructive pulmonary disease (COPD), acute congestive heart failure (CHF), pneumonia, and acute respiratory distress syndrome (ARDS).
Racial disparities in health and healthcare in the United States have been well-documented and are increasingly recognized in terms of the outcomes of acute critical illnesses such as sepsis and ARF (2–5). Previously reported epidemiologic studies in the United States have shown an association between black race or Hispanic ethnicity and increased risk for and mortality from ARDS (6–9). However, other studies reported no difference in ARDS risk and mortality for these groups when compared with non-Hispanic whites (10–12).
Variability in case definition and data accuracy might explain the observed discrepancies on the association between black race or Hispanic ethnicity and ARDS mortality. In large database studies, there are currently no validated standardized criteria for identification of ARDS. This potentially leads to disease misclassification because these databases rely on International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), codes to identify cases of ARDS. Unfortunately, there is no specific diagnostic code for ARDS, and several ICD-9-CM codes are used to describe various subtypes of ARF.
An alternative and more practical approach is to capture cases of severe ARF not resulting from acute asthma exacerbations, acute exacerbations of COPD, or acute CHF exacerbation by using an algorithm that excludes these subgroups of patients while including those who required intubation and mechanical ventilation.
In this analysis, we used a large, well-characterized, representative nationwide database of adults hospitalized in the United States from 2008 to 2012 to identify cases of ARF that closely approximate ARDS by using well-defined selection criteria to exclude ARF resulting from acute asthma exacerbations, acute exacerbations of COPD, and acute CHF. Our main objective was to examine the racial differences in hospital mortality among patients hospitalized with severe ARF. We hypothesized that compared with non-Hispanic whites, black and Hispanic patients hospitalized with severe ARF will exhibit a greater mortality.
Methods
Study Design, Data Source, and Study Population
We performed a retrospective study using discharge data from the largest all-payer inpatient healthcare database in the United States, the Nationwide Inpatient Sample (NIS), Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality (HCUP-NIS). This database has been maintained by the Agency for Healthcare Research and Quality since 1988. Unweighted, it includes data from approximately 8 million hospital stays per year, representing a 20% stratified probability sample of all nonfederal acute care hospitalizations in the United States. When expanded to include nationwide discharges (weighted), this database estimates data corresponding to approximately 40 million annual hospitalizations. Each hospitalization is treated as an individual database entry.
The HCUP-NIS database contains the following types of data: patient and hospital demographics, admission and treating diagnoses, inpatient procedures, in-hospital mortality rates, hospital length of stay, hospital charges, and discharge status. Data from the 5-year period from 2008 to 2012 were used for this analysis. We used the principal diagnosis, secondary diagnoses, and procedural diagnoses associated with each hospitalization, as presented in the HCUP-NIS database, to identify patient hospitalizations relevant for this analysis.
We identified hospitalizations with severe ARF for adult patients older than 18 years during the study period. In accordance with previous literature (6, 7, 13, 14), we defined severe ARF as use of ICD-9-CM codes for ARF and use of ICM-9-CM codes for continuous invasive mechanical ventilation. Patients with primary ICD-9-CM codes for acute asthma exacerbations, acute exacerbations of COPD, and acute CHF exacerbation were excluded from the analysis. The detailed codes we used to identify these hospitalizations are provided in Table 1.
Table 1.
List of International Classification of Diseases, Ninth Revision, Clinical Modification, codes used to identify acute respiratory distress syndrome
| ICD-9-CM Codes | ICD-9 Code Description |
|---|---|
| Inclusion criteria | |
| 518.81 | Acute respiratory failure |
| 518.82 | Other pulmonary insufficiency, not elsewhere classified; includes acute respiratory distress, acute respiratory insufficiency, and adult respiratory distress syndrome, not elsewhere classified |
| 518.84 | Acute and chronic respiratory failure |
| 518.51 | Acute respiratory failure after trauma and surgery |
| 518.52 | Other pulmonary insufficiency, not elsewhere classified, after trauma and surgery |
| 518. 53 | Acute and chronic respiratory failure after trauma and surgery |
| 518.4 | Acute edema of lung unspecified |
| 518.7 | Transfusion related acute lung injury |
| 785.52 | Septic shock |
| 995.92 | Severe sepsis |
| 96.70 | Continuous invasive mechanical ventilation of unspecified duration |
| 96.71 | Continuous invasive mechanical ventilation for less than 96 consecutive hours |
| 96.72 | Continuous invasive mechanical ventilation for 96 consecutive hours or more |
| Exclusion criteria | |
| 493.91 | Status asthmaticus |
| 493.92 | Acute asthma exacerbation |
| 493.22 | Acute exacerbation of chronic obstructive pulmonary disease |
Definition of abbreviation: ICD-9-CM = International Classification of Disease, Ninth Revision.
Study Variables
Our primary outcome of interest was all-cause in-hospital mortality, and the main predictor variable was race. We identified patient demographic characteristics (age, sex, and race), associated comorbidities, disease severity index, the primary payer for the hospitalization, type of hospital (urban vs rural and teaching vs nonteaching), and median income for patient ZIP code as a surrogate for socioeconomic status by using the appropriate variables from the HCUP-NIS database. Median income for patient ZIP code is an ordinal variable in the HCUP-NIS database that is used as a surrogate for socioeconomic status
The database provides a quartile classification of the estimated median household income of residents in the patient’s ZIP code. The quartiles are identified by values of 1 to 4, indicating the poorest (quartile 1) to wealthiest (quartile 4) populations. These values are derived from ZIP code-demographic data obtained from Claritas Inc (15). Hospitalizations with missing data on in-hospital mortality or race/ethnicity were excluded.
Statistical Analysis
Using the weights provided in the HCUP-NIS database, national estimates for the number of overall severe ARF hospitalizations, race, and sex were generated. Demographic and clinical characteristics were expressed as mean with standard deviations or percentages across all 5 years (2008–2012). Chi-square testing was used to compare categorical variables and ANOVA for continuous data.
A multiple logistic regression model was fit, with in-hospital mortality as the outcome variable and the following covariates: indicator of sex, age in years at admission (revised), race (uniform), calendar year, median household income national quartile for patient ZIP code, Agency for Healthcare Research and Quality comorbidity measure (diabetes, uncomplicated), Agency for Healthcare Research and Quality comorbidity measure (diabetes with chronic complications), all patient refined Diagnosis-Related Group (risk for mortality subclass), rural vs urban, nonteaching vs teaching. All covariates were selected a priori and entered into the regression model.
All data analyses were conducted using STATA/IC 13.1 (StataCorp; College Station, TX) and SPSS (IBM SPSS Statistics for Macintosh, Version 23.0; IBM Corp, Armonk, NY). The University of Arizona Institutional Review Board granted an exemption from review for this study. The study conforms to the data-use agreement for the HCUP-NIS database.
Results
Patient Characteristics
We identified a total of 821,902 patient discharges for severe ARF in the HCUP-NIS database during the study period (2008–2012). The majority of patients were non-Hispanic white (68%), and male (53%). The mean age of the patients was 64 years. The majority came from ZIP codes in the lowest quartile for median income (31% vs 21% or less for the other quartiles). The primary payer for the majority of patients was Medicare (60%), followed by private insurance (19%), and Medicaid (14%). Detailed characteristics of the patients, by year are presented in Table 2.
Table 2.
Baseline characteristics of patient discharges for Acute Respiratory Distress Syndrome in the Healthcare Cost and Utilization Project–Nationwide Inpatient Sample Database, 2008–2012
| Year | 2008 | 2009 | 2010 | 2011 | 2012 | Total |
|---|---|---|---|---|---|---|
| All patients, N |
130,446 |
150,285 |
164,980 |
184,336 |
191,855 |
821,902 |
| Racial/ethnic groups, N (%) | ||||||
| White | 85,172 (67.7) | 96,462 (67.0) | 106,475 (67.4) | 119,233 (67.5) | 124,810 (68.3) | 532,152 (67.6) |
| Black | 20,686 (14.2) | 24,658 (13.9) | 30,563 (16.3) | 32,548 (15.5) | 32,065 (14.1) | 140,520 (14.8) |
| Hispanic | 13,513 (10.1) | 16,570 (10.8) | 16,733 (9.6) | 19,500 (10.0) | 19,940 (9.9) | 86,256 (10.1) |
| Asian and Pacific Islander | 5,184 (3.7) | 5,575 (3.5) | 4,891 (2.8) | 5,137 (2.6) | 5,990 (2.9) | 26,777 (3.1) |
| Native American | 1,031 (0.8) | 1,179 (0.9) | 1,175 (0.8) | 1,310 (0.8) | 1,485 (0.8) | 6,180 (0.8) |
| Other | 4,860 (3.6) | 5,841 (3.9) | 5,143 (3.1) | 6,608 (3.6) | 7,565 (4.0) | 30,017 (3.6) |
| Sex, N (%) | ||||||
| Female | 74,948 (47.4) | 79,843 (46.6) | 85,720 (47.9) | 70,961 (46.8) | 92,815 (46.1) | 42,7135 (46.7) |
| Mean age, years, (SD) | ||||||
| Age | 64.6 (17.3) | 63.5 (17.5) | 63.8 (17.0) | 64.0 (17.0) | 64.0 (16.6) | 64.0(17.1) |
| Age groups, % | ||||||
| <65 yr | 45.6 | 48.2 | 47.3 | 47.5 | 47.6 | 47.3 |
| 65–84 yr | 43.7 | 41.9 | 42.5 | 42.6 | 42.4 | 42.6 |
| ≥85 yr | 10.7 | 9.9 | 10.2 | 9.9 | 10 | 10.1 |
| Socioeconomic status represented in quartiles, %* | ||||||
| Quartile 1 | 29.4 | 29.3 | 31.3 | 30.8 | 31.9 | 30.6 |
| Quartile 2 | 25.7 | 24.8 | 24.3 | 24.1 | 24.1 | 24.5 |
| Quartile 3 | 23 | 24.7 | 23.4 | 25.3 | 23.6 | 24 |
| Quartile 4 | 22 | 21.2 | 21 | 19.8 | 20.5 | 20.8 |
| Expected Primary Insurance Payer, %† | ||||||
| Medicare | 59.8 | 58.6 | 59.2 | 60.8 | 61 | 59.9 |
| Medicaid | 13 | 14.1 | 14.7 | 13.9 | 14 | 14 |
| Private Insurance | 20.5 | 20.2 | 19.3 | 18.4 | 17.4 | 19.1 |
| Self-pay | 3.8 | 4.3 | 4 | 4 | 4.6 | 4.1 |
| Other | 2.5 | 2.5 | 2.5 | 2.4 | 2.7 | 2.5 |
Healthcare Cost and Utilization Project’s National Inpatient Sample provides a quartile classification of the estimated median household income of residents in the patient's ZIP code. The quartiles are identified by values of 1 to 4, indicating the poorest (quartile 1) to wealthiest (quartile 4) populations. These values are derived from ZIP code-demographic data obtained from Claritas.
Expected primary payer: Medicare includes both fee-for-service and managed care Medicare patients; Medicaid includes both fee-for-service and managed care Medicaid patients; private insurance (PAY1 = 3) includes BlueCross, commercial carriers, and private health maintenance organizations and preferred provider organizations; and other includes worker's compensation, Civilian Health and Medical Program of the Uniformed Services, Civilian Health and Medical Program of the Department of Veterans Affairs, Title V, and other government programs.
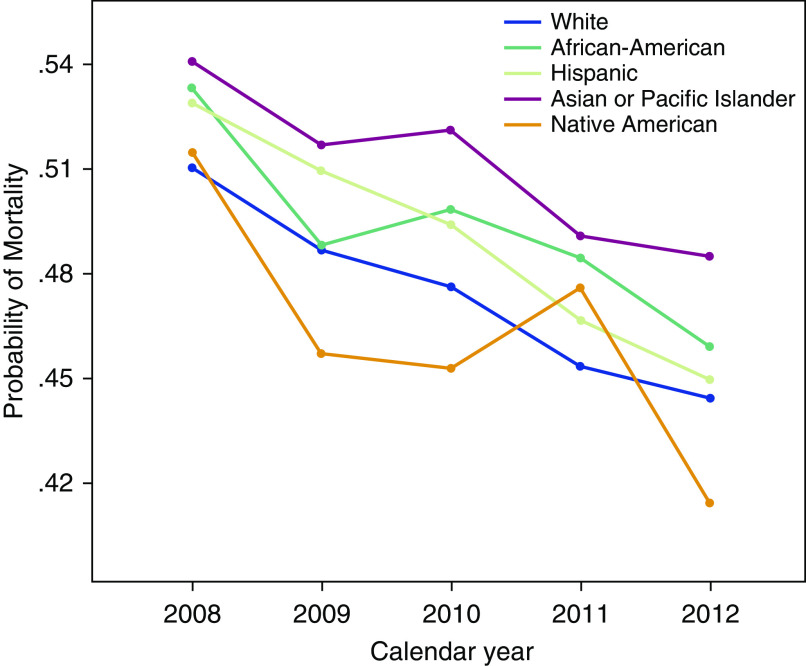
Trends in Mortality
The overall all-cause inpatient mortality for those with severe ARF declined progressively from 52% in 2008 to 45% in 2012 (P < 0.001). This trend was observed across all racial and ethnic groups (Figure 1).
Figure 1.
Trends in mortality from severe acute respiratory failure, 2008–2012.
Mortality Differences by Race
The overall all-cause inpatient mortality rate for those with severe ARF during the study period was 48%. When compared with non-Hispanic whites, blacks, Hispanics, and Asian and Pacific Islanders each exhibited significantly higher inpatient mortality rates. (Table 3; Figure 1). After adjusting for sex, age, race, disease severity, type of hospital, and median household income for patient ZIP code, blacks had a greater odds ratio of in-hospital mortality when compared with non-Hispanic whites (odds ratio, 1.13; 95% confidence interval [CI], 1.11–1.14; P < 0.001), and Hispanics also had a greater odds ratio of in-hospital mortality when compared with non-Hispanic whites (odds ratio, 1.17; 95% CI, 1.15–1.19; P < 0.001), and so did Asian and Pacific Islanders (odds ratio, 1.15; 95% CI, 1.12–1.18; P < 0.001) and Native Americans (odds ratio, 1.08; 95% CI, 1.00–1.15; P < 0.001) when compared with non-Hispanic whites (odds ratio, 1.0).
Table 3.
Results of multiple logistic regression analysis to predict in-hospital mortality among 821,902 patients based on sex, age, race/ethnicity, year, socioeconomic status, and history of diabetes mellitus
| Variables | Parameter Estimates (β) | Standard Errors | Wald χ2 | P Value | Odds Ratio | 95% Confidence Interval (Lower) | 95% Confidence Interval (Upper) |
|---|---|---|---|---|---|---|---|
| Intercept | −1.114 | 0.013 | |||||
| Male (reference) | 1 | ||||||
| Female | −0.012 | 0.005 | 7.09 | 0.008 | 0.99 | 0.98 | 1.00 |
| Age | 0.018 | 0.000 | 17,011 | <0.001 | 1.02 | 1.01 | 1.04 |
| Race/ethnicity | |||||||
| White (reference) | 809 | 1 | |||||
| Black | 0.138 | 0.006 | 467 | <0.001 | 1.13 | 1.11 | 1.14 |
| Hispanic | 0.160 | 0.008 | 430 | <0.001 | 1.17 | 1.15 | 1.19 |
| Asian or Pacific islander | 0.136 | 0.013 | 110 | <0.001 | 1.15 | 1.12 | 1.18 |
| Native American | 0.098 | 0.028 | 12 | <0.001 | 1.08 | 1.00 | 1.15 |
| Year | |||||||
| 2009 (reference) | 1,568 | 1 | |||||
| 2010 | −0.080 | 0.008 | 106 | <0.001 | 0.95 | 0.93 | 0.96 |
| 2011 | −0.130 | 0.008 | 289 | <0.001 | 0.87 | 0.85 | 0.89 |
| 2012 | −0.212 | 0.007 | 810 | <0.001 | 0.83 | 0.82 | 0.84 |
| Socioeconomic status represented in quartiles, (%)* | |||||||
| Quartile 1 (reference) | 68 | 1 | |||||
| Quartile 2 | −0.038 | 0.006 | 36.4 | <0.001 | 0.96 | 0.95 | 0.97 |
| Quartile 3 | −0.050 | 0.006 | 60.13 | <0.001 | 0.95 | 0.94 | 0.96 |
| Quartile 4 | −0.029 | 0.007 | 20 | <0.001 | 0.97 | 0.96 | 0.98 |
| Type of hospital | |||||||
| Rural vs urban | 0.040 | 0.012 | 2,713 | <0.001 | 1.04 | 1.02 | 1.07 |
| Nonteaching vs teaching | −0.116 | 0.005 | 486 | <0.001 | 0.89 | 0.88 | 0.90 |
Healthcare Cost and Utilization Project’s National Inpatient Sample provides a quartile classification of the estimated median household income of residents in the patient's ZIP code. The quartiles are identified by values of 1 to 4, indicating the poorest (quartile 1) to wealthiest (quartile 4) populations. These values are derived from ZIP code-demographic data obtained from Claritas.
Adjustment covariates included in the regression analysis: indicator of sex, age in years at admission (revised), race (uniform), calendar year, median household income national quartile for patient ZIP code, Agency for Healthcare Research and Quality comorbidity measure: Diabetes, uncomplicated, Agency for Healthcare Research and Quality comorbidity measure: diabetes with chronic complications, all patient refined Diagnosis-Related-Group: risk for mortality subclass (Ordinal variable with 4 subclasses ranging from: 1, minor likelihood of dying, to 4, extreme likelihood of dying), Rural_Urban, NonTeach_Teach.
Discussion
In this retrospective analysis of the largest inpatient database in the United Sates, we showed that in-hospital mortality rate among patients hospitalized for severe ARF was significantly higher for all minorities (blacks, Hispanics, Native Americans, and Asian and Pacific Islanders) compared with non-Hispanic whites. We also found that among all racial groups, there has been a progressive decline in in-hospital mortality rate among patients hospitalized with severe ARF during the period from 2008 to 2012, yet the overall mortality remains unacceptably high.
Misclassification of ARDS has been cited as a major limitation of previous studies that employed large databases to explore racial disparities in mortality (6, 7, 9). In the current report, we used the largest nationwide database in the United States with information on important covariates to show association between racial minorities and increased mortality from severe ARF.
Our findings that blacks are at increased risk of mortality in severe ARF are in agreement with those of Moss and Mannino, who first described racial differences in ARDS mortality in the United States more than 20 years ago. In their analysis, they relied on entries from death certificates to identify cases of ARDS. The main racial comparison was between African-Americans and whites. African-American men as a group experienced the highest age-adjusted ARDS mortality rates (6). The analysis did not include other racial and ethnic groups, and the authors did not have the variables to adjust for possible confounders such as comorbidities and socioeconomic status that could explain a higher risk among blacks.
Our findings of increased mortality rates in severe ARF among Hispanics when compared with non-Hispanic whites is in agreement with previous findings (8, 9). We report for the first time that, when compared with non-Hispanic whites, Asians and Pacific Islanders, as well as Native Americans, have higher mortality rates from severe ARF. We also report a progressive decline in ARF-associated hospital mortality rates among all racial groups during the period from 2008 to 2012.
There are several potential explanations for the observed racial differences in mortality rates in our study. Blacks, Hispanics, Native Americans, or Asian and Pacific Islanders might have greater severity of illness at hospital admission, have higher levels of comorbidity, or present at an advanced stage of the disease process, as has been previously suggested. Additional factors may include genetic susceptibility, racial bias in the healthcare delivery system, or socioeconomic disparities including lack of insurance (1, 2, 4, 21–28). We attempted to accommodate these factors by adjusting for socioeconomic status, using median household income for patient ZIP code as a surrogate. However, given the limitations that are inherent to the retrospective analysis of large databases, we could not adjust for all possible confounders.
We found that Hispanics had the greatest odds of ARF-associated mortality rates when compared with non-Hispanic whites. It can be speculated that several possible factors are at play, including an increased risk among Hispanics, delay in the diagnosis as a result of late presentation to hospital, the effect of more severe comorbidities among Hispanics, or perhaps an increased genetic susceptibility. Language barrier has been shown as a predictor of worse health outcomes for chronic diseases in the outpatient setting (29). However, such would less likely be the case in the intensive care unit setting.
Strengths and Limitations
Our findings are strengthened by several factors. First, we used an algorithm that focused on identifying cases of severe ARF while excluding ARF because of asthma, COPD, or CHF exacerbation. With these strict exclusion criteria, we hoped to minimize misclassification of cases of severe ARF.
Although we analyzed a large nationally representative database to examine the racial differences in mortality rates, our study has important limitations. Our analysis was limited by the constraints of ICD-9-CM coding in the HCUP-NIS database. In a large database such as the HCUP-NIS, accuracy of ICD-9-CM coding is very important for the identification of patients and disease diagnosis. Several studies have shown that factors such as variations in billing, physician documentation, and practices influence accurate assignments of ICD-9-CM codes (16–18). This presents a specific challenge in capturing hospitalizations for specific forms of respiratory failure such as ARDS. Therefore, in our analysis, there was a possibility of disease misclassification with inclusion of other rare causes of ARF, such as acute pulmonary embolism. However, we attempted to minimize this by capturing only those patients who were intubated and mechanically ventilated for acute respiratory failure with sepsis and septic shock, and excluding cases coded as acute asthma exacerbation, acute COPD exacerbation, or acute CHF exacerbation. The strict algorithm used to define severe ARF in our analysis might explain the high overall inpatient mortality rate observed when compared with other studies (19, 20). The higher-than-expected mortality rate indicates that we are indeed capturing severe cases of ARF.
Another important limitation is that the HCUP-NIS database does not include variables that would enable us to estimate the racial differences in the risk of developing ARF. It is possible that we might be identifying the racial differences associated with conditions such as pneumonia that are known to cause ARF. In the HCUP-NIS database, each hospitalization is treated as a separate observation without the possibility of identifying readmissions. However, unlike diseases such as asthma, COPD, or CHF, which are characterized by frequent acute exacerbations that might require recurrent admissions, the course of severe ARF is such that recurrent hospitalizations for the same individual, although possible, are less likely. Despite these limitations, the use of a large, nationally representative database allows for generation of estimates that are more accurate and easily generalizable.
Conclusions
We have shown that when compared with non-Hispanic whites, blacks, Hispanics, and other racial minorities in the United States have significantly higher mortality rates from severe ARF. Large-scale prospective studies are needed to better understand the genetic and nongenetic factors that might underlie such observed racial and ethnic differences in severe ARF.
Supplementary Material
Acknowledgments
Acknowledgment
The authors thank the HCUP Data Partners in the following states who contribute to HCUP: Alaska, Arizona, Arkansas, California, Colorado, Connecticut, District of Columbia, Florida, Georgia, Hawaii, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Missouri, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, South Dakota, Tennessee, Texas, Utah, Vermont, Virginia, Washington, West Virginia, Wisconsin, Wyoming.
Footnotes
Supported by the University of Arizona Health Sciences Career Development Grant.
Author Contributions: All authors listed participated in the conception or design of the manuscript, acquired the data, drafted the analysis plan, and performed analysis and interpretation of the data, and drafted and revised the manuscript and approved the final version of manuscript.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Frieden TR Centers for Disease Control and Prevention (CDC) CDC health disparities and inequalities report: United States, 2013: foreword. MMWR Suppl. 2013;62:1–2. [PubMed] [Google Scholar]
- 2.Barnes KC. Genetic determinants and ethnic disparities in sepsis-associated acute lung injury. Proc Am Thorac Soc. 2005;2(3):195–201. doi: 10.1513/pats.200502-013AC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elixhauser A, Friedman B, Stranges E Septicemia in US Hospitals, 2009. HCUP Statistical Brief 122. Rockville, MD: Agency for Healthcare Research and Quality; 2011. [PubMed] [Google Scholar]
- 4.Stefan MS, Shieh MS, Pekow PS, Rothberg MB, Steingrub JS, Lagu T, Lindenauer PK. Epidemiology and outcomes of acute respiratory failure in the United States, 2001 to 2009: a national survey. J Hosp Med. 2013;8:76–82. doi: 10.1002/jhm.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cochi SE, Kempker JA, Annangi S, Kramer MR, Martin GS. Mortality trends of acute respiratory distress syndrome in the united states from 1999 to 2013. Ann Am Thorac Soc. 2016;13:1742–1751. doi: 10.1513/AnnalsATS.201512-841OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moss M, Mannino DM. Race and gender differences in acute respiratory distress syndrome deaths in the United States: an analysis of multiple-cause mortality data (1979-1996) Crit Care Med. 2002;30:1679–1685. doi: 10.1097/00003246-200208000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Cooke CR, Erickson SE, Eisner MD, Martin GS. Trends in the incidence of noncardiogenic acute respiratory failure: the role of race. Crit Care Med. 2012;40:1532–1538. doi: 10.1097/CCM.0b013e31824518f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Erickson SE, Shlipak MG, Martin GS, Wheeler AP, Ancukiewicz M, Matthay MA, Eisner MD National Institutes of Health National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome Network. Racial and ethnic disparities in mortality from acute lung injury. Crit Care Med. 2009;37:1–6. doi: 10.1097/CCM.0b013e31819292ea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lemos-Filho LB, Mikkelsen ME, Martin GS, Dabbagh O, Adesanya A, Gentile N, Esper A, Gajic O, Gong MN US Critical Illness and Injury Trials Group: Lung Injury Prevention Study Investigators (USCIITG-LIPS ) Sex, race, and the development of acute lung injury. Chest. 2013;143:901–909. doi: 10.1378/chest.12-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brown LM, Kallet RH, Matthay MA, Dicker RA. The influence of race on the development of acute lung injury in trauma patients. Am J Surg. 2011;201:486–491. doi: 10.1016/j.amjsurg.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moore JX, Donnelly JP, Griffin R, Safford MM, Howard G, Baddley J, Wang HE. Black-white racial disparities in sepsis: a prospective analysis of the Reasons for Geographic and Racial Differences In Stroke (REGARDS) cohort. Crit Care. 2015;19:279. doi: 10.1186/s13054-015-0992-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barnato AE, Alexander SL, Linde-Zwirble WT, Angus DC . Racial variation in the incidence, care, and outcomes of severe sepsis: analysis of population, patient, and hospital characteristics. Am J Respir Crit Care Med. 2008;177:279–284. doi: 10.1164/rccm.200703-480OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sakhuja A, Kumar G, Gupta S, Mittal T, Taneja A, Nanchal RS. Acute kidney injury requiring dialysis in severe sepsis. Am J Respir Crit Care Med. 2015;192:951–957. doi: 10.1164/rccm.201502-0329OC. [DOI] [PubMed] [Google Scholar]
- 14.Reynolds HN, McCunn M, Borg U, Habashi N, Cottingham C, Bar-Lavi Y. Acute respiratory distress syndrome: estimated incidence and mortality rate in a 5 million-person population base. Crit Care. 1998;2:29–34. doi: 10.1186/cc121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barrett M, Hickey K, Coffey R, Levit K.Population denominator data for use with the HCUP databases (updated with 2014 Population Data). HCUP Methods Series Report #2015-07 ONLINE. September 1, 2015. Rockville, MD: U.S. Agency for Healthcare Research and Quality; 2015 [accessed 2016 Aug 30]. Available from: http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp
- 16.Hsia DC, Krushat WM, Fagan AB, Tebbutt JA, Kusserow RP. Accuracy of diagnostic coding for Medicare patients under the prospective-payment system. N Engl J Med. 1988;318:352–355. doi: 10.1056/NEJM198802113180604. [DOI] [PubMed] [Google Scholar]
- 17.Howard AE, Courtney-Shapiro C, Kelso LA, Goltz M, Morris PE. Comparison of 3 methods of detecting acute respiratory distress syndrome: clinical screening, chartreview, and diagnostic coding. Am J Crit Care. 2004;13:59–64. [PubMed] [Google Scholar]
- 18.Rubenfeld GDCE, Steinberg LD, Hudson LD. ICD-9 codes do not accurately identify patients with the acute respiratory distress syndrome (ARDS) [abstract] Am J Respir Crit Care Med. 1998;157:A680. [Google Scholar]
- 19.Zambon M, Vincent JL. Mortality rates for patients with acute lung injury/ARDS have decreased over time. Chest. 2008;133:1120–1127. doi: 10.1378/chest.07-2134. [DOI] [PubMed] [Google Scholar]
- 20.Zambon M, Monti G, Landoni G. Outcome of patients with acute respiratory distress syndrome: causes of death, survival rates and long-term implications. In: Vincent J-L, editor. Annual update in intensive care and emergency medicine 2014. New York: Springer International Publishing; 2014. pp. 245–253. [Google Scholar]
- 21.Kirkpatrick P, Dransfield MT. Racial and sex differences in chronic obstructive pulmonary disease susceptibility, diagnosis, and treatment. Curr Opin Pulm Med. 2009;15:100–104. doi: 10.1097/MCP.0b013e3283232825. [DOI] [PubMed] [Google Scholar]
- 22.Marshall RP, Webb S, Bellingan GJ, Montgomery HE, Chaudhari B, McAnulty RJ, Humphries SE, Hill MR, Laurent GJ. Angiotensin converting enzyme insertion/deletion polymorphism is associated with susceptibility and outcome in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2002;166:646–650. doi: 10.1164/rccm.2108086. [DOI] [PubMed] [Google Scholar]
- 23.Garcia JGN, Sznajder JI. Healthcare disparities in patients with acute respiratory distress syndrome: toward equity. Am J Respir Crit Care Med. 2013;188:631–632. doi: 10.1164/rccm.201307-1394ED. [DOI] [PubMed] [Google Scholar]
- 24.Gao L, Grant A, Halder I, Brower R, Sevransky J, Maloney JP, Moss M, Shanholtz C, Yates CR, Meduri GU, et al. Novel polymorphisms in the myosin light chain kinase gene confer risk for acute lung injury. Am J Respir Cell Mol Biol. 2006;34:487–495. doi: 10.1165/rcmb.2005-0404OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Garcia JG, Moreno Vinasco L. Genomic insights into acute inflammatory lung injury. Am J Physiol Lung Cell Mol Physiol. 2006;291:L1113–L1117. doi: 10.1152/ajplung.00266.2006. [DOI] [PubMed] [Google Scholar]
- 26.Williams DR, Wyatt R. Racial bias in health care and health: challenges and opportunities. JAMA. 2015;314:555–556. doi: 10.1001/jama.2015.9260. [DOI] [PubMed] [Google Scholar]
- 27.Danis M, Linde-Zwirble WT, Astor A, Lidicker JR, Angus DC. How does lack of insurance affect use of intensive care?: a population-based study. Crit Care Med. 2006;34:2043–2048. doi: 10.1097/01.CCM.0000227657.75270.C4. [DOI] [PubMed] [Google Scholar]
- 28.Fowler RA, Noyahr LA, Thornton JD, Pinto R, Kahn JM, Adhikari NK, Dodek PM, Khan NA, Kalb T, Hill A, et al. American Thoracic Society Disparities in Healthcare Group. An official American Thoracic Society systematic review: the association between health insurance status and access, care delivery, and outcomes for patients who are critically ill. Am J Respir Crit Care Med. 2010;181:1003–1011. doi: 10.1164/rccm.200902-0281ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pérez-Stable EJ, Nápoles-Springer A, Miramontes JM. The effects of ethnicity and language on medical outcomes of patients with hypertension or diabetes. Med Care. 1997;35:1212–1219. doi: 10.1097/00005650-199712000-00005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.