Abstract
Accurate diagnosis and management of a femoral vascular injury is important as it is a life-threatening injury with high morbidity and mortality. This is the case of a 75-year-old man admitted to the emergency room with trauma to the right groin due to a horse fall. Computed tomography showed active bleeding of the femoral artery without pelvic or femoral fracture. We inserted a stent-graft, but hypotension persisted. Exploration of the groin was completed, and the bleeding from the external iliac vein was identified and repaired. In conclusion, vascular injury is rare in groin trauma without associated fracture, however, arterial and venous injury should not be completely ruled out. Endovascular therapy is worth recommending as a quicker and safer management than surgery in patients with active bleeding in the femoral artery. However, the possibility of combined injury of the femoral vein should be suspected in case of ongoing hemodynamic instability.
Keywords: Femoral artery, Iliac vein, Nonpenetrating injuries, Endovascular procedures, Groin
INTRODUCTION
Accurate diagnosis and treatment of vascular injuries in the extremities are important as they can lead to limb loss and death if not properly managed [1]. Wolma et al. [2] reported that after arterial injury, the limb amputation rate was 50% when treatment was delayed for more than 6 hours while it was less than 6% within 6 hours. Femoral artery injury usually occurs due to a penetrating injury or a blunt trauma with an associated fracture of the pelvis or femur [3,4]. Blunt vascular trauma involving the extremity is relatively rare [5]. Patients with isolated vascular injuries have a higher limb salvage rate than those with associated bone fractures [6]. This blunt injury without fracture was first described as the motor-scooter handlebar syndrome in 1968 and was presumed to be due to compression of the artery by the inguinal ligament [7]. We describe a blunt trauma with simultaneous injury of the external pudendal artery (EPA), a branch of common femoral artery (CFA), and external iliac vein (EIV) sustained by horse fall.
CASE
A 75-year-old man presented at the emergency room shortly after he sustained an injury from a horse fall. When he fell, the horse lost balance and fell on him, crushing his groin. His past history showed he was diabetic. His heart rate (HR) was 90 beats/min and blood pressure (BP) was 50/0 mmHg. Bruising, swelling, and distention were seen in the right groin on inspection. A large pulsatile hematoma in the right groin was palpated. There was a right lower quadrant tenderness, and no rebound tenderness or guarding (Fig. 1). The ankle pulses were palpable and there were no edema and ischemic changes in the lower extremities. His hemoglobin level was 10.2 g/dL on admission but decreased 1 hour later to 6.7 g/dL. After rapid transfusion of five units of packed red blood cells (RBCs) and five units of fresh frozen plasma (FFP) through a central venous catheter, his vital signs stabilized. His BP was 95/50 mmHg and his HR was 90 beats/min. An emergency computed tomography angiogram showed a hematoma in the right inguinal and femoral region, and active bleeding of the iliac or femoral artery was confirmed. There were no accompanying fractures of the pelvis or lower extremities (Fig. 2).
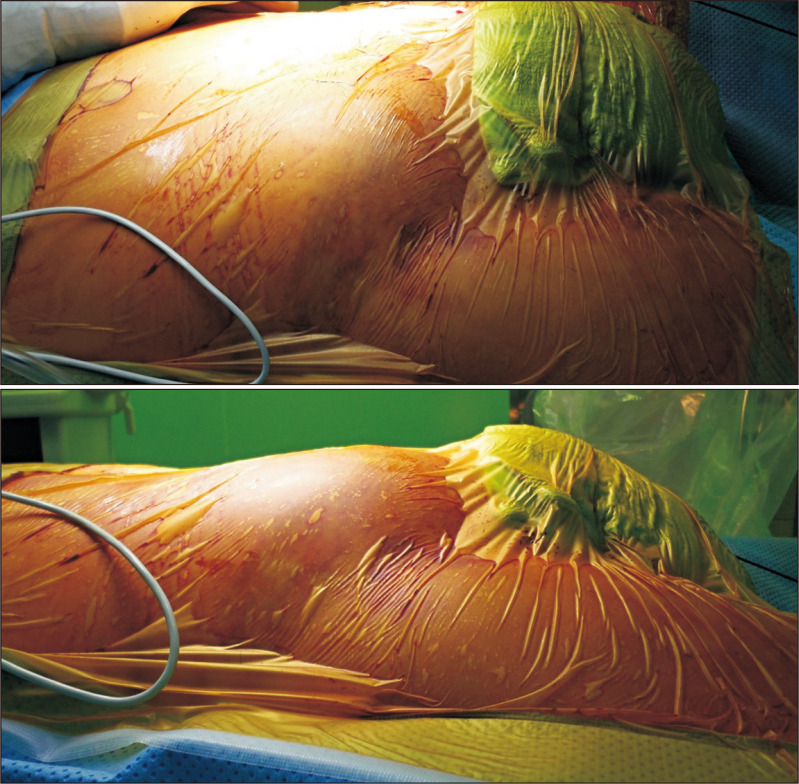
Fig. 1.
On the operating table before surgery, severe swelling was seen in the right lower abdomen and groin.
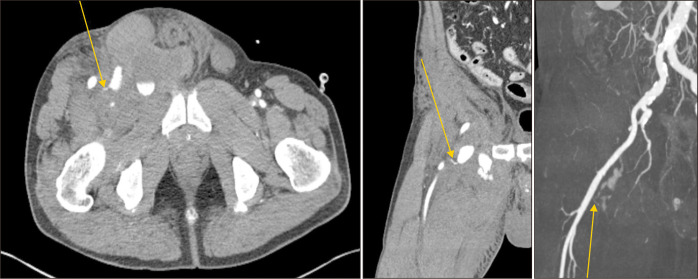
Fig. 2.
Preoperative computed tomography angiography (axial, coronal and maximal intensity projection view): Orange arrows indicate active bleeding from external pudendal artery, a branch of common femoral artery.
We determined that it would be difficult to access the injury site and secure the field during open surgery due to severe swelling and hematoma. If it took a lot of time to access the surgical site, the patient’s chances of resuscitation would be expected low. Therefore, we decided to perform an emergent endovascular procedure for rapid hemostasis under general anesthesia with C-arm. We directly punctured the left CFA and inserted a catheter to the right external iliac artery in a crossover approach. Active bleeding of the iliac artery was not seen on the intraoperative angiogram, but extravasation of the contrast media was confirmed in the femoral artery. The rupture site was the EPA, below the inguinal ligament, and quite above the bifurcation of superficial femoral artery and deep femoral artery. The rupture site was covered with an 8×50 mm Viabahn® stent-graft (W.L. Gore & Associates, Inc., Flagstaff, AZ, USA) (Fig. 3). The final angiography confirmed that there was no more bleeding from the artery, and blood flow to the right lower extremity was not disrupted.
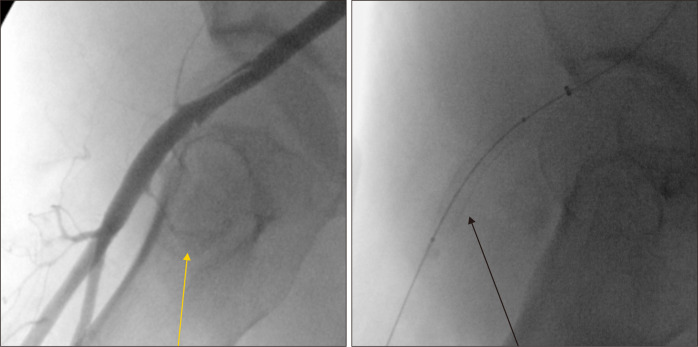
Fig. 3.
Angiography before and after deployment of the Viabahn® stent-graft: Orange arrow indicates active bleeding from external pudendal artery. Black arrow on the right indicates Viabahn® stent-graft and active bleeding is not visible.
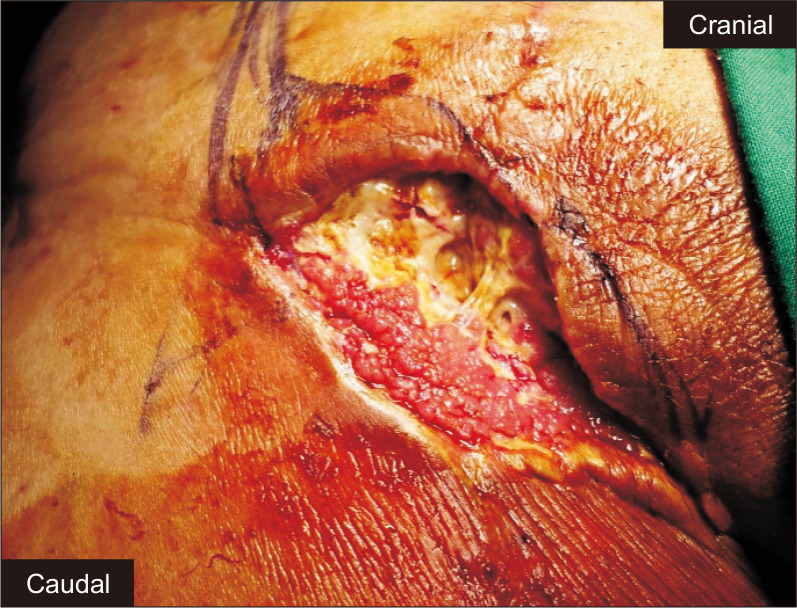
After removing of the endovascular device and compressing the puncture site for hemostasis, BP decreased to 70/35 mmHg and did not rise thereafter. After rapid transfusion of 3 units of RBCs and 1 unit of FFP through the Fluid Management System (Model 2516 universal 3-Spike disposable set; Belmont Inst., Billerica, MA, USA), BP rose to 110/50 mmHg. Bleeding from other sites was suspected; therefore, we performed a longitudinal incision and explored the right inguinal area. A 3-mm defect was found on the anterior wall of EIV above the right inguinal ligament. And a primary repair was performed with a prolene suture 5-0 (Fig. 4). Minor bleeding was controlled, a 200 mL Jackson-Pratt drain was inserted, and the incision was closed. The patient was then moved to the intensive care unit. Dual antiplatelet therapy (aspirin and clopidogrel) were started on the 10th day postoperatively, when the bleeding tendency decreased and disseminate intravascular coagulation improved.
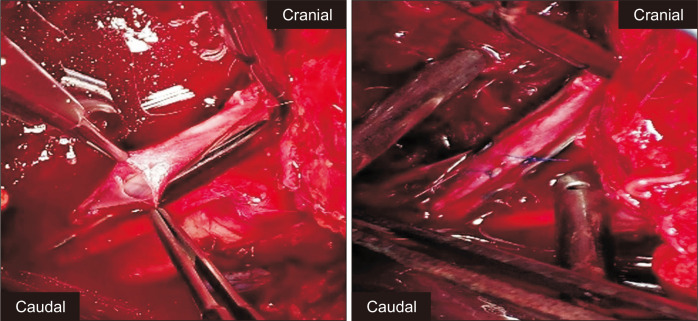
Fig. 4.
Laceration of the external iliac vein above the right inguinal ligament was confirmed, and primary repair was performed with prolene suture 5-0.
During the second postoperative month, pulmonary edema developed, and a non-ST-elevation myocardial infarction was diagnosed. A percutaneous coronary intervention was done, and a coronary stent was placed. There was repeated surgical site infection by staphylococcus epidermidis, a skin flora at the groin, and it was improved by intravenous administration of vancomycin. Wound debridement and skin grafts were performed twice (Fig. 5). As the inguinal wound improved, the patient was discharged 94 days after surgery. He has been continually monitored through the outpatient clinic, and 71 months after the deployment of the Viabahn® stent-graft, it is still patent (Fig. 6).
Fig. 5.
After two months after the first surgery, surgical site at right groin remained unhealed due to surgical site infection.
Fig. 6.
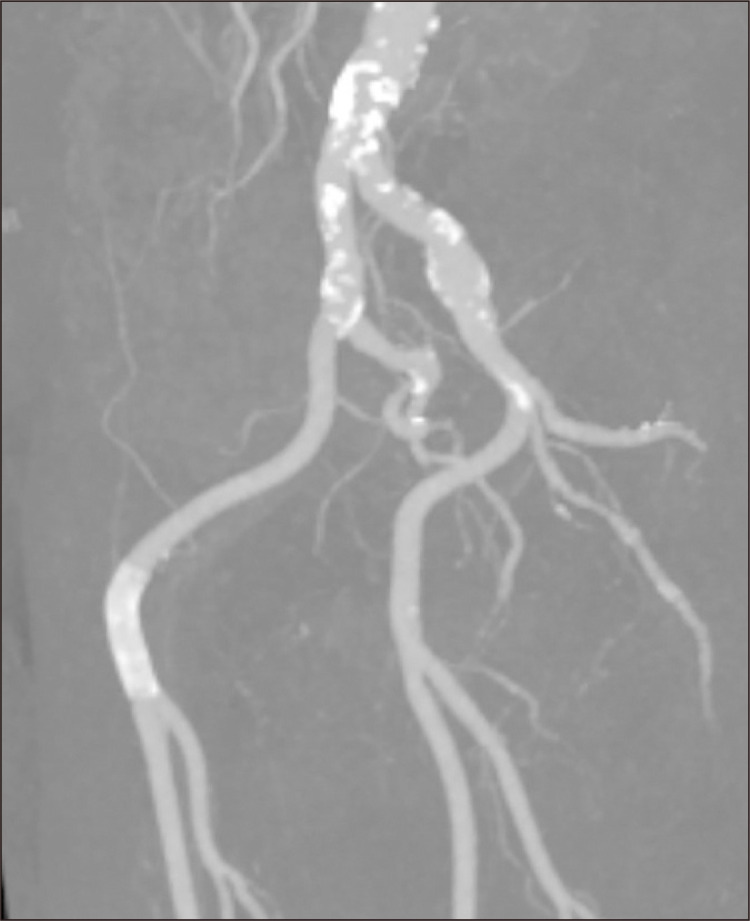
Follow-up computed tomography angiogram after 6 years showed the patency of the Viabahn® stent-graft.
DISCUSSION
Major vascular damage from abdominal trauma can have fatal outcomes and if not properly treated, it can lead to massive bleeding and death. Injuries to the external iliac vessel and common femoral vessel rarely occur after a blunt lower abdominal trauma [8]. In two large series of arterial injuries, the reported incidence of arterial injuries after blunt trauma was 6% [9] and 16% [10] of all vascular trauma. The incidence of femoral artery injury was 2% to 8% [3]. CFA injury following blunt trauma was reported as <1% to 2.2% [11].
Isolated vascular lesions, as in our case, are described as the motor-scooter handlebar syndrome. The CFA is a superficial vessel between the inguinal ligament and the superior pubic ramus [12]. Two types of injuries are hypothesized; one caused by a rapid deceleration of opposed forces on vessels [13] and the other caused by direct forceful compression of the relatively immobile vessels on the pubic ramus [3]. In our case, there was no calcified lesion in CFA, and it can be assumed that the EPA compressed between the femur head and the compression site was injured.
In our case, the patient suffered simultaneous injury to the EPA and EIV as the horse collapsed on him. The incidence of such a presentation is low and could delay the diagnosis. Therefore, a high index of suspicion is necessary to diagnose blunt vascular trauma in the extremity. A thorough history including the mechanism of injury and a physical examination should be performed [14]. Arterial bleeding was expected due to a sudden drop in BP and swelling of the inguinal area. Because cases of venous bleeding are rare, we misdiagnosed it as less likely and not evaluated for venous injury. If the possibility of vein injury had been recognized, it would have been better to evaluate through duplex ultrasonography.
Open surgical repair has been the standard management for peripheral vascular injuries. However, as endovascular treatment has become more refined, it has been increasingly used to treat patients with trauma-related vascular injuries [15]. There are various methods of endovascular interventions including temporary vascular control with a balloon, embolization of a bleeding vessel, and covered stent repair of an injury. Endovascular management has several advantages. First, it helps make an access possible to injured vessels in difficult anatomic areas to approach. Second, it reduces the risk of injury to nearby nerves and alleviates the need for surgically traversing already injured or sometimes necrotic tissues. Finally, patients have a decreased operation time, reduced blood loss, and decreased mortality when compared with open surgical repair of similar injuries [14-16]. Particularly, covered stents are an attractive option for the management of peripheral arterial injury in areas that are difficult to expose surgically. A series of 62 patients with upper and lower extremity arterial trauma treated with a covered stent was reported by White et al. [17]. The 1-year primary patency rates for stents in the iliac artery and femoral artery were 76% and 86%, respectively. They found that the use of covered stents significantly reduced ischemia and operative time. However, there are several disadvantages. Devices such as stent grafts suitable for the patient’s anatomy should be provided. Acute renal failure due to hypovolemia can be exacerbated by contrast media. If endovascular procedure fails, additional procedures or surgery may be required. There is a high risk of prosthetic graft infection.
In our case, the rupture site of the CFA was treated with an 8×50 mm Viabahn® stent-graft, which is patent for 6 years. Given these rationales and experience, endovascular interventions are worth considering in the management of trauma-related peripheral vascular injury.
Venous repair is one of the most controversial subjects related to the management of combined arterial and venous injuries [18]. Combined injuries to the femoral artery and vein can be extremely difficult to manage because of the difficulty in obtaining control of the vein and its tributaries in the femoral triangle [19]. In the case of lower extremity venous injury, ligation is better tolerated and more common than arterial ligation. However, in these dual vascular injuries, there is an increased extremity loss when there is inadequate venous drainage. Therefore, venous repair is preferred to ligation [20]. Venous repair has several benefits. First, the patency of associated arterial repairs is improved because preserved venous patency maintains normal vascular resistance; thus, optimizing blood flow and reducing congestion. Second, it reduces the incidence of chronic venous insufficiency and postphlebitic syndrome [19]. We performed a primary repair for the injured EIV. There were no symptoms of venous insufficiency such as edema of the lower extremities. He recovered without venous complications such as venous insufficiency and deep vein thrombosis.
This case presentation sends a message about the following considerations. First, though vascular injury is rare in groin trauma without associated fractures, clinicians should consider it as a differential diagnosis in patients with such presentations. Second, though arterial injury in groin trauma is more common, venous injury should not be completely ruled out. Third, venous repair should be preferred to ligation for combined femoral arterial and venous injuries. Finally, endovascular therapy is worth recommending as a quicker and safer management than surgery in patients with active bleeding in the femoral artery [14,17]. It can stabilize patients and prevent complications that can lead to death.
Footnotes
CONFLICTS OF INTEREST
The authors have nothing to disclose.
AUTHOR CONTRIBUTIONS
Concept and design: SSL, SKK. Analysis and interpretation: DHK, WGC. Data collection: JHM, JHP. Writing the article: JHM, JHP. Critical revision of the article: DHK, SKK, WGC. Final approval of the article: all authors. Statistical analysis: none. Obtained funding: none. Overall responsibility: SSL, JHP.
REFERENCES
- 1.Kim HY, Park JH, Kim MY, Hwang SW. Management of vascular injuries to the extremities after trauma. Korean J Thorac Cardiovasc Surg. 2009;42:46–52. doi: 10.1136/tsaco-2020-000486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wolma FJ, Larrieu AJ, Alsop GC. Arterial injuries of the legs associated with fractures and dislocations. Am J Surg. 1980;140:806–809. doi: 10.1016/0002-9610(80)90122-1. [DOI] [PubMed] [Google Scholar]
- 3.Chadha M, Balain B, Dhal A, Kumar S, Arora A. Isolated, closed rupture of the common femoral artery resulting from blunt trauma. Arch Orthop Trauma Surg. 2003;123:245–246. doi: 10.1007/s00402-003-0504-1. [DOI] [PubMed] [Google Scholar]
- 4.Suliman A, Ali MW, Kansal N, Tian Y, Angle N, Coimbra R. Complete femoral artery and vein avulsion from a hyperextension injury: a case report and literature review. Ann Vasc Surg. 2009;23:411.e9–411.e15. doi: 10.1016/j.avsg.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 5.Paling AJ, Viersma JH. Blunt trauma of the common femoral artery. J Pediatr Surg. 1999;34:1557–1558. doi: 10.1016/S0022-3468(99)90130-6. [DOI] [PubMed] [Google Scholar]
- 6.Kohli A, Singh G. Management of extremity vascular trauma: Jammu experience. Asian Cardiovasc Thorac Ann. 2008;16:212–214. doi: 10.1177/021849230801600307. [DOI] [PubMed] [Google Scholar]
- 7.Deutsch V, Sinkover A, Bank H. The motor-scooter-handlebar syndrome. Lancet. 1968;2:1051–1053. doi: 10.1016/S0140-6736(68)91527-4. [DOI] [PubMed] [Google Scholar]
- 8.Muck PE, Nunez TC, Hruska L, Kasper GC, Chang CK, Welling RE. Blunt injury to the external iliac artery: a case report. Am Surg. 2002;68:11–14. [PubMed] [Google Scholar]
- 9.Morris GC, Jr, Beall AC, Jr, Roof WR, De Bakey ME. Surgical experience with 220 acute arterial injuries in civilian practice. Am J Surg. 1960;99:775–781. doi: 10.1016/0002-9610(60)90028-3. https://doi.org/10.1016/0002-9610(60)90028-3 . [DOI] [Google Scholar]
- 10.Bole PV, Purdy RT, Munda RT, Moallem S, Devanesan J, Clauss RH. Civilian arterial injuries. Ann Surg. 1976;183:13–23. doi: 10.1097/00000658-197601000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martin LC, McKenney MG, Sosa JL, Ginzburg E, Puente I, Sleeman D, et al. Management of lower extremity arterial trauma. J Trauma. 1994;37:591–598. doi: 10.1097/00005373-199410000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Sarfati MR, Galt SW, Treiman GS, Kraiss LW. Common femoral artery injury secondary to bicycle handlebar trauma. J Vasc Surg. 2002;35:589–591. doi: 10.1067/mva.2002.118811. [DOI] [PubMed] [Google Scholar]
- 13.Milas ZL, Dodson TF, Ricketts RR. Pediatric blunt trauma resulting in major arterial injuries. Am Surg. 2004;70:443–447. [PubMed] [Google Scholar]
- 14.Doody O, Given MF, Lyon SM. Extremities--indications and techniques for treatment of extremity vascular injuries. Injury. 2008;39:1295–1303. doi: 10.1016/j.injury.2008.02.043. [DOI] [PubMed] [Google Scholar]
- 15.Branco BC, DuBose JJ, Zhan LX, Hughes JD, Goshima KR, Rhee P, et al. Trends and outcomes of endovascular therapy in the management of civilian vascular injuries. J Vasc Surg. 2014;60:1297–1307.e1. doi: 10.1016/j.jvs.2014.05.028. [DOI] [PubMed] [Google Scholar]
- 16.Alam HB, DiMusto PD. Management of lower extremity vascular trauma. Curr Trauma Rep. 2015;1:61–68. doi: 10.1007/s40719-014-0007-2. [DOI] [Google Scholar]
- 17.White R, Krajcer Z, Johnson M, Williams D, Bacharach M, O'Malley E. Results of a multicenter trial for the treatment of traumatic vascular injury with a covered stent. J Trauma. 2006;60:1189–1195. doi: 10.1097/01.ta.0000220372.85575.e2. [DOI] [PubMed] [Google Scholar]
- 18.Hafez HM, Woolgar J, Robbs JV. Lower extremity arterial injury: results of 550 cases and review of risk factors associated with limb loss. J Vasc Surg. 2001;33:1212–1219. doi: 10.1067/mva.2001.113982. [DOI] [PubMed] [Google Scholar]
- 19.Carrillo EH, Spain DA, Miller FB, Richardson JD. Femoral vessel injuries. Surg Clin North Am. 2002;82:49–65. doi: 10.1016/S0039-6109(03)00140-3. [DOI] [PubMed] [Google Scholar]
- 20.Bilgen S, Türkmen N, Eren B, Fedakar R. Peripheral vascular injury-related deaths. Ulus Travma Acil Cerrahi Derg. 2009;15:357–361. [PubMed] [Google Scholar]