Background.
Acute kidney injury (AKI) is a common complication after lung transplant (LTx), and continuous renal replacement therapy (CRRT) is increasingly of use to critically ill patients who have developed AKI. However, the optimal timing or threshold of kidney impairment for which to commence CRRT after LTx has been uncertain. There has also been limited information on the impact of CRRT among LTx recipients (LTRs) introduced in the early posttransplant period on survival, graft function, and renal function. We aimed to review LTRs who developed AKI requiring CRRT postoperatively and followed their long-term outcomes at Tohoku University Hospital (TUH).
Methods.
Medical records of consecutive patients who underwent LTx at TUH between 2000 and 2018 were reviewed, with follow-up to 2019 inclusive.
Results.
Although mortality in those who required CRRT (n = 21) was increased versus those who did not require CRRT (n = 85)(P = 0.024), conditional survival beyond 3-month posttransplant was not affected (P = 0.131). Additionally, the cumulative incidence of chronic lung allograft rejection (P = 0.160) and the development of chronic kidney disease (P = 0.757) were not significant between groups.
Conclusions.
The initiation of CRRT posttransplant may be a useful strategy to preserve cardiac and optimize volume management among critically ill patients.
Lung transplant (LTx) can offer both a survival benefit and improved quality of life for selected patients with advanced lung disease. Nongraft complications after lung transplant can have considerable effects on the morbidity and mortality of recipients. Acute kidney injury (AKI) is a common posttransplant complication, with up to 65% of recipients experiencing at least 1 episode of AKI within the first 2 weeks after transplantation.1 Any episodes of posttransplant AKI have been associated with an increased risk of CKD and mortality in previous long-term observational studies.1 Renal replacement therapy (RRT) is increasingly of use to critically ill patients who have developed AKI,2 and continuous renal replacement therapy (CRRT) is favored in the intensive care unit setting rather than conventional intermittent hemodialysis (IHD) due to hemodynamic instability in most patients, especially LTR in the early postoperative period. However, the optimal timing or threshold of kidney impairment for which to commence RRT has been uncertain. There has also been limited information published on the benefit of CRRT among LTRs in the early posttransplant period, such as survival, graft function, and renal function. We aimed to review LTRs who developed AKI requiring CRRT postoperatively and followed their long-term outcomes in our facility.
MATERIALS AND METHODS
Study Design and Data Collection
Medical records of consecutive lung transplant recipients (LTRs) at Tohoku University Hospital (TUH) between January 1, 2000, and December 31, 2018, were retrospectively reviewed, with follow-up data collected up to December 31, 2019 inclusive. LTRs who received living-donor transplant were excluded from the study (Figure 1). Baseline data pretransplantation and peritransplantation were collected from all participants, and follow-up data were gathered at months 3, 6, 9, and annually posttransplant. The study protocol was reviewed by the Institutional Review Board at TUH on January 30, 2020. In light of the retrospective design, the requirement of informed consent was waived.
FIGURE 1.
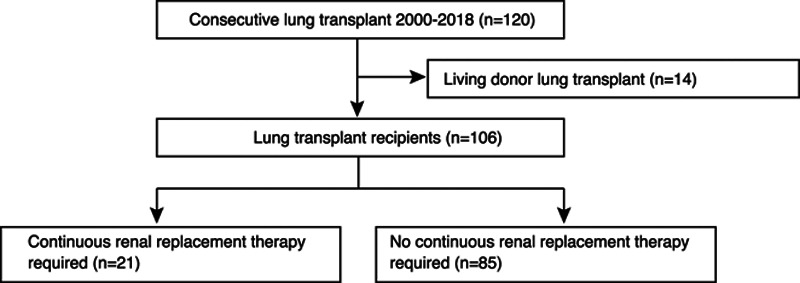
Study flowchart indicates inclusion of consecutive LTx recipients between January 2000 and December 2018 (n = 106) and further analyzed based on CRRT requirement (n = 21 vs 85). CRRT, continuous renal replacement therapy; LTx, lung transplant.
Definition of CKD and Chronic Lung Allograft Dysfunction
The glomerular filtration rate (GFR) was used as an index of global kidney function and estimated from a revised equation for serum creatinine-based estimated GFR in Japan as follows: 194 × serum creatinine (mg/dL) (−1.094) × age(−0.287) (×0.739 if female).3 AKI was defined by an increase in serum creatinine of ≥0.3 mg/dL within 48 hours or ≥1.5 times baseline, or urine output <0.5 mL/kg/h for 6 hours.4 CKD was defined as an irreversible decline in GFR <60 mL/min/1.73 m2, and severe CKD <30 mL/min/1.73 m2.5 chronic lung allograft dysfunction (CLAD) was defined as an irreversible decline in FEV1 to <80% from the baseline confirmed twice at least 3 weeks apart and at least 3 months posttransplant.6
Data Analysis
Differences across groups were reported with chi-square or Fisher’s exact tests for categoric variables and the Mann–Whitney test for continuous variables, as appropriate. The Kaplan–Meier analysis was used to model time-to-event outcomes, and differences between groups were calculated with the log-rank test. Risk factors for mortality were assessed using a Cox proportional hazards model. Variables associated with CRRT requirement in chi-square or Fisher’s exact tests (P < 0.05) and those with biological plausibility were analyzed in the univariable and multivariable model. Hazard ratios (HRs) were presented with their 95% confidence intervals (CIs). P values of <0.05 were considered statistically significant. Statistical analyses and graph generation were performed with GraphPad Prism 6.0 (GraphPad Software Inc., La Jolla, CA) or StatPlus:macLE (AnalystSoft Inc., Walnut, CA).
RESULTS
Characteristics of Lung Transplant Recipients at TUH
One hundred six patients who underwent LTx between 2000 and 2018 were included into the study (Table 1). Median age of LTRs was 45 [interquartile range (IQR) 34–51], and 67.3% were female. Single lung transplantation was performed more often than double lung transplantation at 56.7% versus 43.3%. Obstructive lung disease was the indication for 43.4% of LTx, followed by pulmonary arterial hypertension (PAH) at 20.8% and nonidiopathic pulmonary fibrosis interstitial pneumonia at 13.2%. There were 2 LTRs with pretransplant CKD and 7 with diabetes. The incidence of hypertension [systolic blood pressure (BP) ≥130 mm Hg, diastolic BP≥ 80 mm Hg or taking antihypertensive drugs at the time of transplant7] (16.3%, 17/106) and proteinuria through urinalysis5,8 (13.5%, 14/106) was reviewed. The median operation time was 521 minutes (IQR 383–842) and the median ischemic time of 525 minutes (IQR 438–688). The median survival of all participants was 58 months (IQR 20–84, n = 106), and for those who underwent LTx between 2000 and 2012, excluding recent transplants (2013–2018), the median survival was 91 months (IQR 26–116, n = 45).
TABLE 1.
Baseline characteristics of patients at the time of lung transplant (n = 106, A) and lung transplant recipients with/without CRRT implementation (n = 21 vs 85, respectively, B)
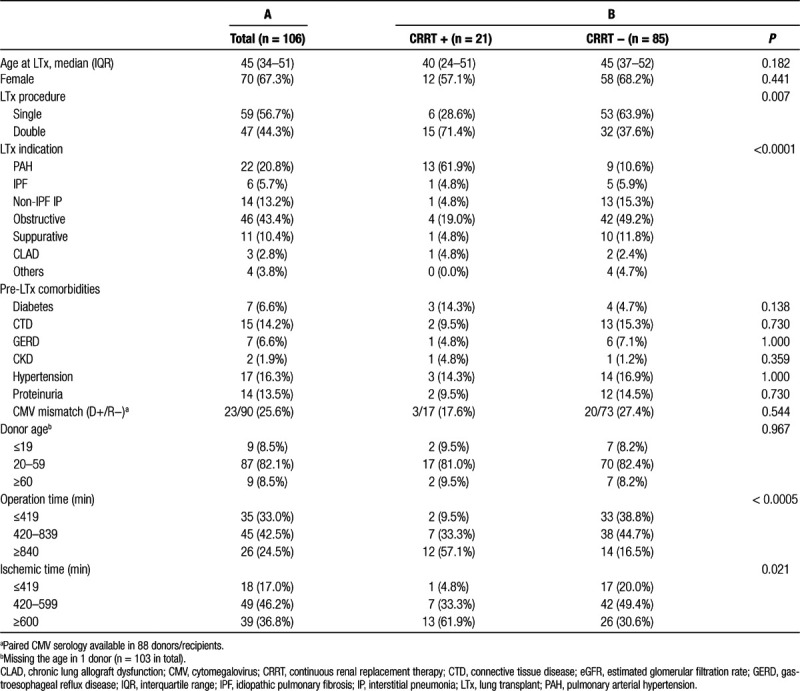
Twenty-one LTRs required CRRT (CRRT+), and 85 did not need CRRT (CRRT−) (Table 1B). The median age was not different at 40 (IQR 24–51) versus 45 (IQR 37–52) (P = 0.182), and there was no statistically significant difference in gender (P = 0.441) between categories. CRRT+ patients were more likely to have undergone double transplantation (71.4%) versus CRRT− (37.6%) (P = 0.007). Unsurprisingly, PAH was the most common indication for transplant in CRRT+ (61.9%), whereas obstructive lung disease was the most common indication in CRRT− (49.2%) (P < 0.0001). There was no significant difference in pretransplant comorbidities between groups. The proportion of CMV mismatch was also not different between groups (17.6% versus 27.4%, P = 0.544). Donor age in both CRRT+ and CRRT– showed a similar distribution (P = 0.967). The operation time in CRRT+ was longer than that of CRRT− (P < 0.0005), likely owing to the higher proportion of patients transplanted for PAH in CRRT+ patients. Total ischemic time in the majority of LTRs with CRRT+ was over 600 minutes, whereas that of CRRT− was significantly shorter (P = 0.021).
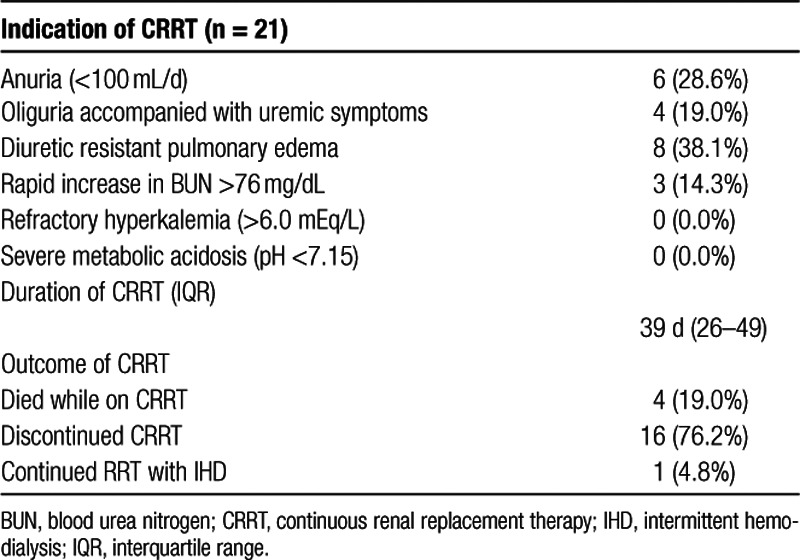
CRRT
During the observation period, 21 LTRs required CRRT postoperatively. Although optimal timing2 or consensus proposal to start CRRT9 has been documented in previous work, our indications for CRRT are summarized in Table 2. All LTRs requiring CRRT were critically ill postoperatively (unstable hemodynamic state and requiring mechanical ventilation support and tracheostomy). The major indications for CRRT were pulmonary edema resistant to diuretic therapy (38.1%), followed by anuria (28.6%) and oliguria accompanied with uremic symptoms (19.0%). No LTRs had hyperkalemia or acidemia as an indication for CRRT. The median duration of CRRT was 39 days (IQR 26–49). Among 21 LTRs treated with CRRT, 4 died while on CRRT, 16 successfully discontinued, and 1 switched from CRRT to IHD.
TABLE 2.
Potential indications for CRRT and the study outcomes of CCRT implemented after LTx (n = 21)
Postoperative Outcomes in Patients Requiring CRRT After LTx
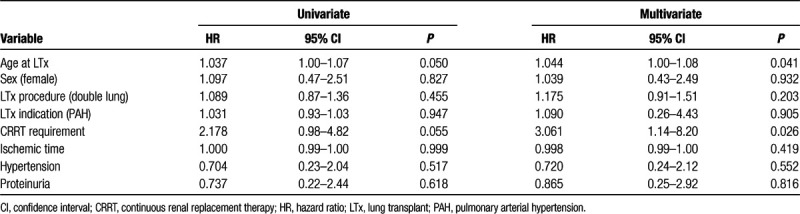
LTRs who required CRRT perioperatively demonstrated lower survival than those who were not on CRRT (Log-rank P = 0.024) (Figure 2A). However, there were likely other factors affecting mortality in the early postoperative phase for CRRT+ patients, because LTRs on CRRT are generally critically ill. Because of this, conditional survival beyond 3-month posttransplant was also analyzed (Figure 2B), illustrating that CRRT requirement was not associated with long-term mortality (Log-rank P = 0.131). Other risk factors for mortality after LTx were analyzed in a univariate Cox model (Table 3), showing only an age at the time of transplant was associated with mortality (HR: 1.037, 95% CI: 1.00-1.07). Both age and CRRT requirement were associated with mortality in the multivariate Cox analysis (HR: 1.044, 95% CI: 1.00-1.08 and HR: 3.061, 95% CI: 1.42-8.20, respectively). The LTx procedure (double lung versus single transplant) and LTx indication (PAH versus others) were not associated with an increased risk of mortality (Table 3).
FIGURE 2.
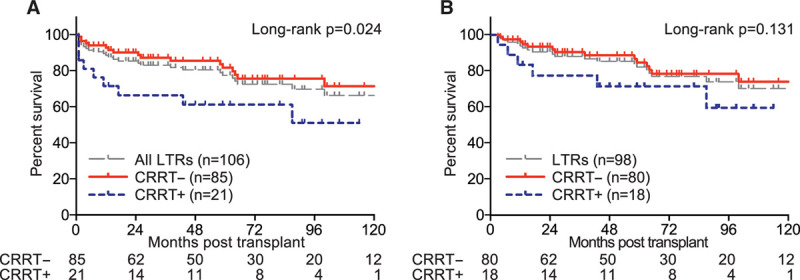
A, Kaplan–Meier survival stratified by the posttransplant CRRT requirement (CRRT+ n = 21 with solid line in blue, CRRT– n = 83 with dashed line in red and all participants n = 106 with dashed line in gray) is shown by months after transplantation. The number of patients at risk is documented according to time. B, Kaplan–Meier conditional survival beyond 3-mo posttransplant survival stratified by the posttransplant CRRT requirement (CRRT+ n = 18 with solid line in blue, CRRT– n = 80 with dashed line in red and all participants with dashed line in gray) is illustrated by months after transplantation. CRRT, continuous renal replacement therapy.
TABLE 3.
Hazard ratios for mortality from univariate and multivariate Cox model
Graft function posttransplant was reviewed, and the cumulative incidence of CLAD was analyzed (Figure 3A). There was no difference in the incidence of CLAD among patients with or without CRRT implementation (Log-rank P = 0.160). The use of CRRT in the acute posttransplant phase was not associated with the development of any severity of CKD (Log-rank P = 0.757) (Figure 3B). In addition, postoperative CRRT was also not associated with the development of severe CKD (Log-rank P = 0.642) (Figure 3C). Among LTRs who developed severe CKD, IHD was commenced in 3 LTRs, including 1 patient in the CRRT+ group (2 mo post-LTx, transitioned from CRRT) and 2 patients in the CRRT− category (5 and 9 y post-LTx, respectively).
FIGURE 3.
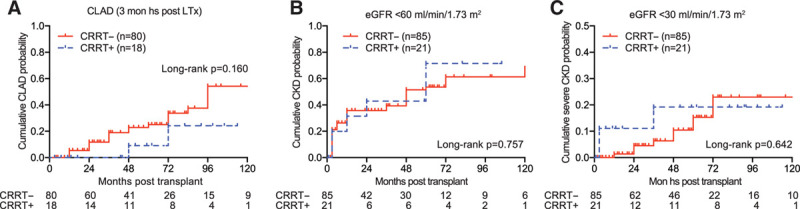
A, The cumulative incidence of CLAD stratified by the posttransplant CRRT requirement (+ n = 18, solid line in blue vs – n = 80, dashed line in red) is shown by months after transplantation. LTRs that survived over 3 mo posttransplantation were reviewed. The number of patients at risk is documented according to time. B, The cumulative incidence of CKD, defined by irreversible decline in GFR <60 mL/min/1.73 m2, is illustrated to see the impact of the posttransplant CRRT requirement (+ n = 21, solid line in blue vs – n = 83, dashed line in red) based on months after transplantation. C, The cumulative incidence of severe CKD, defined by irreversible decline in <30 mL/min/1.73 m2, is shown to see the impact of the posttransplant CRRT requirement (+ n = 21, solid line in blue vs – n = 83, dashed line in red) based on months after transplantation. CKD, chronic kidney disease; CLAD, chronic lung allograft rejection; CRRT, continuous renal replacement therapy; eGFR, estimated glomerular filtration rate; LTR, lung transplant recipient.
DISCUSSION
Although AKI is one of the most common nongraft LTx complications10 and is known as a risk factor associated with mortality,1 few studies have evaluated the effect of the renal replacement therapy, which is a widely accepted strategy, to perioperatively preserve renal function for AKI.2 We therefore described our experience in CRRT for those whose kidney function acutely dropped in the early phase after transplantation. In our analysis, mortality in those who required CRRT was significantly higher than those who were not on CRRT. These are similar outcomes in comparison to a previous report,10 in which the survival rate between recipients with and without RRT was 35.8% versus 85.5% at 1-year posttransplant, respectively, and 20.0% versus 56.4% in 5-year posttransplant. However, it is hard to conclude whether CRRT installation is causal to high mortality because many of LTRs were likely critically ill postoperatively and required CRRT because of hemodynamic instability and other complications that could contribute to survival. CRRT requirement was not related to conditional survival beyond 3-month posttransplant (P = 0.131), indicating that there is no difference in mortality when LTRs survived over 3 months regardless of CRRT implementation. Furthermore, CRRT posttransplant was not associated with the development of CLAD (P = 0.161) and CKD in both moderate (P = 0.757) and severe (P = 0.642) forms (Figure 3). The overall survival and the cumulative incidence of severe CKD also showed a similar trend with a large scale study, in which 654 LTRs were analyzed.1 We thus believe LTRs even who experienced severe AKI requiring CRRT could demonstrate a similar long-term outcome to those who did not require it, provided they are being well managed with CRRT.
PAH was the most common indication for LTx among those who required CRRT therapy (61.9%), although it accounted for minority (10.6%) in LTRs who did not require CRRT (Table 1). This was likely related to the prolonged ischemic time (P = 0.021) as the majority of recipients with CRRT after transplant received double transplant rather than the single (P = 0.007) and thus needed longer operation time (P < 0.0005). LTRs with PAH are known to require hemodynamic and respiratory support immediately after transplantation due to frequently seen left ventricular (LV) failure.1,11,12 Swift normalization of pulmonary vascular resistance, followed by an immediate upturn in cardiac output and a rapid increment in left ventricular filling, leads to drastic LV impairment in PAH patients postoperatively. Therefore, it may be reasonable to implement CRRT in the early posttransplant phase for PAH patients: the removal of a large amount of intravascular fluid can reduce preload, resulting in a reduction in cardiac output and a decrease in the capillary wedge pressure. We thus propose that the initiation of CRRT for PAH patients posttransplant for volume control even though there is no indication for electrolyte or acid-base management (Table 2), to potentially avoid posttransplant LV dysfunction in these recipients. On the other hand, a recent study suggested an extended usage of extracorporeal membrane oxygenation postoperatively until the LV capacity has adapted to the altered hemodynamics after transplantation.12,13 With those features in mind, combined extracorporeal membrane oxygenation with CRRT could be a rescue strategy to preserve cardiac and renal function among critically ill patients after lung transplantation.
Given that this is a single-center retrospective analysis, there are several limitations that warrant discussion. Potential institutional bias should be considered where PAH is responsible for 20% of all LTRs in our facility, which is higher proportion than the International Society for Heart and Lung Transplantation registry14 in which overall PAH accounted for <5.0% of entire recipients. Furthermore, analyzing survival in a larger-scale study would be prudent given the small sample size. The outcome of our study was different from a previous report based on United Network for Organ Sharing database,10 in which a perioperative need for post-LTx RRT was reviewed with the outcome that post-LTx RRT had a lower survival rate than those who did not require RRT. As this was a retrospective registry study from United Network for Organ Sharing, the details of RRT, such as the type (peritoneal, intermittent, or continuous), the duration, and the indication, were unable to be gathered. Therefore, we cannot directly compare the study with our outcome. On the other hand, the transplant circumstance is unique in Japan, where the donor shortage is a major issue. To overcome the shortage, living-donor transplant is one of the transplant procedures,15 yet it is not the current transplant practice worldwide.16 The relationship of the recipient with the donor is different between the living and the deceased donors, which affects the recipient’s condition and outcome, such as waiting time, histocompatibility, ischemic time, etc. For those reasons, the living-donor transplant was excluded from the analysis. Moreover, to cope with an insufficient number of donation, the single-lung transplant still outnumbers the double,15 which is not carried out as frequently today throughout the world.14 Accordingly, the diagnosis of CLAD among recipients with single LTX has not been well established, which should be discussed in the future trial.
In conclusion, we documented our experience with mortality, graft outcomes, and renal function with CRRT use for those who developed AKI after LTx. Although mortality in those who required CRRT was high, conditional survival beyond 3-month posttransplant was not affected. Additionally, the cumulative incidence of CLAD and the development of CKD in CRRT+ were not significant in comparison to those who were not on CRRT. Initiation of CRRT posttransplant may be a useful strategy to preserve cardiac and optimize volume management among critically ill patients, yet further study is needed to overcome some limitation.
Footnotes
Published online 28 May, 2020.
This work is supported in a part by Kurozumi Medical Foundation, Tokyo-Hokenkai Byotai-Seiri Laboratory and Takeda Science Foundation. No additional external funding was received for this study.
The authors declare no conflicts of interest.
The study protocol was reviewed by the Institutional Review Board at Tohoku University Hospital on January 30, 2020. In light of the retrospective design, the requirement of informed consent was waived.
M.K. and T.H. contributed equally to this work and the guarantors of this manuscript. S.E., T.S., H.N., M.N., and Ak.S. have full access to all of the data in the study, gathered information from the database or patients, and took care of patients in the study who underwent lung transplant. H.O., Y.M., and T.S. contributed substantially to the study design, the data analysis and interpretation, reviewed CT images and wrote the manuscript. Am.S. is responsible for statistical analysis. Y.O. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
REFERENCES
- 1.Wehbe E, Brock R, Budev M, et al. Short-term and long-term outcomes of acute kidney injury after lung transplantation. J Heart Lung Transplant. 2012; 31:244–251 [DOI] [PubMed] [Google Scholar]
- 2.Bagshaw SM, Wald R. Strategies for the optimal timing to start renal replacement therapy in critically ill patients with acute kidney injury. Kidney Int. 2017; 91:1022–1032 [DOI] [PubMed] [Google Scholar]
- 3.Matsuo S, Imai E, Horio M, et al. ; Collaborators developing the Japanese equation for estimated GFR. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009; 53:982–992 [DOI] [PubMed] [Google Scholar]
- 4.Kidney Disease Improving Global Outcomes (KDIGO). KDIGO clinical practice guidelines for acute kidney injury. 2012. Available at https://kdigo.org/guidelines/acute-kidney-injury/. Accessed May 12, 2020. [Google Scholar]
- 5.National Institute for Health and Care Excellence. Chronic kidney disease in adults: assessment and management. NICE website. 2014Available at https://www.nice.org.uk/guidance/cg182. Accessed May 12, 2020. [PubMed]
- 6.Verleden GM, Glanville AR, Lease ED, et al. Chronic lung allograft dysfunction: Definition, diagnostic criteria, and approaches to treatment-A consensus report from the Pulmonary Council of the ISHLT. J Heart Lung Transplant. 2019; 38:493–503 [DOI] [PubMed] [Google Scholar]
- 7.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: a report of the American College of Cardiology/American Heart Association Task F. Circulation 2018; 138:e426–e483 [DOI] [PubMed] [Google Scholar]
- 8.Samal L, Linder JA. The primary care perspective on routine urine dipstick screening to identify patients with albuminuria. Clin J Am Soc Nephrol. 2013; 8:131–135 [DOI] [PubMed] [Google Scholar]
- 9.Ronco C, Ricci Z, De Backer D, et al. Renal replacement therapy in acute kidney injury: controversy and consensus. Crit Care. 2015; 19:146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.George TJ, Arnaoutakis GJ, Beaty CA, et al. Acute kidney injury increases mortality after lung transplantation. Ann Thorac Surg 2012; 94:185–192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bartolome S, Hoeper MM, Klepetko W. Advanced pulmonary arterial hypertension: mechanical support and lung transplantation. Eur Respir Rev 2017; 26:185–192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tudorache I, Sommer W, Kühn C, et al. Lung transplantation for severe pulmonary hypertension–awake extracorporeal membrane oxygenation for postoperative left ventricular remodelling. Transplantation. 2015; 99:451–458 [DOI] [PubMed] [Google Scholar]
- 13.Gupta S, Torres F, Bollineni S, et al. Left ventricular dysfunction after lung transplantation for pulmonary arterial hypertension. Transplant Proc. 2015; 47:2732–2736 [DOI] [PubMed] [Google Scholar]
- 14.Schultz G. International Society for Heart and Lung Transplantation. Available at https://ishlt.org/. Accessed May 12, 2020.
- 15.Date H. Current status and problems of lung transplantation in Japan. J Thorac Dis 2016; 8Suppl 8S631–S636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Valapour M, Lehr CJ, Skeans MA, et al. OPTN/SRTR 2017 annual data report: lung. Am J Transplant 2019; 19Suppl 2404–484 [DOI] [PubMed] [Google Scholar]


