Abstract
Objective
The objective of this study was to define the threatened perception types of pregnant women during the COVID-19 pandemic and determine the correlations between the perception types and their demographic factors, their preventive knowledge of COVID-19 and their mental status in order to provide suggestions for pregnant women during pandemic.
Methods
Latent class analysis were used to explore the optimal numbers of clusters. Multinomial logistic regression and multiple correspondence analysis were used to analyze the demographic variables of the latent categories. MANOVA was used to analyze the difference of knowledge of COVID-19 obtained among clusters and their psychological status, and chi-square test was used determine the relationship between the latent clusters and the participant’s COVID-19 worry level.
Results
Five clusters were found: the first cluster (n = 120, 39%) was unthreatened and confident. Cluster 2(n = 84, 28%) was unthreatened but not confident. Cluster 3 (n = 49, 17%) was threatened but confident. Cluster 4 (n = 25, 9%) was threaten, not confident and knowledgeable, and Cluster 5 (n = 20, 7%) was threatened, not confident and lacking knowledge. Three demographic variables were shown an effect on the classification, they were support from work, family support and intrapartum and postpartum complications.
Conclusion
This study can help assess the mental health risks of pregnant women during an epidemic. The results could be helpful for families, work units, communities and medical institutions to make targeted intervention decisions for pregnant women.
Introduction
The novel coronavirus was first detected in Hubei province in December of 2019 and quickly spread throughout China, then worldwide [1]. Panic and worry permeated communities over this lethal virus for which there is currently no cure. Pregnant women are a special group for consideration under the current situation because the levels of the hormones estrogen and progesterone go up during pregnancy, causing the upper respiratory tract to get more easily infected, and the immunological tolerance status of pregnant women makes them hypoimmunity [2]. Besides, there were robust evidences that COVID-19 outbreak as an acute life-threating stressor to pregnant women is harmful to the course of pregnancy and their baby, such as lower infant birth weight, increase the risk of having complications related to the pregnancy, has higher level of depressive, anxiety, dissociative symptoms [3]. The perception of threat that pregnant women have might simply and directly imply how the novel coronavirus affect them. We were interested in whether pregnant women have different perception types face the current coronavirus pandemic? If the answer is positive, how many perception types exist among pregnant women? What causes the difference? What mental care should be given to different perception types? All of questions mentioned above were barely discussed.
Thus, the goal of this research was to classify the different perception types of pregnant women under the threat of a pandemic and investigate the factors causing the differences between the types. The factors considered were the women’s demographic information, amount of knowledge on the coronavirus and their psychological status. We believe the mental health of pregnant women under the stress of a pandemic can be improved by understanding the correlation between perception types and the various indexes, and that this knowledge could offer practical ways to raise public awareness for this group and useful guidance for helping them.
Methods
1. Study design and participants
This cross-sectional mixed-method study was conducted online during February 17 to March 11, Chinese pregnant women were invited to participate an anonymously online survey through Wen Juan Xing platform (https://www.wjx.cn/wjx/design/previewq.aspx?activity=57626820&s=1). All the data received were automatically uploaded on the Wen Juan Xing platform at the end of the survey. All procedures were approved by the Ethics Committee of Wengjiang District People’s Hospital of Chengdu (reference number: EC-2020-002) and an informed consent was signed by all participants. All methods employed were conducted in accordance with the relevant guidance of the ethics committee. The study protocol and data using policy were disclosed at the beginning of first page.
In total, 311 pregnant women were approached, 303 voluntary participants took part in the survey without payment, so the response rate was 97.4%. After eliminated 5 questionnaires with apparent error (2 questionnaires had wrong answers to age, 3 questionnaire had unvaried responses to all questions in at least one of the same questionnaire page).
298 participants from 27 cities in eight provinces were involved in the current study. The age of the participants ranged from 19 to 45 (average age 28.63±4.57 years old); other relevant information was presented in Table 1.
Table 1. Descriptive statistics.
| N | % | |
|---|---|---|
| Education background | ||
| Middle school | 42 | 14.1 |
| High school/technical secondary school | 59 | 19.8 |
| Junior college | 73 | 24.5 |
| Undergraduate | 93 | 31.2 |
| Postgraduate and above | 31 | 10.4 |
| Location | ||
| Urban area | 118 | 39.6 |
| Suburban | 178 | 59.7 |
| Others | 2 | 0.7 |
| Marriage status | ||
| Single | 11 | 3.7 |
| Married | 285 | 95.6 |
| Divorced | 1 | 0.3 |
| Widowed | 1 | 0.3 |
| Histories of abnormal pregnancy | ||
| Negative | 250 | 83.9 |
| Positive | 48 | 16.1 |
| History of pregnancy Complication | ||
| Negative | 202 | 67.8 |
| Positive | 96 | 32.2 |
| Frequency of contact with COVID-19 Patients? | ||
| Never | 213 | 71.5 |
| Low | 57 | 19.1 |
| Sometimes | 24 | 8.1 |
| Always | 4 | 1.3 |
| Were they Previously diagnosed with COVID-19? | ||
| Yes | 1 | 0.3 |
| No | 297 | 99.7 |
aFrequency of contact with COVID-19 patients: never (no contact with diagnosed patients either directly or indirectly); low frequency (lived near diagnosed patients in the same complex); sometimes (lived in the same community as diagnosed patients); always (they have been to a COVID-19 clinic or isolation ward).
2. Instruments
A structured questionnaire was developed with 5 sections, namely, demographic information, psychological status on an emergent event of public health, self-rating somatic about COVID-19 scale, perceived social support scale and knowledge of the coronavirus. This questionnaire consisted of standardized close-ended questions.
The demographic information of the pregnant women. A demographic questionnaire was used to collect data regarding the pregnant women, which included age (a4), occupation (a3), workplace (a9), history of pregnancy (b1), place of residence (a8), marital status (a10), education background a6), and so on. Details showed at Table 1.
Psychological questionnaire on an emergent event of public health (PQEEPH)
The study employed a scale originally was compiled by Ting Gao, it is used to measure psychological status of the public under the outbreak of pandemic. This scale consists of five dimensions: depression (P3,P5, P6, P7, P8, P11), neurasthenia (P13, P16, P17, P18, P21), fear (P1, P2, P9, P12, P14), hypochondriasis (P15, P20) the last one is anxious and force at the same time (P4, P10, P19. P22, P23, P24) [4]. The test based on a 4-point likert-type scale ranging from “0 = none” to “3 = serve”, “0” represents participants didn’t have psychological behavior as the test mentioned. “1”,”2”and”3” means the level of psychological behavior of pregnancy women were mild, middle and sever. The score of each psychological status was calculated separately as this scale includes 5 dimensions, firstly, we calculated a total score by adding up scores of each question in each dimension, then use the total score divided the numbers of question. For example, the score of depression equals a sum score of P3, P5, P6, P7, P8, P11 divided six. Any pregnant women with a score of 2 or higher was considered to have serious symptoms, if the score was lower 2 means the symptoms they had weren’t severely [4].
Somatic self-rating scale (SSS)
This scale was created by Jialiang Mao. It consists of 20 factors [5]. This scale also based on a 4 likert-point ranging from “none” to “serve”, namely, “none” represented the patients didn’t have the symptoms when they were ill or felt uncomfortable, “mild” mean patients had the symptoms but didn’t affect their daily lives, “moderate” shows patients hope symptoms lessened or they can be cured, and “serve” means symptoms seriously affect people’s daily life. We scored from 1 to 4, such as “none” for 1, “mild” for 2 and there is no reverse score. It used the total score to measure the degree of somatization (< = 29, basically normal; 30–39, mild; 40–59, moderate; > = 60, severely)
Perceived social support scale (PSSS)
Zimer developed this scale in which three kinds of support were included: family, friends and working. The score of family support tested by H11, H3, H4, H8, the sore of friend support tested by H6, H7, H9, H12, the rest of questions are about the support from work. This scale scored from “highly disagree” to “strongly agree”, its score is ranging from 1 to 7, “1”means “extremely disagree”, “2” means “highly disagree”, “3” means “mildly disagree”, “4” means “neutrality”, “5” means “mildly agree”, “6” represents “highly agree” and “7” means “extremely agree”. The total points of this scale calculated by adding up all the questions scores and it represented the amount support participants received. Three levels of support in each kind of support exist in this scale, which were low, middle, high. The score of high support status, middle support status, low support status was ranging from 21 to 28, 13 to 20, 4 to 12 respectively [6].
Knowledge of the coronavirus
Four questions were designed to determine the pregnant woman’s knowledge of the current situation: whether they were aware of the incubation period of the virus, the epidemiology of suspected cases, how it manifests clinically and the maximum time of using the surgical mask. The total score was 100.
3. Statistical analysis
Latent class analysis processed by LatentGOLD Choice 5.0 software. SPSS 25.0 was used for descriptive data, multinomial logistic regression, multiple correspondence analysis (MCA) and MANOVA.
Results
1. The confirmation of the latent class models and their characters
Based on pregnancy women’s perceptions about COVID-19 pandemic, latenGOLD 5.0 software was performed to identify laten class model to determine the optimum number of clusters. We began with a single model and then added the number of clusters one at a time to six. According to the latentGOLD 5.0 software, a parsimony and substantive model should along with various fit indices of Logarithmic likelihood (LL), Bayesian information Criterion (BIC), Akaike’s information Criterion (AIC), Likelihood chi-square test (G2). A model with smaller values of these indices means better fit. Our study sample was 298, it was far below than 1000, therefore the selection criteria based on AIC instead BIC as our sample was small [7]. Besides, significant Likelihood chi-square value means the correlations didn’t get interpreted, so adding latent variables were necessary. Among six models, the fourth model had the lowest BIC value, but its G2 value was significant (G2 = 57.9952, p<0.05). The fifth model matched our data as its AIC index was the lowest and G2 index was insignificant (G2 = 33.4994, p = 0.26), so the fifth model was chosen. The results showed in Table 2.
Table 2. Fit indices for the latent class models of pregnant women’s perceptions of threat.
| Model | LL | BIC | AIC | Npar | G2 | df | p | Class. Err. |
|---|---|---|---|---|---|---|---|---|
| 1 | -1031.5658 | 2097.3142 | 2075.1316 | 6 | 522.9505 | 57 | 1.60E-76 | 0 |
| 2 | -884.1328 | 1842.3278 | 1794.2656 | 13 | 228.0845 | 50 | 1.40E-24 | 0.0428 |
| 3 | -833.4653 | 1780.8726 | 1706.9307 | 20 | 126.7495 | 43 | 3.40E-10 | 0.0635 |
| 4 | -799.0882 | 1751.9979 | 1652.1764 | 27 | 57.9952 | 36 | 0.012 | 0.0579 |
| 5 | -786.8403 | 1767.3817 | 1641.6806 | 34 | 33.4994 | 29 | 0.26 | 0.0464 |
| 6 | -781.5054 | 1796.5915 | 1645.0107 | 41 | 22.8296 | 22 | 0.41 | 0.0377 |
Abbreviations: LL, Logarithmic likelihood; BIC, Bayesian information Criterion; AIC, Akaike’s information Criterion; G2. likelihood chi-square value
Name five latent clusters of the pregnancy women perception of threats based on their characters.
There were six observed variables about participants’ perception about the pandemic which measured by six questions in our study: 1) Do you think you might get infected? 2) Do you think the people around you might get infected? 3) Do you think the coronavirus is a threat to you and your fetal life? 4) Do you think the coronavirus is a threat to you and your fetal health? 5) Do you think the protections you took were reliable? 6) Do you think you obtained enough preventive knowledge against the pandemic? There are two choices for the above question: (0 = no, 1 = Yes). Then the six problems are analyzed in the potential category model.
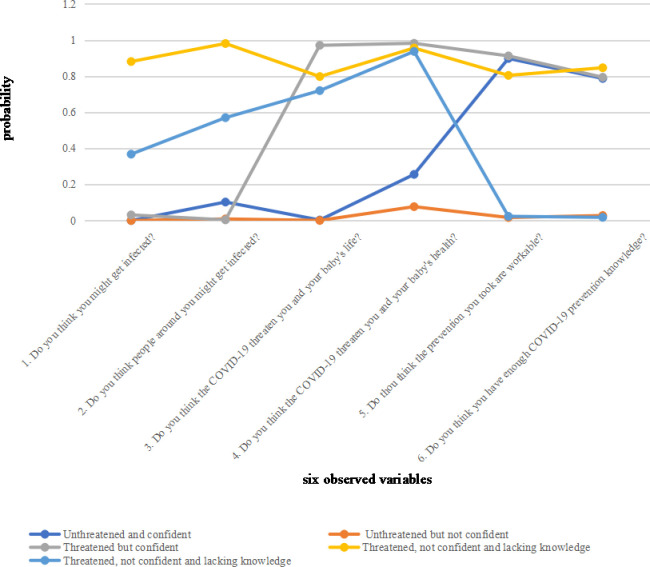
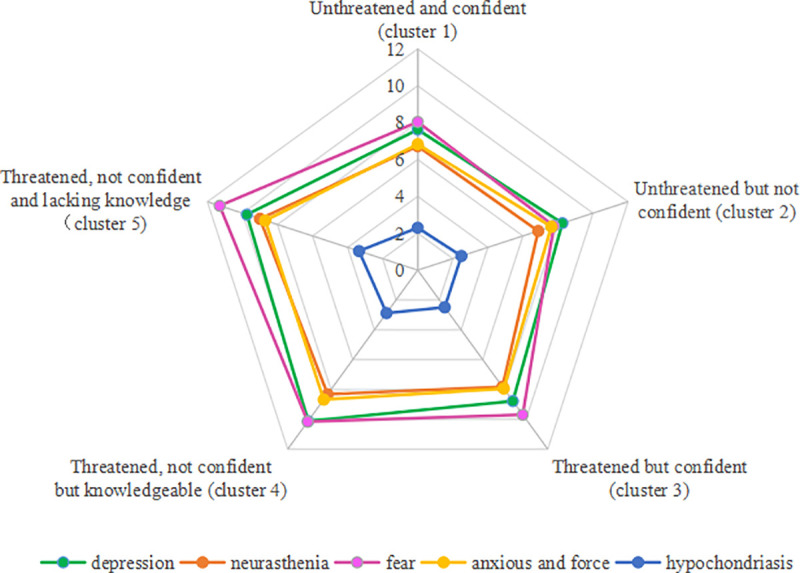
We firstly named five clusters according to the characters they represent after the model was confirmed. Then we sorted out the basic information of each cluster, the cluster membership related to perception of threat, the frequencies (%) of six measures across five clusters. The results showed in Table 3 and Fig 1 as below.
Table 3. The probabilities of choosing six variables by five latent clusters.
| Unthreatened and confident (Cluster 1) | Unthreatened but not confident (Cluster 2) | Threatened but confident (Cluster 3) | Threatened, not confident but knowledgeable (cluster 4) | Threatened, not confident and lacking knowledge (Cluster 5) | |
|---|---|---|---|---|---|
| (n = 120, 39%) | (n = 84, 28%) | (n = 49, 17%) | (n = 25, 9%) | (n = 20, 7%) | |
| Do you think you will get infected? | |||||
| No | 0.4398 | 0.3148 | 0.1866 | 0.0117 | 0.0472 |
| Yes | 0.0005 | 0.0002 | 0.0479 | 0.7298 | 0.2217 |
| Do you think the people around you will get infected? | |||||
| No | 0.4236 | 0.3348 | 0.2059 | 0.0014 | 0.0342 |
| Yes | 0.2336 | 0.0142 | 0.0034 | 0.5263 | 0.2226 |
| Does COVID-19 threaten you and fetal life? | |||||
| No | 0.5486 | 0.3936 | 0.0064 | 0.0256 | 0.0258 |
| Yes | 0.0035 | 0.0001 | 0.576 | 0.2537 | 0.1667 |
| Does COVID-19 threaten you and fetal health? | |||||
| No | 0.5199 | 0.4617 | 0.0049 | 0.0066 | 0.0069 |
| Yes | 0.2269 | 0.0485 | 0.3826 | 0.1996 | 0.1425 |
| Do you think your precautions are useful? | |||||
| No | 0.0958 | 0.6669 | 0.0359 | 0.043 | 0.1583 |
| Yes | 0.5985 | 0.0074 | 0.2663 | 0.1257 | 0.002 |
| Do you think you have enough knowledge of COVID-19? | |||||
| No | 0.1766 | 0.5795 | 0.0747 | 0.0294 | 0.1399 |
| Yes | 0.581 | 0.0141 | 0.2567 | 0.1466 | 0.0016 |
Fig 1. Laten class analysis profile pilot: The conditional probability distribution of six observed variables by membership.
The first cluster thought their precautions were reliable and sufficient. They believed that people around them were least likely to get infected, and so the coronavirus was not a threat to them or their baby. We named members in this cluster as Unthreatened and confident.
The women in the second class thought the virus was not a threat to them or their baby even though the precautions they had taken were neither workable nor sufficient in their own opinion. Members in this cluster called Unthreatened but not confident.
The women in the third cluster still felt they and their baby were unsafe even though they believed nobody around them would get infected. They also believed they had workable precautions and adequate prevention knowledge. Women in this cluster labelled as Threatened but confident.
The women in the fourth cluster both felt threatened and thought people around them might get infected, even though they thought they had enough prevention knowledge and had taken enough practical precautions. Women in this class were named Threatened, not confident and knowledgeable.
The fifth and last cluster has the lowest confidence in their safety in the current situation. They did not think they had enough knowledge and protections, they thought people around them may get infected, and they and their babies were in danger. We labelled women in this cluster as Threatened, not confident and lacking knowledge.
2. The classification results of 5 latent clusters
Firstly, we named 6 observed variables as A, B, C, D, E, F. Then, to get posterior probabilities of membership, we simultaneously calculated latent class probability and conditional probability of six observed variables (item probability) after we parametrized latent model. Lastly, we got classification results according to the maximization principle of posterior probabilities. Details were shown in Table 4. The number of 5 clusters and their proportion were 120(39%), 84(28%), 49(17%), 25(9%), 20(7%) respectively.
Table 4. Posterior probabilities of membership and classification results.
| A | B | C | D | E | F | posterior probabilities of membership | Cluster classification results | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| cluster1 | cluster2 | cluster3 | cluster4 | cluster5 | |||||||
| 0 | 0 | 0 | 1 | 1 | 0 | 0.93 | 0.02 | 0.05 | 0.00 | 0.01 | 1 |
| 0 | 1 | 0 | 1 | 1 | 1 | 0.84 | 0.00 | 0.00 | 0.16 | 0.00 | 1 |
| 0 | 0 | 0 | 0 | 1 | 1 | 1.00 | 0.00 | 0.00 | 0.00 | 0.00 | 1 |
| ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ |
| 0 | 0 | 1 | 1 | 0 | 0 | 0.00 | 0.00 | 0.20 | 0.00 | 0.80 | 5 |
| 0 | 1 | 1 | 1 | 1 | 1 | 0.00 | 0.00 | 0.08 | 0.92 | 0.00 | 4 |
| ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ | ⋮ |
| 0 | 0 | 0 | 0 | 0 | 0 | 0.02 | 0.98 | 0.00 | 0.00 | 0.00 | 2 |
| 0 | 0 | 0 | 0 | 1 | 1 | 1.00 | 0.00 | 0.00 | 0.00 | 0.00 | 1 |
| 0 | 0 | 0 | 0 | 1 | 1 | 1.00 | 0.00 | 0.00 | 0.00 | 0.00 | 1 |
| 0 | 0 | 1 | 1 | 1 | 1 | 0.00 | 0.00 | 1.00 | 0.00 | 0.00 | 3 |
3. The relationship between the demographic information of pregnant women and their latent variables
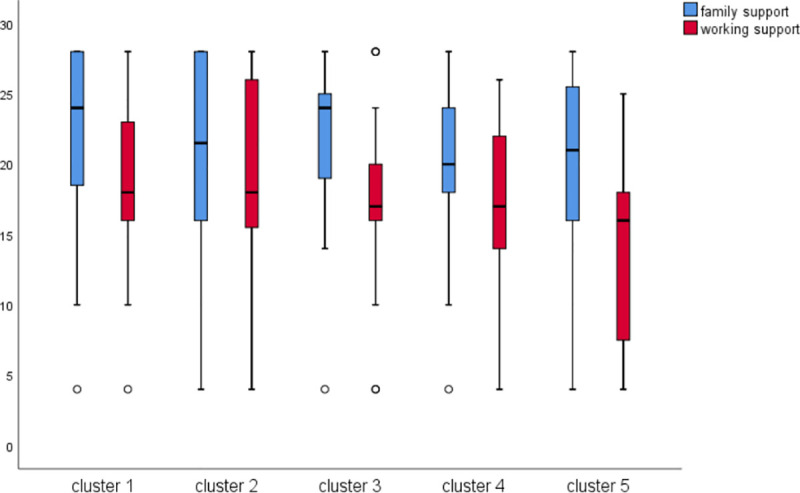
Multinomial logistic regression was used to explore the association between demographic variables and five clusters. We took five latent clusters as independent variables, and demographic information as covariates or dependent variables, and then they were entered into Multinomial logistic regression model. As a result, the two covariates and one dependent variable remained in the regression. Two covariates were ‘family support’ and ‘working support’ and one dependent variable was ‘pregnancy complication’(0 = none,1 = has). The results of the multinomial logistic regression showed that members in Unthreatened and confident (cluster 1) received more support from family than unthreatened but not confident (cluster 2), however, unthreatened but not confident (cluster 2) had a more-supportive working environment than Unthreatened and confident (cluster 1). Meanwhile, members of Threatened, not confident and lacking knowledge (cluster5) had least working support.
The multinomial logistic regression model first defines a certain level of the dependent variable as the reference level, and compare it with other levels, thereby establishing the number of levels-1 general logits model. In this study, cluster1 is selected as the reference level, and the fitted models are respectively:
Logit(πCluster2/πCluster1) = 0.792–0.165×(family_support)+0.116×(working_support)+0.302×(complication = 0).
Logit(πCluster3/πCluster1) = -0.432+0.020×(family_support)-0.063×(working_support)+0.396×(complication = 0).
Logit(πCluster4/πCluster1) = -1.987–0.112×(family_support)+0.028×(working_support)+2.741×(complication = 0).
Logit(πCluster5/πCluster1) = -0.073+0.046×(family_support)-0.177×(working_support)+0.440×(complication = 0).
The details are shown in Table 5 and Fig 2.
Table 5. The influence of demographic variables on five latent clusters by multinomial logistic regression with five latent clusters as independent variables and demographic as covariates and factors variables.
| five latent clustersa | B | Std. Error | Wald | P | OR | 95% Confidence Interval for OR | ||
|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||||
| Unthreatened but not confident (cluster 2) | Intercept | .792 | .588 | 1.813 | .178 | |||
| family support | -.165 | .043 | 14.477 | .000 | .848 | .779 | .923 | |
| working support | .116 | .044 | 6.847 | .009 | 1.123 | 1.030 | 1.226 | |
| [Complication = 0] | .302 | .309 | .953 | .329 | 1.353 | .738 | 2.481 | |
| [Complication = 1] | 0b | . | . | . | . | . | . | |
| Threatened but confident (Cluster 3) | Intercept | -.432 | .755 | .327 | .567 | |||
| family support | .020 | .044 | .201 | .654 | 1.020 | .936 | 1.111 | |
| working support | -.063 | .044 | 2.092 | .148 | .939 | .862 | 1.023 | |
| [Complication = 0] | .396 | .364 | 1.184 | .277 | 1.486 | .728 | 3.036 | |
| [Complication = 1] | 0b | . | . | . | . | . | . | |
| Threatened, not confident but knowledgeable (cluster 4) | Intercept | -1.987 | 1.248 | 2.536 | .111 | |||
| family support | -.112 | .064 | 2.996 | .083 | .894 | .788 | 1.015 | |
| working support | .028 | .068 | .166 | .683 | 1.028 | .900 | 1.174 | |
| [Complication = 0] | 2.741 | 1.041 | 6.936 | .008 | 15.504 | 2.016 | 119.236 | |
| [Complication = 1] | 0b | . | . | . | . | . | . | |
| Threatened, not confident and lacking knowledge (Cluster 5) | Intercept | -.073 | .931 | .006 | .937 | |||
| family support | .046 | .054 | .708 | .400 | 1.047 | .941 | 1.164 | |
| working support | -.177 | .061 | 8.488 | .004 | .838 | .744 | .944 | |
| [Complication = 0] | .440 | .535 | .676 | .411 | 1.553 | .544 | 4.434 | |
| [Complication = 1] | 0b | . | . | . | . | . | . | |
a. The reference category is: Unthreatened and confident (Cluster 1).
b. This parameter is set to zero because it is redundant.
Fig 2. Supporting status of the five perception clusters.
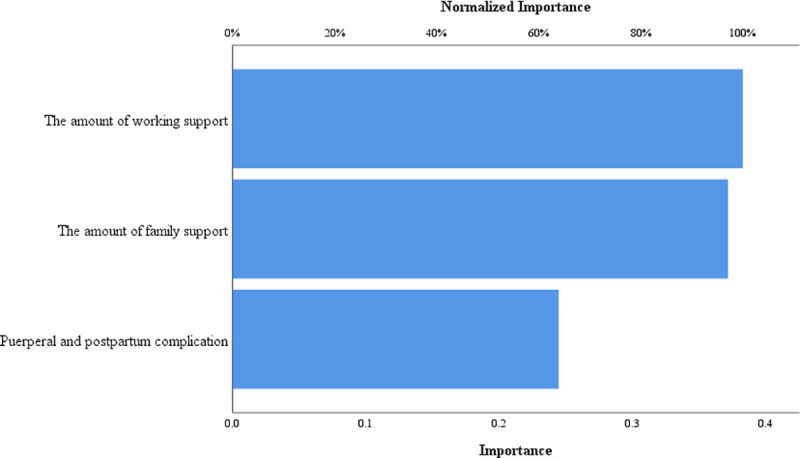
Next, we used a neural network to show the order of importance of factors influencing threat perception categories. The most important variable was woman’s working environment, the second-most important was family support and the least important was complications. The results were shown in Fig 3.
Fig 3. The important grade of variables.
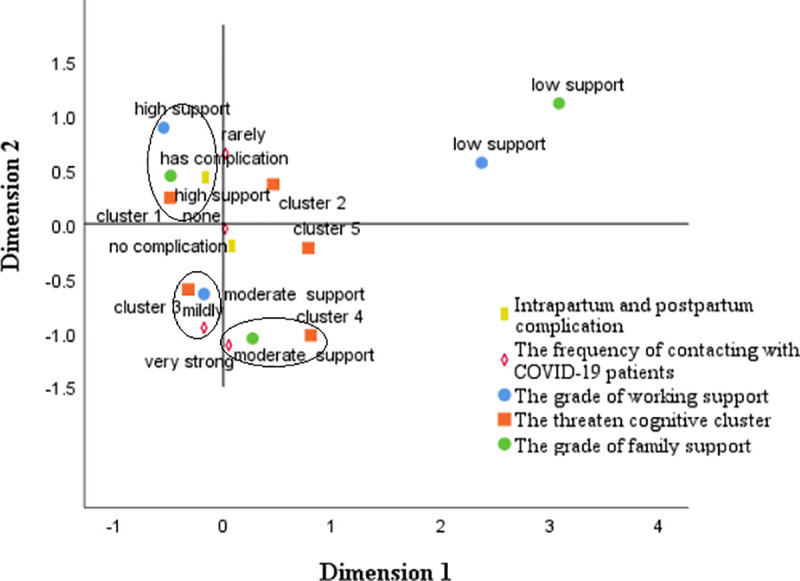
Multiple Correspondence Analysis (MCA) was used to explore the association among support variables, pregnancy complication, the frequency of contacting with diagnosed patients. We firstly transformed all the supporting variables to rank variables, then we put pregnancy complication variables, the frequency of contacting with COVID-19 patients, the grade of support from work, the grade of family support, and five cognitive types into MCA. The criterion of relevance was whether variables part from the origin of the coordinates and assemble together at the same time. The results showed that Unthreatened and confident (cluster 1) strongly correlated with a highly family supportive environment and no pregnancy complications. Threatened but confident (cluster 3) moderately correlated with high-frequency contact and moderate support from work and friends, while Threatened, not confident but knowledgeable (cluster 4) highly correlated to moderate family support and high-frequency contact with diagnosed patients. Details are shown in Fig 4.
Fig 4. Joint category plots: The threatened cognitive types in relation to background factors.
4. The relationship between different threatened cognitive types and mental status
We used the total score of PSSS, the 5 dimensions (depression, neurasthenia, fear, hypochondriasis, anxious and force) of PQEEPH and Knowledge of coronavirus pandemic as dependent variables, and the 5 categories of threat cognition as fixed factors for multivariate analysis of variance (MANOVA). MANOVA showed there was no statistical significance for the comprehension of coronavirus knowledge among the five groups; however, mental health had statistical difference: the index of somatization symptoms in clusters 1 and 2 were significantly lower than in the three other clusters. The index of neurasthenia in clusters 1 and 2 was notably lower than clusters 4 and 5. The degree of depression, anxiety and force at the same time in Unthreatened and confident (cluster 1) was notably lower than clusters 4 and 5. Details were shown in Table 6 and Fig 5.
Table 6. MANOVA of the threatened perception types, knowledge of the coronavirus pandemic and mental status.
| cluster 1 | cluster 2 | cluster 3 | cluster 4 | cluster5 | P | Post hoc | |
|---|---|---|---|---|---|---|---|
| Knowledge of coronavirus pandemic | 85.29 | 88.27 | 87.35 | 92.80 | 84.00 | 0.16 | NA |
| Somatization symptom | 24.48 | 24.60 | 28.86 | 30.60 | 31.00 | 0.00 | 1,2<3,4,5 |
| Depression | 7.62 | 8.25 | 8.78 | 10.12 | 9.75 | 0.00 | 1<4,5 |
| Neurasthenia | 6.72 | 6.87 | 7.82 | 8.32 | 9.00 | 0.00 | 1,2<4,5 |
| Fear | 8.04 | 7.76 | 9.69 | 10.16 | 11.30 | 0.00 | 1,2<3,4,5 |
| Anxious and force | 6.83 | 7.62 | 7.94 | 8.68 | 8.70 | 0.00 | 1<4,5 |
| Hypochondriasis | 2.30 | 2.49 | 2.49 | 2.88 | 3.35 | 0.00 | 1<4<5 |
Fig 5. The relationship between threatened perception clusters and mental status.
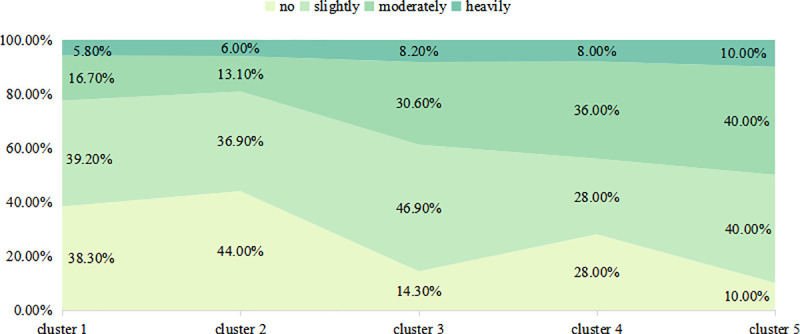
5. The relationship between threatened perception clusters and the amount of maternal anxiousness regarding antenatal care during the coronavirus pandemic
We used chi-squared to test the relationship between the threatened perception types and the amount of maternal anxiousness regarding antenatal care; the result was statistically significant (χ2 = 26.829, df = 12, p<0.01). We then ranked the degree of anxiousness for the five clusters. Unthreatened and confident (cluster 1) was mildly>none>general>severe, Unthreatened but not confident (cluster 2) was none>mildly>general>severe, Threatened but confident (cluster 3) was mildly>general>none>severe, Threatened, not confident but knowledgeable (cluster 4) was general>mildly = none>severe and Threatened, not confident and lacking knowledge (cluster5) was mildly = mildly>severe = none. The details are shown in Fig 6.
Fig 6. The relationship between threatened cognitive types and the amount of maternal anxiousness regarding antenatal care during the coronavirus pandemic.
Discussion
1. The relationship between threatened perception types and demographic variables
This study examined the impact of life-threaten public health event on patterns of pregnant women’s perception of threat. Five latent clusters were carried out by latent class analysis, and three risk factors were confirmed with classification of five latent clusters, which were the puerperal and postpartum complication, support from work and family support. Through subgroups analysis, we found that social support was a vital factor for pregnant women’s mental health, this finding consistent with previous researches. For example, unthreatened and confident (cluster 1) received most support from family and work were more likely to resist negative mental health than other four clusters. Besides, puerperal and postpartum complication was another important variable, we found that threaten, not confident but knowledgeable (cluster 4) had the highest probability having complication, thus they were more likely remain negative status, such as depression and anxiety. Lastly, we found there is no statistical difference regarding to the knowledge of coronavirus.
2. Why is the social support variable so important?
Social support has identified is a vital resource for pregnant women, it provides material and emotion support from family, work, friend to fill their specific needs. There was sufficient evidence that increasing social support can benefit both pregnant women and their babies, such as enhance positive mental health, improve birth outcome, prevent or decreased puerperal complication. In our research, the support from work was the most important variable for pregnancy women. First, from economics reasons, work provides stable wage to cover bills, if women don’t have enough money to pay their bills during their pregnancy could be considered as negative life events or chronic life-stressor. Some previous studies found that pregnant women who work as part time or less have more possibilities to report negative feels, such as anxiety and depress [8]. That is to say, if women were in high or stable financial status would be more likely to think and behave positive [9]. Second, Work takes most of time regarding with daily time arrangement during pregnancy. According to the Special Rules on the Labor Protection of Female Employees in China, female employees are given 98 days of maternity leave and they can start this leave 15 days in advance of the birth of their child [10]. Since pregnancy usually lasts for 40 weeks, this means pregnant women will spend nearly 38 weeks of their pregnancy at work. The legal amount of working hours is 8 hours per day, so most professional females spend one third of the day at work, apart from commuting time, sleep time and so on, it leaves less than 6 hours of the day to spend with family and friends.
Lastly, COVID-19 has official announced that it has human to human transmission. Professional pregnant women have more chance to get infected as the highly population mobility from home to work or highly population density in the workplace. Therefore, pregnant women perceived strong work support were more likely to resist negative mental health.
The grade of family support was another important variable to determine pregnant women perception of coronavirus threat [11]. Pregnant women can confront stress with stronger confident from material and emotional support from family. Previous research demonstrated that after adjusting by family support from family members, particularly husband and parents, had significantly higher adherence mental status and better physical health [12]. The family should acknowledge that bearing and raising the baby is not a task exclusive to the mother but can be done with the help of the whole family [13]. Husbands should give strong emotion and material support, such as communicating with their wives and allowing her to express her feelings, help with share more household and babysitting.
3. What is the relationship between threatened perception types and intrapartum and postpartum complications?
Pregnancy complication commonly happen in pregnant women, there was a national population-based research reported that complication was reported in 34.3% in pregnancy, it highly affects pregnant women and their baby’s health, such as low birth weight [14]. We found out pregnancy complication highly associated with mental health in our research, women in threaten, not confident but knowledgeable cluster had highest probabilities having complication, and women in cluster 4 had higher rate for passive mental health such as depression, anxiety and neurasthenia compared with women in unthreatened and confident cluster.
4. Did the maternal women have enough prevention knowledge of COVID-19?
This result was interesting, we found the variable of the amount of knowledge on the prevention of the coronavirus was not statistical different among 5 clusters. Thus, it is highly possible that maternal women did not understand the amount of risk coronavirus presents to them? This should be a warning about the effectiveness of our media communication on the prevention of the spread of the virus; we should take full advantage of the convenience and propagation velocity of social media. At the same time, we need to broadcast prevention knowledge and confirm how much knowledge is being absorbed by the public.
It is necessary to note that this result we had might because we only used four questions to assess this item in an attempt to avoid the fatigue effect. Future research should use more questions to confirm this result if possible.
5. Which clusters should get more attention?
Unthreatened and confident (cluster 1) had the best mental state, with a significantly lower degree of negative mentality than the other four clusters. Threatened, not confident and lacking knowledge (cluster5) had the highest index of negative mentality among the five clusters, with the other indices of mental status following suit. We found that Threatened, not confident and lacking knowledge (cluster5) had very limited support and lacked confidence in their amount of prevention knowledge. The phenomena might be the result of habitual self-abasement. This is why more attention should be paid to this cluster to make sure they have ample opportunity to gain prevention knowledge; we also need to teach them some necessary psychological techniques to adjust or prevent negative emotion and encourage their families to give them more support. Support from their work environment is also needed.
Another cluster that requires attention is Threatened, not confident but knowledgeable (cluster 4). This cluster’s negative mental index was only slightly behind that of Threatened, not confident and lacking knowledge (cluster5), they had high-frequency contact with COVID-19 diagnosed patients but only received moderate family support. We should attempt to direct the members of this group to transfer into positive ones by reducing their contact with patients and enhancing the extent of their support from family and their work environment.
6. Can pregnant women still go to the hospital for antenatal care?
All five clusters were concerned about their antenatal care, as they were afraid of getting infected during hospital visits. Clusters 4 and 5 had a higher index in this than the other four clusters, and the difference was statistical significant. However, the health department in China considered this at the beginning of the pandemic and enacted some policies. For example, they stipulated that hospitals must set fever clinics in a that keeps non-exposed indiviuals safe [15]; suspected COVID-10 patients were settled in an independent area of the hospital, and diagnosed patients were admitted to a specific hospital managed by government. Thus, pregnant women can trust that the hospital is safe. They should be encouraged to keep in close contact with their attending physician and arrange their antenatal care schedule appropriately; pregnant women should follow their doctor’s orders and let the doctor decide whether it is safe for them to come to the hospital to receive their antenatal care [16]. A further possibility is that the obstetrics and pediatric departments can have their own group chat system, such as QQ, Wechat or What’s up, that can help eliminate or reduce the extent of asymmetric information.
It should be noted that currently there is no special scale for measuring the maternal anxiousness regarding antenatal care, so we have designed a question to let pregnant women to self-evaluate their anxiousness regarding antenatal care. Because there is only one question, it is impossible to test its reliability and validity, and it is difficult to guarantee its objectivity. However, since there was no scale for maternal anxiousness regarding antenatal care, it is unclear whether it is necessary to make a special scale for this. However, this study shows that during the big pandemic, even for the pregnant women with the best psychological conditions, most of them believe that they have anxiousness regarding antenatal care. This result reminds us that it is necessary to pay attention to the anxiousness regarding antenatal care during the epidemic. Therefore, the next step of our research is to develop a scale dedicated to assessing maternal anxiousness regarding antenatal care, so as to provide researchers with more objective and reliable measurement tools.
In conclusion, the threatened cognitive types highly correlated to the amount of support from family and work. Classifying pregnant women into groups can help predict their mental health and provide a theoretical framework for helping their family, work environment, community and hospital make targeted policies.
Supporting information
(SAV)
(PDF)
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
Mengsha Qi was funded by Innovation and Entrepreneurship Project of Sichuan Provincial Science and Technology department (Grand code:2020JDRC0135). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization. Novel Coronavirus-China [EB/OL]. https://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/,2020-01-30/2020-02-12.
- 2.Jain A, Sami-Zakhari IR. Pulmonary complications of obstetric and gynecologic conditions. Respiratory Medicine. 2017, October 24: 139–61. 10.1007/978-3-319-69620-1_8 PMCID: PMC7121584. [DOI] [Google Scholar]
- 3.Urato AC. Consensus bundle on maternal mental health: perinatal depression and anxiety. Obstet&Gynecol. 2017, 130(2): 467–468. 10.1097/AOG.0000000000002178 [DOI] [PubMed] [Google Scholar]
- 4.Gao Y, Xu M, Yang Y, et al. Discussion on the coping style of undergraduates and the correlative factors during the epidemic period of sars. Chinese Medical Ethics. 2004, (02): 60–63. [Google Scholar]
- 5.Zhuang Q, Mao J, Li C, et al. Developing of somatic self-rating scale and its reliability and validity. Chinese Journal of Behavioral Medicine and Brain Science. 2010, 19(9): 847–849. 10.3760/cma.j.issn.1674-6554.2010.09.026 [DOI] [Google Scholar]
- 6.Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. Journal of Personality Assessment. 1988, 52: 30–41. [DOI] [PubMed] [Google Scholar]
- 7.Lin TH, Dayton CM. Model selection information criteria for non-nested latent class models. Journal of Educational and Behavioral Statistics. 1997, 22(3): 249–264. 10.3102/10769986022003249 [DOI] [Google Scholar]
- 8.Kim TH, Connolly JA, Tamim H. The effect of social support around pregnancy on postpartum depression among Canadian teen mothers and adult mothers in the maternity experiences survey. BMC Pregnancy Childbirth. 2014;14:162 Published 2014 May 7. 10.1186/1471-2393-14-162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moshki M, Cheravi K. Relationships among depression during pregnancy, social support and health locus of control among Iranian pregnant women. Int J Soc Psychiatry. 2016;62(2):148–155. 10.1177/0020764015612119 [DOI] [PubMed] [Google Scholar]
- 10.Waibel Duncan MK, Blugis A. Maslow's Needs Hierarchy as a Framework for Evaluating Hospitality Houses' Resources and Services. Journal of Pediatric Nursing. 2011, 26: 325–331. 10.1016/j.pedn.2010.04.003 [DOI] [PubMed] [Google Scholar]
- 11.Zhang L. China: Two Child Policy Becomes Law. Global legal monitor [EB/OL]. https://www.loc.gov/law/foreign-news/article/china-two-child-policy-becomes-law, January 8, 2016.
- 12.Wado YD, Afework MF, Hindin MJ. Effects of maternal pregnancy intention, depressive symptoms and social support on risk of low birth weight: a prospective study from southwestern Ethiopia. PLoS One. 2014;9(5):e96304 Published 2014 May 21. 10.1371/journal.pone.0096304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xie RH, Liao S, Xie H, Guo Y, Walker M, Wen SW. Infant sex, family support and postpartum depression in a Chinese cohort. J Epidemiol Community Health. 2011;65(8):722–726. 10.1136/jech.2009.096651 [DOI] [PubMed] [Google Scholar]
- 14.Wiradnyani LA, Khusun H, Achadi EL, Ocviyanti D, Shankar AH. Role of family support and women's knowledge on pregnancy-related risks in adherence to maternal iron-folic acid supplementation in Indonesia. Public Health Nutr. 2016;19(15):2818–2828. 10.1017/S1368980016001002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Witt WP, Wisk LE, Cheng ER, Hampton JM, Hagen EW. Preconception mental health predicts pregnancy complications and adverse birth outcomes: a national population-based study. Matern Child Health J. 2012;16(7):1525–1541. 10.1007/s10995-011-0916-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.He Y. Psychological coping strategy of pregnant and lying-in woman during the COVID-19 epidemic. Chinese Mental Health Journal. 2020. (03): 259–261 [2020-05-04]. http://kns.cnki.net/kcms/detail/11.1873.r.20200310.1528.050.html. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(SAV)
(PDF)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.