Abstract
This study investigates the forces that contributed to severe shortages in personal protective equipment in the US during the COVID-19 crisis. Problems from a dysfunctional costing model in hospital operating systems were magnified by a very large demand shock triggered by acute need in healthcare and panicked marketplace behavior that depleted domestic PPE inventories. The lack of effective action on the part of the federal government to maintain and distribute domestic inventories, as well as severe disruptions to the PPE global supply chain, amplified the problem. Analysis of trade data shows that the US is the world's largest importer of face masks, eye protection, and medical gloves, making it highly vulnerable to disruptions in exports of medical supplies. We conclude that market prices are not appropriate mechanisms for rationing inputs to health because health is a public good. Removing the profit motive for purchasing PPE in hospital costing models, strengthening government capacity to maintain and distribute stockpiles, developing and enforcing regulations, and pursuing strategic industrial policy to reduce US dependence on imported PPE will help to better protect healthcare workers with adequate supplies of PPE.
Keywords: Personal protective equipment, COVID-19, Coronavirus, N95, Gloves, PPE, Nurses, Supply chain, Shortage, Public good
Highlights
-
•
Market failure and government failure contributed to PPE shortage during COVID-19
-
•
Dysfunctional hospital budgeting models disincentivize adequate inventories of PPE
-
•
Federal government failed to maintain and distribute domestic inventories of PPE
-
•
Pursue strategic industrial policy to reduce US dependence on PPE supply chain
-
•
Market prices are inappropriate mechanisms for rationing inputs to health, like PPE
1. Introduction
Since early 2020 the US has experienced a severe shortage of personal protective equipment (PPE) needed by healthcare workers fighting the COVID-19 pandemic (Emanuel et al., 2020; Livingston et al., 2020). In protests covered by the news media, healthcare workers compared themselves to firefighters putting out fires without water and soldiers going into combat with cardboard body armor. Medical professionals have called for federal government action to mobilize and distribute adequate supplies of protective equipment, especially gloves, medical masks, goggles or face shields, gowns, and N95 respirators. N95 respirators, which have demonstrated efficacy in reducing respiratory infections among healthcare workers, have been in particularly short supply (MacIntyre et al., 2014).
Without proper PPE, healthcare workers are more likely to become ill. A decline in the supply of healthcare due to worker illness combines with intensified demand for care, causing healthcare infrastructure to become unstable, thus reducing the quality and quantity of care available. Sick healthcare workers also contribute to viral transmission. Hence ill practitioners increase the demand for care while simultaneously reducing health system capacity. This endogeneity makes a PPE shortage a systemwide public health problem, rather than solely a worker's rights or occupational health issue. PPE for healthcare workers is a key component of infection prevention and control; ensuring that healthcare workers are protected means more effective containment for all.
We investigate the four main contributing factors behind the US shortage of PPE in 2020 and their interaction. First, a dysfunctional budgeting model in hospital operating systems incentivizes hospitals to minimize costs rather than maintain adequate inventories of PPE. Second, a major demand shock triggered by healthcare system needs as well as panicked marketplace behavior depleted PPE inventories. Third, the federal government failed to maintain and distribute domestic inventories. Finally, major disruptions to the PPE global supply chain caused a sharp reduction in PPE exported to the US, which was already highly dependent on globally-sourced PPE. Market and government failures thus led PPE procurement by hospitals, healthcare providers, businesses, individuals, and governments to become competitive and costly in terms of time and money. The remainder of this article provides detailed support for the argument that the enormous PPE shortages arose from the compounding effects of these four factors. We conclude that because health is a public good, markets are not suitable mechanisms for rationing the resources necessary for health, and transformative changes are necessary to better protect healthcare practitioners.
2. Background
The 2020 shortage of PPE was an eventuality that nonetheless came as a surprise. The US experienced heightened demand for PPE in the mid- to late-1980s following the identification of the Human Immunodeficiency Virus and the release of Centers for Disease Control (CDC) guidelines for protecting health personnel (Segal, 2016). The 2001 attack on the World Trade Center heightened concerns that insufficient PPE left healthcare workers vulnerable to exposure to toxins from bioterrorism and other future public health emergencies (O'Boyle et al., 2006). The 2014 Ebola Virus outbreak made the importance of protection for health workers especially apparent when two nurses with inadequate protection treated an Ebola-infected patient in a Dallas hospital and became infected themselves. Subsequent studies pointed to global PPE shortages as a contributing factor to infections and deaths of hundreds of healthcare workers in West African countries hit hardest by the Ebola Virus (Hersi et al., 2015).
Although various stakeholders (governments, multilateral agencies, health organizations, universities) warned of the possibility of a major infectious disease outbreak, particularly pandemic influenza, most governments were underprepared. The World Economic Forum's annual Global Risks Report even showed a decline in the likelihood and impact of a spread of infectious diseases as a predicted risk factor between 2015 and 2020 (WEF, 2015, WEF, 2020). The problems created by lack of preparation were exacerbated by the high transmissibility of COVID-19 and the severity of symptoms. Contributing to the inadequate stockpiles of PPE were the Trump administration's policies - which included public health budget cuts, “streamlining” the pandemic response team, and a trade war with the country's major supplier of PPE - weakening the CDC's capacity to prepare for a crisis of this magnitude (Devi, 2020).
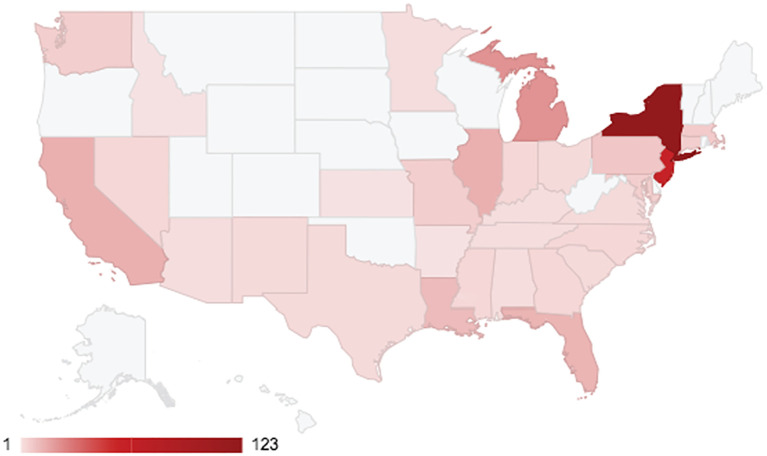
The PPE shortage is reflected in survey data on PPE usage and in data on COVID-19 morbidity and mortality. As of May 2020, 87% of nurses reported having to reuse a single-use disposable mask or N95 respirator, and 27% of nurses reported they had been exposed to confirmed COVID-19 patients without wearing appropriate PPE (NNU, 2020). As of July 28, 2020, at least 1842 nurses, doctors, physicians assistants, medical technicians, and other healthcare workers globally, and 342 in the US, died due to the virus, and many more became sick (Medscape, 2020). The CDC aggregate national data of 172,844 cases among healthcare personnel and 743 deaths (CDC, 2020b). Healthcare workers have died from COVID-related causes in all but 19 states (Fig. 1 ).1
Fig. 1.
Healthcare worker deaths by state, July 28, 2020. *Map created by the authors using Google Sheets and Medscape (2020). Unshaded states had no healthcare worker deaths.
Healthcare worker deaths by state recorded in Medscape (2020) are correlated with CDC (2020b) COVID-19 cases by state (Pearson's r of 0.552, p < 0.00) and even more strongly correlated with CDC-confirmed COVID deaths in the general population (Pearson's r of 0.953, p < 0.00). These correlation coefficients are indicative of healthcare worker exposure to the virus, and of the critical role of PPE and healthcare systems for population health. In other words, population health is a function of the healthcare system and wellbeing of healthcare workers, and the wellbeing of healthcare workers is a function of the healthcare system and PPE.
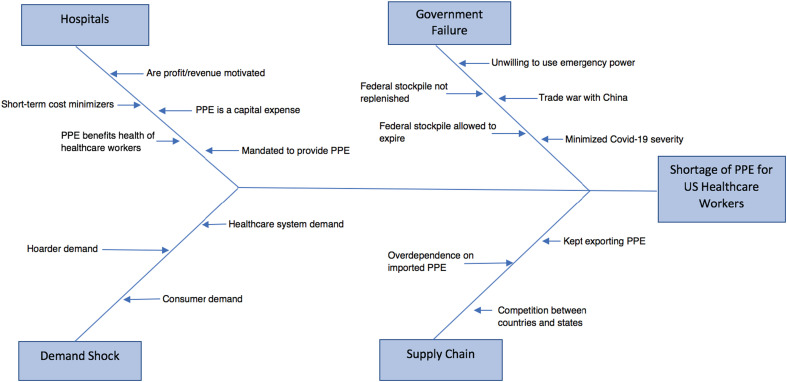
We now turn to our analysis of PPE shortages, which identifies on four contributing factors: the way that hospitals budget for PPE, domestic demand shocks, federal government failures, and disruptions to the global supply chain (Fig. 2 ). These four factors arose from a number of processes and worked concurrently to generate severe shortages.
Fig. 2.
Factors contributing PPE shortage.
3. The PPE Budgeting Model
The first factor-the budgeting model used by hospitals - is a structural weakness in the healthcare system. The Occupational Safety and Health Administration (OSHA) requires employers to provide healthcare workers with PPE free of charge (Barniv et al., 2000; OSHA, 2007). From the perspective of employers, PPE is an expenditure - a cost. PPE is unique compared to all of the other items used to treat patients (such as catheters, bed pans, and medications) which operate on a cost-passing model, meaning they are billed to the patient/insurer.
An ideal model for budgeting PPE would align the interests of employers, healthcare workers, and patients and facilitate effective, efficient care that is safe for all. Instead, the existing structure puts employers who prioritize minimizing costs and healthcare workers who prioritize protecting their safety and the health of their patients in opposition, leaving governmental bodies to regulate these competing priorities (Moses et al., 2013).
Employers, be they privately-owned enterprises, private healthcare clinics, or public hospitals, seek to minimize costs. In economic theory, cost-minimization is compelled through market competition with other suppliers. In practice, cost-minimization is a strategy for maintaining profitability or revenue. Therefore, hospital managers adopt cost-effective behaviors by reducing expenditures in the short term to lower costs (McLellan, 2017). Despite some hospitals' tax-exempt status, hospitals function like other businesses: they pursue efficiency and cost minimization (Bai and Anderson, 2016; Rosenbaum et al., 2015). The pursuit of efficiency means hospitals tend to rely on just-in-time production so that they do not need to maintain PPE inventories. The OSHA requirement effectively acts as an unfunded mandate, imposing responsibility for the provision of PPE, and the costs of provision, on employers.
When it is difficult to pass along the costs of unfunded mandates to workers (in the form of lower wages) or customers (in the form of higher prices), employers resist such cost-raising legal requirements. The tension between healthcare workers and employers over PPE is evident in the way nurses' unions push federal and state agencies to establish protective standards. It is demonstrated by the testimony of Deborah Burger, the co-president of National Nurses United to the Committee on Oversight and Government Reform in the US House of Representatives in October 2014. She advocated for mandated standards for PPE during the Ebola Virus while employers were pushing for voluntary guidelines:
[O]ur long experience with US hospitals is that they will not act on their own to secure the highest standards of protection without a specific directive from our federal authorities in the form of an Act of Congress or an executive order from the White House…The lack of mandates in favor of shifting guidelines from multiple agencies, and reliance on voluntary compliance, has left nurses and other caregivers uncertain, severely unprepared and vulnerable to infection (Govinfo, 2014).
Employer resistance is short-sighted but unsurprising in the existing costing structure. The costing structure for other items, like catheters, allows employers to pass costs on to patients and insurers. The implication is that if employers (hospitals) cannot pass along the cost of the OSHA mandate to insurance companies, then employers do not have an economic incentive to encourage employees to use PPE, replace it frequently, or keep much of it in stock, at least until any gains from cost-minimization are lost due to illness among employees.
The budgeting model is especially problematic when demand increases sharply, such as during the Ebola Virus in 2014 and the H1N1 influenza pandemic in 2009. As the site where new pathogens may be introduced unexpectedly, hospitals are uniquely challenged compared to other employers to provide protection (Yarbrough et al., 2016). But even during predictable fluctuations in demand, the existing model does not ensure that adequate quantities of PPE are available. However, previous studies have framed these problems as consequences of noncompliance among healthcare workers rather than noncompliance among employers (Ganczak and Szych, 2007; Gershon et al., 2000; Nichol et al., 2013; Sax et al., 2005).
Hospitals might be incentivized to avoid shortages by passing PPE costs on to patients and insurers, like other items used in care, but that approach is not the norm. This alternative cost-passing model also leaves much to be desired. Where the current model induces tension between workers and employers, a cost-passing model would effectively situate practitioners against patients (Cerminara, 2001). If patients pay the costs of PPE, they might prefer that practitioners are less safe to defray costs. Such a model is detrimental to both healthcare workers and patients. Introducing tension to a relationship built on care and trust is precisely why the employer, not the patient, should be required to provide PPE to healthcare workers at no cost to the worker. Practitioners and patients should be allowed to share the common goal of improving patients' well-being.
Some labor economists argue that employers could (or do) pay compensating wage differentials to compensate healthcare workers for working in unsafe conditions (Hall and Jones, 2007; Rosen, 1986; Viscusi, 1993). They believe that workers subject to hazardous conditions command a higher wage from employers compared to workers in less dangerous employment. Higher wages for healthcare workers would then be embedded in the costs of care, which include pay for practitioners, that are passed along to insurance companies. However, this counter-argument does not apply to healthcare practitioners because its necessary conditions are not met. Workers would need perfect foresight that a crisis would require more protective equipment, knowledge of their employers' stockpile of PPE, perfect information about the hazards of the disease, and how much higher a wage they would need as compensation for these risks. This information is not available for workers who may be exposed to entirely novel pathogens that have unknowable impacts.
Neither the existing budgeting model nor the cost-passing model align the interests of the employer, healthcare worker, and patient. Yet these three agents have a shared interest in practitioners' use of PPE. PPE, like catheters, are inputs to health. But unlike catheters, the primary beneficiary of PPE use is less easily identifiable than that of other inputs. While healthcare practitioners may appear to be the primary beneficiaries of PPE, the benefits are more diffuse. Patients benefit from having healthy nurses who are not spreading infections, nurses benefit from their own health, and hospitals benefit from have a healthy workforce. Nurses' health is an input to patient health, to the functioning of the hospital, and to the healthcare system. In other words, every beneficiary depends on practitioners' health, which depends on PPE. Still, employers' short-term profit motive dominates the interests of healthcare workers and patients, which suggests that alternative models that are not motivated by profit-seeking should be explored.
4. The Demand Shock
The second contributing factor to the US shortage of PPE during the COVID-19 outbreak was the rapid increase in demand by the healthcare system and the general public. In a national survey of hospital professionals in late March 2020 close to one-third of hospitals had almost no more face masks and 13% had run out of plastic face shields, with hospitals using a number of strategies to try to meet their demand including purchasing in the market and soliciting donations (Kamerow, 2020). American consumers also bought large supplies of PPE as the sheer scale of the crisis and the severity of the disease prompted a surge in panic buying, hoarding, and resales of masks and gloves. As an indicator of scale, in March 2020 Amazon cancelled more than half a million offers to sell masks at inflated prices and closed 4000 accounts for violating fair pricing policies (Cabral and Xu, 2020). Panicked buying contributed to a sudden and sharp reduction in American PPE inventories, which were already inadequate to meet demand from the healthcare system.
There were two different kinds of non-healthcare buyers of PPE. A subset sought profits and bought and hoarded PPE items such as N95 respirators with the intent of reselling them at inflated prices (Cohen, Cohen, 2020a, Cohen, 2020b). It is likely that the majority, however, were worried consumers. While it may be tempting to blame consumers for seemingly irrational consumption, their decisions are more complex. Panic buyers are consumers in the moment of buying PPE, but they are workers as well; people buy PPE because they are afraid of losing the ability to work and support themselves and their families. Put simply, the dependence of workers on wages to pay for basic necessities contributes to panic when their incomes are threatened. This is rational behavior in the short term given existing conditions and economic structures. Still, PPE belongs in the hands of those whose health has many beneficiaries: practitioners. Eventually both the profiteer and the average, panicked worker/consumer will require healthcare, and contributing to the decimation of the healthcare work force is in no one's interest. Underlying consumption behavior was intense fear of not only the disease but also fear of shortages. This panic reverberated throughout the supply chain as manufacturers tried to increase their production capacity to meet the demand for PPE (Mason and Friese, 2020).
One can conceptualize this mismatch between PPE demand and supply in an ability-to-pay framework. In much of economic theory, markets match supply and demand to determine the price of a good or service, and the price operates as a rationing mechanism. Market actors choose to buy or sell at that given price. But there are problems with this framework. On the demand side, some people cannot “choose” to buy a product because they cannot afford it; they lack the ability to pay, so the decision is made for them. An example is a potential trip to the doctor for the uninsured. For many Americans, whether to go to the doctor, or whether to have insurance, is not a choice; the choice is made for them because they are unable to pay.
On the supply side, the ability-to-pay framework remains, except the product in question is an input. In healthcare, the practitioner is the proximate supplier of care and inputs to health are intermediate goods. The supplier's - or their employer's - ability (and willingness) to pay for inputs to care, including PPE, determines the quality and quantity of care the practitioner is able to supply. When healthcare workers do not have PPE (e.g. because others bought it and resold it at extortionary prices), they are unable to provide the care patients need. But reselling behavior is also economically rational, if unethical, at least in the short term. Indeed, ability-to-pay works well for the hoarder/reseller, who both contributes to and profits from the shortage. It is in the pursuit of profits - of monetary gain - that the mismatch between PPE demand and supply resides.
On the demand side there is a person in need of care who is constrained by their inability to pay, while on the supply side there is a practitioner who is constrained by their inability to access the resources required to provide high quality care safely. The ability-to-pay framework is incompatible with the optimal allocation of resources when the ultimate aim is something other than monetary gain. Hence market prices are not a good mechanism for rationing vital inputs to health such as PPE, and the profit motive is ineffective in resolving this mismatch between demand and supply.
5. Government Failure
Given the large-scale failure of the market to ensure sufficient supplies of PPE for practitioners, the government could have taken a number of corrective actions: it could have coordinated domestic production and distribution, deployed supplies from the Strategic National Stockpile, or procured PPE directly from international suppliers (HHS, 2020; Maloney, 2020).
The US government has anticipated PPE shortages since at least 2006 when the National Institute for Occupational Safety and Health commissioned a report examining the lack of preparedness of the healthcare system for supplying workers with adequate PPE in the event of pandemic influenza (Liverman and Goldfrank, 2007). In a scenario in which 30% of the US population becomes ill from pandemic influenza, the estimated need for N95 respirators is 3.5 billion (Carias et al., 2015). However, the actual supply in the US stockpile was far smaller at 30 million, thus serving as a strong rationale to invoke the Defense Production Act to manufacture N95 respirators and other PPE (Azar, 2020; Friese et al., 2020; Kamerow, 2020). Further, the PPE in the national stockpile was not maintained on a timely basis to prevent product expiration, forcing the CDC to recommend use of expired N95s (CDC, 2020a).
Adding to the problems of CDC budget cuts before and during the pandemic and their failure to stockpile PPE was the unwillingness of the federal government to invoke the Defense Production Act to require private companies to manufacture PPE, ventilators, and other critical items needed to treat patients (Devi, 2020). By July 2020, at which time the US already had more COVID-19 cases than any other country in the world, there were still calls from top congressional leaders and healthcare professionals, including the Speaker of the House of Representatives and the president of the American Medical Association, for the Trump administration to use the Defense Production Act to boost domestic production of PPE (Madara, 2020; Pelosi, 2020; Rosen, 2020a). Researchers had also begun to publish studies on how to safely re-use PPE as it became clear that shortages would continue (Rowan and Laffey, 2020). Hence even five months into the crisis, the profit motive was still inadequate to attract new producers, which indicates that markets do not work to solve production and distribution problems in the case of inputs to health.
Not only did the government poorly maintain already-inadequate supplies and fail to raise production directly, it also failed to provide guidance requested by private sector medical equipment distributors and the Health Industry Distributors Association (HIDA), a trade group of member companies (Maloney, 2020). The private sector sought guidance about accessing government inventories, expediting PPE imports, and how to prioritize distribution, as indicated in this communication from HIDA's president:
Specifically, distributors need FEMA and the federal government to designate specific localities, jurisdictions or care settings as priorities for PPE and other medical supplies. The private sector is not in a position to make these judgments. Only the federal government has the data and the authority to provide this strategic direction to the supply chain and the healthcare system (Rowan, 2020).
Moreover, it was not until early April 2020 that the Trump administration issued an executive order for 3 M, one of the largest American producers and exporters of N95 respirators, to stop exporting masks and to redirect them to the US market (Whitehouse.gov, 2020).
Looking up the supply chain, at least one distributor proposed bringing efforts to procure PPE internationally under a federal umbrella to the Trump administration (Maloney, 2020, p. 11). States-as-buyers confront the same market-incentivized structural issues that individual buyers face. A single federal purchaser would reduce state-level competition for buying PPE abroad, and mitigate the resulting inflated prices and price gouging by brokers acting as intermediaries between states-as-buyers and suppliers. The federal government chose not to take on this role.
The profound government failures related to producing, procuring, and distributing PPE effectively, in ways not achievable through markets, are likely to have long-term impacts. The same distribution companies characterized, “the economics of supplying PPE in these circumstances” as “not sustainable” (Maloney, 2020, p. 3). They also expressed concern about the ongoing availability of raw materials required to manufacture PPE in the future. HIDA member companies expressed these concerns about supply chain issues in calls with federal agencies between January and March 2020, specifically with respect to long-term supply chain issues impacting the upcoming 2020-21 flu season (Maloney, 2020, p. 5). In mid-June, FEMA officials acknowledged that, “the supply chain is still not stable” (Maloney, 2020, p. 9).
6. Global Supply Chain Breakdown
A smoothly functioning supply chain has immediate impacts on the ability of governments and health personnel to contain an epidemic. The infectiousness and virulence of the disease affects the demand for PPE, just as the supply chain's functionality impacts the spread of the disease by improving practitioners' ability to treat their patients while remaining safe themselves (Gooding, 2016). The US domestic supply chain of PPE has been unable to sufficiently increase production to meet the enormous surge in demand. A large portion of the PPE in the US is produced in other countries. Excessive reliance on off-shore producers for PPE proved problematic in earlier public health emergencies (especially the 2009 H1N1 influenza pandemic and the 2014 Ebola Virus epidemic), and this lesson appears to be repeating itself during the COVID-19 pandemic (Patel et al., 2017).
The incentive for hospitals and care providers to keep costs down has kept inventories low and driven sourcing to low-cost producers, especially in China. China's low production costs combined with high quality have made it the global leader in producing a vast range of manufactured goods, including protective face masks, gloves, and gowns. Even with the emergence of other low-cost exporters, China dominates the global market for PPE exports. Meanwhile, the US is the world's largest importer of PPE. Yet although the US is extremely dependent on the global supply chain, US manufacturers of PPE are also major exporters given the profits available in world markets.
The trade data in Table 1 show the world's four top exporters of face masks, eye protection, and medical gloves. The data is drawn from the UN Comtrade database, using trade classifications from the WHO's World Customs Organization for COVID-19 medical supplies (WHO, 2020). In these data, the category “face masks” includes textile face masks with and without a replaceable filter or mechanical parts (surgical masks, disposable face-masks, and N95 respirators); “eye protection” includes protective spectacles and goggles as well as plastic face shields; and “medical gloves” includes gloves of different materials such as rubber, cloth, and plastic (WHO, 2020). We collected data for the 2015-2019 period. Because patterns in 2015-2017 were very similar to those of 2018, the table begins with 2018.2
Table 1.
Top 4 Global Exporters and Importers of Face Masks, Eye Protection, and Medical Gloves; market shares (out of 100%) in parentheses.
|
Exports |
Imports |
||
|---|---|---|---|
| 2018 | 2019 | 2018 | 2019 |
| FACE MASKS | |||
| China (38.1%) | China (38.4%) | USA (31.7%) | USA (33.8%) |
| Germany (8.8%) | Germany (8.8%) | Japan (9.0%) | Japan (9.2%) |
| USA (8.0%) | USA (8.6%) | Germany (8.7%) | Germany (8.8%) |
| Viet Nam (4.0%) | Viet Nam (5.0%) | France (4.2%) | France (4.5%) |
| EYE PROTECTION | |||
| China (52.6%) | China (53.3%) | USA (30.3%) | USA (30.2%) |
| Hong Kong (5.4%) | Other Asia nes+ (4.8%) | Japan (6.5%) | Japan (6.7%) |
| Other Asia nes+ (4.8%) | Hong Kong (4.7%) | France (4.6%) | France (4.8%) |
| USA (4.0%) | USA (3.8%) | UK (4.4%) | UK (4.7%) |
| MEDICAL GLOVES | |||
| Malaysia (39.2%) | Malaysia (38.2%) | USA (30.7%) | USA (33.0%) |
| China (20.4%) | China (20.8%) | Germany (8.3%) | Germany (8.5%) |
| Thailand (10.4%) | Thailand (10.8%) | Japan (5.9%) | Japan (6.2%) |
| Belgium (4.6%) | Belgium (4.6%) | France (3.8%) | UK (4.1%) |
Processed by authors using UN Comtrade database for exports and imports (re-exports and re-imports are excluded). We classify COVID-19 medical supplies as: face masks are HS Codes 6307.90 and 9020.00; eye protection is HS Codes 9004.90 and 3926.20; and medical gloves are HS Codes 4015.11, 4015.19, 6116.10, and 6216.00 (WHO, 2020). As of August 2020 China and Other Asia nes had not yet reported their 2019 totals, so market shares for 2019 are approximations based on 2018 values for China and Other Asia nes.
Denotes other territories in Asia not elsewhere specified.
China is the world's largest exporter of medical face masks and eye protection, followed not far behind by the US in terms of rank. The fact that the US recently exported such large amounts of a commodity that in early 2020 was marked by extreme shortages is indicative of the lack of public health planning and political will. Unlike the case of masks and eye protection, the US is not a top exporter of medical gloves. The three largest exporters of medical gloves are all in Asia and are well endowed with natural rubber. Table 1 also shows that the US is by far the largest importer of face masks, eye equipment, and medical gloves in the world market, followed by Japan, Germany, France, and the UK. Overall, this analysis points to the high vulnerability of the US to disruptions in the global supply chain of face masks, eye protection, and medical gloves, and especially to disruptions in exports from China.
The COVID-19 outbreak in China in late 2019 led to a surge in demand within China for PPE, especially for disposable surgical masks as the government required anyone leaving their home to wear a mask. In response to demand, China's government not only restricted its PPE exports, it also purchased a substantial portion of the global supply (Burki, 2020). These shocks contributed to an exceedingly large disruption to the global supply chain of PPE. As the virus spread to other countries, their demand for PPE also increased and resulted in additional pressure on dwindling supplies. In response, other global producers of PPE, including India, Taiwan, Germany, and France, also restricted exports. By March 2020, numerous governments around the world had placed export restrictions on PPE, which in turn contributed to higher costs. The price of surgical masks rose by a factor of six, N95 respirators by three, and surgical gowns by two (Burki, 2020).
While exporting countries used trade policy to curb exports of medical supplies, up through early 2020 the US was using trade policy to protect domestic medical supply manufacturers from otherwise-less-expensive imports with import tariffs, thus raising the price of PPE faced by US hospitals and consumers. In late 2019, the average tariff rate on PPE and other medical supplies from China amounted to 25%, with proposals for additional increases underway (CRS, 2019). The Trump administration's trade war with China thus contributed to higher prices and lower availability of PPE in the US market when the crisis hit.
Overall then, with respect to imports, the US is the biggest importer and so is highly dependent on the global supply chain, and with respect to exports, the US failed to prioritize the country's public health needs. After the COVID-19 outbreak, the US was late to restrict PPE exports as other countries did, and the government failed to take the opportunity to order millions of masks in the years leading up to COVID-19 crisis, including the two-month period between when the virus was recognized in China and when local transmission was detected in the US.
The point here is not that the US should refrain from exporting PPE to other countries altogether; developing countries are dependent upon the same supply chain. Rather, in the case of PPE there is a market failure at the global scale. Healthcare and other inputs to health (particularly PPE) are intermediate goods with substantial impacts on public health that the market mechanism does not allocate in an optimal way. When the desired outcome is a public good like health, rather than monetary gain, market prices are poor directors of production and distribution.
7. Policy Recommendations and Future Research
This analysis has highlighted how markets and the implied profit motive fail to address, and in fact are a source of, the structural weakness in the US healthcare system that laid the foundation for extreme shortages of PPE during the COVID-19 outbreak. Problems with domestic demand and the global supply chain intensified the shortages. The profit motive is dysfunctional in public health because markets also fail to align the interests of the actors involved. Markets are not a good mechanism for rationing resources that are necessary for health because health is a public good. The COVID-19 crisis is not creating new problems in this sense; rather, it is sharpening and revealing existing systemic weaknesses and tensions.
Our analysis did not explicitly reference the gendered dimensions of PPE shortages, but there are several. First, because nurses generally have more direct contact with patients, and nearly 90% of nurses are women, women healthcare workers also bear disproportionately greater risk of exposure to infectious diseases. Overall, women are 75.4% of healthcare practitioners and those in technical occupations and 86.9% of those in healthcare support occupations in the US (authors' calculations from 2019 Current Population Survey data).3 Yet the majority of PPE that is available is designed for men, meaning that women are often left grappling with poorly fitted PPE, especially oversized gloves, goggles, and masks (Criado-Perez, 2019). Further, the overrepresentation of women in healthcare means that under-provision of PPE has gendered impacts. Hence the seemingly gender-neutral costing model described in our analysis does not have gender-neutral outcomes. By implication, a meaningful change in the way healthcare is funded that incentivizes hospitals to invest in adequate inventories of PPE will disproportionately benefit women workers. The gender differential is even more striking in the case of home-health aides. More research is needed on the extent to which men and women are impacted differently by PPE shortages. Another important question is the extent to which gender issues - such as women's relative lack of bargaining power in hospital administration - contributed to shortages to begin with.
Our analysis points to the need for transformative changes and corrective actions to better protect healthcare practitioners. We must consider a full range of tools that not only create incentives for hospitals to protect their practitioners with PPE, but also generate effective institutional capacity to ensure that healthcare providers can mobilize quickly to handle pandemics. We have several recommendations:
(1) prepare hospitals to better protect practitioners by removing the profit motive from consideration in the purchasing and maintenance of PPE inventories;
(2) strengthen the capacity of local, state, and federal government to maintain and distribute stockpiles;
(3) improve enforcement of OSHA's current regulations around PPE, including requirements to source the proper size for each employee;
(4) develop new regulations to reduce practitioner stress and fatigue (Cohen and Venter, 2020; Fairfax, 2020);
(5) improve the federal government's ability to coordinate supply and distribution across hospitals and local and state governments (Patel et al., 2017);
(6) consider strategic industrial policy to increase US production of medical supplies and to reduce the dependence on the global supply chain for PPE;
(7) consider industrial policy to incentivize PPE production using existing technology while encouraging development, testing, and production of higher-quality, reusable PPE.
These changes will address the costing-model issue, the demand problem, the federal government failures, and supply chain vulnerability, but they will not be politically palatable. Creating the institutional capacity for building and maintaining a viable stockpile of PPE will contribute to all of these policy options. Such shifts will help set the stage for what global health should look like moving forward. COVID-19 was not the first pandemic nor will it be the last, especially given the likely impacts of climate change.
CRediT authorship contribution statement
Jennifer Cohen: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing - original draft, Writing - review & editing, Visualization. Yana van der Meulen Rodgers: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing - original draft, Writing - review & editing, Visualization.
Acknowledgements
The authors thank Jacquelyn Baugher, RN, BSN, OCN, for providing insight that aided our understanding of occupational relations internal to hospitals. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
The full dataset is available at doi:https://doi.org/10.6084/m9.figshare.12751850
The full dataset is available at doi:https://doi.org/10.6084/m9.figshare.12915866.v1
The full dataset and data specifically for healthcare workers are available at doi:https://doi.org/10.6084/m9.figshare.12751838
References
- Azar A. 2020. Congressional Testimony: Health and Human Services Fiscal Year 2021 Budget Request. (C-span) [Google Scholar]
- Bai G., Anderson G.F. A more detailed understanding of factors associated with hospital profitability. Health Aff. 2016;35(5):889–897. doi: 10.1377/hlthaff.2015.1193. [DOI] [PubMed] [Google Scholar]
- Barniv, R., Danvers, K., & Healy, J. (2000). The impact of medicare capital prospective payment regulation on hospital capital expenditures. Journal of Accounting and Public Policy, 19(1), 9-40. Doi:doi: 10.1016/S0278-4254(99)00026-5. [DOI]
- Burki T. Global shortage of personal protective equipment. Lancet Infect. Dis. 2020;20(7):785–786. doi: 10.1016/S1473-3099(20)30501-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabral, Xu L. Seller Reputation and Price Gouging: Evidence from the COVID-19 Pandemic. 2020. http://leixu.org/xu_price_gouging.pdf Retrieved from. [DOI] [PMC free article] [PubMed]
- Carias C., Rainisch G., Shankar M., Adhikari B.B., Swerdlow D.L., Bower W.A.…Koonin L.M. Potential Demand for Respirators and Surgical Masks During a Hypothetical Influenza Pandemic in the United States. Clinical Infectious Diseases. 2015;60(suppl_1):S42–S51. doi: 10.1093/cid/civ141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC Considerations for Release of Stockpiled N95s Beyond the Manufacturer-Designated Shelf Life. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/release-stockpiled-N95.html Retrieved from.
- CDC Coronavirus Disease 2019 (COVID-19): Cases, Data & Surveillance. 2020. https://covid.cdc.gov/covid-data-tracker/#health-care-personnel Retrieved from.
- Cerminara K.L. Contextualizing ADR in managed care: a proposal aimed at easing tensions and resolving conflict. Loy. U. Chi. LJ. 2001;33:547. [Google Scholar]
- Cohen J. COVID-19 capitalism: the profit motive versus public health. Public Health Ethics. 2020 doi: 10.1093/phe/phaa025. [DOI] [Google Scholar]
- Cohen J. Theorizing Entrepreneurial Price Gouging: Interdependency, Injustice, and Hand Sanitizer. Rethinking Marxism Dossier. 20202020:205–214. http://rethinkingmarxism.org/Dossier2020/21_Cohen.pdf [Google Scholar]
- Cohen J., Venter W.D.F. The integration of occupational- and household-based chronic stress among south African women employed as public hospital nurses. PLoS One. 2020;15(5) doi: 10.1371/journal.pone.0231693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Criado-Perez C. Harry N. Abrams; New York, NY: 2019. Invisible Women: Data Bias in a World Designed for Men. [Google Scholar]
- CRS U.S.-China tariff actions by the numbers. 2019. https://fas.org/sgp/crs/row/R45949.pdf Washington, DC Retrieved from.
- Devi S. US public health budget cuts in the face of COVID-19. Lancet Infect. Dis. 2020;20(4):415. doi: 10.1016/S1473-3099(20)30182-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emanuel E.J., Persad G., Upshur R., Thome B., Parker M., Glickman A.…Phillips J.P. Fair Allocation of Scarce Medical Resources in the Time of Covid-19. New England Journal of Medicine. 2020;382(21):2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- Fairfax R.E. The occupational safety and health Administration’s impact on employers: what worked and where to go from Here. Am. J. Public Health. 2020;110(5):644–645. doi: 10.2105/AJPH.2020.305624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friese C.R., Veenema T.G., Johnson J.S., Jayaraman S., Chang J.C., Clever L.H. Respiratory protection considerations for healthcare workers during the COVID-19 pandemic. Health Security. 2020;18(3):237–240. doi: 10.1089/hs.2020.0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganczak M., Szych Z. Surgical nurses and compliance with personal protective equipment. J. Hosp. Infect. 2007;66(4):346–351. doi: 10.1016/j.jhin.2007.05.007. [DOI] [PubMed] [Google Scholar]
- Gershon R.R.M., Karkashian C.D., Grosch J.W., Murphy L.R., Escamilla-Cejudo A., Flanagan P.A.…Martin L. Hospital safety climate and its relationship with safe work practices and workplace exposure incidents. American Journal of Infection Control. 2000;28(3):211–221. doi: 10.1067/mic.2000.105288. [DOI] [PubMed] [Google Scholar]
- Gooding E.J. (Massachusetts Institute of Technology); 2016. A Mixed Methods Approach to Modeling Personal Protective Equipment Supply Chains for Infectious Disease Outbreak Response. [Google Scholar]
- Govinfo The Ebola Crisis: Coordination of a Multi-Agency Response. 2014. https://www.govinfo.gov/content/pkg/CHRG-113hhrg94053/pdf/CHRG-113hhrg94053.pdf Retrieved from.
- Hall R.E., Jones C.I. The value of life and the rise in health spending*. Q. J. Econ. 2007;122(1):39–72. doi: 10.1162/qjec.122.1.39. [DOI] [Google Scholar]
- Hersi M., Stevens A., Quach P., Hamel C., Thavorn K., Garritty C.…Moher D. Effectiveness of Personal Protective Equipment for Healthcare Workers Caring for Patients with Filovirus Disease: A Rapid Review. PLOS ONE. 2015;10(10) doi: 10.1371/journal.pone.0140290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HHS . Public Health Emergency; 2020. Strategic National Stockpile.https://www.phe.gov/about/sns/Pages/default.aspx Retrieved from. [Google Scholar]
- Kamerow D. Covid-19: the crisis of personal protective equipment in the US. BMJ. 2020;369:m1367. doi: 10.1136/bmj.m1367. [DOI] [PubMed] [Google Scholar]
- Liverman C.T., Goldfrank L.R. National Academies Press; 2007. Preparing for an influenza pandemic: Personal protective equipment for healthcare Workers. [Google Scholar]
- Livingston E., Desai A., Berkwits M. Sourcing personal protective equipment during the COVID-19 pandemic. JAMA. 2020;323(19):1912–1914. doi: 10.1001/jama.2020.5317. [DOI] [PubMed] [Google Scholar]
- MacIntyre C.R., Wang Q., Rahman B., Seale H., Ridda I., Gao Z.…Dwyer D.E. Efficacy of face masks and respirators in preventing upper respiratory tract bacterial colonization and co-infection in hospital healthcare workers. Preventive Medicine. 2014;62:1–7. doi: 10.1016/j.ypmed.2014.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madara J. Letter from American Medical Association to Vice President Michael Pence. 2020. https://searchlf.ama-assn.org/undefined/documentDownload?uri=%2Funstructured%2Fbinary%2Fletter%2FLETTERS%2F2020-6-30-Letter-to-Pence-re-PPE.pdf Retrieved from.
- Maloney C. U.S. House of Representatives. 2020. Memorandum: Information provided by medical distribution companies on challenges with white house supply chain task force and project Airbridge.https://oversight.house.gov/sites/democrats.oversight.house.gov/files/documents/Project%20Airbridge%20Memo%2007-02-20.pdf Retrieved from. [Google Scholar]
- Mason D.J., Friese C.R. 2020. Protecting Health Care Workers against COVID-19—And Being Prepared for Future Pandemics. (Paper presented at the JAMA Health Forum) [DOI] [PubMed] [Google Scholar]
- McLellan R.K. Work, health, and worker well-being: roles and opportunities for employers. Health Aff. 2017;36(2):206–213. doi: 10.1377/hlthaff.2016.1150. [DOI] [PubMed] [Google Scholar]
- Medscape . Medscape Medical News; 2020. In Memoriam: Healthcare Workers Who Have Died of COVID-19.https://www.medscape.com/viewarticle/927976#vp_1 Retrieved from. [Google Scholar]
- Moses H., III, Matheson D.H.M., Dorsey E.R., George B.P., Sadoff D., Yoshimura S. The anatomy of health care in the United States. JAMA. 2013;310(18):1947–1964. doi: 10.1001/jama.2013.281425. [DOI] [PubMed] [Google Scholar]
- Nichol K., McGeer A., Bigelow P., O’Brien-Pallas L., Scott J., Holness D.L. Behind the mask: determinants of nurse’s adherence to facial protective equipment. Am. J. Infect. Control. 2013;41(1):8–13. doi: 10.1016/j.ajic.2011.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NNU New survey of nurses provides frontline proof of widespread employer, government disregard for nurse and patient safety, mainly through lack of optimal PPE. 2020. https://www.nationalnursesunited.org/press/new-survey-results Retrieved from.
- O’Boyle C., Robertson C., Secor-Turner M. Nurses’ beliefs about public health emergencies: fear of abandonment. Am. J. Infect. Control. 2006;34(6):351–357. doi: 10.1016/j.ajic.2006.01.012. [DOI] [PubMed] [Google Scholar]
- OSHA Employer Payment for Personal Protective Equipment; Final Rule. 2007. https://www.osha.gov/laws-regs/federalregister/2007-11-15-0 Retrieved from Washington, DC.
- Patel A., D’Alessandro M.M., Ireland K.J., Burel W.G., Wencil E.B., Rasmussen S.A. Personal protective equipment supply chain: lessons learned from recent public health emergency responses. Health Security. 2017;15(3):244–252. doi: 10.1089/hs.2016.0129. [DOI] [PubMed] [Google Scholar]
- Pelosi N. Cramer; Mad Money, CNBC: 2020. Transcript of Pelosi Interview on CNBC’s Mad Money with Jim Cramer/Interviewer: J. [Google Scholar]
- Rosen S. The theory of equalizing differences. Handbook of labor economics. 1986;1:641–692. [Google Scholar]
- Rosen J. Rosen, Homeland Security Committee Colleagues Demand Answers from Administration on Strategic National Stockpile. 2020. https://www.rosen.senate.gov/rosen-homeland-security-committee-colleagues-demand-answers-administration-strategic-national Retrieved from.
- Rosenbaum S., Kindig D.A., Bao J., Byrnes M.K., O’Laughlin C. The value of the nonprofit hospital tax exemption was $24.6 billion in 2011. Health Aff. 2015;34(7):1225–1233. doi: 10.1377/hlthaff.2014.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowan M. Letter from health industry distributors association. March. 2020;28:2020. https://oversight.house.gov/sites/democrats.oversight.house.gov/files/BBS000001-BBS000002%20redacted.pdf Retrieved from. [Google Scholar]
- Rowan N.J., Laffey J.G. Challenges and solutions for addressing critical shortage of supply chain for personal and protective equipment (PPE) arising from coronavirus disease (COVID19) pandemic - case study from the Republic of Ireland. Sci. Total Environ. 2020;725:138532. doi: 10.1016/j.scitotenv.2020.138532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sax H., Perneger T., Hugonnet S., Herrault P., Chraïti M.-N., Pittet D. Knowledge of standard and isolation precautions in a large teaching hospital. Infection Control & Hospital Epidemiology. 2005;26(3):298–304. doi: 10.1086/502543. [DOI] [PubMed] [Google Scholar]
- Segal P. Infection Control Today(October 17) 2016. The role of personal protective equipment in infection prevention history.https://www.infectioncontroltoday.com/view/q-and-a-nearly-all-healthcare-workers-fighting-covid-19-need-n95s Retrieved from. [Google Scholar]
- Viscusi W.K. The value of risks to life and health. J. Econ. Lit. 1993;31(4):1912–1946. www.jstor.org/stable/2728331 Retrieved from. [Google Scholar]
- WEF Global Risks Report 2015. 2015. https://reports.weforum.org/global-risks-2015/ Retrieved from Geneva.
- WEF Global Risks Report 2020. 2020. https://www.weforum.org/reports/the-global-risks-report-2020 Retrieved from Geneva.
- Whitehouse.gov Memorandum on Order Under the Defense Production Act Regarding 3M Company. 2020. https://www.whitehouse.gov/presidential-actions/memorandum-order-defense-production-act-regarding-3m-company/ Retrieved from.
- WHO HS classification reference for Covid-19 medical supplies. 2020. http://www.wcoomd.org/-/media/wco/public/global/pdf/topics/facilitation/activities-and-programmes/natural-disaster/covid_19/hs-classification-reference_en.pdf?la=en Retrieved from.
- Yarbrough M.I., Ficken M.E., Lehmann C.U., Talbot T.R., Swift M.D., McGown P.W.…Oke C.A. Respirator Use in a Hospital Setting: Establishing Surveillance Metrics. Journal of the International Society for Respiratory Protection. 2016;33(1):1–11. https://pubmed.ncbi.nlm.nih.gov/27594764 Retrieved from. [PMC free article] [PubMed] [Google Scholar]