ABSTRACT
BACKGROUND:
Diabetic foot ulcers (DFU) are a critical complication of diabetes mellitus (DM) affecting life quality and significantly impacting healthcare resources.
OBJECTIVE:
Determine the direct medical costs associated with treating DFU in King Fahad Hospital of the University and identify factors that could assist in developing resource management guidelines in Saudi Arabia.
DESIGN:
Retrospective study.
SETTING:
SETTING: King Fahad Hospital of the University, Al-Khobar, Saudi Arabia.
PATIENTS AND METHODS:
The study included diabetic patients admitted with foot ulcerations between 2007 and 2017 inclusive. We determined management costs including drug usage, wound dressings, surgical procedures, admissions, and basic investigation.
MAIN OUTCOME MEASURES:
Factors affecting the direct perspective medical costs of managing DFU.
SAMPLE SIZE:
99 patients.
RESULTS:
The overall cost of managing 99 patients with DFU was 6 618 043.3 SAR ($1 764 632.68 USD), which further translates to approximately 6684.9 SAR per patient/year ($1782.6 USD). The highest cost incurred was for admission expenditure (45.6%), followed by debridement (14.5%) and intensive care unit (ICU) admission (10.4%).
CONCLUSION:
The overall healthcare expenditure in treating DFU is high, with hospital admissions and surgical procedures adding a significant increase to the total cost. Focused patient education on overall glycemic control and prevention of DFU may decrease complications and hence, the overall cost.
LIMITATIONS:
Identified only the direct medical costs of DFU as the indirect costs were subjective and more difficult to quantify.
CONFLICT OF INTEREST:
None.
INTRODUCTION
Diabetic foot ulcers (DFUs) are a complication associated with diabetes mellitus (DM) that result from peripheral neuropathy and peripheral vascular disease. Feet deformed by ill-fitting shoes, walking barefoot, neuropathy or an acute injury are susceptible to chronic ulcers, and continued walking on the affected foot may lead to impaired healing. As well, vascular diseases may cause painful and ischemic foot ulcers through minor trauma.1 Chronic, non-healing DFUs may even lead to increased morbidity and mortality rates.2,3
To improve the outcomes of DFU, treatment protocols must include optimal blood sugar control, effective local wound care, control of sepsis, the reduction of pressure areas and the restoration of blood flow to the affected area.4 The selection of specific antibiotic agents for the treatment of DFU depends on the causative pathogen. Antibiotic resistance in patients with DFUs may be a significant determinant in recovery rates,5 with methicillin-resistant staphylococcus aureus as the predominant infection resulting in lengthier hospitalization and increased costs. For example, a population-based study in the United States by McKinnon et al reported that the cost per patient treated with ampicillin/sulbactam was 603.35 USD, as compared with 1306.92 USD for patients treated by imipenem/cilastatin.5
Appropriate choices in wound dressings factor greatly in the healing of DFUs. Since there are few studies on the most cost-effective wound dressing for each specific wound type, healthcare professionals typically make their choices based on the site and clinical appearance of the wound.6,7 Treatment may also include debridement with wound cleaning; an invasive procedure often requiring multiple sessions. Additionally, over 50% of lower limb amputations performed are on patients with diabetes mellitus.8 These patients typically require a longer hospital stay, are at risk of increased mortality and have a low rehabilitation rate; increasing the overall economic impact.8 Furthermore, approximately 50% of patients undergoing an amputation develop a DFU on the remaining limb within 18 months of the surgery.8
DFUs are a major economic burden for any health-care system. It has been estimated to cost around 16 000 USD for the management of a simple DFU, which may exceed 30 000 USD when a major amputation is required.9,10 Topical treatments on an outpatient basis account for approximately 51% of all costs. However, due to the length of treatment time between initial diagnosis and healing, surgical management may be the most cost-effective option for DFU and in this case, surgical intervention would account for 95% of the total cost, with antibiotics consuming approximately 4% of the total.11
To date, there are no studies detailing the cost of treating DFUs in Saudi Arabia, with its hybrid of private and publicly-funded patient care. Studies on diabetic foot-related healthcare costs are sometimes difficult to compare as a result of disparate healthcare systems, reimbursement methods and care delivery models.11 Regardless of the payment option, the work to improve outcomes and minimize the cost of treatment for chronic diseases will help improve resource allocation and provide a better life for patients.
METHODS
The study included all diabetic patients admitted to King Fahad Hospital of the University (KFHU), Al-Khobar, Saudi Arabia between 2007 and 2017 with a diagnosis of a diabetic foot ulcer or a diabetic foot infection. We excluded diabetic patients with DFU who were admitted to the hospital for another medical illness, outpatients, and deceased patients or those with incomplete hospital records. As the cost of care provided to patients in Saudi Arabian Ministry of Health hospitals is fully supported by the government, we were unable to ascertain the exact cost of each individual patient. Thus, in our quest to reach the desired goal of our research, we compared direct perspective medical costs against two private hospitals in the same region and considered the average. The cost of surgical procedures for patients undergoing either local tissue debridement or amputation (major or minor) was determined by the site of the procedure and the level of the amputation. In this study, we took the average cost for each.
Dressings used were either saline, povidone, or antimicrobial impregnated dressings such as Silvercel and Aquacel. We considered the average cost of dressings based on the standard practices in the hospital i.e. (<3 days, a simple dressing, 3-7 days, Silvercel every other day, >7 days Aquacel and Neugel). Antibiotic therapy was generally prescribed empirically and modified based on tissue culture and sensitivity results. The most frequent antibiotic regimen included the following: amoxicillin and clavulanate 1.2 gm IV [3 doses a day for 7 days], clindamycin 600 mg IV [4 times a day for 5 days], ciprofloxacin 400 IV [2 times per day for 7 days], piperacillin/tazobactam 4.5 gm IV [4 times per day for 7 days], or meropenem 1 gm IV [3 times per day for 14 days]. We referred to the hospital's inpatient pharmacy for the cost of the antibiotics. Admission costs included a bed in the general ward and/or intensive care unit. Other costs related to hematological and radiological investigations, swab or tissue cultures, physiotherapy and reconstruction were also considered (Appendix I).
Data analysis was performed using the IBM SPSS version 21 (Armonk, NY: IBM Corp). Numerical variables and normality were determined with a Shapiro Wilk test. For numerical variables that followed a normal distribution, values were summarized as mean and standard deviation. For numerical values that did not follow a normal distribution, the values were summarized as median and interquartile range (expressed as 25th–75th percentile). Qualitative data were expressed in terms of frequencies and percentages. Patients were distributed to two groups according to the average of the total cost: either as high cost or low cost. Mann–Whitney U test and Fisher's exact tests were carried out to identify the characteristics of patients who were associated with high cost. Significance was determined at P<.05 to interpret the results of the tests.
RESULTS
Of 186 diabetic patients admitted to KFHU between 2007 and 2017 that were initially selected for this study, 87 patients were excluded due to unclear information in their files. This analysis examined a total of 99 patients. The mean age was 62.1 (12.9) years (Table 1). Men accounted for 70.7%, and 74.7% were of Saudi nationality. Only 8.1% of patients had HbA1C levels within an acceptable range (less than 6 g/dL), while the vast majority of patients (83.8%) had higher levels, indicating poor glycemic control. Most patients were diagnosed with chronic diseases (hypertension, dyslipoproteinemia, peripheral vascular diseases, coronary artery disease and other cardiovascular disorders. Ulcers were located in the plantar aspect of the foot and toe.
Table 1.
Sociodemographic data of the study population (n=99).
| Age (years) | |
|---|---|
| Minimum-maximum | 29.0 - 95.0 |
| Mean (standard deviation) | 62.1 (12.9) |
| <40 | 6 (6.1) |
| 40–59 | 38 (38.4) |
| ≥60 | 55 (55.6) |
| Sex | |
| Male | 70 (70.7) |
| Female | 29 (29.3) |
| Nationality | |
| Saudi | 74 (74.7) |
| Non-Saudi | 25 (25.3) |
| Body mass index (mg/kg2) | |
| Minimum-maximum | 22.0 – 52.6 |
| Mean (standard deviation) | 30.1 (7.2) |
| Glycated hemoglobin (g/dL) | |
| Minimum-maximum | 2.17 - 14.7 |
| Mean (standard deviation) | 8.7 (3.6) |
| Glycemic control (based on glycated hemoglobin) | |
| Yes | 8 (8.1) |
| No | 83 (83.8) |
| Hypertension | |
| Yes | 73 (73.7) |
| No | 26 (26.3) |
| Dyslipoproteinemia | |
| Yes | 54 (54.5) |
| No | 45 (45.5) |
| Peripheral vascular disease | |
| Yes | 33 (33.3) |
| No | 66 (66.7) |
| Coronary heart disease | |
| Yes | 31 (31.31) |
| No | 68 (68.68) |
| Site of ulcer | |
| Foot | 61 (61.6) |
| Plantar | 42 (42.4) |
| Dorsal | 19 (19.2) |
| Toe | 27 (27.3) |
| Plantar | 19 (19.2) |
| Dorsal | 8 (8.1) |
Data are number (%) unless otherwise noted.
The maximum hospital length of stay was 144 days (Table 2). The mean of hospital admissions for patients with DFU was 1.7 (1.1) times, whereas half of non-DFU diabetic patients were admitted only once, with one-third being admitted twice. Tissue cultures were ordered in most cases (84.8%), with the number of required wound culture tests varying from 1-62, and a median of 3 tests (Table 3). Wound debridement was performed either at the bedside or surgically for 73.7% of the patients, ranging between 1 and 60 times, with a median of 1. Amputation was performed for 39.4% of the patients, and 7.1% underwent multiple amputations. In 5.1% of cases, limb reconstruction (revascularization and flap reconstruction) was performed, totaling 5 cases.
Table 2.
Total length of stay in the hospital, number of admission with DFU of each patient, length of stay in unit and ICU in the hospital, number of tissue cultures and swab culture ordered of the studied patients.
| Hospital length of stay of each patient | |
|---|---|
| Minimum-maximum | 2.0-144.0 |
| Mean (standard deviation) | 26.26 (25.1) |
| Number of admissions with diagnosis of diabetic foot of each patient | |
| Minimum-maximum | 1.0-9.0 |
| Mean (standard deviation) | 1.7 (1.1) |
| Once | 53 (53.5) |
| Twice | 32 (32.3) |
| Three or more | 14 (14.1) |
| Intensive care unit admission | |
| Yes | 10 (10.1) |
| No | 89 (89.9) |
| Length of stay in ICU (days) | |
| Minimum-maximum | 1.0-65.0 |
| Median (interquartile range) | 6.0 (3.0-10.0) |
| Length of stay in the unit (days) | |
| Minimum-maximum | 2.0-97.0 |
| Median (interquartile range) | 18.0 (8.0–33.0) |
| Tissue culture | |
| Yes | 84 (84.8) |
| No | 15 (15.2) |
| Wound swab culture | |
| Minimum-maximum | 1.0-62.0 |
| Median (interquartile range) | 3.0 (1.0-7.0) |
Data are number (%) unless otherwise noted.
Table 3.
Treatment provided to study population (n=99).
| Debridement | |
|---|---|
| Yes | 73 (73.7) |
| No | 26 (26.3) |
| Number of amputation | |
| None | 60 (60.6) |
| One | 32 (32.3) |
| Major | 9 (9.1) |
| Minor | 22 (22.2) |
| Two | 7 (7.1) |
| Major | 7 (7.1) |
| Minor | 6 (6.1) |
| Revascularization and flap reconstruction | |
| Yes (one time) | 5 (5.1) |
| No | 94 (94.9) |
| Number of dressing/day | |
| None | 3.0 (3.0) |
| One | 64 (64.6) |
| Two | 32 (32.3) |
| Type of dressing | |
| Simple dressing | 93 (93.9) |
| Pressure | 1 (1.0) |
| Neugel | 1 (1.0) |
| Aquacel | 2 (2.0) |
| Silvercel | 1 (1.0) |
| Unknown | 1 (1.0) |
| Duration of antibiotics | |
| Minimum-maximum | 0.0-83.0 |
| Median (interquartile range) | 19.0 (11.0-31.0) |
| Physiotherapy | |
| Yes | 9 (9.1) |
| No | 90 (90.9) |
| Duration of physiotherapy (days) | |
| Minimum-maximum | 2.0-16.0 |
| Mean (standard deviation) | 11.5 (6.4) |
Data are number (%) unless otherwise noted.
Dressings were provided for 96.9% of patients, with one change per day in 64.6% and twice daily in 32.3% of cases. A simple dressing was most commonly used in conjunction with penicillin for 93.9% of the patients. The median duration of antibiotic administration was 19 days.
Despite the importance of physiotherapy, it was provided in only 9 cases (9.1%) with an average duration of 11.5 (6.4) days. In most cases (62.6%), a combination of antibiotics was used in the management of acute DFU infection with penicillin prescribed in 30.3% of cases (Figure 1).
Figure 1.
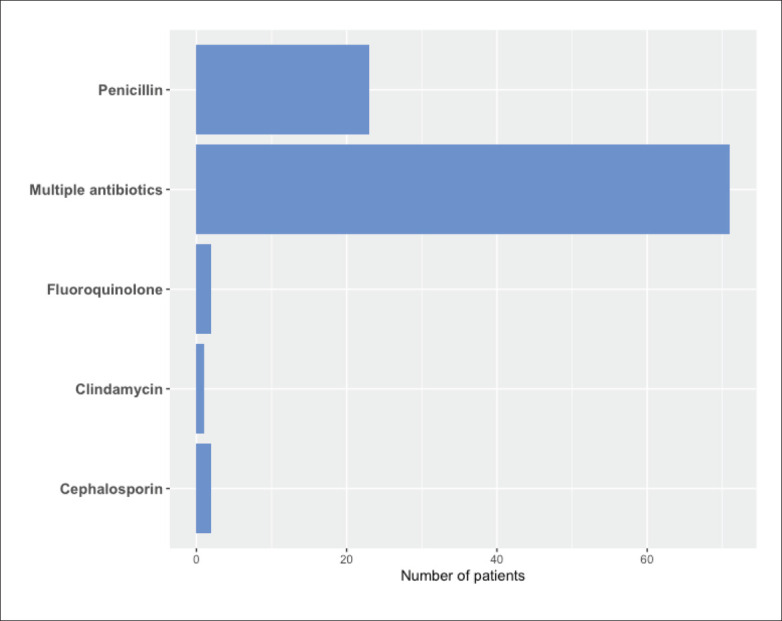
Antibiotics used in treatment of acute diabetic foot ulcer infection in the study patients (n=99).
The overall cost for managing 99 patients with DFU over a 10-year period was 6 618 043.3 SAR (1 764 632.68 USD) with a mean cost of 66,848.9 SAR/patient (17 827.10 USD/patient) (Table 4). Expenditure for one year was estimated to be 661,804.3 SAR (443 165.77 USD).
Table 4.
Cost of management of diabetic foot ulcers.
| Minimum | Maximum | Mean | Standard deviation | Total | Percent of the overall total | |
|---|---|---|---|---|---|---|
| Admission in ward | 2420.00 | 117 370.0 | 30482.22 | 27 474.32 | 3017 740 | 45.6 |
| Admission in ICU | .0 | 390 000.0 | 6969.69 | 40 510.38 | 690 000 | 10.4 |
| HgA1c test | .0 | 2281.5 | 435.3 | 296.5 | 43 095 | 0.7 |
| Tissue culture | .0 | 508.0 | 431.0 | 183.1 | 42 672 | 0.6 |
| Swab culture | .0 | 10230.0 | 881.7 | 1482.4 | 87 285 | 1.3 |
| Debridement | .0 | 210 000.0 | 9722.2 | 25 414.3 | 962 500 | 14.5 |
| Major amputation | .0 | 20 000.0 | 1616.2 | 3965.9 | 160 000 | 2.4 |
| Minor amputation | .0 | 10 000.0 | 1186.9 | 2324.0 | 117 502 | 1.8 |
| Revascularization and flap Reconstruction | .0 | 41 650.0 | 2103.5 | 9167.1 | 208 250 | 3.2 |
| Dressing | .0 | 20 800.0 | 4142.9 | 3985.9 | 410 150 | 6.2 |
| Physiotherapy | .0 | 10 800.0 | 393.9 | 1620.5 | 39 000 | .6 |
| Antibiotics | .0 | 24 275.6 | 4631.7 | 3155.0 | 458 539.3 | 6.9 |
| Investigations | .0 | 2277.0 | 434.4 | 295.9 | 43 010 | 0.7 |
| X-ray | .0 | 810.0 | 154.6 | 105.3 | 15 300 | 0.2 |
| Computed tomography scan | .0 | 17 100.0 | 3262.6 | 2222.4 | 323 000 | 4.9 |
| Total cost for all patients | 9603.8 | 536 665.6 | 66 848.9 | 72 383.3 | 661 8043.3 | 100.0 |
Saudi riyals and US dollars based on the rate: 1 USD =3.75 SAR as per the Saudi Arabian Monetary Authority, 15/10/2018.
The highest contributors to the cost at 45.6% was admission expenditure followed by debridement representing 14.5%; ICU admission, representing 10.4%; antibiotics (representing 6.9%; and dressings, representing 6.2%. X-rays were the lowest expenditure, representing 0.2% (Figure 2).
Figure 2.
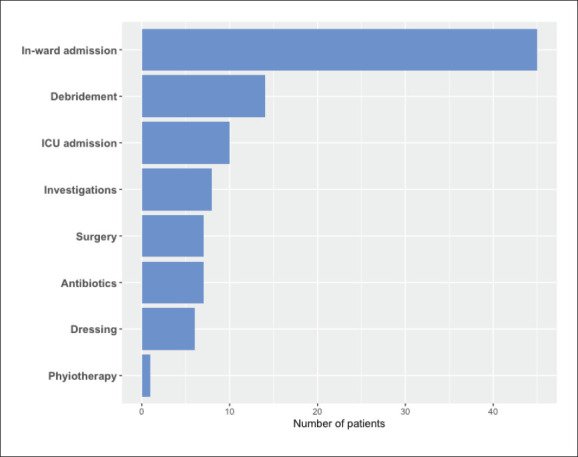
Contributions to the cost of management in the study patients (n=99).
Patients diagnosed with diabetic foot complications who were admitted more than once had a higher mean total cost when compared to patients admitted only once. Similarly, the patients admitted to the unit more than once had a higher mean compared to patients admitted only once. Patients who received debridement more than once had a higher mean of expenditure compared to the group of patients who underwent either one or no debridements. Patients who underwent amputation had a higher mean of total expenditure compared to the group requiring no amputation. There was a higher mean of total expenditure in patients who underwent reconstructive plastic surgery compared to the group who did not require this surgery. A higher mean of total expenditure was observed in the group of patients who received a wound coverage other than a simple dressing. This is an important illustration of the impact dressing choices have on total treatment expenditure. Though other dressings including Silvercel, Aquacel, Neugel and pressure dressings were used only for six patients, their mean price was nearly equal to the mean simple dressing price of the remaining 93 patients.
The mean of total expenditure was more in the group of patients who received penicillin along with adjunctive therapy compared with the groups who received either only penicillin or only cephalosporins (Table 5). There was a higher mean of total expenditure in the group of patients who were admitted into the ICU.
Table 5.
Descriptive statistics of the costs of each management plan or procedure.
| Cost | N | |
|---|---|---|
| Admission in unit | ||
| More than once | 99 564.21 (88 738.402) | 47 |
| Once | 35 592.21 (31 240.753) | 50 |
| Total | 66 588.95 (72 829.468) | 97 |
| Number of debridements | ||
| >1 | 95 401.76 (67 039.634) | 36 |
| 1 | 50 533.011 (70 714.593) | 63 |
| Total | 66 848.922 (72 383.33) | 99 |
| Cost of amputation | ||
| No | 45 059.29 (51 376.89) | 60 |
| Yes | 10 0371.42 (86 664.29) | 39 |
| Total | 66 848.92 (72 383.33) | 99 |
| Cost of revascularization and flap reconstruction | ||
| No | 60 635.46 (65 717.83) | 94 |
| Yes | 18 3661.85 (99 936.373) | 5 |
| Total | 66 848.92 (72 383.33) | 99 |
| Cost of dressings | ||
| Others | 68 418.53 (65 633.902) | 6 |
| Simple dressing | 66 747.65 (73 121.488) | 93 |
| Total | 66 848.9222 (72 383.330) | 99 |
| Cost of antibiotics | ||
| Penicillin + Adjunct | 70 289.63 (75 310.479) | 65 |
| Penicillin | 66 036.02 (69 353.1) | 30 |
| Cephalosporin | 17 034.04 (9452.588) | 4 |
| Total | 66 848.92 (72 383.33) | 99 |
| Cost of physiotherapy | ||
| No | 58 423.38 (54 016.372) | 90 |
| Yes | 151 104.27 (151 449.178) | 9 |
| Total | 66 848.92 (72 383.33) | 99 |
| Admission in ICU | ||
| No | 58 803.59 (54 791) | 89 |
| Yes | 138 452.34 (146 152.116) | 10 |
| Total | 66 848.9222 (72 383.33) | 99 |
Cost are mean (standard deviation).
The univariate analysis saw a significant difference (P<.05) between the high cost group and the low cost group regarding total length of hospital stay (Table 6). Additionally, there was a significant difference (P<.05) in the cost between the group of patients for whom tissue culture, wound swab culture and debridement was performed either once or more than once. The total cost per patient was significantly high (P<.05) for those who underwent amputation, either minor or major. The analysis also revealed that the addition of reconstructive plastic surgery resulted in significantly higher costs. A considerable difference was also found in the dressing cost between the two groups. We conclude that the length of hospital stay, number of tissue cultures, number of wound swab cultures, minor and major amputations, revascularization/flap reconstructions and the number of dressing changes per day all are important contributors to the cost of treating DFU patients.
Table 6.
Univariate analyses of multiple variables to identify risk factors of high cost expenditure.
| Variable | High cost (n=50) | Low cost (n=49) | P value |
|---|---|---|---|
| Patient characteristics | |||
| Age (years) | 62.98 (13.05 (29-90) | 61.16 (12.92 (29-95) | .787 |
| Gender (Male/Female) | 37/13 | 33/16 | .469 |
| Body mass index | 5.64 (11.53) | 10.83 (15.79) | .385 |
| Hemoglobin A1c | 8.36 (4.21) | 9.02 (2.83) | .196 |
| Comorbidity | |||
| Hypertension (Yes/No) | 35/15 | 38/11 | .396 |
| Dyslipidemia (Yes/No) | 27/23 | 27/22 | .913 |
| Peripheral vascular disease (Yes/No) | 20/30 | 13/36 | .157 |
| Coronary heart disease (Yes/No) | 15/35 | 16/33 | .777 |
| Length of hospital stay | |||
| Total LOS | 42.56 (26.53) (9-144) | 9.71 (5.36) (2-23) | .001 |
| Intensive care unit admission (days) | 2.30 (9.40) | - | .206 |
| Ward admission (days) | 40.36 (22.99) | 9.71 (5.37) | .001 |
| Procedure | |||
| No. of tissue cultures | .92 (.27) | .77 (.42) | .045 |
| No. of swab cultures | 9.04 (11.46) | 1.57 (1.35 | .001 |
| No. of debridements | 4.62 (9.89) | .89 (.77) | .045 |
| Minor amputation | .002 | ||
| None | 28 | 43 | |
| Once | 20 | 5 | |
| Twice | 2 | 1 | |
| Major amputation | .009 | ||
| None | 37 | 47 | |
| Once | 12 | 2 | |
| Twice | 1 | 0 | |
| Revascularization and flap reconstruction (Yes/No) | 5/45 | 0/49 | .024 |
| Location of the ulcer | |||
| Dorsal vs planter (dorsal/planter) | 11/34 | 16/27 | .197 |
| Foot vs toes (foot/toes) | 32/14 | 32/14 | .999 |
| Wound care | |||
| No. of dressing/day | .01 | ||
| Once | 39 | 25 | |
| Twice | 11 | 21 | |
| Vacuum-assisted closure (duration in days) | 1.7 (5.40) | 0 | .390 |
| Others | |||
| Duration of antibiotics (days) | 34.28 (21.27) | 13.81 (8.20) | .141 |
| Physiotherapy (days) | 2.56 (7.42) | .04 (.28) | .389 |
Data are number (%) or mean (standard deviation) (range).
DISCUSSION
The rate of diabetes mellitus in Saudi Arabia is on an alarming upswing, with diabetic foot ulcer a major complication affecting life quality and healthcare costs. At this point, no statistics or studies have evaluated the cost of managing DFU in Saudi Arabia. Our study of patients admitted to KFHU with DFU between 2007 and 2017 is the first in this country to estimate the cost of common DFU treatments and identify several factors that significantly contribute to the cost of management.
Management of DFU includes costs incurred during the admission of patients, investigations, procedures, medications and dressings. We found that the total cost of DFU management over a ten-year period for the 99 patients in our study was 6 618 043.3 SAR (1 764 632.68 USD), with a breakdown for one year estimated to be 661 804.3 SAR (176 481.2 USD). This further translates to approximately 6684.9 SAR per patient/year (1 782.6 USD). These numbers were estimated from a sampling of patients in a single tertiary care hospital located in Saudi Arabia, and highlight the impact of DFU on healthcare expenditure. Other studies have reported varying costs. Lam et al.12 studied the cost of acute DFU management in Malaysia and reported a lower total cost of about 11 000 USD per year and 60 USD per patient/per year. Ragnarson, Tennvall and Apelqvist in Sweden13 have reported much higher costs; estimating 17 500 USD to heal a single diabetic foot ulcer and up to 33 500 USD for lower extremity amputation. Their analysis was based on the cost of acute inpatient management of DFU, outpatient podiatrist visits and the cost of orthopedic appliances, along with outpatient topical treatments until resolution of the ulcer, management of the disability or a recurrence of the original ulcer. A further retrospective study of diabetic patients with lower extremity ulcers revealed an average cost per ulcer episode of 13 179 USD.14
Amputations are classified either as major – above the ankle, or minor – below the ankle. In the Ragnarson, Tennvall and Apelqvist study it was also reported that the cost for healing a DFU without amputation was 17 554 USD. With minor amputation, the cost rose to 33 540 USD, while the healing of a major amputation reached 30 135 USD.3 Interestingly, the higher cost of minor amputations compared to major amputations may be attributed to the fact that patients with minor ulcers require ongoing treatments for a longer period of time. Our results were very similar to this study, wherein we revealed that the cost of admission represented the most substantial portion of the overall cost of managing acute DFU at 45.6%.15,16 Lam et al in Malaysia found that antibiotics accounted for most of the treatment costs (5396.6 USD), followed by admission and baseline investigations (2438.7 USD).12 The antibiotic regimen Lam used in his study included sulbactam, ampicillin, cefuroxime, ceftazidime, metronidazole, cloxacillin, fusidic acid, vancomycin, ciprofloxacin and gentamicin. However, in our study, antibiotics accounted only for 6.9% of the total health costs and utilized penicillin, a broad-spectrum antibiotic that is appropriate for polymicrobial infections as in the case of DFU.17 Moderate-to-severe infections requiring multiple groups of parenteral antibiotics for a longer duration occurred in 62.6% of our cases.17
Surgical management depends on the ulcer presentation and includes minor debridement, incision and drainage or amputation; with the diabetic foot seen as the most common cause of therapeutic amputation in Saudi Arabia. People with diabetes are 10–15 times more likely to require a lower extremity amputation than non-diabetic individuals, with a 30–50% higher risk of undergoing a second amputation.18–20 Debridement and surgical procedures (amputation and reconstruction) contributed 14.5% and 7.4% of the overall cost, and it is estimated that managing one patient with an amputation costs between 40 000 to 75 000 USD.17,21 Amputation in cases of DFU is typically due to the progressive effects of neuropathy, minor trauma, ulceration, impaired healing, ischemia and infection.20
The cost of care for diabetic patients with a lower extremity ulcer is a significant economic burden compared to the management of a diabetic patient without ulceration.11 Hence, better glycemic control through patient education on the hazards of diabetic foot and preventive practices may significantly lower healthcare expenditure.22–24 In addition, early recognition of foot problems with effective interventions should also improve outcomes by reducing the need for major amputations.
We attempted to identify patient characteristics that significantly affect healthcare expenditure related to DFU, as recognizing these factors may help sharpen the focus on preventive health education, thereby improving quality of life and reducing overall costs. However, factors known to increase the risk of complications such as uncontrolled HgA1c, the duration of antibiotic therapy, and the presence of other comorbidities, were found to be ineffective against high expenditure in the univariate analysis. This may be attributed to the relatively small sample size in our study and in which case, further studies are required to clarify this point. Earlier studies have reported risk factors for DFU complications including increasing age, poor glycemic control and peripheral vascular disease,25 which is present in approximately one-half of all patients with foot ulcers26 and was seen in about one-third of our cases.
Our study had some limitations. We calculated only the direct costs of DFU, as indirect costs are more subjective and difficult to quantify. These indirect costs include transportation, dressings and the psychological impact on patients. Also, we did consider the change in the value of the money during the period of 10 years. Further studies are required to evaluate DFU costs that also include these expenditures. Prospective studies are also recommended rather than retrospective studies, as our current study lacked some patient record data which if included, may have further clarified more aspects of this topic.
In conclusion, healthcare expenditure in the case of DFU management is high, with the largest portion of cost allocated to hospital admissions and surgical procedures. Increasing awareness of the importance of proper foot care and improved glycemic control may decrease complications and thus reduce the total cost of treatment. Further research and multicenter prospective studies are recommended for the identification of more variables affecting cost management.
Appendix I.
| Surgical Procedure | Cost (SAR) | Cost (USD) |
| Toe amputation | 2500 | 665 |
| Forefoot amputation | 5000 | 1330 |
| Transtibial amputation | 10 000 | 2661 |
| Transfemoral amputation | 15 000 | 3991 |
| Debridement | 3500 | 931 |
| Antibiotic | Cost per dose (SAR) | Cost per dose (USD) |
| Augmentin | 7.61 | 2.03 |
| Clindamycin | 22.0 | 5.85 |
| Ciprofloxacin | 19.16 | 5.10 |
| Tazocin | 27.83 | 7.41 |
| Meropenem | 25.0 | 6.65 |
| Others | Cost (SAR) | Cost (USD) |
| Stay in ward | 1210/day | 321.99 |
| Stay in ICU | 6000/day | 1596.66 |
| Dressing | 130/time | 34.59 |
| CBC | 153.00 | 40.71 |
| Hemoglobin A1C | 253.50 | 67.46 |
| Swab culture | 156.00 | 41.51 |
| Tissue culture | 508.00 | 135.18 |
| CT for foot | 1900.00 | 505.61 |
| X-ray for foot | 90.00 | 23.95 |
| Physiotherapy | 300/time | 79.83 |
Funding Statement
None.
REFERENCES
- 1.Bus SA, Netten JJ, Lavery LA, Monteiro-Soares M, Rasmussen A, Jubiz Y, et al. IWGDF guidance on the prevention of foot ulcers in at-risk patients with diabetes. Diabetes/Metabolism Research and Reviews. 2016; 32(S1):16–24. [DOI] [PubMed] [Google Scholar]
- 2.Alhowaish A. Economic costs of diabetes in Saudi Arabia. Journal of Family and Community Medicine. 2013; 20(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haria J, Singh V, Jain S. Life with diabetic foot ulcer—a cross sectional study. International Journal of Scientific Study. 2014; 1(6):33–5. [Google Scholar]
- 4.Denyer J, Pillay E. Best practice guidelines for skin and wound care in epidermolysis bullosa. International Consensus. Dystrophic Epidermolysis Bullosa Research Association. 2012. 2012.
- 5.McKinnon PS, Paladino JA, Grayson ML, Gibbons GW, Karchmer AW. Cost-effectiveness of ampicillin/sulbactam versus imipenem/cilastatin in the treatment of limb-threatening foot infections in diabetic patients. Clinical infectious diseases journal. 1997; 24(1):57–63. [DOI] [PubMed] [Google Scholar]
- 6.Bishop S, Walker M, Rogers A, Chen W. Importance of moisture balance at the wound-dressing interface. Journal of wound care. 2003; 12 (4):125–8. [DOI] [PubMed] [Google Scholar]
- 7.NICE CfCPa. Diabetic foot problems: in-patient management of diabetic foot problems. 2011[[AUTHOR: Please provide a full citation]]
- 8.Alzahrani HA. Diabetes-related lower extremities amputations in Saudi Arabia: the magnitude of the problem. Annals of vascular diseases. 2012; 5(2):151–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Assal J-P, Mehnert H, Tritschler H-J, Sidorenko A, Keen H. On your feet! Workshop on the Diabetic Foot. Journal of Diabetes and its Complications. 2002; 16(2):183–94. [DOI] [PubMed] [Google Scholar]
- 10.Rathur HM, Boulton AJM. The diabetic foot. Clinics in Dermatology. 2007; 25(1):109–20. [DOI] [PubMed] [Google Scholar]
- 11.Driver VR, Fabbi M, Lavery LA, Gibbons G. The costs of diabetic foot: the economic case for the limb salvage team. Journal of vascular surgery. 2010; 52(3):17S–22S. [DOI] [PubMed] [Google Scholar]
- 12.Lam AWC, Zaim MR, Helmy HH, Ramdhan IMA. Economic Impact of Managing Acute Diabetic Foot Infection in a Tertiary Hospital in Malaysia. Malaysian Orthopaedic Journal. 2014; 8(1):46–9.25279093 [Google Scholar]
- 13.Ragnarson Tennvall G, Apelqvist J. Health-economic consequences of diabetic foot lesions. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2004; 39 Suppl 2:S132–9. [DOI] [PubMed] [Google Scholar]
- 14.Stockl K, Vanderplas A, Tafesse E, Chang E. Costs of lower-extremity ulcers among patients with diabetes. Diabetes care. 2004; 27(9):2129–34. [DOI] [PubMed] [Google Scholar]
- 15.Apelqvist J, Ragnarson?Tennvall G, Larsson J, Persson U. Diabetic foot ulcers in a multidisciplinary setting an economic analysis of primary healing and healing with amputation. Journal of internal medicine. 1994; 235(5):463–71. [DOI] [PubMed] [Google Scholar]
- 16.Tennvall GR, Apelqvist J, Eneroth M. Costs of deep foot infections in patients with diabetes mellitus. Pharmacoeconomics. 2000; 18(3):225–38. [DOI] [PubMed] [Google Scholar]
- 17.Reiber GE, Lipsky BA, Gibbons GW. The burden of diabetic foot ulcers. The American Journal of Surgery. 1998; 176(2A Suppl):5s–10s. [DOI] [PubMed] [Google Scholar]
- 18.Qari FA, Akbar D. Diabetic foot: presentation and treatment. Saudi medical journal. 2000; 21(5):443–6. [PubMed] [Google Scholar]
- 19.Margolis DJ, Allen-Taylor L, Hoffstad O, Berlin JA. Diabetic neuropathic foot ulcers: the association of wound size, wound duration, and wound grade on healing. Diabetes care. 2002; 25(10):1835–9. [DOI] [PubMed] [Google Scholar]
- 20.Pecoraro RE, Reiber GE, Burgess EM. Pathways to diabetic limb amputation: basis for prevention. Diabetes care. 1990; 13(5):513–21. [DOI] [PubMed] [Google Scholar]
- 21.King LB. Impact of a preventive program on amputation rates in the diabetic population. Journal of Wound Ostomy & Continence Nursing. 2008; 35(5):479–82. [DOI] [PubMed] [Google Scholar]
- 22.Al-Wahbi AM. Impact of a diabetic foot care education program on lower limb amputation rate. Vascular Health and Risk Management. 2010; 6:923–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lavery LA, Wunderlich RP, Tredwell JL. Disease management for the diabetic foot: effectiveness of a diabetic foot prevention program to reduce amputations and hospitalizations. Diabetes research and clinical practice. 2005; 70(1):31–7. [DOI] [PubMed] [Google Scholar]
- 24.Tennvall GR, Apelqvist J. Prevention of diabetes-related foot ulcers and amputations: a cost-utility analysis based on Markov model simulations. Diabetologia. 2001; 44(11):2077–87. [DOI] [PubMed] [Google Scholar]
- 25.Armstrong DG, Lavery LA, Harkless LB. Validation of a diabetic wound classification system: the contribution of depth, infection, and ischemia to risk of amputation. Diabetes care. 1998; 21(5):855–9. [DOI] [PubMed] [Google Scholar]
- 26.Prompers L, Huijberts M, Apelqvist J, Jude E, Piaggesi A, Bakker K, et al. High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia. 2007; 50(1):18–25 [DOI] [PubMed] [Google Scholar]


