Abstract
Replication-incompetent adenoviral vectors have been under investigation as a platform to carry a variety of transgenes, and express them as a basis for vaccine development. A replication-incompetent adenoviral vector based on human adenovirus type 26 (Ad26) has been evaluated in several clinical trials.
The Brighton Collaboration Viral Vector Vaccines Safety Working Group (V3SWG) was formed to evaluate the safety and features of recombinant viral vector vaccines. This paper reviews features of the Ad26 vectors, including tabulation of safety and risk assessment characteristics of Ad26-based vaccines.
In the Ad26 vector, deletion of E1 gene rendering the vector replication incompetent is combined with additional genetic engineering for vaccine manufacturability and transgene expression optimization. These vaccines can be manufactured in mammalian cell lines at scale providing an effective, flexible system for high-yield manufacturing. Ad26 vector vaccines have favorable thermostability profiles, compatible with vaccine supply chains.
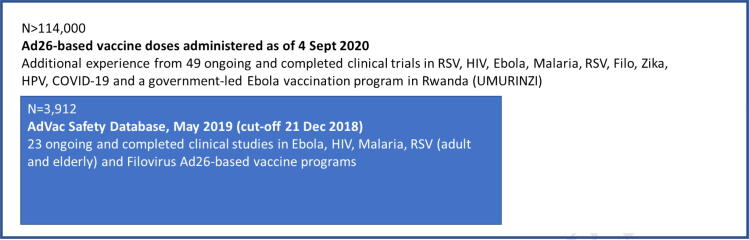
Safety data are compiled in the Ad26 vaccine safety database version 4.0, with unblinded data from 23 ongoing and completed clinical studies for 3912 participants in five different Ad26-based vaccine programs. Overall, Ad26-based vaccines have been well tolerated, with no significant safety issues identified. Evaluation of Ad26-based vaccines is continuing, with >114,000 participants vaccinated as of 4th September 2020.
Extensive evaluation of immunogenicity in humans shows strong, durable humoral and cellular immune responses. Clinical trials have not revealed impact of pre-existing immunity to Ad26 on vaccine immunogenicity, even in the presence of Ad26 neutralizing antibody titers or Ad26-targeting T cell responses at baseline.
The first Ad26-based vaccine, against Ebola virus, received marketing authorization from EC on 1st July 2020, as part of the Ad26.ZEBOV, MVA-BN-Filo vaccine regimen. New developments based on Ad26 vectors are underway, including a COVID-19 vaccine, which is currently in phase 3 of clinical evaluation.
Keywords: Vaccine, Viral vector, Safety, Benefit/risk, Replication-incompetent Ad26
1. Introduction
The Brighton Collaboration (www.brightoncollaboration.org) V3SWG is an established collaboration who aim to enhance the science of vaccine safety research (http://cms.brightoncollaboration.org: 8080/public/what-we-do/setting-standards/case-definitions/process). The Brighton V3SWG uses a standardized template to describe the key characteristics of novel vaccine vectors, compiled from the latest research, to facilitate scientific discourse among key stakeholders [1].
2. Background
The adenovirus type 26 (Ad26) wild type virus was first isolated in 1956 from an anal specimen of a 9-month-old male child [2]. As described in that study, 4 different isolates were obtained from anal and throat swabs from different children, some of whom experienced mild self-limiting enteric infections. Although, none of the illnesses could etiologically be associated with the isolated adenoviruses, it suggests that wild type Ad26 can, presumably, cause asymptomatic or minor illness [2]. Human Ad26 has been considered to be a low-prevalent adenovirus due to the low frequency of Ad26 neutralizing antibodies in various populations compared with human adenovirus type 5. For example, a seroprevalence study of the 51 human adenovirus serotypes known at the time showed that several serotypes from particularly subgroups B and D, including Ad26, were rare in a Belgian population [3], suggesting that vectors (rAd) derived from these serotypes might be useful alternatives to Ad5-based vectors for vaccine development, since for Ad5-based vectors it was shown that their high prevalence hampered their clinical use [4], [5], [6], [7], [8]. More extensive seroprevalence and immunogenicity studies showed that while all of these vectors exhibited low seroprevalence, Ad26-based vaccine candidates were the most immunogenic in animals [9]. Further studies have shown that, depending on geographical location, 10%–90% of people tested have neutralizing antibodies against Ad26. However, neutralization titers are low to intermediate compared with those observed for other adenovirus types [10], [11], [12], [13].
2.1. Ad26 vector development
Adenovirus genomes are linear, non-segmented double-stranded DNA molecules with inverted terminal repeat (ITR) sequences at each end. The vector system for replication-incompetent Ad26 vaccine vectors consists of an adaptor plasmid and a cosmid [9]. The adaptor plasmid contains the left end of the genome containing the left ITR and the packaging signal. It also contains a transgene expression cassette in place of the E1 region and a ∼ 2.5 kb fragment downstream of the E1 region to enable homologous recombination with the cosmid. The cosmid contains the majority of the Ad genome, spanning from the pIX sequence to the right ITR, with a deletion of the E3 region and a modified E4 open reading frame 6 (E4orf6). Transfection into a suitable packaging cell line (HEK293 cells, PER.C6® cells) and subsequent homologous recombination of the adaptor plasmid and cosmid results in the generation of a replication-incompetent E1/E3-deleted Ad26 vector. Packaging cell lines like the HEK293 and PER.C6® cell lines contain the E1 region of adenovirus serotype 5 (Ad5). Because within the adenoviral life cycle, E1 protein 55 K and E4 protein Orf6 form a complex that is pivotal for high-level late-gene expression, the E4-Orf6 sequence of Ad26 is replaced by the corresponding sequence from Ad5 in the vector. This modification has previously been shown to be necessary to allow for the efficient production of rAd35 virus on Ad5 E1-complementing cells [14]. Finally, compensation for the loss of E3 is not needed since the E3 proteins are not essential for adenoviral growth in vitro but are involved in down regulating cellular immunological response mechanisms in an attempt of the adenovirus to escape the host immune system [15].
Most adenovirus serotypes use the coxsackievirus-adenovirus receptor for attachment to the target cell [16], [17]. In contrast, Ad26 has been reported to utilize CD46 as its primary cellular receptor [9], [18], but more recent reports indicated only a limited interaction between Ad26 and CD46, even showing evidence of a role for αvβ3 integrin for efficient transduction of epithelial cells, or interaction with sialic acid [19], [20]. These data suggest that receptor usage by Ad26 might be host cell-type dependent in vitro [19], [20]. Target cells in vivo in the natural host are not known, but Ad26 virus can infect a variety of cell types in vitro. Detailed studies dissecting the attachment, internalization and intracellular trafficking of adenoviral vectors have shown that Ad26, amongst others, accumulate in the late endosome to a larger extent and trigger innate immune pathways differentially compared with Ad5-based vectors [21]. Whether and how these differences may translate into differential profiles of adaptive immunity against the vaccine antigen is not known.
2.2. Manufacturing, formulation and stability
Ad26 vector-based vaccines are manufactured using the E1-complementing PER.C6® cell line, a continuous, human cell line capable of supporting the manufacturing of replication incompetent adenoviral vectors [22]. One of the key strengths of this cell platform is that the cells can grow in suspension in serum-free media to very high cell densities. Cell counts of 100 million cells/mL, with a high percentage of viable cells, can be reached within 10 days of cell culture. Janssen has taken advantage of the ability to grow the PER.C6® cell line at high cell densities in a so called “intensified process”. Cell-specific yields are in the same range as is generally achieved with other Adenoviral vectors and E1-complementing cell lines, therefore, due to the higher cell densities yields per volume unit are higher. The complete manufacturing process has now been scaled up to 1,000 L allowing manufacturing at a commercial scale.
While lyophilized vaccines are generally more heat-stable than non-lyophilized alternatives [23], liquid vaccine formulations may have several advantages over lyophilized vaccines, including ease of manufacture, packaging, and simple administration procedures [24]. For Ad26-based vectors, progress in formulation development has allowed for long-term storage of product at 2–8 °C, enabling product distribution through existing vaccine supply chains. Assessments of robustness during storage, handling and distribution conditions have shown that recombinant Ad26 vectors can be maintained stable under frozen conditions or at 2–8 °C, and, furthermore, showed to be stable in-use with a syringe/needle, also when subjected to agitation or temperature excursions [25].
2.3. Safety, tolerability and immunogenicity of Ad26-based vaccines in humans
Ad26-based vaccines have been extensively tested in completed and ongoing clinical studies from multiple clinical programs (Fig. 1). The following vaccine candidates have been evaluated in clinical programs:
-
•
Ad26.ZEBOV for Ebola virus
-
•
Ad26.Mos.HIV, Ad26.Mos4.HIV, and Ad26.ENVA.01 for HIV
-
•
Ad26.CS.01 for Malaria
-
•
Ad26.RSV.FA2 and Ad26.RSV.preF for RSV
-
•
Ad26.Filo for Filovirus
-
•
Ad26.ZIKV.001 for Zika
-
•
Ad26.HPV16 and Ad26.HPV18 for HPV
Fig. 1.
Summary of number of Ad26-based vaccines administered (full experience and AdVac Safety Database).
The adenoviral vaccine (AdVac) safety database report version 4.0 (14 May 2019) contains data from 23 clinical studies, for a total of 3912 study participants, using the following Ad26-based vaccines: Ad26.ZEBOV (Ebola program; 9 studies [26], [27]; Table 1), Ad26.ENVA.01, Ad26.Mos.HIV, and Ad26.Mos4.HIV (HIV program; 8 studies [28], [29], [30], [31], [32]; Table 2), Ad26.CS.01 (Malaria program; 1 study [33]; Table 3), Ad26.RSV.FA2 and Ad26.RSV.preF (RSV program; 4 studies; Table 4), and Ad26.Filo (Filovirus program; 1 study; Table 5). A full overview of the clinical studies can be found in Table 1, Table 2, Table 3, Table 4, Table 5. The cut-off date for this report was 21 December 2018. Data from all unblinded studies for which the clinical database had been locked and unblinded, either for interim, primary or final analyses, are included in this review (Table 6, [9], [10], [11], [12], [13], [16], [17], [18], [19], [20], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [74], [52], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75]).
Table 1.
Summary of Ad26 Ebola vaccine clinical studies.
| Study | Sponsor (IND holder) | Vaccine | Status | Phase/Blind/Allocation/Participants/ Country | Protocol-specified vaccination groups | Planned number of participants | Reference NCT No. |
|---|---|---|---|---|---|---|---|
|
VAC52150 EBL1001 |
Janssen | Ad26.ZEBOV, MVA-BN-Filo |
Completed | Phase 1/1st part of the study/Double-blind (observer-blind)/Randomized/Healthy adults/UK | 1 × 108 TCID50 MVA-BN-Filo (Day 1) 5 × 1010 vp Ad26.ZEBOV (Day 29) |
15 |
NCT02313077 [26], [27] |
| 1 × 108 TCID50 MVA-BN-Filo (Day 1) 5 × 1010 vp Ad26.ZEBOV (Day 57) |
15 | ||||||
| 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 TCID50 MVA-BN-Filo (Day 29) |
15 | ||||||
| 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 TCID50 MVA-BN-Filo (Day 57) |
15 | ||||||
| Placebo | 12 | ||||||
| 2nd part of the study/Open-label/Non-randomized/Healthy adults/UK | 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 TCID50 MVA-BN-Filo (Day 15) |
15 | |||||
|
VAC52150 EBL1002 |
Janssen | Ad26.ZEBOV, MVA-BN-Filo |
Completed | Phase 1/Double-blind (observer-blind)/Randomized/Healthy adults/US | 1 × 108 TCID50 MVA-BN-Filo (Day 1) 5 × 1010 vp Ad26.ZEBOV (Day 15) |
19 | NCT02325050 |
| 1 × 108 TCID50 MVA-BN-Filo (Day 1) 5 × 1010 vp Ad26.ZEBOV (Day 15) 5 × 1010 vp Ad26.ZEBOV (Day 360) |
11 | ||||||
| 1 × 108 TCID50 MVA-BN-Filo (Day 1) 5 × 1010 vp Ad26.ZEBOV (Day 29) |
4 | ||||||
| 1 × 108 TCID50 MVA-BN-Filo (Day 1) 5 × 1010 vp Ad26.ZEBOV (Day 29) 5 × 1010 vp Ad26.ZEBOV (Day 360) |
11 | ||||||
| 1 × 108 TCID50 MVA-BN-Filo (Day 1) 5 × 1010 vp Ad26.ZEBOV (Day 57) |
3 | ||||||
| 1 × 108 TCID50 MVA-BN-Filo (Day 1) 5 × 1010 vp Ad26.ZEBOV (Day 57) 5 × 1010 vp Ad26.ZEBOV (Day 360) |
12 | ||||||
| 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 TCID50 MVA-BN-Filo (Day 29) |
2 | ||||||
| 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 TCID50 MVA-BN-Filo (Day 29) 5 × 1010 vp Ad26.ZEBOV (Day 360) |
13 | ||||||
| 1 × 108 TCID50 MVA-BN-Filo (Day 1) 1 × 108 TCID50 MVA-BN-Filo (Day 15) 5 × 1010 vp Ad26.ZEBOV (Day 360) |
7 | ||||||
| 5 × 1010 vp Ad26.ZEBOV (Day 1) 5 × 1010 vp Ad26.ZEBOV (Day 15) |
2 | ||||||
| 5 × 1010 vp Ad26.ZEBOV (Day 1) 5 × 1010 vp Ad26.ZEBOV (Day 15) 1 × 108 TCID50 MVA-BN-Filo (Day 360) |
7 | ||||||
| 5 × 1010 vp Ad26.ZEBOV (Day 1) 4.4 × 108 TCID50 MVA-BN-Filo (Day 15) |
4 | ||||||
| 5 × 1010 vp Ad26.ZEBOV (Day 1) 4.4 × 108 TCID50 MVA-BN-Filo (Day 15) 5 × 1010 vp Ad26.ZEBOV (Day 360) |
11 | ||||||
| 1 × 1011 vp Ad26.ZEBOV (Day 1) 4.4 × 108 TCID50 MVA-BN-Filo (Day 29) |
5 | ||||||
| 1 × 1011 vp Ad26.ZEBOV (Day 1) 4.4 × 108 TCID50 MVA-BN-Filo (Day 29) 1 × 1011 vp Ad26.ZEBOV (Day 360) |
10 | ||||||
| 1 × 108 TCID50 MVA-BN-Filo (Day 1) 5 × 1010 vp Ad26.ZEBOV (Day 8) |
15 | ||||||
| Placebo | 25 | ||||||
|
VAC52150 EBL1003 |
Janssen | Ad26.ZEBOV, MVA-BN-Filo |
Completed | Phase 1/Double-blind (observer-blind)/Randomized/Healthy adults/Kenya | 1 × 108 TCID50 MVA-BN-Filo (Day 1) 5 × 1010 vp Ad26.ZEBOV (Day 29) |
15 | NCT02376426 |
| 1 × 108 TCID50 MVA-BN-Filo (Day 1) 5 × 1010 vp Ad26.ZEBOV (Day 57) |
15 | ||||||
| 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 TCID50 MVA-BN-Filo (Day 29) |
15 | ||||||
| 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 TCID50 MVA-BN-Filo (Day 57) |
15 | ||||||
| Placebo | 12 | ||||||
|
VAC52150 EBL1004 |
Janssen | Ad26.ZEBOV, MVA-BN-Filo |
Completed | Phase 1/Double-blind (observer-blind)/Randomized/Healthy adults/Tanzania, Uganda | 1 × 108 TCID50 MVA-BN-Filo (Day 1) 5 × 1010 vp Ad26.ZEBOV (Day 29) |
15 | NCT02376400 |
| 1 × 108 TCID50 MVA-BN-Filo (Day 1) 5 × 1010 vp Ad26.ZEBOV (Day 57) |
15 | ||||||
| 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 TCID50 MVA-BN-Filo (Day 29) |
15 | ||||||
| 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 TCID50 MVA-BN-Filo (Day 57) |
15 | ||||||
| Placebo | 12 | ||||||
|
VAC52150 EBL2001 |
Janssen | Ad26.ZEBOV, MVA-BN-Filo |
Completed | Phase 2/Double-blind (observer-blind)/Randomized/Healthy adults/France, UK | 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 Inf U MVA-BN-Filo (Day 29) |
174 | NCT02416453 |
| 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 Inf U MVA-BN-Filo (Day 57) |
174 | ||||||
| 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 Inf U MVA-BN-Filo (Day 85) |
174 | ||||||
| 5 × 1010 vp Ad26.ZEBOV (Day 1) | 15 | ||||||
| Placebo | 93 | ||||||
|
VAC52150 EBL2002 |
Janssen | Ad26.ZEBOV, MVA-BN-Filo |
Ongoing | Phase 2/Double-blind (observer-blind)/Randomized/Healthy adults 18–70 yrs; HIV+ adults 18–50 yrs; healthy children 4–17 yrs/Burkina Faso, Uganda, Côte D'Ivoire, Kenya | 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 Inf U MVA-BN-Filo (Day 29) |
385 | NCT02564523 |
| 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 Inf U MVA-BN-Filo (Day 57) |
385 | ||||||
| 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 Inf U MVA-BN-Filo (Day 85) |
110 | ||||||
| Placebo | 176 | ||||||
|
VAC52150 EBL3001 |
Janssen | Ad26.ZEBOV, MVA-BN-Filo |
Ongoing | Phase 3/Open-label uncontrolled stage in healthy participants ≥18 years (Stage 1)/Double-blind randomized stage in healthy participants ≥1 year (Stage 2)/Sierra Leone | 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 Inf U MVA-BN-Filo (Day 57) |
772 | NCT02509494 |
| Placebo | 244 | ||||||
|
VAC52150 EBL3002 |
Janssen | Ad26.ZEBOV, MVA-BN-Filo |
Completed | Phase 3/Double-blind (observer-blind)/Randomized/Healthy adults/US | 0.8 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 Inf U MVA-BN-Filo (Day 57) |
150 | NCT02543567 |
| 2 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 Inf U MVA-BN-Filo (Day 57) |
150 | ||||||
| 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 Inf U MVA-BN-Filo (Day 57) |
150 | ||||||
| Placebo | 75 | ||||||
|
VAC52150 EBL3003 |
Janssen | Ad26.ZEBOV, MVA-BN-Filo |
Completed | Phase 3/Double-blind (observer-blind)/Randomized/Healthy adults/US | 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 Inf U MVA-BN-Filo (Day 57) |
282 | NCT02543268 |
| Placebo | 47 | ||||||
Cut-off for studies 21 December 2018.
Ad26, adenovirus serotype 26; BN, Bavarian Nordic; EBOV, Ebola virus; Inf U, infectious unit; MVA, modified vaccinia virus Ankara; TCID50, 50% tissue culture infective dose; vp, viral particles; ZEBOV, Zaire Ebola virus.
Table 2.
Summary of Ad26 HIV vaccine clinical studies.
| Study | Sponsor (IND holder) | Vaccine | Status | Phase/Blind/Allocation/Participants/Country | Protocol-specified vaccination groups | Planned number of participants | Reference NCT No. |
|---|---|---|---|---|---|---|---|
| IPCAVD-001 | DAIDS | Ad26.ENVA.01 | Completed | Phase 1/Double-blind (observer-blind)/Randomized/Healthy adults/US | 1 × 109 vp Ad26.ENVA.01 (Weeks 0, 4, 24) | 10 |
NCT00618605 [28], [29] |
| 1 × 1010 vp Ad26.ENVA.01 (Weeks 0, 4, 24) | 10 | ||||||
| 1 × 1011 vp Ad26.ENVA.01 (Weeks 0, 4, 24) | 10 | ||||||
| 5 × 1010 vp Ad26.ENVA.01 (Weeks 0, 24) | 10 | ||||||
| 1 × 1010 vp Ad26.ENVA.01 (Weeks 0, 24) | 10 | ||||||
| Placebo | 10 | ||||||
| IPCAVD-003 | DAIDS | Ad26.ENVA.01 | Completed | Phase 1/Double-blind (observer-blind)/Randomized/Healthy adults (Ad26 seronegative and Ad26 seropositive)/US | 5 × 1010 vp Ad26.ENVA.01 (Week 0) | 18 |
NCT01103687 [30] |
| Placebo | 6 | ||||||
| IPCAVD-004 | IAVI | Ad26.ENVA.01 Ad35.ENV |
Completed | Phase 1/Double-blind (observer-blind)/Randomized/Healthy adults/US, Kenya, Rwanda, South Africa | 5 × 1010 vp Ad26.ENVA.01 (Month 0) 5 × 1010 vp Ad35.ENV (Month 6) |
10 |
NCT01215149 [31] |
| 5 × 1010 vp Ad35.ENV (Month 0) 5 × 1010 vp Ad26.ENVA.01 (Month 6) |
10 | ||||||
| 5 × 1010 vp Ad26.ENVA.01 (Month 0) 5 × 1010 vp Ad35.ENV (Month 3) |
42 | ||||||
| 5 × 1010 vp Ad35.ENV (Month 0) 5 × 1010 vp Ad26.ENVA.01 (Month 3) |
42 | ||||||
| 5 × 1010 vp Ad26.ENVA.01 (Month 0) 5 × 1010 vp Ad26.ENVA.01 (Month 3) |
32 | ||||||
| 5 × 1010 vp Ad35.ENV (Month 0) 5 × 1010 vp Ad35.ENV (Month 3) |
32 | ||||||
| Placebo | 44 | ||||||
| HIV-V-A004 | Janssen | Ad26.Mos.HIV | Ongoing* | Phase 1/2a/Double-blind/Randomized/Healthy adults/US, Thailand, Rwanda, Uganda, South Africa | 5 × 1010 vp Ad26.Mos.HIV (Weeks 0, 12) 5 × 1010 vp Ad26.Mos.HIV+ 250 mcg gp140 + adjuvant (Weeks 24, 48) |
50 |
NCT02315703 [32] |
| 5 × 1010 vp Ad26.Mos.HIV (Weeks 0, 12) 5 × 1010 vp Ad26.Mos.HIV+ 50 mcg gp140 + adjuvant (Weeks 24, 48) |
50 | ||||||
| 5 × 1010 vp Ad26.Mos.HIV (Weeks 0, 12) 5 × 1010 vp Ad26.Mos.HIV+ placebo (Weeks 24, 48) |
50 | ||||||
| 5 × 1010 vp Ad26.Mos.HIV (Weeks 0, 12) 108 pfu MVA-Mosaic + 250 mcg gp140 + adjuvant (Weeks 24, 48) |
50 | ||||||
| 5 × 1010 vp Ad26.Mos.HIV (Weeks 0, 12) 108 pfu MVA-Mosaic + 50 mcg gp140 + adjuvant (Weeks 24, 48) |
50 | ||||||
| 5 × 1010 vp Ad26.Mos.HIV (Weeks 0, 12) 108 pfu MVA-Mosaic + placebo (Weeks 24, 48) |
50 | ||||||
| 5 × 1010 vp Ad26.Mos.HIV (Weeks 0, 12) 250 mcg gp140 + adjuvant + placebo (Weeks 24, 48) |
50 | ||||||
| Placebo (Weeks 0, 12, 24, 48) | 50 | ||||||
| VAC89220 HPX1002 | Janssen | Ad26.Mos.HIV | Ongoing† | Phase 1/Double-blind/Randomized/Healthy adults/US | 5 × 1010 vp Ad26.Mos.HIV (Weeks 0, 12) 5 × 1010 vp Ad26.Mos.HIV+ 250 mcg Clade C gp140 + adjuvant (Weeks 24, 48) |
10 | NCT02685020 |
| 5 × 1010 vp Ad26.Mos.HIV+ 250 mcg Clade C gp140 + adjuvant (Weeks 0, 12, 24) | 10 | ||||||
| 5 × 1010 vp Ad26.Mos.HIV (Week 0) 5 × 1010 vp Ad26.Mos.HIV+ 250 mcg Clade C gp140 + adjuvant (Week 8, 24) |
10 | ||||||
| Placebo | 6 | ||||||
| VAC89220HPX2003 | Janssen | Ad26.Mos4.HIV | Ongoing‡ | Phase 1/2a/Double-blind/Randomized/Healthy adults/US, Kenya, Rwanda | 5 × 1010 vp Ad26.Mos4.HIV (Weeks 0, 12) 5 × 1010 vp Ad26.Mos.HIV+ 250 mcg Clade C gp140 + adjuvant (Weeks 24, 48) |
25 | NCT02935686 |
| 5 × 1010 vp Ad26.Mos4.HIV (Weeks 0, 12) 5 × 1010 vp Ad26.Mos.HIV+ 250 mcg Clade C + Mosaic gp140 + adjuvant (Weeks 24, 48) |
100 | ||||||
| Placebo | 25 | ||||||
| VAC89220HPX2004 | Janssen | Ad26.Mos.HIV Ad26.Mos4.HIV |
Ongoing§ | Phase 1/2a/Double-blind/Randomized/Healthy adults/US, Rwanda | 5 × 1010 vp Ad26.Mos.HIV (Weeks 0, 12) 5 × 1010 vp Ad26.Mos.HIV+ 250 mcg Clade C gp140 + adjuvant (Weeks 24, 48) |
55 | NCT02788045 |
| 5 × 1010 vp Ad26.Mos4.HIV (Weeks 0, 12) 5 × 1010 vp Ad26.Mos4.HIV+ 250 mcg Clade C gp140 + adjuvant (Weeks 24, 48) |
110 | ||||||
| Placebo | 33 | ||||||
| VAC89220HTX1001 | Janssen | Ad26.Mos.HIV | Completed¶ | Phase 1/2a/Double-blind/Randomized/HIV-1 infected adults/Thailand | 5 × 1010 vp Ad26.Mos.HIV (Weeks 0, 12) 1 × 108 pfu MVA-Mosaic (Weeks 24, 48) |
18 | NCT02919306 |
| Placebo | 9 | ||||||
Cut-off for studies 21 December 2018.
* The main study has been completed; the long-term extension phase is still ongoing. Week 96 Final Analysis has been used in AdVac Safety Database.
† Week 72 Final Analysis has been used in AdVac Safety Database.
‡ Week 52 Interim Analysis was used in AdVac Safety Database.
§ The main study has been completed; the long-term extension phase is still ongoing. Week 72 Final Analysis has been used in AdVac Safety Database.
¶ Week 96 Final Analysis has been used in AdVac Safety Database.
Ad26, adenovirus serotype 26; Ad35, adenovirus serotype 35; Enva, envelope A; gp, glycoprotein; mcg, microgram; Mos, mosaic; MVA, modified vaccinia Ankara; pfu, plaque-forming units; vp, viral particles.
Table 3.
Summary of Ad26 Malaria vaccine clinical studies.
| Study | Sponsor (IND holder) | Vaccine | Status | Phase/Blind/Allocation/ Participants/Country | Protocol-specified vaccination groups | Planned number of participants | Reference NCT No. |
|---|---|---|---|---|---|---|---|
| MAL-V-A001 | Janssen | Ad35.CS.01 Ad26.CS.01 |
Completed | Phase 1/2a/Double-blind (observer-blind)/Randomized/Healthy adults/US | 1 × 1010 vp Ad35.CS.01 (Days 0, 28), 1 × 1010 vp Ad26.CS.01 (Day 55) | 10 | NCT01397227 [33] |
| 5 × 1010 vp Ad35.CS.01 (Days 0, 28), 5 × 1010 vp Ad26.CS.01 (Day 55) | 20 | ||||||
| Placebo | 6 |
Cut-off for studies 21 December 2018.
Ad26, adenovirus serotype 26; Ad35, adenovirus serotype 35; CS, circumsporozoite; vp, viral particles.
Table 4.
Summary of Ad26 RSV vaccine clinical studies.
| Study | Sponsor (IND holder) | Vaccine | Status | Phase/Blind/Allocation/ Participants/Country | Protocol-specified vaccination groups | Planned number of participants | Reference NCT No. |
|---|---|---|---|---|---|---|---|
|
VAC18192 RSV1001 |
Janssen | Ad35.RSV.FA2 Ad26.RSV.FA2 |
Completed | Phase 1/Double-blind (observer-blind)/Randomized/Healthy adults/US | 1 × 1011 vp Ad35.RSV.FA2 (Days 1, 85), 5 × 1010 vp Ad26.RSV.FA2 (Day 169) |
12 | NCT02440035 |
| 1 × 1011 vp Ad35.RSV.FA2 (Days 1, 169), placebo (Day 85) |
12 | ||||||
| 1 × 1011 vp Ad35.RSV.FA2 (Day 1), placebo (Day 85), 5 × 1010 vp Ad26.RSV.FA2 (Day 169) |
12 | ||||||
| Placebo (Days 1, 85), 5 × 1010 vp Ad26.RSV.FA2 (Day 169) |
12 | ||||||
|
VAC18192 RSV1003 |
Janssen | Ad35.RSV.FA2 Ad26.RSV.FA2 |
Completed | Phase 1/Double-blind (observer-blind)/Randomized/Healthy adults/US | 5 × 1010 vp Ad26.RSV.FA2 (Days 1, 85), 1 × 1011 vp Ad35.RSV.FA2 (Day 169) |
12 | NCT02561871 |
| 5 × 1010 vp Ad26.RSV.FA2 (Day 1), 1 × 1011 vp Ad35.RSV.FA2 (Day 85), placebo (Day 169) |
12 | ||||||
| Placebo | 8 | ||||||
|
VAC18193 RSV2002 |
Janssen | Ad26.RSV.preF | Ongoing | Phase 2a/Double-blind (observer-blind)/Randomized/Healthy adults/UK | 1 × 1011 vp Ad26.RSV.preF (Day −28) Challenged intranasally with RSV-A at Day 0 |
22 | NCT03334695 |
| Placebo (Day −28) Challenged intranasally with RSV-A at Day 0 |
22 | ||||||
|
VAC18193 RSV2003 |
Janssen | Ad26.RSV.preF | Completed | Phase 2a/Double-blind (observer-blind)/Randomized/Healthy older adults (≥60 years of age)/US | 1 × 1011 vp Ad26.RSV.preF (Day 1), Fluarix® Quadrivalent (Day 1), placebo (Day 29) |
90 | NCT03339713 |
| Fluarix® Quadrivalent (Day 1), placebo (Day 1), 1 × 1011 vp Ad26.RSV.preF (Day 29) |
90 | ||||||
Cut-off for studies 21 December 2018.
Ad26, adenovirus serotype 26; Ad35, adenovirus serotype 35; FA2, F protein of RSV strain A2; preF, prefusion F protein; RSV, respiratory syncytial virus; vp, viral particles.
Table 5.
Summary of Ad26 Filovirus vaccine clinical studies.
| Study | Sponsor (IND holder) | Vaccine | Status | Phase/Blind/Allocation/ Participants/Country | Protocol-specified vaccination groups |
Planned number of participants | Reference NCT No. |
|---|---|---|---|---|---|---|---|
| VAC69120FLV1001 | Janssen | Ad26.Filo Ad26.ZEBOV |
Completed | Phase 1/Double-blind (observer-blind for subset in Group 3 who received the booster vaccination)/Randomized/Healthy adults/US | 9 × 1010 vp Ad26.Filo (Day 1) 5 × 108 Inf U MVA-BN-Filo (Day 57) |
15 | NCT02860650 |
| 5 × 108 Inf U MVA-BN-Filo (Day 1) 9 × 1010 vp Ad26.Filo (Day 57) |
15 | ||||||
| 5 × 108 Inf U MVA-BN-Filo (Day 1) 9 × 1010 vp Ad26.Filo (Day 15) 9 × 1010 vp Ad26.Filo (Day 92) |
15 | ||||||
| 5 × 1010 vp Ad26.ZEBOV (Day 1) 1 × 108 Inf U MVA-BN-Filo (Day 57) |
15 | ||||||
| Placebo | 12 |
Cut-off for studies 21 December 2018.
Ad26, adenovirus serotype 26; BN, Bavarian Nordic; Inf U, infectious unit; MVA, modified vaccinia Ankara; vp, viral particles; ZEBOV, Zaire Ebola Virus.
Table 6.
Brighton Collaboration Viral Vector Vaccines Safety Working Group (V3SWG) standardized template V2.0 for collection of key information for risk assessment of viral vaccine vector candidates filled with Ad26 data.
| 1. Authorship | Information | ||
| 1.1. Author(s) | |||
| 1.2. Date completed/updated | 21 November 2019 | ||
| 2. Basic vector information | Information | ||
| 2.1. Vector name | Ad26 | ||
| 2.2. Vector origin Family/Genus/Species/subtype | Family adenoviridae subgroup D, Human Adenovirus type 26 | ||
| 2.3. Vector replication in humans (replicating or non-replicating) | Replication incompetent | ||
| 3. Characteristics of the wild type virus from which the vector is derived | Information | Comments/Concerns | Reference(s) |
| 3.1. Name of wild type virus (common name; Family/Genus/Species/subtype) | Family adenoviridae subgroup D, human Adenovirus type 26 | ||
| 3.2. What is the natural host for the wild type virus? | Humans. No evidence that Adenovirus type 26 can infect other non-human animals | ||
| 3.3. How is the wild type virus normally transmitted? | Not known | In general, human adenoviruses can be transmitted via the oral/faecal route, through aerosols and human-to-human contact. | [34], [35] |
| 3.4. Does the wild type virus establish a latent or persistent infection? | Not known for Adenovirus type 26 | In general, Adenovirus infections are self-limiting. In some cases, adenoviruses can establish a persistent infection and can reside in certain tissues for longer periods of time. Also, prolonged shedding of infectious virus has been observed for certain adenovirus types. This is observed more prominent in immunocompromised individuals. | [34], [35] |
| 3.5. Does the wild type virus replicate in the nucleus? | Yes | ||
| 3.6. What is the risk of integration into the human genome? | Negligible | Adenoviruses are considered non-integrating according to the EMA ‘Guideline on nonclinical testing for inadvertent germline transmission of gene transfer vectors’, because they lack the machinery to actively integrate their genome into the host chromosomes. The adenoviral genome remains epichromosomal, thus avoiding the risk of integration of the viral DNA into the host genome following cell infection. Therefore, chromosomal integration of genetic material of Ad26 in the human host is unlikely. | [36], [37], [38], [39] |
| 3.7. List any disease manifestations caused by the wild type virus, the strength of evidence, severity, and duration of disease for the following categories: | |||
|
Unknown for Ad26 | See below | |
|
Unknown for Ad26 | In a challenge study in humans, Kasel et al. reported symptomatic infections of Ad26 wild type in human participants upon inoculation in the conjunctival sac or intranasally. Participants inoculated in the conjunctival sac developed a moderate but self-limiting conjunctivitis with positive virus isolations from the eye in the first week after infection but not thereafter. Symptoms were milder in the presence of pre-existing Ad26 antibodies. Participants who were inoculated intranasally developed barely perceptible rhinitis without associated symptoms or signs. No eye disease occurred after nasal inoculation. Shedding upon intranasal inoculation was not studied. Adenovirus type 26 was isolated from the rectum of participants who were inoculated in the conjunctival sac for up to 48 days after initial inoculation albeit without causing any gastrointestinal or systemic illness. Prolonged isolation of the virus from the gastrointestinal tract could indicate infection of cells in the gastrointestinal tract, in line with first isolation of Ad26 wild type from an anal specimen. | [40], [41] |
|
Limited information for Ad26 but human adenovirus infections has been documented in patients undergoing chemotherapy, allogenic stem cell transplantation or in patients with congenital or acquired immune deficiencies. | One case has been described of disseminated Ad26 infection in an immunocompromised individual with a severe brain tumour and irradiation history causing meningoencephalitis. Ad26 was associated with diarrhoea in a patient with acquired immune deficiency syndrome (AIDS). |
[41], [42], [43] |
|
Wild type Adenovirus type 26 has been isolated in 1956 from an anal specimen of a 9-month-old child. The child yielding Ad26 displayed minor illness; however, the illness could not be aetiologically associated with the isolated adenovirus. | [2] | |
|
Unknown | ||
|
Unknown | [43] | |
| 3.8. What cell types are infected and what receptors are used in the natural host and in humans? | Ad26 can infect a wide range of cell types in vitro. Receptor use in humans (natural host) in vivo is not known. | The adenoviral life cycle (generally <2 days) starts with binding of the viral particle via the viral fibre knob to cell surface receptors; for most of the adenoviruses, this is the coxsackievirus B and adenovirus receptor (CAR). Ad26 is reported to use CD46 as the primary cellular receptor, but more recent reports indicated only a limited interaction between Ad26 and CD46, and even showed evidence of a role for αvβ3 integrins for efficient transduction of epithelial cells or interactions with sialic acids. | [9], [18], [19], [20] |
| 3.9. What is known about the mechanisms of immunity to the wild type virus? | Little is known about the mechanisms of immunity to wild-type adenovirus. However, neutralizing antibodies can inhibit viral entry in vitro. In addition, in immunocompromised people having invasive adenovirus infections, the adoptive transfer of adenovirus-specific T-cells has been successful, suggesting an important role for T-cells in immunity to human adenovirus. | [42], [44] | |
| 3.10. Has disease enhancement been demonstrated with the wild type virus: | |||
|
No | ||
|
No | ||
|
No | ||
| 3.11. Is antibody-dependent enhancement (ADE) a possible contributor to the pathogenesis of wild type disease? | Not reported | ||
| 3.12. What is the background prevalence of natural immunity to the virus? | In humans, depending on the geographical location, 10–90% of the individuals tested have neutralizing antibodies against Ad26. However, neutralization titres are low-intermediate compared to what has been observed for other human adenovirus types, as with Ad5. | [9], [10], [11], [12], [13] | |
| 3.13. Is there any vaccine available for the wild-type virus? If yes: | No | ||
|
n.a. | ||
|
n.a. | ||
| 3.14. Is there treatment available for the disease caused by the wild type virus? | No specific treatments for human adenovirus infections are available. | Ribavirin and cidovir have been used to treat immunocompromised individuals. For Ad4, cidofovir and brincidofovir are effective in vitro and have appeared effective in clinical trials. | [45], [46] |
| 4. Characteristics of the vector from which vaccine(s) may be derived | Information | Comments/Concerns | Reference[s] |
| 4.1. Describe the source of the vector (e.g. isolation, synthesis) | The Ad26 vector is based on human adenovirus type 26, group D. Adenovirus type 26 wild-type virus has been isolated in 1956 from an anal specimen of a 9-month-old child. To create the final Ad26 vector, two cloning plasmids were used, one containing the left arm of the genome, and the second containing the right arm of the genome. These plasmids were used to introduce modifications to the Ad26 vector genome. These modifications include deletion of the complete E1a and E1b region, partial deletion of the E3 region, which is non-essential for in-vitro replication. In addition, Ad26 E4 open reading frame (orf) 6 was exchanged for those of Ad5 to allow production of replication incompetent Ad26 vectors on Ad5 E1 complementing cell lines, i.e., PER.C6® cells. A transgene expression cassette is placed in the E1-deleted region containing a human cytomegalovirus (CMV) immediate-early promoter and a simian virus 40 (SV40) derived polyadenylation (pA) signal for strong expression of a foreign transgene. |
[2], [9] | |
| 4.2. What is the basis of attenuation/inactivation of the wild type virus to create the vector? | Ad26 was rendered replication incompetent by deletion of early region 1 (ΔE1). A partial deletion of non-essential early region 3 (ΔE3) was made to create enough space in the genome for the transgene expression cassette (inserted in E1 region) also further attenuating the vector. | [9] | |
| 4.3. What is known about the replication, transmission and pathogenicity of the vector in humans in the following categories?: | The Ad26 vector is replication incompetent in non-E1 complementing human cells. | ||
|
n.a. | ||
|
n.a. | ||
|
n.a. | ||
|
n.a. | ||
|
n.a. | ||
|
n.a. | ||
| 4.4. Is the vector replication-competent in non-human species? | The Ad26 vector is replication incompetent in non-E1 complementing cells and, as such, will be replication incompetent when administered to non-human species. In addition, insertion of foreign antigens is not expected to change the host-range of the vaccine vector. | ||
| 4.5. What is the risk of reversion to virulence or recombination with wild type virus or other agents? | Recombination of Ad26 vaccine vectors with wild-type viruses would require sequence homology and presence of both the genome of Ad26 vaccine vectors and wild-type adenoviruses to be present in the same cell(s). Nonclinical biodistribution studies show that adenoviral vector DNA of Ad26 vaccine vectors did not distribute widely, as the vector DNA was primarily detected at the site of administration in the muscle, the draining lymph nodes and, to a lesser extent, to the spleen. DNA of intramuscularly administered replication-incompetent Ad vaccine vector and wild-type adenovirus DNA are unlikely to co-locate in the same body compartments. In the unlikely event that recombination occurs between vaccine vector and wild-type adenoviruses, the virulence can maximally be equal to the wild-type adenovirus already present in the tissue. The majority of the theoretical homologous recombination products are replication incompetent or attenuated forms of the Ad26. Reversion of Ad26 virulence by recombination is therefore highly unlikely. Furthermore, reversion of virulence due to nucleotide mutations is impossible since deletion of the E1 gene from the Ad26 vector cannot be restored by random mutations and or indels. Recombination with other viruses has not been described and is considered highly unlikely due to the limited biodistribution and absence of sequence homology and replication. | ||
| 4.6. Is the vector genetically stable in vitro and/or in vivo? | The dsDNA genome of Ad26 virus is relatively stable when compared to RNA viruses. Genetic stability of the vector is confirmed during manufacturing and upscaling by extended passaging and/or genetic stability testing. | [47] | |
| 4.7. What is the potential for shedding and transmission to humans or other species? | Vector shedding is limited and transmission of the Ad26 vector is highly unlikely in view of: (i) the vector is replication-incompetent, and thus, allows only for one-time transduction of the target cell, (ii) the limited shedding as observed in clinical studies, (iii) the limited biodistribution profile as observed in nonclinical studies, and (iv) the very low probability of regaining replication-competence through recombination with co-infecting wild-type virus. | ||
| 4.8. Does the vector establish a latent or persistent infection? | Biodistribution studies in rabbits have shown that vector DNA is not widely distributed, and clearance has been observed indicating that the vector is unlikely to persist in the tissues following intramuscular injection. | In nature, wild-type adenovirus is known to be able to cause persistent infections. Whether the Ad26 vector can persist for longer time in humans is unknown. | |
| 4.9. Does the vector replicate in the nucleus? | The vector is replication incompetent. | ||
| 4.10. What is the risk of integration into the human genome? | See 3.6. | [36], [37], [38], [39] | |
| 4.11. Is there any previous human experience with this or a similar vector (safety and immunogenicity records)? | Yes, numerous vaccine clinical studies have been performed with Ad26-based replication incompetent vectors (see section 7). | [27], [28], [29], [30], [31], [32], [48], [49], [50] | |
| 4.12. What cell types are infected and what receptors are used in humans? | See 3.8. The Ad26 vector is expected to have the same cell tropism as the wild-type Ad26 virus. Receptor use in humans in vivo is unknown. | [9], [18], [19], [20] | |
| 4.13. What is known about the mechanisms of immunity to the vector? | Little is known about the mechanisms of immunity to the vector. However, neutralizing antibodies and cellular responses are induced after Ad26 vector administration to humans and non-human species. Vector specific neutralizing antibodies can specifically inhibit vector entry in vitro. In vivo, little to no indication that neutralizing antibodies inhibit the vector has been found. | [42], [44] | |
| 4.14. Has ADE been demonstrated with the vector: | |||
|
No | ||
|
No | ||
|
No | ||
| 4.15. Is there antiviral treatment available for disease manifestations caused by the vector? | The vector is replication-incompetent; thus, no disease manifestations as seen with wild-type infection are expected. Therefore, there is no need for antiviral treatment. | ||
| 4.16. Can the vector accommodate multigenic inserts or will several vectors be required for multigenic vaccines? | Ad26 can accommodate multigenic inserts, theoretical maximum total insert size up to 8,6 kb (approx. 105% of wild-type Ad26 genome size). In specific cases, multiple vectors may be required to accommodate multigenic vaccines. | As an example, the 4-valent prophylactic HIV vaccine Ad26 component consists of 4 ‘monogenic’ Ad26 vectors combined in one vaccine vial. | [51] |
| 5. Characteristics of vector-based vaccine(s) | Information | Comments/Concerns | Reference[s] |
| 5.1. What is the target pathogen? | Ad26 can serve as a vaccine vector for any target pathogen. | ||
| 5.2. What is identity and source of the transgene? | Antigens of HIV-1 (Env, gag, pol), RSV (FA2, preF), Ebola virus (GP), Sudan virus (GP), Marburg virus (GP), Zika virus (M−E), Human papilloma virus (E2, E6, E7), Plasmodium falciparum (CSP) have been inserted in the replication incompetent Ad26 vector and, have been or, are being tested and evaluated in humans in several clinical trials. | [27], [28], [29], [30], [31], [32], [48], [49], [50], [74], [52], [54], [55], [56], [57], [58], [59], [60], [61] | |
| 5.3. Is the transgene likely to induce immunity to all strains/genotypes of the target pathogen? | This will depend on the design of the antigen and the antigenic diversity of the pathogen. | ||
| 5.4. Where in the vector genome is the transgene inserted? | The transgene is inserted in the E1 region at the site of the E1-deletion. | [9] | |
| 5.5. Does the insertion of the transgene involve deletion or other rearrangement of any vector genome sequences? | The E1 region is deleted to render the vector replication incompetent and together with a deletion in the E3 region provide space for insertion of a transgene expression cassette. | [9] | |
| 5.6. How is the transgene expression controlled (transcriptional promoters, etc.)? | In general, expression of the antigen is regulated using the long human CMV immediate-early promoter, which is thought to be active in most mammalian cells, and an SV40-derived polyadenylation sequence. | [62] | |
| 5.7. Does insertion or expression of the transgene affect the pathogenicity or phenotype of the vector? | The expressed antigen is not part of the viral particle and, as such, it is not expected that the phenotype of the vector nor the pathogenicity (the vector is replication incompetent) of the vector are altered. | ||
| 5.8. Is the vaccine replication-competent in humans or other species? | The Ad26 vector is replication incompetent. | ||
| 5.9. What is the risk of reversion to virulence or recombination with wild type or other agents? | See 4.5. | ||
| 5.10. Is the vaccine genetically stable in vitro and/or in vivo? | Genetic stability of the vaccine vector is confirmed during manufacturing and upscaling by extended passaging and genetic stability testing. | ||
| 5.11. What is the potential for shedding and transmission to humans or other species? | See 4.7. | ||
| 5.12. Does the vaccine establish a latent or persistent infection? | The vaccine is replication incompetent and is unable to establish a productive infection. Persistence/latency is not expected as the vaccine misses the E1 and E3 genes that code for proteins involved in countering the host immune system. In addition, nonclinical biodistribution studies of the vaccine have shown that the Ad26 vaccine vector is cleared from vector positive tissues (see 6.7.). | ||
| 5.13. Does the vaccine replicate in the nucleus? | The vaccine is replication incompetent. The vector genome (linear ds-DNA) travels to the nucleus of the host cell where antigen expression occurs, in the absence of vaccine vector replication. | ||
| 5.14. What is the risk of integration into the human genome? | See 3.6. | [36], [37], [38], [39] | |
| 5.15. List any disease manifestations caused by the vaccine in humans, the strength of evidence, severity, and duration of disease for the following categories: | n.a. | ||
|
n.a. | ||
|
n.a. | ||
|
n.a. | ||
|
n.a. | ||
|
n.a. | ||
| 5.16. What cell types are infected and what receptors are used in humans? | See 3.8. The Ad26 vector is expected to have the same cell tropism as the wild-type Ad26 virus. | [9], [18], [19], [20] | |
| 5.17. What is known about the mechanisms of immunity to the vaccine? | In general, the immune responses to the vaccine antigen encoded by the vector are characterized by a rapid increase in binding and in most cases neutralizing antibodies. In addition, induction of non-neutralizing, functional antibodies with effector functions, like antibody-dependent cellular phagocytosis (ADCP) and antibody-dependent cellular cytotoxicity (ADCC), have been observed. Induction of cellular immunity (both CD4+ and CD8+ T-cells) is also observed. | [27], [28], [29], [30], [31], [32], [74], [52], [54], [55], [56], [57], [58], [59], [60], [61] | |
| 5.18. Has disease enhancement been demonstrated with the vaccine: | |||
|
No | ||
|
No | [55] | |
|
No | ||
| 5.19. What is known about the effect of pre-existing immunity, including both natural immunity and repeat administration of the vector or the vaccine, on ‘take’, safety or efficacy in any animal model or human studies using this vector? | Data acquired to date, in more than 6,000 vaccinated human participants, have not revealed impact of pre-existing vector immunity on the vaccine insert specific humoral or cellular response. Repeated administration with the Ad26 vector leads to an increase in antigen specific humoral responses and a maintenance of cellular responses. With more than 114,000 participants vaccinated overall, no safety issues have been identified. | [28], [32] | |
| 5.20. Is the vaccine transmissible in humans or other species (including arthropods) and/or stable in the environment? | The vaccine is replication incompetent, so no vaccine transmission is expected (see also 4.7.). | ||
| 5.21. Are there antiviral or other treatments available for disease manifestations caused by the vaccine? | The vector is replication-incompetent; thus, no disease manifestations are expected besides local and systemic reactogenicity. Therefore, there is no benefit for antiviral treatment. | ||
| 5.22. Vaccine formulation | Liquid formulation. | ||
| 5.23. Proposed route of vaccine administration | Intramuscular administration. | ||
| 5.24. Target populations for the vaccine (e.g. paediatric, maternal, adult, elderly etc.) | Most target populations can be envisioned. | ||
| 6. Toxicology and potency (Pharmacology) of the vector | Information | Comments/Concerns | Reference[s] |
| 6.1. What is known about the replication, transmission and pathogenicity of the vector in and between animals? | The Ad26 vector does not replicate and does not cause clinical illness in animals. | The Ad26 vector showed a limited distribution following intramuscular injection in rabbits and clearance of the vector was observed, indicating that the vector does not replicate and/or persist in the tissues following intramuscular (IM) injection. The Ad26 vector did not induce any adverse effects in multiple GLP repeat-dose toxicity studies in rabbits (and rats), irrespective of the transgene insert used. | |
| 6.2. For replicating vectors, has a comparative virulence and viral kinetic study been conducted in permissive and susceptible species? (yes/no) If not, what species would be used for such a study? Is it feasible to conduct such a study? | n.a., since the Ad26 vector is replication incompetent. | ||
| 6.3. Does an animal model relevant to assess attenuation exist? | n.a., since the Ad26 vector is replication incompetent. | ||
| 6.4. Does an animal model for safety including immuno-compromised animals exist? | n.a., since the Ad26 vector is replication incompetent. | ||
| 6.5. Does an animal model for reproductive toxicity exist? | n.a., since the Ad26 vector is replication incompetent. | The general (repeat-dose) toxicity studies conducted with the replication incompetent Ad26 vector in rabbits (and rats) have not revealed any effects on male sex organs that would impair male fertility. In addition, the general (repeat-dose) and/or developmental and reproductive toxicity studies did not reveal any evidence of impaired female fertility nor did not indicate harmful effects with respect to reproductive toxicity in female rabbits. | |
| 6.6. Does an animal model for immunogenicity and efficacy exist? | Most mammalian species studied to date have shown induction of insert specific immunity after administration of Ad26-based vaccines, dependent on the studied disease. Several efficacy animal models exist – the most studied animal models have been mice, rabbits, ferrets, cotton rats and several non-human primate (NHP) species. | ||
| 6.7. Does an animal model for antibody enhanced disease or immune complex disease exist? | No | ||
| 6.8. What is known about biodistribution in animal models or in humans? | Biodistribution studies have been conducted in rabbits. Following intramuscular administration, the Ad26 vector did not widely distribute as vector DNA was primarily detected at the site of injection, draining lymph nodes and (to a lesser extent) the spleen. Over time, the number of animals with positive tissues and/or the vector copy number present in those positive tissues declined, indicating clearance of the Ad26 vector. | ||
| 6.9. What is the evidence that vector derived vaccines will generate a beneficial immune response in: | |||
|
Mice, cotton rats, rabbits and ferrets have been shown to develop immune responses against a variety of vaccine inserts. | [9], [52], [54], [55], [58], [63], [64], [65], [66], [67] | |
|
NHP have been shown to develop protective immune responses against a variety of vaccine inserts. | [9], [18], [53], [57], [58], [60], [61], [65], [68], [69] | |
|
Several vaccine inserts in this vector have been shown to be immunogenic in a broad range of populations based on age and location. | [27], [28], [29], [30], [31], [32], [48], [49], [50], [51] | |
| 6.10. Have challenge or efficacy studies been conducted in subjects with: | |||
|
Efficacy studies Efficacy studies are ongoing for Janssen’s HIV and RSV vaccine candidates: HIV VAC89220HPX2008
VAC89220HPX3002
VAC18193RSV2001
Challenge studies have been performed with in malaria and RSV in healthy volunteers.RSV VAC18193RSV2002
MAL-V-A001
|
||
|
Studies in HIV positive participants: There have been no challenge or efficacy studies in HIV-positive participants. A therapeutic vaccination study is ongoing in HIV-positive participants in Thailand. |
The immunogenicity of the Ad26.ZEBOV vaccine has been evaluated in HIV-positive and negative participants in two separate studies. The safety and tolerability profile of the vaccine was similar in HIV-positive and HIV-negative participants (see 8.2). | |
|
n.a. | ||
| 6.11. Have studies been done simultaneously or sequentially administering more than one vector with different transgenes? Is there evidence for interaction/interference? | The prophylactic HIV vaccine is a combination of four vectors, where we have shown that the addition of the fourth vector over the trivalent combination enhanced responses. In a multivalent filovirus vaccine, responses to one out of three of the vaccines was unchanged compared to the single administration. Sequential administration has been shown to be immunogenic upon each following administration, with up to four administrations of the vector tested. | [29], [32], [60] | |
| 7. Adverse Event (AE) Assessment of the Vector (*see Instructions): | Information | Comments/Concerns | Reference[s] |
| 7.1. Approximately how many humans have received this viral vector vaccine to date? If variants of the vector, please list separately. | In total, more than 114,000 participants across 49 clinical studies and Rwanda government led vaccination campaigns have been vaccinated with an Ad26-based vaccine (cut-off: 4 September 2020). The AdVac safety database (version 4, May 2019) contains data from 23 clinical studies using Ad26-based vaccines. Safety data of a total of 3,694 adult participants and 218 children is included in the report of the database. The cut-off date of this report was 21 December 2018. Ebola program Ad26.ZEBOV: 2,668 HIV program Ad26.ENVA.01: 206 Ad26.Mos.HIV: 446 Ad26.Mos4.HIV: 236 Malaria program Ad26.CS.01: 28 RSV program Ad26.RSV.FA2: 59 Ad26.RSV.preF: 211 Filovirus program Ad26.Filo: 43 In more than 40 clinical studies, either ongoing or completed, with a last update as of 4 September 2020 and a vaccination campaign in Rwanda, more than 114,000 participants (including >40,000 children) were vaccinated with an Ad26-based vaccine (cut-off: 4 September 2020; estimate based on the study randomization ratios). |
[70] | |
| 7.2. Method(s) used for safety monitoring: | |||
|
Yes | In most studies, serious AEs and deaths were collected and reported throughout the study or up to 6 months post-vaccination, regardless of time to onset. | |
|
Yes | In most studies, solicited AEs were generally collected for a 7-day post-vaccination period, using a study participant diary. | |
|
Yes | Unsolicited AEs were generally collected up to 28–30 days/4 weeks post-vaccination in most studies. | |
|
Yes | Ebola/Filovirus program: A list of neuroinflammatory disorders were categorized as Immediate Reportable Events (IREs); these were reported to the sponsor within 24 h of becoming aware of the event, using the IRE Form. HIV Program: Confirmed HIV infections and potential immune-mediated diseases were considered an adverse event of special interest (AESI). All AESIs were reported to the sponsor immediately and aggregate analyses performed either at the end of study and possible at interim time points during the studies (for non-efficacy studies only). RSV Pediatric Program (not included in this review): Monitoring for severe lower respiratory tract infection (LRTIs) took place during the whole study period for paediatric participants (enhanced respiratory disease risk [ERD] surveillance). ZIKV Program (not included in this review): A list of neuroinflammatory disorders associated with ZIKV infection were categorized as IRE’s and had to be reported to the sponsor within 24 h after becoming aware of the event using the IRE Form. No IRE’s were reported. |
|
| 7.3. What criteria were used for grading the AEs? | |||
|
Yes | Modified version including company standards for terms, definitions, and grading of solicited AEs. Other modifications are footnoted. | |
|
Yes | Modified version including company standards for terms, definitions, and grading of solicited AEs. Other modifications are footnoted. | |
|
Yes | Modified version including company standards for terms, definitions, and grading of solicited AEs. Other modifications are footnoted. | |
|
Yes | Modified version including company standards for terms, definitions, and grading of solicited AEs. Other modifications are footnoted. | |
| 7.4. List and provide frequency of any related or possibly related serious* AEs observed: | Three suspected unexpected serious adverse reactions (SUSARs) have been reported since the beginning of the Ad26 vaccines programs, as follows: Ad26.Mos.HIV (HIV-V-A004 study): - Hypersensitivity; verbatim: severe allergic response Ad26.ZEBOV (VAC52150EBL2001): - Small fiber neuropathy Ad26.Mos4.HIV (VAC89220HPX2004): - Rheumatoid arthritis |
N = 1 per each reported SUSAR. | [32], [70] |
| 7.5. List and provide frequency of any statistically significantly increased AE or lab abnormality in vaccinee vs. control group: | The safety in Ad26 participants is compared versus placebo participants. All data in the Janssen AdVac safety database were only analyzed descriptively, no statistical testing was performed. Solicited local AEs: Overall, the most frequently reported solicited local AEs were injection-site pain (58.8% of Ad26 participants, compared with 21.9% of placebo participants), injection-site warmth (20.4% and 9.9%, respectively), and injection-site swelling (10.1% and 4.8%, respectively). Injection-site erythema, induration, and pruritus were experienced by fewer than 10% of participants. Solicited systemic AEs: Overall, the most frequently reported solicited systemic AEs for Ad26 participants (reported in ≥30% of participants) were malaise (53.8%), fatigue (49.0%), headache (46.2%), and myalgia (38.9%), all of which were more frequent for Ad26 participants compared with placebo (42.4%, 28.0%, 26.4%, and 16.3% of placebo participants, respectively). Pyrexia was also more frequent in Ad26 participants than in placebo participants (10.7% and 3.2%, respectively). Unsolicited AEs: For Ad26, the most frequently experienced unsolicited AEs were upper respiratory tract infection (4.9%), malaria (3.7%), headache (2.9%), and neutropenia (2.0%). For placebo, these percentages were 6.4%, 1.4%, 2.4%, and 1.6%, respectively. Clinical laboratory evaluation: Decrease in haemoglobin from baseline was the most frequent laboratory abnormality (1,408 of 2,178 Ad26 participants [64.6%] and 235 of 414 placebo participants [56.8%]). It should however be noted that, according to the FDA Toxicity Grading Scale, any decrease in hemoglobin from baseline is considered a laboratory abnormality, even if it is within the normal laboratory reference ranges. Grade 3 abnormalities were infrequent (reported in fewer than 3% of participants) and comparable between Ad26 and placebo participants. |
From the Janssen AdVac safety database (version 4, May 2019). See Section 7.1 | [70] |
|
In most studies, placebo VAC52150EBL3001 (Stage 2 only): MenACWY conjugate vaccine |
||
| 7.6. List and provide frequency of Adverse Events of Special Interest | Three cases of incident HIV infection in Ad26 participants in HIV-V-A004. For all three participants, factors known to increase the risk for HIV infection were present. All three events were assessed by the investigator as not related to study vaccination. | HIV-1 infection is considered an AE of special interest in the Company’s HIV-1 clinical development program with the viral-vectored platform-based vaccines in (including Ad26-based vaccines), and a significant AE under monitoring for the other adenovirus vector-based programs. | [32], [70] |
| 7.7. Did Data Safety Monitoring Board (DSMB) or its equivalent oversee the study? | Yes | All studies are overseen by internal Data Review Committees (DRC) or external Independent Data Monitoring Committees (IDMC) or its equivalent. | |
|
No | IDMC’s/DRC’s did not identify issues. Potential issues were communicated to IDMC’s/DRC’s as per protocol requirements. | |
|
n.a. | ||
| 8. Overall Risk Assessment of the Vector | Information | Comments/Concerns | Reference[s] |
| 8.1. Summarize key safety issues of concern identified to date, if any: | No significant safety issues have been identified. | ||
|
n.a. | ||
| 8.2. What is the potential for causing serious unwanted effects and toxicities in: | Describe the toxicities | Please rate risk as: | |
|
Overall, the Ad26-based vaccines have been well tolerated, without significant safety issues identified. | [70] | |
|
The safety of Ad26.ZEBOV, an Ad26-based vaccine expressing the Ebola GP antigen, has been evaluated in HIV-positive participants on antiretroviral therapy (ART) with CD4+ counts of >350 and >200 cells/µL in two separate studies (VAC52150EBL2002 and VAC52150EBL2003 respectively). In study VAC52150EBL2002, 118 HIV-positive adult participants received a dose of Ad26.ZEBOV at 5 × 1010 vp. In study VAC52150EBL2003, 221 adult participants received a dose of Ad26.ZEBOV at 5 × 1010 vp. The vaccine was well tolerated in terms of local and systemic solicited and non-solicited events, AEs with no SAEs or SUSARs in both studies. The safety and tolerability profile of the vaccine was similar between HIV-positive and HIV-negative participants. | Low risk; HIV-infection was an exclusion criterion in most studies. Exposure HIV-infected adults: VAC52150EBL2002: • 118 HIV-infected adults; CD4+ cells >350 cells/µL VAC52150EBL2003: • 221 HIV-infected adults; CD4+ cells >200 cells/µL VAC89220HTX1001: • 17 HIV-infected adults; CD4+ cells >400 cells/µL VAC89220HTX1002 (actively enrolling): • 20 HIV-infected adults; CD4+ cells >350 cells/µL |
[70] |
|
The AdVac safety database (version 4, May 2019) includes safety data from a total of 218 children between (4 to 17 years of age) who were vaccinated with Ad26.ZEBOV in VAC52150EBL2002. Overall, no safety concerns were identified in children after vaccination with Ad26.ZEBOV. |
Low risk; in seven clinical studies and vaccination campaigns, either ongoing or completed, with a last update of 4 September, >40,000 children (aged 0 to 17 years) were vaccinated with an Ad26-based vaccine (cut-off: 4 September 2020; active only, estimate based on the study randomization ratios). So far, no safety concerns have been identified. | |
|
The AdVac safety database (version 4, May 2019) includes safety data from a total of 180 elderly (≥60 years of age in stable health) who were vaccinated with Ad26.RSV.preF in VAC18193RSV2003. A total of 13 elderly (>64 years of age) participants were also enrolled in VAC52150EBL2002. Overall, no safety concerns were identified in elderly after vaccination with adeno-based vaccines. |
Low risk; In three clinical studies either ongoing or completed with a last update of 21 December 2018, >32,500 elderly participants (≥60 years of age) were vaccinated with an Ad26-based vaccine (cut-off: 1 July 2020; active only, estimate based on the study randomization ratios). No safety concerns were identified. | |
|
The most recent aggregate review of pregnancy exposure data was performed in September 2019; this analysis of the current experience with pregnancies after exposure to the Ebola candidate vaccines (Ad26.ZEBOV, Ad26.Filo) in female participants or partners of male participants did not reveal a safety concern. Serious complications or SAEs during pregnancy were reported in 20 out of a total of 66 pregnancies reported in female study participants. None of these serious complications/SAEs were considered causally associated with the study vaccines by Investigators or the Company. No apparent concernable pattern of AEs is emerging from this review. No congenital malformations were reported to date in foetuses or newborns. Spontaneous abortion was the most commonly observed SAE (9 out of 66 pregnancies) with an incidence of 13.6%, which is within the range of expected spontaneous abortion rates during the first trimester of gestation, even when considering that spontaneous abortion incidences vary significantly depending on geographical areas and individual risk factors (e.g. age, previous abortions). |
Low risk; pregnancy is an exclusion criterion for all Ad26-based vaccine studies except 1 study (described below). Pregnancy tests prior to vaccination and the use of adequate contraception was mandatory for all female participants of childbearing potential. Pregnant women are being enrolled in the ongoing Ebola vaccination study in DRC (DRC-EB-001/EBL3008). |
[71] |
|
n.a. | ||
| 8.3. What is the potential for shedding and transmission in risk groups? | There is no significant risk for shedding and transmission of Ad26-vectored vaccines across the risk groups (e.g. immunocompromised) who have received the vaccine vector. | ||
Extensive safety and immunogenicity data have been obtained from these studies. Overall, in our analysis, all Ad26-based vaccines have been well tolerated, with no significant safety issues identified from the data currently available in the AdVac safety database. Post-vaccination reactogenicity after administration of Ad26-based vaccines consisted of mild-to-moderate adverse events (AEs) that started 1–2 days after vaccination and resolved within 1–3 days. Most participants received Ad26 dose of 5 × 1010 viral particles (vp) but relatively few participants received doses of 1 × 109 vp, 1 × 1010 vp, 9 × 1010 vp, and 1 × 1011 vp making it difficult to establish an effect of dose level on reactogenicity. When only dose groups with more than 100 participants were considered, there was a trend towards an increase in the incidence of local and systemic reactogenicity with an increase in Ad26 dose. Overall, the proportions of participants reporting unsolicited AEs, as well as serious AEs were comparable between the active vaccine and placebo groups. As expected with most vaccines, pyrexia was observed more frequently after administration of Ad26-based vaccines, compared with placebo, and occurred most frequently in younger children. Most episodes of pyrexia were mild or moderate in severity. Occurrences of severe pyrexia were observed with similar frequency after Ad26-based vaccine or placebo administration.
As of 4th September 2020, Ad26-based vaccines have been administered to more than 114,000 individuals and have been shown to have an acceptable safety profile and induce strong and durable humoral and cellular immune responses in clinical trials (Fig. 1). The Ebola vaccine program has largely contributed to this expansion of the experience on Ad26-based vaccines, with two ongoing projects: a large clinical study in the Democratic Republic of the Congo [72] and a government-led vaccination program in Rwanda after conditional approval under exceptional emergency [73]. The Ebola vaccine regimen, consisting of two components, Zabdeno (Ad26.ZEBOV) and Mvabea (MVA-BN-Filo), given approximately 8 weeks apart, has received EC marketing authorization on 1st July 2020 [74].
Ad26-based vaccines are capable of inducing antibodies that have neutralizing and/or other effector functions. The induction of strong CD4+ and CD8+ T cell responses has been correlated with protection or functional cure in pre-clinical models [32], [52], [53]. Responses induced by Ad26-based vaccines can potentially be further augmented and sustained for even longer periods in combination vaccination regimens with, for example, the same antigens in a different presentation format. Combinations with other antigen presentations have been evaluated with soluble proteins, which provided enhanced immune response, or with transgenes in other viral vectors, for instance, the Modified Vaccinia Ankara (MVA) vector, to further expand the humoral and cellular responses.
For Ad5-based vectors, vector-targeting immune responses have been shown to decrease the immune responses against the vaccine insert [4], [5], [6], [7], [8], which limits the use of Ad5-based vectors in human populations worldwide and encourages the development of recombinant adenoviral vectors based on other adenoviral serotypes. In contrast to Ad5-based vaccines, a similarly clear impact of natural- or vector-induced pre-existing immunity to Ad26 on vaccine immunogenicity has not been observed to date in clinical studies. Results from clinical trials assessing repeated administration of Ad26-based vaccination approaches showed that a second or subsequent dose of study vaccine was able to boost humoral and cellular immune responses to HIV antigens (Ad26.EnvA, study IPCAVD001; [28] and Ad26.Mos.HIV, APPROACH study [32]; even in the presence of high Ad26 neutralizing antibody titers induced by the first dose [28]. Similarly, naturally occurring Ad26 neutralizing antibody titers or Ad26-targeting T cell responses at baseline were not associated with decreased immune responses against the vaccine antigen [29], [31].
Very extensive data and evidence have been collected on preclinical immunogenicity and efficacy, preclinical safety, clinical safety and immunogenicity as well as manufacturing and release, supporting the further evaluation and use of Ad26-based vectors for vaccine development. Recently, with a number of partners, the development of a COVID-19 vaccine has started in response to the pandemic caused by the SARS-CoV-2 virus. The prophylactic vaccine, which is based on the Ad26 vector expressing a variant of the SARS-CoV-2 spike protein, has entered in phase 3 clinical trial in September 2020; at the same time, manufacturing is being scaled up with the goal to supply large quantities of vaccine doses across the world [75].
3. Disclaimer
The findings, opinions, conclusions, and assertions contained in this consensus document are those of the individual members of the Working Group. They do not necessarily represent the official positions of any participant’s organization (e.g., government, university, or corporations).
4. Purpose of document
Risk benefit assessment of the Ad26 replication-incompetent viral vector using the Brighton Collaboration V3SWG Standardized Template for Collection of Key Information for Risk Assessment of Viral Vaccine Vector Candidates.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: The Brighton Collaboration V3SWG authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Jerome Custers, Maarten Leyssen, Frank Tomaka, Esther Heijnen, Georgi Shukarev, Dirk Heerwegh, Roy van Heesbeen, Hanneke Schuitemaker, and Macaya Douoguih, are current employees of Janssen Pharmaceuticals and potentially hold stock in J&J.
Acknowledgments
Acknowledgements
We thank the additional V3SWG members and participants for their support and helpful comments, and Patrick Zuber of the World Health Organization for bringing together many of the coauthors for completing the first draft of this template and for his support of the V3SWG. We would also like to thank Wouter Koudstaal (independent scientific writer) and Kerstin Luhn, Benoit Callendret, Maria Pau, Gert Scheper, Jerry Sadoff, Roland Zahn, Ad Knaapen, Jenny Hendriks, Myra Widjojoatmodjo, Marc Ceuppens, Raphaele Roten and Valerie Oriol Mathieu from Janssen for their role in compound development and manuscript preparation, Dan Barouch for his role in the development of Ad26-based vaccine candidates and the Brighton Collaboration Reference Group for their peer review.
Funding for development of Ad26.ZEBOV for Ebola, Ad26.Mos.HIV, Ad26.Mos4.HIV, and Ad26.ENVA.01 for HIV, Ad26.CS.01 for Malaria, Ad26.RSV.FA2 and Ad26.RSV.preF for RSV, Ad26.Filo for Filovirus infection, Ad26.ZIKV.001 for Zika, Ad26.HPV16 and Ad26.HPV18 for HPV including generation of many data presented in the template, was provided by Janssen and/or partners, including in kind support. Main partners are Biological Advanced Research and Development Agency (BARDA), Innovative Medicine Initiative (IMI), Bill and Melinda Gates Foundation (BMGF), Military Health Research Program (MHRP), Beth Israel Deaconess Medical Center, Harvard Medical School (BIDMC), HIV Vaccine Trials Network (HVTN), Ragon Institute and the National Institute of Allergy and Infectious Diseases, National Institutes of Health (NIAID/NIH). Completion of this template was supported by WHO Registration Purchase Order Unit Reference 2019/936983-1202338899-1MVP/EMPISAVISAV.
Authorship
All authors attest they meet the ICMJE criteria for authorship.
Footnotes
Purpose of document: Risk benefit assessment of the Ad26 replication-incompetent viral vector using the Brighton Collaboration V3SWG Standardized Template for Collection of Key Information for Risk Assessment of Viral Vaccine Vector Candidates.
References
- 1.Monath T.P., Fast P.E., Modjarrad K., Clarke D.K., Martin B.K., Fusco J. rVSVΔG-ZEBOV-GP (also designated V920) recombinant vesicular stomatitis virus pseudotyped with Ebola Zaire glycoprotein: standardized template with key considerations for a risk/benefit assessment. Vaccine X. 2019;1 doi: 10.1016/j.jvacx.2019.100009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rosen L., Baron S., Bell J.A. Four newly recognized adenoviruses. Proc Soc Exp Biol Med. 1961;107:434–437. doi: 10.3181/00379727-107-26648. [DOI] [PubMed] [Google Scholar]
- 3.Vogels R., Zuijdgeest D., van Rijnsoever R., Hartkoorn E., Damen I., de Bethune M.P. Replication-deficient human adenovirus type 35 vectors for gene transfer and vaccination: efficient human cell infection and bypass of preexisting adenovirus immunity. J Virol. 2003;77(15):8263–8271. doi: 10.1128/JVI.77.15.8263-8271.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Priddy F.H., Brown D., Kublin J., Monahan K., Wright D.P., Lalezari J. Safety and immunogenicity of a replication-incompetent adenovirus type 5 HIV-1 clade B gag/pol/nef vaccine in healthy adults. Clin Infect Dis. 2008;46(11):1769–1781. doi: 10.1086/587993. [DOI] [PubMed] [Google Scholar]
- 5.McElrath M.J., De Rosa S.C., Moodie Z., Dubey S., Kierstead L., Janes H. HIV-1 vaccine-induced immunity in the test-of-concept Step Study: a case-cohort analysis. Lancet. 2008;372(9653):1894–1905. doi: 10.1016/S0140-6736(08)61592-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frahm N., DeCamp A.C., Friedrich D.P., Carter D.K., Defawe O.D., Kublin J.G. Human adenovirus-specific T cells modulate HIV-specific T cell responses to an Ad5-vectored HIV-1 vaccine. J Clin Invest. 2012;122(1):359–367. doi: 10.1172/JCI60202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheng C., Wang L., Gall J.G., Nason M., Schwartz R.M., McElrath M.J. Decreased pre-existing Ad5 capsid and Ad35 neutralizing antibodies increase HIV-1 infection risk in the Step trial independent of vaccination. PLoS One. 2012;7(4) doi: 10.1371/journal.pone.0033969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Catanzaro A.T., Koup R.A., Roederer M., Bailer R.T., Enama M.E., Moodie Z. Phase 1 safety and immunogenicity evaluation of a multiclade HIV-1 candidate vaccine delivered by a replication-defective recombinant adenovirus vector. J Infect Dis. 2006;194(12):1638–1649. doi: 10.1086/509258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abbink P., Lemckert A.A., Ewald B.A., Lynch D.M., Denholtz M., Smits S. Comparative seroprevalence and immunogenicity of six rare serotype recombinant adenovirus vaccine vectors from subgroups B and D. J Virol. 2007;81(9):4654–4663. doi: 10.1128/JVI.02696-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mast T.C., Kierstead L., Gupta S.B., Nikas A.A., Kallas E.G., Novitsky V. International epidemiology of human pre-existing adenovirus (Ad) type-5, type-6, type-26 and type-36 neutralizing antibodies: correlates of high Ad5 titers and implications for potential HIV vaccine trials. Vaccine. 2010;28(4):950–957. doi: 10.1016/j.vaccine.2009.10.145. [DOI] [PubMed] [Google Scholar]
- 11.Ersching J., Hernandez M.I., Cezarotto F.S., Ferreira J.D., Martins A.B., Switzer W.M. Neutralizing antibodies to human and simian adenoviruses in humans and New-World monkeys. Virology. 2010;407(1):1–6. doi: 10.1016/j.virol.2010.07.043. [DOI] [PubMed] [Google Scholar]
- 12.Chen H., Xiang Z.Q., Li Y., Kurupati R.K., Jia B., Bian A. Adenovirus-based vaccines: comparison of vectors from three species of adenoviridae. J Virol. 2010;84(20):10522–10532. doi: 10.1128/JVI.00450-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barouch D.H., Kik S.V., Weverling G.J., Dilan R., King S.L., Maxfield L.F. International seroepidemiology of adenovirus serotypes 5, 26, 35, and 48 in pediatric and adult populations. Vaccine. 2011;29(32):5203–5209. doi: 10.1016/j.vaccine.2011.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Havenga M., Vogels R., Zuijdgeest D., Radosevic K., Mueller S., Sieuwerts M. Novel replication-incompetent adenoviral B-group vectors: high vector stability and yield in PER.C6 cells. J Gen Virol. 2006;87(Pt 8):2135–2143. doi: 10.1099/vir.0.81956-0. [DOI] [PubMed] [Google Scholar]
- 15.Lichtenstein D.L., Toth K., Doronin K., Tollefson A.E., Wold W.S. Functions and mechanisms of action of the adenovirus E3 proteins. Int Rev Immunol. 2004;23(1–2):75–111. doi: 10.1080/08830180490265556. [DOI] [PubMed] [Google Scholar]
- 16.Roelvink P.W., Lizonova A., Lee J.G., Li Y., Bergelson J.M., Finberg R.W. The coxsackievirus-adenovirus receptor protein can function as a cellular attachment protein for adenovirus serotypes from subgroups A, C, D, E, and F. J Virol. 1998;72(10):7909–7915. doi: 10.1128/jvi.72.10.7909-7915.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bergelson J.M., Cunningham J.A., Droguett G., Kurt-Jones E.A., Krithivas A., Hong J.S. Isolation of a common receptor for Coxsackie B viruses and adenoviruses 2 and 5. Science. 1997;275(5304):1320–1323. doi: 10.1126/science.275.5304.1320. [DOI] [PubMed] [Google Scholar]
- 18.Li H., Rhee E.G., Masek-Hammerman K., Teigler J.E., Abbink P., Barouch D.H. Adenovirus serotype 26 utilizes CD46 as a primary cellular receptor and only transiently activates T lymphocytes following vaccination of rhesus monkeys. J Virol. 2012;86(19):10862–10865. doi: 10.1128/JVI.00928-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nestic D., Uil T.G., Ma J., Roy S., Vellinga J., Baker A.H. αvβ3 integrin is required for efficient infection of epithelial cells with human adenovirus type 26. J Virol. 2019;93(1):e01474–18. doi: 10.1128/JVI.01474-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baker A.T., Mundy R., Davies J., Rizkallah P.J., Parker A.L. Adenovirus serotype 26 utilises sialic acid bearing glycans as a primary cell entry receptor. Sci Adv. 2019;5(9):eaax3567. doi: 10.1126/sciadv.aax3567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Teigler J.E., Kagan J.C., Barouch D.H. Late endosomal trafficking of alternative serotype adenovirus vaccine vectors augments antiviral innate immunity. J Virol. 2014;88(18):10354–10363. doi: 10.1128/JVI.00936-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fallaux F.J., Bout A., van der Velde I., van den Wollenberg D.J., Hehir K.M., Keegan J. New helper cells and matched early region 1-deleted adenovirus vectors prevent generation of replication-competent adenoviruses. Hum Gene Ther. 1998;9(13):1909–1917. doi: 10.1089/hum.1998.9.13-1909. [DOI] [PubMed] [Google Scholar]
- 23.Galazka A., Milstien J., Zaffran M. Thermostability of vaccines. November 2019;1998:04. http://apps.who.int/iris/bitstream/10665/64980/1/WHO_GPV_98.07.pdf Available from. [Google Scholar]
- 24.Chen D., Kristensen D. Opportunities and challenges of developing thermostable vaccines. Exp Rev Vacc. 2009;8(5):547–557. doi: 10.1586/erv.09.20. [DOI] [PubMed] [Google Scholar]
- 25.Capelle M.A.H., Babich L., van Deventer-Troost J.P.E., Salerno D., Krijgsman K., Dirmeier U. Stability and suitability for storage and distribution of Ad26.ZEBOV/MVA-BN(R)-Filo heterologous prime-boost Ebola vaccine. Eur J Pharm Biopharm. 2018;129:215–221. doi: 10.1016/j.ejpb.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 26.Winslow R.L., Milligan I.D., Voysey M., Luhn K., Shukarev G., Douoguih M. Immune responses to novel adenovirus type 26 and modified vaccinia virus ankara-vectored Ebola vaccines at 1 year. JAMA. 2017;317(10):1075–1077. doi: 10.1001/jama.2016.20644. [DOI] [PubMed] [Google Scholar]
- 27.Milligan I.D., Gibani M.M., Sewell R., Clutterbuck E.A., Campbell D., Plested E. Safety and immunogenicity of novel adenovirus type 26- and modified vaccinia ankara-vectored Ebola vaccines: a randomized clinical trial. JAMA. 2016;315(15):1610–1623. doi: 10.1001/jama.2016.4218. [DOI] [PubMed] [Google Scholar]
- 28.Baden L.R., Walsh S.R., Seaman M.S., Tucker R.P., Krause K.H., Patel A. First-in-human evaluation of the safety and immunogenicity of a recombinant adenovirus serotype 26 HIV-1 Env vaccine (IPCAVD 001) J Infect Dis. 2013;207(2):240–247. doi: 10.1093/infdis/jis670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barouch D.H., Liu J., Peter L., Abbink P., Iampietro M.J., Cheung A. Characterization of humoral and cellular immune responses elicited by a recombinant adenovirus serotype 26 HIV-1 Env vaccine in healthy adults (IPCAVD 001) J Infect Dis. 2013;207(2):248–256. doi: 10.1093/infdis/jis671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baden L.R., Liu J., Li H., Johnson J.A., Walsh S.R., Kleinjan J.A. Induction of HIV-1-specific mucosal immune responses following intramuscular recombinant adenovirus serotype 26 HIV-1 vaccination of humans. J Infect Dis. 2015;211(4):518–528. doi: 10.1093/infdis/jiu485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baden L.R., Karita E., Mutua G., Bekker L.G., Gray G., Page-Shipp L. Assessment of the safety and immunogenicity of 2 novel vaccine platforms for HIV-1 prevention: a randomized trial. Ann Intern Med. 2016;164(5):313–322. doi: 10.7326/M15-0880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barouch D.H., Tomaka F.L., Wegmann F., Stieh D.J., Alter G., Robb M.L. Evaluation of a mosaic HIV-1 vaccine in a multicentre, randomised, double-blind, placebo-controlled, phase 1/2a clinical trial (APPROACH) and in rhesus monkeys (NHP 13–19) Lancet. 2018;392(10143):232–243. doi: 10.1016/S0140-6736(18)31364-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Talley A.K., Healy S.A., Salas C.J., Hume J.C.C., Wang R., Lundebjerg S.J. Safety and preliminary efficacy of CS-based recombinant adenoviral serotype 35 and serotype 26 malaria vaccine candidates in prime-boost vaccination of healthy adults undergoing subsequent experimental P. falciparum sporozoite challenge (ABSTRACT) 61st ASTMH Meeting. 2012 [Google Scholar]
- 34.CDC. Adenovirus Transmission: National Center for Immunization and Respiratory Diseases, Division of Viral Diseases, Atlanta, GA, USA; 2019 [updated August 28, 2019. Available from: https://www.cdc.gov/adenovirus/about/transmission.html.
- 35.Crenshaw B.J., Jones L.B., Bell C.R., Kumar S., Matthews Q.L. Perspective on adenoviruses: epidemiology, pathogenicity, and gene therapy. Biomedicines. 2019;7(3):61. doi: 10.3390/biomedicines7030061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rauschhuber C., Noske N., Ehrhardt A. New insights into stability of recombinant adenovirus vector genomes in mammalian cells. Eur J Cell Biol. 2012;91(1):2–9. doi: 10.1016/j.ejcb.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 37.Feuerbach F.J., Crystal R.G. Progress in human gene therapy. Kidney Int. 1996;49(6):1791–1794. doi: 10.1038/ki.1996.269. [DOI] [PubMed] [Google Scholar]
- 38.Ehrhardt A., Haase R., Schepers A., Deutsch M.J., Lipps H.J., Baiker A. Episomal vectors for gene therapy. Curr Gene Ther. 2008;8(3):147–161. doi: 10.2174/156652308784746440. [DOI] [PubMed] [Google Scholar]
- 39.EMA. Guideline on nonclinical testing for inadvertent germline transmission of gene transfer vectors 2006 28 February 2019. Available from: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-non-clinical-testing-inadvertent-germline-transmission-gene-transfer-vectors_en.pdf.
- 40.Kasel J.A., Evans H.E., Spickard A., Knight V. Conjunctivitis and enteric infection with adenovirus types 26 and 27: responses to primary, secondary and reciprocal cross-challenges. Am J Hyg. 1963;77:265–282. doi: 10.1093/oxfordjournals.aje.a120318. [DOI] [PubMed] [Google Scholar]
- 41.Dubberke E.R., Tu B., Rivet D.J., Storch G.A., Apisarnthanarak A., Schmidt R.E. Acute meningoencephalitis caused by adenovirus serotype 26. J Neurovirol. 2006;12(3):235–240. doi: 10.1080/13550280600846633. [DOI] [PubMed] [Google Scholar]
- 42.Lion T. Adenovirus infections in immunocompetent and immunocompromised patients. Clin Microbiol Rev. 2014;27(3):441–462. doi: 10.1128/CMR.00116-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hierholzer J.C. Adenoviruses in the immunocompromised host. Clin Microbiol Rev. 1992;5(3):262–274. doi: 10.1128/cmr.5.3.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sprangers M.C., Lakhai W., Koudstaal W., Verhoeven M., Koel B.F., Vogels R. Quantifying adenovirus-neutralizing antibodies by luciferase transgene detection: addressing preexisting immunity to vaccine and gene therapy vectors. J Clin Microbiol. 2003;41(11):5046–5052. doi: 10.1128/JCM.41.11.5046-5052.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wold W.S., Toth K. New drug on the horizon for treating adenovirus. Exp Opin Pharmacother. 2015;16(14):2095–2099. doi: 10.1517/14656566.2015.1083975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.CDC. Adenovirus Prevention and Treatment: National Center for Immunization and Respiratory Diseases, Division of Viral Diseases, Atlanta, GA, USA; 2019 [updated August 29, 2019. Available from: https://www.cdc.gov/adenovirus/about/prevention-treatment.html.
- 47.Sanjuan R., Nebot M.R., Chirico N., Mansky L.M., Belshaw R. Viral mutation rates. J Virol. 2010;84(19):9733–9748. doi: 10.1128/JVI.00694-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shukarev G, Callendret B, Luhn K, Douoguih M, Consortium E. A two-dose heterologous prime-boost vaccine regimen eliciting sustained immune responses to Ebola Zaire could support a preventive strategy for future outbreaks. Hum Vaccin Immunother 2017;13(2):266–70. [DOI] [PMC free article] [PubMed]
- 49.Mutua G., Anzala O., Luhn K., Robinson C., Bockstal V., Anumendem D. Safety and immunogenicity of a 2-dose heterologous vaccine regimen with Ad26.ZEBOV and MVA-BN-Filo Ebola vaccines: 12-month data from a phase 1 randomized clinical trial in Nairobi, Kenya. J Infect Dis. 2019;220(1):57–67. doi: 10.1093/infdis/jiz071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Anywaine Z., Whitworth H., Kaleebu P., Praygod G., Shukarev G., Manno D. Safety and immunogenicity of a 2-dose heterologous vaccination regimen with Ad26.ZEBOV and MVA-BN-Filo Ebola vaccines: 12-month data from a phase 1 randomized clinical trial in Uganda and Tanzania. J Infect Dis. 2019;220(1):46–56. doi: 10.1093/infdis/jiz070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bett A.J., Prevec L., Graham F.L. Packaging capacity and stability of human adenovirus type 5 vectors. J Virol. 1993;67(10):5911–5921. doi: 10.1128/jvi.67.10.5911-5921.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Khan S., Oosterhuis K., Wunderlich K., Bunnik E.M., Bhaggoe M., Boedhoe S. Development of a replication-deficient adenoviral vector-based vaccine candidate for the interception of HPV16- and HPV18-induced infections and disease. Int J Cancer. 2017;141(2):393–404. doi: 10.1002/ijc.30679. [DOI] [PubMed] [Google Scholar]
- 53.Borducchi E.N., Cabral C., Stephenson K.E., Liu J., Abbink P., Ng'ang'a D. Ad26/MVA therapeutic vaccination with TLR7 stimulation in SIV-infected rhesus monkeys. Nature. 2016;540(7632):284–287. doi: 10.1038/nature20583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zahn R., Gillisen G., Roos A., Koning M., van der Helm E., Spek D. Ad35 and ad26 vaccine vectors induce potent and cross-reactive antibody and T-cell responses to multiple filovirus species. PLoS One. 2012;7(12) doi: 10.1371/journal.pone.0044115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Widjojoatmodjo M.N., Bogaert L., Meek B., Zahn R., Vellinga J., Custers J. Recombinant low-seroprevalent adenoviral vectors Ad26 and Ad35 expressing the respiratory syncytial virus (RSV) fusion protein induce protective immunity against RSV infection in cotton rats. Vaccine. 2015;33(41):5406–5414. doi: 10.1016/j.vaccine.2015.08.056. [DOI] [PubMed] [Google Scholar]
- 56.Mooney T., Smout E., Leigh B., Greenwood B., Enria L., Ishola D. EBOVAC-Salone: Lessons learned from implementing an Ebola vaccine trial in an Ebola-affected country. Clin Trials. 2018;15(5):436–443. doi: 10.1177/1740774518780678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kang Z.H., Bricault C.A., Borducchi E.N., Stephenson K.E., Seaman M.S., Pau M. Similar epitope specificities of IgG and IgA antibodies elicited by Ad26 vector prime, Env protein boost immunizations in rhesus monkeys. J Virol. 2018;92(15):e00537–18. doi: 10.1128/JVI.00537-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Geisbert T.W., Bailey M., Hensley L., Asiedu C., Geisbert J., Stanley D. Recombinant adenovirus serotype 26 (Ad26) and Ad35 vaccine vectors bypass immunity to Ad5 and protect nonhuman primates against ebolavirus challenge. J Virol. 2011;85(9):4222–4233. doi: 10.1128/JVI.02407-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cox F., van der Fits L., Abbink P., Larocca R.A., van Huizen E., Saeland E. Adenoviral vector type 26 encoding Zika virus (ZIKV) M-Env antigen induces humoral and cellular immune responses and protects mice and nonhuman primates against ZIKV challenge. PLoS One. 2018;13(8) doi: 10.1371/journal.pone.0202820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Callendret B., Vellinga J., Wunderlich K., Rodriguez A., Steigerwald R., Dirmeier U. Correction: A prophylactic multivalent vaccine against different filovirus species is immunogenic and provides protection from lethal infections with Ebolavirus and Marburgvirus species in non-human primates. PLoS One. 2018;13(4) doi: 10.1371/journal.pone.0192312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Barouch D.H., Alter G., Broge T., Linde C., Ackerman M.E., Brown E.P. Protective efficacy of adenovirus/protein vaccines against SIV challenges in rhesus monkeys. Science. 2015;349(6245):320–324. doi: 10.1126/science.aab3886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Boshart M., Weber F., Jahn G., Dorsch-Hasler K., Fleckenstein B., Schaffner W. A very strong enhancer is located upstream of an immediate early gene of human cytomegalovirus. Cell. 1985;41(2):521–530. doi: 10.1016/s0092-8674(85)80025-8. [DOI] [PubMed] [Google Scholar]
- 63.Weaver E.A., Barry M.A. Low seroprevalent species D adenovirus vectors as influenza vaccines. PLoS One. 2013;8(8) doi: 10.1371/journal.pone.0073313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Radosevic K., Rodriguez A., Lemckert A.A., van der Meer M., Gillissen G., Warnar C. The Th1 immune response to Plasmodium falciparum circumsporozoite protein is boosted by adenovirus vectors 35 and 26 with a homologous insert. Clin Vaccine Immunol. 2010;17(11):1687–1694. doi: 10.1128/CVI.00311-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Penaloza-MacMaster P., Provine N.M., Ra J., Borducchi E.N., McNally A., Simmons N.L. Alternative serotype adenovirus vaccine vectors elicit memory T cells with enhanced anamnestic capacity compared to Ad5 vectors. J Virol. 2013;87(3):1373–1384. doi: 10.1128/JVI.02058-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cuburu N., Khan S., Thompson C.D., Kim R., Vellinga J., Zahn R. Adenovirus vector-based prime-boost vaccination via heterologous routes induces cervicovaginal CD8(+) T cell responses against HPV16 oncoproteins. Int J Cancer. 2018;142(7):1467–1479. doi: 10.1002/ijc.31166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Alyahya S.A., Nolan S.T., Smith C.M., Bishai W.R., Sadoff J., Lamichhane G. Immunogenicity without Efficacy of an Adenoviral Tuberculosis Vaccine in a Stringent Mouse Model for Immunotherapy during Treatment. PLoS One. 2015;10(5) doi: 10.1371/journal.pone.0127907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Teigler J.E., Iampietro M.J., Barouch D.H. Vaccination with adenovirus serotypes 35, 26, and 48 elicits higher levels of innate cytokine responses than adenovirus serotype 5 in rhesus monkeys. J Virol. 2012;86(18):9590–9598. doi: 10.1128/JVI.00740-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Abbink P, Larocca RA, Visitsunthorn K, Boyd M, De La Barrera RA, Gromowski GD, et al. Durability and correlates of vaccine protection against Zika virus in rhesus monkeys. Sci Transl Med 2017;9(420):eaa04163. [DOI] [PMC free article] [PubMed]
- 70.Janssen Vaccines and Prevention B.V. Adenoviral Vaccine Safety Database V4.0. 14 May ed2019.
- 71.Delabaere A., Huchon C., Deffieux X., Beucher G., Gallot V., Nedellec S. Epidemiology of loss pregnancy. J Gynecol Obstet Biol Reprod (Paris) 2014;43(10):764–775. doi: 10.1016/j.jgyn.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 72.Johnson & Johnson. Innovation: Johnson & Johnson announces donation of up to 500,000 regimens of Janssen’s investigational Ebola vaccine to support outbreak response in Democratic Republic of the Congo (DRC). New Brunswick, NJ, October 31 2019. https://www.jnj.com/johnson-johnson-announces-donation-of-up-to-500-000-regimens-of-janssens-investigational-ebola-vaccine-to-support-outbreak-response-in-democratic-republic-of-the-congo-drc (Accessed June 11 2020).
- 73.Johnson & Johnson. Our Company: Johnson & Johnson announces commitment to support Republic of Rwanda’s preparedness against Ebola outbreak. New Brunswick, NJ, December 8 2019. https://www.jnj.com/johnson-johnson-announces-commitment-to-support-republic-of-rwandas-preparedness-against-ebola-outbreak (Accessed June 11 2020).
- 74.European Commission. Vaccine against Ebola: Commission grants new market authorisations. July 1 2020. https://ec.europa.eu/commission/presscorner/detail/en/ip_20_1248 (Accessed September 1 2020).
- 75.Johnson & Johnson. Our efforts to develop a vaccine and identify therapies for COVID-19. https://www.jnj.com/coronavirus/prevention-and-treatment (Accessed June 11 2020).