Abstract
Background:
Spinal teratomas are rare in adults. The clinical findings are nonspecific, reflecting only in the intramedullary location of these lesions. The potential differential diagnosis for intramedullary spinal teratomas include schwannomas, dermoids, epidermoids, and neurofibromas.
Case Description:
A 25-year-old male presented with RLE weakness (iliopsoas/quadriceps [4/5], and extensor hallucis longus/dorsiflexor [0/5]) and urinary incontinence. As the contrast, MR showed a heterogeneous intramedullary lesion with well-defined edges located at the T12-L1 level, the patient underwent a focal laminectomy for gross total tumor excision. Pathologically, it proved to be a mature teratoma.
Conclusion:
Teratomas should be considered among the differential diagnostic considerations for intramedullary spinal cord lesions. Although gross total resection is preferred, these lesions have a low recurrence rate, and therefore, partial removal is also valid, where lesions are densely adherent to adjacent neural structures.
Keywords: Intradural intramedullary, Spinal tumor, Teratoma of spinal cord

INTRODUCTION
Spinal teratomas constitute only 0.15–0.18% of all intraspinal tumors and are more commonly found in children. Potential differential diagnoses for these lesions include schwannomas, dermoids, epidermoids, and neurofibromas.[1] Here, we present[2] a 25-year-old male who underwent total excision of aT12-L1 thoracolumbar intramedullary mature teratoma.[2]
CASE REPORT
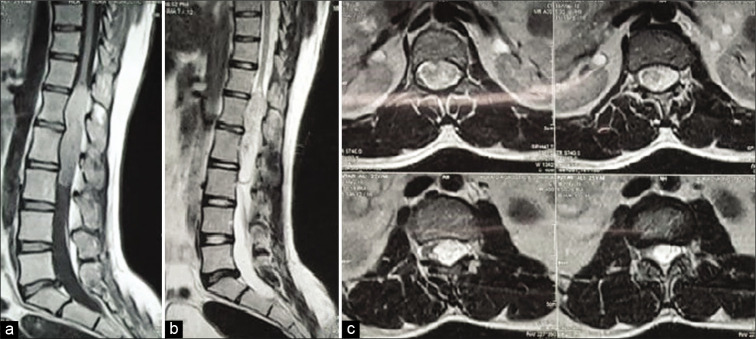
A 25-year-old male presented with backache and a progressive left lower extremity proximal paresis (iliopsoas/quadriceps 4/5) and a distal severe foot drop (extensor hallucis longus/ dorsiflexor 0/5) of 5 months duration. As his bladder was not completely emptying, he required a Foley catheter. The enhanced MRI of the lumbar spine showed a T12-L1 intramedullary lesion involving the conus medullaris/proximal filum terminale [Figure 1].
Figure 1:
MRI images showing T1 sagittal image (a), T2 sagittal image of dorsolumbar spine (b), and (c) axial contrast images showing hetertogenous intradural intramedullary involving dorsal cord and conus.
Surgery
Following a D12-L1 laminectomy, gross total excision of an intramedullary lesion was achieved, including total removal of tumor capsule. Postoperatively, the improved within 1 month (e.g., left iliopsoas/quadriceps 5/5 and the left-sided foot drop (2/5), and the urinary dysfunction resolved. Histopathologically, the tumor was found to be a mature teratoma [Figures 2 and 3].
Figure 2:
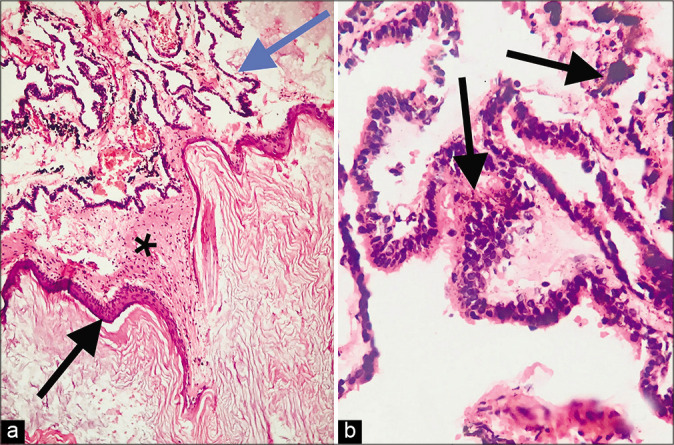
Histopathology showed mature teratoma comprising of (a) cyst lined by keratinizing stratified squamous epithelium (black arrow) filled with keratin flakes, beneath which was seen glial tissue (starred), and choroidal tissue (blue arrow) comprised convoluted strips of epithelium forming papillae (H&E, 100x). (b) High magnification showing stratified tall columnar epithelium with intracytoplasmic and stromal neuromelanin pigment (black arrows) (H&E, 400×).
Figure 3:
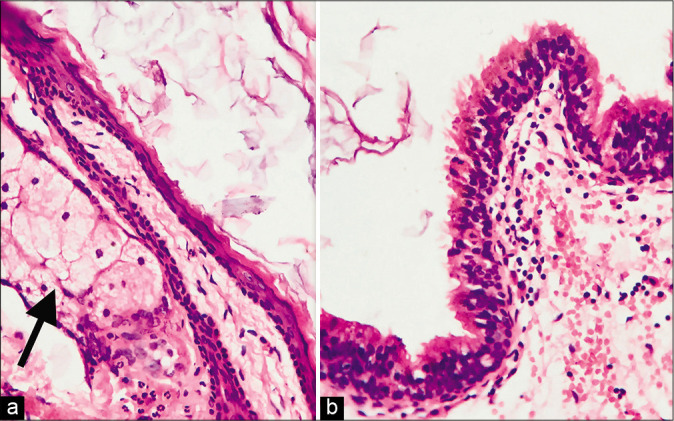
High power magnification showed (a) pilosebaceous units (arrow) embedded in cyst wall and (b) focal lining by stratified ciliated columnar epithelium. (H&E, 400×).
DISCUSSION
Frequency of spinal teratomas
In pediatric patients, 5–10% of spinal lesions are intraspinal teratomas,[4-7] while the incidence in adults is far lower.[4-7] Mature teratomas constitute approximately 0.15–0.18% of all spinal tumors,[3-5] MRI is the most valuable preoperative diagnostic tool, but a tissue diagnosis is critical to confirm the histopathology.[3,7]
Treatment options
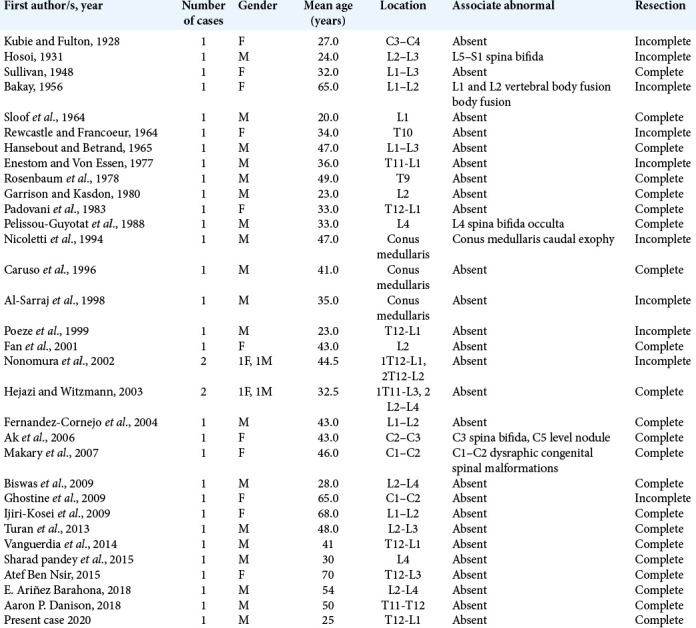
The treatment for spinal teratomas is primarily surgery, whether ideally gross total or subtotal/partial resection. It was found that intramedullary teratomas could be completely removed in 61.8% of cases.[4] Nevertheless, symptomatic recurrence rates for mature teratomas are extremely low including for incomplete resections.[5,8] Therefore, \subtotal and partial tumor excisions are viable alternatives, particularly where lesion’s capsule is densely adherent to critical adjacent neural structures risking increased neurological deficits with “aggressive” tumor removal. Of interest, adjuvant radiotherapy is not recommended for benign teratomas, just malignant lesions, and there is no role adjuvant chemotherapy [Table 1].[2-7]
Table 1:
Table showing details of previously reported similar cases.
The use of intraoperative electrophysiologic monitoring is extremely helpful in the resection of these lesions, as it signals when dissection should be stopped (e.g., for densely adherent lesions) before incurring permanent neurological sequelae.
CONCLUSION
Intradural spinal teratomas are very rare in adults. Once documented on preoperative MR studies, either gross total, subtotal, or partial resections are viable surgical alternatives as all result in good long-term outcomes with a low recurrence rate.
Footnotes
How to cite this article: Acharya A, Grewal SS, Sobti S, John PS, Bind RK, Bhardwaj MK, et al. Intramedullary mature teratoma of spinal cord: A rare tumor with review of literature. Surg Neurol Int 2020;11:266.
Contributor Information
Ashish Acharya, Email: ashish.acharya@live.in.
Sarvpreet Singh Grewal, Email: sarvpreetgrewal@yahoo.co.in.
Shivender Sobti, Email: sobtish@gmail.com.
Paul Sudhakar John, Email: paulsjohn@gmail.com.
Ravindra Kumar Bind, Email: drrkbind.medic@gmail.com.
Maneesh Kumar Bhardwaj, Email: maneeshkbhardwaj@gmail.com.
Shefin J. Mathews, Email: shef.mattrdr@gmail.com.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Agay AK, Garg S, Hedaoo K. Spinal intradural extramedullary mature cystic teratoma in young adult: A rare tumor with review of literature. Int J Res Med Sci. 2016;4:5481–3. [Google Scholar]
- 2.Banna M, Talalla A. Intraspinal dermoids in adults. Br J Radiol. 1975;48:28–30. doi: 10.1259/0007-1285-48-565-28. [DOI] [PubMed] [Google Scholar]
- 3.Danison AP, Ramanathan D, Matin M, Kim K, Panchal RR. Adult thoracic intradural exophytic mature teratoma: Case report and literature review. Asian J Neurosurg. 2018;13:1182–5. doi: 10.4103/ajns.AJNS_370_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garrison JE, Kasdon DL. Intramedullary spinal teratoma: Case report and review of the literature. Neurosurgery. 1980;7:509–12. doi: 10.1227/00006123-198011000-00018. [DOI] [PubMed] [Google Scholar]
- 5.Nonomura Y, Miyamoto K, Wada E, Hosoe H, Nishimoto H, Ogura H, et al. Intramedullary teratoma of the spine: Report of two adult cases. Spinal Cord. 2002;40:40–3. doi: 10.1038/sj.sc.3101247. [DOI] [PubMed] [Google Scholar]
- 6.Rosenbaum TJ, Soule EH, Onofrio BM. Teratomatous cyst of the spinal canal. Case report. J Neurosurg. 1978;49:292–7. doi: 10.3171/jns.1978.49.2.0292. [DOI] [PubMed] [Google Scholar]
- 7.Shikata J, Yamamuro T, Mikawa Y, Kotoura Y. Intraspinal epidermoid and dermoid cysts. Surgical results of seven cases. Arch Orthop Trauma Surg. 1988;107:105–9. doi: 10.1007/BF00454496. [DOI] [PubMed] [Google Scholar]