Abstract
As with many other infectious and chronic conditions, the COVID-19 crisis in the United States (U.S.) reveals severe inequities in health. The objective of this study was to describe public perceptions of disparities in mortality from COVID-19 and examine correlates of those perceptions. We fielded a nationally-representative survey in late April 2020, asking participants how much they agreed with four statements describing group-level COVID-19 disparities: older people compared to younger, people with chronic health conditions compared to those without, poorer people compared to wealthier, and Black people compared to white people. We also measured personal characteristics, experience with COVID-19, and information sources. Overall agreement with age- and health condition-related disparities was high (>80%) while agreement with socioeconomic (SES) and racial disparities was lower (52%). Higher education and income were generally associated with greater agreement with disparities. Partisanship and information sources used were associated with perceptions of SES- and racial-disparities, with Democrats and those attune to national news—but not Fox cable news—more likely to perceive these disparities. As of April 2020, information about age- and health condition-related disparities in COVID-19 was well known by the U.S. public, while information about social disparities was less recognized and varied along socioeconomic and partisan lines.
Keywords: Public opinion, COVID-19, Media, United States, Health disparities
Highlights
-
•
Survey data show most people recognized age- and health-related COVID-19 disparities.
-
•
Fewer (52%) people recognized COVID-19 mortality disparities by income or race.
-
•
People with higher income or education recognized disparities more.
-
•
Democrats recognized social group disparities more than Republicans.
-
•
The news sources people reported using related to their perceptions of disparities.
The killing of George Floyd by police in Minneapolis in late May 2020 led to demonstrations around the United States (U.S.), putting racial inequities—in policing, as well as in health—at the top of the media agenda by mid-2020. But in the weeks prior to late May, evidence was already emerging about COVID-19 disparities. As with many other infectious and chronic conditions, the COVID-19 crisis in the United States reveals severe health inequity (Williams and Cooper, 2020). Specifically, data from the U.S. and elsewhere indicate older people, people with chronic conditions, people of lower socioeconomic status (SES), and people of color are all more likely to die of COVID-19 than other groups (CDC, 2020b; Williams and Cooper, 2020; Williamson et al., 2020).
While the disproportionate burden of COVID-19 infections and mortality among Black people and lower-wage workers had received attention among public health scholars (Bailey et al., 2020) and some U.S. national media outlets (Bouie, 2020; Pinsker, 2020) in the early stages of the pandemic (March–April 2020), how much this information had disseminated to inform the public's understanding is unclear. This is important because public perceptions of health inequities influence policy, practice, and behavior change (Niederdeppe et al., 2013; Williams and Purdie-Vaughns, 2016). If the general public (and key stakeholders) understand the disproportionate risk faced by certain demographic groups, they may, for example, advocate for policy change or allocation of resources to ameliorate inequity, as public awareness of an issue is a pre-requisite for advocacy and strategic pressure on elected officials (Farrer et al., 2015). Further, given documented group differences across the public in understanding of COVID-19 (Alsan et al., 2020), improved understanding of differential risk could contribute to risk mitigation for groups most vulnerable to negative outcomes.
Previous survey research has documented relatively low awareness of health disparities among the public (Benz et al., 2011; Booske et al., 2011; Bye et al., 2016; Carman et al., 2019) and policymakers alike (Purtle et al., 2018). Booske et al. (2011) found that while 73% of Americans were aware of health disparities by income, only 46% were aware of racial health disparities between African Americans and whites. Similarly, Benz et al. (2011) found that 40% of Americans were aware that African Americans are worse off than whites in terms of getting needed health care, 45% were aware of racial disparities in life expectancy, and 35% were aware of racial disparities in general health. Bye et al. (2016) found that only 32% of Americans believed that African Americans have a more difficult time accessing health care than whites.
Individual-level factors may explain this variation. First, partisan or ideological identity shapes acknowledgement of health disparities (Booske et al., 2011; Gollust and Cappella, 2014) as well as acceptance of the broader social determinants of health (Gollust et al., 2009). For example, in one study, conservatives were 30 percentage points less likely than liberals to be aware of racial health disparities (Booske et al., 2011). Second, people with higher SES tend to have higher awareness of health disparities (Booske et al., 2011; Bye et al., 2016). Partisanship and SES are thus likely to correlate with perceptions of disparities in COVID-19, as well.
Personal or community experience could also shape these perceptions. Because of vast geographic variation in COVID-19 incidence and mortality rates (CDC, 2020a), information flows and public understanding will also vary, with those people with personal experience or who reside in communities where mortality rates are higher potentially being more aware of disparities.
Information sources may also play a role. More people get their news from local outlets than from national sources (Pew, 2019), and given the county-by-county variation in the severity of the COVID-19 crisis, variation in attention to disparities in local news may also contribute to differential perceptions among the public. Differences in structural factors at news outlets (i.e., staffing, ownership, political ideology) may also contribute to differences in coverage of disparities across local media environments (Gollust et al., 2019; Gollust and Lantz, 2009). Explanations of racial health disparities in COVID-19 appeared in some national news sources as early as April, likely because of proximity to the areas where striking disparities statistics were available, such as New York City (Bouie, 2020). Emerging research suggests that media sources presented the COVID-19 pandemic in very different ways, with more accurate presentations on national network TV news (e.g., ABC, CBS) and national print news, and more misinformation or downplaying the threat on cable TV, particularly Fox News (Jamieson and Albarracin, 2020; Motta et al., 2020) Finally, people access COVID-19 information not only through news outlets but also through other information channels like health departments; it is unclear whether exposure to such sources contributed to different understanding of the pandemic.
The purpose of this study was to describe the U.S. public's perceptions of disparities in COVID-19 as of late April 2020. Using a nationally-representative survey of Americans, we estimated public perceptions of COVID-19 mortality disparities and then examined correlates of these perceptions, including media sources, partisanship, and both personal and community-level experience with COVID-19.
1. Methods
1.1. Data
Data were collected as part of the AmeriSpeak Omnibus survey, fielded by NORC through online and phone modes from April 23–27, 2020. Respondents were drawn from the AmeriSpeak Panel, a panel of approximately 43,000 research participants recruited through area probability and address-based sampling to be representative of the national U.S. household population. The panel recruitment rate is 34.2%. Researchers use the AmeriSpeak panel to assess public opinion about a range of public health issues.(McGinty et al., 2020; Stone et al., 2020) The Omnibus survey is a bi-weekly cross-sectional survey of AmeriSpeak panelists and is a shared platform on which researchers can contribute items. The Omnibus on which study items were included had a final sample size of 1007 adults and a completion rate of 14.4% among those invited to participate. The University of Minnesota Institutional Review Board approved this study, determining it to have met the criteria for exemption (Category 2).
1.2. Measures
1.2.1. Perceptions of disparities
The main outcomes were four items asking participants how much they agreed with statements describing disparities: “Older people are more likely to die of complications from COVID-19 (coronavirus) than younger people”; “People with chronic health conditions are more likely to die of complications from COVID-19 (coronavirus) than people without such conditions”; “Poorer people are more likely to die of complications from COVID-19 (coronavirus) than wealthier people”; and “Blacks/African Americans are more likely to die of complications of COVID-19 (coronavirus) than White people.” Responses were measured as “Strongly Disagree”, “Disagree”, “Neither Agree nor Disagree”, “Agree”, and “Strongly Agree.” We also created dichotomous measures of agreement, combining “Agree” and “Strongly Agree.”
1.2.2. Demographic characteristics, region of residence, and partisanship
Demographic characteristics were provided by NORC and categorized as follows: gender (male, female), age (18–29, 30–44, 45–59, 60+), race/ethnicity (White, non-Hispanic; Black, non-Hispanic; Hispanic; other), education (less than high school; high school graduate; some college; bachelor's degree or higher), annual household income (<$25,000, $25,000–$49,999, $50,000–$74,999, $75,000–$99,000, $100,000+) and region of residence (Northeast, Midwest, South, West). To measure partisan affiliation, we included a 7-point self-placement measure(Green and Schickler, 1993) (“Strong Democrat”, “Democrat”, “Someone who leans Democratic”, “An Independent”, “Someone who leans Republican”, “A Republican”, and “A strong Republican”) from which we constructed three categories: Democrat (including leaners), Independent, and Republican (including leaners).
1.2.3. Personal experience with COVID-19
The first item measuring personal experience with COVID-19 asked, “Have you been told by a doctor or other health care professional that you have COVID-19 (coronavirus)?” Response options were “No”, “No, but I have or have had concerning symptoms”, “Yes” and “I don't know.” The second item asked, “Do you personally know anyone, other than yourself, who has been told by a doctor or other health care provider that they have COVID-19 (coronavirus)? Response options included “No”, “Yes”, and “I don't know.” A dichotomous measure of personal experience was created by combining those who indicated they themselves had coronavirus or symptoms or that they personally knew someone who did (1) compared to “no” and “I don't know” options (0).
1.2.4. Community experience with COVID-19
Since perceptions of disparities in mortality might be a function of how severe mortality was in participants' communities when surveyed, we merged a measure of contemporaneous county-level COVID-19 mortality rate (collected by Kaiser Health News, as of April 22, 2020) (Szabo and Recht, 2020) to the survey data based on participants' county of residence. We categorized mortality rates by quartile (<1 per 100,000, 1–3 per 100,000, 3–9 per 100,000, >9 per 100,000).
1.2.5. Information sources about COVID-19
Participants were asked: “Thinking now about specific information sources, which of the following sources have you turned to for information about COVID-19 (coronavirus) in the past week?” Respondents could check all that apply from a list of 16 options (see Appendix). Based on our expectations that certain partisan-oriented sources might convey different information about COVID-19 disparities and that national and local news sources might differ, we constructed the following dichotomous categories from the checklist: (1) Fox News; (2) CNN or MSNBC; (3) National news (combining national network TV news, NPR, the New York Times, and the Washington Post; (4) Local news (combining local TV news and local print news); (5) State governor briefings—Republican state (measured as 1 if respondent indicated they got information from a Governor's briefing, and they lived in a state with a Republican governor in April 2020; 0 otherwise); (6) State governor briefings—Democratic state (as measured as 1 if respondent indicated they got information from a Governor's briefing, and they lived in a state with a Democratic governor; 0 otherwise); (7) White House press briefings; (8) health information source (CDC, WHO, or a state health department); and (9) Other people.
1.3. Analysis
We used descriptive statistics to summarize agreement with the four disparities statements. We estimated multivariable logistic regression models of agreement with each of the types of disparities including demographic characteristics, partisanship, media / information sources used, experience with COVID-19, and county-level mortality rates. Odds ratios (OR) and 95% confidence intervals (CI) are presented. We then calculated predicted probabilities of agreeing with each disparity statement from these models and their associated 95% CIs. We conducted a sensitivity analysis to account for the potential correlation among multiple participants within a county; results were not substantively different and so are not presented. All analyses were conducted using SAS 9.4 (Cary, NC) and STATA 13.0. Analyses used the NORC-provided survey weights to adjust the estimates to be nationally-representative; weighted percentages are presented. Sample descriptive characteristics are presented in Appendix Table A1.
2. Results
Table 1 displays the percent of participants who agreed with the four COVID-19 mortality disparities statements. Specifically, 81.6% agreed that older people compared to younger people are more likely to die from COVID-19 and 85.8% agreed that people with chronic health conditions are more likely to die compared to those without such conditions. In contrast, only 51.9% agreed that people in poverty are more likely to die from COVID-19 than wealthier people and 51.5% agreed that Black people are more likely to die from COVID-19 than white people.
Table 1.
Agreement with Disparities in Mortality from COVID-19, April 23–27, 2020 (N = 1007).
| Distribution of agreement |
||||||
|---|---|---|---|---|---|---|
| Type of group disparity | Overall agreement | Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly agree |
| Older people compared to younger people | 81.6% | 1.3% | 5.4% | 11.8% | 40.0% | 41.6% |
| People with chronic health conditions compared to people without such conditions. | 85.8% | 1.7% | 1.5% | 11.0% | 37.4% | 48.5% |
| Poorer people compared to wealthier people. | 51.9% | 9.2% | 15.2% | 23.7% | 32.7% | 19.2% |
| Black/African American people compared to white people. | 51.5% | 8.5% | 12.0% | 28.1% | 32.0% | 19.5% |
Note. Each item asked respondents how much they agreed that: “[Group A] are more likely to die of complications from COVID-19 (coronavirus) than [Group B]”. Overall agreement was calculated by summing “agree” and “strongly agree”.
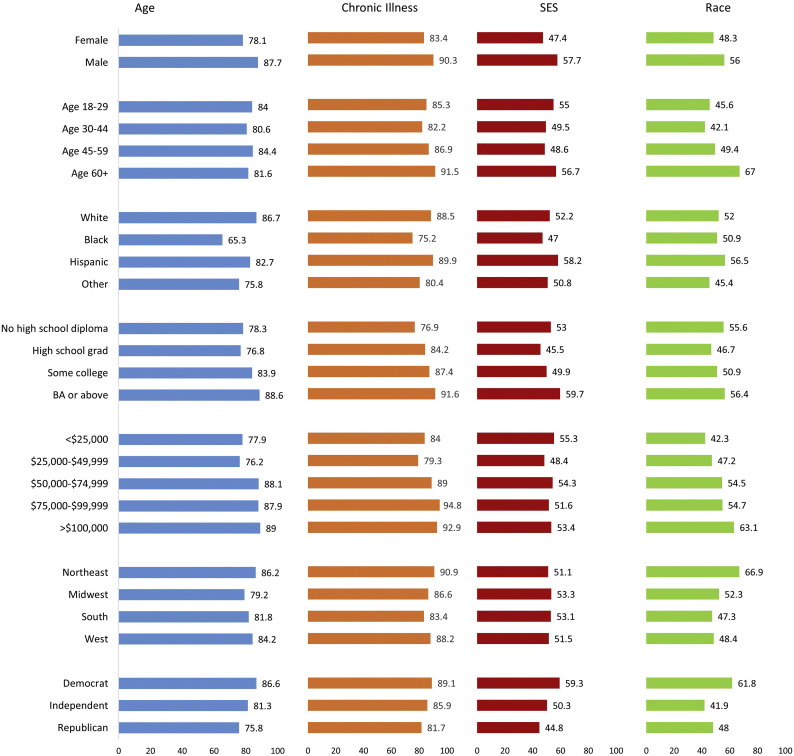
Table 2 illuminates variation in participants' perceptions of disparities in COVID-19 mortality. Across all four models, men had significantly higher odds of agreeing that there are group disparities than did women. Higher household income was also related to higher odds of agreeing with disparities by age, chronic disease, and race—but, interestingly, income was not related to agreement that there are socioeconomic disparities in COVID-19. People with higher income were no more likely than those with lower income to agree that there are disparities in mortality for people in poverty compared to wealthier people (see Fig. 1 for an illustration of patterns across disparity type).
Table 2.
Factors predicting agreement with group disparities in COVID-19 mortality, April 23–27, 2020.
| Older people (N = 978) |
Chronic health conditions (N = 983) |
Lower SES (N = 978) |
Black/African American (N = 977) |
|
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Gender | p = 0.004 | p = 0.019 | p = 0.016 | p = 0.036 |
| Female | 1.00 | 1.00 | 1.00 | 1.00 |
| Male | 2.20 (1.28, 3.78) | 2.08 (1.13, 3.84) | 1.67 (1.10, 2.53) | 1.54 (1.03, 2.30) |
| Age (years) | p = 0.768 | p = 0.107 | p = 0.293 | p < 0.0001 |
| 18–29 | 1.00 | 1.00 | 1.00 | 1.00 |
| 30–44 | 0.76 (0.34, 1.68) | 0.75 (0.33, 1.72) | 0.76 (0.38, 1.52) | 0.83 (0.42, 1.61) |
| 45–59 | 1.04 (0.44, 2.43) | 1.17 (0.49, 2.81) | 0.73 (0.37, 1.42) | 1.23 (0.61, 2.48) |
| 60+ | 0.82 (0.36, 1.88) | 2.06 (0.81, 5.23) | 1.09 (0.56, 2.11) | 3.25 (1.65, 6.41) |
| Race/ethnicity | p = 0.0005 | p = 0.005 | p = 0.579 | p = 0.541 |
| White, non-Hispanic | 1.00 | 1.00 | 1.00 | 1.00 |
| Black, non-Hispanic | 0.24 (0.12, 0.47) | 0.31 (0.14, 0.68) | 0.77 (0.39, 1.53) | 0.94 (0.50, 1.77) |
| Hispanic | 0.71 (0.35, 1.44) | 1.19 (0.47, 3.00) | 1.35 (0.72, 2.52) | 1.29 (0.67, 2.50) |
| Other race / multiracial | 0.43 (0.19, 1.00) | 0.46 (0.18, 1.22) | 0.93 (0.46, 1.91) | 0.69 (0.35, 1.35) |
| Education | p = 0.045 | p = 0.041 | p = 0.032 | p = 0.208 |
| No high school diploma | 1.00 | 1.00 | 1.00 | 1.00 |
| High school grad/equiv. | 0.90 (0.35, 2.32) | 1.80 (0.64, 5.04) | 0.70 (0.29, 1.67) | 0.61 (0.24, 1.55) |
| Some college | 1.52 (0.61, 3.81) | 2.48 (0.95, 6.49) | 0.86 (0.37, 1.98) | 0.77 (0.30, 1.94) |
| BA or above | 2.38 (0.89, 6.34) | 4.16 (1.46, 11.87) | 1.39 (0.60, 3.20) | 1.04 (0.42, 2.60) |
| Household income | p = 0.011 | p = 0.003 | p = 0.787 | p = 0.008 |
| <$25,000 | 1.00 | 1.00 | 1.00 | 1.00 |
| $25,000–$49,999 | 0.89 (0.47, 1.70) | 0.68 (0.32, 1.45) | 0.71 (0.39, 1.29) | 1.32 (0.76, 2.29) |
| $50,000–$74,999 | 2.30 (1.11, 4.75) | 1.64 (0.71, 3.78) | 0.95 (0.50, 1.81) | 1.97 (1.02, 3.78) |
| $75,000–$99,999 | 2.24 (0.91, 5.53) | 4.09 (1.2, 13.91) | 0.83 (0.42, 1.65) | 1.98 (0.96, 4.10) |
| $100,000+ | 2.53 (1.04, 6.14) | 2.83 (0.91, 8.77) | 0.91 (0.49, 1.69) | 3.16 (1.66, 6.03) |
| Region of United States | p = 0.501 | p = 0.359 | p = 0.978 | p = 0.015 |
| Northeast | 1.00 | 1.00 | 1.00 | 1.00 |
| Midwest | 0.56 (0.23, 1.35) | 0.59 (0.21, 1.71) | 1.12 (0.62, 2.01) | 0.44 (0.23, 0.84) |
| South | 0.68 (0.27, 1.73) | 0.44 (0.16, 1.20) | 1.10 (0.60, 2.03) | 0.33 (0.17, 0.66) |
| West | 0.83 (0.32, 2.20) | 0.70 (0.23, 2.12) | 1.02 (0.53, 1.96) | 0.35 (0.17, 0.73) |
| Political affiliation | p = 0.068 | p = 0.222 | p = 0.032 | p < 0.0001 |
| Democrat | 2.40 (1.09, 5.27) | 2.14 (0.88, 5.21) | 2.01 (1.16, 3.47) | 2.11 (1.20, 3.70) |
| Independent | 1.50 (0.69, 3.25) | 1.49 (0.62, 3.60) | 1.30 (0.75, 2.26) | 0.72 (0.43, 1.18) |
| Republican | 1.00 | 1.00 | 1.00 | 1.00 |
| Respondent OR someone personally known has COVID-19 | p = 0.196 | p = 0.180 | p = 0.046 | p = 0.220 |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 1.45 (0.83, 2.55) | 1.56 (0.82, 2.98) | 1.49 (1.01, 2.19) | 1.28 (0.86, 1.91) |
| County-level COVID-19 mortality rate | p = 0.861 | p = 0.480 | p = 0.076 | p = 0.520 |
| <1 per 100,000 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1–3 per 100,000 | 0.97 (0.44, 2.17) | 1.11 (0.44, 2.79) | 1.99 (1.14, 3.45) | 1.14 (0.64, 2.01) |
| 3–9 per 100,000 | 0.83 (0.41, 1.67) | 1.03 (0.48, 2.22) | 1.74 (1.04, 2.91) | 1.06 (0.61, 1.83) |
| >9 per 100,000 | 0.78 (0.38, 1.61) | 0.65 (0.28, 1.50) | 1.34 (0.76, 2.37) | 0.72 (0.38, 1.36) |
| COVID-19 information source | ||||
| Fox news | p = 0.732 | p = 0.873 | p = 0.021 | p = 0.022 |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 1.11 (0.60, 2.06) | 0.94 (0.45, 1.96) | 0.55 (0.33, 0.91) | 0.58 (0.37, 0.92) |
| CNN or MSNBC | p = 0.531 | p = 0.817 | p = 0.004 | p = 0.0002 |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 1.20 (0.68, 2.09) | 1.08 (0.58, 2.02) | 1.79 (1.2, 2.66) | 2.13 (1.44, 3.16) |
| National news | p = 0.285 | p = 0.024 | p = 0.027 | p < 0.0001 |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 0.71 (0.38, 1.33) | 0.44 (0.22, 0.90) | 1.67 (1.06, 2.61) | 2.59 (1.64, 4.11) |
| Local news | p = 0.246 | p = 0.195 | p = 0.034 | p = 0.047 |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 1.32 (0.83, 2.10) | 1.46 (0.83, 2.57) | 1.51 (1.03, 2.22) | 1.48 (1.01, 2.18) |
| State governors – GOP | p = 0.096 | p = 0.005 | p = 0.357 | p = 0.964 |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 1.87 (0.89, 3.89) | 3.54 (1.46, 8.59) | 0.77 (0.45, 1.34) | 0.99 (0.56, 1.75) |
| State governors – Dem | p = 0.047 | p < 0.0001 | p = 0.369 | p = 0.929 |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 1.91 (1.01, 3.60) | 4.70 (2.24, 9.86) | 1.25 (0.77, 2.05) | 1.02 (0.63, 1.66) |
| White House briefings | p = 0.691 | p = 0.943 | p = 0.071 | p = 0.292 |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 1.15 (0.59, 2.23) | 0.97 (0.44, 2.13) | 0.68 (0.44, 1.03) | 0.79 (0.52, 1.22) |
| Direct health | p = 0.876 | p = 0.765 | p = 0.631 | p = 0.229 |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 1.04 (0.62, 1.74) | 1.10 (0.59, 2.06) | 1.11 (0.73, 1.67) | 1.29 (0.85, 1.96) |
| Other people | p = 0.737 | p = 0.967 | p = 0.277 | p = 0.052 |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 1.11 (0.61, 2.01) | 1.02 (0.51, 2.00) | 0.78 (0.49, 1.23) | 0.64 (0.40, 1.00) |
Note. The p-values listed for each category of independent variable is the omnibus test for that characteristic. OR refers to Odds Ratio.
Fig. 1.
Predicted Probability of Agreeing with COVID-19 Disparities, by Personal Characteristics. Note: Figure shows the predicted probability of agreeing with each type of group disparity in COVID-19 mortality for individual demographic characteristics and partisanship, adjusting for all other characteristics in the model simultaneously (see Table 2). Personal experience with COVID-19 and county-level COVID-19 mortality not shown.
A gradient in recognition of disparities by age was apparent for both chronic health condition disparities and racial disparities, but only for the latter did people older than 65 have significantly higher odds of perceiving disparities. The relationship between race and perception of disparity also varied by disparity type: Black participants had significantly lower odds than white participants of agreeing that there were disparities in COVID-19 mortality by age and by chronic health conditions. However, there were no such racial differences in perceptions of the two social group disparities. Higher educational attainment was associated with significantly higher odds of recognizing age-related, chronic health condition, and socioeconomic disparities, but not racial disparities in COVID-19 mortality (Table 2).
Table 2 highlights distinct differences in perceptions of disparities by partisanship. Democrats had higher odds of agreeing with age (OR: 2.40, 95% CI 1.09–5.27), socioeconomic (OR: 2.01, 95% CI 1.16–3.47) and racial health disparities (OR: 2.11, 95% CI: 1.20, 3.70) compared to Republicans. These divergent patterns are evident in Fig. 1. Adjusting for all other characteristics in the model, 44.8% (95% CI 36.5–53.0) of Republicans agreed that there were socioeconomic disparities compared to 59.3% (95% CI 53.1–65.5) of Democrats and 50.3% (95% CI 43.1–57.6) of Independents. The partisan gap was similar for racial disparities, with 48.0% (95% CI 41.1–55.0) of Republicans agreeing that there are racial disparities compared to 61.8% (95% CI 55.6–68.1) of Democrats and 41.9% (95% CI 36.5–47.3) of Independents.
The region in which participants lived was unrelated to their perceptions of age-related, chronic illness, or socioeconomic disparities. However, people living in the Midwest, South, and West all had significantly lower odds of agreeing that there are racial disparities in COVID-19 mortality compared to those living in the Northeast. While individuals with personal COVID-19 experience had higher odds of agreeing with all four disparities, the relationship was only statistically significant for socioeconomic status. The county-level COVID-19 mortality rate was not related to perceptions of disparities.
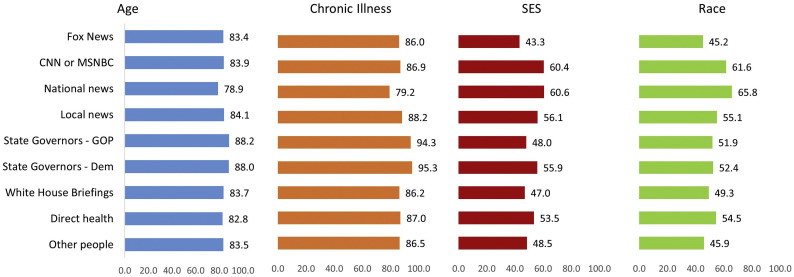
The sources of information participants reported were associated with their perceptions of disparities (Table 2 and Fig. 2 ). For instance, while there was no relationship between viewing Fox News and perceiving age-related or chronic health condition disparities, people who reported viewing Fox News had significantly lower odds of agreeing with socioeconomic (OR: 0.55, 95% CI 0.33–0.91) and racial disparities (OR: 0.58, 95% CI 0.37–0.92). In contrast, those who reported watching CNN or MSNBC, watching or reading national news, and watching or reading local news all had significantly higher odds of agreeing with socioeconomic and racial disparities (see Fig. 2). These differences were not only statistically significant but also substantively meaningful: adjusting for all other characteristics, 45.2% (95% CI 38.5–51.9) of participants who reported watching Fox News agreed that there are racial disparities in COVID-19, while 65.8% (95% CI 58.6–73.0) of participants who reported watching or reading national news sources agreed that there are racial disparities. Participants who noted they were attuned to their state governors' briefings (regardless of the governors' political party) had higher odds of agreeing that there are disparities in COVID-19 mortality for older people and those with chronic health conditions, but were no more likely to agree with socioeconomic or racial disparities. Finally, there were no statistically significant differences in perceptions of disparities for those reporting information from health sources (e.g., CDC, WHO) nor from White House briefings. However, participants who noted that other people were a source of information (OR: 0.64, 95% CI 0.40–1.00) had lower odds of agreeing that there are racial disparities in COVID-19 mortality.
Fig. 2.
Predicted Probability of Agreeing with COVID-19 Disparities, by COVID-19 Information Sources. Note: Figure shows the predicted probability of agreeing with each type of group disparity in COVID-19 mortality, adjusting for all other characteristics in the model simultaneously (see Table 2).
3. Discussion
This study reveals wide gaps in U.S. public understanding about disparities in COVID-19 mortality in late April 2020. While the vast majority of participants in a nationally-representative survey recognized that older people and people with chronic health conditions are more likely to die from COVID-19 than younger people and those without other conditions, public recognition of social group disparities was much lower. Only half of participants recognized that people of lower SES (compared to wealthier people) or Black people (compared to white people) are more likely to die from COVID-19. These findings are consistent with the gaps in public awareness of health disparities that past researchers have observed (Benz et al., 2011; Booske et al., 2011; Bye et al., 2016). They are also consistent with more recent evidence. In a survey conducted in mid-June 2020, researchers at KFF (Kaiser Family Foundation) found that only 50% of Americans recognized that Black Americans are more likely to “get sick or die from coronavirus” compared to white Americans—as compared to the 51.2% who recognized this disparity in our study (Hamel et al., 2020). Thus, even after heightened media attention to racial health disparities in COVID-19 as spurred by national public outrage and attention to the treatment of Black Americans in early June 2020, level of public recognition of COVID-19 racial disparities remained essentially at the same level we observed in our sample in late April.
Our multivariable findings further illuminate the unequal distribution of recognition of COVID-19 health disparities among the U.S. population. Notably, political partisanship—as others have found in previous surveys on health disparities (Booske et al., 2011; Gollust and Cappella, 2014)—corresponds with recognition of disparities, particularly racial and socioeconomic group disparities. KFF researchers also identified partisan differences in their June survey: 69% of Democrats but only 34% of Republicans noted that Black Americans were more likely than White Americans to get sick or die from coronavirus (Hamel et al., 2020).
While our study was not designed to identify the causal mechanisms underlying this gap, our results suggest a few explanations. First, information sources likely play a role, as we found significant associations between participants' identification of their media sources and their recognition of disparities. Among the media sources we queried, participants who noted following Fox News were less likely to recognize socioeconomic and racial disparities, while participants who attended to other types of cable, national, and local news media were more likely to recognize these disparities—all adjusting for their own partisanship and other demographic characteristics like education. The fact that these media sources were associated with disparities perceptions above and beyond other individual characteristics suggests that the media environment varies with respect to content about COVID-19 (Jamieson and Albarracin, 2020). Differential media selection by partisanship (Iyengar and Hahn, 2009) would support the idea that different media “diets” contribute to a different understanding of the experience of COVID-19. Second, the partisan gap may also be explained by psychological processes underlying the recognition and reporting of disparities. Even if study participants had equal access to information about disparities, there may be differences in their willingness to accept, incorporate, and acknowledge those disparities, a process known as motivated reasoning (Strickland et al., 2011). The fact that the KFF poll also identified political differences with different question wording (asking if Black people were more or less affected, as opposed to asking about “agreement” as we did) suggests that differential perceptions by partisanship are evidence of a deeper phenomenon. Indeed, longstanding social science research has documented political and ideological differences in recognition of various types of inequalities in the U.S. (Kluegel, 1990; Skitka et al., 2002).
Our findings also point toward regional differences. Survey respondents in the Northeastern U.S. perceived racial disparities more than in other regions; this was not only a product of local proximity to higher mortality rates, as this regional difference held even after adjusting for the localized mortality rates in a participant's county. As the virus has spread rapidly across the U.S. since April, it is important to track how geographic variation in understanding of COVID-19 has changed.
Finally, our findings raise some intriguing individual-level demographic associations with disparity perceptions. Adjusting for all other characteristics, men were more likely to report agreeing with disparities. That has not, to our knowledge, been identified in other research. We also found gradients in recognition of disparities by income and education, which is consistent with other work (Booske et al., 2011; Bye et al., 2016). Curiously, we found no such relationship between income and recognition of income-related disparities, just as there was no relationship between age of respondents and agreeing with age-related disparities—both trends suggestive of biased processing of information based on demographic characteristics, or the idea that people prefer information that makes themselves or their group look favorable (Reed and Aspinwall, 1998).
3.1. Limitations
This cross-sectional survey does not allow us to identify causal mechanisms underlying the perceptions we observe. As is true for any point-in-time survey, the context at the time (late April 2020) is relevant, when the national conversation about disparities in COVID-19 was in its infancy relative to how broadly discussed racial disparities in particular became in summer 2020 after nation-wide protests reignited attention to structural racism. Still, the nationally-representative nature of the study is a strength. Future research efforts should continue to ascertain public understanding of disparities in COVID-19 as the pandemic evolves, given that mass public opinion mobilization can be one avenue toward advocacy and policy action to ameliorate these inequities (Burstein, 2003; Farrer et al., 2015; Kingdon, 2003). However, efforts to promote broader public awareness of health disparities in COVID-19 should be mindful of potential unintended consequences or backlash, particularly when communicating about racial disparities (Niederdeppe et al., 2013). Specifically, when disparities statistics are communicated without providing sufficient explanation of the structural and systemic causes of these differences, the public may fill in stereotypical explanations (i.e., about lifestyle behaviors of people in poor health, or reductionist and inaccurate biological pathways) or even stigmatize whole communities when COVID-19 racial disparities data are applied to neighborhoods (Chowkwanyun and Reed Jr, 2020).
4. Public health implications
The message that older people and people with chronic health conditions are more at risk of dying from COVID-19 had largely disseminated to the general public by late April 2020, suggesting successful public health education efforts. However, information about disparities by income and race was less well disseminated or accepted, with only half of the public recognizing these social disparities by income and race. Studies have consistently shown that while the public health community broadly recognizes health disparities—and increasingly recognizes structural racism as a cause of racial disparities in particular (Williams et al., 2019)—the public is still not widely aware of these phenomena. Evidence-based communication efforts are needed to build public will to address racial disparities in general and in COVID-19 in particular, while avoiding negative consequences. It is also important to acknowledge the partisan barriers (individual beliefs as well as media outlets that contribute to a polarized public) that may stand in the way of shared recognition of disparities.
CRediT authorship contribution statement
Sarah E. Gollust: Conceptualization, Methodology, Writing - original draft, Writing - review & editing. Rachel I. Vogel: Conceptualization, Formal analysis, Data curation, Methodology, Writing - review & editing. Alexander Rothman: Conceptualization, Writing - review & editing. Marco Yzer: Conceptualization, Writing - review & editing. Erika Franklin Fowler: Conceptualization, Writing - review & editing. Rebekah H. Nagler: Funding acquisition, Conceptualization, Methodology, Writing - review & editing, Supervision.
Acknowledgments
This work was supported by a COVID-19 Rapid Response Grant from the Office of the Vice President for Research at the University of Minnesota. Additional support was provided by a grant from the National Cancer Institute (1R21CA218054-02). This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank Mike Schommer and Kate Awsumb from the Minnesota Department of Health for their support of this project.
Appendix A
Table A1.
Sample characteristics (N = 1007).
| Variable | Weighted % |
|---|---|
| Gender | |
| Male | 48.6 |
| Female | 51.4 |
| Age (years) | |
| 18–29 | 18.1 |
| 30–44 | 26.7 |
| 45–59 | 24.5 |
| 60+ | 30.7 |
| Race/ethnicity | |
| White, non-Hispanic | 62.6 |
| Black, non-Hispanic | 12.0 |
| Hispanic | 16.5 |
| Other | 8.9 |
| Education | |
| Less than high school | 8.8 |
| High school graduate or equivalent | 27.5 |
| Some college | 28.5 |
| Bachelor's degree or above | 35.3 |
| Household income | |
| <$25,000 | 20.5 |
| $25,000–$49,999 | 25.6 |
| $50,000–$74,999 | 18.5 |
| $75,000–$99,999 | 12.8 |
| $100,000+ | 22.5 |
| Region of United States | |
| Northeast | 17.6 |
| Midwest | 20.7 |
| South | 37.8 |
| West | 23.9 |
| Political affiliation | |
| Democrat | 42.8 |
| Independent | 27.4 |
| Republican | 29.8 |
| Respondent OR someone personally known has COVID-19 | |
| No | 64.8 |
| Yes | 35.2 |
| County-level COVID-19 mortality rate | |
| <1 per 100,000 | 23.9 |
| 1–3 per 100,000 | 25.3 |
| 3–9 per 100,000 | 26.4 |
| >9 per 100,000 | 24.4 |
| COVID-19 information source | |
| Fox news | |
| No | 73.4 |
| Yes | 26.6 |
| CNN or MSNBC | |
| No | 65.7 |
| Yes | 34.3 |
| National news | |
| No | 75.5 |
| Yes | 24.5 |
| Local news | |
| No | 44.4 |
| Yes | 55.6 |
| State governors – GOP | |
| No | 85.7 |
| Yes | 14.3 |
| State governors – Dem | |
| No | 74.5 |
| Yes | 25.5 |
| White house briefings | |
| No | 67.5 |
| Yes | 32.5 |
| Direct health | |
| No | 53.4 |
| Yes | 46.6 |
| Other people | |
| No | 76.7 |
| Yes | 23.3 |
Appendix B
Battery of information sources participants could select:
-
1.
Fox News or its website
-
2.
MSNBC or its website
-
3.
CNN or its website
-
4.
NPR or its website
-
5.
The New York Times or its website
-
6.
The Washington Post or its website
-
7.
Local television news in your area or their websites
-
8.
Local newspaper in your area or its website
-
9.
National network news (ABC World News Tonight, CBS Evening News, or NBC Nightly News) or their websites
-
10.
White House press briefings
-
11.
State governor briefings
-
12.
Centers for Disease Control (CDC)
-
13.
World Health Organization (WHO)
-
14.
State or local health department
-
15.
Other people (such as family, friends, or co-workers)
-
16.
Another source (specify).
Participants could select all that apply (participants selected 4.2 sources on average, SD = 2.7); the order in which sources appeared was randomized.
References
- Alsan M., Stantcheva S., Yang D., Cutler D. Disparities in coronavirus 2019 reported incidence, knowledge, and behavior among US adults. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.12403. e2012403-e03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey Z., Barber S., Robinson W., Slaughter-Acey J., Ford C., Sealy-Jefferson S. 2020. Racism in the Time of COVID-19.https://iaphs.org/racism-in-the-time-of-covid-19/ Available at: [Google Scholar]
- Benz J.K., Espinosa O., Welsh V., Fontes A. Awareness of racial and ethnic health disparities has improved only modestly over a decade. Health Aff. 2011;30:1860–1867. doi: 10.1377/hlthaff.2010.0702. [DOI] [PubMed] [Google Scholar]
- Booske B.C., Robert S.A., Rohan A.M. Awareness of racial and socioeconomic health disparities in the United States: the national opinion survey on health and health disparities, 2008–2009. Prev. Chronic Dis. 2011;8:A73. [PMC free article] [PubMed] [Google Scholar]
- Bouie J. Why coronavirus is killing African-Americans more than others. New York Times. 2020 https://www.nytimes.com/2020/04/14/opinion/sunday/coronavirus-racism-african-americans.html April 14, 2020. [Google Scholar]
- Burstein P. The impact of public opinion on public policy: a review and an agenda. Polit. Res. Q. 2003;56:29–40. [Google Scholar]
- Bye L., Ghirardelli A., Fontes A. Promoting health equity and population health: how Americans’ views differ. Health Aff. 2016;35:1982–1990. doi: 10.1377/hlthaff.2016.0730. [DOI] [PubMed] [Google Scholar]
- Carman Katherine, Chandra Anita, Weilant Sarah, Miller Carolyn, Tait Margaret. 2018 National Survey of Health Attitudes: Description and Top-Line Summary Data. RAND Corporation; Santa Monica, CA: 2019. https://www.rand.org/pubs/research_reports/RR2876.html [Google Scholar]
- CDC Geographic differences in COVID-19 cases, deaths, and incidence — United States, February 12–April 7, 2020. MMWR Morb. Mortal. Wkly Rep. 2020;69:465–471. doi: 10.15585/mmwr.mm6915e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC People at Increased Risk. 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/index.html Available at:
- Chowkwanyun M., Reed A.L., Jr. Racial health disparities and Covid-19—caution and context. N. Engl. J. Med. 2020;383:201–203. doi: 10.1056/NEJMp2012910. [DOI] [PubMed] [Google Scholar]
- Farrer L., Marinetti C., Cavaco Y.K., Costongs C. Advocacy for health equity: a synthesis review. Milbank Q. 2015;93:392–437. doi: 10.1111/1468-0009.12112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gollust S.E., Cappella J.N. Understanding public resistance to messages about health disparities. J. Health Commun. 2014;19:493–510. doi: 10.1080/10810730.2013.821561. [DOI] [PubMed] [Google Scholar]
- Gollust S.E., Lantz P.M. Communicating population health: print news media coverage of type 2 diabetes. Soc. Sci. Med. 2009;69:1091–1098. doi: 10.1016/j.socscimed.2009.07.009. [DOI] [PubMed] [Google Scholar]
- Gollust S.E., Lantz P.M., Ubel P.A. The polarizing effect of news media messages about the social determinants of health. Am. J. Public Health. 2009;99:2160–2167. doi: 10.2105/AJPH.2009.161414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gollust S.E., Fowler E.F., Niederdeppe J. Television news coverage of public health issues and implications for public health policy and practice. Annu. Rev. Public Health. 2019;40:167–185. doi: 10.1146/annurev-publhealth-040218-044017. [DOI] [PubMed] [Google Scholar]
- Green D.P., Schickler E. Multiple-measure assessment of party identification. Public Opin. Q. 1993;57:503–535. [Google Scholar]
- Hamel L., Kearney A., Kirzinger A., Lopes L., Munana C., Brodie M. KFF Health Tracking Poll - June 2020. 2020. https://www.kff.org/racial-equity-and-health-policy/report/kff-health-tracking-poll-june-2020/ Available at:
- Pew . 2019. For local news, Americans embrace digital but still want strong community connection.https://www.journalism.org/2019/03/26/for-local-news-americans-embrace-digital-but-still-want-strong-community-connection/ Available at: [Google Scholar]
- Iyengar S., Hahn K.S. Red media, blue media: evidence of ideological selectivity in media use. J. Commun. 2009;59:19–39. [Google Scholar]
- Jamieson K.H., Albarracin D. Harvard Kennedy School Misinformation Review. 2020. The relation between media consumption and misinformation at the outset of the SARS-CoV-2 pandemic in the US.https://misinforeview.hks.harvard.edu/article/the-relation-between-media-consumption-and-misinformation-at-the-outset-of-the-sars-cov-2-pandemic-in-the-us/ Available at: [Google Scholar]
- Kingdon J. 2nd ed. Longman; New York: 2003. Agendas, Alternatives, and Public Policies. [Google Scholar]
- Kluegel J.R. Trends in whites’ explanations of the black-white gap in socioeconomic status, 1977–1989. Am. Sociol. Rev. 1990;55:512–525. [Google Scholar]
- McGinty E.E., Presskreischer R., Han H., Barry C.L. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. 2020;324(1):93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motta M., Stecula D., Farhart C. How right-leaning media coverage of COVID-19 facilitated the spread of misinformation in the early stages of the pandemic. Can. J. Polit. Sci. 2020 doi: 10.1017/S0008423920000396. [DOI] [Google Scholar]
- Niederdeppe J., Bigman C.A., Gonzales A.L., Gollust S.E. Communication about health disparities in the mass media. J. Commun. 2013;63:8–30. [Google Scholar]
- Pinsker J. 2020. The Pandemic Will Cleave America in Two, The Atlantic. (April 10) [Google Scholar]
- Purtle J., Henson R.M., Carroll-Scott A., Kolker J., Joshi R., Diez Roux A.V. US mayors’ and health commissioners’ opinions about health disparities in their cities. Am. J. Public Health. 2018;108:634–641. doi: 10.2105/AJPH.2017.304298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed M.B., Aspinwall L.G. Self-affirmation reduces biased processing of health-risk information. Motiv. Emot. 1998;22:99–132. [Google Scholar]
- Skitka L.J., Mullen E., Griffin T., Hutchinson S., Chamberlin B. Dispositions, scripts, or motivated correction? Understanding ideological differences in explanations for social problems. J. Pers. Soc. Psychol. 2002;83:470–487. doi: 10.1037/0022-3514.83.2.470. [DOI] [PubMed] [Google Scholar]
- Stone E.M., Barry C.L., Crifasi C.K., Webster D.W., Vernick J.S., McGinty E.E. Support for gun policies among young adults in the US, 2017–2019. Prev. Med. 2020;135 doi: 10.1016/j.ypmed.2020.106094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strickland A.A., Taber C.S., Lodge M. Motivated reasoning and public opinion. J. Health Polit. Policy Law. 2011;36:935–944. doi: 10.1215/03616878-1460524. [DOI] [PubMed] [Google Scholar]
- Szabo L., Recht H. The Other COVID Risks: How Race, Income, Zip Code Influence Who Lives Or Dies, Kaiser Health News. 2020. https://khn.org/news/covid-south-other-risk-factors-how-race-income-zip-code-influence-who-lives-or-dies/ Available at:
- Williams D.R., Cooper L.A. COVID-19 and health equity—a new kind of “herd immunity”. JAMA. 2020;323(24):2478–2480. doi: 10.1001/jama.2020.8051. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Purdie-Vaughns V. Needed interventions to reduce racial/ethnic disparities in health. J. Health Polit. Policy Law. 2016;41(4):627–651. doi: 10.1215/03616878-3620857. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Lawrence J.A., Davis B.A. Racism and health: evidence and needed research. Annu. Rev. Public Health. 2019;40:105–125. doi: 10.1146/annurev-publhealth-040218-043750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson E.J., Walker A.J., Bhaskaran K., Bacon S., Bates C., Morton C.E., Curtis H.J., Mehrkar A., Evans D. OpenSAFELY: factors associated with COVID-19 death in 17 million patients. Nature. 2020;584:430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]