Abstract
Coronavirus disease 2019 (COVID-19) has affected patients across all age groups, with a wide range of illness severity from asymptomatic carriers to severe multi-organ dysfunction and death. Although early reports have shown that younger age groups experience less severe disease than older adults, our understanding of this phenomenon is in continuous evolution. Recently, a severe multisystem inflammatory syndrome in children (MIS-C), with active or recent COVID-19 infection, has been increasingly reported. Children with MIS-C may demonstrate signs and symptoms of Kawasaki disease, but also have some distinct differences. These children have more frequent and severe gastrointestinal symptoms and are more likely to present with a shock-like presentation. Moreover, they often present with cardiovascular involvement including myocardial dysfunction, valvulitis, and coronary artery dilation or aneurysms. Here, we present a review of the literature and summary of our current understanding of cardiovascular involvement in children with COVID-19 or MIS-C and identifying the role of a pediatric cardiologist in caring for these patients.
Keywords: COVID-19, Pediatric, Cardiovascular, MIS-C
Introduction
A global pandemic was declared by the World Health Organization (WHO) on March 11, 2020 when the coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spiraled into a global health crisis [1]. COVID-19 has created unprecedented challenges from public health, economic, medical, and research standpoints. It has been reported across all age groups and leading to a wide spectrum of illness severity from asymptomatic carriers to severe multi-organ dysfunction and death. Early observational studies have reported less severe presentation among children and young adults as compared to the older adults [2–7]. Rarely, children with active or recent infection with SARS-CoV-2 can also present with a severe inflammatory syndrome and features similar to those encountered in Kawasaki disease [8–11]. In Bergamo province of Italy, a 30-fold increase in the incidence of Kawasaki-like disease in comparison to the last five years has been described [8]. As of May 2020, the New York State Department of Health has also identified over 200 children with similar presentations [12]. This novel presentation has been termed as multisystem inflammatory syndrome in children (MIS-C) [12, 13], or pediatric multisystem inflammatory syndrome (PMIS) [14] or pediatric inflammatory multisystem syndrome (PIMS) [15]—these terms are used interchangeably in this article.
With an evolving understanding of this disease and rapidly expanding literature, keeping up with the clinically relevant information is important to our patients and us as clinicians. Here we present a summary of our current understanding of the role of a pediatric cardiologist in caring for children and adolescents with COVID-19 and MIS-C.
Case Definitions
COVID-19
The WHO has proposed case definitions for COVID-19 that are regularly updated based on new evidence (Table 1) [1, 16]. Generally cases are classified as suspect, probable or confirmed based on the presence of acute respiratory symptoms, exposure and travel history in addition to confirmatory COVID-19 testing.
Table 1.
Case definitions of COVID-19 and MIS-C
| WHO case definitions of COVID-19 | |
| Suspect case |
Acute respiratory illness AND a history of travel or residence in a location with community transmission or contact with a confirmed or probable case of COVID-19 in the last 14 days prior to symptoms OR exposure to confirmed or probable COVID-19 case in 14 days prior to symptoms onset OR Severe acute respiratory illness requiring hospitalization in the absence of alternative diagnosis |
| Probable case | A suspect case with inconclusive COVID-19 testing or if testing could not be performed for any reason |
| Confirmed case | Patient with laboratory confirmation of COVID-19 irrespective of clinical signs or symptoms |
| Illness severity |
Mild/moderate No new or increased supplemental oxygen requirement Severe New or increased supplemental oxygen requirement without needing new or increased non-invasive/invasive mechanical ventilation Critical New or increased non-invasive/invasive mechanical ventilation requirement OR presence of sepsis or multi-organ failure or rapidly worsening clinical trajectory |
| Case definitions of MIS-C | |
| CDC definition |
Age < 21 years presenting with fever (38 °C for at least 24 h), laboratory evidence of inflammation and evidence of clinically severe illness requiring hospitalization with multisystem (> 2) organ involvement (cardiac, renal, respiratory, hematologic, gastrointestinal, dermatologic or neurological) with no alternative plausible diagnoses AND Positive for current or recent SARS-CoV-2 infection (RT-PCR, serology or antigen test) or COVID-19 exposure within 4 weeks prior to symptoms onset |
| WHO definition |
Age 0–19 years with fever > 3 days AND at least two of the following: (i) Rash or bilateral non-purulent conjunctivitis or mucocutaneous inflammation (ii) Hypotension or shock (iii) Features of myocardial dysfunction, pericarditis, valvulitis, or coronary abnormalities (echo findings, elevated troponin/BNP) (iv) Evidence of coagulopathy (prolonged PT or PTT, elevated D-Dimer) (v) Acute gastrointestinal problems (diarrhea, vomiting, or abdominal pain) AND Elevated markers of inflammation (ESR, CRP, Procalcitonin) with no other obvious microbial cause of inflammation AND Evidence of COVID-19 (RT-PCR, antigen test or serology positive), or likely contact with patients with COVID-19 |
COVID-19 coronavirus disease 2019, MIS-C/PMIS multisystem inflammatory syndrome in children/pediatric multisystem inflammatory syndrome, RT-PCR reverse transcription polymerase chain reaction, SARS-CoV-2 severe acute respiratory syndrome coronavirus
MIS-C
For children with MIS-C, two current definitions have been proposed, that may be subject to change as more evidence becomes available (Table 1). The initial case definition for MIS-C was proposed by the Royal College of Paediatrics and Child Health in UK and subsequently accepted by the WHO, Center for Disease Control and Prevention (CDC) and European Center for Disease Prevention and Control [14, 15, 17]. This definition was broad and included children under the age of 21 years presenting with fever, laboratory evidence of inflammation, and evidence of clinically severe illness requiring hospitalization with current or recent history (within 4 weeks) of SARS-CoV-2 infection or exposure. This initial classification was able to identify all the pediatric patients within a critical spectrum of the disease that often required intensive care. Nevertheless, a less severe expression of the disease was also being seen and soon after, the WHO provided a more inclusive definition recognizing additional patients who did not require escalation of care. The age cut off was decreased to 19 years, fever duration of 3 days was introduced in the criteria and a combination of clinical, laboratory and microbiological criteria were also introduced in order to embrace all the patients under the same diagnosis (Table 1) [18].
Differences Between Children and Adults
There are numerous differences between children and adults with regards to disease prevalence, severity and complications of COVID-19 (Table 2). The percentage of children affected by COVID-19 is much lower than adults and they tend to have milder symptoms and significantly lower morbidity and mortality [2–7, 14, 19, 20]. Some of the frequently reported cardiac manifestations of COVID-19 in adults include; myocardial injury, myocardial dysfunction, myocardial infarction, Takotsubo cardiomyopathy, cardiogenic shock, pericardial effusion, arrhythmias, and conduction abnormalities, but these manifestations are quite rare in pediatric patients [21–27]. The cardiac findings encountered to date in the pediatric population include myocarditis, myocardial dysfunction and coronary artery involvement in MIS-C [8, 10, 12, 28–31]. In adults patients, comorbidities such as hypertension, diabetes, and obesity may predispose them to more severe manifestations of the disease [4, 32, 33]. In children, those that have comorbidities including medical complexity (dependent on technological support in association with developmental delay and/or genetic anomalies), obesity and those less than a year of age, seem to be at a risk for more severe disease [3, 34].
Table 2.
Difference between adults and children with COVID-19
| Adults | Children | |
|---|---|---|
| Rates of infection | High | Low |
| Evidence |
Chinese Center for Disease Control and Prevention reported only 2% of patients younger than 20 years of age among 44,672 cases [20] United States Center for Disease Control and Prevention (CDC) reported only 1.7% children less than 18 years of age among 149,082 reported cases [7] |
|
| Severity of illness | High | Low |
| Evidence |
Chinese data: 14% of adult patients classified as ‘severe’ and 5% as ‘critical’ disease [20] Italian data: 25% of adult patients classified as ‘severe’ and 5% as ‘critical’ [6] |
Chinese data: 5% of pediatric patients classified as ‘severe’ and < 1% as ‘critical’ disease [36] Italian data: 2% of pediatric patients classified as ‘severe’ or ‘critical’ disease [5] |
| Complications and mortality | High | Low |
| Evidence |
United States data: Among 2634 adults hospitalized adults in 12 hospitals in New York City, 14% required intensive care and 12% received mechanical ventilation with a case fatality rate of 21% [4] Chinese data: Case fatality 2.3% of overall COVID-19 affected population [20] Italian data: Case fatality of overall COVID-19 affected population 7% [6] |
United States data: Among 46 North American Pediatric ICUs, only 48 children were admitted to intensive care with a case fatality rate of 4.2% [3] Chinese data: 1 death [36] Italian data: No deaths [5] |
| Potential risk factors leading to severe disease | Hypertension, diabetes, and obesity [4] | Infants < 1 years of age, medical complexitya, immune suppression, obesity [3, 5] |
aDefined as dependence on technological support (tracheostomy with or without ventilator dependence) in association with developmental delay and/or genetic anomalies
Clinical History and Physical Examination
COVID-19
A thorough history and physical examination is crucial in the diagnosis and assessment of a suspected COVID-19 patient. A detailed history of comorbid conditions, history of exposure to confirmed or probable cases of COVID-19 and travel history should be obtained. The most commonly reported symptoms in children are fever and cough [5, 34–40]. Some children present with gastrointestinal (GI) symptoms including nausea, vomiting, diarrhea or abdominal pain [34, 41–43]. Some cutaneous manifestations have also been reported in young patients such as ‘pseudo-chilblains’ described as areas of erythema with vesicles or pustules on hands and feet [44, 45]. Children with SARS-CoV-2 infection may also be asymptomatic carriers of the disease [7, 34, 35]. Other reported symptoms in adults include temporary loss of smell (anosmia) or taste (ageusia) sensation, headaches and thromboembolic phenomena [32, 33, 46–48].
MIS-C
In children with COVID-19, the latest concern is development of MIS-C, a Kawasaki-like syndrome with signs of heart failure or shock [8, 10, 12, 17, 49]. In multiple case series, as high as 50–80% of the children with MIS-C developed signs of systemic hypoperfusion or shock, which is contrary to Kawasaki disease where only up to 5% of the cases may require vasopressor support [8–10, 31, 50]. One of the clinical difference between MIS-C and Kawasaki syndrome is a higher incidence of GI symptoms in MIS-C related to SARS-CoV-2 than with classic Kawasaki disease. These GI symptoms include nausea, vomiting, diarrhea, and/or moderate to severe abdominal pain sometimes mimicking acute appendicitis or enteritis [10, 31, 50, 51]. In children with MIS-C, there is multisystem organ involvement including cardiac, renal, hematological, or neurological manifestations [8, 10, 12, 17, 31]. Severe respiratory symptoms are relatively rare in MIS-C [50]. Therefore, children presenting with persistent fever (≥ 38 °C or 100.4°F, ≥ 3 days), gastrointestinal complaints, rash, conjunctivitis, oral/mucosal changes, or cervical lymphadenopathy require assessment for MIS-C. Signs of heart failure such as edema, organomegaly, murmur, gallop or friction rub maybe present. It is essential to pay attention to the vital signs and hydration status of patients. However, MIS-C is still a rare phenomenon and other sources of infection that may cause fever or systemic inflammation should also be considered in differential diagnosis.
Microbiological Diagnosis
There are two categories of tests currently being utilized for the diagnosis of COVID-19 infection, diagnostic tests for identifying active infection and serologic tests to identify past infection. Diagnostic tests include direct detection of SARS-CoV-2 RNA by reverse transcription polymerase chain reaction (RT-PCR) or detection of SARS-CoV-2 antigens by rapid antigen tests [52]. Detection of viral RNA by RT-PCR, from nasopharyngeal swab or other upper respiratory tract specimens, is the most commonly used and reliable test [53]. Although RT-PCR is highly specific for the virus, negative tests should be interpreted with caution as the specificity of the test depends on the type of assay, site and quality of specimen obtained in addition to the timeline of illness at the time of testing [53, 54]. Rapid antigen tests are also available for the diagnosis of active infection but are less commonly used. They are less sensitive than RT-PCR but are highly specific for the virus [55]. Serologic tests detect antibodies (IgM and IgG) to SARS-CoV-2 and are generally suggestive of a past infection. Serologic tests demand careful interpretation based on timeline of infection [53].
Laboratory Abnormalities
Common laboratory findings in hospitalized adult patients with COVID-19 include lymphopenia, neutrophilia, and elevations of serum amino-transaminases, lactate dehydrogenase (LDH), creatine kinase (CK) and other inflammatory markers such as C-reactive protein (CRP), procalcitonin, ferritin and erythrocyte sedimentation rate (ESR) [32, 38, 39]. Elevation of troponin and brain natriuretic peptide (BNP) or N terminal pro BNP (NT-pro-BNP) is associated with admission to the ICU, intubation, and death in adult patients [21, 32, 38, 56–60]. These laboratory abnormalities have also been reported in children, but data are limited due to a relative lack of studies focused on the pediatric population [61, 62]. Children presenting with MIS-C consistently demonstrate these laboratory abnormalities including elevated Troponin and BNP levels [8, 10, 12, 15, 17, 50]. Additionally thrombocytopenia, elevated D-dimer, elevated fibrinogen and hypoalbuminemia may be seen [8–10, 15, 50].
Pathophysiology of Cardiovascular Manifestations
The etiopathogenesis of cardiovascular manifestations in COVID-19 are unclear. Several mechanisms have been proposed including direct myocyte injury from viral infection, myocardial inflammation, myocardial ischemia/infarction, hypoxia induced apoptosis, microvascular disease, and cytokine storm [63]. A direct correlation between CRP and troponin levels has been shown suggesting an additional inflammatory role in the pathogenesis of the clinical manifestations [60]. Downregulation of the myocardial protective enzyme angiotensin converting enzyme 2 (ACE-2) by SARS-CoV-2 has also been proposed as a potential mechanism of injury to the myocardium [64]. The mechanism of coronary artery dilation may be extrapolated from Kawasaki disease and inlammatory vasculopathy [65]. Myocardial dysfunction, coronary artery involvement, and factors like hypoxia, electrolyte abnormalities, QT prolonging medications may predispose these patients to various arrhythmias [66, 67].
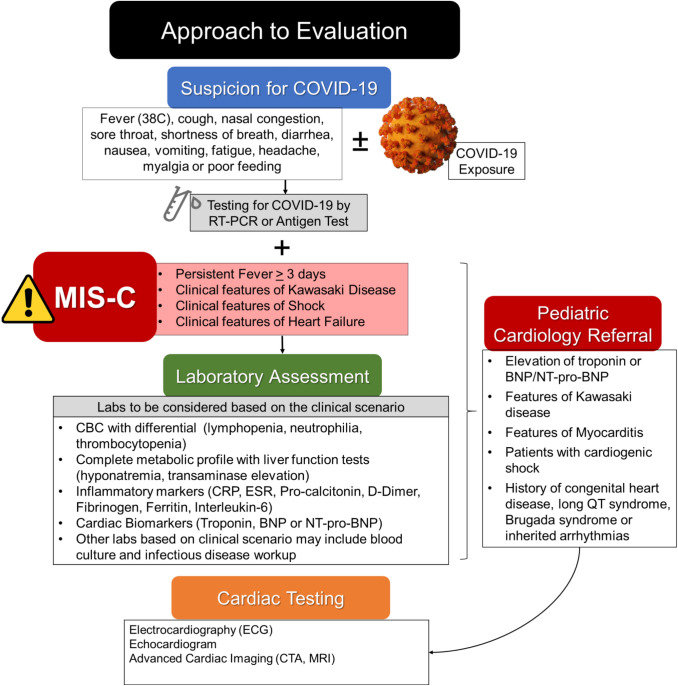
Approach to Evaluation and Indications for Pediatric Cardiology Referral
A general approach towards the evaluation of COVID-19 and MIS-C, as guided by the most recent recommendation by the CDC and American Academy of Pediatrics (AAP), is shown in Fig. 1. [14, 17, 68, 69] Pediatric cardiology may be consulted for patients with COVID-19 with a concern for cardiac involvement or those with MIS-C (Fig. 3). Presence of chest pain, palpitations, persistent tachycardia, tachypnea, or new murmurs should prompt further evaluation by laboratory testing, electrocardiogram (ECG) or echocardiogram. Laboratory evaluation in patients with significant cardiac symptoms should also include measurement of biomarkers such as troponin or BNP/NT-pro-BNP. An ECG may be considered in patients with concerning cardiac symptoms, elevated cardiac biomarkers, or prior to initiation of any therapy that could prolong the QT interval. Those with elevated troponin and BNP/NT-pro-BNP may also benefit from an echocardiogram Patients with cardiogenic and/or distributive shock in the intensive care should prompt a pediatric cardiology consultation.
Fig. 1.
Approach in children with COVID-19 and MIS-C with red flags for pediatric cardiology referral
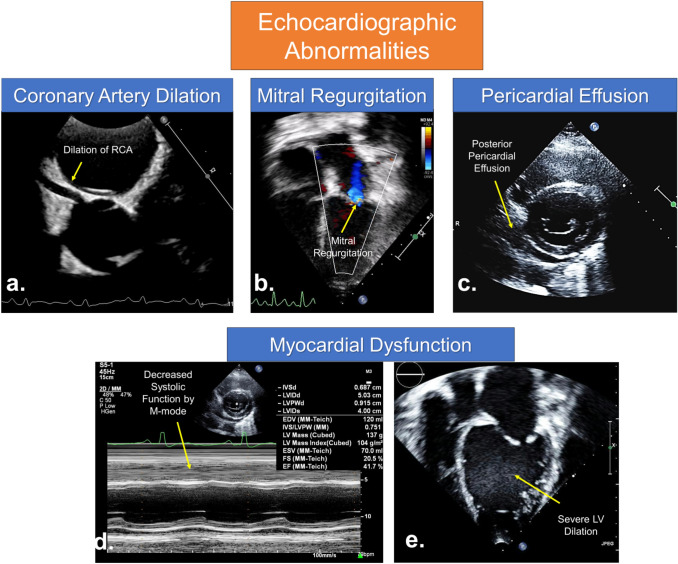
Fig. 3.
Echocardiographic abnormalities in children with COVID-19 and MIS-C. a Parasternal short axis view at the level of aortic valve demonstrating diffuse dilation of right coronary artery (RCA) and coronary artery walls are echogenic. b Apical 4 chamber view demonstrating mitral valve regurgitation. c Parasternal short axis view at the level of mitral valve showing tiny posterior pericardial effusion in a patient with myocarditis. d M-mode demonstrating decreased systolic function. e Apical 4 chamber view demonstrating severe left ventricular (LV) dilation due to myocardial dysfunction
Electrocardiographic Abnormalities and Arrhythmia
Patients affected with COVID-19 or MIS-C may be predisposed to various arrhythmias or electrocardiographic (ECG) abnormalities, not only from the disease itself but also from the arrhythmogenic potential of pharmacotherapies. In adults, a higher prevalence of both atrial [38] and ventricular arrhythmias [59] were noted among hospitalized patients with COVID-19 which has been linked to an increased risk of in-hospital death [59].
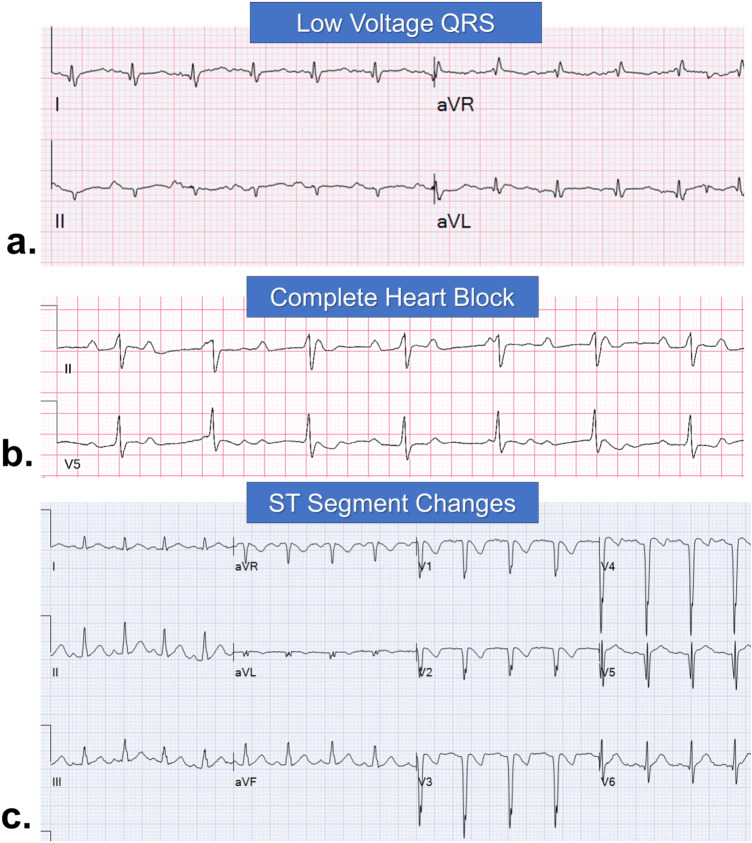
Possible ECG findings in children with COVID-19 or MIS-C are listed in Table 3 and shown in Fig. 2. In patients with myocardial dysfunction, diffuse ST segment changes, T wave inversions in lateral leads, low-voltage QRS, atrioventricular conduction block and sinus node dysfunction has been reported [26, 70–74]. Premature ventricular contractions [30], monomorphic [74] or polymorphic ventricular tachycardia (VT) [50] have also been reported. Patients with MIS-C may present with ECG abnormalities similar to those expressed in Kawasaki disease (Table 3) [9, 10]. QT prolongation can be seen in critically ill patients with systemic inflammation, fever, electrolyte abnormalities or hypoxia. In addition pharmacotherapies for COVID-19 such as hydroxychloroquine and azithromycin may cause fatal arrhythmias due to QT prolongation [75–77]. It is important to obtain a baseline ECG in patients with COVID-19 to measure a baseline QT interval, especially in those with congenital long QT syndrome or other genetic arrhythmias [75, 78–80]. Fever in patients with COVID-19 may unmask the classic Brugada pattern on ECG [67, 75, 76, 81, 82].
Table 3.
Potential electrocardiographic and echocardiographic findings in MIS-C
| Electrocardiographic abnormalities and arrhythmias | |
| Abnormalities related to myocardial dysfunction or myocarditis |
Diffuse ST segment elevation or depression T wave abnormality (inversion in lateral leads) Low QRS voltages Premature ventricular contractions Ventricular tachycardia |
| Abnormalities similar to Kawasaki disease |
Non-specific ST and T wave changes Myocardial ischemia PR prolongation Ventricular arrhythmia |
| Sinus node dysfunction and heart block |
Sinus node dysfunction (bradycardia) PR prolongation Atrioventricular block |
| Inherited arrhythmias and sudden death |
Prolonged QT Unmasking of Brugada pattern in patients with underlying Brugada syndrome in setting of fever Sudden cardiac death due to fatal arrhythmias |
| Echocardiographic abnormalities | |
| Ventricles | Depressed function of either or both ventricles, may be severe and may exhibit global or regional dysfunction |
| Abnormal myocardial strain | |
| Apical thrombus in setting of severely depressed function | |
| Coronary arteries | Abnormal enhancement of coronary arterial walls |
| Coronary arterial ectasia or dilation | |
| Aneurysm formation | |
| Thrombus formation in setting of severe coronary dilation | |
| Valves | Valvulitis with valvar insufficiency, particularly the mitral valve |
| Pericardium | Pericardial effusion |
| Aortic root | Aortic root dilation |
Fig. 2.
Electrocardiographic abnormalities in children with COVID-19 and MIS-C. a Low-voltage QRS complex in a patient with myocarditis. b Complete heart block in a patient with myocarditis. c ST segment changes in anterior leads suggestive of anterior infarction in a patient with giant coronary artery aneurysms and thrombosis
Cardiac Imaging
Echocardiographic Evaluation
During acute COVID-19 infection in hospitalized adult patients, echocardiographic features supportive of myopericarditis, stress-induced cardiomyopathy, and/or myocardial ischemia, injury, or infarction have been described [83]. There may be global or segmental mild to severe myocardial dysfunction involving the left ventricle in isolation or both ventricles [22, 23]. Left ventricular apical ballooning and dysfunction consistent with Takotsubo cardiomyopathy [27, 84] as well as pericardial effusions have been reported [22, 23]. In the pediatric population, data are lacking regarding echocardiographic findings during the acute infection likely due to the decreased incidence of clinically severe illness compared with adults [3, 34, 37].
However, echocardiographic information is available for pediatric patients with MIS-C. The initial alert to the international community first identifying MIS-C described myocarditis, valvulitis, pericardial effusion, and coronary artery dilation as features of the disease [14]. Of the 8 children from the United Kingdom (UK) reported by Riphagen et al., ventricular dysfunction was present in 6 patients. Only 1 child had severely dilated coronaries and 1 had peri-coronary echogenicity [9]. Subsequently, Belhhadjer et al. reported data regarding 35 children with MIS-C with acute left ventricular dysfunction (68% with cardiogenic shock) [10]. One of these patients had localized akinesis of the apical segment consistent with Takotsubo cardiomyopathy. Fortunately, 71% recovered LV function fully by day 7 of illness with therapy [10]. Coronary artery dilation (Z score > 2) was present in only 17% and pericardial effusions were seen in 8%. Verdoni et al. reported 10 patients with features of typical or atypical Kawasaki Disease and COVID-19, with ventricular dysfunction (ejection fraction < 55%) in 5, mitral insufficiency in 4 and coronary aneurysms (> 4 mm) in 2 patients [8]. Most recently, Whittaker et al. reported on 55 children from 8 hospitals in the UK who underwent echocardiography. Coronary dilation (Z score > 2) was noted in 8 (14%), including 2 with giant aneurysms (Z scores > 10). Of these eight, five had shock alone, one with fever and inflammation, and two with some mucocutaneous features of Kawasaki disease. Of the 29 children with shock, 62% had LV dysfunction on echo [50]. In a recent study from US constituting 186 children with MIS-C, Feldstein et al. reported coronary artery aneurysm (Z score > 2.5) in 9% (15/170) of the children who had echocardiogram [31].
For pediatric patients presenting with concern for MIS-C, hemodynamic shock and/or features of classic or atypical Kawasaki disease, a careful echocardiographic assessment (Table 3; Fig. 3) of left and right ventricular function, the pericardium, coronary arteries, and cardiac valves should be performed on admission to establish a baseline, as well as to guide initial vasoactive management for patients presenting with features of shock. It is important that the individual performing the echo have the skills to obtain all the necessary images in a time efficient manner to limit exposure. The American Society of Echocardiography (ASE) statement regarding echocardiography services during the COVID-19 pandemic can serve as a useful reference with regards to best practices [85]. The optimal interval between echocardiographic assessments remains to be determined. Primarily, a change in clinical status should guide the echocardiographic evaluation in individual cases. For patients requiring ICU management, daily echocardiograms may be warranted given the potential for rapid changes. For those on acute care floors, repeat echocardiograms every 2–3 days may be helpful although should be guided by the clinical scenario. Serial echocardiographic assessment of the coronary arteries for evolving dilation or development of coronary aneurysms is important as well, as this will impact decisions regarding immunomodulatory therapies and anti-thrombotic regimens. Previously published guidelines for optimal coronary artery imaging in Kawasaki Disease can be utilized [65, 86]. For patients with severe ventricular dysfunction or severe coronary dilation, serial assessment for thrombus is important. All MIS-C or Kawasaki disease spectrum type patients should have a follow-up with a pediatric cardiologist with an echocardiogram. Timing of follow-up and imaging tests will depend upon the clinical course, as well as the type and severity of cardiac involvement. Long term outcomes of children with MIS-C are unknown. Patients with continued coronary artery abnormalities or depressed ventricular function should continue to follow with a pediatric cardiologist while these sequelae of MIS-C are present. Given the unknowns, even those with recovery of ventricular function or resolution of coronary dilation likely warrant continued follow-up over time.
Advanced Imaging
Advanced cardiac imaging with computed tomographic angiography (CTA) may be necessary for demonstration of coronary arteries in older children and adolescents if poor acoustic windows limit echocardiographic assessment. Similar to Kawasaki disease, CTA also plays an important role in assessing distal vessels for evidence of dilation [65]. CTA is also critical in the evaluation of suspected coronary thrombus. Data regarding the use of cardiac magnetic resonance (CMR) imaging in the pediatric age group with COVID-19 are lacking although utilization of CMR imaging can be guided by previous evidence from viral myocarditis. Decisions should be made on case by case basis in consideration with the pediatric cardiologist. In the adult population, the utility of CMR has been described in a case report of myocarditis due to COVID-19, where it was used to confirm the diagnosis and to demonstrate the extent and severity of myocardial edema [30].
Management of Cardiovascular Complications in COVID-19
General Considerations
COVID-19 can lead to a wide spectrum of illness severity (Table 1) which guides the management [16]. Some general considerations for management of COVID-19 patients are stated in Table 4. The efficacy of various antiviral therapies in COVID-19 has yet to be established [16]. Therefore until more evidence is available; therapies such as remdesivir and hydroxychloroquine should be used in context of a clinical trial while weighing the risks and benefits of the therapy [16]. These decisions are individualized to every patient keeping in consideration the various risk factors including young age, immunocompromised status, underlying cardiac or pulmonary disease, obesity or diabetes [16].
Table 4.
Considerations for management of children with COVID-19 or MIS-C and cardiovascular involvement
| Considerations for management of typical COVID-19 with cardiovascular involvement | |
| General considerations |
Supplemental oxygen, non-invasive or invasive mechanical ventilation may be needed for patients as appropriate Fluid replenishment and adequate electrolyte monitoring Empiric antibiotics as clinically appropriate Antiviral therapies are to be used in the settings of a clinical trial in discussion with an infectious disease team |
| Cardiac considerations | For myocardial dysfunction, arrhythmias or other manifestations, see management suggestions listed below |
| Considerations for management of MIS-C with cardiovascular involvement | |
| General considerations |
Level of care is determined by the severity of illness Given multisystem involvement, patients may benefit from care by a multidisciplinary team of specialists Sequential laboratory markers of inflammation, coagulation studies, liver function tests and cardiac biomarkers may be warranted in hospitalized patients Additional management, as appropriate, is as per the intensivist or hospitalist based on the clinical presentation |
| Myocardial dysfunction or myocarditis |
Serial laboratory monitoring of cardiac biomarkers including troponin and BNP/NT-pro-BNP Serial echocardiographic assessment of myocardial function Continuous cardiac monitoring for arrhythmias Hemodynamic support utilizing inotropes and ECMO as indicated Care should be taken while sedating or intubating patients with severely depressed ventricular function Consideration for therapies such as IVIG, steroids or biological agents in the setting of a multidisciplinary team discussion regarding current evidence and best practices, risks and benefits |
| Arrhythmias |
12 lead ECG may obtained in all hospitalized children, those with elevated cardiac biomarkers or cardiac symptoms and before initiating any QT prolonging pharmacotherapies Aggressive fever reduction with acetaminophen is necessary for patients with Brugada syndrome Aggressive electrolyte correction is necessary for patients with inherited arrhythmias and channelopathies Modified ACLS and BLS guidelines should be utilized during cardiopulmonary resuscitation |
| Coronary artery and thrombotic complications |
Antiplatelet therapy should be considered for patients with MIS-C Anticoagulation guided by Kawasaki guidelines can be utilized based on degree of coronary artery involvement Pediatric cardiology follow-up and serial echocardiographic assessment is critically important for patients with coronary artery dilation due to MIS-C |
| Considerations for children with underlying cardiovascular conditions | |
| Chronic medications | Continue ACE inhibitors or ARBs in patients who are chronically receiving these therapies for hypertension, heart failure or other underlying diseases [66] |
| Anticoagulation | Certain exploratory antiviral therapies such as ropinavir/ritonavir, ribavirin, and adjunctive therapies such as sarilumab, tocilizumab interferon and methylprednisolone may interact with Warfarin. Therefore adequate INR monitoring should be performed with these therapies [66] |
| Aspirin should be continued in children and adolescents on chronic therapy for their underlying cardiovascular condition | |
| Immunosuppression | There is insufficient evidence regarding the potential role of reduction or changes in T-cell immunosuppressive therapy among infected patients after cardiac transplant patients with COVID-19. A detailed discussion with cardiac transplant team weighing risks and benefits of reduction in T-cell immunosuppression is warranted [16] |
ACE angiotensin converting enzyme, ARBs angiotensin receptor blockers, ACLS advanced cardiac life support, BLS basic life support, BNP brain natriuretic peptide, INR international normalized ratio, MIS-C multisystem inflammatory syndrome in children
Approach to Cardiovascular Complications
Myocardial Injury and Myocarditis
Although myocardial dysfunction is uncommon among children with typical COVID-19 infection; children presenting with MIS-C may have significant myocardial involvement [8–10, 50]. Evidence regarding optimal management of myocardial injury in patients with COVID-19 is limited. The management may be guided by the extent of myocardial injury based on laboratory (elevated Troponin or BNP/NT-pro-BNP) and imaging (echocardiography or CMR) assessment. Serial monitoring of biomarkers is prudent during admission as detailed in the section on laboratory evaluation. Hemodynamically stable children with mild myocardial dysfunction should be medically managed and optimized with careful fluid resuscitation, diuretics and heart failure therapy as appropriate. Children with hemodynamically significant or severe myocardial dysfunction may require inotropic support, mechanical ventilation to reduce metabolic demand and mechanical circulatory support with extracorporeal membrane oxygenation (ECMO) in those with critical hemodynamic compromise [10]. Shock in patients with MIS-C is often vasoplegic rather than cardiogenic and the use of norepinehrine to treat is effective but treatment may be guided by the degree of ventricular dysfunction [9].
Children with MISC and myocardial dysfunction may warrant treatment with intravenous immunoglobulin (IVIG) and/or steroids although the evidence is currently limited (Table 5) [8–10, 50, 87]. In six case series constituting 314 patients with MIS-C or Kawasaki-like presentation, a majority of patients were initially treated with IVIG (77%, 241/314) with or without steroids (53%, 167/314) [8–10, 50, 87]. Other immunomodulatory agents like anakinara was used in 20 patients, 8 received infliximab and 1 received tocilizumab. Among studies with available data, almost half of the patients (50%, 64/128) received combined therapy with at least 2 immunomodulatory agents generally IVIG and steroids.
Table 5.
Evidence on utilization of intravenous immune globulin and steroids in MIS-C
| Total No of Pts | IVIG | Steroids | Others | Combined therapy (≥ 2 agents) | |
|---|---|---|---|---|---|
|
Belhadjer et al. [10] (France and Switzerland) |
35 | 71% (25) | 34% (12) | Anakinara (3) | 14% (5) |
|
Riphagen et al. [9] (United Kingdom) |
8 | 100% (8) | 62% (5) | None | 62% (5) |
|
Verdoni et al. [8] (Italy) |
10 | 100% (10) | 80% (8) | None | 80% (8) |
|
Cheung et al. [87] (United States) |
17 | 76% (13) | 82% (14) | Tocilizumab (1) | 65% (11) |
|
Whittaker et al. [50] (England) |
58 | 70% (41) | 64% (37) |
Anakinara (3) Infliximab (8) |
60% (35) |
|
Feldstein et al. [31] (United States) |
186 | 77% (144) | 49% (91) | Anakinara (14) | - |
| Combined studies | 314 | 77% (241) | 53% (167) | 50% (64) |
Values are reported as % (n)
IVIG intravenous immune globulin
Arrhythmias
Although arrhythmias may be a rare manifestation of COVID-19, they are not uncommon in critically ill children with COVID-19 and MIS-C [9, 10, 75]. Critically ill patients with COVID-19 or MIS-C requiring intensive care or those with increased arrhythmia risk should be placed on continuous ECG monitoring [76]. Management should be tailored to the individual patient and arrhythmia. For instance in patients with Brugada syndrome, aggressive fever reduction with acetaminophen is prudent [77]. General considerations for management of arrhythmias are stated in Table 4. Additionally, the American Heart Association has released interim guidelines for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19 with attention to reducing provider exposure, prioritizing oxygenation and ventilation strategies, and considering the appropriateness of resuscitation [88].
Thrombotic Complications
Considering similarities between MIS-C and Kawasaki disease, these patients may also be at a higher risk of thrombotic complications. Among combined 278 patients from five recent studies who had echocardiograms, coronary dilation or aneurysm was reported in 12% (132/278) of patients [8, 10, 12]. Therefore, patients with MIS-C who fulfill criteria for Kawasaki disease, whether complete or incomplete, should be treated with appropriate anti-thrombotic therapy based on the degree of coronary artery involvement. Antiplatelet therapy should also be considered for all patients with MIS-C and evidence of coronary artery involvement [65]. Similarly patients with significant left ventricular dysfunction should also receive systemic anticoagulation as appropriate [89].
Pre-existing Cardiovascular Conditions
Children with congenital heart diseases or underlying cardiovascular conditions such as hypertension, heart failure or cardiac transplant pose certain unique challenges to their providers. It is critical to pay attention to their underlying disease process and chronic medications [16, 66]. Currently there is insufficient evidence to suggest any concern around safety of ACE inhibitors or Angiotensin receptor blockers (ARBs) in patients with COVID-19. Therefore multiple societies have endorsed and recommended to continue ACE inhibitors or ARBs therapy in patients who are chronically receiving these therapies for hypertension, heart failure or other underlying diseases [66]. Certain exploratory antiviral therapies like ropinavir/ritonavir, ribavirin, sarilumab, tocilizumab and adjunctive therapies like interferon or methylprednisolone may interact with Warfarin [66]. Therefore patients on chronic anticoagulation therapy should have adequate monitoring of INR while pursuing these therapies. Aspirin should be continued in children and adolescents on chronic therapy for their underlying cardiovascular condition. Currently there is insufficient evidence regarding role of reduction or changes in T-cell immunosuppressive therapy among infected patients after cardiac transplant [16]. A detailed discussion with cardiac transplant team weighing risks and benefits of reduction in T-cell immunosuppression is warranted.
Outcome and Follow-up
In a recent study by Feldstein et al. constituting 186 children from US, 8 patients required ECMO and 4 deaths were reported [31]. Among 230 cases of suspected MIS-C associated with COVID-19 reported to European Centre for Disease Prevention and Control, at least two deaths have been reported [11]. Currently we do not have enough data to predict future complications in MIS-C associated with COVID-19. As we steer through this uncharted territory of COVID-19, we may have to extrapolate evidence from conditions with similar presentations such as viral myocarditis or Kawasaki disease. Recommendations for follow-up, long term anticoagulation return to school and sports participation should be individualized to every patient. Follow-up should be individualized based on the degree of myocardial dysfunction, arrhythmia burden, and cardiac biomarkers along with a potential role of advanced imaging with CMR, as per the guidelines by AHA and American College of Cardiology (ACC) [90, 91].
Cardiac Interventions
The COVID-19 pandemic has seriously affected surgical and interventional practices, both catheterization and electrophysiology, in pediatric and congenital cardiology [92, 93]. Majority of centers have canceled or rescheduled elective procedures during the first phase of the pandemic and utilized a multidisciplinary committee to determine the candidacy of patients for urgent or emergent procedures. The definition of elective, urgent or emergent procedures is dependent on institutional policy and various society guidelines are now available to guide decisions [93, 94]. Generally, procedures are considered urgent or emergent if there is a substantial risk of clinical decompensation, hospitalization, or death if procedures are not performed [93, 94]. It is necessary to maintain a focus on resource utilization, preservation of medical supplies and minimization of exposure to hospital staff and other patients while making these decisions [92]. Pre-procedural COVID-19 testing is being performed in many centers to ensure safety and adequate personal protective equipment (PPE) utilization by health care team. Recommendations related to PPE continue to change. There is a concern that there may be a backlog of purely elective cases, a so called “surge after the surge”, that may continue on for months [95]. Each program should have a plan on how to deal with these cases [95].
Impact on the Economy and Insurance Policies
The negative effects of the COVID-19 pandemic on our national and global economy have been dramatic, affecting almost every industry. The majority of health insurance companies have followed the lead of the federal government and Centers for Medicare and Medicaid Services (CMS) to rapidly expand coverage to patients with COVID-19. All testing for COVID-19 has been designated an Essential Health Benefit (EHB), meaning it is to be covered by all Affordable Care Act—compliant plans. In March 2020, Congress passed the Families First Coronavirus Response Act [96] which requires the majority of private health plans to cover COVID-19 testing and all related urgent care center and emergency room visits, telehealth services, and in-person medical provider encounters, all with no cost sharing (co-payments, co-insurance and deductibles) and no prior authorization during the emergency period [96]. There continue to be discrepancies across states and insurance policies, so it is advised that the patient, physician and billing department stay abreast of this rapidly changing market and their implications. If patients are experiencing financial difficulties due to COVID-19, there are a number of government programs available, including but not limited to unemployment coverage:Supplemental Nutrition Assistance Program (SNAP), Women, Infants, and Children (WIC), Child’s Health Insurance Program (CHIP) and Medicaid. For children, the CHIP offers free or low-cost medical and dental care to uninsured patients through 19 years of age, whose family income is above Medicaid’s limit but below their state’s CHIP limit. Many states have modified their CHIP enrollment criteria and dates to expand eligibility and eliminate or waive premiums. The CARES act and SBA loans have provided some financial support to medical practices and hospitals.
Future Directions
COVID-19 has had a profound impact on the practice of medicine and will continue to impact all elements of patient care. As more pediatric data become available, the approach to the evaluation and management of children with COVID-19, including those with suspicion for cardiac injury, will necessarily evolve. Pediatric cardiologists can have a meaningful impact in the care and outcomes of these patients.
Abbreviations
- AAP
American Academy of Pediatrics
- ACC
American College of Cardiology
- AHA
American Heart Association
- ASE
American Society of Echocardiography
- BNP
Brain natriuretic peptide
- CDC
Center for Disease Control and Prevention
- CHIP
Child’s Health Insurance Program
- CK
Creatine kinase
- CMR
Cardiac magnetic resonance
- CMS
Centers for Medicare and Medicaid Services
- COVID-19
Coronavirus disease 2019
- CRP
C-reactive protein
- CTA
Computed tomographic angiography
- ECG
Electrocardiogram
- ECMO
Extracorporeal membrane oxygenation
- EHB
Essential Health Benefit
- ESR
Erythrocyte sedimentation rate
- GI
Gastrointestinal
- ICU
Intensive care unit
- IVIG
Intravenous immunoglobulin
- LDH
Lactate dehydrogenase
- MIS-C
Multisystem inflammatory syndrome in children
- NT-pro-BNP
N terminal pro brain natriuretic peptide
- PIMS
Pediatric inflammatory multisystem syndrome
- PMIS
Pediatric multisystem inflammatory syndrome
- RT-PCR
Reverse transcription polymerase chain reaction
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2
- SNAP
Supplemental Nutrition Assistance Program
- UK
United Kingdom
- VT
Ventricular tachycardia
- WHO
World Health Organization
- WIC
Women, Infants and Children
Funding
No funding was utilized for this manuscript.
Compliance with Ethical Standards
Conflict of interest
The authors have indicated they have no potential conflicts of interest to disclose. Authors have indicated they have no financial relationships relevant to this article to disclose.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Global Surveillance for human infection with coronavirus disease (COVID-19) https://www.who.int/publications-detail/global-surveillance-for-human-infection-with-novel-coronavirus-(2019-ncov). Accessed 1 June 2020
- 2.Tagarro A, Epalza C, Santos M, Sanz-Santaeufemia FJ, Otheo E, Moraleda C, Calvo C. Screening and severity of coronavirus disease 2019 (COVID-19) in children in Madrid, Spain. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shekerdemian LS, Mahmood NR, Wolfe KK, Riggs BJ, Ross CE, McKiernan CA, Heidemann SM, Kleinman LC, Sen AI, Hall MW, Priestley MA, McGuire JK, Boukas K, Sharron MP, Burns JP, Collaborative ftIC-P Characteristics and outcomes of children with coronavirus disease 2019 (COVID-19) infection admitted to US and Canadian pediatric intensive care units. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parri N, Lenge M, Buonsenso D. Children with Covid-19 in pediatric emergency departments in Italy. N Engl J Med. 2020 doi: 10.1056/NEJMc2007617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Livingston E, Bucher K. Coronavirus disease 2019 (COVID-19) in Italy. JAMA. 2020;323(14):1335–1335. doi: 10.1001/jama.2020.4344. [DOI] [PubMed] [Google Scholar]
- 7.Covid CD, et al. Coronavirus Disease 2019 in Children - United States, February 12-April 2, 2020 (2020) MMWR Morb Mortal Wkly Rep. 2020;69(14):422–426. doi: 10.15585/mmwr.mm6914e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Verdoni L, Mazza A, Gervasoni A, Martelli L, Ruggeri M, Ciuffreda M, Bonanomi E, D’Antiga L. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020 doi: 10.1016/S0140-6736(20)31103-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020 doi: 10.1016/S0140-6736(20)31094-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Belhadjer Z, Méot M, Bajolle F, Khraiche D, Legendre A, Abakka S, Auriau J, Grimaud M, Oualha M, Beghetti M, Wacker J, Ovaert C, Hascoet S, Selegny M, Malekzadeh-Milani S, Maltret A, Bosser G, Giroux N, Bonnemains L, Bordet J, Filippo SD, Mauran P, Falcon-Eicher S, Thambo J-B, Lefort B, Moceri P, Houyel L, Renolleau S, Bonnet D. Acute heart failure in multisystem inflammatory syndrome in children (MIS-C) in the context of global SARS-CoV-2 pandemic. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.048360. [DOI] [PubMed] [Google Scholar]
- 11.Rapid risk assessment: Paediatric inflammatory multisystem syndrome and SARS -CoV-2 infection in children. https://www.ecdc.europa.eu/sites/default/files/documents/covid-19-risk-assessment-paediatric-inflammatory-multisystem-syndrome-15-May-2020.pdf. Accessed May 24 2020
- 12.Network HA (2020) Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with Coronavirus Disease 2019 (COVID-19). https://emergency.cdc.gov/han/2020/han00432.asp. Accessed May 23 2020
- 13.Multisystem Inlfammtory Syndrome (MIS-C) (2020) https://www.cdc.gov/mis-c/hcp/. Accessed 8 June 2020
- 14.Royal College of Paediatrics and Child Health Guidance: Paediatric multisystem inflammatory syndrome temporally associated with COVID-19. https://www.rcpch.ac.uk/sites/default/files/2020-05/COVID-19-Paediatric-multisystem-%2520inflammatory%2520syndrome-20200501.pdf. Accessed 31 May 2020
- 15.European Centre for Disease Prevention and Control Rapid Risk Assessment: Paediatric inflammatory multisystem syndrome and SARS CoV 2 infection in children. https://www.ecdc.europa.eu/sites/default/files/documents/covid-19-risk-assessment-paediatric-inflammatory-multisystem-syndrome-15-May-2020.pdf. Accessed 31 May 2020
- 16.Chiotos K, Hayes M, Kimberlin DW, Jones SB, James SH, Pinninti SG, Yarbrough A, Abzug MJ, MacBrayne CE, Soma VL, Dulek DE, Vora SB, Waghmare A, Wolf J, Olivero R, Grapentine S, Wattier RL, Bio L, Cross SJ, Dillman NO, Downes KJ, Timberlake K, Young J, Orscheln RC, Tamma PD, Schwenk HT, Zachariah P, Aldrich M, Goldman DL, Groves HE, Lamb GS, Tribble AC, Hersh AL, Thorell EA, Denison MR, Ratner AJ, Newland JG, Nakamura MM. Multicenter initial guidance on use of antivirals for children with COVID-19/SARS-CoV-2. J Pediatr Infect Dis Soc. 2020 doi: 10.1093/jpids/piaa045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Center for Disease Control and Prevention, Center for Preparedness and Response: Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with Coronavirus Disease 2019 (COVID-19), Clinician Outreach and Communication (COCA) Webinar. https://emergency.cdc.gov/coca/calls/2020/callinfo_051920.asp?deliveryName=USCDC_1052-DM28623. Accessed 31 May 2020
- 18.Multisystem inflammatory syndrome in children and adolescents with COVID-19. https://www.who.int/publications-detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19. Accessed 1 June 2020
- 19.Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, Huang H, Zhang L, Zhou X, Du C, Zhang Y, Song J, Wang S, Chao Y, Yang Z, Xu J, Zhou X, Chen D, Xiong W, Xu L, Zhou F, Jiang J, Bai C, Zheng J, Song Y. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the chinese center for disease control and prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 21.Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1286. [DOI] [PubMed] [Google Scholar]
- 22.Fried JA, Ramasubbu K, Bhatt R, Topkara VK, Clerkin KJ, Horn E, Rabbani L, Brodie D, Jain SS, Kirtane A, Masoumi A, Takeda K, Kumaraiah D, Burkhoff D, Leon M, Schwartz A, Uriel N, Sayer G. The variety of cardiovascular presentations of COVID-19. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hendren NS, Drazner MH, Bozkurt B, Cooper LT. Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bangalore S, Sharma A, Slotwiner A, Yatskar L, Harari R, Shah B, Ibrahim H, Friedman GH, Thompson C, Alviar CL, Chadow HL, Fishman GI, Reynolds HR, Keller N, Hochman JS. ST-segment elevation in patients with Covid-19: a case series. N Engl J Med. 2020 doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kuck KH. Arrhythmias and sudden cardiac death in the COVID-19 pandemic. Herz. 2020 doi: 10.1007/s00059-020-04924-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Azarkish M, Laleh Far V, Eslami M, Mollazadeh R. Transient complete heart block in a patient with critical COVID-19. Eur Heart J. 2020 doi: 10.1093/eurheartj/ehaa307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meyer P, Degrauwe S, Van Delden C, Ghadri JR, Templin C. Typical takotsubo syndrome triggered by SARS-CoV-2 infection. Eur Heart J. 2020;41(19):1860. doi: 10.1093/eurheartj/ehaa306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Craver R, Huber S, Sandomirsky M, McKenna D, Schieffelin J, Finger L. Fatal eosinophilic myocarditis in a healthy 17-year-old male with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2c) Fetal Pediatr Pathol. 2020 doi: 10.1080/15513815.2020.1761491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oberweis M-L, Codreanu A, Boehm W, Olivier D, Pierron C, Tsobo C, Kohnen M, Abdelrahman TT, Nguyen NT, Wagner K, de la Fuente GI. Pediatric life-threatening coronavirus disease 2019 with myocarditis. Pediatr Infect Dis J Online First. 2020 doi: 10.1097/inf.0000000000002744. [DOI] [PubMed] [Google Scholar]
- 30.Kim I-C, Kim JY, Kim HA, Han S. COVID-19-related myocarditis in a 21-year-old female patient. Eur Heart J. 2020;41(19):1859–1859. doi: 10.1093/eurheartj/ehaa288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Feldstein LR, Rose EB, Horwitz SM, Collins JP, Newhams MM, Son MBF, Newburger JW, Kleinman LC, Heidemann SM, Martin AA, Singh AR, Li S, Tarquinio KM, Jaggi P, Oster ME, Zackai SP, Gillen J, Ratner AJ, Walsh RF, Fitzgerald JC, Keenaghan MA, Alharash H, Doymaz S, Clouser KN, Giuliano JS, Gupta A, Parker RM, Maddux AB, Havalad V, Ramsingh S, Bukulmez H, Bradford TT, Smith LS, Tenforde MW, Carroll CL, Riggs BJ, Gertz SJ, Daube A, Lansell A, Coronado Munoz A, Hobbs CV, Marohn KL, Halasa NB, Patel MM, Randolph AG. Multisystem inflammatory syndrome in U.S. children and adolescents. N Engl J Med. 2020;383(4):334–346. doi: 10.1056/NEJMoa2021680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cummings MJ, Baldwin MR, Abrams D, Jacobson SD, Meyer BJ, Balough EM, Aaron JG, Claassen J, Rabbani LE, Hastie J, Hochman BR, Salazar-Schicchi J, Yip NH, Brodie D, Donnell MR. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet. 2020 doi: 10.1016/S0140-6736(20)31189-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, Tong S. Epidemiology of COVID-19 among children in China. Pediatrics. 2020 doi: 10.1542/peds.2020-0702. [DOI] [PubMed] [Google Scholar]
- 35.Hong H, Wang Y, Chung H-T, Chen C-J. Clinical characteristics of novel coronavirus disease 2019 (COVID-19) in newborns, infants and children. Pediatr Neonatol. 2020;61(2):131–132. doi: 10.1016/j.pedneo.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lu X, Zhang L, Du H, Zhang J, Li YY, Qu J, Zhang W, Wang Y, Bao S, Li Y, Wu C, Liu H, Liu D, Shao J, Peng X, Yang Y, Liu Z, Xiang Y, Zhang F, Silva RM, Pinkerton KE, Shen K, Xiao H, Xu S, Wong GWK. SARS-CoV-2 infection in children. N Engl J Med. 2020;382(17):1663–1665. doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Castagnoli R, Votto M, Licari A, Brambilla I, Bruno R, Perlini S, Rovida F, Baldanti F, Marseglia GL. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1467. [DOI] [PubMed] [Google Scholar]
- 38.Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, Satlin MJ, Campion TR, Jr, Nahid M, Ringel JB, Hoffman KL, Alshak MN, Li HA, Wehmeyer GT, Rajan M, Reshetnyak E, Hupert N, Horn EM, Martinez FJ, Gulick RM, Safford MM. Clinical characteristics of COVID-19 in New York city. N Engl J Med. 2020 doi: 10.1056/NEJMc2010419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS, China Medical Treatment Expert Group for C Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cai X, Ma Y, Li S, Chen Y, Rong Z, Li W. Clinical characteristics of 5 COVID-19 cases with non-respiratory symptoms as the first manifestation in children. Front Pediatr. 2020 doi: 10.3389/fped.2020.00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hon KL, Leung CW, Cheng WT, Chan PK, Chu WC, Kwan YW, Li AM, Fong NC, Ng PC, Chiu MC, Li CK, Tam JS, Fok TF. Clinical presentations and outcome of severe acute respiratory syndrome in children. Lancet. 2003;361(9370):1701–1703. doi: 10.1016/s0140-6736(03)13364-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chiu WK, Cheung PC, Ng KL, Ip PL, Sugunan VK, Luk DC, Ma LC, Chan BH, Lo KL, Lai WM. Severe acute respiratory syndrome in children: experience in a regional hospital in Hong Kong. Pediatr Crit Care Med. 2003;4(3):279–283. doi: 10.1097/01.Pcc.0000077079.42302.81. [DOI] [PubMed] [Google Scholar]
- 44.Galván Casas C, Català A, Carretero Hernández G, Rodríguez-Jiménez P, Fernández Nieto D, Rodríguez-Villa Lario A, Navarro Fernández I, Ruiz-Villaverde R, Falkenhain D, Llamas Velasco M, García-Gavín J, Baniandrés O, González-Cruz C, Morillas-Lahuerta V, Cubiró X, Figueras Nart I, Selda-Enriquez G, Romaní J, Fustà-Novell X, Melian-Olivera A, Roncero Riesco M, Burgos-Blasco P, Sola Ortigosa J, Feito Rodriguez M, García-Doval I. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol. 2020 doi: 10.1111/bjd.19163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34(5):e212–e213. doi: 10.1111/jdv.16387. [DOI] [PubMed] [Google Scholar]
- 46.Dolhnikoff M, Duarte-Neto AN, de Almeida Monteiro RA, Ferraz da Silva LF, Pierre de Oliveira E, Nascimento Saldiva PH, Mauad T, Marcia Negri E. Pathological evidence of pulmonary thrombotic phenomena in severe COVID-19. J Thrombos Haemost. 2020 doi: 10.1111/jth.14844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, Nigoghossian CD, Ageno W, Madjid M, Guo Y, Tang LV, Hu Y, Giri J, Cushman M, Quéré I, Dimakakos EP, Gibson CM, Lippi G, Favaloro EJ, Fareed J, Caprini JA, Tafur AJ, Burton JR, Francese DP, Wang EY, Falanga A, McLintock C, Hunt BJ, Spyropoulos AC, Barnes GD, Eikelboom JW, Weinberg I, Schulman S, Carrier M, Piazza G, Beckman JA, Steg PG, Stone GW, Rosenkranz S, Goldhaber SZ, Parikh SA, Monreal M, Krumholz HM, Konstantinides SV, Weitz JI, Lip GYH. COVID-19 and Thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol. 2020 doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Giacomelli A, Pezzati L, Conti F, Bernacchia D, Siano M, Oreni L, Rusconi S, Gervasoni C, Ridolfo AL, Rizzardini G, Antinori S, Galli M. Self-reported olfactory and taste disorders in SARS-CoV-2 patients: a cross-sectional study. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jones VG, Mills M, Suarez D, Hogan CA, Yeh D, Segal JB, Nguyen EL, Barsh GR, Maskatia S, Mathew R. COVID-19 and Kawasaki disease: novel virus and novel case. Hosp Pediatr. 2020 doi: 10.1542/hpeds.2020-0123. [DOI] [PubMed] [Google Scholar]
- 50.Whittaker E, Bamford A, Kenny J, Kaforou M, Jones CE, Shah P, Ramnarayan P, Fraisse A, Miller O, Davies P, Kucera F, Brierley J, McDougall M, Carter M, Tremoulet A, Shimizu C, Herberg J, Burns JC, Lyall H, Levin M, Group ftP-TS. EUCLIDS, Consortia P Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2. JAMA. 2020 doi: 10.1001/jama.2020.10369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tullie L, Ford K, Bisharat M, Watson T, Thakkar H, Mullassery D, Giuliani S, Blackburn S, Cross K, De Coppi P, Curry J. Gastrointestinal features in children with COVID-19: an observation of varied presentation in eight children. Lancet Child Adolesc Health. 2020 doi: 10.1016/s2352-4642(20)30165-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.FDA Coronavirus Testing Basics. https://www.fda.gov/consumers/consumer-updates/coronavirus-testing-basics. Accessed 30 May 2020
- 53.Sethuraman N, Jeremiah SS, Ryo A. Interpreting diagnostic tests for SARS-CoV-2. JAMA. 2020 doi: 10.1001/jama.2020.8259. [DOI] [PubMed] [Google Scholar]
- 54.Watson J, Whiting PF, Brush JE. Interpreting a covid-19 test result. BMJ Clin Res. 2020;369:m1808. doi: 10.1136/bmj.m1808. [DOI] [PubMed] [Google Scholar]
- 55.FDA US Food and Drug Administration Statement: Coronavirus (COVID-19) Update: FDA Authorizes First Antigen Test to Help in the Rapid Detection of the Virus that Causes COVID-19 in Patients. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-first-antigen-test-help-rapid-detection-virus-causes. Accessed 30 May 2020
- 56.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/s0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bonow RO, Fonarow GC, O'Gara PT, Yancy CW. Association of coronavirus disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1105. [DOI] [PubMed] [Google Scholar]
- 58.Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gao L, Jiang D, Wen XS, Cheng XC, Sun M, He B, You LN, Lei P, Tan XW, Qin S, Cai GQ, Zhang DY. Prognostic value of NT-proBNP in patients with severe COVID-19. Respir Res. 2020;21(1):83. doi: 10.1186/s12931-020-01352-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Henry BM, Lippi G, Plebani M. Laboratory abnormalities in children with novel coronavirus disease 2019. Clin Chem Lab Med. 2020 doi: 10.1515/cclm-2020-0272. [DOI] [PubMed] [Google Scholar]
- 62.Chao JY, Derespina KR, Herold BC, Goldman DL, Aldrich M, Weingarten J, Ushay HM, Cabana MD, Medar SS. Clinical characteristics and outcomes of hospitalized and critically ill children and adolescents with coronavirus disease 2019 (COVID-19) at a Tertiary Care Medical Center in New York City. J Pediatr. 2020 doi: 10.1016/j.jpeds.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tersalvi G, Vicenzi M, Calabretta D, Biasco L, Pedrazzini G, Winterton D. Elevated troponin in patients with coronavirus disease 2019: possible mechanisms. J Card Fail. 2020 doi: 10.1016/j.cardfail.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Vaduganathan M, Vardeny O, Michel T, McMurray JJV, Pfeffer MA, Solomon SD. Renin–angiotensin–aldosterone system inhibitors in patients with COVID-19. N Engl J Med. 2020;382(17):1653–1659. doi: 10.1056/NEJMsr2005760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, Baker AL, Jackson MA, Takahashi M, Shah PB, Kobayashi T, Wu M-H, Saji TT, Pahl E. Diagnosis, treatment, and long-term management of kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135(17):e927–e999. doi: 10.1161/CIR.0000000000000484. [DOI] [PubMed] [Google Scholar]
- 66.Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, Brown TS, Der Nigoghossian C, Zidar DA, Haythe J, Brodie D, Beckman JA, Kirtane AJ, Stone GW, Krumholz HM, Parikh SA. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75(18):2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lazzerini Pietro E, Boutjdir M, Capecchi Pier L. COVID-19, arrhythmic risk and inflammation: mind the gap! Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047293. [DOI] [PubMed] [Google Scholar]
- 68.AAP CDC details COVID-19-related inflammatory syndrome in children. https://www.aappublications.org/news/2020/05/14/covid19inflammatory051420. Accessed 4 June 2020
- 69.CDC Information for Pediatric Healthcare Providers. https://www.cdc.gov/coronavirus/2019-ncov/hcp/pediatric-hcp.html#anchor_1587145914005. Accessed 4 June 2020
- 70.Doyen D, Moceri P, Ducreux D, Dellamonica J. Myocarditis in a patient with COVID-19: a cause of raised troponin and ECG changes. Lancet. 2020;395(10235):1516. doi: 10.1016/S0140-6736(20)30912-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, Cani DS, Cerini M, Farina D, Gavazzi E, Maroldi R, Adamo M, Ammirati E, Sinagra G, Lombardi CM, Metra M. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hua A, O'Gallagher K, Sado D, Byrne J. Life-threatening cardiac tamponade complicating myo-pericarditis in COVID-19. Eur Heart J. 2020 doi: 10.1093/eurheartj/ehaa253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Paul J-F, Charles P, Richaud C, Caussin C, Diakov C. Myocarditis revealing COVID-19 infection in a young patient. Eur Heart J. 2020 doi: 10.1093/ehjci/jeaa107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Peigh G, Leya MV, Baman JR, Cantey EP, Knight BP, Flaherty JD. Novel coronavirus 19 (COVID-19) associated sinus node dysfunction: a case series. Eur Heart J. 2020 doi: 10.1093/ehjcr/ytaa132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Roden DM, Harrington RA, Poppas A, Russo AM. Considerations for Drug interactions on QTc interval in exploratory COVID-19 treatment. J Am Coll Cardiol. 2020;75(20):2623–2624. doi: 10.1016/j.jacc.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Giudicessi JR, Noseworthy PA, Friedman PA, Ackerman MJ. Urgent guidance for navigating and circumventing the QTc-prolonging and torsadogenic potential of possible pharmacotherapies for coronavirus disease 19 (COVID-19) Mayo Clin Proc. 2020 doi: 10.1016/j.mayocp.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wu C-I, Postema PG, Arbelo E, Behr ER, Bezzina CR, Napolitano C, Robyns T, Probst V, Schulze-Bahr E, Remme CA, Wilde AAM. SARS-CoV-2, COVID-19, and inherited arrhythmia syndromes. Heart Rhythm. 2020 doi: 10.1016/j.hrthm.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bessière F, Roccia H, Delinière A, Charrière R, Chevalier P, Argaud L, Cour M. Assessment of QT Intervals in a case series of patients with coronavirus disease 2019 (COVID-19) infection treated with hydroxychloroquine alone or in combination with azithromycin in an intensive care unit. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chorin E, Dai M, Shulman E, Wadhwani L, Bar-Cohen R, Barbhaiya C, Aizer A, Holmes D, Bernstein S, Spinelli M, Park DS, Chinitz LA, Jankelson L. The QT interval in patients with COVID-19 treated with hydroxychloroquine and azithromycin. Nat Med. 2020 doi: 10.1038/s41591-020-0888-2. [DOI] [PubMed] [Google Scholar]
- 80.Mercuro NJ, Yen CF, Shim DJ, Maher TR, McCoy CM, Zimetbaum PJ, Gold HS. Risk of QT interval prolongation associated with use of hydroxychloroquine with or without concomitant azithromycin among hospitalized patients testing positive for coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chang D, Saleh M, Garcia-Bengo Y, Choi E, Epstein L, Willner J. COVID-19 infection unmasking Brugada syndrome. Heart Rhythm Case Rep. 2020 doi: 10.1016/j.hrcr.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Vidovich MI. Transient brugada-like electrocardiographic pattern in a patient with COVID-19. JACC Case Rep. 2020 doi: 10.1016/j.jaccas.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kang Y, Chen T, Mui D, Ferrari V, Jagasia D, Scherrer-Crosbie M, Chen Y, Han Y. Cardiovascular manifestations and treatment considerations in COVID-19. Heart. 2020;2020:317056. doi: 10.1136/heartjnl-2020-317056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sala S, Peretto G, Gramegna M, Palmisano A, Villatore A, Vignale D, De Cobelli F, Tresoldi M, Cappelletti AM, Basso C, Godino C, Esposito A. Acute myocarditis presenting as a reverse Tako-Tsubo syndrome in a patient with SARS-CoV-2 respiratory infection. Eur Heart J. 2020;41(19):1861–1862. doi: 10.1093/eurheartj/ehaa286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Barker PCA, Lewin MB, Donofrio MT, Altman CA, Ensing GJ, Arya B, Swaminathan M. Specific considerations for pediatric, fetal, and congenital heart disease patients and echocardiography service providers during the 2019 novel coronavirus outbreak: Council on Pediatric and Congenital Heart Disease Supplement to the Statement of the American Society of Echocardiography Endorsed by the Society of Pediatric Echocardiography and the Fetal Heart Society. J Am Soc Echocardiogr. 2020 doi: 10.1016/j.echo.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Altman CA. Clinical assessment of coronary arteries in Kawasaki disease: focus on echocardiographic assessment. Congenit Heart Dis. 2017;12(5):636–640. doi: 10.1111/chd.12496. [DOI] [PubMed] [Google Scholar]
- 87.Cheung EW, Zachariah P, Gorelik M, Boneparth A, Kernie SG, Orange JS, Milner JD. Multisystem Inflammatory Syndrome Related to COVID-19 in Previously Healthy Children and Adolescents in New York City. JAMA. 2020 doi: 10.1001/jama.2020.10374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Edelson DP, Sasson C, Chan PS, Atkins DL, Aziz K, Becker LB, Berg RA, Bradley SM, Brooks SC, Cheng A, Escobedo M, Flores GE, Girotra S, Hsu A, Kamath-Rayne BD, Lee HC, Lehotzky RE, Mancini ME, Merchant RM, Nadkarni VM, Panchal AR, Peberdy MAR, Raymond TT, Walsh B, Wang DS, Zelop CM, Topjian A. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: from the Emergency Cardiovascular Care Committee and get with the Guidelines-Resuscitation Adult and Pediatric Task Forces of the American Heart Association in Collaboration with the American Academy of Pediatrics, American Association for Respiratory Care, American College of Emergency Physicians, The Society of Critical Care Anesthesiologists, and American Society of Anesthesiologists: Supporting Organizations: American Association of Critical Care Nurses and National EMS Physicians. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lin KY, Kerur B, Witmer CM, Beslow LA, Licht DJ, Ichord RN, Kaufman BD. Thrombotic events in critically ill children with myocarditis. Cardiol Young. 2014;24(5):840–847. doi: 10.1017/s1047951113001145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pelliccia A, Solberg EE, Papadakis M, Adami PE, Biffi A, Caselli S, La Gerche A, Niebauer J, Pressler A, Schmied CM, Serratosa L, Halle M, Van Buuren F, Borjesson M, Carrè F, Panhuyzen-Goedkoop NM, Heidbuchel H, Olivotto I, Corrado D, Sinagra G, Sharma S. Recommendations for participation in competitive and leisure time sport in athletes with cardiomyopathies, myocarditis, and pericarditis: position statement of the Sport Cardiology Section of the European Association of Preventive Cardiology (EAPC) Eur Heart J. 2018;40(1):19–33. doi: 10.1093/eurheartj/ehy730. [DOI] [PubMed] [Google Scholar]
- 91.Maron BJ, Udelson JE, Bonow RO, Nishimura RA, Ackerman MJ, Estes NAM, Cooper LT, Link MS, Maron MS. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task Force 3: hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy and other cardiomyopathies, and myocarditis. Circulation. 2015;132(22):e273–e280. doi: 10.1161/CIR.0000000000000239. [DOI] [PubMed] [Google Scholar]
- 92.Morray BH, Gordon BM, Crystal MA, Goldstein BH, Qureshi AM, Torres AJ, Epstein SM, Crittendon I, Ing FF, Sathanandam SK. Resource allocation and decision making for pediatric and congenital cardiac catheterization during the novel coronavirus SARS-CoV-2 (COVID-19) pandemic: a U.S. multi-institutional perspective. J Invasive Cardiol. 2020;32(5):E103–E109. doi: 10.25270/jic/20.00189. [DOI] [PubMed] [Google Scholar]
- 93.Lakkireddy DR, Chung MK, Gopinathannair R, Patton KK, Gluckman TJ, Turagam M, Cheung J, Patel P, Sotomonte J, Lampert R, Han JK, Rajagopalan B, Eckhardt L, Joglar J, Sandau K, Olshansky B, Wan E, Noseworthy PA, Leal M, Kaufman E, Gutierrez A, Marine JM, Wang PJ, Russo AM. Guidance for cardiac electrophysiology during the coronavirus (COVID-19) Pandemic from the Heart Rhythm Society COVID-19 Task Force; Electrophysiology Section of the American College of Cardiology; and the Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology, American Heart Association. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Welt FGP, Shah PB, Aronow HD, Bortnick AE, Henry TD, Sherwood MW, Young MN, Davidson LJ, Kadavath S, Mahmud E, Kirtane AJ. Catheterization laboratory considerations during the coronavirus (COVID-19) pandemic: from the ACC’s Interventional Council and SCAI. J Am Coll Cardiol. 2020;75(18):2372–2375. doi: 10.1016/j.jacc.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Salenger R, Etchill EW, Ad N, Matthew T, Alejo D, Whitman G, Lawton JS, Lau CL, Gammie CF, Gammie JS. The Surge after the Surge: cardiac Surgery post-COVID-19. Ann Thorac Surg. 2020 doi: 10.1016/j.athoracsur.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.H.R.6201 - Families First Coronavirus Response Act. https://www.congress.gov/bill/116th-congress/house-bill/6201. Accessed 7 June 202