Abstract
The problem with the regulation of the autonomic nervous system or paroxysmal reflex vagal activation episodes may have an important role in the pathophysiology of vasovagal syncope (VVS), sinus bradycardia or periods of sinus arrest, and variable-degree atrioventricular block (AVB). Because existence of structural heart disease tends to shift the vagosympathetic balance towards a sympathetic predominance, vagally-mediated bradyarrhythmias (VMB) usually occurs in young individuals with structurally normal hearts. However, similar reflex problems may be observed in the elderly people and even those with structural heart disease. Modification of the efferent arm of autonomic nervous system by ablation of main ganglionated plexi (GPs) is called as cardioneuroablation (CNA) and seems as a promising treatment option for appropriately selected patients with VMB. This review outlines the process of patient selection for CNA on the basis of supporting evidence.
Keywords: Cardioneuroablation, Syncope, Atrioventricular Block, Bradycardia, Ganglionated Plexi
Introduction
Abnormal autonomic activity may play a critical role in occurrence of clinical bradyarrhythmias such as vasovagal syncope (VVS), sinus node dysfunction (SND), and functional atrioventricular block (AVB) 1,2. In patients with VVS, cardiovascular autonomic reflexes become intermittently exaggerated, in response to a trigger, which is associated with bradycardia (cardioinhibitory response) and/or hypotension (vasodepressor response), likely mediated by parasympathetic over-activity and/or sympathetic withdrawal 3. Symptomatic SND and AVB are special entities whose prognoses depend strongly on etiology. Even after ruling out the obvious and reversible causes, it is often difficult to differentiate benign vagal over-activity from structural dysfunction of the sinus node and atrioventricular conduction system 4,5. However, paroxysmal AVB and asystole episodes are most likely to be autonomic 6. There is still no well-defined treatment option in case of vagal induced bradyarrhythmias. In cases of symptomatic and refractory vagal induced bradyarrhythmias, pacemaker implantation may be necessary to prevent bradycardic episodes.
Modification of the cardiac autonomic innervation by radiofrequency catheter ablation of main ganglionated plexi (GPs) which are part of the intrinsic nervous system of the heart is called as cardioneuroablation (CNA) and may reduce the impact of hyper vagotonia on the heart 7-10.
This review discusses how we can select suitable candidates for CNA on the basis of supporting evidence.
The process of patient selection for cardioneuroablation
Assess the contribution of parasympathetic system
The initial step in assessing if an individual patient is suitable for CNA is to determine the level of contribution of vagal overactivity in the occurrence of the clinical condition.
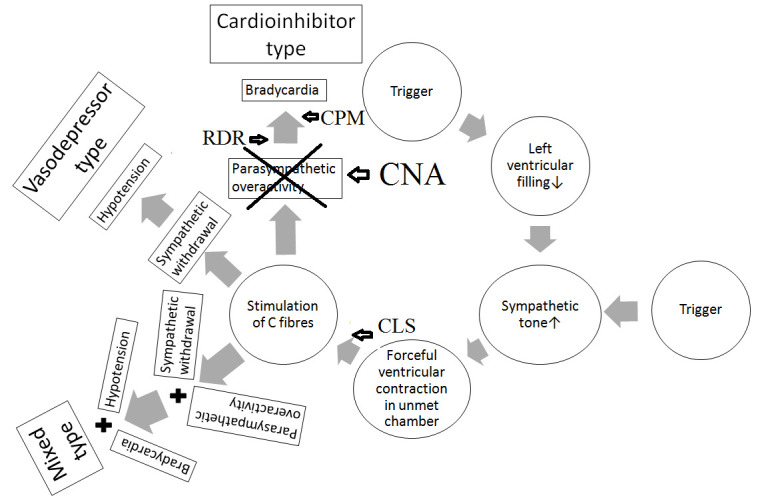
Vasovagal syncope
VVS is the most common type of syncope and is characterized by an abrupt dysregulation of the autonomic nervous system to maintain adequate blood pressure and or heart rate for cerebral perfusion 3. As a response to a potential trigger, 3 well-defined responses might be seen: a cardioinhibitory response due to vagal activation manifested by persistent bradycardia or prolonged pauses and the absence of significant hypotension, a vasodepressor response due to sympathetic withdrawal manifested by significant hypotension in the absence of bradycardia, and a mixed response manifested by co-existing bradycardia and hypotension Figure 1-11.
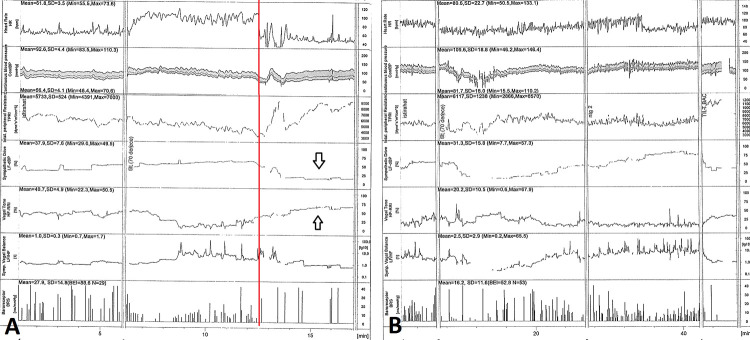
Figure 1. Pathophysiology of Vasovagal Syncope.
According to ventricular theory, the activation of left ventricular mechanoreceptors in response to a trigger, such as a decrease in venous return due to volume depletion or prolonged standing, causes an increase in cardiac contractility via sympathetic activation and stimulation of C fibers, respectively. The reflex leads to vagal activation and/or withdrawal of sympathetic outflow, which causes a drop in cerebral perfusion and syncope.
Theoretically, in VVS, CNA works to prevent vagal efferent arm of reflex arc in cardioinhibitory type or in mixed type with a predominant cardioinhibitory response Figure 2.
Figure 2. Invasive treatment options based on pathophysiology of vasovagal syncope.
CLS, close-loop stimulation systems; CNA, cardioneuroablation; CPM, classical pacemakers; RDR, rate drop response pacemakers
Sinus node dysfunction
SND is most often related to age-dependent progressive fibrosis of the sinus nodal tissue and surrounding atrial myocardium 12. Because the sinus node is rich in both sympathetic and parasympathetic nerve innervations, both a vagal and a catecholamine component appeared to be important in selected patients 13. Furthermore, intranodal and even internodal conduction time may also prolong during vagal discharge. Therefore, the most important part of patient selection for CNA is discrimination of intrinsic SND from the vagal induced one. While the permanent forms of bradycardia are caused by an intrinsic disease of the sinus node, the etiology is usually unclear in intermittent forms and may result from variable contributions of intrinsic and extrinsic mechanisms 6.
Enhanced parasympathetic tone itself can be entirely physiologic and asymptomatic, as seen during sleep, in healthy and young individuals, but patients with sustained or frequent bradyarrhythmia are often symptomatic 14. The mechanism is quite similar with reflex syncope in the intermittent form. There is no precise minimum heart rate threshold to decide the need for treatment; therefore, establishing temporal correlation between symptoms and ECG is important when deciding on the necessity of treatment. Although a rest ECG is usually enough in the diagnosis of persistent bradycardia, longer-term ECG recordings by external or internal loop recorders should be preferred in diagnostic process due to the higher diagnostic yield than 24- or 48-hour Holter monitoring in paroxysmal cases. Potential contribution of abrupt heart rate slowing, and inadequate vascular response should be detected in these cases.
As an anti-muscarinic agent, response of atropine which accelerates both sinus node and atrial myocyte automaticity and increases the speed of atrioventricular conduction to confirm adequate sinus chronotropic response should be evaluated in all cases before decision of CNA. Atropine should be given intravenously with 0.04 mg/kg under continuous ECG recording for 15 min. A sinus rate increase of ≥25% or a sinus rate ≥90 bpm in the first 15 min after infusion should be considered as a positive response 15. In case of unresponsiveness, it should be accepted as an indicator for existence of intrinsic sinus node disease or sinus node-atrial conduction abnormality and as an exclusion criterion for CNA.
Theoretically, in SND, CNA migh be attempted before pacing in patients with symptomatic vagal induced sinus bradycardia or sinus arrest.
Atrioventricular block
The permanent forms of AVB are usually caused by an intrinsic disease of atrioventricular conduction system whereas determination of the etiology in paroxysmal AVB which indicates a sudden change from normal atrioventricular conduction to transient second- or third-degree AVB might be difficult. In vagal induced or functional AVB, the main cause of these episodes is parasympathetic influence on cardiac conduction 4. The other types of paroxysmal AVB are intrinsic and extrinsic idiopathic paroxysmal AVBs. In the intrinsic one which is also called as Phase must be 4 block or pause-dependent block, prolongation of the P-P interval or the long pause after atrial, His or ventricular premature complexes, or termination of supraventricular tachycardia can cause slow spontaneous depolarization of the diseased His-Purkinje system 16. The extrinsic one is characterized by paroxysmal AVB with long pauses, absence of cardiac and ECG abnormalities, and existence of low baseline endogenous adenosine values 17.
To select potential candidate for CNA, vagal induced paroxysmal AVB should be differentiated from the intrinsic and extrinsic ones. While intrinsic and extrinsic forms are usually characterized by recurrent syncope episodes with a duration of prodromal symptoms of ⩽5 s, vagal induced AVB is associated with well characterized prodromal symptoms prior to syncope which last longer than 5 s 13,18,19. In vagal induced AVB, a sinus node slowing before and during AVB is seen. As a main difference from phase 4 block, there is also a progressive PR prolongation before AVB episode. In extrinsic one, AVB occurs without P-P cycle lengthening or PR interval prolongation 17. In case of a negative holter despite existence of typical symptoms, external or internal loop recorders should be preferred to rule out the presence of paroxysmal AVB and to establish a symptom–rhythm correlation. In case of ongoing clinical suspicion, an electrophysiological study or an adenosine test may be used to exclude the diagnosis of intrinsic or extrinsic AVB, respectively.
In our recently published works, we demonstrated that hypervagatonia may still be the main underlying cause of AVB in some persistent cases 9,20. In case of persistent AVB, to differentiate the intrinsic from the extrinsic one, atropine challenge test might be useful 21. After demonstration of rhythm-symptom temporal correlation and complete recovery on atrioventricular conduction with atropine, CNA might be attempted in patients with symptomatic vagal induced AVB regardless of paroxysmal or persistent status.
Diagnostic tools to assess the type of vasovagal syncope for cardioneuroablation
Initial assessment of syncope includes history, physical examination, measurement of supine and standing blood pressure, and ECG, followed by additional diagnostic tests such as head-up tilt table test (HUT) and implantable loop recorder (ILR) if it is needed Figure 3.
Figure 3. Diagnostic and therapeutic steps for vasovagal syncope.
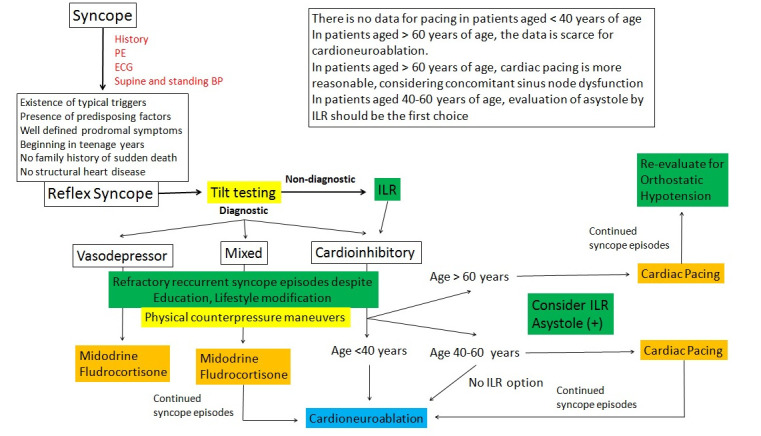
BP, blood pressure; H, history; ILR, implantable loop recorder; PE, physical examination;
Head-up tilt table test
As a frequently used method years passed, HUT enables the reproduction of VVS in a laboratory setting with a specificity of 92-94% Figure 4-22. Although the most common indication for HUT is to confirm a diagnosis of VVS in patients in whom this diagnosis has been suspected but not confirmed by the initial evaluation, HUT is recommended to define relative contributions of parasympathetic and sympathetic efferent arms in syncope episode in case of CNA. There are 3 types of response to tilting 23: (1) type 1 mixed: Heart rate falls at the time of syncope, but the ventricular rate does not fall to <40 beats/min , or falls to <40 beats/min for <10 s with or without asystole of <3 s.; (2) type 2A, cardioinhibition without asystole: Heart rate falls to a ventricular rate <40 beats/min for >10 s, but asystole of >3 s does not occur. Blood pressure falls before the heart rate falls; (3) type 2B, cardioinhibition with asystole: Asystole occurs for > 3 s. Heart rate fall coincides with or precedes blood pressure fall; (4) type 3 vasodepressor: Heart rate does not fall >10%, from its peak, at the time of syncope.
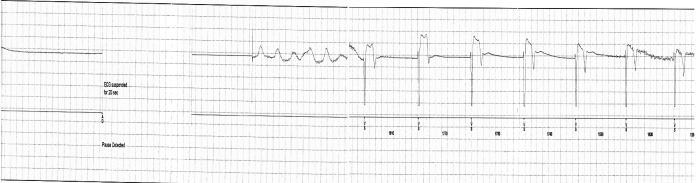
Figure 4. Hemodynamic results of head-up tilt table test before (A) and at 6th months of follow-up after cardioneuroablation (B).
Top trace shows the heart rate curve; bottom trace shows continuous blood pressure curves. Blood pressure stabilizes shortly after the assumption of the upright position with no changes for the duration of the preparatory phase; the heart rate immediately rises, then stabilizes. The vertical red line indicates the time of onset of the vasovagal reaction, which is characterized, at first, by a mild decrease in blood pressure with a steep fall in heart rate and syncope occurs. A. Arrows demonstrate a decrease on sympathetic tone and increase on parasympathetic tone before cardioneuroablation. B. After cardioneuroablation, vagal tone stays stable during tilting.
HR=heart rate; BP=blood pressure
In case of syncope reproduction with the hypotension and/or bradycardia/asystole, the test is accepted as positive. Despite this simple view of the test, its diagnostic performance depends significantly on several patient and methodological factors such as which protocol is used, whether and how a drug challenge is used, and low reproducibility. In our current approach, we prefer the Newcastle protocol which includes tilting to 70, a passive unmedicated phase of 20 minutes, if positivity/discontinuation criteria not reached, application of 300-400 μg sublingual nitroglycerine at the 20th minute and an additional 15-20 minutes of standing to select potential candidates for CNA 24. Despite well known limitations, clinical usage of HUT to select potential candidate for pacing was recently confirmed in double-blind, controlled SPAIN study 25. Patients with a cardioinhibitory HUT response (type 2A or type 2B) were included in the study and dual-chamber pacing with closed loop stimulation significantly reduced syncope burden.
Implantable loop recorder
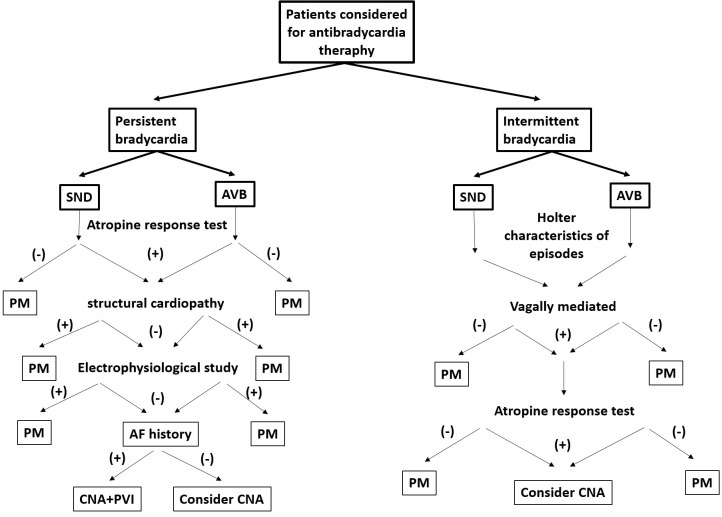
Despite a detailed screening of patients and often multidisciplinary investigation, more than one third of the patients may remain undiagnosed. By implanting a device subcutaneously, ILR documents the ECG findings of events either automatically with rate algorithms, or manually with magnet application to unravel the cause of unexplained syncope Figure 5-26. Because prolonged asystole was the most frequent finding at the time of syncope, pacing or potentially CNA was the specific therapy mostly used in the ILR population.
Figure 5. Tracing of implantable loop recorder.
Recording of an implantable loop recorder demonstrates an episode of prolonged asystole as a cause for the patient’s recurrent syncopal episodes. This patient underwent cardioneuroablation and the episodes of syncope and asystole resolved thereafter.
Applied selection criteria in the studies to date
As is mentioned by Dougles P. Zipes 27, altering the patient’s own body by catheter ablation of bradyarrhythmias to improve his or her health without implanting devices or leaving surgical footprints is a great achievement and, as long as the manipulation has no negative consequences, a preferred treatment approach. However, there are still some unknowns related CNA: (1) the best method to identify GPs; (2) the best ablation strategy; (3) complete or partial denervation; (4) the selection of suitable candidates. The first 3 question will be discussed in another topic of the current issue. So, we will try to summarize the last one. Because there were significant discrepancies between studies in terms of applied patient selection criteria and non-uniform distribution of selected cases, relevant literature will be divided into following groups: (1) CNA in patients with a combination of different conditions; (2) CNA in patients with pure VVS; (3) CNA in patients with pure SND. There is no study to investigate the role of CNA in patients with pure AVB.
CNA in patients with a combination of different conditions Table 1
Table 1. Published trials of cardioneuroablation in patients with a combination of different vagal induced bradyarrhythmia.
*In the original paper, results of 21 patients were presented. However, in methods section, the diagnoses were VVS in 6, AVB in 7, and SND in 13. As a possible explanation of this difference, there was overlapping of those conditions in some of the cases. The procedure had not been performed due to anatomical anomaly in 1 of 21 cases.
**All patients and 9 of 20 patients completed their 6 and 12-month follow-up, respectively. *** On Holter recordings, second degree AVB was detected in 3 of 12 VVS cases. §Patients who were referred permanent pacemaker implantation and had at least one syncope episode attributable to VVS, AVB, or SND were included in studies. In some of the cases, there was overlapping of these conditions. In such a situation, the most possible diagnosis for syncope occurrence was selected after a detailed history, ECG evaluation, and analysis of Holter recordings or HUT results. AVB, atrioventricular block; CI, cardioinhibitory; HUT, head-up tilt table test; M, mixed; NI, not indicated; SND, sinus node dysfunction; VVS, vosavagal syncope
| Trial | Pachon7 | Aksu8 | Rivarola45 | Debruyne46 | Aksu43§ | Aksu44§ | ||
|---|---|---|---|---|---|---|---|---|
| Age (years) | 47 ± 16 | 42 ± 14 | 34 ±13 | 41 ± 18 | 39 ±14 | 39 ±14 | ||
| Follow-up (months) | 9 ± 4 | 9 ± 3 | 22 ±11 | NI** | 9 ± 6 | 14 ±17 | ||
| VVS | 5* | 8 | 4 | 12 | 25 | 46 | ||
| Case number | SND | 7* | 7 | 1 | 8 | 15 | 8 | |
| AVB | 13* | 7 | 9 | 0*** | 9 | 11 | ||
| VVS | HUT | CI | CI or M | CI | CI or M | CI or M | CI or M | |
| Holter | + | + | + | + | + | + | ||
| Diagnostic tools | Exercise | + | + | + | + | + | + | |
| SND | HUT | + | - | + | +/- | - | - | |
| Holter | + | + | + | + | + | + | ||
| Exercise | + | + | + | + | + | + | ||
| AVB | HUT | + | - | + | NI | - | - | |
| Holter | + | + | + | NI | + | + | ||
| Exercise | + | + | + | NI | + | + | ||
| Pre-enrollment syncope burden (n) | VVS | NI | ≥3 | ≥3 (syncope or presyncope) | ≥2 or 1 with an injury or an accident | ≥3 | ≥3 | |
| SND | NI | ≥3 | NI | NI | ≥1 | ≥1 | ||
| AVB | NI | ≥3 | NI | NI | ≥3 | ≥3 | ||
| Atropine challenge test | All cases | SND and AVB | All cases | All cases | All cases |
CNA was first attempted by Pachon et al 8 in a mixed patient population consisting of VVS, SND, and AVB. As a main limitation, inclusion and exclusion criteria were rather vague in this study. Although demonstration of cardioinhibitory response on HUT was selected as the main inclusion criterion in VVS, pre-enrollment syncope burden was not indicated in the study. The patients demonstrating paroxysmal sinus bradycardia or AVB on 24-hour holter recordings were evaluated by exercise and atropine to exclude structural heart disease. All patients with vagal induced bradycardia were included in the study regardless of pre-enrollment symptom status.
Well defined selection criteria were applied by our group in a similar patient population and the efficacy of these criteria in this population was confirmed by following 2 studies 9,28,29. In VVS group, the major inclusion criterion was at least 3 syncope episodes accompanied by type 1 or type 2B response on HUT. Failure with conventional therapies consisting of optimal fluid intake and counterpressure maneuvers were demonstrated in all patients before enrollment. All AVB cases had at least one syncope episode and had documented functional second or third degree AVB episodes during the 12 months preceding enrollment. Differently, the patients with not only paroxysmal, but also with persistent AVB were included in the studies after demonstration of complete resolution of AVB by using atropine challenge and exercise tests. In SND, all patients had at least one syncope episode and had a documented pause >2 seconds on Holter recordings during the 12 months preceding enrollment.
Contrary to previous retrospective studies, effects of CNA in this mixed population were also prospectively studied by 2 groups although number of cases was small 30,31. In the first one, existence of at least 3 syncope episodes with HUT confirmed cardioinhibitory response was an inclusion criterion for VVS whereas ≥2 syncopal episodes in a lifetime or one syncopal episode complicated by an injury or an accident with cardioinhibitory or mixed response on HUT was accepted as inclusion criterion by Debruyne et al 31. A documented pause of ≥3 seconds during 24-hour Holter recording was an inclusion criterion for SND cases 30,31. Positive atropine response was confirmed in all cases before enrollment 31. Diagnosis of AVB referred to patients with episodes of >2 consecutive P waves blocked resulting in pauses >3 seconds during 24-hour Holter recording 30. Demonstration of symptom-bradycardia correlation was accepted enough for inclusion regardless of syncope status in cases with VVS or AVB 30,31.
CNA in patients with pure VVS Table 2
Table 2. Published trials of cardioneuroablation in patients with pure vasovagal syncope.
* Clinical assessments, 12-lead ECG, and 24-h Holter-monitor recordings were obtained at baseline and 1, 3, and 6 months after the ablation procedure in electroanatomic-mapping-guided CNA group. In combined approach group, the prospective follow-up consisted of a clinical evaluation (at discharge, 1 month, 3, 6, 12, and 24 months), ECG (at discharge, 1 month, 3, 6, 12, and 24 months), Holter monitoring (at discharge, 1 month, 3, 6, 12, and 24 months), and HUT (at 6 months and in case of symptoms).** Cardioinhibition with reproduction of symptoms occurred in all the patients. Patients with type 2 response or type 1 response in addition to important cardioinhibitory responses were included in the study.*** In one of cases of combined approach group, situational syncope was accompanied by VVS which was related with defecation. In one of the case of EAM-guided CNA group, paroxysmal atrial fibrillation episodes were detected on Holter recordings.HUT, head-up tilt table test; IQR, interquartile range; NI, not indicated; SD, Standard deviation
| Trial | Pachon47 | Yao48 | Sun49 | Hu50 | Aksu51 | |
|---|---|---|---|---|---|---|
| Age | 32 ± 15 | 50 ± 6 | 43 ±13 | 42 ± 17 | 36 ±12 | |
| Follow-up | 45 ± 22 | 30 ± 16 | 36 ±22 | 21 ± 13 | NI* | |
| Case number | 43 | 10 | 57 | 115 | 20 | |
| Type of vasovagal syncope | Type 1 | NI** | NI | NI | 74.8% | 20% |
| Type 2 | NI** | NI | NI | 11.3% | 80%*** | |
| Type 3 | excluded | NI | NI | 13.9% | excluded | |
| Diagnostic tool | HUT | + | + | + | + | + |
| Holter | + | + | + | + | + | |
| Exercise | + | - | - | - | + | |
| Counterpressure maneuvers | + | + | + | + | + | |
| Medication | NI | + | + | + | NI | |
| Mean±SD or median (IQR) syncope burden | 4 ± 2 | 6.5 (3-100) | 9 (4-15) | 6 ± 6 | 4 ± 1 | |
| Atropine challenge test | + | - | - | - | + |
Patient selection criteria were more clearly defined in these studies. In the first study consisting only of cases with VVS, the clinical efficiency of CNA was studied in 43 VVS cases by Pachon et al 32. Contrary to previous cohort of the same group, both cases with cardioinhibitory and mixed type responses on HUT were included in the study. Although mean pre-enrollment syncope burden was indicated as 4.7 ± 2, lower limit of syncope number required for inclusion were not reported. Then, Yao et al 33 reported their initial experience on 10 patients with highly symptomatic VVS. Although HUT was used for diagnosis of VVS, they did not specify subgroups of VVS in the text. Following 2 studies by same group investigated long-term efficacy and safety of CNA from the left atrium 34,35. In the first study, a total of 57 patients with ≥3 syncope episodes and failed conventional treatments including optimal fluid intake, physical counterpressure training, and pharmacological treatments were included in the study 34. The authors did not indicate the VASIS class of the syncopal episodes in this study. The largest study investigating effects of CNA in VVS included 115 patients and assessed the effects of CNA on heart rate 35. As a main difference from the previous cohorts, most participants in this study had a mixed (74.8%) HUT response. Surprisingly, patients with type 3 HUT response (13.9%) also demonstrated excellent benefit from CNA. In a recently published study, we defined a new GP detection method by using electrogram characteristics without using any additional equipment during electrophysiological study and compared this technique with a hybrid approach in which a combination of high-frequency stimulation, spectral analysis, and additional anatomical ablation 36. The major inclusion criterion is recurrent syncope episodes (at least three episodes in preceding 6 months) accompanied by type 1 or type 2B response HUT. There was no new syncopal episode in any patient at the end of six-month follow-up.
CNA in patients with pure SND
Potential usage of CNA in patients with pure SND was studied by same group in 2 cohort studies 37,38. In the first one, the efficacy and safety of CNA for treating the symptomatic long-standing sinus bradycardia were studied in patients younger than 60 years old. A total 11 patients presenting with symptomatic (dizziness, fatigue, and palpitation) sinus bradycardia for over 5 years detected by electrocardiography or Holter monitoring were included in the study 37. Existence of sinus pause >2s, no atropine response, and corrected sinus node recovery time (cSNRT) >525 ms were exclusion criteria. The patients were divided into 2 groups: under 50 years old and between 50 and 60 years old. Younger age was found related more increases in mean heart rate. In the second study, 62 patients were investigated to define age dependent effects of CNA by using similar clinical characteristics and exclusion criteria.
Although symptoms and quality of life improved in all patients, 5 of the 8 domains of the Medical Outcomes Study Short-Form 36 Health Survey did not show obvious improvements in older patients at 12 months 38.
Selection of Candidates for Cardioneuroablation Based on Supporting Evidence
Vasovagal syncope Figure 3
Nonpharmacological treatment, including education, lifestyle modification, and physical counterpressure maneuvers is the cornerstone of management of VVS patient and should be suggested in all cases before any interventional attempt. As is mentioned for cardiac pacing in syncope guidelines, CNA should be considered for patients with severe syncope forms, such as very frequent VVS affecting quality of life; recurrent syncope without prodromal symptoms, which exposes the patient to a risk of trauma; and syncope occurring during a high-risk activity in case of failure with nonpharmacological treatment 3,39. The current guidelines suggest that cardiac pacing should be considered in patients with frequent recurrent reflex syncope aged >40 years when bradycardia-syncope correlation was confirmed by ILR (class IIa) or HUT (class IIb). Although, in all cohorts related CNA, VVS cases were included in the study according to HUT results, we recently demonstrated that ILR may be used not only to select perfect candidates but also to evaluate absolute effectiveness of CNA 40. Therefore, similar diagnostic parameters might be applied for CNA to demonstrate symptom-ECG relationship with high level of evidence for HUT. Cardiac pacing is not suggested for patients with cardioinhibitory syncope under the age of 40 because these patients were not included in the studies demonstrating positive results, like ISSUE-3 and SUP 2 41,42. Thus, for CNA, it may be possible to make strong recommendations for subgroups of people of a young age and with the cardioinhibitory or mixed type of VVS Figure 5. Given considering low persistence of ablation effect after a year in patients >60 years of age by SND experience, decision of CNA should be considered after detailed discussion with the patient and family and CNA should be attempted in only patients who refused pacemaker implantation 37,38. Although not only patients with cardioinhibitory and mixed types but also patients with vasodepressor HUT response showed excellent benefit from CNA, evidence is still weak to suggest a clear mechanism to explain such an effect 34. Therefore, CNA should not be suggested in vasodepressor cases.
Sinus node dysfunction Figure 5
According to available evidence co-existence of following parameters might be applied to select potential candidates: symptomatic daytime sinus bradycardia or arrest when the correlation between symptoms and ECG is established; absence of structural cardiopathy exclusion of intrinsic sinus node dysfunction with positive atropine response (a sinus rate increase of ≥25% or a sinus rate ≥90 bpm with 0.04 mg/kg intravenous atropine sulfate); and age of ≤ 60 years old. Although corrected sinus node recovery time of >525 ms was used as an exclusion criterion in two sinus node dysfunction studies, our results demonstrated excellent success in this group, too 9,28,29.
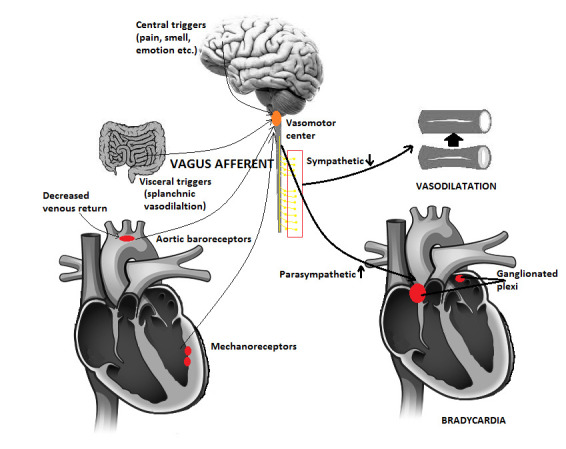
Atrioventricular block Figure 6
Figure 6. Therapeutic steps for clinical bradyarrhythmias based on the patient’s presentation.
AF, atrial fibrillation; AVB, atrioventricular block; CNA, cardioneuroablation; PM, pacemaker; PVI, pulmonary vein isolation; SND, sinus node dysfunction
Because the patients with AVB constitute the least group of patients where efficacy of CNA has been investigated, we cannot make definitive recommendations for this subgroup. However co-existence of following parameters might be applied to select potential candidates: existence of symptomatic AVB; demonstration of functional nature of AVB; absence of structural cardiopathy; in case of persistent AVB, demonstration of complete resolution of AVB by atropine challenge test; and age of ≤ 60 years old.
Looking to the future
CNA is still an emerging treatment modality and it should not be accepted the universal “one fits all solution” to treat patients with VMB. Although CNA seems promising to correct sinus rate and atrioventricular conduction properties, effects of the technique in non-heart rate related symptoms of vagal predominance such as dyspnea due to bronchospasm and gastrointestinal problems has been still unknown 43. Therefore, in addition to CNA, management of patients with autonomic nervous system dysregulation likely requires a multidisciplinary, multimodal and integrated care model to control all components of the polymorphic functional symptom complexes limiting life-quality and functionality irrespective of the presence of VMB.
Conclusions
CNA is a feasible and valuable adjunctive therapy in patients with VVS, vagal induced atrioventricular block and sinus node dysfunction. Because positive results of pacemaker implantation demonstrated a powerful placebo effect as well as an obvious direct effect on heart rate and select patients, one may wonder whether CNA would have a similar effect. Therefore, multicenter randomized-controlled trials between CNA and pacing and/or sham control studies may be required to investigate non-inferiority for efficiency and possible superiority for safety of the technique.
References
- 1.Aksu Tolga, Guler Tumer Erdem, Yalin Kivanc, Mutluer Ferit Onur, Ozcan Kazim Serhan, Calò Leonardo. Catheter Ablation of Bradyarrhythmia: From the Beginning to the Future. Am. J. Med. Sci. 2018 Mar;355 (3):252–265. doi: 10.1016/j.amjms.2017.11.016. [DOI] [PubMed] [Google Scholar]
- 2.Correction to: 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2019 Aug 20;140 (8):e506–e508. doi: 10.1161/CIR.0000000000000721. [DOI] [PubMed] [Google Scholar]
- 3.Brignole Michele, Moya Angel, de Lange Frederik J, Deharo Jean-Claude, Elliott Perry M, Fanciulli Alessandra, Fedorowski Artur, Furlan Raffaello, Kenny Rose Anne, Martín Alfonso, Probst Vincent, Reed Matthew J, Rice Ciara P, Sutton Richard, Ungar Andrea, van Dijk J Gert. 2018 ESC Guidelines for the diagnosis and management of syncope. Eur. Heart J. 2018 Jun 01;39 (21):1883–1948. doi: 10.1093/eurheartj/ehy037. [DOI] [PubMed] [Google Scholar]
- 4.Aksu Tolga, Guler Tumer Erdem, Bozyel Serdar, Yalin Kivanc. Potential usage of cardioneuroablation in vagally mediated functional atrioventricular block. SAGE open medicine. 2019;7 () doi: 10.1177/2050312119836308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brignole M, Menozzi C, Gianfranchi L, Oddone D, Lolli G, Bertulla A. Neurally mediated syncope detected by carotid sinus massage and head-up tilt test in sick sinus syndrome. Am. J. Cardiol. 1991 Oct 15;68 (10):1032–6. doi: 10.1016/0002-9149(91)90491-3. [DOI] [PubMed] [Google Scholar]
- 6.Brignole Michele, Auricchio Angelo, Baron-Esquivias Gonzalo, Bordachar Pierre, Boriani Giuseppe, Breithardt Ole-A, Cleland John, Deharo Jean-Claude, Delgado Victoria, Elliott Perry M, Gorenek Bulent, Israel Carsten W, Leclercq Christophe, Linde Cecilia, Mont Lluís, Padeletti Luigi, Sutton Richard, Vardas Panos E, Zamorano Jose Luis, Achenbach Stephan, Baumgartner Helmut, Bax Jeroen J, Bueno Héctor, Dean Veronica, Deaton Christi, Erol Cetin, Fagard Robert, Ferrari Roberto, Hasdai David, Hoes Arno W, Kirchhof Paulus, Knuuti Juhani, Kolh Philippe, Lancellotti Patrizio, Linhart Ales, Nihoyannopoulos Petros, Piepoli Massimo F, Ponikowski Piotr, Sirnes Per Anton, Tamargo Juan Luis, Tendera Michal, Torbicki Adam, Wijns William, Windecker Stephan, Kirchhof Paulus, Blomstrom-Lundqvist Carina, Badano Luigi P, Aliyev Farid, Bänsch Dietmar, Baumgartner Helmut, Bsata Walid, Buser Peter, Charron Philippe, Daubert Jean-Claude, Dobreanu Dan, Faerestrand Svein, Hasdai David, Hoes Arno W, Le Heuzey Jean-Yves, Mavrakis Hercules, McDonagh Theresa, Merino Jose Luis, Nawar Mostapha M, Nielsen Jens Cosedis, Pieske Burkert, Poposka Lidija, Ruschitzka Frank, Tendera Michal, Van Gelder Isabelle C, Wilson Carol M. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur. Heart J. 2013 Aug;34 (29):2281–329. doi: 10.1093/eurheartj/eht150. [DOI] [PubMed] [Google Scholar]
- 7.Hanna Peter, Rajendran Pradeep S, Ajijola Olujimi A, Vaseghi Marmar, Andrew Armour J, Ardell Jefrrey L, Shivkumar Kalyanam. Cardiac neuroanatomy - Imaging nerves to define functional control. Auton Neurosci. 2017 Nov;207 ():48–58. doi: 10.1016/j.autneu.2017.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chiou C W, Eble J N, Zipes D P. Efferent vagal innervation of the canine atria and sinus and atrioventricular nodes. The third fat pad. Circulation. 1997 Jun 03;95 (11):2573–84. doi: 10.1161/01.cir.95.11.2573. [DOI] [PubMed] [Google Scholar]
- 9.Pachon Jose C, Pachon Enrique I, Pachon Juan C, Lobo Tasso J, Pachon Maria Z, Vargas Remy N A, Jatene Adib D. "Cardioneuroablation"--new treatment for neurocardiogenic syncope, functional AV block and sinus dysfunction using catheter RF-ablation. Europace. 2005 Jan;7 (1):1–13. doi: 10.1016/j.eupc.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 10.Aksu Tolga, Golcuk Ebru, Yalin Kivanç, Guler Tümer Erdem, Erden Ismail. Simplified Cardioneuroablation in the Treatment of Reflex Syncope, Functional AV Block, and Sinus Node Dysfunction. Pacing Clin Electrophysiol. 2016 Jan;39 (1):42–53. doi: 10.1111/pace.12756. [DOI] [PubMed] [Google Scholar]
- 11.Hainsworth Roger. Pathophysiology of syncope. Clin. Auton. Res. 2004 Oct;14 Suppl 1 ():18–24. doi: 10.1007/s10286-004-1004-2. [DOI] [PubMed] [Google Scholar]
- 12.Desai J M, Scheinman M M, Strauss H C, Massie B, O'Young J. Electrophysiologic effects on combined autonomic blockade in patients with sinus node disease. Circulation. 1981 Apr;63 (4):953–60. doi: 10.1161/01.cir.63.4.953. [DOI] [PubMed] [Google Scholar]
- 13.Han Dan, Tan Hui, Sun Chaofeng, Li Guoliang. Dysfunctional Nav1.5 channels due to SCN5A mutations. Exp. Biol. Med. (Maywood) 2018 Jun;243 (10):852–863. doi: 10.1177/1535370218777972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.M Brodsky, D Wu, P Denes, C Kanakis, KM Rosen. Arrhythmias documented by 24 hour continuous electrocardiographic monitoring in 50 mate medical students without apparent heart disease. Am J Cardiol. 0;0:0–0. doi: 10.1016/s0002-9149(77)80094-5. [DOI] [PubMed] [Google Scholar]
- 15.Mandel W J, Hayakawa H, Allen H N, Danzig R, Kermaier A I. Assessment of sinus node function in patients with the sick sinus syndrome. Circulation. 1972 Oct;46 (4):761–9. doi: 10.1161/01.cir.46.4.761. [DOI] [PubMed] [Google Scholar]
- 16.Bansal Raghav, Mahajan Ankit, Rathi Chetan, Mehta Akshay, Lokhandwala Yash. What is the mechanism of paroxysmal atrioventricular block in a patient with recurrent syncope? Journal of arrhythmia. 2019 Dec;35 (6):870–872. doi: 10.1002/joa3.12245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brignole Michele, Deharo Jean-Claude, De Roy Luc, Menozzi Carlo, Blommaert Dominique, Dabiri Lara, Ruf Jean, Guieu Regis. Syncope due to idiopathic paroxysmal atrioventricular block: long-term follow-up of a distinct form of atrioventricular block. J. Am. Coll. Cardiol. 2011 Jul 05;58 (2):167–73. doi: 10.1016/j.jacc.2010.12.045. [DOI] [PubMed] [Google Scholar]
- 18.Calkins H, Shyr Y, Frumin H, Schork A, Morady F. The value of the clinical history in the differentiation of syncope due to ventricular tachycardia, atrioventricular block, and neurocardiogenic syncope. Am. J. Med. 1995 Apr;98 (4):365–73. doi: 10.1016/S0002-9343(99)80315-5. [DOI] [PubMed] [Google Scholar]
- 19.Brignole Michele, Deharo Jean-Claude, Guieu Regis. Syncope and Idiopathic (Paroxysmal) AV Block. Cardiol Clin. 2015 Aug;33 (3):441–7. doi: 10.1016/j.ccl.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 20.Aksu Tolga, Golcuk Sukriye Ebru, Erdem Guler Tümer, Yalin Kıvanç, Erden Ismail. Functional permanent 2:1 atrioventricular block treated with cardioneuroablation: Case report. HeartRhythm case reports. 2015 Mar;1 (2):58–61. doi: 10.1016/j.hrcr.2014.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aksu Tolga, Güler Tümer Erdem, Yalın Kıvanç. Step-by-Step Cardioneuroablation Approach in Two Patients with Functional Atrioventricular Block. Balkan Med J. 2019 Oct 28;36 (6):301–310. doi: 10.4274/balkanmedj.galenos.2019.2019.9.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moya Angel, Sutton Richard, Ammirati Fabrizio, Blanc Jean-Jacques, Brignole Michele, Dahm Johannes B, Deharo Jean-Claude, Gajek Jacek, Gjesdal Knut, Krahn Andrew, Massin Martial, Pepi Mauro, Pezawas Thomas, Ruiz Granell Ricardo, Sarasin Francois, Ungar Andrea, van Dijk J Gert, Walma Edmond P, Wieling Wouter. Guidelines for the diagnosis and management of syncope (version 2009). Eur. Heart J. 2009 Nov;30 (21):2631–71. doi: 10.1093/eurheartj/ehp298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brignole M, Menozzi C, Del Rosso A, Costa S, Gaggioli G, Bottoni N, Bartoli P, Sutton R. New classification of haemodynamics of vasovagal syncope: beyond the VASIS classification. Analysis of the pre-syncopal phase of the tilt test without and with nitroglycerin challenge. Vasovagal Syncope International Study. Europace. 2000 Jan;2 (1):66–76. doi: 10.1053/eupc.1999.0064. [DOI] [PubMed] [Google Scholar]
- 24.Parry S W, Reeve P, Lawson J, Shaw F E, Davison J, Norton M, Frearson R, Kerr S, Newton J L. The Newcastle protocols 2008: an update on head-up tilt table testing and the management of vasovagal syncope and related disorders. Heart. 2009 Mar;95 (5):416–20. doi: 10.1136/hrt.2007.136457. [DOI] [PubMed] [Google Scholar]
- 25.Baron-Esquivias Gonzalo, Morillo Carlos A, Moya-Mitjans Angel, Martinez-Alday Jesus, Ruiz-Granell Ricardo, Lacunza-Ruiz Javier, Garcia-Civera Roberto, Gutierrez-Carretero Encarnacion, Romero-Garrido Rafael. Dual-Chamber Pacing With Closed Loop Stimulation in Recurrent Reflex Vasovagal Syncope: The SPAIN Study. J. Am. Coll. Cardiol. 2017 Oct 03;70 (14):1720–1728. doi: 10.1016/j.jacc.2017.08.026. [DOI] [PubMed] [Google Scholar]
- 26.Brignole Michele, Sutton Richard, Menozzi Carlo, Garcia-Civera Roberto, Moya Angel, Wieling Wouter, Andresen Dietrich, Benditt David G, Grovale Nicoletta, De Santo Tiziana, Vardas Panos. Lack of correlation between the responses to tilt testing and adenosine triphosphate test and the mechanism of spontaneous neurally mediated syncope. Eur. Heart J. 2006 Sep;27 (18):2232–9. doi: 10.1093/eurheartj/ehl164. [DOI] [PubMed] [Google Scholar]
- 27.Zipes Douglas P. Ablation of Atrial Gangionated Plexi to Treat Symptomatic Sinus Bradycardia. JACC Clin Electrophysiol. 2017 Sep;3 (9):960–961. doi: 10.1016/j.jacep.2017.02.010. [DOI] [PubMed] [Google Scholar]
- 28.Aksu Tolga, Guler Tumer Erdem, Bozyel Serdar, Yalin Kivanc. Vagal responses during cardioneuroablation on different ganglionated plexi: Is there any role of ablation strategy? Int. J. Cardiol. 2020 Apr 01;304 ():50–55. doi: 10.1016/j.ijcard.2019.12.003. [DOI] [PubMed] [Google Scholar]
- 29.Aksu Tolga, Guler Tumer Erdem, Bozyel Serdar, Golcuk Sukriye Ebru, Yalin Kivanc, Lakkireddy Dhanunjaya, Gopinathannair Rakesh. Medium-term results of cardioneuroablation for clinical bradyarrhythmias and vasovagal syncope: effects on QT interval and heart rate. J Interv Card Electrophysiol. 2020 Feb 07; () doi: 10.1007/s10840-020-00704-2. [DOI] [PubMed] [Google Scholar]
- 30.Rivarola Esteban W, Hachul Denise, Wu Tan, Pisani Cristiano, Hardy Carina, Raimundi Fabrizio, Melo Sissy, Darrieux Francisco, Scanavacca Mauricio. Targets and End Points in Cardiac Autonomic Denervation Procedures. Circ Arrhythm Electrophysiol. 2017 Feb;10 (2) doi: 10.1161/CIRCEP.116.004638. [DOI] [PubMed] [Google Scholar]
- 31.Debruyne Philippe, Rossenbacker Tom, Collienne Christine, Roosen John, Ector Bavo, Janssens Luc, Charlier Filip, Vankelecom Bart, Dewilde Willem, Wijns William. Unifocal Right-Sided Ablation Treatment for Neurally Mediated Syncope and Functional Sinus Node Dysfunction Under Computed Tomographic Guidance. Circ Arrhythm Electrophysiol. 2018 Sep;11 (9) doi: 10.1161/CIRCEP.118.006604. [DOI] [PubMed] [Google Scholar]
- 32.Pachon Jose Carlos M, Pachon Enrique Indalecio M, Cunha Pachon Maria Zelia, Lobo Tasso Julio, Pachon Juan Carlos M, Santillana Tomas Guilhermo P. Catheter ablation of severe neurally meditated reflex (neurocardiogenic or vasovagal) syncope: cardioneuroablation long-term results. Europace. 2011 Sep;13 (9):1231–42. doi: 10.1093/europace/eur163. [DOI] [PubMed] [Google Scholar]
- 33.Yao Yan, Shi Rui, Wong Tom, Zheng Lihui, Chen Wensheng, Yang Long, Huang Wen, Bao Jingru, Zhang Shu. Endocardial autonomic denervation of the left atrium to treat vasovagal syncope: an early experience in humans. Circ Arrhythm Electrophysiol. 2012 Apr;5 (2):279–86. doi: 10.1161/CIRCEP.111.966465. [DOI] [PubMed] [Google Scholar]
- 34.Sun Wei, Zheng Lihui, Qiao Yu, Shi Rui, Hou Bingbo, Wu Lingmin, Guo Jinrui, Zhang Shu, Yao Yan. Catheter Ablation as a Treatment for Vasovagal Syncope: Long-Term Outcome of Endocardial Autonomic Modification of the Left Atrium. J Am Heart Assoc. 2016 Jul 08;5 (7) doi: 10.1161/JAHA.116.003471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hu Feng, Zheng Lihui, Liang Erpeng, Ding Ligang, Wu Lingmin, Chen Gang, Fan Xiaohan, Yao Yan. Right anterior ganglionated plexus: The primary target of cardioneuroablation? Heart Rhythm. 2019 Oct;16 (10):1545–1551. doi: 10.1016/j.hrthm.2019.07.018. [DOI] [PubMed] [Google Scholar]
- 36.Aksu Tolga, Guler Tumer Erdem, Mutluer Ferit Onur, Bozyel Serdar, Golcuk Sukriye Ebru, Yalin Kivanc. Electroanatomic-mapping-guided cardioneuroablation versus combined approach for vasovagal syncope: a cross-sectional observational study. J Interv Card Electrophysiol. 2019 Mar;54 (2):177–188. doi: 10.1007/s10840-018-0421-4. [DOI] [PubMed] [Google Scholar]
- 37.Zhao Liang, Jiang Weifeng, Zhou Li, Wang Yuanlong, Zhang Xiaodong, Wu Shaohui, Xu Kai, Liu Xu. Atrial autonomic denervation for the treatment of long-standing symptomatic sinus bradycardia in non-elderly patients. J Interv Card Electrophysiol. 2015 Aug;43 (2):151–9. doi: 10.1007/s10840-015-9981-8. [DOI] [PubMed] [Google Scholar]
- 38.Qin Mu, Zhang Yu, Liu Xu, Jiang Wei-Feng, Wu Shao-Hui, Po Sunny. Atrial Ganglionated Plexus Modification: A Novel Approach to Treat Symptomatic Sinus Bradycardia. JACC Clin Electrophysiol. 2017 Sep;3 (9):950–959. doi: 10.1016/j.jacep.2017.01.022. [DOI] [PubMed] [Google Scholar]
- 39.Correction to: 2017 ACC/AHA/HRS Guideline for the Evaluation and Management of Patients With Syncope: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2017 Oct 17;136 (16):e271–e272. doi: 10.1161/CIR.0000000000000537. [DOI] [PubMed] [Google Scholar]
- 40.Aksu Tolga, Guler Tumer E, Saygı Serkan, Yalin Kivanc. Usage of implantable loop recorder to evaluate absolute effectiveness of cardioneuroablation. J. Cardiovasc. Electrophysiol. 2019 Dec;30 (12):2986–2987. doi: 10.1111/jce.14243. [DOI] [PubMed] [Google Scholar]
- 41.Brignole Michele, Donateo Paolo, Tomaino Marco, Massa Riccardo, Iori Matteo, Beiras Xulio, Moya Angel, Kus Teresa, Deharo Jean Claude, Giuli Silvia, Gentili Alessandra, Sutton Richard. Benefit of pacemaker therapy in patients with presumed neurally mediated syncope and documented asystole is greater when tilt test is negative: an analysis from the third International Study on Syncope of Uncertain Etiology (ISSUE-3). Circ Arrhythm Electrophysiol. 2014 Feb;7 (1):10–6. doi: 10.1161/CIRCEP.113.001103. [DOI] [PubMed] [Google Scholar]
- 42.Brignole Michele, Arabia Francesco, Ammirati Fabrizio, Tomaino Marco, Quartieri Fabio, Rafanelli Martina, Del Rosso Attilio, Rita Vecchi Maria, Russo Vitantonio, Gaggioli Germano. Standardized algorithm for cardiac pacing in older patients affected by severe unpredictable reflex syncope: 3-year insights from the Syncope Unit Project 2 (SUP 2) study. Europace. 2016 Sep;18 (9):1427–33. doi: 10.1093/europace/euv343. [DOI] [PubMed] [Google Scholar]
- 43.Linz Dominik, Stavrakis Stavros. Cardioneuroablation for vagally mediated bradyarrhythmia: The universal one fits all solution? Int. J. Cardiol. 2020 Apr 01;304 ():45–46. doi: 10.1016/j.ijcard.2020.01.007. [DOI] [PubMed] [Google Scholar]