Abstract
There is an increasing number of people who convert to a plant-based diet. The desire for health benefits, including weight management, is often a contributing factor behind this dietary choice. The purpose of this review was to evaluate intervention studies assessing the effects of different plant-based diets on body mass index and weight. A literature search was conducted in PubMed until December 2019. Twenty-two publications from 19 studies were included. The majority of them were randomized controlled trials comparing a low-fat vegan diet to an omnivore diet in participants with overweight, type 2 diabetes mellitus and/or cardiovascular disease. All studies reported weight reductions, of which seven revealed significant differences, and four revealed non-significant differences between the intervention and the control groups. The results suggest that plant-based diets may improve weight status in some patient groups. Due to restrictions in fat intake in many studies, followed by reduced energy intake, the effects of the different interventions differ depending on the specific plant-based diets investigated. Future research should aim to include a representative study population and apply study diets without dietary restrictions.
Keywords: vegan diet, vegetarian diet, human nutrition, preventive nutrition, body weight, weight reduction
Introduction
Plant-based diets are mainly characterized by the elimination of all types of meat, including fish, occasionally with the elimination of other animal products like eggs and dairy. These diets are predominantly based on foods with plant origin, such as grains, legumes, root vegetables, vegetables, fruits, nuts and mushrooms.1 The main categories of plant-based diets are lacto-ovo-vegetarianism, lacto-vegetarianism, ovo-vegetarianism and veganism. Semi-vegetarianism, pescetarianism and flexitarianism can be regarded as subcategories of plant-based diets, and involve consumption of meat and/or fish to a greater or lesser extent.1 Of note, the term “plant-based” is used differently by people and has no specific definition. Definitions of diets associated with the term “plant-based” are presented in Table 1.
Table 1.
Classification of Various Types of Diets
| Diet | Definition |
|---|---|
| Vegan | Excludes all animal products |
| WFPB | Excludes heavily processed foods while focusing on foods in their most natural form |
| Raw vegan | Excludes all animal products, along with products that cannot be consumed uncooked or raw |
| Lacto-ovo-vegetarian | Excludes all forms of meat, but permits other animal products (dairy, eggs, honey etc.) |
| Lacto-vegetarian | Excludes all forms of meat and eggs, but permits dairy products, honey etc. |
| Ovo-vegetarian | Excludes all forms of meat and dairy products, but permits eggs, honey etc. |
| Pescatarian | Excludes meat, but permits fish, dairy products, eggs, honey etc. |
| Semi-vegetarian/flexitarian | Switches between vegetarian and meat-based diets; consists mainly of a vegetarian diet, with a minimal intake of meat |
| Omnivore | Does not exclude any animal products |
Abbreviation: WFPB, whole food plant-based.
Plant-based diets have existed since the beginning of mankind,2 however the interest in the topic has increased in the recent years and more research on health-related effects of different plant-based diets have recently been conducted.3,4 Animal welfare, as well as possible health benefits, such as weight management, are among the most common reasons for converting to a plant-based diet. Furthermore, ecological, economic and religious factors,1,4 along with an escalated global concern for the impact of animal food production on greenhouse-gas emissions, can explain some of the increased interest in plant-based diets.5
Together with the exclusion of meat, plant-based diets have been shown to lead to a reduced risk for development of cardiovascular disease, hypertension, diabetes, and certain cancer types.1,6,7 Overweight and obesity are the most important risk factors for mortality and morbidity in relation to these diseases.1,6 It is estimated that 2.7 billion people, equivalent to one-third of the world’s population, will be overweight or obese by 2025.8 Hence, there is a need to evaluate dietary strategies in the prevention and treatment of overweight and obesity.
Existing literature have suggested that weight loss can be achieved through a reduced intake of fat, which is a way of achieving an diet facilitating reduced energy intake.9 An observational study with more than 10,000 participants eating different diets, revealed that the participants who ate plant-based had a significantly lower intake of energy, total fat and saturated fat, compared to those who did not eat a plant-based diet.10 Thus, it may be assumed that a transition to a plant-based diet will result in reductions in weight. The aim of this review was to evaluate the effect of a plant-based diet intervention on body weight and BMI, by a systematic review of relevant publications.
Methods
The checklist and flowchart of the PRISMA (Preferred Reporting for Systematic Reviews and Meta-Analyses) guidelines were followed for this systematic review.
Search Strategy and Criteria for Inclusion
The primary outcomes of the current study were changes in body weight and/or BMI after a transition from a diet including meat to a plant-based diet, excluding meat. The term “plant-based diets” as used in the current review includes all diets excluding meat and fish, being both vegan and vegetarian diets. For clarification, the term vegetarian refers to lacto-ovo-vegetarian, lacto-vegetarian and ovo-vegetarian, while there was a distinction between vegetarian and vegan diets.
A literature search was conducted in PubMed until December 31st 2019, using the search combination “(plant based diet OR vegetarian OR vegan) AND (weight OR BMI)”. The results were limited by filters to studies on “humans”, “clinical trial” and “review”. The criteria for inclusion and exclusion are shown in Table 2.
Table 2.
Criteria for Inclusion and Exclusion in This Review
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Intervention studies (both RCTs, non-randomized and non-controlled studies) | Cohort studies, case-control studies, cross-sectional studies, pilot studies and meta-analyses |
| Outcomes that included changes in body weight and/or BMI | Outcomes that excluded changes in body weight and/or BMI |
| The absence of hypocaloric restrictions in both study groups | The application of hypocaloric restrictions in both study groups |
| A plant-based (vegetarian or vegan) intervention | An intervention that included meat or merely one plant protein source (ie almonds or soy) |
| A standard diet that included meat and virtually resembled the participants’ usual diet | A standard diet that excluded meat and did not resemble the participants’ usual diet |
| Duration of intervention ≥ 4 weeks | Duration of intervention < 4 weeks |
| Full-text available | Full-text non-available |
| Language: Norwegian or English | Other language than Norwegian and English |
| Adults (≥ 18 years) | Children (< 18 years) |
Abbreviations: RCT, randomized controlled trials; BMI, body mass index.
Results
Literature Search
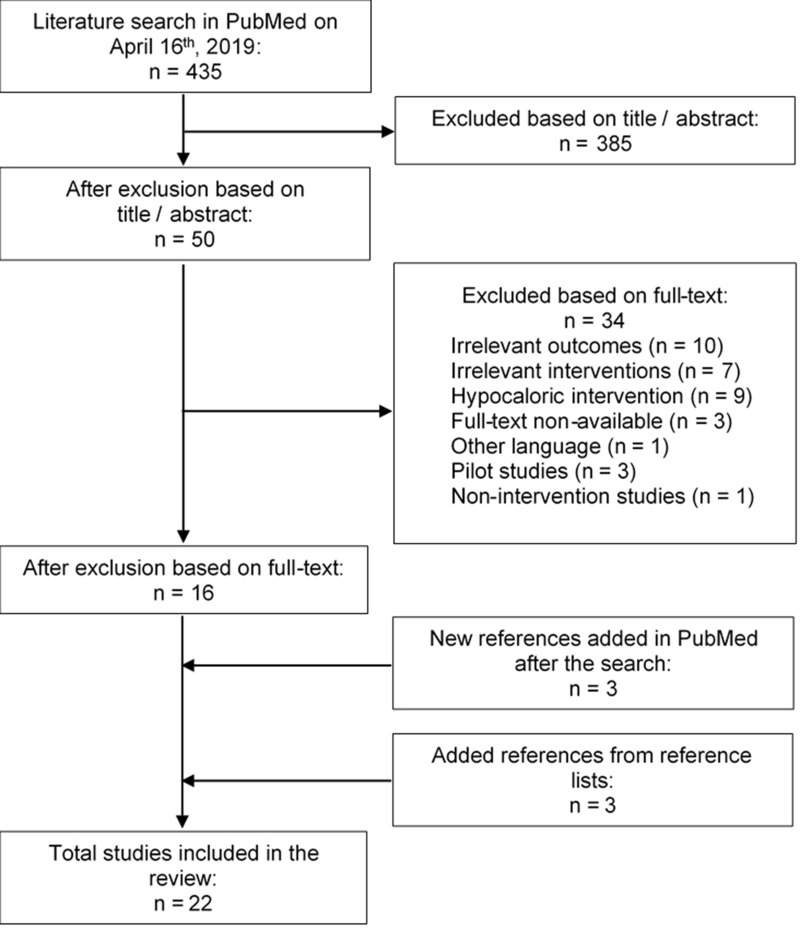
The search identified in total 435 articles, of which 22 publications were included in the review. The 22 publications reported results from a total of 19 different intervention studies. A flow diagram of the selection process is illustrated in Figure 1.
Figure 1.
A flow diagram of the selection progress in the review.
All included studies were intervention studies assessing the weight change occurring in a population undergoing a plant-based intervention diet for more than 4 weeks. This comprised studies that applied additional interventions besides the change of diet. The excluded studies were non-intervention studies, had irrelevant outcomes, used a hypocaloric intervention with the intention of catalyzing weight loss, or used an intervention diet that included meat and/or fish.
Study Characteristics
The included studies11,32 were published between 1991 and 2019, most of them in the US,11–14,16,21–23,25,27,29–31 of which multiple publications reported from the same studies.21–23,26,31 The majority of the articles were randomized controlled trials (RCTs), with the exception of three non-randomized16,18,20 and two non-controlled studies.19,27 Two RCTs had a crossover design11,28 while one randomized trial presented in two publications was five-armed.26,31 An overview of the included studies is shown in Table 3. In most of the studies, body weight was measured after an overnight fast with the participants wearing undergarments or light clothing.11,12,21–23,25,28,29,31,32 In multiple studies, the participants were encouraged not to make changes to their exercise routine during the entire study period12,14,16,22,23,25,28,30 or during a part of the study period.13
Table 3.
An Overview of the Studies Included in This Review
| First Author, Year Published, Country |
Study Design | n Participants (Completed) | Study Population | Intervention Diet | Standard Diet | Duration of Intervention |
|---|---|---|---|---|---|---|
| Barnard et al 200011 USA |
RCT crossover |
51 (35) | Premenopausal women | Low-fat vegetarian diet | Original diet with supplement pills (vitamin B12 or placebo) | 2 menstrual cycles |
| Barnard et al 200512 USA |
RCT | 64 (59) Intervention n=29 |
Overweight, postmenopausal women | Low-fat vegan diet | NCEP guidelines | 14 weeks |
| Barnard et al 200913 USA |
RCT | 99 Intervention n=49 |
Individuals with T2DM | Low-fat vegan diet with low GI | 2003 ADA guidelines (participants with a BMI >25 were prescribed energy intake deficits of 500–100 kcal) | 22 weeks and 74 weeks |
| Barnard et al 201814 USA |
RCT | 45 (40) Intervention n=21 |
Individuals with T2DM | Low-fat vegan diet with low GI | Portion-controlled eating plan with energy intake limits (500 kcal deficit/day) | 20 weeks |
| Elkan et al 200815 Sweden |
RCT | 68 Intervention n=38 |
Rheumatoid arthritis | A 1-day low-energy fast followed by a gluten-free vegan diet for 1 year | Well-balanced non-vegan diet | 1 year |
| Ferdowsian et al 201016 USA |
Non-randomized, controlled study, multi-center | 113 (109) Intervention n=68 |
Overweight and/or previous T2DM | Low-fat vegan diet | 22 weeks | |
| Jakse et al 201718 Slovenia |
Non-randomized, controlled study | 325 (325) Intervention n=241 |
Participants who wanted to be included after spontaneously attending an introductory lecture | Low-fat vegan diet supplemented with two daily meal replacements | Individuals who only wanted to attend the lectures and adjust their diet by their own judgment | 10 weeks |
| Johansson et al 199219 Sweden |
Non-controlled study | 20 | Normal weight, non-smoking | Lacto-vegetarian diet | 3 months | |
| Kaartinen et al 200020 Finland |
Non-randomized, controlled study | 28 Intervention n=18 |
Women with fibromyalgia (of which 66% were overweight) | Low-salt, raw vegan diet rich in lactobacteria | Omnivore diet | 3 months |
| Kahleova et al 201821 USA |
RCT single-center | 75 (72) Intervention n=38 |
Overweight | Low-fat, high-carbohydrate vegan diet | Current diet | 16 weeks |
| Kahleova et al 201822 USA |
RCT single-center | 75 (72) Intervention n=38 |
Overweight | Low-fat, high-carbohydrate vegan diet | Current diet | 16 weeks |
| Kjeldsen-Kragh et al 199124 Norway |
RCT | 53 (34) Intervention n=27 |
Rheumatoid arthritis | A 1-month health farm program consisting of 7–10 days of fast followed by a gluten-free vegan diet (3.5 months) and a lacto-ovo-vegetarian diet (9 months) | Omnivore diet | 13 months |
| Mishra et al 201325 USA |
RCT multi-center | 291 (211) Intervention n=142 (94) |
Overweight and/or T2DM | Low-fat vegan diet | Current diet | 18 weeks |
| Moore et al 201526 USA |
RCT five-armed | 63 (58) | Overweight | Low-fat diets with low GI: vegan (n=12), vegetarian (n=13), pesco-vegetarian (n=13), semi-vegetarian (n=13) or omnivore (n=12) | 2 months and 6 months | |
| Pischke et al 201927 USA |
Non-controlled study | 440 (333) | Non-smoking patients with coronary artery disease with or without diabetes mellitus (predominantly T2DM) | Low-fat plant-based diet, exercise, and stress management | 1 year | |
| Sofi et al 201928 Italy |
RCT crossover | 118 (100) | Overweight omnivores with a low-to-moderate cardiovascular risk profile | Low-calorie lacto-ovo-vegetarian diet | Low-calorie Mediterranean diet | 3 months x2 |
| Toobert et al 200029 USA |
RCT | 28 (25) Intervention n=undisclosed |
Postmenopausal women with cardiovascular disease | 1-week retreat with cooking and exercise classes, followed by a very low-fat vegetarian diet, stress management, exercise, group support and smoking cessation | «Usual care» | 1 week |
| Turner-McGrievy et al 200730 USA |
RCT | 62 (59) Intervention n=31 |
Overweight, postmenopausal women | Low-fat vegan diet | NCEP guidelines | 14 weeks |
| Turner-McGrievy et al 201531 USA |
RCT five-armed | 63 (50) | Overweight | Low-fat diets with low GI: vegan (n=12), vegetarian (n=13), pesco-vegetarian (n=13), semi-vegetarian (n=13) or omnivore (n=12) | 2 months and 6 months | |
| Wright et al 201732 New Zealand |
RCT single-center | 65 (49) Intervention n=33 |
Overweight or obesity and at least one of the following: T2DM, ischemic heart disease, hypertension or hypercholesterolemia | Low-fat WFPB diet | «Normal care» | 12 weeks |
Abbreviations: RCT, randomized controlled trials; T2DM, type 2 diabetes mellitus; GI, glycemic index; NCEP, National Cholesterol Education Program; ADA, American Diabetes Association; WFPB, whole-food plant-based diet.
The number of participants varied between 20 and 440, with the average age between 40 and 64 years. For a larger fraction of the studies, the study population was overweight or obese12,16,21–23,25,26,30–32 and/or had type 2 diabetes mellitus (T2DM).16,25,32 Otherwise, the criteria for the study populations were related to menopause,11,12,30 various types of cardiovascular disease and hypertension,28 only T2DM,13,14 rheumatoid arthritis,15,17,24 fibromyalgia20 or combinations of these conditions.27,29 Only one study included normal weight, clinically healthy participants.19 Most studies consisted predominantly of female participants, of which either all were women11,12,20,29,30 or had a percentage of female participants between 62% and 89%.16,17,22–26,31,32
Besides 1 five-armed trial presented in two different articles,26,31 the included studies compared a plant-based intervention diet and a standard omnivore diet. The larger part applied a low-fat vegan or vegetarian diet intervention, while the rest applied other plant-based variations.15,17,19,20,24,28,32 Some studies had an additional lifestyle alteration, including physical activity.27,29 The participants in the control group were either prescribed their present omnivore diet,11,15,17,20–25,29,32 a Mediterranean diet,28 or an omnivore diet based on guidelines from National Cholesterol Education Program (NCEP)30 or American Diabetes Association (ADA) 2003.13 The two latter were launched with the intent of diabetes control and reduction in cholesterol levels, respectively.33,34 The diet types applied in the included studies are listed in Table 3. The dietary intake, along with compliance and adherence, was evaluated in most studies. For instance, participants had to record their food intake,11–13,15,16,18,20–24,28,30 attend individual meetings, fill out surveys and answer unannounced phone calls from dieticians.11–14,16,17,19,21–23,25,26,28,31 The duration of intervention ranged between 10 weeks and one year, five of which had a follow-up period between 5 and 24 months.20,27,29,30,32
Main Findings
Eight of 22 articles revealed a significant reduction in body weight and/or BMI in the intervention group alone,11,16,20–23,25,32 of which three utilized the same data,21–23 and one was a non-randomized, controlled study.20 Nine other articles reported a significant greater reduction of the outcomes in the intervention groups compared with the control groups,12,15,17,18,24,26,29–31 of which six utilized the same data,17,24,26,31 and one was a non-randomized, controlled study.18 Among the 17 RCTs, seven demonstrated significant differences between the study groups,15,16,25,26,30–32 whereas one study reported non-significant differences favoring the plant-based intervention.12
Three of the RCTs operated with a standard diet with calorie restrictions, in addition to a plant-based diet that was either low-fat or low-calorie. All found significant weight reductions in both study groups. However, none reported significant differences between the groups.13,14,28 This review also included two non-controlled studies, which found significant weight reductions among all the participants.19,27 A summary of the outcomes and main findings is listed in Table 4.
Table 4.
A Summary of Relevant Outcomes and Main Findings in the Included Studies
| First Author, Publication Year, Country |
Primary Outcomes | Secondary Outcomes | Main Findings Related to Weight | Significance (P) | Mean Change in Weight Status (Body Weight in kg or BMI in kg/m2) |
|---|---|---|---|---|---|
| Barnard et al 200011 USA |
Serum total and LDL cholesterol concentrations | Weight | Reductions in weight and BMI. Participants who started the intervention first did not regain their original weight during the subsequent supplement phase. Changes in weight were associated with changes in energy intake | <0.001 | Intervention: −2,5 kg; −0,9 kg/m2 |
| Barnard et al 200512 USA |
Dietary intake, body weight and composition, resting metabolic rate, thermic effect of food, insulin sensitivity | Significant weight reduction in the vegan group, but no significant difference between the vegan and NCEP groups | =0.012 | Intervention: −5,8 kg ± 3.2 kg Control: −3,8 kg ± 2.8 kg |
|
| Barnard et al 200913 USA |
HbA1c, plasma lipids, weight | Sustained weight reductions in both the vegan and ADA groups, with no significant difference between the groups | =0.25 | Intervention: −4,4 kg (non-completers); −6,8 kg (completers) Control: −3,0 kg (non-completers); −4,9 kg (completers) |
|
| Barnard et al 201814 USA |
Body weight, HbA1c, plasma lipids, urinary albumin, BP | Weight reductions in both groups, with no significant difference between the groups | =0.10 for weight, =0.075 for BMI | Intervention: −6,3 kg; −2,3 kg/m2 Control: −4,4 kg; −1,5 kg/m2 |
|
| Elkan et al 200815 Sweden |
Blood lipids, oxLDL, anti-PC | BMI | Weight reductions in both groups, but the change was significant only in the intervention group | <0.001 | Intervention: −4,2 kg; −1,4 kg/m2 Control: −0,7 kg; −0,4 kg/m2 |
| Ferdowsian et al 201016 USA |
Changes in body weight, anthropometric measures, BP, lipid profile, dietary intake | Weight reductions only in the intervention group, the difference was significant between the groups. Sex, age, and changes in intake of total fat and fiber, were not significant predictors for weight loss | <0.001 | Intervention: −5,1 kg ± 0.6 kg; −2,0 kg/m2 Control: +0,1 kg ± 0.6 kg; −0 kg/m2 |
|
| Haugen et al 199317 Norway |
Nutritional status | Height, BMI, UAC, TSF | BMI was significantly lower in the intervention group compared with the control group | =0.04 | Intervention: −3.0 kg/m2 (among completers after 4 months) |
| Jakse et al 201718 Slovenia |
Body composition indices (body fat percentage, visceral fat, weight, muscle mass) | Significant reductions in weight and body fat with relative preservation of muscle mass | <0.001 | Intervention: −5,6 kg Control: −1,2 kg |
|
| Johansson et al 199219 Sweden |
Mutagenic activity in urine and feces | Weight | Mean weight reduction among the participants | <0.01 | Intervention: −2 kg |
| Kaartinen et al 200020 Finland |
VAS, joint stiffness, quality of sleep, questionnaires | BMI | Significant weight reductions in the intervention group. In the beginning of the study 66% of the participants were overweight. BMI in the intervention group was within normal values at the end of the study, and there was a clear increase after the intervention period | =0.0001 | Intervention: −4 kg/m2 Control: −0 kg/m2 |
| Kahleova et al 201821 USA |
Weight, body composition, insulin resistance | Reductions in weight and BMI only in the intervention group, which was associated with increased carbohydrate and fiber intake. The associations remained significant after adjustment for energy intake | <0.001 | Intervention: −6,5 kg; −2,0 kg/m2 Control: +0,57 kg |
|
| Kahleova et al 201822 USA |
Weight, body composition, insulin resistance | Reductions in weight and BMI only in the intervention group, which was associated with increased intake of plant protein | <0.001 | Intervention: −6,5 kg; −2,0 kg/m2 Control: +0,57 kg |
|
| Mishra et al 201325 USA |
Dietary intake, body weight, plasma lipids, BP, HbA1c | Weight reductions in the intervention group, with significant difference between the groups | <0.001 | Intervention: -2,9 kg (non-completers) -4,3 kg (completers) -1,04 kg/m2 (non-completers) -1,5 kg/m2 (completers) Control: -0,06 kg (non-completers) -0,08 kg (completers) -0,01 kg/m2 (non-completers) 0.02 kg/m2 (completers) |
|
| Moore et al 201526 USA |
Diet adherence, weight loss, changes in animal products intake by adherence status | Significantly greater weight loss among non-adherent vegan/vegetarian participants compared with non-adherent omnivore participants. However, there was no difference in weight loss among participants who adhered to their diet, regardless of the diet | =0.04 | Intervention: −6,0 ± 6.7% (non-adherent participants) Control: −0,4 ± 0.6% (non-adherent participants) |
|
| Pischke et al 201927 USA |
Medical characteristics (height, weight, percentage body fat, BP, angina pectoris, plasma lipids), lifestyle, quality of life | Significant weight reductions in all participants, regardless of sex and diabetic status | <0.001 | Intervention: −5 kg | |
| Sofi et al 201928 Italy |
Difference in body weight, BMI, and fat mass changes between the groups | Difference in cardiovascular risk parameters changes between the groups | Significant weight reductions in both groups, with no significant difference between the groups | Intervention: −1,88 kg; −0,64 kg/m2 Control: −1,77 kg; −0,67 kg/m2 |
|
| Toobert et al 200029 USA |
Changes in cardiovascular risk factors: lipid profile, BMI, BP, medications, quality of life | Significant reductions in BMI in the intervention group compared with the control group | =0.041 | Intervention: −3,9 kg (12 months); −1 kg/m2 (24 months) Control: −0,06 kg (12 months); −0 kg/m2 (24 months) |
|
| Turner-McGrievy et al 200730 USA |
Weight loss maintenance and diet adherence | Significantly greater weight reduction in the intervention group compared with the NCEP group after 1 and 2 years | <0.05 | Intervention: −4,9 kg (1 year); −3,1 kg (2 year) Control: −1,8 kg (1 year); −0,8 kg (2 year) |
|
| Turner-McGrievy et al 201531 USA |
Weight loss | Significantly greater weight loss in the vegan group compared to the pesco-vegetarian, semi-vegetarian and omnivore groups | <0.01 | −7,5% vegan -6,3% vegetarian -3,1% omnivore |
|
| Wright et al 201732 New Zealand |
BMI, cholesterol | Significant weight reductions in weight and BMI in the intervention group compared with the control group | <0.0001 | Intervention: -12,1 kg (6 months) -11,5 kg (12 months) -4,4 kg/m2 (6 months) -4,2 kg/m2 (12 months) |
Abbreviations: BMI, body mass index; HbA1c, glycated hemoglobin; oxLDL, oxidized low-density lipoprotein; anti-PC, anti-phosphorylcholine; ADA, American Diabetes Association; T2DM, type 2 diabetes mellitus; BP, blood pressure; UAC, upper arm circumference; TSF, triceps skin fold; VAS, visual analog scale; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein; WBC, white blood cells; NCEP, National Cholesterol Education Program; WFPB, whole-food plant-based.
Low-Fat Vegan or Vegetarian Diets
Of the included studies, thirteen studies investigated the impact of a low-fat vegan or vegetarian diet on weight status.11–14,16,18,21–23,25,26,30,31 The group of Barnard et al were responsible for four of these.11–14 One of their studies assessed the effect of a low-fat vegetarian diet in premenopausal women by conducting an RCT with a crossover design.11 The study revealed significant reductions in weight and BMI, and reported that the participants did not regain their initial weight when they resumed to the standard diet.11 Another RCT by Barnard et al concluded that a shift to a low-fat vegan diet resulted in significant weight loss among overweight postmenopausal women.12
The two other RCTs conducted by Barnard et al were the only studies in this review that prescribed energy deficits only in the control group, and not in the plant-based intervention group.13,14 One study concluded that a low-fat vegan diet and a diet based on ADA 2003 guidelines, the latter with specific energy intake restrictions for overweight participants, were associated with a persistent reduction in weight among individuals with T2DM.13 The last study found weight reductions among individuals with T2DM who had undergone a low-fat and low-glycemic vegan diet, and a portion-controlled standard diet, combined with weekly group lectures in a private clinic. No significant difference between the groups were observed.14
Kahleova et al conducted one RCT, with results reported in three different publications. These articles targeted the intake of carbohydrates, proteins, and fats, respectively, that resulted from a low-fat and high-carbohydrate vegan diet compared to a standard diet in overweight individuals.21–23 The first article found an increased intake of carbohydrates and fiber in the intervention group, which was associated with beneficial effects on body weight and fat mass.21 The second article reported a larger intake of plant proteins, along with a lower intake of animal proteins, which was associated with reductions in weight and fat mass.22 The third article concluded that a reduced intake of saturated and trans-fats, together with a relative increase in intake of polyunsaturated fats, was associated with a reduction in BMI and fat mass.23 Taken together, these results highlight several beneficial health effects in terms of weight management in response to a low-fat vegan diet.
In the study reported by Mishra et al, individuals with overweight and/or T2DM were recruited from an American insurance company (GEICO) and randomized to either a low-fat vegan diet or a standard diet. They observed significant improvements in body weight in the intervention group, but not in the control group.25 Similarly, Ferdowsian et al recruited GEICO employees with overweight and/or T2DM to the same types of diets and revealed that the average weight reduction was significantly higher in the intervention group than for the participants following a standard diet. Of note, this study was non-randomized.16
In a non-randomized trial conducted by Jakse et al, they incorporated a low-fat vegan diet supplemented with two daily meal replacements like milkshake or smoothie. The participants were allowed, but not encouraged, to consume meat once a week to relieve social pressure. The intervention was carried out ad libitum, meaning that the participants were permitted to eat to full satiety under free-living conditions. The study reported a significant reduction in both weight and body fat, with relative preservation of muscle mass.18
One of the two studies performed by Turner-McGrievy et al, investigated whether the diet criteria and weight were maintained one and two years after the intervention period, among postmenopausal women with overweight.30 Half of the participants in each study group were offered follow-up group meetings. All participants were encouraged to maintain their diet after the study period. The study demonstrated significant weight loss among participants who received follow-up, regardless of diet. Nevertheless, the intervention group had a significantly greater weight loss than the control group, regardless of their diet adherence.30
The randomized study presented in the publications by Turner-McGrievy31 and Moore26 et al was the exception where a plant-based diet was not compared to a standard omnivore diet. Rather, it compared four different types of low-fat and low-glycemic plant-based diets (vegan, vegetarian, pesco-vegetarian and semi-vegetarian), in addition to an omnivore diet. The aim was to evaluate the differences in weight loss31 and diet adherence26 in overweight individuals following these different diets. Although this implied a weight loss hypothesis, the references were included in the review due to the absence of hypocaloric modifications. Turner-McGrievy et al reported that vegan diets, followed by vegetarian diets, may result in greater weight loss than more modest diet types. The difference in body weight reduction between the vegan group and the other groups was significant after six months.31 Moore et al found no difference in diet adherence, nor did they find any difference in weight loss between participants who adhered to their prescribed diet. However, among participants who did not adhere to their prescribed diet, the weight loss was greater in vegan and vegetarian participants compared to participants who consumed fish or meat.26
Effect of Plant-Based Diets in Different Patient Groups
Kaartinen et al conducted a non-randomized, controlled intervention on the impact of a low-salt, raw vegan diet compared to an omnivore diet on fibromyalgia symptoms in Finnish women. In the beginning of the study, the majority of the participants were overweight, and there was no significant difference between the groups. In the end of the study, significant reductions in weight and BMI were found, with the average BMI being within normal range in the intervention group. There was an increase in BMI values in the intervention group after the study period, while BMI in the control group remained the same.20
The two publications from the Norwegian research group consisting of Kjeldsen-Kragh24 and Haugen17 et al were based on an RCT on patients with rheumatoid arthritis. The intervention started with 7–10 days of fasting, followed by a gluten-free vegan diet for 3.5 months. The first 4 weeks were located to a health farm. Finally, the participants underwent a vegetarian diet for 9 months. The study reported a significant reduction in BMI in the intervention group compared with the control group.17,24 A more simplified intervention, consisting of a gluten-free vegan diet, was carried out by the Swedish research group led by Elkan et al, the intervention seemed to induce a significant reduction in mean BMI in patients with rheumatoid arthritis. The weight change was non-significant in the control group.15
Vegetarian Diets in Clinically Healthy Individuals
Sofi et al conducted a randomized, controlled crossover trial on clinically healthy overweight Italians with a low-to-moderate cardiovascular risk profile.28 The study compared a vegetarian diet to a Mediterranean diet, with hypocaloric week plans given to the participants. Even though the calorie deficit contradicted the inclusion criteria in this review, the study was included as an exception, as the interventions were specified as low-calorie in nature and were isocaloric between them. Both diets were found to reduce weight, BMI, and fat mass equally, with non-significant differences between the groups.28
The non-controlled Swedish study published by Johansson et al was the only study in this review that included healthy normal weight participants. The participants’ mean body weight was reduced after the transition to a vegetarian diet.19
Low-Fat Plant-Based Diets with Stress Management and Exercise in Individuals with Cardiovascular Risk
Two studies managed a lifestyle trial consisting of low-fat plant-based diets, stress management and physical activity.27,29 Toobert et al conducted an RCT in postmenopausal women with cardiovascular risk, assessing changes in risk factors like BMI after implementing lifestyle changes. The intervention group underwent a 1-week retreat followed by group meetings twice a week, while the participants in the control group continued their current lifestyle. The study reported a significantly reduced BMI in the intervention group compared to the control group.29
Pischke et al on the other hand, conducted a non-controlled study in non-smoking participants with coronary artery disease, with or without diabetes mellitus (predominantly T2DM).27 The subjects with diabetes mellitus were classified into two groups based on the severity of their coronary artery disease, and compared with the subjects without diabetes mellitus. All participants underwent a lifestyle intervention consisting of a low-fat plant-based diet, stress management and physical activity, and all participants lost a significant amount of weight. The results were found to be regardless of sex and diabetic status.27
Whole-Food Plant-Based Diets in Individuals with High Cardiovascular Risk
The RCT carried out by Wright et al in New Zealand evaluated a whole-food plant-based (WFPB) diet in overweight patients with either T2DM, ischemic heart disease, hypertension, or hypercholesterolemia. This intervention was characterized by low-fat contents, and the participants could eat to full satiety. The study found a significantly improved BMI in the intervention group compared with the control group.32
Discussion
Primary Outcome
Overall, the results in this review suggest that a transition from an omnivore diet to a plant-based diet is associated with weight reduction in a majority of subjects, when applied in intervention studies. In multiple cases, there was a significant difference in weight loss between the plant-based group and the omnivore group, the former having reduced the most weight. This is consistent with findings from observational studies. One survey with 10,000 vegetarians and non-vegetarians demonstrated a significantly lower mean BMI among the vegetarians.10 The Adventist Health Study 2, including more than 60,000 participants, assessed discrepancies in BMI among people on different diets. The vegan group, followed by the vegetarian group, were found to have the lowest average BMI, whereas the omnivore group had the highest average value.35 These findings is supported by the findings in the EPIC-Oxford cohort study, concluding that during 5 years follow up, vegans and vegetarians showed overall a smaller weight gain than meat-eaters.36
Using BMI as a measure on weight status imposes some issues. A change in BMI does not necessarily imply changes in body fat mass, muscle mass, fluid or composition. Neither does it necessarily give information about weight change.37 Using BMI as a marker for adiposity may also contribute to underestimations of normal weight individuals with a high amount of adipose tissue.38 Nonetheless, BMI is a helpful and frequently used measure on weight and weight alterations in larger populations.38,39 Of note, a recent study reporting on effects of ad-libitum consumed low-fat plant-based diets supplemented with plant-based meal replacements on body composition, reported that low-fat plant based-diets eaten ad libitum enabled significant reduction of body fat and relative preservation of muscle mass.18 This suggests that a plant-based diet pose beneficial changes to body composition that might not be visible only by a BMI measure.
Mechanisms
Multiple studies reported lower intakes of protein, fat and cholesterol, along with higher intakes of fiber and carbohydrate, in the intervention group compared with the control group.11–14,16,17,19,21–23,25,30 Almost all operated with low-fat plant-based intervention diets. The findings correspond with studies that have reported an association between a reduced risk for overweight and diets high in plant protein. The association is in contrary to diets high in animal protein.38 The findings are also in accordance with observational studies and meta-analyses, which have described an association between a relatively low BMI and low-fat, high-carbohydrate diets,10 including plant-based diets.40 Plant-based diets are usually low in fats, particularly saturated fats,40 as a natural consequence of the elimination of animal products.41 Consequently, these diets are less energy dense than omnivore diets.21,23 Furthermore, higher intakes of fiber tend to result in increased satiety, reduced hunger, and therefore reduced intakes of energy.13,25 Previous studies have shown that a vegetarian diet itself results in reduced energy intakes compared with a diet that includes meat.10 In this review, reductions in energy intake were observed in the intervention groups in several controlled studies.12–14,16,21–23,25 Hence, the fact that a shift to a plant-based diet could have caused a lower intake of fat and a higher intake of fiber, leading to a lower intake of energy, increased thermic effect of the food and weight loss, cannot be ignored. In addition, beneficial effects of plant-based diets with a higher intake of plant-based proteins and a lower intake of animal proteins are suggested to include mechanisms related to improved gut-microbiota composition, reduced trimethylamine-N-oxide (TMAO) levels and improved insulin sensitivity.41
Effects of Different Plant-Based Diets
Most studies in this review applied a vegan diet, which complicates the differentiation in impact resulting from a vegan and a vegetarian diet. The studies conducted by Turner-McGrievy31 and Haugen17 et al were the only ones that assessed both diets. Both studies revealed a greater weight reduction on a low-fat and low-glycemic vegan diet,31 and a gluten-free vegan diet,17 respectively. Nevertheless, the difference between the vegan and vegetarian diets was non-significant.17,31 Similarly, meta-analyses have shown a missing significant difference in weight loss between studies applying a vegetarian diet, and studies applying a vegan diet.42 Of note, this may overall implicate a beneficial effect on body weight status due to a shift to a plant-based diet, regardless of the specific type of diet.
An Intention of Weight Loss
Several issues must be considered when interpreting the results. The interventions are substantially research specific and not necessarily typical for plant-based diets. Standard diets following NCEP or ADA guidelines, or low-calorie modifications, all used as control diets in the included studies, are designed for management of weight loss, cholesterol, and diabetes. Hence, the participants did not remain untreated. Studies comparing two weight management diets fail to address this issue, and do not give absolute numbers on weight change resulting from a diet shift.42 Furthermore, the intervention groups in half of the included studies in this review were prescribed low-fat or low-glycemic diets, based on an association between the actual modification and weight reduction,9,43 thus catalyzing weight loss.
Three of four studies demonstrating a non-significant difference in weight change between the intervention and control groups, were the only studies imposing calorie restrictions.13,14,28 Sofi et al did not inform of any object of weight loss. Still, the applied intervention and standard diets were low-calorie in nature and often clinically used with the purpose of reducing weight or cardiovascular risk.28 Barnard et al operated with low-fat intervention diets and energy-restricted standard diets.13,14 This only suggests that such diet modifications result in weight loss. It is rather difficult to conclude whether the weight reductions were caused by the actual plant-based diet, as some weight loss may be caused by other aspects of interventions, such as reduction in overall fat content.
Another issue is whether the included participants intended to lose weight, whether they were informed of the objective of the study, and if one of the inclusion criteria was, in fact, a purpose of weight loss. The latter was the case for multiple studies in this review.13,16,25,30,31 Many participants may be motivated by a desire to gain health-related benefits, such as weight reduction, and these probably have a greater tendency to succeed than the general population.
The motivation to proceed with a plant-based diet, as well as the types of foods consumed, tend to change with time in favor of a lower intake of animal products.2 This seems to be a strength of studies with long durations of intervention and/or follow-up and is probably related to an acquired increase in knowledge about the diet.2 Of note, although a change in diet could demonstrate a significant weight change initially and/or during the whole intervention period, more research is needed on the long-term effects of plant-based diets.6
Study Design and Study Population
Most of the studies in this review were RCTs, hence they were performed according to the gold standard for diet interventions. Crossover trials likely have increased strength. The studies with non-randomized or non-controlled designs, however, allowed participants to choose their preferred diet. These may have selection biases and false-positive findings, which complicates the conclusion about the weight reduction and the plant-based diet in the studies. Most likely, the weight changes demonstrate the impact of engaging in an intervention study, rather than the actual diet.
The majority of the studies were performed by the same research groups in an American population. The risk and prevalence of cardiovascular disease, overweight and T2DM is high in the US, potentially making the participants more aware of their health.28 Furthermore, the access to different foods, as well as the nutritional content in different products, vary from country to country. Thus, the results from an American study may not be applicable to other countries or populations. Furthermore, all the included studies were conducted in developed countries, which problematizes the application to developing countries. For instance, no difference was found in average BMI between vegetarians and non-vegetarians in a study with 7000 participants from India.40
Only one study, the one by Johansson et al, assessed weight change in clinically healthy and normal weight individuals.19 One of the studies conducted by Barnard et al were performed on allegedly healthy and normal weight women in their reproductive years.11 The effect of plant-based diets is therefore uncertain in this group. There is not sufficient evidence to tell whether normal weight individuals remain normal weight or become underweight when transiting to plant-based diets. Additionally, most studies in this review investigated older populations, mostly women, some excluding premenopausal women due to a potential hormonal effect on metabolic measures.12,30 As young women constitute a large part of people who eat plant-based,2,3 this complicates the conclusion.
Compliance and Confounding Factors
Studies that included exercise, stress management and smoking cessation18,27,29 ran a risk of having the results influenced by confounding factors. Studies that did not control for these factors16,18 thus have a limitation. Interventions that included health farms or retreats,17,24,29 weekly group meetings,14,27,29,30 and exercise classes27,29 are neither realistic nor feasible outside a study setting. Studies assessing the effects in free-living individuals, hereby having a more realistic approach, only demanded a report of food intake three days a week. Hence, they could not control completely for compliance. The results from these studies should be interpreted with caution.
Clinical Implication
There are numerous perceptions on plant-based diets, and the definitions are regularly modified, which makes it challenging to do consistent research within this topic.3 The only constant factor in plant-based diets is the absence of meat.7 However, studies have shown that although many people regard themselves as vegetarians, a larger part occasionally consume meat or fish.2 A plant-based diet could nonetheless be nutritionally inadequate. In some countries, meat substitutes could be based exclusively on one source, like soy. Thus, there may be large variations in the foods consumed, which may generate variations in the results and findings.44
Overall, data seems to suggest positive effects on weight in some patient groups after a shift to a plant-based diet, regardless of the strictness of the diet. Still, several studies have found that vegan and vegetarian diets reduce the body weight at least as much as calorie restricted diets, in addition to being easier to follow and maintain.11,14 The findings are particularly applicable considering the increasing prevalence of overweight and obesity,8 and their association with mortality and morbidity in relation to cardiovascular disease, diabetes, cancer, and musculoskeletal diseases. Consequently, a normal, but relatively low, BMI among vegans and vegetarians may be a protective factor.1,6
Conclusion
The results in this review propose that a shift to a plant-based diet may have beneficial health effects on body weight and BMI in individuals with overweight, T2DM, cardiovascular risk/disease and rheumatoid arthritis. The weight reduction can be explained by an increased intake of fiber, polyunsaturated fats and plant proteins, including a reduced intake of energy, saturated fats and animal proteins. Due to restrictions in fat intake in many studies, followed by reduced energy intake, the effects of the different interventions differ depending on the specific plant-based diets investigated. Hence, the observed effects can most likely not be attributed solely to a plant-based diet, but also the different nutrient composition and energy content in the different plant-based diets investigated.
Further research should aim for larger and more representative study populations in the form of normal weight and healthy individuals, including improvements in demographics. To quantify the effects of eliminating animal products with no other dietary changes, research designs would need to be chosen appropriately.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Pilis W, Stec K, Zych M, Pilis A. Health benefits and risk associated with adopting a vegetarian diet. Rocz Pantsw Zakl Hig. 2014;65(1):9–14. [PubMed] [Google Scholar]
- 2.Ruby MB. Vegetarianism. A blossoming field of study. Appetite. 2012;58(1):141–150. doi: 10.1016/j.appet.2011.09.019 [DOI] [PubMed] [Google Scholar]
- 3.Corrin T, Papadopoulos A. Understanding the attitudes and perceptions of vegetarian and plant-based diets to shape future health promotion programs. Appetite. 2017;109:40–47. [DOI] [PubMed] [Google Scholar]
- 4.Rosenfeld DL, Burrow AL. Vegetarian on purpose: understanding the motivations of plant-based dieters. Appetite. 2017;116:456–463. doi: 10.1016/j.appet.2017.05.039 [DOI] [PubMed] [Google Scholar]
- 5.Watts N, Amann M, Arnell N, et al. The 2019 report of The Lancet Countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet. 2019;394(10211):1836–1878. doi: 10.1016/S0140-6736(19)32596-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Craig WJ. Health effects of vegan diets. Am J Clin Nutr. 2009;89(5):1627–1633. doi: 10.3945/ajcn.2009.26736N [DOI] [PubMed] [Google Scholar]
- 7.McEvoy CT, Temple N, Woodside JV. Vegetarian diets, low-meat diets and health: a review. Public Health Nutr. 2012;15(12):2287–2294. doi: 10.1017/S1368980012000936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boseley S [Internet] Global cost of obesity-related illness to hit $1.2tn a year from 2025 2017. Guardian. Available from: https://www.theguardian.com/society/2017/oct/10/treating-obesity-related-illness-will-cost-12tn-a-year-from-2025-experts-warn. Accessed, 2020. [Google Scholar]
- 9.Ramage S, Farmer A, Eccles K, McCargar L. Healthy strategies for successful weight loss and weight maintenance: a systematic review. Appl Physiol Nutr Metab. 2014;39:1–20. doi: 10.1139/apnm-2013-0026 [DOI] [PubMed] [Google Scholar]
- 10.Kennedy ET, Bowman S, Spence J, Freedman M, King J. Popular diets: correlation to health, nutrition, and obesity. J Am Diet Assoc. 2001;101:411–420. doi: 10.1016/S0002-8223(01)00108-0 [DOI] [PubMed] [Google Scholar]
- 11.Barnard ND, Scialli AR, Bertron P, Hurlock D, Edmonds K, Talev L. Effectiveness of a low-fat vegetarian diet in altering serum lipids in healthy premenopausal women. Am J Cardiol. 2000;85(8):969–972. doi: 10.1016/S0002-9149(99)00911-X [DOI] [PubMed] [Google Scholar]
- 12.Barnard ND, Scialli AR, Turner-McGrievy G, Lanou AJ, Glass J. The effects of a low-fat, plant-based dietary intervention on body weight, metabolism, and insulin sensitivity. Am J Med. 2005;118(9):991–997. doi: 10.1016/j.amjmed.2005.03.039 [DOI] [PubMed] [Google Scholar]
- 13.Barnard ND, Cohen J, Jenkins DJ, et al. A low-fat vegan diet and a conventional diabetes diet in the treatment of type 2 diabetes: a randomized, controlled, 74-wk clinical trial. Am J Clin Nutr. 2009;89(5):1588–1596. doi: 10.3945/ajcn.2009.26736H [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barnard ND, Levin SM, Gloede L, Flores R. Turning the waiting room into a classroom: weekly classes using a vegan or a portion-controlled eating plan improve diabetes control in a randomized translational study. J Acad Nutr Diet. 2018;118(6):1072–1079. doi: 10.1016/j.jand.2017.11.017 [DOI] [PubMed] [Google Scholar]
- 15.Elkan AC, Sjoberg B, Kolsrud B, Ringertz B, Hafstrom I, Frostegard J. Gluten-free vegan diet induces decreased LDL and oxidized LDL levels and raised atheroprotective natural antibodies against phosphorylcholine in patients with rheumatoid arthritis: a randomized study. Arthritis Res Ther. 2008;10(2):R34. doi: 10.1186/ar2388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferdowsian HR, Barnard ND, Hoover VJ, et al. A multicomponent intervention reduces body weight and cardiovascular risk at a GEICO corporate site. Am J Health Promot. 2010;24(6):384–387. doi: 10.4278/ajhp.081027-QUAN-255 [DOI] [PubMed] [Google Scholar]
- 17.Haugen MA, Kjeldsen-Kragh J, Skakkebaek N, et al. The influence of fast and vegetarian diet on parameters of nutritional status in patients with rheumatoid arthritis. Clin Rheumatol. 1993;12(1):62–69. doi: 10.1007/BF02231561 [DOI] [PubMed] [Google Scholar]
- 18.Jakse B, Pinter S, Jakse B, Bucar Pajek M, Pajek J. Effects of an ad libitum consumed low-fat plant-based diet supplemented with plant-based meal replacements on body composition indices. Biomed Res Int. 2017;2017:9626390. doi: 10.1155/2017/9626390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johansson G, Holmen A, Persson L, et al. The effect of a shift from a mixed diet to a lacto-vegetarian diet on human urinary and fecal mutagenic activity. Carcinogenesis. 1992;13:153–157. doi: 10.1093/carcin/13.2.153 [DOI] [PubMed] [Google Scholar]
- 20.Kaartinen K, Lammi K, Hypen M, Nenonen M, Hanninen O, Rauma AL. Vegan diet alleviates fibromyalgia symptoms. Scand J Rheumatol. 2000;29(5):308–313. doi: 10.1080/030097400447697 [DOI] [PubMed] [Google Scholar]
- 21.Kahleova H, Dort S, Holubkov R, Barnard ND. A plant-based high-carbohydrate, low-fat diet in overweight individuals in a 16-week randomized clinical trial: the role of carbohydrates. Nutrients. 2018;10(9):1302. doi: 10.3390/nu10091302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kahleova H, Fleeman R, Hlozkova A, Holubkov R, Barnard ND. A plant-based diet in overweight individuals in a 16-week randomized clinical trial: metabolic benefits of plant protein. Nutr Diabetes. 2018;8(1):58. doi: 10.1038/s41387-018-0067-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kahleova H, Hlozkova A, Fleeman R, Fletcher K, Holubkov R, Barnard N. Fat quantity and quality, as part of a low-fat, vegan diet, are associated with changes in body composition, insulin resistance, and insulin secretion. a 16-week randomized controlled trial. Nutrients. 2019;11:615. doi: 10.3390/nu11030615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kjeldsen-Kragh J, Haugen M, Borchgrevink CF, et al. Controlled trial of fasting and one-year vegetarian diet in rheumatoid arthritis. Lancet. 1991;338:899–902. doi: 10.1016/0140-6736(91)91770-U [DOI] [PubMed] [Google Scholar]
- 25.Mishra S, Xu J, Agarwal U, Gonzales J, Levin S, Barnard ND. A multicenter randomized controlled trial of a plant-based nutrition program to reduce body weight and cardiovascular risk in the corporate setting: the GEICO study. Eur J Clin Nutr. 2013;67(7):718–724. doi: 10.1038/ejcn.2013.92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moore WJ, McGrievy ME, Turner-McGrievy GM. Dietary adherence and acceptability of five different diets, including vegan and vegetarian diets, for weight loss: the New DIETs study. Eat Behav. 2015;19:33–38. doi: 10.1016/j.eatbeh.2015.06.011 [DOI] [PubMed] [Google Scholar]
- 27.Pischke CR, Weidner G, Elliott-Eller M, et al. Comparison of coronary risk factors and quality of life in coronary artery disease patients with versus without diabetes mellitus. Am J Cardiol. 2006;97(9):1267–1273. doi: 10.1016/j.amjcard.2005.11.051 [DOI] [PubMed] [Google Scholar]
- 28.Sofi F, Dinu M, Pagliai G, et al. Low-calorie vegetarian versus mediterranean diets for reducing body weight and improving cardiovascular risk profile: cardiveg study (cardiovascular prevention with vegetarian diet). Circulation. 2018;137:1103–1113. doi: 10.1161/CIRCULATIONAHA.117.030088 [DOI] [PubMed] [Google Scholar]
- 29.Toobert DJ, Glasgow RE, Radcliffe JL. Physiologic and related behavioral outcomes from the Women’s Lifestyle Heart Trial. Ann Behav Med. 2000;22(1):1–9. doi: 10.1007/BF02895162 [DOI] [PubMed] [Google Scholar]
- 30.Turner-McGrievy GM, Barnard ND, Scialli AR. A two-year randomized weight loss trial comparing a vegan diet to a more moderate low-fat diet. Obesity. 2007;15(9):2276–2281. doi: 10.1038/oby.2007.270 [DOI] [PubMed] [Google Scholar]
- 31.Turner-McGrievy GM, Davidson CR, Wingard EE, Wilcox S, Frongillo EA. Comparative effectiveness of plant-based diets for weight loss: a randomized controlled trial of five different diets. Nutrition. 2015;31(2):350–358. doi: 10.1016/j.nut.2014.09.002 [DOI] [PubMed] [Google Scholar]
- 32.Wright N, Wilson L, Smith M, Duncan B, McHugh P. The BROAD study: A randomised controlled trial using a whole food plant-based diet in the community for obesity, ischaemic heart disease or diabetes. Nutr Diabetes. 2017;7(3):e256. doi: 10.1038/nutd.2017.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Executive summary of the third report of the national cholesterol education program (NCEP). JAMA. 2001;285(19):2486–2497. doi: 10.1001/jama.285.19.2486 [DOI] [PubMed] [Google Scholar]
- 34.Franz M, Bantle J, Beepe C, Brunzell J, Chiasson J, Garg A. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diab Care. 2003;26(suppl 1):51–61. [DOI] [PubMed] [Google Scholar]
- 35.Tonstad S, Butler T, Yan R, Fraser GE. Type of vegetarian diet, body weight, and prevalence of type 2 diabetes. Diab Care. 2009;32:791–796. doi: 10.2337/dc08-1886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosell M, Appleby P, Spencer E, Key T. Weight gain over 5 years in 21,966 meat-eating, fish-eating, vegetarian, and vegan men and women in EPIC-Oxford. Int J Obes. 2006;30(9):1389–1396. doi: 10.1038/sj.ijo.0803305 [DOI] [PubMed] [Google Scholar]
- 37.Andreoli A, Garaci F, Cafarelli FP, Guglielmi G. Body composition in clinical practice. Eur J Radiol. 2016;85(8):1461–1468. doi: 10.1016/j.ejrad.2016.02.005 [DOI] [PubMed] [Google Scholar]
- 38.Navas-Carretero S, San-Cristobal R, Livingstone KM, et al. Higher vegetable protein consumption, assessed by an isoenergetic macronutrient exchange model, is associated with a lower presence of overweight and obesity in the web-based Food4me European study. Int J Food Sci Nutr. 2019;70(2):240–253. doi: 10.1080/09637486.2018.1492524 [DOI] [PubMed] [Google Scholar]
- 39.Muller MJ, Braun W, Enderle J, Bosy-Westphal A. Beyond BMI: conceptual issues related to overweight and obese patients. Obes Facts. 2016;9:193–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Clarys P, Deliens T, Huybrechts I, et al. Comparison of nutritional quality of the vegan, vegetarian, semi-vegetarian, pesco-vegetarian and omnivorous diet. Nutrients. 2014;6(3):1318. doi: 10.3390/nu6031318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Najjar RS, Feresin RG. Plant-based diets in the reduction of body fat: physiological effects and biochemical insights. Nutrients. 2019;11(11):2712. doi: 10.3390/nu11112712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Appleby PN, Key TJ. The long-term health of vegetarians and vegans. Proc Nutr Soc. 2016;75(3):287–293. doi: 10.1017/S0029665115004334 [DOI] [PubMed] [Google Scholar]
- 43.Barnard ND, Levin SM, Yokoyama Y. A systematic review and meta-analysis of changes in body weight in clinical trials of vegetarian diets. J Acad Nutr Diet. 2015;115(6):954–969. [DOI] [PubMed] [Google Scholar]
- 44.Hooper L, Abdelhamid A, Bunn D, Brown T, Summerbell C, Skeaff CM. Effects of total fat intake on body weight. Cochrane Database Syst Rev. 2015;(8):CD011834. [DOI] [PMC free article] [PubMed] [Google Scholar]