Abstract
Background
Coronaviruses are a large family of viruses that cause a wide range of illness from the common cold to more severe diseases. The COVID-19 pandemic is a public emergency of international concern that affects several nations. The widespread outbreak of COVID-19 virus has brought not only the risk of death but also major psychological pressure. However, the psychological impact on university students has not been studied in Ethiopia.
Objective
To assess the psychological impacts of COVID-19 pandemic among university students in Bench-Sheko Zone, South-west, Ethiopia, 2020.
Methods
A community-based cross-sectional study was conducted from May 15 to June 15/2020. A systematic sampling technique was employed to select the study participants. The data were entered into EpiData 3.1 and exported to SPSS version 24 for analysis. Bivariate and multivariable logistic regression were used to identify candidates and independent factors respectively. Independent factors of depression, anxiety, and stress were assessed using AORs with 95% confidence level at P-value <0.05 cut point.
Results
Three hundred and twenty-two university students were included with a 97.5% response rate. The prevalence of depression, anxiety, and stress was 21.2%, 27.7%, and 32.5%, respectively. Being female, staying at home, history of medical illness, and poor and moderate social support increased the risk of depression. Not living with their parents, relatives got coronavirus and low family income were risk factors for anxiety. Moreover, substance use, depression, anxiety, and poor social support were increasing the risk of stress among university students.
Conclusions and Recommendations
This study revealed a higher prevalence of depression, anxiety, and stress among university students. Thus, governments and policy makers should develop health system strategies to provide crisis-oriented psychological services for university students to minimize the mental health impact of the outbreak.
Keywords: psychology, COVID-19, impact, coronavirus
Introduction
Coronaviruses are a large family of viruses that are known to cause a wide range of illness from the common cold to more severe diseases such as Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS). They are often zoonotic and several known coronaviruses are circulating in animals that have not yet infected humans. A novel coronavirus (COVID-19) is a new strain of coronavirus that has not been previously identified in humans.1
The novel corona virus (COVID-19) outbreak, which was first detected in Wuhan, China, in December 2019, has been evolving rapidly. On 30 January 2020, the WHO Director-general declared that the current outbreak constituted a public health emergency of international concern, and on 12 March 2020 the COVID-19 the outbreak was declared a pandemic.2
Worldwide, until July 24, 2020, over 15.5 million confirmed cases, about 9.5 million recovered, and more than 650,000 confirmed deaths were reported.3 In Africa, over 750,000 were confirmed cases, nearly 450,000 recovered, and 6500 deaths were reported. The most affected countries are: South Africa, Egypt, Nigeria Ghana, Algeria, and Morocco, together, these countries account for 75% of the cases reported in the region.4 Ethiopia reported a confirmed case of novel coronavirus for the first time on April 2, 2020. Until July 24, 2020, 11,939 confirmed cases, 5645 recoveries, and 197 deaths were reported. Currently, Ethiopia is under a state of emergency declared to fight the coronavirus (COVID-19) pandemic.5
Moreover COVID-19 has negative mental and social consequences, for example, a broad body of research links social isolation and loneliness to poor mental health; and recent data shows that significantly higher share of people who were sheltering in place (47%) reported negative mental health effects resulting from worry or stress related to coronavirus than among those not sheltering in place (37%). Negative mental health effects due to social isolation may be particularly pronounced among older adults and households with adolescents, as these groups are already at risk for depression or suicidal ideation.6
The widespread outbreaks of infectious diseases, such as COVID-19 are associated with psychological distress and symptoms of mental illness.7 A study conducted in China during the initial outbreak of COVID-19 found that 53.8% of rated psychological impact of the outbreak, 16.5% reported moderate to severe depression, 28.8% reported moderate to severe anxiety and 8.1% reported moderate to severe stress level.8 A review of existing literature revealed that that symptoms of anxiety and depression (16 to 28%) and self-reported stress (8%) are common psychological reactions to the COVID-19 pandemic.9
The continuous spread of novel coronavirus (COVID-19), strict isolation measures, and delays in starting school, colleges and universities across the country is expected to influence the mental health of university students. Despite its mental health impacts, no detailed study on the psychological impacts of university students facing the epidemic has been conducted. Therefore, this study aims to show the psychological impact of COVID-19 outbreak and its associated factors among university students in the Bench-Sheko zone. The finding of this will help as baseline data for policy makers and programmers to develop mental health programs for individuals during the outbreak.
Methods and Materials
Study Setting, Design, and Period
A community based cross-sectional study was conducted in the Bench-Sheko zone of south-west Ethiopia, from May 15 to June 15, 2020. The administrative center of Bench Sheko is Mizan Aman Zone located 582 km from Addis Ababa. The zone has a total of two administrative towns and six woredas (third-level administrative districts). According to the zonal statistics office, the total population of the Bench-Sheko zone is 681,549. According to zonal youth and women affairs and zonal education bureau, the zone has a total of 1350 university students that attend their education in different Ethiopian universities.
Source Population
All university students who live in the Bench-Sheko zone.
Study Population
All university students who live in the Bench-Sheko zone who fully fill the inclusion criteria.
Eligibility Criteria
All systematically selected university students who live in Bench-Sheko zone were included in the study. Students with severe mental illness and hearing difficulties were excluded.
Sample Size Determination and Sampling Technique
The sample size for both objectives was determined by using a single population proportion formula. Since there was no research done about psychological impact towards COVID-19 and its associated factors among university students in Africa including Ethiopia, we took 50% to determine the sample size.
 |
Where; n=sample size
Z=reliability coefficient with 95% confidence level=1.96
P=population variance available from previous data (q=1-p)
d=degree of precision or margin of error=0.05
 |
With 10% nonresponse rate, the sample size became 422. Since the total university students on average 1350 which is less than 10,000 we had to consider the correction formula, n final=n/1+n/N, then the final sample size became 322.
Sampling Technique and Procedure
Systematic random sampling technique was used to select all 322 samples. The list of all accessible university students with their phone number was collected from zonal education bureau and Bench-Sheko Zone Youth and Women Affairs. We calculated the skip interval, k=4. The first study subject was selected using lottery method. We selected the student every fourth interval starting from the student registered at third place. Since the government announced a state of emergency due to the COVID-19 pandemic, students were interviewed via phone calls.
Study Variables
The dependent variables were psychological impacts (depression, anxiety, and stress), while the independent variables were sociodemographic variables (age, sex, residence, religion, and ethnicity, family income, and living with parents) and clinical factors (history of medical illness, relatives got COVID) and substance use were the independent variables.
Measures and Operational Definitions
Depression: A score of 10 and above in DASS-D indicates the presence of depression.10
Anxiety: A score of eight and above in DASS-A indicates the presence of anxiety.10
Stress: A score of 15 and above in DASS-S indicates the presence of stress.10
Social support: Oslothree-item social support scale, it is a three-item questionnaire, the sum score scale ranging from 3–14, which has three categories: poor support 3–8, moderate support 9–11 and strong support 12–14.11
Substance use: use of chat, alcohol, cigarette smoking, or others at least once in the last three months.
Data Collection Procedures and Tools
The data were collected using a structured interviewer-administered questionnaire through a phone call to assess sociodemographic, clinical factors, and psychological impacts of the COVID-19 pandemic. Data on psychological impacts of COVID-19 were collected using depression, anxiety, and stress (DASS). DASS is cross-culturally validated tool to assess psychological impacts of pandemic disease. A number of items are 21 items and three subscales. Anxiety subscale (DASS-A), depression subscale (DASS-D), and stress subscale (DASS-S). There are seven depression items measuring cognitive and emotional aspects of depression, predominantly anhedonia; seven anxiety items focused on cognitive and emotional aspects of anxiety; and seven items assess stress.
The data collectors and supervisors were nurses who work in Mizan Tepi University Teaching Hospital. There were three data collectors, a supervisor, and the overall activities were supervised by the principal investigator. Training was given to the data collectors and supervisors by the principal investigator on the objective of the study, maintenance of ethical standards, the methods of data collection, and data collectors were familiarized with data collection tools with respect to the study with practical exercises. A supervisor checked the completeness of the collected data daily.
Data Quality Assurance
Data completeness was checked manually before being entered into EpiData 3.1 and necessary correction was made. The questionnaire was prepared in English and translated into local language, Amharic, and back-translated to English to assess consistency. Training was given to the data collectors and supervisors on the objective of the study, maintenance of ethical standards, and methods of data collection. Data coding and cleaning was performed by cross-checking the printout data for possible errors. The missing values and outliers were checked before analysis by running a descriptive analysis.
Data Analysis Procedures
The data were entered into EpiData 3.1 and exported to SPSS Version 24 for analysis. After data coding and cleaning were performed, descriptive statistics were presented in frequency, tables and graphs. Normality assumption was checked for continuous variables. The association between depression, anxiety, and stress with each covariate was assessed first with bivariate logistic regression to identify a candidate variable for multivariate logistic regression. Variables with a P-value <0.25 were taken into multiple logistic regression analysis to identify independent predictors of depression, anxiety, and stress.
Backward likelihood ratio with 0.1 probability of removal was used to develop the model. Goodness of fit of the final model was checked using Hosmer–Lemeshow test of goodness of fit considering good fit at P-value >0.05. Finally, independent predictors of depression, anxiety and stress were declared at P-value <0.05 cutoff point and strength of the association was assessed using AORs with their corresponding at 95% confidence level.
Ethical Statement
The research was approved by the Institutional Review Board (IRB) of Mizan-Tepi University and ethical clearance was obtained. In addition, support letters were written to Bench-Sheko zone. The objective and purpose of the study were verified briefly to the study participant and confidentiality was assured. Finally, oral consent was obtained from study participants before conducting the interview. This study was conducted in accordance with the Declaration of Helsinki.
Results
Sociodemographic Characteristics
A total of 322 university students who were living in the Bench-Sheko zone were interviewed with a response rate of 97.5%. The mean age of the respondents was 22.58±2.8SD years and about 199 (63.4%) of them were females. From the total participants, 210 (66.9%) of the respondents were urban and 137 (43.6%) were Bench in ethnicity. Concerning to their religion, about 133 (42.4%) were protestant (See Table 1).
Table 1.
Sociodemographic Characteristics of University Students in the Bench-Sheko Zone, South-west Ethiopia, 2020 (N=314)
| Variables | Category | Frequency (N) | Percent |
|---|---|---|---|
| Age | 18–25 | 230 | 73.2 |
| ≥25 | 84 | 26.8 | |
| Sex | Male | 199 | 63.4 |
| Female | 115 | 36.6 | |
| Residence | Urban | 210 | 66.9 |
| Rural | 104 | 33.1 | |
| Living with parents | Yes | 182 | 58 |
| No | 133 | 42 | |
| Religion | Protestant | 133 | 42.4 |
| Orthodox | 116 | 36.9 | |
| Muslim | 65 | 20.7 | |
| Ethnicity | Bench | 137 | 43.6 |
| Amhara | 91 | 29.0 | |
| Oromo | 71 | 22.6 | |
| Others | 15 | 4.8 | |
| Family income | <2500ETB | 156 | 49.7 |
| ≥2500ETB | 158 | 50.3 |
Clinical Characteristics
This study also revealed the clinical characteristics of the study participants. About 31 (9.9%) of the respondents had history of chronic illness. One-fourth of 80 (25.5%) used substance and about 110 (35%) of the respondent stay at their home for the prevention of COVID-19. Nearly one-quarter of 81 (25.8%) of the students had poor social support (see Table 2).
Table 2.
Clinical and Substance-related Characteristics of University Students in the Bench-Sheko Zone, South-west Ethiopia, 2020 (N=314)
| Variables | Category | Frequency (N) | Percent |
|---|---|---|---|
| Chronic medical illness | Yes | 31 | 9.9 |
| No | 283 | 90.1 | |
| Substance use | Yes | 80 | 25.5 |
| No | 234 | 74.5 | |
| Stay at home | Yes | 110 | 35.0 |
| No | 204 | 65.0 | |
| Relatives got COVID | Yes | 46 | 14.6 |
| No | 268 | 85.4 | |
| Social support | Poor | 81 | 25.8 |
| Moderate | 145 | 46.2 | |
| Strong | 88 | 28.0 |
Depression, Anxiety, and Stress of University Students
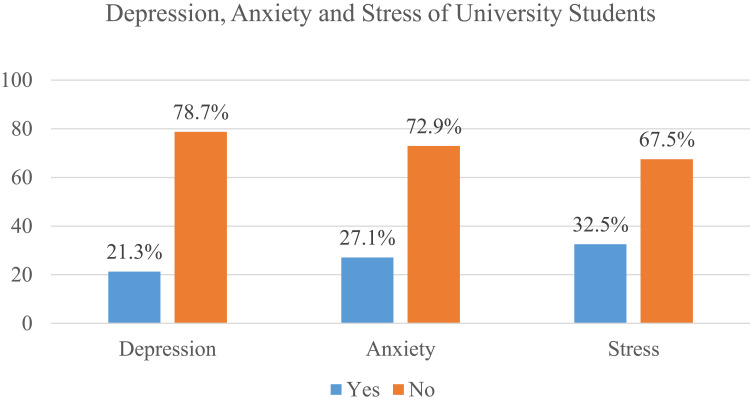
The prevalence of depression, anxiety, and stress was 21.3% (95%CI: 16.6–25.8), and 27.1% (95%CI: 21.6–31.9), 32.5% (95%CI: 27.1–38.2), respectively (see Figure 1).
Figure 1.
Prevalence of depression and anxiety among university students in the Bench-Sheko zone, South-west Ethiopia, 2020 (N=314).
Factors Associated with Depression
From the total variable entered in the multivariable regression, four variables were found to be independently associated with depression among university students. Female students had 2.1 times (AOR: 2.11, 95%CI: 1.15–3.88), higher risk of developing depression compared to males. Students who stayed at home had 3.6 times (AOR: 3.60, 95%CI: 1.95–6.66), higher risk of developing depression when compared to those who did not stay at home.
Students who had history of medical illness had a 3.1 times (AOR: 3.10, 95%CI: 1.28–7.42), higher risk of developing depression compared to those who did not. University students who had poor and moderate social support had 2.8 times (AOR: 2.84, 95%CI: 1.16–6.90), and 2.6 times (AOR: 2.61, 95%CI: 1.15–5.92), higher risk of developing depression compared with those who had strong social support, respectively (See Table 3).
Table 3.
Multivariable Analysis of Factors Associated with Depression Among University Students from the Bench-Sheko Zone, South-west Ethiopia, 2020 (N=314)
| Variables | Category | Depression | COR (95%CI) |
AOR (95%CI) | P value | |
|---|---|---|---|---|---|---|
| Yes N (%) | No N (%) | |||||
| Sex | Male | 28 (41.8) | 171 (69.2) | 1 | 1 | 0.016* |
| Female | 39 (58.2) | 76 (30.8) | 3.13 (1.79–5.46) | 2.11 (1.15–3.88) | ||
| Religion | Protestant | 27 (40.3) | 106 (42.9) | 1 | 1 | 0.372 0.274 |
| Orthodox | 21 (31.3) | 95 (38.5) | 0.86 (0.46–1.63) | 0.72 (0.35–1.47) | ||
| Muslim | 19 (28.4) | 46 (18.6) | 1.62 (0.82–3.20) | 1.56 (0.70–3.46) | ||
| Ethnicity | Bench | 27 (40.3) | 110 (44.5) | 1 | 1 | |
| Amhara | 26 (38.8) | 65 (26.3) | 1.63 (0.87–3.02) | 1.44 (0.70–2.99) | 0.315 0.542 0.739 |
|
| Oromo | 12 (17.9) | 59 (23.9) | 0.82 (0.39–1.75) | 0.76 (0.32–1.79) | ||
| Others | 2 (3.0) | 13 (5.3) | 0.62 (0.13–2.94) | 0.73 (0.12–4.40) | ||
| Living with parents | Yes | 32 (47.8) | 150 (60.7) | 1 | 1 | 0.065 |
| No | 35 (52.2) | 97 (39.1) | 1.69 (0.98–2.91) | 1.77 (0.96–3.25) | ||
| Stay at home | Yes | 44 (65.7) | 73 (29.6) | 4.56 (2.56–8.09) | 3.6 (1.95–6.66) | <0.001* |
| No | 23 (34.3) | 174 (70.4) | 1 | 1 | ||
| Relatives got COVID | Yes | 15 (22.4) | 31 (12.6) | 2.01 (1.01–3.99) | 1.53 (0.68–3.45) | 0.302 |
| No | 52 (77.6) | 216 (87.4) | 1 | 1 | ||
| Medical illness | Yes | 15 (22.4) | 16 (6.5) | 4.16 (1.93–8.95) | 3.10 (1.28–7.42) | 0.012* |
| No | 52 (77.6) | 231 (93.5) | 1 | 1 | ||
| Social support | Poor | 25 (37.3) | 54 (21.9) | 3.88 (1.73–8.73) | 2.84 (1.16–6.90) | 0.022* 0.021* |
| Moderate | 32 (47.8) | 109 (44.1) | 2.46 (1.14–5.29) | 2.61 (1.15–5.92) | ||
| Strong | 10 (14.9) | 84 (34.0) | 1 | 1 | ||
Note: *P value <0.05, 1=reference category.
Factors Associated with Anxiety
From the total variable entered in the multivariable regression, three variables were found to be independently associated with anxiety among university students. Students who were not living with their parents had 3.3 times [AOR: 3.34, 95% CI: (1.87–5.97)], higher risk of developing anxiety as compared to those who live together with their parents.
University students whose relatives got corona virus had 2.4 times [AOR: 2.40, 95% CI: (1.17–4.90)], higher risk of corona virus when compared with those who had not. Students whose family income below 2500 ETB was 2.8 times [AOR: 2.86, 95% CI: (1.60–5.14)], higher risk of developing anxiety when compared to those students whose family income greater than 2500 ETB (See Table 4).
Table 4.
Multivariable Analysis of Factors Associated with Anxiety Among University Students from Bench-Sheko Zone, South-west Ethiopia, 2020 (N=314)
| Variables | Category | Anxiety | COR (95% CI) | AOR (95% CI) | Pvalue | |
|---|---|---|---|---|---|---|
| Yes N (%) | No N (%) | |||||
| Sex | Male | 45 (52.9) | 154 (67.2) | 1 | 1 | 0.364 |
| Female | 40 (47.1) | 75 (32.8) | 1.82 (1.09–3.03) | 0.75 (0.42–1.38) | ||
| Residence | Urban | 49 (57.6) | 161 (70.3) | 1 | 1 | 1 |
| Rural | 36 (42.4) | 68 (29.7) | 1.74 (1.04–2.91) | 1.18 (0.64–2.17) | 0.594 | |
| Religion | Protestant | 36 (42.4) | 97 (42.4) | 1 | 1 | 1 |
| Orthodox | 25 (29.4) | 91 (39.7) | 0.74 (0.41–1.33) | 0.48 (0.25–1.02) | 0.54 | |
| Muslim | 24 (28.2) | 41 (17.9) | 1.57 (0.84–2.96) | 1.50 (0.74–3.03) | 0.255 | |
| Living with parents | Yes | 31 (36.5) | 151 (65.9) | 1 | 1 | <0.001* |
| NO | 54 (64.5) | 78 (34.1) | 3.37 (2.00–5.66) | 3.34 (1.87–5.97) | ||
| Relatives got COVID | Yes | 23 (27.1) | 23 (10.0) | 3.32 (1.74–6.32) | 2.40 (1.17–4.90) | 0.017* |
| No | 62 (72.9) | 206 (90.0) | 1 | |||
| Substance Use | Yes | 16 (18.8) | 64 (27.9) | 0.57 (0.32–1.10) | 0.40 (0.36–1.60) | 0.802 |
| No | 69 (81.8) | 165 (72.1) | 1 | 1 | ||
| Medical illness | Yes | 15 (17.6) | 16 (7.0) | 2.85 (1.34–6.06) | 2.18 (0.94–5.06) | 0.07 |
| No | 70 (82.4) | 213 (93.0) | 1 | |||
| Family Income | <2500ETB ≥ 2500ETB |
62 (72.9) 23 (27.1) |
94 (41.0) 135 (59.0) |
3.87 (2.24–6.68) 1 |
2.86 (1.60–5.14) 1 |
<0.001* |
Note: *P value <0.05, 1=reference category.
Factors Associated with Stress
From the total variable entered in the multivariable regression four variables namely, substance use, depression, anxiety, and social support were found to be independently associated with stress among university students. Students who had depression had 2.3 times (AOR: 2.35, 95%CI: 1.08–5.13), higher risk of developing stress compared to those who had not. Students who used any substance were 3.4 times (AOR: 3.45, 95%CI: 1.9–6.28), at higher risk of developing stress compared to those who did not use any substance. University students who develop anxiety were 2.8 times (AOR: 2.79, 95%CI: 1.33–5.86), at higher risk of developing stress compared to those who did not have anxiety. Furthermore, students who had poor social support were 2.86 times (AOR: 2.86, 95%CI: 1.40–5.86), higher risk of developing stress compared to those who had strong social support (See Table 5).
Table 5.
Multivariable Analysis of Factors Associated with Stress Among University Students in the Bench-Sheko Zone, South-west Ethiopia, 2020 (N=314)
| Variables | Category | Stress | COR (95%CI) | AOR (95%CI) | P-value | |
|---|---|---|---|---|---|---|
| Yes N (%) | No N (%) | |||||
| Living with parents | Yes | 54 (52.9) | 128 (60.4) | 1 | 1 | 0.712 |
| No | 48 (47.1) | 84 (39.6) | 1.35 (0.84–2.18) | 0.89 (0.512–1.58) | ||
| Ethnicity | Bench | 49 (48.0) | 88 (41.5) | 1 | 1 | 1 |
| Amhara | 33 (32.4) | 58 (27.4) | 1.02 (0.58–1.77) | 1.03 (0.55–1.94) | 0.920 | |
| Oromoo | 15 (14.7) | 56 (26.4) | 0.48 (0.24–0.94) | 0.60 (0.28–1.26) | 0.180 | |
| Others | 5 (4.9) | 10 (4.7) | 0.89 (0.29–2.77) | 0.99 (0.29–3.36) | 0.987 | |
| Stay at home | Yes | 50 (49.0) | 67 (31.6) | 2.08 (1.28–3.37) | 1.52 (0.86–2.70) | 0.148 |
| No | 52 (51.0) | 145 (68.4) | 1 | 1 | ||
| Medical illness | Yes | 15 (14.7) | 16 (7.5) | 2.11 (0.99–4.46) | 1.15 (0.45–2.77) | 0.76 |
| No | 87 (85.3) | 196 (92.5) | 1 | 1 | ||
| Depression | Yes | 61 (59.8) | 186 (87.7) | 4.80 (2.72–8.50) | 2.35 (1.08–5.13) | 0.031* |
| No | 41 (40.2) | 26 (12.3) | 1 | |||
| Substance use | Yes | 38 (37.3) | 42 (19.8) | 2.40 (1.22–4.06) | 3.45 (1.90–6.28) | <0.001* |
| No | 64 (62.7) | 170 (80.2) | 1 | |||
| Anxiety | Yes | 56 (54.9) | 173 (81.6) | 3.64 (2.16–6.14) | 2.79 (1.33–5.86) | 0.007* |
| No | 46 (45.1) | 39 (18.4) | 1 | |||
| Social support | Low | 38 (37.3) | 41 (19.3) | 2.86 (1.50–5.45) | 2.86 (1.40–5.86) | 0.004* 0.896 |
| Moderate | 41 (40.2) | 100 (47.2) | 1.26 (0.69–2.29) | 1.04 (0.55–1.98) | ||
| Strong | 23 (25.5) | 71 (33.5) | 1 | 1 | ||
Note: *P value <0.05, 1=reference category.
Discussion
The COVID-19 pandemic was declared as a public health emergency of the world and this emergency causes stress to the whole population as well as university students. The present study assessed the psychological impact (depression, anxiety, and stress) and its associated factors among university students in the Bench-Sheko zone South-west, Ethiopia.
This study revealed that the prevalence of depression was 21.3%, which is in line with a review of existing literature (16–28%),9 but lower than studies conducted in Pakistan (45%), Spain (34.1%),12,13 and higher than Iran (15%) and India (13.97%).14,15 The present study also indicated that the prevalence of anxiety was 27.1%, this finding is supported with a study done in China (24.9%) and review of existing literature (16–28%),9,16 but higher than Iran (20%), India (12.63%) and Spain (21.3%),13–15 and lower than a study done Jordan (69.5%), Pakistan (34%), France (60.2%), and Turkey (69.9%).12,17–19 Furthermore, this study also showed that the prevalence of stress was 32.5%. This result is supported with a study done in Spain (28.14%),13 but higher than Indian (15.57%),15 and lower than a study done in France (61.6%), and Jordan (69.5%).17,18 The possible reason for the discrepancy might be due to difference in strict quarantine, high incidence rate, effect of lockdown, difference in literacy level and study sittings difference.
This study revealed sex is significantly associated with depression. Female university students had 2.1 times higher risk of developing depression compared to male students. This finding supported a study done in India.9 This may be due to females being more commonly exposed to mental illness, cultural factors, economic deprivation or due to hormonal fluctuations.20 Students who stay at home had 3.6 times higher risk of developed depression compared to those did not stay at home This is the fact isolation, social distancing, and extreme changes in daily life cause clinical depression because of COVID-19.21
Students who had history of medical illness had 3.1 times higher risk of developing depression compared to those who did not. This is due to the fact that having previous history of medical illness may exacerbate the impacts COVID-19. This finding is supported with a systematic review of COVID-19 pandemic and mental health consequences.22
This study also assessed factors affecting anxiety. Students who were not living with their parents had 3.3 times higher risk of developing anxiety compared to those who live together. Previous studies have indicated that the risk factors associated with emotional and anxiety disorders in adults include the death of parents in childhood, not living with parents, and parents’ psychological problems and mental illnesses.16
This study showed that students whose family income less than 2500 ETB were 2.8 times higher risks of developing anxiety as compared to counterparts. Which could be explained by increased psychological and economic pressure. This is supported with a study done in China among college students.16 Relatives being infected with COVID-19 were an independent risk factor in university students’ anxiety about the epidemic, which might be related to the high contagiousness of the new coronavirus pneumonia.23
Moreover, this study also showed factors that increase stress of university students related to COVID-19. Students who had depression and anxiety had 2.3 and 2.8 higher risk of developing stress compared to those who had no depression and anxiety. This may be due to an exaggerated information dissemination about the health, social and economic crisis of COVID-19. The finding is in line with a systematic review of the COVID-19 pandemic and mental health consequences: systematic.22
Students who had poor social support had 2.8 times higher risk of developing depression and stress compared to their counterparts. Lack of social support may add a pressure to economic, social, and health impacts. Evidence showed that loneliness and poor social support risks depression and stress.24 Moreover, students who used substance had 3.4 times higher risk of developing stress compared to those who had not use substance. People who use substance are a marginalized and stigmatized group with weaker immunity responses, and vulnerability to stress.25 This finding is supported with a study done in Dessie, Ethiopia, substance use was significantly associated with mental distress of students.26
Conclusions and Recommendation
According to this study the psychological (depression, anxiety and stress) among university students related to COVID-19 were high. Being female, staying at home, history of medical illness, poor and moderate social support were factors that increased the risks of depression. Factors increasing the risk of anxiety were not living with their parents, relatives got corona virus and low family income. Moreover substance use, depression, anxiety, and poor social support were among the factors that increase the risk of stress.
Governmental and private organization and health-care providers also provide psychosocial and mental health services alongside health-care service and various media channels. Moreover the government should incorporate mental health and psychological intervention within COVID-19 outbreak prevention and mitigation program.
Limitation of the Study
Since the data were collected by phone call the respondents may not provide accurate information for the study, which may have an effect on the findings of this study. Unlike a longitudinal study, the cross-sectional nature of the data makes it impossible to draw inferences about the direction of relations and it does not show cause and effect relationship among study variables.
Funding Statement
The study was funded by Mizan Tepi University.
Abbreviations
AOR, adjusted odds ratio; COR, crude odds ratio; COVID-19, 2019 novel coronavirus; ETB, Ethiopian Birr; SPSS, Statistical Package for the Social Sciences.
Data Sharing Statement
The datasets generated and analyzed during the study will be made available to organizations and individuals based on reasonable request.
Author Contributions
NS, MA and RM were involved to conception and design of the study, acquisition of data, analysis and interpretation of data, drafting and revising the article, agreed to submit to the current journal, gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.WHO. Coronavirus [Internet]. 2020. Available from: https://www.who.int/images/default-source/health-topics/coronavirus/gettyimages-1203376093.tmb-1920v.png?Culture=en&sfvrsn=6e0c1bc7_61920w. Accessed September8, 2020.
- 2.Director-general WHO. WHO director-general’ s opening remarks at the Mission briefing on COVID-19 - [Internet]; 2020. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-mission-briefing-on-covid-19---16-april-2020.
- 3.Fast IFO, Trick S, Defeats E, Nerve S How I ended neuropathy.Total Cases (worldwide) Daily Cases (worldwide) [Internet]. Vol. 576; 2020. Available from: https://www.worldometers.info/coronavirus/?fbclid=IwAR3ix-1RitkdGqHLX_wnjCvw7t9nBK-Z16Qej1GBgZ4MjcpyBKR86LCc2Oo. Accessed April 25, 2020.
- 4.WHO African region. COVID-19 [Internet]; 2020. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed September8, 2020.
- 5.WHO. COVID 19 Public Health Emergency of International Concern (PHEIC). Global research and innovation forum: towards a research roadmap. [Internet]. 2020. Available from: https://en.wikipedia.org/wiki/2020_coronavirus_pandemic_in_Ethiopia. Accessed September8, 2020.
- 6.Panchal N, Kamal R, Orgera K, et al. The implications of COVID-19 for mental health and substance use. Kaiser Fam Found. 2020;1–16. [Google Scholar]
- 7.Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rajkumar RP. COVID-19 and mental health: A review of the existing literature. Asian J Psychiatr. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheung T, Yip PSF. Depression, anxiety and symptoms of stress among Hong Kong nurses: a cross-sectional study. Int J Environ Res Public Health. 2015;12(9):11072–11100. doi: 10.3390/ijerph120911072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kocalevent RD, Berg L, Beutel ME, et al. Social support in the general population: standardization of the Oslo social support scale (OSSS-3). BMC Psychol. 2018;6(1):1–18. doi: 10.1186/s40359-018-0249-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salman M, Asif N, Mustafa ZU, Khan TM, Shehzadi N, Hussain K. Psychological Impact of COVID-19 on Pakistani university students and how they are coping. medRxiv. 2020;1–6. doi: 10.1101/2020.05.21.20108647 [DOI] [Google Scholar]
- 13.Odriozola-gonzález P, Planchuelo-gómez Á, Jesús M, De Luis-garcía R. Psychological e ff ects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 2020;290:113108. doi: 10.1016/j.psychres.2020.113108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shahriarirad R. The Mental Impact of COVID-19 Outbreak: A Population-Based Survey in Iran; 1975:1–21. Springer Nature. doi: 10.21203/rs.3.rs-23425/v1 [DOI] [Google Scholar]
- 15.Rehman U, Shahnawaz MG, Khan NH, Kharshiing KD, Khursheed M. Depression, anxiety and stress among Indians in times of Covid-19 lockdown. Community Ment Health J. 2020. doi: 10.1007/s10597-020-00664-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cao W, Fang Z, Hou G, Han M, Xu X, Dong J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al-tammemi AB, Akour A, Alfalah L. Is it just about physical health? An internet-based cross-sectional study exploring the psychological impacts of COVID-19 pandemic on university students in Jordan using Kessler Psychological Distress Scale. medRxiv 2020:1–6. doi: 10.1101/2020.05.14.20102343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Husky MM, Kovess-masfety V, Swendsen JD. Stress and anxiety among university students in France during Covid-19 mandatory con fi nement. Compr Psychiatry. 2020;102:152191. doi: 10.1016/j.comppsych.2020.152191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Özdede M, Sahin SC. Views and anxiety levels of Turkish dental students during the COVID-19 pandemic. J Stomatol. 2020;73(3):123–128. doi: 10.5114/jos.2020.96867 [DOI] [Google Scholar]
- 20.Albert PR. Why is depression more prevalent in women? J Psychiatry Neurosci. 2015;40(4):219–221. doi: 10.1503/jpn.150205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boehnert J. Find expert insight and analysis, from coronavirus to climate change, in our daily newsletter. Surviving climate change means transforming both economics and design. 2020;1–7. Available from: https://theconversation.com/covid-19-could-lead-to-an-epidemic-of-clinical-depression-and-the-health-care-system-isnt-ready-for-that-either-134528. Accessed September8, 2020.
- 22.Vindegaard N, Eriksen Benros M. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Page OT, Articles R. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2 methods. Emerg Infect Dis. 2020;26(7):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang J, Mann F, Lloyd-Evans B, Ma R, Johnson S. Associations between loneliness and perceived social support and outcomes of mental health problems: A systematic review. BMC Psychiatry. 2018;18:1–39. doi: 10.1186/s12888-018-1736-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Levin S, Albers TNH, Mitchener KJ, et al. COVID-19 and substance use disorders. Econ Hist Rev. 2019;73(1):202–246. doi: 10.3386/w22921 [DOI] [Google Scholar]
- 26.Kelemu RT, Kahsay AB, Ahmed KY. Prevalence of mental distress and associated factors among Samara university students, Northeast Ethiopia. Hindawi. 2020;2020. doi: 10.1155/2020/78362960A. [DOI] [PMC free article] [PubMed] [Google Scholar]