Abstract
The presence of respiratory symptoms in Parkinson's disease (PD) has been known since the first description of the disease, even though the prevalence and incidence of these disturbances are not well defined. Several causes have been reported, comprising obstructive and restrictive pulmonary disease and changes in the central ventilatory control, and different pathogenetic mechanisms have been postulated accordingly. In our review, we encompass the current knowledge about respiratory abnormalities in PD, as well as the impact of anti-Parkinsonian drugs as either risk or protective factors. A description of putative pathogenetic mechanisms is also provided, and possible treatments are discussed, focusing on the importance of recognising and treating respiratory symptoms as a key manifestation of the disease itself. A brief description of respiratory dysfunctions in atypical Parkinsonism, especially α-synucleinopathies, is also provided.
Short abstract
This review addresses current knowledge about respiratory dysfunctions in Parkinson's disease, from the aetiopathology to pharmacological and invasive treatments, describing the different clinical phenotypes https://bit.ly/2X7OLtN
Introduction
Parkinson's disease (PD) is a neurodegenerative disorder due to a progressive loss of striatal dopamine, thus leading to tremor, bradykinesia, rigidity and postural instability.
The presence of respiratory abnormalities in PD has been well known for many years, but its prevalence is probably underestimated. In his first description, Parkinson [1] noted this association describing a man who “fetched his breath rather hard”. Since the half of the last century, many studies have discussed respiratory impairment in PD, even in early stages and in asymptomatic patients [2]. Respiratory dysfunctions may be responsible for the mortality and morbidity associated with PD [3]. Although respiratory changes are usually correlated with peripheral motor impairment [4–6], several causes have been reported, including obstructive and restrictive patterns, as well as changes in the central ventilatory control. Overall, respiratory dysfunctions in PD seem to correlate with motor scores, but the relationship with pharmacological therapies, disease phenotypes and nonmotor symptoms is not completely understood.
In this review, we encompass the current knowledge about respiratory changes in PD, focusing on obstructive and restrictive patterns, as well as on the role of the central respiratory control, highlighting the underlying putative pathogenetic mechanisms. A brief discussion about pneumonia in PD it is also provided; an overview of the impact of anti-Parkinsonian drugs and deep brain stimulation (DBS) is also described. Finally, we briefly discuss the presence of respiratory abnormalities in atypical Parkinsonisms, especially multiple system atrophy (MSA), dementia with Lewy bodies (DLB) and supranuclear palsy (PSP).
Materials and methods
A literature search was updated from March 2019 to June 2020 and referred to PubMed and Google Scholar, using the terms “Parkinson's disease”, “Parkinson”, “Parkinson disease” combined with “respiratory failure”, “drugs respiratory failure”, “pulmonary dysfunction”, “respiratory dysfunction” and “ventilatory dysfunction”. Another search combined the terms “Parkinson's disease”, “Parkinson”, “Parkinson disease” with terms “sleep” and “sleep apnea”. We included articles in English only. Exclusion criteria included animal studies and other neurological disorders different from PD or Parkinsonisms.
Obstructive respiratory dysfunction
Several studies have shown obstructive respiratory dysfunction in PD (table 1). Many authors have described upper airway obstruction (UAO), with a highly variable prevalence ranging from 6.7% to 67% [8, 9]. Dyspnoea could be a manifestation of UAO, even if other common indicators may include hypophonia, shaky voice, stridor or wheeze [17].
TABLE 1.
Main studies considered in our review about the presence of obstructive, restrictive and central respiratory dysfunction in Parkinson's disease patients
| First author [ref] (year) | Number of patients | Clinical score | Disease duration | Pharmacological washout | Obstructive defect | Restrictive defect | Central ventilatory dysfunction |
| Vincken [7] (1984) | 27 | H&Y 4 (mean in the obstructive patients) | Not available | Not reported | 10 (upper airway) | Not found | Not assessed |
| Izquierdo-Alonso [8] (1994) | 63 | H&Y 2.55 (mean), UPDRS 30 (mean) | 5 years (mean) | No | 13 (upper airway) | 54 | Not assessed |
| Sabatè [9] (1996) | 58 | UPDRS III, mean not available | Not available | 8 h | 36 (upper airway) versus 21 (lower airway) | 16 | Not assessed |
| Onodera [10] (2000) | 25 | H&Y 2–3 | Not available | No | Not assessed | Not assessed | Impairment response to hypoxia versus control group |
| Herer [11] (2001) | 21 | H&Y 2.6 (mean) | 0.25–11 years | 12 h | 5 (upper airways obstruction) | Not found | Not assessed |
| De Pandis [12] (2002) | 12 | H&Y 4.08 (mean) | 8–25 years | 12 h | Not found | More severe pattern in off stage | Not assessed |
| Weiner [13] (2002) | 20 | H&Y 2–3, UPDRS III 41.4 (mean in off) | Not available | Not reported | Not found | Mild restrictive pattern | Not assessed |
| Sathyaprabha [14] (2005) | 35 | H&Y 1–2 | 1–5 years | 12 h | 2 | 33 | Not assessed |
| Seccombe [15] (2011) | 19 | H&Y 2.5 (mean) | 2–23 years | No | 1 | 2 | Impairment response to hypercapnia versus control group |
| Baille [16] (2018) | 41 | UPDRS III 19 (mean) | 0.20–3.6 years | 12 h | 6 | 1 | Not assessed |
H&Y: Hoehn & Yahr; UPDRS: Unified Parkinson's Disease Rating Scale.
Two types of UAO have been described by spirometry and fibre optic endoscopy for the first time by Vincken and co-workers [7], and was further confirmed by subsequent studies [8, 9, 11]. The first type (“respiratory flutter”) is characterised by regular consecutive flow decelerations and accelerations superimposed on the general flow-volume loop, with a frequency similar to the hands’ tremor (5–8 Hz). In the second type, abrupt and irregular changes in flow (often dropping to zero) are seen on an abnormal flow-volume loop due to irregular and jerky movements of the glottic and supraglottic structures, thus leading to intermittent airways closure.
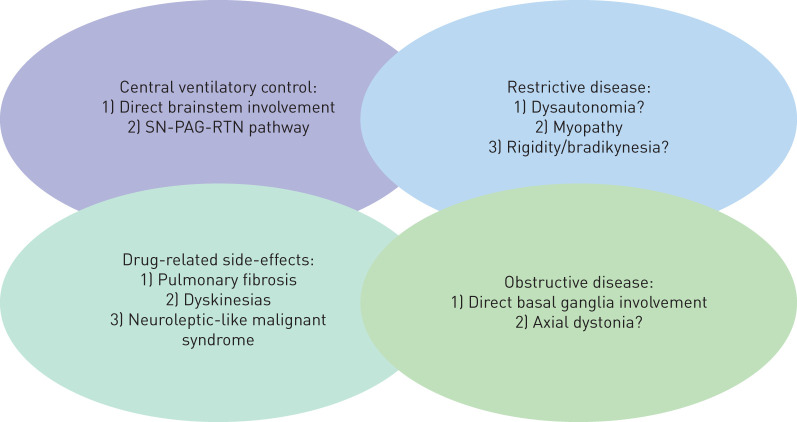
Although the pathophysiology is still debated, both patterns probably reflect dysfunctions in the basal ganglia (figure 1). In PD, α-synuclein deposition starts in the caudal portion of the brainstem, involving the dopaminergic neurons in the substantia nigra (SN) [18]. Loss of dopaminergic stimulation is known to lead to motor disturbances such as tremor, bradykinesia and rigidity and movement abnormalities in the phonatory structures may ultimately resemble those observed in peripheral muscles. These data are consistent with electromyographic abnormalities of laryngeal, rib cage and neck muscles [19, 20], even if these changes are not specific and may be present also in other movement disorders [7].
FIGURE 1.
Putative contributing mechanisms leading to respiratory dysfunctions in Parkinson's disease and atypical Parkinsonisms. SN: substantia nigra; RTN: retrotrapezoid nucleus; PAG: periaqueductal grey.
A possible correlation between UAO and tremor has been reported by some authors [21], even if it should be stated that other types of Parkinsonisms were included in the study. Sabatè et al. [9] have, nevertheless, reported the association of UAO with bradykinesia more than rigidity and tremor. Moreover, an association of UAO with dystonia has been described by Jankovich et al. [22]. All these data seem to further suggest a correlation between UAO and peripheral motor disorders, due to basal ganglia dysfunctions. UAO has been correlated also with dorsal column arthrosis, which may be explained by chronic anomalous postures in advanced stages [9].
Lower airway obstruction has been reported and differentiated by UAO in the work of Sabatè et al. [9], correlating with rigidity, resistance to passive mobilisation of the cervical column and cervical spine arthrosis. Obstructive abnormalities have been described in other papers, although differences between UAO and lower airway obstruction have not been systematically assessed [14–16]. Moreover, a small number of obstructive pattern patients in PD was found in these studies, and no further characterisation has been provided to date [14–16].
Differences among studies may be related to the characteristic of the cohorts examined such as number of the patients enrolled, disease duration and the timing of pharmacological washout before the spirometric evaluation (table 1).
Restrictive respiratory dysfunction
Papers describing a restrictive respiratory pattern are summarised in table 1. Restrictive respiratory dysfunction has been described both in symptomatic and asymptomatic patients, with variable prevalence ranging from 28% to 94% [8, 9, 12, 14].
Even for restrictive dysfunction, the pathogenesis is controversial; several hypotheses have been postulated, including dysautonomia related to PD and adverse effects referred to ergot-derived drugs [8, 9], whereas myopathic weakness of the chest wall seems unlikely (figure 1) [5, 23]. No correlation with tremor, bradykinesia or rigidity has been described, while a probable relationship with dorsal spine arthrosis has been postulated [9]. Moreover, some authors reported a correlation with motor features, such as gait freezing and falls, in moderate to severe PD, and a correlation with camptocormia and kyphoscoliosis in more advanced stages [24].
Others reported conflicting data showing a possible correlation with rigidity and bradykinesia, but not with tremor [25]. These data may be, at least in part, in line with other studies. De Pandis et al. [12] identified a restrictive pattern in a cohort of advanced parkinsonian patients (mean Hoehn and Yahr stage 4.08) worsened in the “off” condition, probably due to chest wall muscle rigidity and reduction of chest wall range of movements. Similar results were obtained by Sathyaprabha et al. [14], showing a high percentage of PD patients with a restrictive pattern worsened during the “off” condition and more pronounced in later stages (Hoehn and Yahr 2).
Even in this case, reduction in rigidity may result in improved muscle coordination and facilitation of chest wall movements. A really small number of restrictive pattern patients was found in other studies, but these patterns have not been further characterised (table 1) [15, 16].
Central ventilatory control
As aforementioned, the deposition of α-synuclein in PD starts in the caudal portion of the brainstem, and structures involved in the respiratory control, as those responsible for coordinating ventilation and detecting peripheral hypoxaemia or hypercapnia, may be directly affected by neurodegeneration at an early stage [18, 26–29].
These data seem to agree with what has been reported in literature. Onodera et al. [10] described a reduced central chemosensitivity to hypoxia even in the early stages, without abnormalities in the response to hypercapnia. Other authors, as opposed, found an abnormal ventilatory response to carbon dioxide in patients with normal lung volumes and flows, especially in mild to moderate PD, but not for mild hypoxia (table 1) [15].
Despite these little discrepancies among different studies, according to the Braak hypothesis, the early involvement of the brainstem in PD may lead to dysfunction of the medullary respiratory centres and consequently of the central drive of breathing [30]. Moreover, other mechanisms have been reported to explain the impaired central control (figure 1). Neurodegeneration involves not only dopaminergic neurons, but also astrocytes: losing astrocytes in key regions involved in breathing activity will produce ATP deficiency, which in turn will fail to stimulate breathing [31–33].
In addition, an indirect mechanism underlying central ventilator control has been recently proposed in animals, basing on the demonstration of a di-synaptic excitatory pathway from the dopaminergic neurons of the SN to the retrotrapezoid nucleus (RTN), passing through the periaqueductal grey (PAG) [34]. PAG is engaged in a number of physiological functions, comprising nociception, arterial pressure and heart rate, while RTN is critically involved in the chemosensory control of breathing [31, 35–37]. PAG also coordinates motor output, including respiratory muscles, based on the integration of input arising from limbic, pre-frontal and anterior cingulate cortex regions [38]. Overall, degeneration of SN dopaminergic neurons, as occurs in PD, may lead to a progressive loss of functions along the SN–PAG–RTN pathway. These findings further emphasise the key role of a central breathing control failure in PD respiratory dysfunction, in addition to the loss of dopaminergic stimulation due to the direct basal ganglia involvement.
Central breathing dysfunction may explain at least in part the abnormal perception of dyspnoea (POD), as reported in some papers. Many patients with spirometric abnormalities may be asymptomatic, and blunted POD may contribute. The reduced response to hypoxia described by Onodera et al. [10] may play an important role. This report, however, is not consistent with a more recent study, which demonstrated an increased POD in PD compared to controls [13]. Physiologically, dyspnoea is perceived as respiratory muscle effort, and the degree of perception is linked to the strength of respiratory muscles [39]. The patients examined by Weiner et al. [40] had an abnormal pulmonary test function (restrictive pattern and inspiratory muscle endurance) and a more severe disease compared to the cohort of Onodera et al. [10] so in this case mechanical factors may have contributed to the increased POD.
Mechanical factors, independently or in addition to a central dysfunction, may also explain the exacerbated POD in patients experiencing respiratory dyskinesias [40].
Apnoea in Parkinson's disease
The presence of apnoea syndrome has been studied in PD as well. Apnoea syndrome is probably related to a central dysfunction of the brainstem respiratory centres and/or a peripheral airways involvement. However, different studies have produced conflicting results, probably according to the different samples of patients and methods used.
Apnoea occurring during sleep could be classified as central (if the airflow drops down due to a failure in activation of respiratory muscles), obstructive (if the occlusion of the upper airways stops the airflow despite respiratory muscle effort) and mixed [41]; nonetheless, these patterns have not been studied systematically in PD and a clear stratification is not available in the current literature. Most studies focused on obstructive apnoea rather than central.
Conflicting results have been reported about the prevalence of obstructive apnoea syndrome in PD patients; Maria et al. [42] identified a higher prevalence of obstructive apnoea in PD populations, whereas others found less occurrence of obstructive apnoea compared to controls [43, 44], or even no apnoea or sleep abnormalities [45]. De Cock et al. [44] tried to explain this phenomenon, postulating a possible protective contribution due to rapid eye movement (REM) sleep behaviour disorder (RBD), in which the physiological muscle atonia during REM sleep is absent and may prevent upper airway closure.
Surprisingly, the authors found that patients with abnormal persistence of chin muscle tone still presented obstructive apnoea during REM sleep, and similar findings were described by Huang et al. [46]. It may be reasonable that there is a correlation between motor disability and apnoea, as suggested in some studies [42, 44], but the role of PD medications is not clear, and it has to be specified that in these studies, motor disability and apnoea were assessed in the “on” state, so the real contribution of dopaminergic drugs could not be clearly assessed. Continuous positive airway pressure (CPAP) seems to be effective in reducing events, improving oxygen saturation, and deepening sleep in patients with PD and obstructive sleep apnoea [47, 48].
The issue of pneumonia in Parkinson's disease
Aspiration pneumonia represents a dramatic complication that may explain the acute/subacute onset of fever and respiratory insufficiency in a PD patient. Physiologically, swallowing requires adequate coordination between pharyngeal and respiratory musculature, but this mechanism is frequently impaired in PD [49]. Dysphagia is typical in the advanced stages of disease, on average 10–11 years after motor symptoms onset [50], when bradykinesia, rigidity and dyskinesias are predominant; however, a cough dysfunction in more than 50% of asymptomatic PD patients has been demonstrated [51] and this may also contribute to silent aspiration and increased risk of pneumonia [52]. Moreover, in these patients the cough mechanism becomes weak because of cough reflex impairment and chest wall rigidity, further increasing the risk of aspiration [53]. A blunted urge to cough (UTC), a respiratory sensation that precedes the cough reflex, is also present and correlates with the severity of dysphagia and consequently, with an increased risk of aspiration [54].
The key for adequate management of aspiration pneumonia is prevention. A soft mechanical diet is usually the first step, followed as dysphagia progresses, by liquid thickening. A chin-down posture while swallowing may be helpful, and sometimes a speech or swallowing therapist may be required. The beneficial role of dopaminergic stimulation is controversial; despite the importance of dopaminergic basal ganglia circuits in the swallowing process [55], conflicting results have been reported by different studies [56, 57]. Finally, for patients with marked sialorrhea, who may have an increased risk of aspiration, treatment with anticholinergics drugs or botulinum injections in the salivary glands may be indicated.
Effects of dopaminergic therapy: risk or protection?
Studies have provided controversial results about the therapeutic effects of dopaminergic stimulation, and the role of drugs commonly used in the treatment of PD is still debated, strictly depending both on disease stage and administration modality.
Most papers strengthen the role of anti-Parkinsonian drugs as a protective factor against the development of respiratory failure. Levodopa increases inspiratory muscle function in anaesthetised dogs [58], and dopamine improves diaphragm function during acute respiratory failure in patients with COPD [59]. In early stages, the levodopa equivalent daily dose does not correlate with pulmonary functional testing; as the disease progresses, anti-Parkinsonian medications may be responsible for the maintenance of the maximal inspiratory mouth pressure and sniff nasal inspiratory pressure [16]. Accordingly, bedtime controlled-release levodopa (Sinemet CR) is associated with less severe obstructive sleep apnoea in PD [60]. Because dopamine is not known to increase muscle strength, it may ameliorate respiratory function by improving muscle coordination by a central activity [16].
Among the side effects of anti-Parkinsonian drugs, we have to consider pleura-pulmonary fibrosis induced by dopamine agonists like bromocriptine [61], and levodopa-induced diaphragmatic dyskinesias, which may present as marked dyspnoea [40, 62, 63]. The presence of other dyskinesias more commonly seen in PD, such as trunk, face or limb abnormal involuntary movements, should alert the physician to the presence of diaphragmatic dyskinesias in patients complaining of breath shortness.
Many authors have investigated the effect of dopaminergic therapy on aforementioned respiratory dysfunction, especially on obstructive and restrictive patterns (table 2).
TABLE 2.
Main findings of major studies we considered about the effects of dopaminergic drugs on respiratory parameters and respiratory dysfunctions
| First author [ref] (year) | Number of patients | Clinical score | Disease duration | Pharmacological washout | Study design | Main results |
| Herer [11] (2001) | 21 | H&Y 2.6 (mean) | 0.25–11 years | 12 h | PD patients versus control group. Basal spirometry (pharmacological washout) then spirometry after 45–60 min of levodopa administration (1–2.6 mg·kg−1) versus placebo | Improvement of obstructive parameters and/or of saw-tooth spirometry pattern after levodopa |
| De Pandis [12] (2002) | 12 | H&Y 4.08 (mean) | 8–25 years | 12 h | PD patients with fluctuating symptoms; spirometry in on state versus off state | Restrictive pattern in severe PD, with worsening in the off state |
| Weiner [13] (2002) | 20 | H&Y 2–3, UPDRS III 41.4 (mean in off) | Not available | Not reported | Spirometry in on versus off state compared to healthy controls | Mild restrictive pattern not influenced by levodopa; decreased respiratory muscle strength and endurance in off state, with a nonsignificant trend to increase after levodopa. POD attenuated after dopaminergic medications |
| Sathyaprabha [14] (2005) | 35 | H&Y 1–2 | 1–5 years | 12 h | PD patients versus control group. Spirometry in off state versus on state | Predominantly restrictive pattern ameliorating with levodopa (on condition) |
| Lim [64] (2008) | 10 | H&Y 2.4 (mean) | 8.5 years (mean) | 12 h | PD patients, spirometry in on condition versus off condition | Improvement of restrictive parameters in on condition, even if small |
| Pal [25] (2007) | 53 | H&Y 2.4 (mean) | 3.1 years (mean) | 12 h for levodopa, 18 h for dopamine agonists | PD patients versus controls; spirometry in off condition after washout versus on condition | Restrictive disfunction partially reversed by levodopa |
| Baille [16] (2018) | 41 | UPDRS III 19 (mean) | 0.20–3.6 years | 12 h | Spirometry at the time of recruitment and then two after 2 years of follow-up (both on pharmacological washout) | Inspiratory muscle weakness at time of recruitment, without worsening after 2 years. Motor outcome not different among PD patients with inspiratory muscle weakness compared to patients without |
PD: Parkinson's disease; H&Y: Hoehn & Yahr; UPDRS: Unified Parkinson's Disease Rating Scale; POD: perception of dyspnoea.
Indirect evidence of the beneficial role of dopaminergic therapy on the UAO has been supported by the acute respiratory failure that may occur after these medications are suspended [65, 66], or by the response of UAO to intravenous apomorphine [67, 68]. Further evidence about the beneficial effect of dopaminergic therapy on UAO was provided by Herer et al. [11]. In contrast, other authors strengthened a key role of dopaminergic drugs in reversing, at least partially, restrictive changes [12, 14, 25, 64]. However, a recent meta-analysis of four major clinical trials showed no clear effects of dopaminergic stimulations on the obstructive pattern [11, 12, 14, 64], proving some efficacy on restrictive pattern parameters instead [69]. In this view, there are only few data about the effects of dopaminergic agents on brainstem ventilatory control. Interestingly, Weiner et al. [13] demonstrated an attenuated POD after levodopa intake; given that the respiratory muscle strength was not significantly different in the “on” compared to the “off” condition, the authors speculated about a possible central effect of levodopa contributing to the decrease of POD.
These discrepancies may be explained at least in part by the different study design and the different characteristics of the cohort such as number of patients, PD duration and severity; differences in the dosage of levodopa administered in the “off” stage and in the duration of pharmacological washout may also play a role. Only one of those studies is considered to have specified a different washout timing for levodopa and dopamine agonist [25], and only one has assessed spirometry after a standardised weight-based levodopa intake [11].
Finally, a growing body of evidence suggests that both a sudden withdrawal and a significant reduction of anti-Parkinsonian drugs are risk factors for the so-called neuroleptic malignant-like syndrome (NMLS), a rare but severe clinical condition, resembling the well-known neuroleptic malignant syndrome, characterised by hyperthermia, impaired consciousness, autonomic dysfunction (e.g. respiratory failure) and elevated serum creatine kinase levels. Independent risk factors for NMLS are the use of cholinesterase inhibitors, a rapid switchover from bromocriptine to pergolide and enteral nutrition, as high protein intake critically impairs the absorption of levodopa [70–72].
Finally, only few data have been reported concerning the relationship between the enteral infusion of levodopa and the development of respiratory dysfunctions, except for sporadic cases of pneumonia and pulmonary embolism [73].
Correlation between pneumological drugs and PD
In this scenario, the effects of drugs commonly used by the pneumologist should also be considered. For instance, some studies recently reviewed by Hopfner et al. [74] postulated the possible correlation between β-adrenoreceptors (both agonists and antagonists) and PD [75]. Anticholinergic drugs are frequently used for obstructive pulmonary disorders and systemic anticholinergics may play a part in PD [76]. Acetylcholine has a key role in modulating dopaminergic activity in the basal ganglia, and its inhibition may increase central dopaminergic tone [77]. Anticholinergic bronchodilators might have central effects, as reported by some authors [78]. An effect on motor disturbances in PD may be reasonable, even if to our knowledge this has not been investigated in the current literature. However, it should be considered that anticholinergics may be associated with cognitive impairment and delirium [78], and these adverse effects may be even more common in the advanced stage of PD, when dementia is a very common feature.
Deep brain stimulation and respiratory failure
DBS is an effective strategy for the treatment of advanced PD, thus improving motor fluctuations and bradykinesia.
Nonetheless, the classical target of the subthalamic nucleus (STN)-DBS reserves stimulation-induced side effects in the long-term period, comprising gait and speech impairment, as well as a progressively worsening of tremor. In this scenario, only few papers have specifically investigated respiratory failure. In particular, STN-DBS may increase the risk of a fixed epiglottis and modify velopharyngeal control [79]; these effects seem to strictly depend on frequency parameters, with low-frequency stimulation leading to a clinical improvement, whereas higher frequencies are associated with a detrimental effect on velopharyngeal control [80].
In support of this view, Hammer et al. [81] have recently found that in STN-DBS patients, respiratory changes do not correlate with limb function, but speech-related respiratory and laryngeal control may benefit when the stimulation is delivered at low frequencies (145 Hz) and shorter pulse width (60 µs). In addition to stimulation frequency, other factors may account for these correlations, including variability in localisation of the active DBS electrodes, individual variability in somatotopic organisation of STN, stimulation fields and potential current spread beyond the STN target (e.g. internal capsule). Data on the relationship between respiratory changes and novel DBS targets, such as the pedunculopontine nucleus (PPN), have not been extensively reported so far.
PPN has been only recently suggested as a new target for DBS in PD, given its key role in gait control and posture maintenance [82].
PPN surgery may modify central ventilation control, as PPN directly changes sympathetic activity [83]; moreover, PPN could indirectly modulate both breathing regulation, through cholinergic projections to RTN, and expiratory output arising from the parafacial respiratory group in the ventrolateral medulla [84].
A recent study has confirmed beneficial effects of low-frequency PPN-DBS on the upper airways function, also showing a significant correlation between the increase of oscillatory α-band activity and forced respiratory manoeuvres [85]; this effect was particularly marked when the rostral PPN was stimulated, as a part of the “mesencephalic locomotor region” (MLR); in animal studies, the MLR has been shown to project directly to a medullary respiratory generator and plays a key role in changes in respiration linked to motion [86].
Respiratory dysfunction in Parkinsonisms
As described above, the presence of respiratory dysfunction in PD may be explained, at least in part, by dysregulation in basal ganglia and in other brainstem structures that control the central respiratory drive or peripheral airway muscles. In this scenario, it is reasonable to assume the presence of some kind of dysfunction in other forms of Parkinsonism, either secondary or primary degenerative, in which these structures may be involved [22, 87].
Besides this, to the best of our knowledge, systematic studies on degenerative parkinsonians are still lacking, with only few data currently available about MSA and DLB, two degenerative disorders belonging to α-synucleinopathies along with PD.
Respiratory dysfunction is considered one of the “red flags” that may help to distinguish PD from MSA [88], and includes nocturnal stridor and obstructive sleep apnoea [89]. In MSA, deposition of synuclein preferentially involves the caudal brainstem and the ventral medullary region, a key area for the vocal cord control and central respiratory drive [90]. Respiratory dysfunction, including sleep disordered breathing as inspiratory stridor, represents a typical feature of MSA and probably reflects degeneration of brainstem respiratory nuclei involved in respiratory rhythmogenesis and chemosensitivity, including the pre-Bötzinger complex, nucleus raphe pallidus and nucleus raphe obscurus; the same nuclei are also impaired in DLB, although less severely than in MSA [91]. In addition to the reduced ventilatory response to hypercapnia, and in line with PD, respiratory dysfunctions in DLB also comprise both impaired cough reflex and UTC responses [92–94]. In particular, UTC seems to be controlled by the insula, a region primarily and critically involved during DLB progression [94].
Inspiratory stridor is probably related to vocal cord paralysis or vocal cord and laryngeal dystonia, leading to glottis closure [95, 96], and the presence of nocturnal stridor is classically considered an important predictor of sudden death in these patients [97]. No data about the role of dopaminergic therapy or DBS are available in MSA, and some authors proposed an approach with CPAP or botulinum toxin injection into vocal cords [98, 99]. Obstructive sleep apnoea has been related to pharyngeal narrowing due to brainstem neurons degeneration [100], and similarly to other forms of obstructive apnoea CPAP is the preferential treatment.
Among tauopathies, respiratory dysfunctions have been investigated in PSP, where a critical impairment of voluntary respiratory control has been reported, while automatic and limbic control seem to be preserved; accordingly, nocturnal respiratory abnormalities were not found even in the most severely disabled patients [101, 102]; in particular, the conflict between volitional and automatic breathing in PSP may explain the “respiratory ataxia” sometimes described in these patients [102].
Practical recommendations for the clinician
Neurological and pneumological dysfunction are strictly connected in PD patients. Pneumologists should be aware that breathing problems in this class of patients may be a direct consequence of disease progression and/or of the dopaminergic stimulation, as already mentioned for dyspnoea due to levodopa-induced diaphragmatic dyskinesias. Moreover, pneumologists should consider the spirometric abnormalities that could be found even in the early stages of the disease, and the potential therapeutic role on the airways function exercised by dopaminergic stimulation more than that seen with conventional inhaled drugs. Neurologists, in the same way, should always consider the role of pneumological evaluation in the clinical history of a PD patient and focus on respiratory function as a potential therapeutic target to improve quality of life in a patient complaining of breathing disturbances. Finally, the physician should remember also the potential benefit of pulmonary rehabilitation on functional respiratory tests and exercise tolerance even in the early stages [103], and it is reasonable to consider a respiratory training program in parallel with dopaminergic therapy in patients who report respiratory symptoms.
Conclusions
PD is frequently associated with respiratory disturbances, even in pre-motor stages and these should be considered as a part of the disease itself rather than a different problem. In this view, the presence of breathing symptoms should alert the physician of a PD not well controlled or in progression. Even if the role of anti-Parkinsonian drugs is still controversial, it should be considered that they may have a potential role in ameliorating pulmonary function as well as the possible negative contribution to muscle incoordination and worsening of shortness of breath in patients experiencing dyskinesias.
DBS may be considered for PD, and stimulation of the STN does not significantly impair respiratory drive, when delivered at low frequencies and short pulse width, even if no data are currently available on novel DBS targets and the development of respiratory alterations. In the near future, new targets such as the PPN may induce a better control of axial motor symptoms, potentially avoiding respiratory changes at the same time.
Finally, the presence of respiratory symptoms should be considered in patients with other form of Parkinsonism, even if more systematic studied are needed to investigate this topic, as well as needing more proof of the exact impact of a dopaminergic beneficial role in respiratory dysfunctions.
Footnotes
Author contributions: A.M. D'Arrigo, S. Floro, F. Bartesaghi and C. Casellato designed the review, performed the literature research and prepared the manuscript. A. Priori, T. Bocci, G.F. Sferrazza Papa and S. Centanni prepared the manuscript and reviewed the work.
Conflict of interest: A.M. D'Arrigo has nothing to disclose.
Conflict of interest: S. Floro has nothing to disclose.
Conflict of interest: F. Bartesaghi has nothing to disclose.
Conflict of interest: C. Casellato has nothing to disclose.
Conflict of interest: G.F Sferrazza Papa has nothing to disclose.
Conflict of interest: S. Centanni has nothing to disclose.
Conflict of interest: A. Priori has nothing to disclose.
Conflict of interest: T. Bocci has nothing to disclose.
References
- 1.Parkinson J. An essay on the shaking palsy. 1817. J Neuropsychiatry Clin Neurosci 2002; 14: 223–236. doi: 10.1176/jnp.14.2.223 [DOI] [PubMed] [Google Scholar]
- 2.Hovestadt A, Bogaard JM, Meerwaldt JD, et al. . Pulmonary function in Parkinson's disease. J Neurol Neurosurg Psychiatry 1989; 52: 329–333. doi: 10.1136/jnnp.52.3.329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehanna R, Jankovic J. Respiratory problems in neurologic movement disorders. Parkinsonism Relat Disord 2010; 16: 628–638. doi: 10.1016/j.parkreldis.2010.07.004 [DOI] [PubMed] [Google Scholar]
- 4.Tzelepis GE, McCool FD, Friedman JH, et al. . Respiratory muscle dysfunction in Parkinson's disease. Am Rev Respir Dis 1988; 138: 266–271. doi: 10.1164/ajrccm/138.2.266 [DOI] [PubMed] [Google Scholar]
- 5.Solomon NP, Hixon TJ. Speech breathing in Parkinson's disease. J Speech Lang Hear Res 1993; 36: 294–310. doi: 10.1044/jshr.3602.294 [DOI] [PubMed] [Google Scholar]
- 6.Levin OS, Khutorskaia OE, Amosova NA, et al. . Clinical and electromyographical analysis of peculiarities of parkinsonian syndrome in multiple system atrophy and Parkinson's disease. Zh Nevrol Psikhiatr Im S S Korsakova 2003; 103: 4–9. [PubMed] [Google Scholar]
- 7.Vincken WG, Gauthier SG, Dollfuss RE, et al. . Involvement of upper-airway muscles in extrapyramidal disorders. a cause of airflow limitation. N Engl J Med 1984; 311: 438–442. doi: 10.1056/NEJM198408163110704 [DOI] [PubMed] [Google Scholar]
- 8.Izquierdo-Alonso JL, Jimenez-Jimenez FJ, Cabrera-Valdivia F, et al. . Airway dysfunction in patients with Parkinson's disease. Lung 1994; 172: 47–55. doi: 10.1007/BF00186168 [DOI] [PubMed] [Google Scholar]
- 9.Sabaté M, González I, Ruperez F, et al. . Obstructive and restrictive pulmonary dysfunctions in Parkinson's disease. J Neurol Sci 1996; 138: 114–119. doi: 10.1016/0022-510X(96)00003-2 [DOI] [PubMed] [Google Scholar]
- 10.Onodera H, Okabe S, Kikuchi Y, et al. . Impaired chemosensitivity and perception of dyspnoea in Parkinson's disease. Lancet 2000; 356: 739–740. doi: 10.1016/S0140-6736(00)02638-6 [DOI] [PubMed] [Google Scholar]
- 11.Herer B, Arnulf I, Housset B. Effects of levodopa on pulmonary function in Parkinson's disease. Chest 2001; 119: 387–393. doi: 10.1378/chest.119.2.387 [DOI] [PubMed] [Google Scholar]
- 12.De Pandis MF, Starace A, Stefanelli F, et al. . Modification of respiratory function parameters in patients with severe Parkinson's disease. Neurol Sci 2002; 23: Suppl. 2, s69–s70. doi: 10.1007/s100720200074 [DOI] [PubMed] [Google Scholar]
- 13.Weiner P, Inzelberg R, Davidovich A, et al. . Respiratory muscle performance and the perception of dyspnea in Parkinson's disease. Can J Neurol Sci 2002; 29: 68–72. doi: 10.1017/S031716710000175X [DOI] [PubMed] [Google Scholar]
- 14.Sathyaprabha TN, Kapavarapu PK, Pal PK, et al. . Pulmonary functions in Parkinson's disease. Indian J Chest Dis Allied Sci 2005; 47: 251– 257. [PubMed] [Google Scholar]
- 15.Seccombe LM, Giddings HL, Rogers PG, et al. . Abnormal ventilatory control in Parkinson's disease—Further evidence for non-motor dysfunction. Respir Physiol Neurobiol 2011; 179: 300–304. doi: 10.1016/j.resp.2011.09.012 [DOI] [PubMed] [Google Scholar]
- 16.Baille G, Perez T, Devos D, et al. . Early occurrence of inspiratory muscle weakness in Parkinson's disease. PLoS ONE 2018; 13: e0190400. doi: 10.1371/journal.pone.0190400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shill H, Stacy M. Respiratory complications of Parkinson's disease. Semin Respir Crit Care Med 2002; 23: 261–266. doi: 10.1055/s-2002-33034 [DOI] [PubMed] [Google Scholar]
- 18.Braak H, Del Tredici K, Rüb U, et al. . Staging of brain pathology related to sporadic Parkinson's disease. Neurobiol Aging 2003; 24: 197–211. doi: 10.1016/S0197-4580(02)00065-9 [DOI] [PubMed] [Google Scholar]
- 19.Guindi GM, Bannister R, Gibson WP, et al. . Laryngeal electromyography in multiple system atrophy with autonomic failure. J Neurol Neurosurg Psychiatry 1981; 44: 49–53. doi: 10.1136/jnnp.44.1.49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Estenne M, Hubert M, De Troyer A. Respiratory-muscle involvement in Parkinson's disease. N Engl J Med 1984; 311: 1516–1517. doi: 10.1056/NEJM198412063112314 [DOI] [PubMed] [Google Scholar]
- 21.Neu HC, Connolly JJ Jr, Schwertley FW, et al. . Obstructive respiratory dysfunction in parkinsonian patients. Am Rev Respir Dis 1967; 95: 33–47. [DOI] [PubMed] [Google Scholar]
- 22.Jankovic J, Tintner R. Dystonia and parkinsonism. Parkinsonism Relat Disord 2001; 8: 109–121. doi: 10.1016/S1353-8020(01)00025-6 [DOI] [PubMed] [Google Scholar]
- 23.Estenne M, Hubert M, De Troyer A. Respiratory-muscle involvement in Parkinson's disease. N Engl J Med 1984; 311: 1516–1517. doi: 10.1056/NEJM198412063112314 [DOI] [PubMed] [Google Scholar]
- 24.Sabaté M, Rodriguez M, Méndez E, et al. . Obstructive and restrictive pulmonary dysfunction increases disability in Parkinson disease. Arch Phys Med Rehabil 1996; 77: 29–34. doi: 10.1016/S0003-9993(96)90216-6 [DOI] [PubMed] [Google Scholar]
- 25.Pal PK, Sathyaprabha TN, Tuhina P, et al. . Pattern of subclinical pulmonary dysfunctions in Parkinson's disease and the effect of levodopa. Mov Disord 2007; 22: 420–424. doi: 10.1002/mds.21330 [DOI] [PubMed] [Google Scholar]
- 26.Troche MS, Huebner I, Rosenbek JC, et al. . Respiratory-swallowing coordination and swallowing safety in patients with Parkinson's disease. Dysphagia 2011; 26: 218–224. doi: 10.1007/s00455-010-9289-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hammer MJ, Murphy CA, Abrams TM. Airway somatosensory deficits and dysphagia in Parkinson's disease. J Parkinsons Dis 2013; 3: 39–44. doi: 10.3233/JPD-120161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tuppy M, Barna BF, Alves-Dos-Santos L, et al. . Respiratory deficits in a rat model of Parkinson's disease. Neuroscience 2015; 297: 194–204. doi: 10.1016/j.neuroscience.2015.03.048 [DOI] [PubMed] [Google Scholar]
- 29.Zhang LY, Liu WY, Kang WY, et al. . Association of rapid eye movement sleep behavior disorder with sleep-disordered breathing in Parkinson's disease. Sleep Med 2016; 20: 110–115. doi: 10.1016/j.sleep.2015.12.018 [DOI] [PubMed] [Google Scholar]
- 30.Braak H, Brack E. Pathoanatomy of Parkinson's disease. J Neurol 2000; 247: Suppl. 2, II3–I10. [DOI] [PubMed] [Google Scholar]
- 31.Fernandes-Junior SA, Carvalho KS, Moreira TS, et al. . Correlation between neuroanatomical and functional respiratory changes observed in an experimental model of Parkinson's disease. Exp Physiol 2018; 103: 1377–1389. doi: 10.1113/EP086987 [DOI] [PubMed] [Google Scholar]
- 32.Gourine AV, Kasymov V, Marina N, et al. . Astrocytes control breathing through pH-dependent release of ATP. Science 2010; 329: 571–575. doi: 10.1126/science.1190721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wenker IC, Kréneisz O, Nishiyama A, et al. . Astrocytes in the retrotrapezoid nucleus sense H+ by inhibition of a Kir4. 1–Kir5. 1-like current and may contribute to chemoreception by a purinergic mechanism. J Neurophysiol 2010; 104: 3042–3052. doi: 10.1152/jn.00544.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lima JC, Oliveira LM, Botelho MT, et al. . The involvement of the pathway connecting the substantia nigra, the periaqueductal gray matter and the retrotrapezoid nucleus in breathing control in a rat model of Parkinson's disease. Exp Neurol 2018; 302: 46–56. doi: 10.1016/j.expneurol.2018.01.003 [DOI] [PubMed] [Google Scholar]
- 35.Subramanian HH, Holstege G. Stimulation of the midbrain periaqueductal gray modulates preinspiratory neurons in the ventrolateral medulla in the rat in vivo. J Comp Neurol 2013; 521: 3083–3098. doi: 10.1002/cne.23334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Holstege G. The periaqueductal gray controls brainstem emotional motor systems including respiration. Prog Brain Res 2014; 209: 379–405. [DOI] [PubMed] [Google Scholar]
- 37.Lopes LT, Biancardi V, Vieira EB, et al. . Participation of the dorsal periaqueductal grey matter in the hypoxic ventilatory response in unanaesthetized rats. Acta Physiol (Oxf) 2014; 211: 528–537. doi: 10.1111/apha.12254 [DOI] [PubMed] [Google Scholar]
- 38.Subramanian HH, Balnave RJ, Holstege G. The midbrain periaqueductal gray control of respiration. J Neurosci 2008; 28: 12274–12283. doi: 10.1523/JNEUROSCI.4168-08.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Killian KJ, Gandevia SC, Summers E, et al. . Effect of increased lung volume on perception of breathlessness, effort, and tension. J Appl Physiol Respir Environ Exerc Physiol 1984; 57: 686–691. [DOI] [PubMed] [Google Scholar]
- 40.Weiner WJ, Goetz CG, Nausieda PA, et al. . Respiratory dyskinesias: extrapyramidal dysfunction and dyspnea. Ann Intern Med 1978; 88: 327–331. doi: 10.7326/0003-4819-88-3-327 [DOI] [PubMed] [Google Scholar]
- 41.Jones BE. Paradoxical sleep and its chemical/structural substrates in the brain. Neuroscience 1991; 40: 637–656. doi: 10.1016/0306-4522(91)90002-6 [DOI] [PubMed] [Google Scholar]
- 42.Maria B, Sophia S, Michalis M, et al. . Sleep breathing disorders in patients with idiopathic Parkinson's disease. Respir Med 2003; 97: 1151–1157. doi: 10.1016/S0954-6111(03)00188-4 [DOI] [PubMed] [Google Scholar]
- 43.Diederich NJ, Vaillant M, Leischen M, et al. . Sleep apnea syndrome in Parkinson's disease. a case–control study in 49 patients. Mov Disord 2005; 20: 1413–1418. doi: 10.1002/mds.20624 [DOI] [PubMed] [Google Scholar]
- 44.De Cock VC, Abouda M, Leu S, et al. . Is obstructive sleep apnea a problem in Parkinson's disease? Sleep Med 2010; 11: 247–252. doi: 10.1016/j.sleep.2009.05.008 [DOI] [PubMed] [Google Scholar]
- 45.Apps MC, Sheaff PC, Ingram DA, et al. . Respiration and sleep in Parkinson's disease. J Neurol Neurosurg Psychiatry 1985; 48: 1240–1245. doi: 10.1136/jnnp.48.12.1240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Huang JY, Zhang JR, Shen Y, et al. . Effect of rapid eye movement sleep behavior disorder on obstructive sleep apnea severity and cognition of Parkinson's disease patients. Chin Med J 2018; 131: 899– 906. doi: 10.4103/0366-6999.229888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Neikrug AB, Liu L, Avanzino JA, et al. . Continuous positive airway pressure improves sleep and daytime sleepiness in patients with Parkinson disease and sleep apnea. Sleep 2014; 37: 177–185. doi: 10.5665/sleep.3332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Terzaghi M, Spelta L, Minafra B, et al. . Treating sleep apnea in Parkinson's disease with C-PAP: feasibility concerns and effects on cognition and alertness. Sleep Med 2017; 33: 114–118. doi: 10.1016/j.sleep.2017.01.009 [DOI] [PubMed] [Google Scholar]
- 49.Gross RD, Atwood CW, Ross SB, et al. . The coordination of breathing and swallowing in Parkinson's disease. Dysphagia 2008; 23: 136–145. doi: 10.1007/s00455-007-9113-4 [DOI] [PubMed] [Google Scholar]
- 50.Müller J, Wenning GK, Verny M, et al. . Progression of dysarthria and dysphagia in postmortem-confirmed parkinsonian disorders. Arch Neurol 2001; 58: 259–264. doi: 10.1001/archneur.58.2.259 [DOI] [PubMed] [Google Scholar]
- 51.Fuh JL, Lee RC, Wang SJ, et al. . Swallowing difficulty in Parkinson's disease. Clin Neurol Neurosurg 1997; 99: 106–112. doi: 10.1016/S0303-8467(97)80006-6 [DOI] [PubMed] [Google Scholar]
- 52.Nobrega AC, Rodrigues B, Melo A. Is silent aspiration a risk factor for respiratory infection in Parkinson's disease patients? Parkinsonism Relat Disord 2008; 14: 646–648. doi: 10.1016/j.parkreldis.2007.12.007 [DOI] [PubMed] [Google Scholar]
- 53.Ebihara S, Saito H, Kanda A, et al. . Impaired efficacy of cough in patients with Parkinson disease. Chest 2003; 124: 1009–1015. doi: 10.1378/chest.124.3.1009 [DOI] [PubMed] [Google Scholar]
- 54.Troche MS, Brandimore AE, Okun MS, et al. . Decreased cough sensitivity and aspiration in Parkinson disease. Chest 2014; 146: 1294–1299. doi: 10.1378/chest.14-0066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Leopold NA, Daniels SK. Supranuclear control of swallowing. Dysphagia 2010; 25: 250–257. doi: 10.1007/s00455-009-9249-5 [DOI] [PubMed] [Google Scholar]
- 56.Menezes C, Melo A. Does levodopa improve swallowing dysfunction in Parkinson's disease patients? J Clin Pharm Ther 2009; 34: 673–676. doi: 10.1111/j.1365-2710.2009.01031.x [DOI] [PubMed] [Google Scholar]
- 57.Sutton JP. Dysphagia in Parkinson's disease is responsive to levodopa. Parkinsonism Relat Disord 2013; 19: 282–284. doi: 10.1016/j.parkreldis.2012.11.007 [DOI] [PubMed] [Google Scholar]
- 58.Fujii Y. Olprinone/dopamine combination for improving diaphragmatic fatigue in pentobarbital-anesthetized dogs. Curr Ther Res Clin Exp 2006; 67: 204–213. doi: 10.1016/j.curtheres.2006.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Aubier M, Murciano D, Menu Y, et al. . Dopamine effects on diaphragmatic strength during acute respiratory failure in chronic obstructive pulmonary disease. Ann Intern Med 1989; 110: 17–23. doi: 10.7326/0003-4819-110-1-17 [DOI] [PubMed] [Google Scholar]
- 60.Gros P, Mery VP, Lafontaine AL, et al. . Obstructive sleep apnea in Parkinson's disease patients: effect of Sinemet CR taken at bedtime. Sleep Breath 2016; 20: 205–212. doi: 10.1007/s11325-015-1208-9 [DOI] [PubMed] [Google Scholar]
- 61.Bhatt MH, Keenan SP, Fleetham JA, et al. . Pleuropulmonary disease associated with dopamine agonist therapy. Ann Neurol 1991; 30: 613–616. doi: 10.1002/ana.410300416 [DOI] [PubMed] [Google Scholar]
- 62.Jankovic J, Nour F. Respiratory dyskinesia in Parkinson's disease. Neurology 1986; 36: 303–304.doi: 10.1212/WNL.36.2.303-b [DOI] [PubMed] [Google Scholar]
- 63.Ko PW, Kang K, Lee HW. Levodopa-induced respiratory dysfunction confirmed by levodopa challenge test: a case report. Medicine (Baltimore) 2018; 97: e12488. doi: 10.1097/MD.0000000000012488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lim A, Leow L, Huckabee ML, et al. . A pilot study of respiration and swallowing integration in Parkinson's disease: “on” and “off” levodopa. Dysphagia 2008; 23: 76–81. doi: 10.1007/s00455-007-9100-9 [DOI] [PubMed] [Google Scholar]
- 65.Fink M, Klebanoff L, Lennihan L, et al. . Acute respiratory failure during drug manipulation in patients with Parkinson disease: PP578. Neurology 1989; 39. [Google Scholar]
- 66.Riley DE, Grossman G, Martin L. Acute respiratory failure from dopamine agonist withdrawal. Neurology 1992; 42: 1843–1844. doi: 10.1212/WNL.42.9.1840-c [DOI] [PubMed] [Google Scholar]
- 67.de Bruin PF, de Bruin VM, Lees AJ, et al. . Effects of treatment on airway dynamics and respiratory muscle strength in Parkinson's disease. Am Rev Respir Dis 1993; 148: 1576–1580. doi: 10.1164/ajrccm/148.6_Pt_1.1576 [DOI] [PubMed] [Google Scholar]
- 68.Wei L, Chen Y. Neuroleptic malignant-like syndrome with a slight elevation of creatine-kinase levels and respiratory failure in a patient with Parkinson's disease. Patient Prefer Adherence 2014; 8: 271–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Monteiro L, Souza-Machado A, Valderramas S, et al. . The effect of levodopa on pulmonary function in Parkinson's disease: a systematic review and meta-analysis. Clin Ther 2012; 34: 1049–1055. doi: 10.1016/j.clinthera.2012.03.001 [DOI] [PubMed] [Google Scholar]
- 70.Reimer J, Kuhlmann A, Müller T. Neuroleptic malignant-like syndrome after rapid switch from bromocriptine to pergolide. Parkinsonism Relat Disord 2002; 9: 115–116. doi: 10.1016/S1353-8020(01)00045-1 [DOI] [PubMed] [Google Scholar]
- 71.Ikebe SI, Harada T, Hashimoto T, et al. . Prevention and treatment of malignant syndrome in Parkinson's disease: a consensus statement of the malignant syndrome research group. Parkinsonism Relat Disord 2003; 9: Suppl. 1, S47–S49. doi: 10.1016/S1353-8020(02)00123-2 [DOI] [PubMed] [Google Scholar]
- 72.Bonnici A, Ruiner CE, St-Laurent L, et al. . An interaction between levodopa and enteral nutrition resulting in neuroleptic malignant-like syndrome and prolonged ICU stay. Ann Pharmacother 2010; 44: 1504–1507. doi: 10.1345/aph.1P242 [DOI] [PubMed] [Google Scholar]
- 73.Lang AE, Rodriguez RL, Boyd JT, et al. . Integrated safety of levodopa-carbidopa intestinal gel from prospective clinical trials. Mov Disord 2016; 31: 538–546. doi: 10.1002/mds.26485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hopfner F, Höglinger GU, Kuhlenbäumer G, et al. . β-adrenoreceptors and the risk of Parkinson's disease. Lancet Neurol 2020; 19: 247–254. doi: 10.1016/S1474-4422(19)30400-4 [DOI] [PubMed] [Google Scholar]
- 75.Hernán MA, Takkouche B, Caamaño-Isorna F, et al. . A meta-analysis of coffee drinking, cigarette smoking, and the risk of Parkinson's disease. Ann Neurol 2002; 52: 276–284. doi: 10.1002/ana.10277 [DOI] [PubMed] [Google Scholar]
- 76.Nishtala PS, Salahudeen MS, Hilmer SN. Anticholinergics: theoretical and clinical overview. Expert Opin Drug Saf 2016; 15: 753–768. doi: 10.1517/14740338.2016.1165664 [DOI] [PubMed] [Google Scholar]
- 77.Benarroch EE. Effects of acetylcholine in the striatum: recent insights and therapeutic implications. Neurology 2012; 79: 274–281. doi: 10.1212/WNL.0b013e31825fe154 [DOI] [PubMed] [Google Scholar]
- 78.Gupta P, O'Mahony MS. Potential adverse effects of bronchodilators in the treatment of airways obstruction in older people. Drugs Aging 2008; 25: 415–443. doi: 10.2165/00002512-200825050-00005 [DOI] [PubMed] [Google Scholar]
- 79.Kataoka H, Yanase M, Kawahara M, et al. . Subthalamic nucleus stimulation in Parkinson's disease is associated with a risk of fixed epiglottis. BMJ Case Rep 2009; 2009: bcr08.2008.0706. doi: 10.1136/bcr.08.2008.0706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Törnqvist AL, Ahlström G, Widner H, et al. . Fulfilment of patients’ goals after thalamic deep brain stimulation: a follow-up study. Parkinsonism Relat Disord 2007; 13: 29–34. doi: 10.1016/j.parkreldis.2006.06.005 [DOI] [PubMed] [Google Scholar]
- 81.Hammer MJ, Barlow SM, Lyons KE, et al. . Subthalamic nucleus deep brain stimulation changes speech respiratory and laryngeal control in Parkinson's disease. J Neurol 2010; 257: 1692–1702. doi: 10.1007/s00415-010-5605-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.French IT, Muthusamy KA. A review of the pedunculopontine nucleus in Parkinson's disease. Front Aging Neurosci 2018; 10: 99. doi: 10.3389/fnagi.2018.00099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Fink AM, Dean C, Piano MR, et al. . The pedunculopontine tegmentum controls renal sympathetic nerve activity and cardiorespiratory activities in nembutal-anesthetized rats. PLoS ONE 2017; 12: e0187956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lima JD, Sobrinho CR, Falquetto B, et al. . Cholinergic neurons in the pedunculopontine tegmental nucleus modulate breathing in rats by direct projections to the retrotrapezoid nucleus. J Physiol (Lond) 2019; 597: 1919–1934. doi: 10.1113/JP277617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hyam JA, Wang S, Roy H, et al. . The pedunculopontine region and breathing in Parkinson's disease. Ann Clin Transl Neurol 2019; 6: 837–847. doi: 10.1002/acn3.752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gariépy JF, Missaghi K, Chevallier S, et al. . Specific neural substrate linking respiration to locomotion. Proc Natl Acad Sci USA 2012; 109: E84–E92. doi: 10.1073/pnas.1113002109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lilker ES, Woolf CR. Pulmonary function in Parkinson's syndrome: the effect of thalamotomy. CMAJ 1968; 99: 752. [PMC free article] [PubMed] [Google Scholar]
- 88.Köllensperger M, Geser F, Seppi K, et al. . Red flags for multiple system atrophy. Mov Disord 2008; 23: 1093–1099. doi: 10.1002/mds.21992 [DOI] [PubMed] [Google Scholar]
- 89.Vetrugno R, Provini F, Cortelli P, et al. . Sleep disorders in multiple system atrophy: a correlative video-polysomnographic study. Sleep Med 2004; 5: 21–30. doi: 10.1016/j.sleep.2003.07.002 [DOI] [PubMed] [Google Scholar]
- 90.Benarroch EE, Schmeichel AM, Low PA, et al. . Depletion of putative chemosensitive respiratory neurons in the ventral medullary surface in multiple system atrophy. Brain 2007; 130: 469–475. doi: 10.1093/brain/awl357 [DOI] [PubMed] [Google Scholar]
- 91.Presti MF, Schmeichel AM, Low PA, et al. . Degeneration of brainstem respiratory neurons in dementia with Lewy bodies. Sleep 2014; 37: 373–378. doi: 10.5665/sleep.3418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Takahashi S, Mizukami K, Arai T, et al. . Ventilatory response to hypercapnia predicts dementia with Lewy bodies in late-onset major depressive disorder. J Alzheimers Dis 2016; 50: 751–758. doi: 10.3233/JAD-150507 [DOI] [PubMed] [Google Scholar]
- 93.Mizukami K, Homma T, Aonuma K, et al. . Decreased ventilatory response to hypercapnia in dementia with Lewy bodies. Ann Neurol 2009; 65: 614–617. doi: 10.1002/ana.21613 [DOI] [PubMed] [Google Scholar]
- 94.Ebihara T, Gui P, Ooyama C, et al. . Cough reflex sensitivity and urge-to-cough deterioration in dementia with Lewy bodies. ERJ Open Res 2020; 6: 00108–02019. doi: 10.1183/23120541.00108-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bannister R, Gibson W, Micheals L, et al. . Laryngeal abductor paralysis in multiple system atrophy. A report on three necropsied cases, with observations on the laryngeal muscles and the nuclei ambigui. Brain 1981; 104: 351–368. doi: 10.1093/brain/104.2.351 [DOI] [PubMed] [Google Scholar]
- 96.Merlo IM, Occhini A, Pacchetti C, et al. . Not paralysis, but dystonia causes stridor in multiple system atrophy. Neurology 2002; 58: 649–652. doi: 10.1212/WNL.58.4.649 [DOI] [PubMed] [Google Scholar]
- 97.Silber MH, Levine S. Stridor and death in multiple system atrophy. Mov Disord 2000; 15: 699–704. doi: [DOI] [PubMed] [Google Scholar]
- 98.Ghorayeb I, Yekhlef F, Bioulac B, et al. . Continuous positive airway pressure for sleep-related breathing disorders in multiple system atrophy: long-term acceptance. Sleep Med 2005; 6: 359–362. doi: 10.1016/j.sleep.2004.10.002 [DOI] [PubMed] [Google Scholar]
- 99.Marion MH, Klap P, Perrin A, et al. . Stridor and focal laryngeal dystonia. Lancet 1992; 339: 457–458. doi: 10.1016/0140-6736(92)91060-L [DOI] [PubMed] [Google Scholar]
- 100.Gilman S, Chervin RD, Koeppe RA, et al. . Obstructive sleep apnea is related to a thalamic cholinergic deficit in MSA. Neurology 2003; 61: 35–39. doi: 10.1212/01.WNL.0000073624.13436.32 [DOI] [PubMed] [Google Scholar]
- 101.De Bruin VS, Machado C, Howard RS, et al. . Nocturnal and respiratory disturbances in Steele–Richardson–Olszewski syndrome (progressive supranuclear palsy). Postgrad Med J 1996; 72: 293–296. doi: 10.1136/pgmj.72.847.293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hazoui P, Chenuel B, Barroche G. Interactions between volitional and automatic breathing during respiratory apraxia. Respir Physiol Neurobiol 2006; 152: 169–175. doi: 10.1016/j.resp.2005.08.004 [DOI] [PubMed] [Google Scholar]
- 103.Köseoğlu F, Inan L, Ozel S, et al. . The effects of a pulmonary rehabilitation program on pulmonary function tests and exercise tolerance in patients with Parkinson's disease. Funct Neurol 1997; 12: 319–325. [PubMed] [Google Scholar]