Abstract
Pott’s puffy tumor is characterized by forehead swelling from subperiosteal abscess and frontal bone osteomyelitis. It is encountered mainly in children; rarely in adults. When it does occur in the latter population, the most common risk factors include head trauma, sinusitis, or cocaine abuse. Generally, the organisms thought to be involved include streptococci, staphylococci and oral anaerobic flora. We present a case of a 53 year old female who presented with forehead swelling of 3 month duration after a dental procedure, found to be secondary to Actinomyces naeslundii. Actinomyces is a very rare etiology of this disease and has been reported only twice earlier in the literature. We present an uncommon infectious disease along with summary of clinical characteristics of this entity in the adult population.
Keywords: Pott’s puffy tumor, Actinomycosis
Introduction
Pott’s Puffy Tumor (PPT) is a clinical diagnosis of a subperiosteal abscess and osteomyelitis of the frontal bone [1]. It is encountered mainly in children, and rarely seen in adults [1]. When it does occur in the latter population, the most common risk factors include head trauma, sinusitis, or cocaine abuse [1]. Complications from PPT include meningitis, epidural empyema, frontal lobe abscess, and cavernous sinus thrombosis; hence the need for prompt diagnosis and aggressive treatment [1].
Case report
A 53 year-old Caucasian female with history of sleep apnea and acid reflux presented with gradual swelling of her forehead for 3 months. She denied having any history of chronic sinusitis or illicit drug use. She did smoke tobacco, 1 pack per day for 30 years. About 6 months prior to presentation, the patient had undergone a tooth extraction; shortly thereafter that she developed symptoms of sinus pressure and congestion. She was initially treated with multiple courses of antimicrobials and steroids for presumed sinusitis without improvement. About three weeks prior to presenting, the patient underwent sinus surgery and was placed on oral levofloxacin for five days. No cultures were obtained at that time.
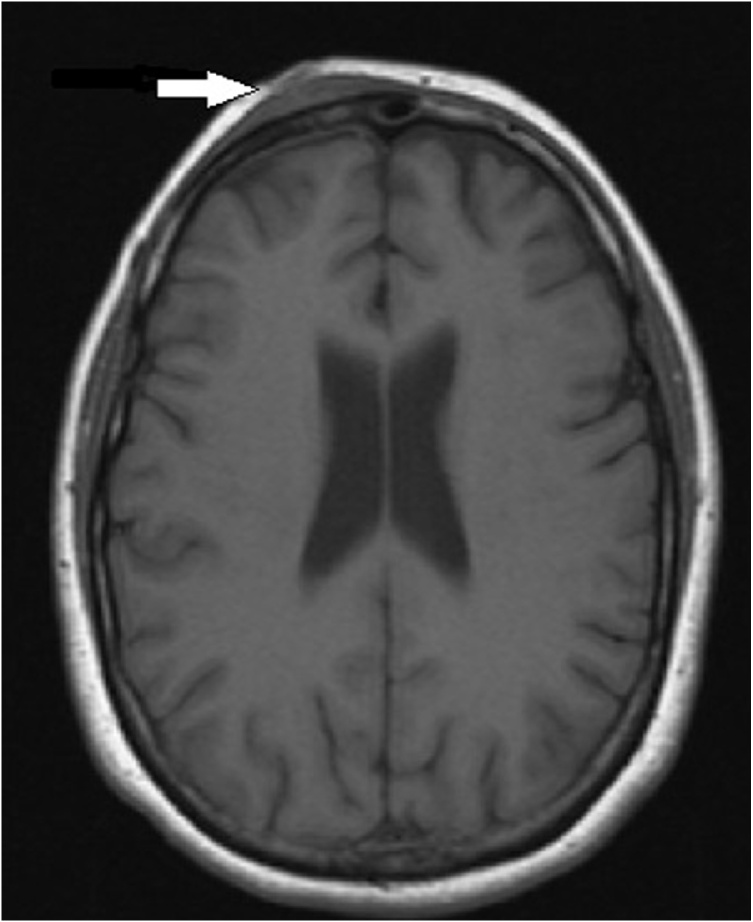
About a week after surgery, the patient started to develop fevers, chills and worsening headache. She reported that while she did have forehead swelling prior to surgery on her sinuses, it became much more pronounced post-operatively. Three weeks after surgery the patient had a CT head that revealed a peripherally enhancing fluid collection measuring 3.1 cm × 5.9 cm along the right frontal scalp in close proximity to the frontal sinuses and enhancement of the frontal subdural space. MRI head confirmed the findings (Fig. 1). The patient underwent surgical debridement of the abscess with frontal sinus trephination. Cultures were obtained, which grew Actinomyces naeslundi. Due to history of being allergic to penicillin the patient was treated with intravenous (IV) ceftriaxone for 9 weeks and then transitioned to oral doxycycline for a total of 6 months of therapy. At 6 month follow up, her symptoms and radiological abnormalities had resolved.
Fig. 1.
MRI head revealing right frontal subgaleal abscess along with involvement of the right frontal bone.
Discussion
Subperiosteal abscess and frontal bone osteomyelitis, also known as Pott’s Puffy Tumor (PPT) was first described by Sir Percival Pott in 1768 in association with head trauma and sinusitis [2]. It occurs as the result of infection traversing through the venous drainage of the frontal sinus or due to direct inoculation to the frontal bone [3]. In order to better understand the clinical characteristics of this disease in the adult population, we reviewed case reports (a total of 47 cases, Table 1) of PPT in adults to determine common risk factors, microbial involvement, management, and outcome of this relatively rare condition. The details are tabulated, and some salient features are described here. With regards to precipitating or underlying risk factors, chronic sinusitis, penetrating defects (either through trauma or surgical interventions), dental issues, and cocaine abuse appeared to be present in majority of the patients. It is felt that the presence of cocaine or tobacco use results in disruption of the mucosal barrier of the nasal passage ways, predisposing to infection [1]. In our patient, we suspect that the preceding dental procedure was the inciting event leading to the development of PPT.
Table 1.
Clinical characteristics of adult patients with Pott’s puffy tumor.
| Ref No. |
Sex | Age | Past medical history | Precipitating cause | Duration of onset | Organism | Antibiotic | Outcome |
|---|---|---|---|---|---|---|---|---|
| [6] | M | 49 | No prior history | Insect bite | 1 wk | Staph aureus | Flucloxacillin, fusidic acid, metronidazole for 6 weeks | Resolved at 6 weeks |
| [7] | F | 55 | No prior history | Prior surgical history along the frontal bone 8 yr ago | 2 mo | Staph aureus | Antibiotic NR, treated for 8 weeks | NR |
| [8] | M | 55 | Alcoholism, cirrhosis, epilepsy, tobacco abuse, HTN | Prior history of sinus surgery | 1 mo | Viridans group strep | Vancomycin and clindamycin, unknown duration | Patient lost to follow up |
| [9] | F | 54 | Cocaine/heroin, tobacco abuse, hepatitis C | Trauma to forehead | 1 mo | Coagulase negative Staphylococci and beta-hemolytic Streptococci | 2.4 million units of benzathine penicillin; 2 IM injections | Resolution by day 5 |
| [10] | M | 25 | Allergic rhinitis and asthma | No known cause | 3 wk | Staph aureus | Ceftriaxone 2 g IV daily and then switched to PO antibiotics for 8 weeks (did not specify antibiotic) | Resolved at 6 month follow up |
| [11] | M | 33 | No prior medical history | No known cause | 5 mo | Staph aureus, Peptostreptococcus, S. pneumoniae, H. influenzae | Ceftriaxone 2 g Q 12 h and metronidazole for 2 weeks, followed by oral metronidazole and amoxicillin-clavulanate for 4 weeks | No recurrence for 7 yrs |
| [12] | M | NR | Hx of headaches and recurrent abscesses along the frontal soft tissue | No known cause | Not known | Strep anginosus | Moxifloxacin and metronidazole for 3 months | NR |
| [13] | M | 41 | Chronic sinusitis, tobacco use, cocaine use | No known cause | 26 days | Strep intermedius | Ceftriaxone and metronidazole, unknown duration | NR |
| [14] | M | 37 | Chronic exophthalmia | No known cause | 2 yr | Mycoplasma | Doxycycline, unknown duration | Symptoms resolved at 2 months |
| [15] | M | 46 | No prior medical history | No known cause | 6 mo | No organism identified by culture | NR | Recurred twice and required second I&D |
| [16] | M | 26 | No prior medical history | No known cause | 2 mo | H. influenzae | antibiotic NR - for 5 weeks | resolved |
| [16] | M | 34 | No prior medical history | Cocaine use | 6 wk | B. melaninogenicus, Fusobacterium, Propionibacterium, group A Strep | IV ampicillin/sulbactam 2 wks then oral amoxicillin/clavulaunate for 4 wks | NR |
| [16] | F | 54 | No prior medical history | No known cause | Not known |
No organism isolated | PO amox/clav and cloxacillin for 1 mo, PO penicillin for 1 mo | resolved |
| [16] | M | 83 | Unknown | Head trauma | 4 yr | H. influenzae | Ceftriaxone for 2 weeks followed by cefprozil for 4 week | No recurrence for 1 yr f/u |
| [17] | M | 74 | Unknown | Scalp injections for hair loss | 2 mo | Staph aureus | IV nafcillin 1 mo, Po dicloxacillin 4 weeks | resolved |
| [18] | M | 21 | No prior medical history | Dental sepsis | 3 wk | Streptococcus intermedius, Bacteroides melaninogenicus | 4 weeks of IV ampicillin | resolved |
| [19] | M | 53 | None | Head trauma | 3 wk | Streptococcus milleri | Unknown | Died 5 days after admission |
| [20] | M | 39 | None | No known cause | 3 mo | Streptococcus milleri | IV benzyl penicillin for 3 weeks followed by amoxicillin for 3 weeks | resolved |
| [21] | F | 67 | None | No known cause | Not known |
Pseudomonas aeruginosa | Unknown | NR |
| [22] | M | 58 | Diabetes mellitus | Head trauma | 2 mo | No organism isolated | Cefuroxime, unknown duration | No recurrence |
| [23] | M | 27 | Diabetes mellitus | Head trauma 13 yrs prior | 3 wk | Staph aureus | NR | Unknown |
| [24] | M | 35 | No prior medical problems | No known cause | 9 mo | Aspergillus flavus | NR | No recurrence at 3 mo f/u |
| [25] | F | 62 | Diabetes, CKD, HTN | No known cause | 1 wk | mucormycosis | Amphotericin B for 3 weeks | No recurrence |
| [26] | M | 54 | Hx of frontal bone reconstruction 30 yrs prior | URI- cold virus | 15 days | No organism isolated | Ampicillin/sulbactam for 10 days followed by amoxicillin/clavulanate for 15 days | Did well at 24 month follow up |
| [1] | M | 37 | No prior medical history | No known cause | 1 mo | unknown | Unknown | No recurrence |
| [1] | M | 36 | No prior medical history | No known cause | 1 mo | unknown | Unknown | No recurrence |
| [1] | M | 76 | Aplastic anemia, Diabetes | No known cause | 2 wk | Streptococcus anginosus, Micromonas micros | Unknown | No Recurrence |
| [1] | M | 38 | History of cranioplasty for pituitary tumor | No known cause | 2 days | Prevotella oralis, Fusobacterium, Micromonas micros | Unknown | Had recurrence requiring further surgical intervention |
| [1] | M | 28 | No prior medical history | No known cause | 2 yr | unknown | Unknown | No recurrence |
| [27] | F | 21 | Pregnancy | No known cause | not knwon |
Strep milleri | IV ceftriaxone for 3 weeks, oral amoxicillin/clavulanate for 4 weeks | Unknown |
| [28] | M | 37 | No prior medical history | Traumatic head injury | 1 mo | No growth | Ciprofloxacin 3 weeks | Resolved at 6 mo follow up |
| [29] | M | 60 | HTN, DM | No known cause | 8 wks | Strep anginosus | Ceftriaxone and metronidazole for 6 wks | 2 wk f/u swelling resolved |
| [30] | F | 41 | rhinosinusitis | No known cause | not known |
Peptostreptococcus prevotii, Streptococcus constellatus | Amp/sulbactam, vancomycin, meropenem, netilmycin For 4−8 weeks |
Deceased |
| [30] | M | 60 | rhinosinusitis | No known cause | Proteus | Amp/sulbactam 4−8 weeks |
Resolved at 6 mo | |
| [30] | + | 27 | rhinosinusitis | No known cause | unknown | Amp/sulbactam 4−8 weeks |
Resolved | |
| [30] | M | 24 | Rhinosinusitis, | No known cause | E. coli and staph aureus | Amp/sulbactam, meropenem, netilmycin 6 weeks |
Resolved at 3 months | |
| [31] | M | 56 | sinusitis | Traumatic injury | 1 month | No growth | IV antibiotics for 1 month, type NR | Drain removed and had full recovery at 3 months follow up |
| [32] | F | 72 | NR | No known cause | 4 yr | MSSA and Coagulase negative Staphylococci | A third generation cephalosporin, duration NR | No recurrence at one year follow up |
| [33] | F | 62 | No prior medical problems | No known cause | 6 mo | Prevotella | Clindamycin for 2 weeks, ertapenem + metronidazole for 6 weeks and then clindamycin for another 6 weeks | Resolved at 12 month follow up |
| [34] | M | 21 | sinusitis | Teeth extractions | 3 wk | Eikenella corrodens, Prevotella bivia, streptococcus intermedius | IV vancomycin and metronidazole for 4 weeks, then PO moxifloxacin for unknown duration | Resolved at 6 month follow u[p |
| [35] | M | 29 | none | trauma | 5 yr after surgery | Staph aureus | Levofloxacin, duration NR | Refused surgery, recurred after 2 months |
| [36] | M | 27 | none | Poor dentition | unknown | unknown | Broad spectrum abx for 6 weeks | Resolved without surgical intervention |
| [37] | M | 61 | none | Prior hx of Pott’s puffy tumor 5 mo prior | 5 day | Unknown | Unknown | Unknown |
| [38] | M | 63 | Chronic rhinosinusitis | No known cause | 2 wk | Strep milleri | Co-amoxiclav, unknown duration | Unknown |
| [2] | F | 58 | Recurrent sinusitis | No known cause | 3 wk | Pasteurella multocida | IV cefotaxime and PO clindamycin for four weeks followed by PO penicillin for 5 mo | Required further debridement 5 months later |
| [4] | M | 79 | HTN, prostate cancer, CKD | No known cause | unknown | Actinomyces | Antibiotics for 6 months; po course with amoxicillin-clavulanate | unknown |
| [5] | M | 52 | none | Trauma | 1 mo | Actinomyces, Fusobacterium, Propionibacterium | 4 weeks IV antibiotic vancomycin, ceftazidime, metronidazole; then 4 weeks oral amoxicillin | Resolved at 6 mo follow up |
NR: not reported.
Symptom onset ranged from weeks to years, depending on the risk factors and type of organism implicated. Microbes like Actinomyces and anaerobes are more indolent compared to others like Staphylococcus aureus or agents of mucormycosis which tend to be more aggressive and onset of clinical symptoms tends to be relatively faster. Of these 47 cases reviewed, Actinomyces was reported in two previous cases [4,5].
Treatment most often involves surgical debridement followed by antimicrobial therapy for 4−8 weeks targeted towards the isolated pathogens [1]. In the cases with unknown bacterial involvement, antimicrobials were targeted towards α-hemolytic streptococci and anaerobes. The majority of cases had good outcomes, with near complete resolution of symptoms. Our patient was treated for 9 weeks with IV ceftriaxone, followed by 6 months of PO doxycycline due to the presence of Actinomyces naeslundi which generally requires a longer course of treatment.
Pott’s puffy tumor should be considered as a potential diagnosis in people who present with a forehead swelling, particularly in the presence of known risk factors such as sinusitis, head trauma, dental procedures, and cocaine abuse. While staphylococci and streptococci have been commonly implicated, rarely Actinomyces may be encountered, especially in indolent cases.
Credit author statement
All the authors have contributed to the writing of the manuscript of the case report.
Sources of funding
No funding applicable to this article
Consent
Not applicable. We have ensured to not report any potential identifying information in the manuscript.
Declaration of Competing Interest
The authors report no declarations of interest.
References
- 1.Akiyama K., Karaki M., Mori N. Evaluation of adult Pott’s puffy tumor: our five cases and 27 literature cases. Laryngoscope. 2012;122:2382–2388. doi: 10.1002/lary.23490. [DOI] [PubMed] [Google Scholar]
- 2.Skomro R., McClean K.L. Frontal osteomyelitis (Pott’s puffy tumour) associated with Pasteurella multocida- A case report and review of the literature. Can J Infect Dis. 1998;9:115–1121. doi: 10.1155/1998/457984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldberg A.N., Oroszlan G., Anderson T.D. Complications of frontal sinusitis and their management. Otolaryngol Clin North Am. 2001;34:211–225. doi: 10.1016/s0030-6665(05)70307-8. [DOI] [PubMed] [Google Scholar]
- 4.Terre Falcon R., Gil-Paraiso P., Ayerbe-Torrero V., Bernat-Gili A., Sanchez-Rubio P. Frontal sinus osteomyelitis by actinomycosis: pott’s puffy tumor. Alternative endoscopic treatment. O.R.L. Aragon. 2013;16:24–25. [Google Scholar]
- 5.Pellejero J.C., Muñoz A.L., Elenwoke N., Franco S.C. Pott’s puffy tumor by Actinomyces after minor head trauma. Neurocirugia (Astur) 2019;304:198–201. doi: 10.1016/j.neucir.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 6.Raja V., Low C., Sastry A., Moriarty B. Pott’s puffy tumor following an insect bite. J Postgrad Med. 2007;53:114–116. doi: 10.4103/0022-3859.32212. [DOI] [PubMed] [Google Scholar]
- 7.Minutilli E., Pompucci A., Anile C. Cutaneous fistula is a rare presentation of Pott’s puffy tumour. J Plast Reconstr Aesthet Surg. 2008;61:1246–1248. doi: 10.1016/j.bjps.2008.01.026. [DOI] [PubMed] [Google Scholar]
- 8.Lamoreau K.P., Fanciullo L.M. Pott’s puffy tumour mimicking preseptal cellulitis. Clin Exp Optom. 2008;91:400–402. doi: 10.1111/j.1444-0938.2007.00234.x. [DOI] [PubMed] [Google Scholar]
- 9.Martinez-Diaz G.J., Hsia R. Pott’s puffy tumor after minor head trauma. Am J Emerg Med. 2008;26:739. doi: 10.1016/j.ajem.2007.11.038. [DOI] [PubMed] [Google Scholar]
- 10.Jung J., Lee H.C., Park I.H., Lee H.C.M. Endoscopic endonasal treatment of a Pott’s puffy tumor. Clin Exp Otorhinolaryngol. 2012;5:112–115. doi: 10.3342/ceo.2012.5.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Perić A., Milojević M., Ivetić D. A Pott’s puffy tumor associated with epidural-cutaneous fistula and epidural abscess: case report. Balkan Med. 2017;34:284–287. doi: 10.4274/balkanmedj.2016.1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ball S.L., Carrie S. Pott’s puffy tumour: a forgotten diagnosis. BMJ Case Rep. 2015 doi: 10.1136/bcr-2015-211099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bannon P., McCormack R.F. Pott’s puffy tumor and epidural abscess arising from pansinusitis. J Emerg Med. 2011;41:616–622. doi: 10.1016/j.jemermed.2008.04.050. [DOI] [PubMed] [Google Scholar]
- 14.Ciobanu A.M., Roşca T., Vlădescu C.T. Frontal epidural empyema (Pott’s puffy tumor) associated with Mycoplasma and depression. Rom J Morphol Embryol. 2014;55:1203–1207. [PubMed] [Google Scholar]
- 15.Tatsumi S., Ri M., Higashi N., Wakayama N., Matsune S., Tosa M. Pott’s puffy tumor in an adult: a case report and review of literature. J Nippon Med Sch. 2016;83:211–214. doi: 10.1272/jnms.83.211. [DOI] [PubMed] [Google Scholar]
- 16.Verbon A., Husni R.N., Gordon S.M., Lavertu P., Keys T.F. Pott’s puffy tumor due to Haemophilus influenzae: case report and review. Clin Infect Dis. 1996;23:1305–1307. doi: 10.1093/clinids/23.6.1305. [DOI] [PubMed] [Google Scholar]
- 17.Koch S.E., Wintroub B.U. Pott’s puffy tumor. A clinical marker for osteomyelitis of the skull. Arch Dermatol. 1985;121:548–549. [PubMed] [Google Scholar]
- 18.Chandy B., Todd J., Stucker F.J., Nathan C.A. Pott’s puffy tumor and epidural abscess arising from dental sepsis: a case report. Laryngoscope. 2001;111:1732–1734. doi: 10.1097/00005537-200110000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Tattersall R., Tattersall R. Pott’s puffy tumour. Lancet. 2002;359:1060–1063. doi: 10.1016/S0140-6736(02)08098-4. [DOI] [PubMed] [Google Scholar]
- 20.Kung S.W., Chan D.T.M., Suen P.Y., Boet R., Poon W.S. Pott’s puffy tumour. Hong Kong Med J. 2002;8:381–382. [PubMed] [Google Scholar]
- 21.Canbaz B., Tanriverdi T., Kaya A.H., Tüzgen S. Pott’s puffy tumour: a rare clinical entity. Lancet Infect Dis. 2003;3:721. doi: 10.1016/s1473-3099(03)00805-3. [DOI] [PubMed] [Google Scholar]
- 22.Goldfarb A., Hocwald E., Gross M., Eliashar R. Frontal sinus cutaneous fistula: a complication of Pott’s puffy tumor. Otolaryngol Head Neck Surg. 2004;130:490–491. doi: 10.1016/j.otohns.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 23.Evliyaoglu C., Bademci G., Yucel E., Keskil S. Pott’s puffy tumor of the vertex years after trauma in a diabetic patient: case report. Neurocirugia (Astur) 2005;16:54–57. doi: 10.1016/s1130-1473(05)70435-8. [DOI] [PubMed] [Google Scholar]
- 24.Panda N.K., Reddy C.E.E. Primary frontal sinus aspergillosis: an uncommon occurrence. Mycoses. 2005;48:235–237. doi: 10.1111/j.1439-0507.2005.01078.x. [DOI] [PubMed] [Google Scholar]
- 25.Effat K.G., Karam M., El-Kabani A. Pott’s puffy tumour caused by mucormycosis. J Laryngol Otol. 2005;119:643–645. doi: 10.1258/0022215054516304. [DOI] [PubMed] [Google Scholar]
- 26.Collet S., Grulois V., Ph Eloy, Ph Rombaux, Bertrand B. Pott’s puffy tumour as a late complication of a frontal sinus reconstruction: a case report and literature review. Rhinology. 2009;47:470–475. doi: 10.4193/Rhin07.060. [DOI] [PubMed] [Google Scholar]
- 27.Domville-Lewis C., Friedland P.L., Santa Maria P.L. Pott’s puffy tumour and intracranial complications of frontal sinusitis in pregnancy. J Laryngol Otol. 2013;127:S35–S38. doi: 10.1017/S0022215112001673. [DOI] [PubMed] [Google Scholar]
- 28.Clarós P., Ahmed H., Clarós A. Post-traumatic Pott’s puffy tumour: a case report. Eur Ann Otorhinolaryngol Head Neck Dis. 2016;133:119–121. doi: 10.1016/j.anorl.2015.08.018. [DOI] [PubMed] [Google Scholar]
- 29.Miller B. A 60-year-old man with forehead swelling. Cleve Clin J Med. 2016;83:95. doi: 10.3949/ccjm.83a.15011. [DOI] [PubMed] [Google Scholar]
- 30.Ketenci I., Unlu Y., Tucer B., Vural A. The Pott’s puffy tumor: a dangerous sign for intracranial complications. Eur Arch Otorhinolaryngol. 2011;268:1755–1763. doi: 10.1007/s00405-011-1660-5. [DOI] [PubMed] [Google Scholar]
- 31.Masterson L., Leong P. Pott’s puffy tumour: a forgotten complication of frontal sinus disease. Oral Maxillofac Surg. 2009;13:115–117. doi: 10.1007/s10006-009-0155-7. [DOI] [PubMed] [Google Scholar]
- 32.Shin J.W., Ik G.C., Jung S., Kwon H., Shon W.I., Moon S.H. Pott’s puffy tumor appearing with a frontocutaneous fistula. J Craniofac Surg. 2012;23:e158–e160. doi: 10.1097/SCS.0b013e31824cdcc0. [DOI] [PubMed] [Google Scholar]
- 33.Tacon L.J., Parkinson J.F., Hudson B.J., Brewer J.M., Little N.S., Clifton-Bligh R.J. Headache of a diagnosis: frontotemporal pain and inflammation associated with osteolysis. Med J Aust. 2008;189:591–592. doi: 10.5694/j.1326-5377.2008.tb02190.x. [DOI] [PubMed] [Google Scholar]
- 34.Elyassi A.R., Prenzel R., Closmann J.J. Pott’s puffy tumor after maxillary tooth extraction. J Oral Maxillofac Surg. 2012;70:e190–e192. doi: 10.1016/j.joms.2011.11.018. [DOI] [PubMed] [Google Scholar]
- 35.Upadhyay S. Recurrent Pott’s puffy tumor, a rare clinical entity. Neurol India. 2010;58:815–817. doi: 10.4103/0028-3886.72206. [DOI] [PubMed] [Google Scholar]
- 36.Rehman A., Noor M., Moallam F. Pott’s puffy tumor: a rare complication of sinusitis. Ann Saudi Med. 2013;33:79–80. doi: 10.5144/0256-4947.2012.26.5.1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rajwani K.M., Desai K., Lew-Gor S. Forehead swelling and frontal headache: pott’s puffy tumour. BMJ Case Rep. 2014 doi: 10.1136/bcr-2013-202737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Williams S., Wilkie M. Pott’s puffy tumour: an unforgettable complication of frontal sinusitis. BMJ Case Rep. 2014 doi: 10.1136/bcr-2014-204061. [DOI] [PMC free article] [PubMed] [Google Scholar]