The high morbidity and mortality rates of COVID‐19 have led many countries to impose a lockdown as an extreme measure to prevent contagion. Accordingly, concerns were raised about the worsening of symptoms in patients with Parkinson's disease (PD) 1 , 2 , 3 as well as for their caregivers' mental health. We hypothesized that different PD features may impact on patients' and caregivers' stress under lockdown. To this aim, we prospectively carried out a series of structured telephone interviews to each pair (PD/caregivers) conducted by the treating neurologist during the last 10 days of lockdown in Italy. The study was approved by the ethical committee of Brotzu General Hospital (PG/2020/11022). Patients and caregivers provided written consent by email.
Inclusion criteria were diagnosis of PD according to Movement Disorder Society clinical diagnostic criteria 4 and having a family member as caregiver. The change in stress level of patients with PD and caregivers was compared to the time prior to home confinement and assessed with a self‐reported judgment (verbal rating scale). Answers were transposed on a scale from 0 (severely worsened) to 6 (much improved), where 3 stood for unchanged. The verbal rating scale for each item was categorized in worsened (score 0–2) and unchanged/improved (score 3–6). The following clinical variables were assessed in PD: Unified Parkinson's Disease Rating Scale Part II, Non‐Motor Symptoms Scale (NMSS), Questionnaire for Impulsive‐Compulsive Disorders in Parkinson's Disease–Rating Scale, and Parkinson's Disease Questionnaire‐8. Hospital Anxiety and Depression Scale (HADS) scores were retrieved in PD and caregivers, who also underwent the Zarit Burden Interview. Patients with PD were also categorized in 2 groups based on whether they continued to practice at least 45 minutes per day of physical activity during the home confinement. Full methods, including statistical analysis, are in the Supplementary Material.
We enrolled 32 patient with PD and 32 caregivers (Supplementary Table S1). Level of stress during home confinement was rated as worsened in 43.8% of patients with PD and 53.1% of caregivers. Patients with PD experiencing increased stress levels had worse HADS‐Anxiety (P = 0.006) and NMSS (P = 0.012) scores. Specifically, thad significant worse mood/cognition scores of NMSS (P < 0.05). Worsening of stress occurred in caregivers of PD patients with higher NMSS scores (P = 0.018). This result was determined by significant higher scores of thecardiovascular, mood/cognition, urinary, and miscellaneous domains of the NMSS (P < 0.05) (Fig. 1). On multivariate binary logistic regression, worsening stress in caregivers was associated with patients' HADS‐Anxiety scores (P = 0.032) and NMSS scores (P = 0.018). Similarly, on multivariate linear regression analysis, a higher Zarit Burden Interview score in caregivers was associated with a higher NMSS score in PD (P = 0.029) (Supplementary Table S2). Patients with PD practicing daily physical activity had lower scores on HADS‐Anxiety compared with those who were inactive (6.0 ± 3 vs. 8.7 ± 3; P = 0.044). The 2 groups were similar in other clinical and demographic features. Multivariate linear regression showed a significant association between HADS‐Anxiety in patients with PD and lack of physical activity during home confinement, even when controlling for age, disease duration, total levodopa equivalent daily dose, Unified Parkinson's Disease Rating Scale Part II, NMSS, and Questionnaire for Impulsive‐Compulsive Disorders in Parkinson's Disease–Rating Scale (Supplementary Tables S3 and S4).
FIG. 1.
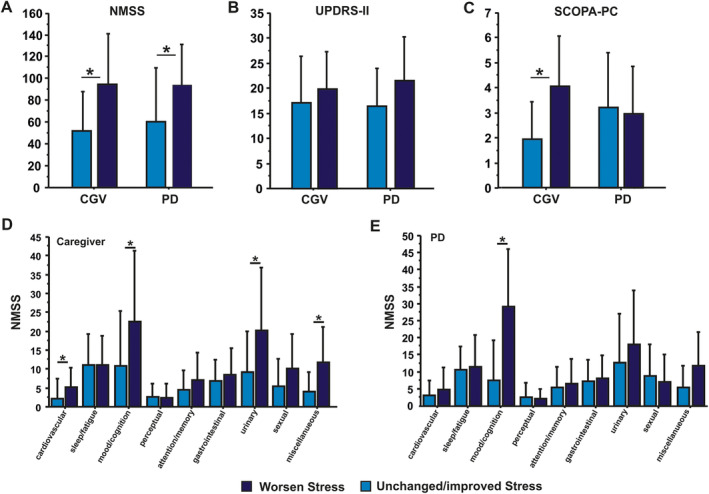
(A‐C) Patients with PD experiencing increased stress level during lockdown had worse NMSS (*P = 0.012) and Hospital Anxiety and Depression Scale–Anxiety (*P = 0.006) scores. The patients' feature associated with higher levels of stress in caregivers was worse NMSS score (*P = 0.018). The UPDRS‐II score was not associated with higher stress levels in patients with PD or caregivers. (D) Worsening of stress occurred in caregivers of PD patients scoring higher at cardiovascular, mood/cognition, urinary, and miscellaneous domains of the NMSS (*P < 0.05). (E) PD patients with increased stress had significant worse mood/cognition score of NMSS (*P < 0.05). PD, Parkinson's disease; NMSS, Non‐Motor Symptoms Scale; SCOPA‐PC, Scales for Outcomes in Parkinson's Disease–Psychiatric Complications; UPDRS‐II, Unified Parkinson's Disease Rating Scale Part II.
The binary and multiple regression models adequately fit the data. There was no evidence of collinearity between NMSS and Unified Parkinson's Disease Rating Scale Part II (Supplementary Material).
Nonmotor symptoms, particularly neuropsychiatric 5 and sleep disturbances, 6 are known predictors of caregiver burden. The COVID‐19 related confinement period resulted in an additional load of pressure on the caregivers especially caused by patients' nonmotor symptoms belonging to the neuropsychiatric and autonomic domain. Only anxiety was a significant determinant of worsening stress in patients with PD, as recently reported. 2 Limitations of our study are the small sample size and the use of telephone interviews.
Despite the small sample size and the use of a nonvalidated outcome measure such as the verbal rating scale, we believe these findings should be taken into account in the postpandemic time. The maintenance of a minimum level of physical activity should also represent an essential nonpharmacological measure for the management of PD anxiety. Moreover, our study highlights that, under strict home confinement, different PD symptoms have a distinct but significant impact not only on patients' but also on caregivers' stress. Postpandemic health care systems should take care of such an unpaid compassionate group that bears a huge and growing burden on society.
Author Roles
(1) Research project: A. Conception, B. Organization, C. Execution; (2) Statistical Analysis: A. Design, B. Execution, C. Review and Critique; (3) Manuscript: A. Writing of the first draft, B. Review and Critique;
V.O.: 1A, 1B, 1 C, 3A, 3B
G.S.: 1A, 1B, 1 C, 3A, 3B
G.F.: 1C, 2A, 2B, 2C, 3B
D.M.: 1C, 3B
L.R.: 2C, 3B
M.M.: 2C, 3B
F.M.: 1A,1B, 2A,2C, 3B
G.C.: 1A, 1B, 2A, 2C, 3B
Disclosures
Ethical Compliance Statement: Institutional ethics approval was obtained from AOU Brotzu, Cagliari Ethical committee (PG/2020/11022). The study was conducted in accordance with the Declaration of Helsinki. Each participant provided written informed consent which was scanned and sent by email. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.
Funding Sources and Conflict of Interests: No specific funding was received for this work.
Full Financial Disclosures for the Previous 12 Months: Giuseppe Fenu reports speaking honoraria, consultancies fees, travel grants, and advisory board fees from Biogen Idec, Sanofi Genzyme, Merck Serono, and Novartis and is a member of the editorial board of BMC Neurology. Lucia Ricciardi reports research support from UK's Medical Research Council and Clinical Academic Research Partnerships. Francesca Morgante reports speaking honoraria from Abbvie, Medtronic, Zambon, Bial, and Merz; travel grants from the International Parkinson's Disease and Movement Disorder Society; advisory board fees from Merz; consultancies fees from Merz and Bial; research support from Boston Scientific, Merz, and Global Kynetic; royalties for the book Disorders of Movement from Springer; and is a member of the editorial boards of Movement Disorders, Movement Disorders Clinical Practice, and European Journal of Neurology. Giovanni Cossu reports speaking honoraria from UCB Pharma, Bial, AbbVie, Zambon, and Boston and research support from “Fondazione di Sardegna.” Valentina Oppo, Giulia Serra, Daniela Murgia, and Maurizio Melis report no disclosures.
References
- 1. Papa SM, Brundin P, Fung VSC, et al. Impact of the COVID‐19 pandemic on Parkinson's disease and movement disorders. Mov Disord Clin Pract 2020;7:357–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Salari M, Zali A, Ashrafi F, et al. Incidence of anxiety in Parkinson's disease during coronavirus disease (COVID‐19) pandemic. Mov Disord 2020;35:1095–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shalash A, Roushdy T, Essam M, et al. Mental health, physical activity and quality of life in Parkinson's disease during COVID‐19 pandemic. Mov Disord 2020;35:1097–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Postuma RB, Berg D, Stern M, et al. MDS clinical diagnostic criteria for Parkinson's disease. Mov Disord 2015;30:1591–1601. [DOI] [PubMed] [Google Scholar]
- 5. Martinez‐Martin P, Rodriguez‐Blazquez C, et al. Neuropsychiatric symptoms and caregiver's burden in Parkinson's disease. Parkinsonism Relat Disord 2015;21:629–634. [DOI] [PubMed] [Google Scholar]
- 6. Happe S, Berger K, FAQT Study Investigators . The association between caregiver burden and sleep disturbances in partners of patients with Parkinson's disease. Age Ageing 2002;31:349–354. [DOI] [PubMed] [Google Scholar]
Supporting information
Appendix S1. Supplemental Material
Valentina Oppo and Giulia Serra equally contributed to this article.
Francesca Morgante and Giovanni Cossu share senior authorship.
Relevant disclosures and conflicts of interest are listed at the end of this article.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supplemental Material


