Abstract
Background:
High failure rates have been documented after anterior cruciate ligament reconstruction (ACLR) in pediatric patients, and revision surgery is indicated due to high activity levels of children and adolescents.
Purpose:
To define trends in revision ACLR in patients who underwent initial ACLR at younger than 18 years.
Study Design:
Case series; Level of evidence, 4.
Methods:
An electronic medical record was used to retrospectively identify revision ACLR procedures performed by 2 surgeons between the years 2010 and 2016 in patients younger than 18 years at initial reconstruction. Descriptive information, intraoperative findings, surgical techniques, and rehabilitation data were recorded from initial and revision surgeries. Descriptive statistics were used.
Results:
A total of 32 patients (17 girls, 15 boys) met the inclusion criteria, with a mean age of 15.8 years at initial reconstruction. For initial reconstructions, 15 patients underwent transphyseal procedures, 3 patients underwent adult-type procedures using an anatomic reconstruction technique that did not take into account the physis, and 2 patients underwent partial intraepiphyseal procedures. Graft types included hamstring autograft (n = 17), allograft (n = 5), hybrid (n = 4), and bone–patellar tendon–bone autograft (BTB; n = 3). Average primary reconstruction graft diameter was 8.0 mm (girls, 7.72 mm; boys, 8.36 mm; P = .045). After initial reconstruction, 10 patients had postoperative protocol noncompliance, and 8 patients reported delayed recovery. Mean time to retear was 565 days (range, 25-1539 days). At revision, BTB autograft was used in 50% (n = 16), followed by hamstring autograph (31.3%; n = 10) and allograft (12.5%; n = 4); mean graft diameter was 9.05 mm. Chondral surgery was more common during revision (25% for revision vs 0% for index; P = .031). There were 4 patients who required staged reconstruction with bone grafting. At mean final follow-up of 29.5 months (SD, 22.2 months), there were 3 graft failures (9.4%) and 5 contralateral ACL ruptures (15.6%).
Conclusion:
Most patients with ACL graft failure were adequately treated with a single revision. Conversion from a soft tissue graft to a BTB autograft was the most common procedure. Infrequently, patients required staged reconstructions. Providers should have a high index of suspicion for associated intra-articular injuries resulting from graft failure in adolescent patients.
Keywords: knee ligament, ACL, allografts, pediatric sports medicine
Anterior cruciate ligament (ACL) injuries have become increasingly common in active youth, despite the historical notion that these were rare injuries in skeletally immature patients.4 A study of hospital admissions for ACL injuries in Australia reported a 148% increase in annual ACL injuries in 5- to 14-year-olds between 2005 and 2015.48 An analysis of a private-payer database between 2007 and 2011 similarly demonstrated an increase in ACL injury and reconstruction among pediatric patients.54 Increasing participation in pediatric sports, increased sport specialization, and participation in year-round athletics all likely contribute to the increase in ACL injuries in pediatric and adolescent patients.
Because nonoperative treatment of these injuries results in predictably poor outcomes,2,16 most patients are offered surgical reconstruction. Concern about potential growth disturbance has shaped the surgical techniques developed for the skeletally immature athlete. Furthermore, graft choice has been an area of active study in the young, high-risk population, with autograft favored based on contemporary literature.17,25,26 However, these patients remain at high risk for graft failure. Pediatric and adolescent athletes have excellent return-to-play rates after ACL reconstruction,27,33 and this leads to repeat exposure and increased rerupture rates relative to those in older athletes.13 Injury of the ipsilateral or contralateral ACL after reconstruction has been reported in up to one-third of young athletes, with the highest rates of ACL rerupture within the first 5 years after reconstruction.38,52,53
Although techniques and outcomes for primary reconstruction of the ACL in pediatric patients have been well-described, there is a scarcity of literature regarding revision ACL reconstruction in adolescent patients. The purpose of this study was to identify trends in revision ACL reconstruction in patients with ACL reconstruction performed during adolescence at a single institution.
Methods
Descriptive Data
This was a retrospective electronic chart review of all revision ACL reconstructions performed by 2 senior surgeons (1 sports medicine surgeon [C.A.] and 1 pediatric fellowship-trained surgeon [N.K.P.]) at a single institution between the years 2010 and 2016. Institutional review board approval was obtained (approval No. 16-20219). Patients were excluded if they underwent initial ACL reconstruction after age 18. Descriptive data were collected for each patient, including age, sex, primary sport, surgical history, and injury mechanism. Operative notes were queried from both initial and revision surgeries for surgical technique, graft choice and size, presence of meniscal and chondral injuries, and concomitant pathologies addressed.
Surgical Techniques
Surgical techniques used for the index procedure included partial intraepiphyseal, transphyseal, and adult-type reconstructions. Patients who were skeletally immature and not within 2 years of physeal closure were indicated for partial intraepiphyseal reconstruction to minimize the chance of growth disturbance. Adolescents within 2 years to 6 months of physeal closure were indicated for transphyseal reconstruction. Patients who were skeletally mature or within 6 months of physeal closure were indicated for adult-type reconstruction. Partial intraepiphyseal reconstruction involved transphyseal tibial drilling and intraepiphyseal femoral drilling.8 The transphyseal reconstruction technique involved transphyseal tibial drilling, but the tibial interference screw was placed in the metaphysis, not crossing the physis.45 On the femoral side, the tunnel was positioned more vertically so as to cross the physis with as little surface area as possible. Adult-type reconstruction was an anatomic reconstruction technique that does not take into account the physis, entailing a tibial tunnel screw or bone block that may be positioned in the physis or physeal scar and resulting in a more horizontally oriented femoral tunnel that may cross the physis or physeal scar with a large surface area.
All revision procedures were performed via an adult-type reconstruction using the above method. Preoperatively, tunnels were evaluated for tunnel widening and appropriate position. At our institution, the decision to proceed with bone grafting is based on bone tunnel measurements on radiographs and magnetic resonance imaging scans. Tunnels that were in the appropriate position were redrilled using a guidewire through the tunnel to prepare for the new graft. If a tunnel was not in the appropriate position, care was taken to avoid overlapping with that tunnel.
Skeletally immature patients were eligible for soft tissue grafts only, with avoidance of fixation across the physis as described above. Patients who were skeletally mature were given the choice of hamstring autograft, bone–patellar tendon–bone (BTB) autograft, or allograft for primary graft. Soft tissue grafts used suspensory fixation on the femoral side and interference screw fixation or were tied over a post on the tibial side. BTB autografts were performed using a 2-incision technique with outside-in femoral interference screw placement and a standard tibial interference screw.
Postreconstruction Follow-up
The rehabilitation protocol used by both surgeons consisted of patients using a full-time hinge knee brace for 6 weeks: Full weightbearing and full range of motion were allowed if no meniscal repair was performed, and nonweightbearing with 0° to 90° of motion was allowed if meniscal repair was performed. From 6 weeks to 4 months, athletes were weaned from brace use, and strengthening exercises were prescribed. Straight-line running was allowed at 4 months. At 6 months, agility work was added, and return to sports was allowed at 1 year for patients with revisions (as opposed to 9 months for patients with primary ACL reconstruction). Postoperative rehabilitation data after the index procedure were collected. Noncompliance was defined as deviation from standardized postoperative instructions, prescribed physical therapy, or return-to-play protocol. This included issues with physical therapy, noncompliance with postoperative precautions, and delayed recovery (eg, stiffness or persistent instability). Time to ACL graft retear was documented, as well as time to final surgery from index procedure. The electronic chart was queried for date of final follow-up with a medical provider, and revision graft failure and contralateral ACL rupture during the follow-up period were documented.
Statistical Analysis
Statistical analysis was performed using R programming language. Group means were compared using the Student t test. Categorical data were compared using chi-square test.
Results
Descriptive Data
A total of 35 patients met the inclusion criteria; 3 patients were excluded because they had not completed a staged revision. The final analysis included 32 patients, with 17 female and 15 male patients (Table 1). In 22 patients for whom skeletal maturity was documented, 11 patients were skeletally immature at index reconstruction. Mean age at initial surgery was 15.8 years (range, 12-17 years). Soccer (n = 12), football (n = 8), and basketball (n = 5) were the most common primary sports played. Mechanisms of injury were available for 15 patients; most common were twisting injury and collision or contact.
Table 1.
Patient Descriptive and Surgical Dataa
| Index Reconstruction | Revision Reconstruction | P | |
|---|---|---|---|
| Age, y, mean (range) | 15.8 (12-17) | 18.0 (14-23) | |
| Skeletally mature | 11/22 (50.0) | 32/32 (100) | |
| Graft type by surgery | (n = 30) | (n = 32) | |
| Hamstring autograft | 17 (56.7) | 10 (31.3) | |
| Bone–patellar tendon–bone autograft | 3 (10) | 16 (50.0) | |
| Allograft | 5 (16.7) | 4 (12.5) | |
| Hybrid hamstring autograft-allograft | 4 (13.3) | 2 (6.3) | |
| Quadriceps tendon | 1 (3.3) | 0 (0) | |
| Surgical technique | (n = 20) | (n = 32) | |
| Partial intraepiphyseal | 2 (10.0) | 0 | |
| Transphyseal | 15 (75.0) | 0 | |
| Adult type | 3 (15.0) | 32 (100) | |
| Graft size, mm | (n = 16) | (n = 32) | |
| Average size | 8.00 | 9.05 | <.01b |
| Female patients | 7.72 | 9.00 | |
| Male patients | 8.36 | 9.10 | |
| Meniscal surgery | (n = 25) | (n = 32) | |
| 14 (56.0) | 17 (53.1) | .855 | |
| Meniscal repair | (n = 25) | (n = 32) | |
| 3 (12.0) | 8 (25.0) | .37 | |
| Chondral pathology | NR | (n = 32) | |
| NR | 19 (59.4) | NA | |
| Chondral surgery | (n = 22) | (n = 32) | |
| 0 | 8 (25.0) | .031b |
aValues are expressed as n (%) unless otherwise noted. NA, not applicable; NR, not reported; Adult type reconstruction = standard ACL reconstruction performed without any techniques to prevent physeal damage.
bP < .05.
Index Surgery
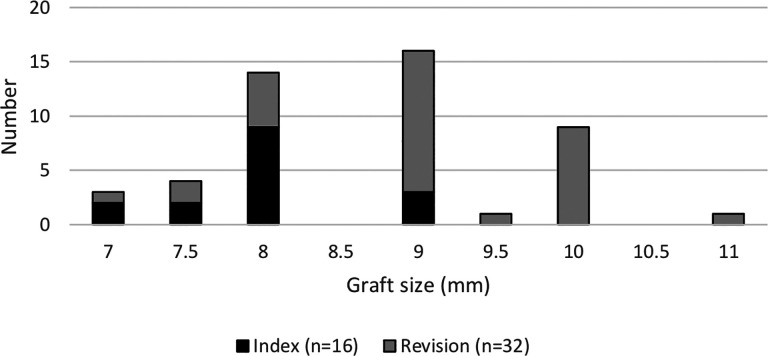
Table 1 summarizes surgical techniques, graft details, and adjuvant procedures by index and revision surgery. The majority of patients for whom index procedure information was available underwent transphyseal reconstructions (n = 15), with a minority undergoing adult-type (n = 3) or partial intraepiphyseal (n = 2) procedures. Hamstring autograft (HA) was used as the initial graft of choice in the majority of patients (n = 17), followed by allograft (n = 5), hybrid HA-allograft (n = 4), and BTB autograft (n = 3). All 5 patients who received allograft at index reconstruction underwent surgery at an outside facility, and the indication for using allograft was not documented. Average initial graft diameter was 8.0 mm (Figure 1). Female patients had smaller grafts on average than did male patients (7.72 vs 8.36 mm, respectively; P = .045) (Figure 2A). Of 25 patients for whom data were available, 14 patients (56%) had meniscal surgery at the time of their index operation. This involved meniscal repair in 3 patients (all medial), lateral meniscal debridement or partial meniscectomy in 11 patients, and medial meniscal debridement or partial meniscectomy in 4 patients. Of 22 patients for whom operative reports were available, none had documented chondral procedures.
Figure 1.
Graft size by index and revision reconstruction.
Figure 2.
(A) Index and (B) revision graft size by sex.
A total of 10 patients (10/30; 33.3%) had documented noncompliance postoperatively (Table 2), including premature return to weightbearing, premature return to sports, or lack of physical therapy follow-up. Noncompliance was more common in male patients (42.9%) than female patients (25%); this difference was not statistically significant (P = .512). Further, 8 patients reported delayed recovery, including prolonged stiffness or instability, 5 of whom also had recorded noncompliance.
Table 2.
Reasons for Noncompliance After Index Reconstruction (n = 10)a
| Reason | n |
|---|---|
| Lack of physical therapy or delay in initiating physical therapy | 7 |
| Noncompliance with postoperative protocol | 6 |
| Lost to follow-up during recovery period | 1 |
| Drug use | 1 |
aSome patients had >1 reason for noncompliance.
Revision Surgery
Mean time to graft rupture was 565 days (range, 25-1539 days); however, 11 of 22 patients (50%) for whom data were available had graft failure within 1 year of index procedure. There was no significant difference between sexes in time to reinjury. Among patients for whom graft retear dates were available, average time to retear was 677 days for patients who adhered to postoperative protocols and therapy (n = 14) and 369 days for patients with documented noncompliance (n = 8); this difference was not significant (P = .221). Patients averaged 18.0 years of age at time of revision (range, 14-23 years). Of the 25 patients for whom a mechanism of retear was reported, sports participation was listed as the mechanism for 18 patients (7 patients within 1 year; 11 patients after >1 year). Revision was performed in 1 patient because of infection. All patients were treated using adult-type reconstructions. The most commonly used graft for revision was BTB autograft (n = 16), followed by HA (n = 10) (Table 1). Hybrid HA-allograft was used in 2 patients, and allograft alone was used in 4 patients. Mean graft diameter was 9.05 mm, which was significantly larger than the graft diameter at the index procedure (P < .01) (Figures 1 and 2B), with no sex difference (9.0 mm in females and 9.10 mm in males).
Three-fourths of patients required a procedure to address intra-articular pathology at the time of revision. Half of the patients underwent meniscal surgery (Table 1). The most common meniscal procedures performed were medial meniscal repair (n = 8) and meniscal debridement (n = 8); 1 patient underwent meniscal transplant. Although a higher percentage of patients required meniscal repair at revision versus the index procedure (n = 8/32 [25%] vs n = 3/25 [12%], respectively), this was not significant (P = .37). Chondral pathology was identified at the time of revision in 59.4% of patients, and damage was most common on the medial femoral condyle (n = 10). Of patients who had meniscal surgery at the index procedure, 10/14 (71%) had chondral injury at revision, whereas only 4/11 (36%) of patients who did not have meniscal surgery had chondral injury at the time of revision; this was not statistically significant (P = .178). Chondral surgery was performed in 8 patients at revision, which was significantly more patients than at the index procedure (n = 8/32 vs n = 0/22, respectively; P = .031), including chondroplasty in 7 patients and microfracture in 1 patient.
Staged Reconstructions and Subsequent Surgery
Staged reconstruction with bone tunnel grafting was performed in 4 patients (12.5%) (3 female, 1 male). Initial graft data were available for 3 patients; 1 patient had quadriceps tendon allograft, 1 patient underwent HA-allograft hybrid, and 1 patient had an allograft. Average postrevision length of follow-up with a medical provider was 29.5 months (SD, 22.2 months).
Three patients had retears (9.4%) at final follow-up. One patient initially underwent revision with BTB allograft and required staging with bone grafting followed by reconstruction with HA-allograft hybrid. The second patient underwent initial revision with HA and, after failure, underwent revision with BTB autograft. The third patient initially underwent revision with HA, was noncompliant with postoperative protocols, and required staged revision with bone grafting followed by ACL reconstruction with contralateral HA. A total of 5 patients (15.6%) experienced contralateral ACL rupture in the follow-up period. No other secondary procedures were recorded during the follow-up period.
Discussion
This retrospective study is one of the first to present descriptive and surgical data for patients undergoing revision for ACL reconstruction performed during adolescence. Hamstring autograft was the most commonly used initial graft, whereas BTB autograft was the most commonly used revision graft. Transphyseal technique was used most frequently at index procedure, whereas adult-type reconstruction was used in all revisions. Noncompliance was particularly high in patients whose reconstruction had failed, although this did not reach statistical significance. Finally, meniscal repairs and chondral surgery were more likely to be performed at the time of revision than at the index procedure, which may indicate a greater degree of intra-articular damage after reinjury compared with the index procedure. A total of 4 patients required staged reconstruction for tunnel grafting, and 8 patients experienced either ipsilateral or contralateral ACL rupture at nearly 2.5-year average follow-up.
Historically, patients with open physes who sustained an ACL rupture were counseled to delay surgical intervention until after reaching skeletal maturity. However, delaying surgical intervention leads to increased risk of recurrent instability and intra-articular damage.2,15,21,34,44 Techniques for revision ACL reconstruction in the pediatric population have evolved in the past 2 decades, with the goal of minimizing growth disturbance in skeletally immature patients while providing appropriate stability to the knee joint. An all-epiphyseal, extra-articular approach using the ilitotibial band as a local graft without drilling tunnels has been popularized by Kocher et al30 (the Micheli approach) and is recommended for patients with bone age <8 years or with >3 years of bone growth remaining. In a single-surgeon study of 22 male patients undergoing Micheli ACL reconstruction, Willimon et al55 reported a 27% rate of reoperation, 14% revision ACL operation, and no angular or leg-length deformities at 3 years of follow-up. However, the technique is nonanatomic and may lead to biomechanical overconstraint of the knee,29 leading some surgeons to opt for different techniques. The all-epiphyseal ACL reconstruction involves femoral and tibial intraepiphyseal drilling, with suspensory or interference screw soft tissue graft fixation; proponents recommend use in patients with bone age 8 to 12 years. In a retrospective study of 23 adolescent patients (average age, 12 years) undergoing all-epiphyseal reconstruction with HA, Cordasco et al11 demonstrated that 6 athletes had leg-length discrepancy between 5 and 18 mm (none clinically significant) and 2 had reoperations (1 for revision ACL reconstruction and 1 for failed meniscal repair). Pennock et al,40 reporting minimum 2-year outcomes for 30 patients who underwent all-epiphyseal reconstruction with a mean bone age of 11.8 years, described high patient satisfaction rates, 94% return to sports, a 15% failure rate, and a single patient with a leg-length discrepancy requiring no additional intervention. For patients nearing skeletal maturity who are at lower risk for growth disturbance but who still have open physes, the transphyseal technique has been advocated. This technique involves physeal-respecting drilling with more vertical tunnels (minimizing surface area), use of soft tissue grafts, and avoidance of placement of fixation or bone plugs across the physis. A major advantage of this procedure is the anatomic placement of the graft. A number of small studies have reported favorable rates of patient satisfaction and return to sports with negligible incidence of clinically significant growth disturbance.7,18,22,31 In the current study, the majority of the patients for whom data were available had undergone a transphyseal technique at the time of their index operation. We noted that 2 patients, a 12-year-old boy and a 12-year-old girl, underwent a hybrid partial intraepiphyseal technique with a femoral intraepiphyseal tunnel and a tibial transphyseal tunnel. This technique aims to minimize damage to the femoral physis with more potential growth remaining while allowing for anatomic tibial tunnel placement.
Graft choice is also an important consideration for pediatric and adolescent patients, given the anticipated high rate of return to sports.27 Autografts have consistently shown lower rerupture rates compared with allografts in pediatric patients.17,25,26 In adults, the Multicenter ACL Revision Study has demonstrated that autograft had significantly lower failure rates than allograft.37 Within possible autograft choices, BTB autograft has lower reported failure rates than does HA.19,23,41,43 At index surgery, the majority of our patients with autografts received HA or HA-allograft hybrid. The benefits of using a soft tissue graft in skeletally immature patients lie in avoiding harvesting BTB from an open tibial tubercle apophysis and avoiding the bone plug or interference screw crossing and potentially arresting the physis.50 The tradeoff may be a higher risk of graft rupture with HA or HA-allograft hybrid; for this reason, in adolescent patients nearing skeletal maturity returning to high-risk activities, we offer BTB autograft. Graft size is also a modifiable parameter to reduce risk of graft failure. In a systematic review examining graft size for quadrupled-strand HA, patients with grafts <8 mm had a 6.8 times greater risk of graft rupture compared with those who had grafts ≥8 mm.10 In some cases, the harvested autograft size may be insufficient to reach a minimum acceptable diameter, in which case allograft may be used for augmentation. In the current study, 13.3% and 6.3% of patients received hybrid graft at index and revision procedures, respectively. Some studies have shown increased failure rate with use of hybrid grafts,6,40,57 whereas others have shown no difference.1,24,35 At this time, in our practice we avoid hybrid grafts unless necessary to meet minimum graft size. Another technique to increase HA diameter and avoid hybridization is making a 5-strand graft, which is feasible in the majority of adult patients.20,32
Despite advances in techniques for ACL reconstruction, pediatric patients remain at high risk for graft rerupture relative to adult patients,25,36 likely related to return to high-risk activities.27 In a study of 85 pediatric patients with minimum of 2-year follow-up after ACL reconstruction, Dekker et al13 found that 91% had returned to sports, 19% had sustained an ipsilateral graft rupture, and 13% had sustained contralateral ACL rupture. The only significant predictor of ACL rupture was time to return to sports. Ho et al23 reported a failure rate of 9.6% with mean follow-up of just over 1 year, and predictors of failure included use of soft tissue graft rather than BTB, open physes (which were correlated with soft tissue graft reconstruction), and use of transphyseal rather than adult-type reconstruction. DeFrancesco et al12 described causes for unplanned return to the operating room after primary ACL reconstruction in 419 pediatric patients, which at 3 years occurred in 16.3% of patients: 10.3% for ipsilateral ACL graft failure and 7.1% for contralateral ACL rupture. Nearly half of retears occurred before clearance to activity. In a meta-analysis of complications after ACL reconstruction in pediatric patients, Wong et al56 analyzed surgical outcomes in 1321 patients from 45 studies with an average follow-up of 49.6 months. Rerupture rate was 8.7%, and 94.6% of athletes who had graft failure underwent revision. In that study, ipsilateral or contralateral ACL rupture occurred in 25% of patients. Given the anatomic challenges of the pediatric population, coupled with high rates of graft failure and contralateral ACL rupture, more research is needed regarding the optimal techniques and rehabilitation in the setting of ACL revision in the pediatric population.
Two studies have described demographics, surgical techniques, and patient outcomes after revision ACL reconstruction in children and adolescents. Christino et al9 followed 88 pediatric patients for a minimum of 1 year after revision ACL reconstruction over a 16-year period at a single institution. Average patient age was 15.1 years at index procedure and 16.6 years at revision. Index graft failure had occurred within 1 year in 52.3% of patients; we similarly found a 1-year index graft failure rate of 50%. The majority (85%) of patients underwent transtibial femoral drilling during revision, and 61% received allograft at revision. There are a number of important distinctions between the study by Christino et al and our study. First, they selected patients who were younger than 18 years at revision, whereas we selected athletes younger than 18 years at the time of the index procedure. This may have led to the use of transphyseal techniques at the time of revision in the Christino study, whereas all of our patients received adult-type reconstructions at time of revision. Furthermore, 12.5% of our patients received allograft at the time of revision versus the majority of patients in the Christino study. This may be related to avoidance of BTB autograft because of younger average patient age (29% of patients remained skeletally immature at revision), or it may be because of the earlier time period of Christino’s study, during which allograft was a more popular revision graft choice (1997-2013 vs 2010-2016 in our study). Christino et al reported ipsilateral graft reinjury rate was 20% and contralateral knee ACL rupture rate was also 20% with average 5-year follow-up. In another retrospective study of revision ACL reconstruction in adolescent patients (index procedure at age <18 years, revision at age <20 years), Ouillette et al39 demonstrated decreased patient-reported outcomes, higher rates of graft failure, and increased intra-articular injury rate in patients undergoing revision compared with those undergoing primary reconstruction. Revision graft failure occurred in 27% of patients in the revision cohort at an average follow-up of 4.4 years. Taken with the present study, these findings underscore the need for further optimization of surgical techniques and return-to-play protocols for this high-risk population.
In addition to reestablishing joint stability, surgeons should address concomitant intra-articular pathology in the pediatric patient. High rates of intra-articular pathology have been associated with delay in ACL reconstruction at the time of initial injury2,15,28; however, ACL revision has not been studied as a risk factor for intra-articular pathology. At the time of revision in the current study, >75% of patients required an additional intra-articular procedure to address meniscal or chondral injuries. Similarly, Christino et al9 reported that 74.4% of their patients had additional intra-articular procedures performed at revision. In this study, chondral procedures were significantly more likely to be performed during revision9. It is not clear whether these cartilage injuries represent the sequelae of trauma incurred at initial ACL rupture or arise from repetitive microtrauma related to recurrent instability after ACL reconstruction. In a comparative study of the Multicenter Orthopaedic Outcomes Network and Multicenter ACL Revision Study (MARS) cohorts, the authors found an association between previous meniscectomy at index procedure and chondral damage at time of ACL revision.5 When we examined this association in our cohort, we noted a trend toward increased chondral damage in the setting of a previous meniscal surgery, but the trend was not significant. In this study, meniscal repair was also more common at the time of revision than at index procedure; however, the data were underpowered to detect a significant difference. These findings underscore the need for larger longitudinal studies of the ACL reconstruction in the pediatric population to identify risk factors and prevention strategies for intra-articular damage.
Bone tunnel widening after ACL reconstruction is a well-described entity that affects the surgeon’s approach to revision ACL reconstruction.3,46,47 Use of a 2-stage ACL revision reconstruction has been advocated by some authors because of concern for tunnel widening or tunnel overlap.49 However, the MARS group has reported higher rates of reoperation after 2-stage revision (odds ratio = 1.93) compared with single-stage revision, and higher rates of another ACL graft rupture (5% vs 2%), although neither finding was statistically significant.14 In the current study, 4 of 32 patients met the criteria (based on radiography and magnetic resonance imaging) for bone grafting and underwent a 2-stage technique; 1 of these patients had revision graft failure at <2 years after completion of her 2-stage revision. No literature is available addressing bone tunnel grafting in the pediatric population; this may be explained by the adjustment of tunnel placement upon revision in the pediatric population, which may be less common in the adult population.
Approximately one-third of the patients in this study had documented noncompliance. Compliance rates have not been reported in the pediatric population after ACL reconstruction. In this study, we included lack of attendance to physical therapy in the category of noncompliance, as structured rehabilitation has been shown to improve postoperative outcomes42,51 and is part of our institutional protocol. The average time to repeat tear trended toward less for patients who were noncompliant, although this was not significant. Thorough counseling of the patient and family is imperative to explain risks of early return to sports. Imminently, wearable and application-based technologies may allow surgeons, physical therapists, and athletic trainers to monitor and modify postoperative care.
This is only the third study of revision of ACL reconstruction performed during adolescence, and it has a number of limitations. The findings are from a single institution, although with 2 surgeons performing revisions there was some heterogeneity in surgical decision making, such as graft choice. Heterogeneity decreases statistical power but may more accurately capture the practices in the community. As such, the study is underpowered to detect differences between subgroups or between adjunct procedures. Only half of the study population was skeletally immature at the time of initial surgery; this limits the applicability of findings to the skeletally immature population but maintains applicability to adolescent athletes who are highly active. Furthermore, a number of the index ACL reconstructions were performed at outside institutions, thereby affecting data completeness, such as the availability of preoperative imaging (including measurement of posterior tibial slope), skeletal maturity assessment, and operative reports from the index procedure. No control group of athletes without graft rerupture was included, and therefore we cannot draw conclusions about risk factors for failure. No patient-reported outcomes were measured as part of follow-up for these patients. Finally, the average follow-up of 2.5 years can be improved upon in future studies, as many of these young athletes will continue to participate in high-risk activities for the better part of a decade after their revision ACL reconstruction.
Conclusion
Adolescent patients pose unique challenges in the setting of revision ACL reconstruction. Surgical techniques have been designed to avoid or minimize physeal damage in the skeletally immature patient, but these techniques may limit the surgeon’s ability to use certain graft types or tunnel trajectories. The majority of the patients with ACL graft failure treated at our institution were adequately treated using a single revision, with conversion from a soft tissue graft to BTB autograft being the most common procedure. Surgeons should expect and be prepared to address intra-articular pathology during revision and counsel patients as to the importance of compliance and the high risk for ipsilateral or contralateral ACL injury.
Footnotes
Final revision submitted April 13, 2020; accepted April 24, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: A.A.P. has received educational support from Sequoia Surgical. N.K.P. has received educational support from Evolution Surgical and consulting fees from OrthoPediatrics. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from UCSF Benioff Children’s Hospital Oakland (ID No. 16-20219).
References
- 1. Abouljoud MM, Everhart JS, Sigman BO, Flanigan DC, Magnussen RA. Risk of retear following anterior cruciate ligament reconstruction using a hybrid graft of autograft augmented with allograft tissue: a systematic review and meta-analysis. Arthroscopy. 2018;34(10):2927–2935. [DOI] [PubMed] [Google Scholar]
- 2. Anderson AF, Anderson CN. Correlation of meniscal and articular cartilage injuries in children and adolescents with timing of anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(2):275–281. [DOI] [PubMed] [Google Scholar]
- 3. Araki D, Kuroda R, Matsumoto T, et al. Three-dimensional analysis of bone tunnel changes after anatomic double-bundle anterior cruciate ligament reconstruction using multidetector-row computed tomography. Am J Sports Med. 2014;42(9):2234–2241. [DOI] [PubMed] [Google Scholar]
- 4. Beck NA, Lawrence JTR, Nordin JD, DeFor TA, Tompkins M. ACL tears in school-aged children and adolescents over 20 years. Pediatrics. 2017;139(3):e20161877. [DOI] [PubMed] [Google Scholar]
- 5. Borchers JR, Kaeding CC, Pedroza AD, Huston LJ, Spindler KP, Wright RW. Intra-articular findings in primary and revision anterior cruciate ligament reconstruction surgery: a comparison of the MOON and MARS study groups. Am J Sports Med. 2011;39(9):1889–1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Burrus MT, Werner BC, Crow AJ, et al. Increased failure rates after anterior cruciate ligament reconstruction with soft-tissue autograft-allograft hybrid grafts. Arthroscopy. 2015;31(12):2342–2351. [DOI] [PubMed] [Google Scholar]
- 7. Calvo R, Figueroa D, Gili F, et al. Transphyseal anterior cruciate ligament reconstruction in patients with open physes: 10-year follow-up study. Am J Sports Med. 2015;43(2):289–294. [DOI] [PubMed] [Google Scholar]
- 8. Chambers CC, Monroe EJ, Allen CR, Pandya NK. Partial transphyseal anterior cruciate ligament reconstruction: clinical, functional, and radiographic outcomes. Am J Sports Med. 2019;47(6):1353–1360. [DOI] [PubMed] [Google Scholar]
- 9. Christino MA, Tepolt FA, Sugimoto D, Micheli LJ, Kocher MS. Revision ACL reconstruction in children and adolescents. J Pediatr Orthop. 2020;40(3):126–134. [DOI] [PubMed] [Google Scholar]
- 10. Conte EJ, Hyatt AE, Gatt CJ, Jr, Dhawan A. Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy. 2014;30(7):882–890. [DOI] [PubMed] [Google Scholar]
- 11. Cordasco FA, Mayer SW, Green DW. All-inside, all-epiphyseal anterior cruciate ligament reconstruction in skeletally immature athletes: return to sport, incidence of second surgery, and 2-year clinical outcomes. Am J Sports Med. 2017;45(4):856–863. [DOI] [PubMed] [Google Scholar]
- 12. DeFrancesco CJ, Storey EP, Flynn JM, Ganley TJ. Pediatric ACL reconstruction and return to the operating room: revision is less than half of the story. J Pediatr Orthop. 2019;39(10):516–520. [DOI] [PubMed] [Google Scholar]
- 13. Dekker TJ, Godin JA, Dale KM, Garrett WE, Taylor DC, Riboh JC. Return to sport after pediatric anterior cruciate ligament reconstruction and its effect on subsequent anterior cruciate ligament injury. J Bone Joint Surg Am. 2017;99(11):897–904. [DOI] [PubMed] [Google Scholar]
- 14. Ding DY, Zhang AL, Allen CR, et al. Subsequent surgery after revision anterior cruciate ligament reconstruction: rates and risk factors from a multicenter cohort. Am J Sports Med. 2017;45(9):2068–2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dumont GD, Hogue GD, Padalecki JR, Okoro N, Wilson PL. Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears: relationship of treatment time and patient-specific factors. Am J Sports Med. 2012;40(9):2128–2133. [DOI] [PubMed] [Google Scholar]
- 16. Dunn KL, Lam KC, Valovich McLeod TC. Early operative versus delayed or nonoperative treatment of anterior cruciate ligament injuries in pediatric patients. J Athl Train. 2016;51(5):425–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Engelman GH, Carry PM, Hitt KG, Polousky JD, Vidal AF. Comparison of allograft versus autograft anterior cruciate ligament reconstruction graft survival in an active adolescent cohort. Am J Sports Med. 2014;42(10):2311–2318. [DOI] [PubMed] [Google Scholar]
- 18. Gaulrapp HM, Haus J. Intraarticular stabilization after anterior cruciate ligament tear in children and adolescents: results 6 years after surgery. Knee Surg Sports Traumatol Arthrosc. 2006;14(5):417–424. [DOI] [PubMed] [Google Scholar]
- 19. Gifstad T, Foss OA, Engebretsen L, et al. Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med. 2014;42(10):2319–2328. [DOI] [PubMed] [Google Scholar]
- 20. Goyal S, Matias N, Pandey V, Acharya K. Are pre-operative anthropometric parameters helpful in predicting length and thickness of quadrupled hamstring graft for ACL reconstruction in adults? A prospective study and literature review. Int Orthop. 2016;40(1):173–181. [DOI] [PubMed] [Google Scholar]
- 21. Guenther ZD, Swami V, Dhillon SS, Jaremko JL. Meniscal injury after adolescent anterior cruciate ligament injury: how long are patients at risk? Clin Orthop Relat Res. 2014;472(3):990–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Higuchi T, Hara K, Tsuji Y, Kubo T. Transepiphyseal reconstruction of the anterior cruciate ligament in skeletally immature athletes: an MRI evaluation for epiphyseal narrowing. J Pediatr Orthop B. 2009;18(6):330–334. [DOI] [PubMed] [Google Scholar]
- 23. Ho B, Edmonds EW, Chambers HG, Bastrom TP, Pennock AT. Risk factors for early ACL reconstruction failure in pediatric and adolescent patients: a review of 561 cases. J Pediatr Orthop. 2018;38(7):388–392. [DOI] [PubMed] [Google Scholar]
- 24. Jacobs CA, Burnham JM, Makhni E, Malempati CS, Swart E, Johnson DL. Allograft augmentation of hamstring autograft for younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(4):892–899. [DOI] [PubMed] [Google Scholar]
- 25. Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Spindler KP. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43(7):1583–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kane PW, Wascher J, Dodson CC, Hammoud S, Cohen SB, Ciccotti MG. Anterior cruciate ligament reconstruction with bone-patellar tendon-bone autograft versus allograft in skeletally mature patients aged 25 years or younger. Knee Surg Sports Traumatol Arthrosc. 2016;24(11):3627–3633. [DOI] [PubMed] [Google Scholar]
- 27. Kay J, Memon M, Marx RG, Peterson D, Simunovic N, Ayeni OR. Over 90% of children and adolescents return to sport after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1019–1036. [DOI] [PubMed] [Google Scholar]
- 28. Kay J, Memon M, Shah A, et al. Earlier anterior cruciate ligament reconstruction is associated with a decreased risk of medial meniscal and articular cartilage damage in children and adolescents: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2018;25(12):3738–3753. [DOI] [PubMed] [Google Scholar]
- 29. Kennedy A, Coughlin DG, Metzger MF, et al. Biomechanical evaluation of pediatric anterior cruciate ligament reconstruction techniques. Am J Sports Med. 2011;39(5):964–971. [DOI] [PubMed] [Google Scholar]
- 30. Kocher MS, Garg S, Micheli LJ. Physeal sparing reconstruction of the anterior cruciate ligament in skeletally immature prepubescent children and adolescents. J Bone Joint Surg Am. 2005;87(11):2371–2379. [DOI] [PubMed] [Google Scholar]
- 31. Kocher MS, Smith JT, Zoric BJ, Lee B, Micheli LJ. Transphyseal anterior cruciate ligament reconstruction in skeletally immature pubescent adolescents. J Bone Joint Surg Am. 2007;89(12):2632–2639. [DOI] [PubMed] [Google Scholar]
- 32. Krishna L, Panjwani T, Mok YR, Lin Wong FK, Singh A, Toh SJ. Use of the 5-strand hamstring autograft technique in increasing graft size in anterior cruciate ligament reconstruction. Arthroscopy. 2018;34(9):2633–2640. [DOI] [PubMed] [Google Scholar]
- 33. Lai CCH, Ardern CL, Feller JA, Webster KE. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med. 2018;52(2):128–138. [DOI] [PubMed] [Google Scholar]
- 34. Lawrence JT, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med. 2011;39(12):2582–2587. [DOI] [PubMed] [Google Scholar]
- 35. Li J, Kong F, Gao X, Shen Y, Gao S. Prospective randomized comparison of knee stability and proprioception for posterior cruciate ligament reconstruction with autograft, hybrid graft, and gamma-irradiated allograft. Arthroscopy. 2016;32(12):2548–2555. [DOI] [PubMed] [Google Scholar]
- 36. Maletis GB, Chen J, Inacio MC, Funahashi TT. Age-related risk factors for revision anterior cruciate ligament reconstruction: a cohort study of 21,304 patients from the Kaiser Permanente anterior cruciate ligament registry. Am J Sports Med. 2016;44(2):331–336. [DOI] [PubMed] [Google Scholar]
- 37. MARS Group. Effect of graft choice on the outcome of revision anterior cruciate ligament reconstruction in the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med. 2014;42(10):2301–2310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Morgan MD, Salmon LJ, Waller A, Roe JP, Pinczewski LA. Fifteen-year survival of endoscopic anterior cruciate ligament reconstruction in patients aged 18 years and younger. Am J Sports Med. 2016;44(2):384–392. [DOI] [PubMed] [Google Scholar]
- 39. Ouillette R, Edmonds E, Chambers H, Bastrom T, Pennock A. Outcomes of revision anterior cruciate ligament surgery in adolescents. Am J Sports Med. 2019;47(6):1346–1352. [DOI] [PubMed] [Google Scholar]
- 40. Pennock AT, Chambers HG, Turk RD, Parvanta KM, Dennis MM, Edmonds EW. Use of a modified all-epiphyseal technique for anterior cruciate ligament reconstruction in the skeletally immature patient. Orthop J Sports Med. 2018;6(7):2325967118781769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Persson A, Fjeldsgaard K, Gjertsen JE, et al. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004-2012. Am J Sports Med. 2014;42(2):285–291. [DOI] [PubMed] [Google Scholar]
- 42. Przybylak K, Sibinski M, Domzalski M, Kwapisz A, Momaya AM, Zielinska M. Supervised physiotherapy leads to a better return to physical activity after anterior cruciate ligament reconstruction. J Sports Med Phys Fitness. 2019;59(9):1551–1557. [DOI] [PubMed] [Google Scholar]
- 43. Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind M. Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: results from the Danish registry of knee ligament reconstruction. Am J Sports Med. 2014;42(2):278–284. [DOI] [PubMed] [Google Scholar]
- 44. Ramski DE, Kanj WW, Franklin CC, Baldwin KD, Ganley TJ. Anterior cruciate ligament tears in children and adolescents: a meta-analysis of nonoperative versus operative treatment. Am J Sports Med. 2014;42(11):2769–2776. [DOI] [PubMed] [Google Scholar]
- 45. Redler LH, Brafman RT, Trentacosta N, Ahmad CS. Anterior cruciate ligament reconstruction in skeletally immature patients with transphyseal tunnels. Arthroscopy. 2012;28(11):1710–1717. [DOI] [PubMed] [Google Scholar]
- 46. Robbrecht C, Claes S, Cromheecke M, et al. Reliability of a semi-automated 3D-CT measuring method for tunnel diameters after anterior cruciate ligament reconstruction: a comparison between soft-tissue single-bundle allograft vs. autograft. Knee. 2014;21(5):926–931. [DOI] [PubMed] [Google Scholar]
- 47. Sabat D, Kundu K, Arora S, Kumar V. Tunnel widening after anterior cruciate ligament reconstruction: a prospective randomized computed tomography–based study comparing 2 different femoral fixation methods for hamstring graft. Arthroscopy. 2011;27(6):776–783. [DOI] [PubMed] [Google Scholar]
- 48. Shaw L, Finch CF. Trends in pediatric and adolescent anterior cruciate ligament injuries in Victoria, Australia 2005-2015. Int J Environ Res Public Health. 2017;14(6):599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Thomas NP, Kankate R, Wandless F, Pandit H. Revision anterior cruciate ligament reconstruction using a 2-stage technique with bone grafting of the tibial tunnel. Am J Sports Med. 2005;33(11):1701–1709. [DOI] [PubMed] [Google Scholar]
- 50. Thompson SM, Salmon LJ, Waller A, Linklater J, Roe JP, Pinczewski LA. Twenty-year outcome of a longitudinal prospective evaluation of isolated endoscopic anterior cruciate ligament reconstruction with patellar tendon or hamstring autograft. Am J Sports Med. 2016;44(12):3083–3094. [DOI] [PubMed] [Google Scholar]
- 51. van Melick N, van Cingel RE, Brooijmans F, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;50(24):1506–1515. [DOI] [PubMed] [Google Scholar]
- 52. Webster KE, Feller JA. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(11):2827–2832. [DOI] [PubMed] [Google Scholar]
- 53. Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(3):641–647. [DOI] [PubMed] [Google Scholar]
- 54. Werner BC, Yang S, Looney AM, Gwathmey FW., Jr Trends in pediatric and adolescent anterior cruciate ligament injury and reconstruction. J Pediatr Orthop. 2016;36(5):447–452. [DOI] [PubMed] [Google Scholar]
- 55. Willimon SC, Jones CR, Herzog MM, May KH, Leake MJ, Busch MT. Micheli anterior cruciate ligament reconstruction in skeletally immature youths: a retrospective case series with a mean 3-year follow-up. Am J Sports Med. 2015;43(12):2974–2981. [DOI] [PubMed] [Google Scholar]
- 56. Wong SE, Feeley BT, Pandya NK. Complications after pediatric ACL reconstruction: a meta-analysis. J Pediatr Orthop. 2019;39(8):e566–e571. [DOI] [PubMed] [Google Scholar]
- 57. Xu H, Lin W, Jin G, et al. Graft choice for anatomic anterior cruciate ligament reconstruction: the comparison between thin autograft and thick hybrid graft. An observational study. Medicine (Baltimore). 2018;97(30):e11597. [DOI] [PMC free article] [PubMed] [Google Scholar]