STRUCTURED ABSTRACT
Study design.
Analytical and numerical simulations.
Background.
Traditionally, low back pain (LBP) is studied using a reductionist approach, in which the factors contributing to the clinical presentation of LBP are studied in isolation to identify the primary pathology or condition linked to LBP. We argue that reductionism may not be suitable for studying LBP considering the complex, multi-factorial nature of this condition.
Objectives.
To quantify the likelihood of successfully subclassifying LBP patients and effectively targeting treatment based on a single, dominant factor contributing to LBP.
Methods.
Both the analytical and numerical simulations (Monte Carlo) of one million patients with LBP were performed. A number of factors contributing to LBP were randomly assigned to each individual. The following outcome measures were computed based on a number of factors: (1) The percentage of individuals that could be subclassified by identifying a single factor exceeding a certain threshold and (2) The average reduction in LBP when a treatment eliminates the largest contributing factor versus a multimodal treatment that eliminates a number of the randomly selected factors.
Results.
With an increasing number of factors, the probability of subclassifying an individual to a subgroup based on a single factor tends to zero. A multimodal treatment arbitrarily addressing any two or more factors was more effective than diagnosing and treating a single factor that maximally contributed to LBP.
Conclusion.
Results suggest that reductionism is not appropriate for subclassifying LBP or targeting treatment. The use of reductionist approaches may explain some of the challenges with creating LBP classification system and designing more effective treatment interventions.
Keywords: Randomized clinical trials, Subgrouping, Classification, Risk factors, Monte Carlo simulation
INTRODUCTION
Low back pain (LBP) is a multifactorial problem associated with many biological, psychological, and social factors8, 20, 28, 30. In most cases, the exact causes underlying LBP are unknown; hence, the “non-specific” LBP term is often used. This non-specificity makes selecting the appropriate treatment challenging for clinicians. Therefore, much of the current research efforts are directed toward identifying specific causal factors underlying the clinical presentation of LBP or subclassifying patients with specific characteristics (collection of factors that determine the nature of their LBP) to formulate the appropriate intervention strategies addressing these specific factors (hereafter referred to as “factors contributing to LBP”). This approach is based on the rationale that if more is known about the etiology of LBP, the treatment can be more specific in addressing the factors contributing to LBP and resulting in better outcomes. Subsequently, randomized clinical trials (RCTs) are conducted to evaluate whether such matching between factors contributing to LBP and treatment leads to improved outcomes in comparison to other treatments, standard care, or a sham treatment.
The above-outlined strategy in LBP research is termed a “reductionist” approach in the parlance of systems science1. With the reductionist approach, the system is broken-down into smaller parts to isolate and study them comprehensively. The reductionist approach is well-suited for containable diseases such as local infection. However, reductionism is less helpful when the problem is multi-factorial and where interactions between biological subsystems exist1. These features make the behavior of a complex system difficult to predict, even when the behavior of its parts is well defined1. For example, studying motor control in LBP patients is a reductionist approach whereby patho-mechanics of neuromuscular control are evaluated in isolation from all other biological, psychological, and social factors in a search for the primary pathology or condition linked to LBP. A natural extension of this approach is the development of intervention strategies attempting to correct such patho-mechanics27. Reductionism is not inherently wrong as it allows for the identification of parts of the system (e.g., factors associated with LBP), and has been useful for establishing factors associated with patient presentations (phenotypes) as an important part of patient care. The problem lies in the assumption that information about individual parts is sufficient to explain the behavior of the entire system. In this case, the assumption being other biological, psychological and social factors have minimal or no influence on motor control. Perhaps in some patients this may be the case, but the evidence suggests motor control interventions are not superior to other interventions in the management of patients with LBP27, which raises questions about other factors and interactions involved.
In contrast to reductionism, a systems approach takes the entire system into consideration when describing its behavior and identifying interdependence between its subsystems1. The attempts toward such an approach have been made with conceptual, structural equation, or collaborative modeling to account for a number of factors contributing to LBP simultaneously5, 6, 9, 18, 25. Yet, research in LBP substantially lags behind systems biology, which rapidly progressed in recent years with its effective application of systems science4, 14. There is a critical lack of knowledge regarding the number of factors and their interactions needed to adequately represent LBP, which in turn limits the ability to target them through treatment modalities. As spine research evolves, the trend points towards more complexity with more subsystems and their interactions requiring consideration6, 11.
There have been over 1,000 RCTs published evaluating various interventions for LBP, such as manual therapy, massage, acupuncture, dry needling, physical therapy, and specific exercise15. Unfortunately, this literature collectively shows low to moderate effects and practically no differences between various interventions3. More importantly, to date, “no classification system is supported by sufficient evidence to recommend its implementation into clinical practice”2, 7, 13. Even a triage based on various clinical prediction rules has not materialized in better outcomes13. One possible explanation for the lack of success in documenting large positive treatment outcomes could be the reductionist approach, typically applied in LBP research, whereby unimodal intervention strategies targeting the dominant factor believed to be contributing to LBP are compared and studied in RCTs. While this approach has its place in research, considering the extreme biological complexity of the spine system, the multi-factorial nature of LBP, and interactions among these factors20, 30 suggest that the reductionist approach may not be appropriate for LBP research and the development of more effective intervention strategies.
The goal of this paper is to highlight the challenges of studying a complex condition using reductionist approaches. Specifically, using analytical and numerical simulations, we quantified the likelihood of correctly identifying the dominant factor contributing to LBP and effectively treating LBP by modifying such a dominant factor. The following two hypotheses were tested: (1) When dealing with a large number of factors contributing to LBP, it is not possible to identify subgroups effectively based on the dominant factor, and (2) On a population scale, providing a number of treatments targeting any two or more factors is more effective than identifying and treating a single factor that maximally contributes to LBP. If these hypotheses are true, perhaps a different research approach, based on a systems approach1, could lead to the development of more effective intervention strategies for LBP.
METHODS
We performed both analytical and numerical simulations (Monte Carlo) of a large population (n=106) with LBP. Factors contributing to LBP for each individual were uniformly distributed random variates (U1, U2, U3, . . . Uk) between 0 and 1 (Fig. 1). For each individual, each factor Ui was normalized by dividing it by the sum of k factors to create a fraction contribution to LBP, e.g., the total pain/disability effect of 1: (X1+X2+…+Xk)=1. For example, for three factors (k=3), a person with LBP may have normalized factors such as X1=0.3, X2=0.1 and X3=0.6. This is interpreted as factor X1 contributes 30%, factor X2 contributes 10%, and factor X3 contributes 60% to the overall presentation of LBP, totaling 100%. To test the two hypotheses, we calculated: (1) Percentage of individuals that could be subclassified by identifying a single normalized factor Xi exceeding a certain threshold θ (where θ=0.2, 0.3, 0.4) and (2) The average reduction in pain/disability when the largest factor contributing to LBP is identified and eliminated with the targeted, unimodal treatment versus a number of treatments (i.e., multimodal treatment) eliminating a number of randomly selected factors.
FIGURE 1.
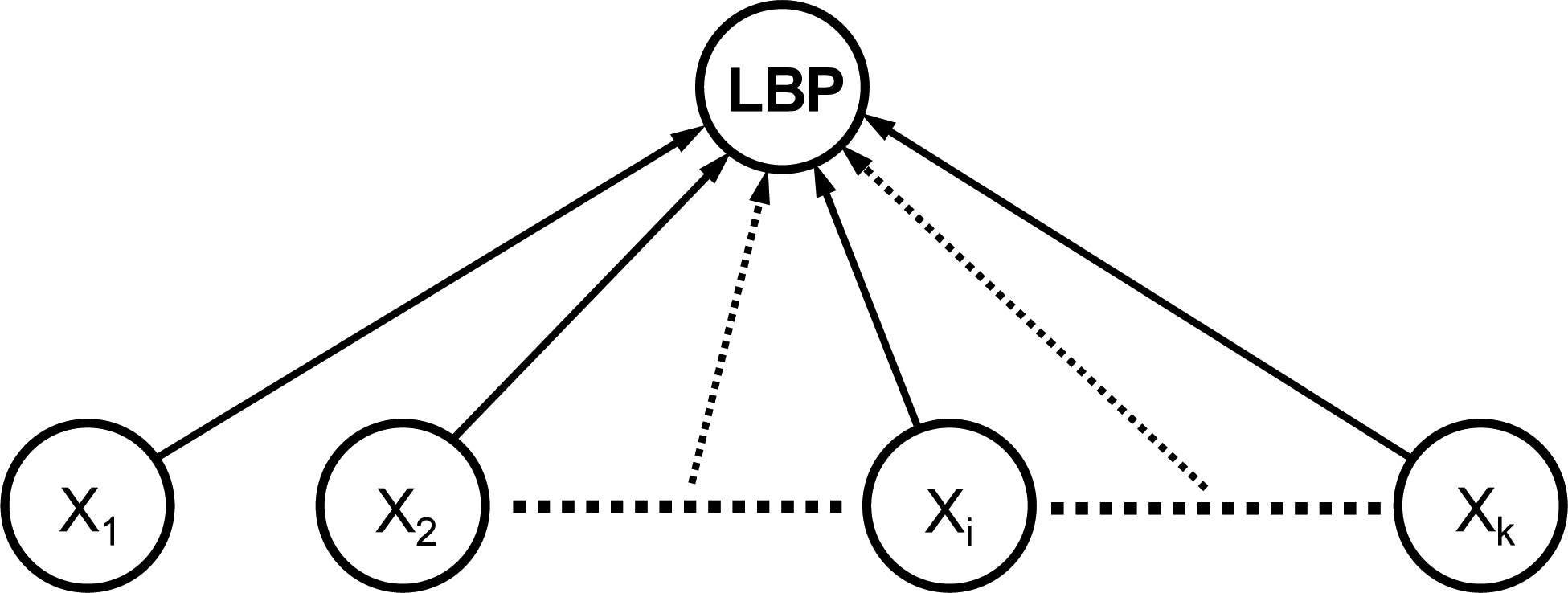
A schematic of a multifactorial, uniformly-distributed model of low back pain (LBP) used in this study. All factors contributing to the clinical presentation LBP were independent. Note that the sum of all factors (Xi) contributing to LBP is equal to 1 in every case simulated.
The analytical derivation and calculation of the hypothesized values is presented in the Appendix. To validate these analytical calculations, a numerical model simulation (Monte Carlo) was performed twice (Excel 2010 macro feature, Microsoft Corp.) by seeding an array with 106 random variables between 0 and 1 and calculating the values derived analytically.
RESULTS
The maximum difference between any analytically derived values and the two simulation results was 5.28×10−4 and 4.75×10−4. These small differences indicate an excellent agreement between the two methods, validating the analytical approach.
With an increasing number of factors, the probability of a single factor exceeding a certain threshold (Xi > θ) tends to zero (Fig. 2). In our model, this result represents the diminishing likelihood of classifying an individual to a subgroup of patients with LBP based on a single factor reaching some set threshold contribution to the overall LBP (Fig. 2). Even with a low threshold of θ = 0.2 (accounting for 20% of LBP symptoms), less than 1% of the LBP population can be subclassified when the number of factors exceeds 11.
FIGURE 2.
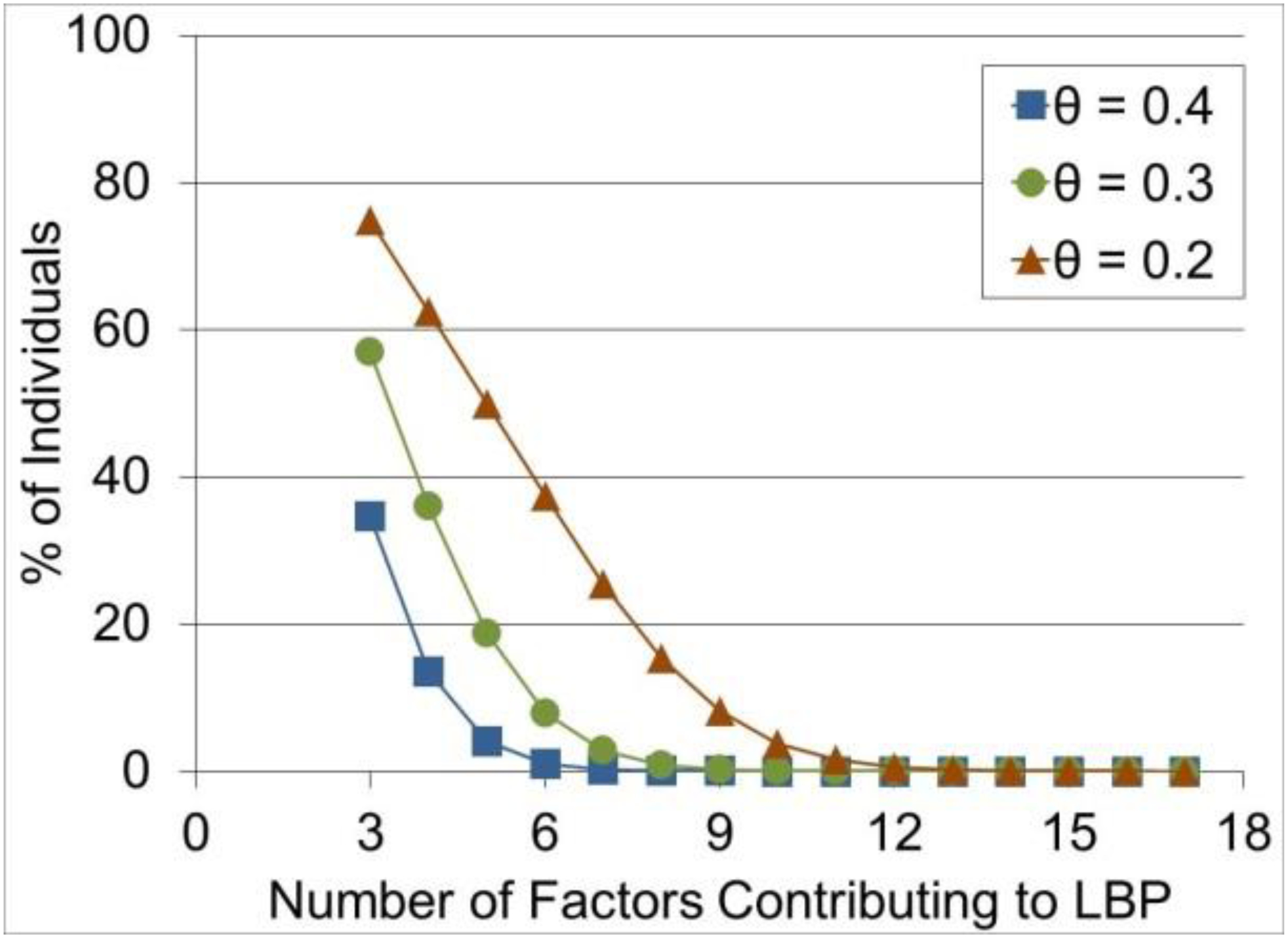
Percentage of individuals with low back pain (LBP) that can be subclassified based on a single factor exceeding a certain threshold θ.
On average, in a multifactorial model, the sum of any two or more factors is greater than the largest factor identified in each individual (Fig. 3). This simulation result illustrates that a multimodal intervention addressing any two or more factors, will likely be more effective in the population of patients with LBP than diagnosing and treating a single dominant factor that maximally contributes to LBP in each individual.
FIGURE 3.
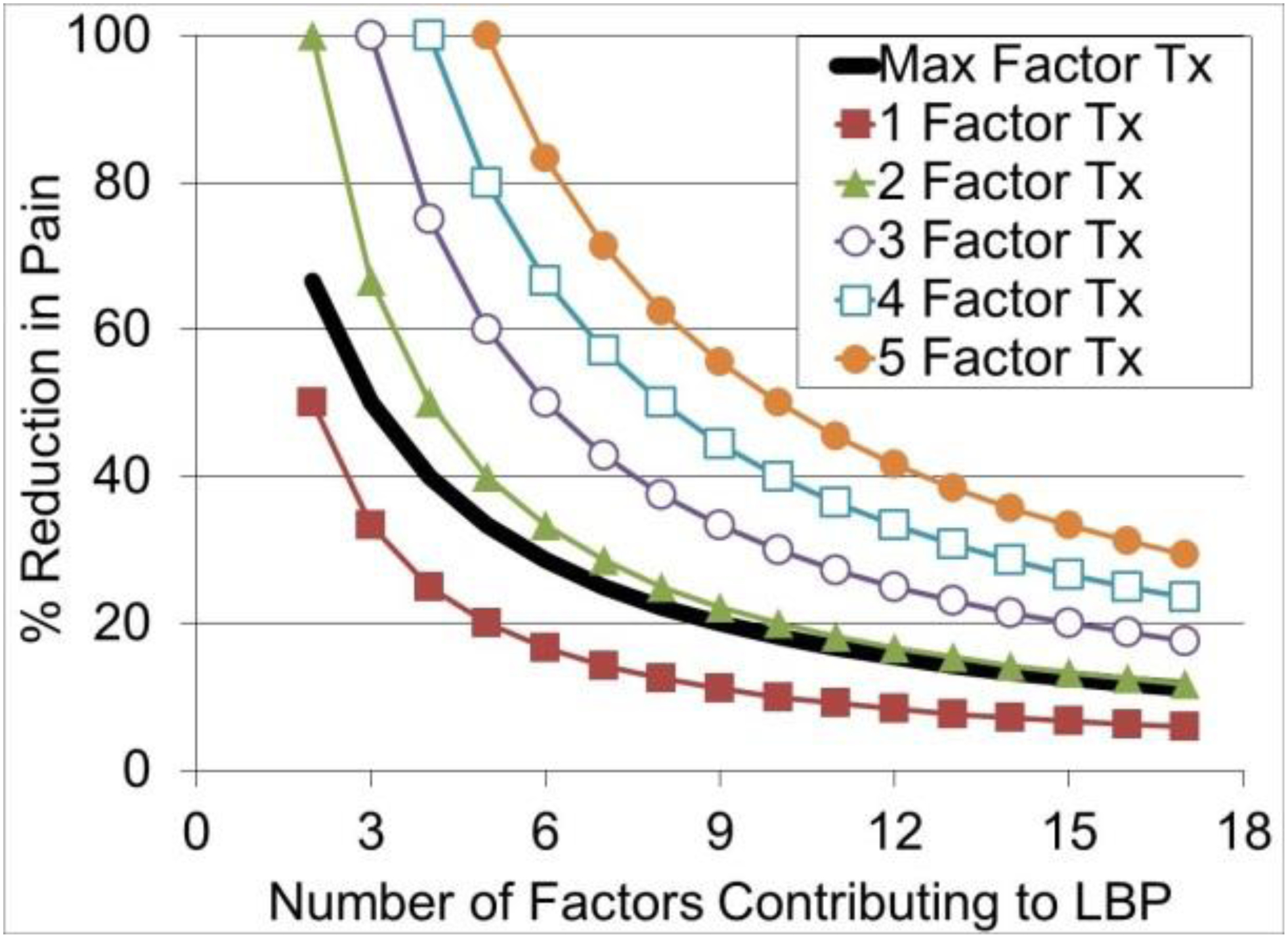
The average reduction in low back pain (LBP) when a given unimodal treatment eliminates the single largest contributing factor to LBP (Max Factor Tx) (solid black line) compared to a multimodal treatment eliminating a number of arbitrarily selected factors (1 Factor Tx, 2 Factor Tx, …, 5-Factor Tx) (lines with symbols). These results are plotted for different scenarios (number of total factors contributing to LBP) on the horizontal axis. Please note that 100% reduction in LBP is expected when a number of factors targeted by a treatment is the same as the total number of factors contributing to LBP.
DISCUSSION
The results from our analytical and numerical simulations of a multifactorial presentation of LBP are consistent with the data reported in the literature. With respect to the first hypothesis, our results show that with increasing number of factors contributing to LBP, there is diminishing likelihood of classifying an individual to a subgroup of patients based on the dominant factor. This could explain why attempts to identify subgroups of patients that would respond more favorably to a particular treatment have not yet been successful or reproduced2, 7, 13, 22, 23. Our simulations suggest that such a result would be expected if LBP were a large multifactorial problem. Reductionist research approaches, focusing at most on a few dominant factors contributing to LBP, are not able to address the entire complexity of this condition, nor document meaningful impact of interventions targeting those dominant factors. This scenario can be further complicated if many different mechanisms and factors interact and overlap, rendering the presence of pure subgroups rare16.
Based on the number of existing baseline predictors and the variance in outcomes they explain, Mistry et al., 2014 concluded that it is unlikely we can identify a single, strong moderator of LBP treatment effects19. None of the RCTs they reviewed were powered sufficiently to identify the differential subgroup effects and appropriately powered studies would be practically unrealistic19. To circumvent this problem, Patel et al., 2016 pooled data from 19 back pain trials that provided a data set of 9,328 patients23. Yet, they too did not find any subgroups that would benefit from specific treatment and, more importantly, they calculated that such an approach to identifying patients would not be cost-effective. Our simulations are in line with such findings. With only 12 factors contributing to LBP, only 0.5% of LBP population could be subclassified based on a single factor and treated to achieve a minimal clinically important difference of 20% reduction in pain21 (θ = 0.2, Fig. 2). What if there were 21 factors24, 69 factors8, or more6? Our simulation results indicate this percentage is 10−6 and 10−36 for 21 and 69 factors, respectively. Even if such an RCT could be conducted, it would likely have little clinical relevance.
With respect to the second hypothesis, it appears that multi-disciplinary (i.e., multimodal) rehabilitation strategies consistently show better results when compared to any single approach12. Likewise, our simulations suggest that when dealing with a multifactorial problem, it is more effective to treat several factors than trying to diagnose and treat the single dominant factor that contributes the most to LBP in each individual. Perhaps future research efforts should focus on designing effective multimodal, integrative, and adaptive approaches to the management of LBP17. As the management of patients with LBP continues to progress toward personalized medicine, multimodal treatment sequence, timing and interaction effects will need to be considered.
There are, however, instances in the literature where the combination of two treatment approaches (e.g., physical therapy (PT) and cognitive behavioral therapy (CBT)29) was not superior to a unimodal treatment (PT). One possibility in this example is that a single treatment modality (PT) affected several factors contributing to LBP31, including those targeted by the CBT. In our model, such a situation could be simulated by a comparison of a single treatment targeting a number of factors contributing to LBP versus the same number of unimodal treatments targeting a single factor. Both interventions would show the same effectiveness in such a comparison. Alternatively, in the above example, the psychological factors targeted by CBT might not have been important factors contributing to LBP in these patients.
Several assumptions determine the behavior of this model simulation. The assumption having probably the biggest effect on the results was that various factors contributing to LBP are uniformly distributed across the population with LBP. That is, all factors have the same probability of being present in each individual and there is no factor occurring more frequently in the LBP population. If some factors were occurring more frequently, it would have been easier to identify a cluster of patients with these factors. We submit, however, that in reality the distribution of factors contributing to LBP might be closer to uniform, because the studies thus far failed to identify a dominant, modifiable factor or subgroups of patients with LBP13. The simulated treatments were unrealistic because they completely eliminated the targeted factors contributing to LBP in every case. Most likely the real treatment effects would have been much smaller because interventions for LBP are not 100% effective and not all individuals respond to them. Another assumption that impacted the model results was that the model was unstructured (Fig. 1). Such a model assumes that each factor is independent and directly linked to LBP, which is unlikely the case. However, we purposefully chose such a model given that it represents the common factorial analyses used in back pain research. The addition of interactions between the factors, which could represent serial, parallel and feedback connections, would make the model more complex, strengthening the argument that the reductionist approaches are not appropriate to study the complex phenomena represented by such a model.
CONCLUSION
Research that aims to identify factors, or a group of factors, contributing to LBP is necessary, as is understanding the efficacy of individual treatment interventions, but neither are sufficient to effectively address the LBP problem. As it was demonstrated with our unstructured, multifactorial model of LBP, simply identifying the components within the model and not the structure of the model (i.e., interactions between these components) will not likely lead to robust classification or better treatment effects. To advance LBP research, more sophisticated modeling methods that consider the structure of the system being studied18,9 and possibly the dynamics of the system1 (i.e., LBP symptoms and treatment effects are not static and change with time) are needed. This will involve a paradigm shift towards a systems approach, which allows for integration of knowledge in a more systematic and effective way26. Systems approaches were specifically developed to address complexity and have been successful implemented in engineering, but also appear well suited for studying medical conditions that are multifactorial in nature1.
KEY POINTS.
Findings:
Analytical and numerical simulations of a reductionist approach to low back pain were performed.
With an increasing number of factors contributing to low back pain, the probability of finding subgroups of patients, based a single factor exceeding a certain threshold, tends to zero.
Arbitrarily applying treatments addressing any two or more factors was more effective in the simulated population of patients with LBP than diagnosing and treating a single factor that maximally contributed to LBP in each individual.
Implications:
A reductionist approach aiming toward identifying one or a few dominant factors contributing to LBP or subclassifying patients based on those factors will likely not result in the discovery of strong modifiers of treatment effects.
The simulations suggest that multimodal management of LBP will likely be more effective than unimodal treatment.
Caution:
The main assumptions influencing the specific numerical results were the uniformly distributed factors contributing to LBP and no interactions among them. While these assumptions affect the complexity of the modeled LBP problem, the simulation trends will likely hold for more complex models.
Acknowledgement
This publication was made possible in part by grant number U19AT006057 from the National Center for Complementary and Integrative Health (NCCIH) at the National Institutes of Health. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NCCIH.
APPENDIX
Hypothesis 1.
To estimate how many people can be subclassified based on identifying a single factor exceeding a certain threshold θ, we needed to calculate the probability (P) of a factor X1 > θ in the population with LBP. The following derivation is a consequence of the sampling distribution of a large number of uniform variates on the unit interval (0, 1).
Let U1, U2, . . , be independent, random variables uniformly distributed on the unit interval (0, 1). Let θ be a given number, 0 < θ < 1. Let Sk+1 = U1 + … + Uk+1, Xi = Ui ÷ Sk+1, 1 ≤ i ≤ k + 1.
We start with a set of cases where X1 > θ:
then probability P(X1 > θ)
where u has uniform distribution on (0, 1). For large k, the distribution of Sk is approximately normal with mean k/2 and standard deviation (Irwin-Hall distribution)10. Therefore,
in which Φ(z, μ, σ) denotes the cumulative distribution function of the normal variate with mean μ and standard deviation σ.
Hypothesis 2.
To address hypothesis 2, we have to estimate the expected value of the sum of m factors E(X1 + X2 + ⋯+ Xm) and the expected value of the maximum factor E(Xmax). Based on the same Irwin-Hall distribution10,
and
Therefore,
The expected value of the maximum factor is a ratio of 2 random variables and the first order approximation is:
Footnotes
The authors certify that they have no affiliations with or financial involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in the article.
REFERENCES
- 1.Ahn AC, Tewari M, Poon CS, Phillips RS. The limits of reductionism in medicine: could systems biology offer an alternative? PLoS Med. 2006;3:e208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Apeldoorn AT, Ostelo RW, van Helvoirt H, et al. A randomized controlled trial on the effectiveness of a classification-based system for subacute and chronic low back pain. Spine. 2012;37:1347–1356. [DOI] [PubMed] [Google Scholar]
- 3.Artus M, van der Windt DA, Jordan KP, Hay EM. Low back pain symptoms show a similar pattern of improvement following a wide range of primary care treatments: a systematic review of randomized clinical trials. Rheumatology. 2010;49:2346–2356. [DOI] [PubMed] [Google Scholar]
- 4.Bose B Systems biology: a biologist’s viewpoint. Prog Biophys Mol Biol. 2013;113:358368. [DOI] [PubMed] [Google Scholar]
- 5.Buchbinder R, Batterham R, Elsworth G, Dionne CE, Irvin E, Osborne RH. A validity-driven approach to the understanding of the personal and societal burden of low back pain: development of a conceptual and measurement model. Arthritis Res Ther. 2011;13:R152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cholewicki J, Popovich JM Jr., Aminpour P, Gray SA, Lee AS, Hodges PW. Development of a collaborative model of low back pain: report from the 2017 NASS consensus meeting. Spine J. 2018; in press. [DOI] [PubMed] [Google Scholar]
- 7.Deyo RA, Dworkin SF, Amtmann D, et al. Report of the NIH task force on research standards for chronic low back pain. Spine. 2014;39:1128–1143. [DOI] [PubMed] [Google Scholar]
- 8.Dolphens M, Vansteelandt S, Cagnie B, et al. Multivariable modeling of factors associated with spinal pain in young adolescence. Eur Spine J. 2016;25:2809–2821. [DOI] [PubMed] [Google Scholar]
- 9.Fritz JM, Koppenhaver SL, Kawchuk GN, Teyhen DS, Hebert JJ, Childs JD. Preliminary investigation of the mechanisms underlying the effects of manipulation: exploration of a multivariate model including spinal stiffness, multifidus recruitment, and clinical findings. Spine. 2011;36:1772–1781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hall P The distribution of means for samples of size n drawn from a population in which the variate takes values between 0 and 1, all such values being equally probable. Biometrika. 1927;19:240–244. [Google Scholar]
- 11.Hodges PW. Adaptation and rehabilitation: from motorneurons to motor cortex and bahaviour In: Hodges PW, Cholewicki J, Van Dieen JH, eds. Spinal control: the rehabilitation of back pain. State of the art and science. Edinburgh: Elsevier; 2013:59–73. [Google Scholar]
- 12.Kamper SJ, Apeldoorn AT, Chiarotto A, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ. 2015;350:h444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kamper SJ, Maher CG, Hancock MJ, Koes BW, Croft PR, Hay E. Treatment-based subgroups of low back pain: a guide to appraisal of research studies and a summary of current evidence. Best Pract Res Clin Rheumatol. 2010;24:181–191. [DOI] [PubMed] [Google Scholar]
- 14.Kesic S Systems biology, emergence and antireductionism. Saudi J Biol Sci. 2016;23:584–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J. 2010;19:2075–2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lemeunier N, Leboeuf-Yde C, Gagey O, Wedderkopp N, Kjaer P. Do number of days with low back pain and patterns of episodes of pain have similar outcomes in a biopsychosocial prediction model? Eur Spine J. 2016;25:2774–2787. [DOI] [PubMed] [Google Scholar]
- 17.Maiers MJ, Westrom KK, Legendre CG, Bronfort G. Integrative care for the management of low back pain: use of a clinical care pathway. BMC Health Serv Res. 2010;10:298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Melton BL, Moqbel M, Kanaan S, Sharma NK. Structural Equation Model of Disability in Low Back Pain. Spine. 2016;41:1621–1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mistry D, Patel S, Hee SW, Stallard N, Underwood M. Evaluating the quality of subgroup analyses in randomized controlled trials of therapist-delivered interventions for nonspecific low back pain: a systematic review. Spine. 2014;39:618–629. [DOI] [PubMed] [Google Scholar]
- 20.O’Sullivan P, Caneiro JP, O’Keeffe M, O’Sullivan K. Unraveling the Complexity of Low Back Pain. J Orthop Sports Phys Ther. 2016;46:932–937. [DOI] [PubMed] [Google Scholar]
- 21.Ostelo RW, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine. 2008;33:90–94. [DOI] [PubMed] [Google Scholar]
- 22.Patel S, Friede T, Froud R, Evans DW, Underwood M. Systematic review of randomized controlled trials of clinical prediction rules for physical therapy in low back pain. Spine. 2013;9:762–769. [DOI] [PubMed] [Google Scholar]
- 23.Patel S, Hee SW, Mistry D, et al. Identifying back pain subgroups: developing and applying approaches using individual patient data collected within clinical trials. Programme Grants Appl Res. 2016;4: [PubMed] [Google Scholar]
- 24.Pincus T, Santos R, Breen A, Burton AK, Underwood M, Multinational Musculoskeletal Inception Cohort Study C. A review and proposal for a core set of factors for prospective cohorts in low back pain: a consensus statement. Arthritis Rheum. 2008;59:14–24. [DOI] [PubMed] [Google Scholar]
- 25.Poitras S, Rossignol M, Dionne C, et al. An interdisciplinary clinical practice model for the management of low-back pain in primary care: the CLIP project. BMC Musculoskelet Disord. 2008;9:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reeves NP, Cholewicki J. Spine Systems-Science: a primer on the systems approach In: Hodges PW, Cholewicki J, Van Dieen JH, eds. Spinal Control: The Rehabilitation of Back Pain. Oxford, UK: Elsevier; 2013:7–13. [Google Scholar]
- 27.Saragiotto BT, Maher CG, Yamato TP, et al. Motor control exercise for chronic nonspecific low-back pain. Cochrane Database Syst Rev. 2016;CD012004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Serbic D, Pincus T, Fife-Schaw C, Dawson H. Diagnostic uncertainty, guilt, mood, and disability in back pain. Health Psychol. 2016;35:50–59. [DOI] [PubMed] [Google Scholar]
- 29.Smeets RJ, Vlaeyen JW, Hidding A, et al. Active rehabilitation for chronic low back pain: cognitive-behavioral, physical, or both? First direct post-treatment results from a randomized controlled trial [ISRCTN22714229]. BMC Musculoskelet Disord. 2006;7:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sullivan MJ. Toward a biopsychomotor conceptualization of pain: implications for research and intervention. Clin J Pain. 2008;24:281–290. [DOI] [PubMed] [Google Scholar]
- 31.van Middelkoop M, Rubinstein SM, Verhagen AP, Ostelo RW, Koes BW, van Tulder MW. Exercise therapy for chronic nonspecific low-back pain. Best Pract Res Clin Rheumatol. 2010;24:193–204. [DOI] [PubMed] [Google Scholar]


