ABSTRACT
Background: Posttraumatic stress disorder (PTSD) is common in patients with personality disorders. This comorbidity is accompanied by a lower quality of life, and a higher risk of suicide attempts than patients with only one of these diagnoses.
Objective: The aim of this systematic review and meta-analysis was to evaluate the scientific evidence of the efficacy of PTSD treatments for this population.
Method: A literature search was performed from 1946 through June 2020. Standardized mean effect sizes of psychotherapy for PTSD were computed.
Results: The literature search revealed that psychotherapy was the only intervention that was systematically explored. Fourteen studies were included. In 12 of these studies solely patients with borderline personality disorder participated. Analysis of the four RCTs showed a significant, moderate to high standardized effect size for reducing PTSD symptom severity (Hedges’ g = 0.54), with effects being maintained at least 3 months (Hedges’ g = 0.82). Effect sizes for all studies were also significant, with moderate to high standardized values for symptoms of PTSD (Hedges’ g = 1.04). PTSD improvements were again maintained at 3-month follow-up and beyond (Hedges’ g = 0.98). In addition, a significant decrease in symptoms of depression, anxiety, borderline symptoms, and PTSD in patients with borderline personality disorder could be revealed for all studies (Hedges’ g 0.48–1.04). No increase in self-injurious behaviour, suicide attempts, or hospitalization was observed, while the mean weighted dropout rate during PTSD treatment was 17%.
Conclusions: Psychotherapy for PTSD is efficacious and safe for patients with borderline personality disorder and should not be withheld from these vulnerable individuals.
KEYWORDS: borderline personality disorder, psychotherapy, clinical trial, efficacy, safety, trauma
HIGHLIGHTS: • Psychotherapy reduces PTSD symptom severity in patients with borderline personality disorder.• The duration of the reduction of PTSD symptom severity after psychotherapy is at least three months.• Risks associated with psychotherapy for PTSD are low in this population.
Antecedentes: El trastorno de estrés postraumático (TEPT) es común en pacientes con trastornos de la personalidad. Esta comorbilidad se acompaña de una menor calidad de vida y un mayor riesgo de intentos de suicidio que los pacientes con solo uno de estos diagnósticos.
Objetivo: El propósito de esta revisión sistemática y metanálisis fue evaluar la evidencia científica de la eficacia de los tratamientos de TEPT para esta población.
Método: Se realizó una búsqueda bibliográfica desde 1946 hasta junio de 2020. Se calcularon los tamaños de efecto promedio estandarizados de la psicoterapia para el TEPT.
Resultados: La búsqueda de la literatura reveló que la psicoterapia fue la única intervención explorada sistemáticamente. Se incluyeron catorce estudios. En doce de estos estudios participaron únicamente pacientes con trastorno límite de la personalidad. El análisis de los cuatro ECA mostró un tamaño de efecto estandarizado significativo, moderado a alto, para reducir la gravedad de los síntomas de TEPT (Hedges’ g = 0.54), con efectos que se se mantenían al menos tres meses (Hedges’ g = 0.82). Los tamaños del efecto para todos los estudios también fueron significativos, con valores estandarizados moderados a altos para síntomas de TEPT (Hedges’ g = 1.04). Las mejoras del TEPT también se mantuvieron a los 3 meses de seguimiento y más allá (Hedges’ g = 0.98). Adicionalmente, en todos los estudios podría ser revelada una disminución significativa de los síntomas de depresión, ansiedad, síntomas límite y trastorno de estrés postraumático en pacientes con trastorno límite de la personalidad (Hedges‘g 0.48 – 1.04). No se observó aumento en el comportamiento autolesivo, intentos de suicidio u hospitalización, mientras que la tasa de abandono ponderada media durante el tratamiento del TEPT fue del 17%.
Conclusiones: La psicoterapia para el trastorno de estrés postraumático es eficaz y segura para pacientes con trastorno límite de la personalidad y no debiera ser negada a estos individuos vulnerables.
PALABRAS CLAVE: trastorno límite de la personalidad, psicoterapia, ensayo clínico, la seguridad
背景: 创伤后应激障碍 (PTSD) 在人格障碍患者中很常见。这种并发情况相较于只有一种诊断的患者, 伴随着更低的生活质量和更高的自杀企图风险。
目的: 本系统评综述和元分析旨在评估PTSD治疗对该人群疗效的科学证据。
方法:从1946年至2020年6月进行文献检索。计算了PTSD心理治疗的标准化平均效应量。
结果: 文献检索表明, 心理治疗是唯一被系统性探讨的干预措施。纳入了十四项研究。其中12项研究只有边缘性人格障碍患者参与了研究。对四个随机对照试验的分析显示了PTSD症状严重程度下降具有中等到较高的显著标准化效应量 (Hedges g= 0.54), 并且效果至少维持了三个月 (Hedges g= 0.82) 。所有研究的效应量也显著, PTSD症状具有中等至较高的标准化值 (Hedges g= 1.04) 。 PTSD的改善在3个月及以后的随访中均得以维持 (Hedges g= 0.98) 。此外, 所有研究均显示, 边缘性人格障碍患者的抑郁, 焦虑, 边缘性症状和PTSD症状显著减少 (Hedges’ g :0.48– 1.04) 。没有发现自残行为, 自杀企图或住院的增加, 而PTSD治疗期间的平均加权退出率为17%。
结论: 对于边缘型人格障碍的患者, PTSD的心理治疗是有效且安全的, 不应被这些易受伤个体拒绝。
关键词: 心理治疗, 临床试验, 安全性
1. Introduction
Posttraumatic stress disorder (PTSD) is a severe mental disorder characterized by traumatic intrusions and the persistent avoidance of stimuli associated with the traumatic event(s) (American Psychiatric Association, 2013). Its lifetime prevalence in the general population varies between 1.3% in Japan and 9.2% in the US (Atwoli, Stein, Koenen, & McLaughlin, 2015). PTSD is associated with serious consequences for the people suffering from the syndrome, affecting their daily functioning and quality of life, while increasing the use of health and social services (Atwoli et al., 2015).
With relaxation training and medication being offered widely, of all available interventions for PTSD, psychotherapy is the treatment of choice. Several meta-analyses have evaluated the efficacy of such PTSD programmes (Bisson et al., 2007; Carpenter et al., 2018; Chen et al., 2014; Ehring et al., 2014; Khan et al., 2018; Lewis, Roberts, Andrew, Starling, & Bisson, 2020). In their meta-analysis of treatments for chronic PTSD, Bisson et al. found cognitive-behavioural therapy (CBT), eye movement desensitization and reprocessing (EMDR), and stress management to be superior to a waiting-list condition and usual care, finding moderate to high standardized mean differences (i.e. 0.43 up to 1.51) (2007). Comparing CBT, trauma-focused CBT, EMDR, and other interpersonal, emotion-focused treatments, Ehring et al. (2014) obtained an effect size of 0.72 for psychotherapy for patients suffering from PTSD resulting from childhood abuse. In a third meta-analysis, EMDR was found to significantly reduce symptoms of PTSD, depression, anxiety, and subjective distress, with effect sizes ranging from 0.64 to 0.96 (Chen et al., 2014). A recent increase in randomized-controlled trials of psychological therapies for PTSD, resulted in a more confident recommendation of trauma-focused CBT and EMDR as the first-line treatments (Lewis et al., 2020). In addition, the findings of a meta-analysis of Khan and colleagues suggest that EMDR may be better than CBT in reducing posttraumatic symptoms and anxiety (Khan et al., 2018).
In these meta-analyses, treatments all targeted patients diagnosed with PTSD without the presence or absence of comorbid disorders being investigated or reported. The results can therefore not be extrapolated to patients with known comorbid conditions such as personality disorders. Already coping with impairments in cognition, emotion regulation, interpersonal functioning, and impulse control, arguably, this group is even more vulnerable to trauma; reported rates of childhood abuse are, for instance, high. Systematic knowledge about PTSD in this population is, however, mostly restricted to patients with a borderline personality disorder (BPD), who have a prevalence rate up to 3% within the normal population (Samuals et al., 2002). Childhood maltreatment in terms of verbal, physical, and sexual abuse, has been reported in 72%, 46% and 26%, respectively (Zanarini, Gunderson, Marino, Schwartz, & Frankenburg, 1989).
With prevalence rates of 34% to 46% being mentioned, PTSD is quite common in patients with BPD (Slotema, Blom, Niemantsverdriet, Deen, & Sommer, 2018; Zanarini et al., 1998). Due to this comorbidity, they are known to have a lower quality of life, other comorbid disorders, a higher risk of suicide attempts, and a higher prevalence of childhood trauma than patients with only one of the diagnoses (Pagura et al., 2010). Within patients with BPD and comorbid PTSD, it is recommended that management of suicidal and non-suicidal self-injury behaviours take place before the onset of trauma-focused treatment (Ursano et al., 2004). However, the exclusion of patients with this behaviour seems problematic as many of these patients exhibit this behaviour in order to reduce their suffering from intrusions or dissociative states (Albach & Everaerd, 1992; Amir, Kaplan, Efroni, & Kotler, 1999). Lastly, Zanarini et al. documented a prevalence rate of PTSD for personality disorders other than BPD of 22% in an American sample of inpatients (Zanarini et al., 1998).
In 2001, Cloitre and Koenen were the first to report on a clinical trial evaluating interpersonal process group therapy in female patients with PTSD and personality disorders (2001). They found that in the subgroup of women with BPD, PTSD symptoms had not improved. Since then, more clinical trials have been conducted, some of which did observe a positive influence of psychotherapy on the severity of PTSD in personality disorders. We accordingly felt it was opportune to examine the evidence on the efficacy of PTSD interventions in these vulnerable patients. In the present systematic review and meta-analysis we sought to answer the following questions: 1. Can we quantify the effects of PTSD treatment on the severity of PTSD-related symptoms in patients with all types of personality disorders? 2. Does PTSD treatment ameliorate other symptoms unrelated to the PTSD, such as depression, anxiety and borderline symptoms? 3. What is the outcome of PTSD treatment on PTSD symptom severity in patients with BPD? And 4. What is known about the effects of PTSD treatment on PTSD symptom severity three months after treatment conclusion and beyond?
In our systematic review of the relevant literature, we were curious to learn what has been reported about the risks assumed to be associated with PTSD interventions in comorbid populations, such as suicidal – and nonsuicidal self-injurious behaviour, and the number of patients dropping out of the trauma-focused treatments.
2. Methods
The review protocol was registered with The International Prospective Register of Systematic Reviews (PROSPERO), number of identification CRD42020144999 and conducted conform PRISMA guidelines for systematic reviews.
2.1. Literature search
A systematic search of the literature was conducted by two independent reviewers using Medline and Pre-Medline (PubMed alike) 1946 to June 2020, EMBASE 1974 to June 2020, and PsycINFO 1806 to June 2020 with the following key words: posttraumatic stress disorder, personality disorder and treatment for PTSD. The Boolean connector AND was used to combine the three key words.
The exact literature search was as follows:
A search of the literature was conducted using Medline and Pre-Medline (PubMed alike) 1946 – June 2020, EMBASE 1974 to June 2020, and PsycINFO 1806 – June 2020 with the search terms:
(personality disorders, antisocial personality disorder, borderline personality disorder, compulsive personality disorder, dependent personality disorder, histrionic personality disorder, hysteria, paranoid personality disorder, passive-aggressive personality disorder, schizoid personality disorder, schizotypal personality disorder, narcissism, narcissistic personality disorder, obsessive-compulsive personality disorder, stress disorders, schizoidism, borderline state, character disorder, Diogenes syndrome, psychopathy, compulsion, obsession, dark triad, avoidant personality disorder, obsessive personality, hoarding disorder, narcissus or sadomasochistic personality)
AND (post-traumatic, PTSD, posttraumatic stress disorder, or post-traumatic stress disorder, complex PTSD, or DESNOS)
AND (therapeutics, psychiatry, psychology, clinical, emergency services, psychiatric, electroshock, pharmacological actions, treatment outcome, treatment failure, program(me) evaluation, therapy, diet, therapy, drug therapy, health care, therapeutic processes, rehabilitation, psychotherapy, program, intervention, counsel, pharmacotherapy, medication, drug, lifestyle, coaching, clinical psychology, clinical outcome, patient-reported outcome, psychiatric treatment, psychopharmacology, psychotropic agent, treatment, effectiveness evaluation, counselling, couples therapy, client treatment matching, posttreatment, follow-up, prescribing, side effects, or follow-up)
Titles and abstracts were screened with the aid of the inclusion criteria. Any uncertainties and disagreements were discussed until consensus was reached. The website Google Scholar was examined to identify additional studies that had not yet been included in the aforementioned databases by checking the citations of the studies that were included into the systematic review. Furthermore, a hand search of reference lists of all relevant papers and major reviews was conducted.
2.2. Inclusion criteria
For our meta-analyses, we used the following nine inclusion criteria: 1. Presence of current PTSD according to the Diagnostic and Statistical Manual of Mental Disorders IV and 5 (DSM-IV and −5), 2. Presence of a personality disorder according to the DSM-IV and −5, 3. Outcome measures including PTSD symptom severity assessed using a validated instrument (self-report or structured clinical interview), 4. Randomized-controlled, nonrandomized, or uncontrolled studies design, 5. A control condition other than treatment for PTSD in case of a randomized-controlled design, 6. At least pre- and post-treatment assessments or a pre-treatment and at least one follow-up assessment, 7. Written in English, 8. Published in a peer-reviewed journal, and 9. Sufficient data for the computation of standardized effect sizes (i.e. sample size, means, standard deviations (SDs), or exact t, F or p values) for the main effect for change scores.
We intended to perform a meta-analysis if at least three randomized-controlled trials (RCTs) could be included, where we regarded RCTs comparing at least one active treatment to at least one control condition as the gold standard. However, in a developing research area such as this, with a small number of RCTs having been conducted, it may be useful to also include studies with weaker designs. Therefore, we performed separate meta-analyses for RCTs and the total number of eligible studies identified, including nonrandomized and uncontrolled research reports. Publications that failed to meet criterion 8 (sufficient data) but did report whether the change in PTSD severity was significant, were excluded from the meta-analyses but nevertheless considered relevant and included in our qualitative review.
2.3. Data extraction
Data were extracted and reviewed by two authors independently of each other according to the current review protocol and checked against the original manuscripts. The data collected for the meta-analyses comprised the number of patients per treatment condition, pre- and posttreatment means and SDs for PTSD symptom severity at baseline and at the end of treatment, or exact F, t, or p values. In addition, we documented the study design, population(s) (i.e. type of personality disorders), type of trauma, type of treatment, and the number and duration of sessions.
When publications contained insufficient and/or incomplete results, the authors were approached personally with a request to grant access to any additional data. The analysis was restricted to the largest sample size in the case of different publications with overlapping patient samples. If PTSD symptom severity was assessed with both a structured clinical interview and a self-report instrument, the first was used for the meta-analysis. Comparators other than treatment for PTSD were accepted as control condition in RCTs. Examples of control conditions are waiting list, treatment as usual for personality disorders and psycho-education.
2.4. Computation of effect sizes
We opted for the mean weighted effect size, Hedges’ g, which was computed with the aid of the Comprehensive Meta-Analysis, Version 3 (Biostat, Englewood, NJ). The analyses were performed in a random-effects model given that Hedges’ g is a standardized effect-size measure that corrects for the bias introduced by using the sample SD of treatment responses instead of the population SD. Effect sizes (Hedges’ g) were calculated for the mean change in PTSD symptom severity (pre-to-posttreatment states) for the separate study conditions and divided by the SD reported in the study. If posttreatment data were absent, data derived from follow-up measurements were used. In studies reporting on more than one treatment arm and a control condition, the active treatments were each compared separately with the placebo condition. Finally, meta-analytic methods were used to obtain a pooled, standardized effect size.
2.5. Heterogeneity
We used a random-effects model in order to account for variation among studies. A homogeneity statistic, I2, was computed to test whether the studies could be taken to share a common population effect size (Higgins & Thompson, 2002). Furthermore, heterogeneity in the effect sizes obtained for the various studies was determined by means of a moderator analysis again using the Comprehensive Meta-Analysis method. The parameters entered into the analyses were: type of population(s) dichotomously categorized as patients with personality disorders or BPD, type of psychotherapy, treatment intensity in terms of the total number of minutes, nature of the intervention, i.e. stand-alone or add-on treatment, individual, group, or a combination of individual and group therapy, and treatment venue, i.e. in- or outpatient setting. Q-values represent the results of these analyses. This value consists of a weighted sum of squared deviations around the mean of the effect in each study (DerSimonian & Laird, 1986). The Benjamini-Hochberg procedure was used to correct for multiple testing (Benjamini & Hochberg, 1995). In this procedure the individual P values are placed in order, from smallest to largest, and compared to the Benjamini-Hochberg critical value, i.e., 0.05 divided by the rank of the individual P value. The P values below this critical value are significant.
2.6. Publication bias
Because effect sizes can be over- or underestimated due to the absence of studies with negative results, a fail-safe number was computed, that is, an estimation of the number of missing studies necessary to change the results of the meta-analysis from significant to nonsignificant (Rosenthal, 1997). In addition, a funnel plot was created to visually examine the potential influence of publication bias. Egger’s regression intercept was used as a formal test of funnel-plot asymmetry (Egger, Smith, Schneider, & Minder, 1997).
2.7. Quality of studies
The quality of all eligible publications was inspected based on the following criteria: Was PTSD diagnosed using a structural clinical interview? Were random sequence generation and masked outcome assessments applied? Were the number of withdrawals during treatment and tolerability reported on? Were outcomes re-assessed at follow-up in addition to post-treatment and intention-to-treat analyses? These criteria were based on the validity assessment method of Bisson and colleagues (Bisson et al., 2007).
2.8. Dropout
A mean-weighted dropout rate was computed, with dropout being defined as the percentage of the total number of patients having terminated the PTSD treatment prematurely.
3. Results
3.1. Systematic review
3.1.1. Characteristics of eligible studies
The literature search revealed a total number of hits of 925 for Medline, 3358 for EMBASE and 179 for PsycINFO. The reasons for exclusion are listed in Figure 1. Of the same 3888 studies, 3871 did not meet our inclusion criteria for a systematic review. Seventeen studies (with a total of 509 patients) were included for review, comprising eight RCTs (totalling 225 patients), two controlled studies (totalling 33 patients), and seven open-label studies (totalling 251 patients) (see Table 1 part A and B). Data regarding treatment, outcome measures, and population types are presented in Table 1. In all 17 studies, psychotherapy was the intervention used to treat PTSD; in approximately half, the therapy was offered as an addition to other ongoing treatments unrelated to PTSD (Harned, Korslund, & Linehan, 2014; Kredlow et al., 2017; Pabst et al., 2014; Slotema, van den Berg, Driessen, Wilhelmus, & Franken, 2019; Steuwe et al., 2016; Walter, Bolte, Owens, & Chard, 2012). Fourteen of the 17 studies reviewed reported a statistically significant reduction in PTSD symptom severity.
Figure 1.
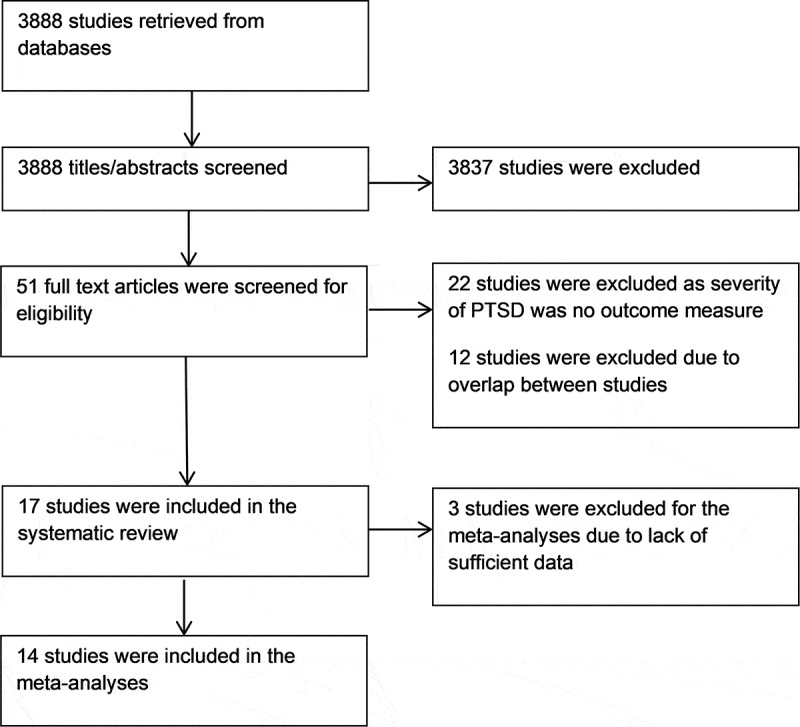
Flowchart of studies exploring the effects of psychotherapy of posttraumatic stress disorder (PTSD) in patients with personally disorders.
Table 1.
The studies exploring the efficacy of psychotherapy for PTSD in patients with personality disorders included in the meta-analyses (part A) and additional studies added in the review (part B).
| Study | Design | N active arm | N control condition | Personality disorder | Intervention | Control | Treatment intensity | Outcome measure | Statistical significant | Dropout | Population and trauma |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Part A | |||||||||||
| Bohus et al., 2013 | RCT | 17 | 16 | BPD | DBT-PTSD | TAU WL | Group and individual, sessions totalling 7280 min | CAPS PDS |
+ + |
6% and 8% (with and without BPD) | Women – childhood sexual abuse and treatment-resistant PTSD |
| Harned et al., 2014 | RCT | 17 | 9 | BPD | DBT+PE | DBT | Individual, mean 13 90-min sessions | PSS-I | + | 25% | Women – (non)suicidal self-injurious behaviour, childhood abuse and other traumas |
| Kredlow et al., 2017 I | RCT | 15 | 12 | BPD | CBT | TAU | Individual, 12–16 50- mins essions | CAPS | + | 14% | Women and men – childhood abuse and other traumas |
| Kredlow et al., 2017 II | RCT | 29 | 26 | BPD | CBT | BT | Individual, 12–16 50-min sessions | CAPS | - | 26% and 13% | Women and men – childhood abuse and other traumas Severe PTSD CAPS ≥65 |
| Feeny et al., 2002 | RCT | 9 | - | BPC | PE, SIT, or PE + SIT | - | Individual, 9 sessions mean 97 min | PSS-I | + | 25% | Women – sexual and nonsexual assault Chronic PTSD |
| Walter et al., 2012 | Open | 110 | - | Personality disorders | CPT | - | 12 sessions of 90-min group CPT, 13 individual sessions 50–60 min | CAPS PCL |
+ + |
7% (with and without PD) | Female and male patients – combat, childhood sexual abuse and other traumas |
| Harned et al., 2012 | Open | 13 | - | BPD | DBT+PE | - | Individual 90 min, mean 13 sessions Plus DBT |
PSS-I | + | 23% | Women – (non)suicidal self-injurious behaviour, childhood abuse and other traumas |
| Pabst et al., 2014 | CT | 11 | 11 | BPD | NET | TBE | Individual, 17 to 90 min | PDS | - | 18% | Women – physical and sexual abuse |
| Steuwe et al., 2016 | Open | 11 | - | BPD | NET | - | Individual, 15 sessions mean 97 min | PDS | + | 9% | Female and male patients – childhood abuse and other traumas |
| Holder et al., 2017 | RCT | 7 | - | BPD | CPT | - | Individual, 12 sessions, minutes NA | CAPS PCL |
+ + |
29% | Women – military sexual trauma, only patients randomized for CPT were included |
| Meyers et al., 2017 | Open | 14 | - | BPD | DBT + PE | - | Group and individual, sessions NA, min NA | PCL | + | 29% | Female and male patients – veterans Data available for 14 patients |
| Slotema et al., | Open | 47 | - | Personality disorders | EMDR | - | Individual, median 4 sessions, mean 75 min | PDS | + | 32% | Female and male patients – 82% childhood trauma and other traumas |
| Steil et al., 2018 | Open | 21 | - | ≥ 4 BPD criteria, 75% BPD | DBT-PTSD | - | Group and individual, up to 40 hours | CAPS DTS |
+ + |
19% | Women – childhood sexual abuse |
| De Jongh et al., 2020 | Open | 35 | - | Borderline symptom List ≥2 | PE + EMDR Physical exercise, psycho-education |
- | Individual 1440 minutes | CAPS PCL |
+ + |
0 | Woman and men with childhood abuse and other traumas |
| Part B | |||||||||||
| Cloitre & Koenen, 2001 | CT | 5 | 6 | BPD | Interpersonal process group therapy | WL | Group, 12 sessions, 90 min | PSS | - | NA | Data not sufficient for meta-analysis Women – childhood sexual abuse |
| Hembree et al., 2004 | RCT | 29 | - | Personality disorders | PE or PE/CR | - | Individual, number of sessions NA, 105 min |
PSS-I Prevalence of PTSD |
NA + |
NA | Prevalence of PTSD outcome measure Data not sufficient for meta-analysis Women – rape or nonsexual assault in adulthood or sexual abuse in childhood, chronic PTSD |
| Clarke et al., 2008 | RCT | 39 | - | BPD | CBT | - | Individual, 9 sessions, mean 87 min | CAPS | + | 36% with and without PD | Data not sufficient for meta-analysis Female rape victims |
BPC = borderline personality characteristics, BPD = borderline personality disorder, BT = brief treatment (involving breathing training and psycho-education about trauma and PTSD), CAPS = Clinician-Administered PTSD Scale, CBT = cognitive-behavioural therapy, CPT = cognitive-processing therapy, CT = controlled trial, DBT = dialectical behavioural therapy, DTS = Davidson Trauma Scale, EMDR = eye movement desensitization and reprocessing, NA = not applicable, NET = narrative exposure therapy, PCL = Posttraumatic stress disorders CheckList, PD = personality disorder, PDS = Posttraumatic Stress Diagnostic Scale, PE = prolonged exposure, PE/CR = prolonged exposure and cognitive restructuring, PSS = Posttraumatic Stress Symptom Scale, PSS-I = Posttraumatic Stress Symptom Scale – Interview, PTSD = posttraumatic stress disorder, RCT = randomized-controlled trial, SIT = stress inoculation training, TAU = treatment as usual, TBE = treatment by experts (for borderline personality disorder), WL = waiting list.
3.1.2. PTSD treatments provided
Psychotherapy was the only PTSD intervention evaluated in patients with personality disorders, of which prolonged exposure (PE) therapy was the intervention most frequently offered (5 studies)(Feeny, Zoellner, & Foa, 2002; Harned, Korslund, Foa, & Linehan, 2012; Harned et al., 2014; Hembree, Cahill, & Foa, 2004; Meyers et al., 2017). In three of these studies, PE was combined with dialectical behavioural therapy (DBT)(Harned et al., 2012, 2014; Meyers et al., 2017). Two other studies offered DBT in combination with other trauma-focused interventions (Bohus et al., 2013; Steil et al., 2018), while the efficacy of CBT was explored in three studies (Clarke, Rizvi, & Resick, 2008; Kredlow et al., 2017). Two studies assessed the effects of cognitive processing therapy (CPT)(Holder, Holliday, Pai, & Surís, 2017; Walter et al., 2012) and two the outcomes of narrative exposure therapy (NET)(Pabst et al., 2014; Steuwe et al., 2016). EMDR was studied by our group (Slotema et al., 2019) and interpersonal process group therapy also in a single study (Cloitre & Koenen, 2001). A combination of EMDR, PE with physical training and psycho-education was offered in one study (De Jongh et al., 2020).
The trauma-focused treatments were offered in an individual setting in the majority of the studies, while seven provided a combination of group and individual therapy (Bohus et al., 2013; Clarke et al., 2008; Harned et al., 2012; Hembree et al., 2004; Meyers et al., 2017; Steil et al., 2018; Walter et al., 2012), with one investigating group therapy. In four studies, treatments were delivered in an inpatient setting (Bohus et al., 2013; De Jongh et al., 2020; Steuwe et al., 2016; Walter et al., 2012), in one both in an in- and an outpatient setting (Pabst et al., 2014), and the other 12 studies all had outpatient settings.
The PTSD interventions comprised a mean or median of 4 up to 25 sessions and session durations ranged between 50 and 120 min, while treatment intensity varied between 300 and 7,280 minutes.
3.1.3. Populations and trauma types
The majority of studies included patients with BPD; only three studies explored the efficacy of PTSD treatments in personality disorders in general (Hembree et al., 2004; Slotema et al., 2019; Walter et al., 2012). Hembree and colleagues included 29 patients with the following personality disorders: avoidant – (28%), obsessive-compulsive – (24%), depressive – (24%), borderline – (10%), and negativistic -, schizoid -, antisocial – and narcissistic personality disorder (3% each). The population of Walter and colleagues consisted of 110 patients with paranoid – (45%), avoidant – (30%), borderline – (15%), obsessive-compulsive – (11%), passive-aggressive – (4%), depressive – (6%), dependent – (5%), antisocial – (3%), narcissistic – (2%) and schizotypal personality disorder (1%). In the study of Slotema and colleagues 47 patients with the following personality disorders participated: borderline – (47%), unspecified – (43%), and paranoid -, antisocial -, narcissistic -, avoidant – and dependent personality disorder (2% each).
In seven studies both male and female patients participated (De Jongh et al., 2020; Kredlow et al., 2017; Meyers et al., 2017; Slotema et al., 2019; Steuwe et al., 2016; Walter et al., 2012), with the other studies evaluating treatments in female patients only.
The following traumas were reported: childhood sexual abuse and other traumas in nine studies (De Jongh et al., 2020; Harned et al., 2012, 2014; Hembree et al., 2004; Kredlow et al., 2017; Slotema et al., 2019; Steuwe et al., 2016; Walter et al., 2012), childhood sexual abuse in three studies (Bohus et al., 2013; Cloitre & Koenen, 2001; Steil et al., 2018), sexual and nonsexual assault in two (Feeny et al., 2002; Pabst et al., 2014), and military sexual assault, military assault and sexual assault in one, respectively (Clarke et al., 2008; Holder et al., 2017; Meyers et al., 2017).
3.1.4. Safety of PTSD treatment
During the treatment phase, the severity of self-injurious behaviour was reduced in three studies (Bohus et al., 2013; Harned et al., 2014; Steil et al., 2018), with results in one study being similar to those in the control condition (DBT)(Harned et al., 2014). None of the patients showed an increase in any problematic behaviour, such as suicidality, self-harm, or need for hospitalization (Meyers et al., 2017; Slotema et al., 2019; Steil et al., 2018). Suicide attempts during the treatment phase were absent in three studies (Bohus et al., 2013; Slotema et al., 2019; Steil et al., 2018), but in both the studies of Harned and colleagues one patient did try to commit suicide, which was not an increase from baseline (Harned et al., 2012, 2014). No suicide attempts occurred in the DBT control group.
3.1.5. Dropout
The patients leaving the PTSD interventions prematurely are presented in Table 1. Dropout rates varied between 0% and 36%, with a mean weighted dropout of 17%.
3.2. Meta-analyses
A total of 3888 studies were considered, of which 3874 did not fulfil our criteria for meta-analysis. The reasons for exclusion are presented in Figure 1. Fourteen studies comprising a total of 430 patients were found fit for inclusion; the details of these studies are described in Table 1, part A. Of the selected studies, four were RCTs with a total of 78 patients participating in the active condition and 63 in the control condition. Another two RCTs were treated as uncontrolled trials as the data on patients with personality disorders in the control condition were lacking (Feeny et al., 2002; Holder et al., 2017). Two further RCTs were only included in the systematic review because the data were not sufficient for statistical evaluation (Clarke et al., 2008; Hembree et al., 2004). No studies regarding other interventions than psychotherapy could be included.
3.2.1. Quality of studies
The results on the methodological quality of studies included in the meta-analyses are presented in Table 2. Eleven studies used a structured clinical interview to diagnose or confirm PTSD (79%) and in nine of these the interviewers were blind (64%). In the study of Slotema et al. (2019) patients participated if they had a diagnosis of PTSD according to the DSM-IV-TR (American Psychiatric Association, 2000) and a summed score on the Posttraumatic Diagnostic Scale ≥ 18. Walter et al. (2012) included patients with current PTSD, and Steuwe et al. (2016) included patients with PTSD as defined by the DSM-IV-TR. Patients with PTSD were allocated to an intervention by randomization in six studies (43%). Two studies solely used trauma-focused self-report assessments. Fourteen studies reported the number of patients dropping out (100%) and results regarding treatment tolerability were reported in 10 (71%). Data considering posttreatment and follow-up assessments were presented in nine studies (64%), with nine conducting intention-to-treat-analyses (64%). The four RCTs included in the meta-analyses fulfilled all seven quality criteria.
Table 2.
Quality of studies exploring PTSD-focused psychotherapy in patients with personality disorders included in the meta-analyses.
| Study | Structured clinical interview for PTSD | Randomization | Blind data assessment | Drop out | Tolerability | Post-treatment and follow-up assessments included | Intention-to-treat analysis |
|---|---|---|---|---|---|---|---|
| Bohus et al., 2013 | + | + | + | + | + | + | + |
| Harned et al., 2014 | + | + | + | + | + | + | + |
| Kredlow et al., 2017 I | + | + | + | + | + | + | + |
| Kredlow et al., 2017 II | + | + | + | + | + | + | + |
| Feeny et al., 2002 | + | + | + | + | - | + | - |
| Walter et al., 2012 | - | - | - | + | - | - | - |
| Harned et al., 2012 | + | - | + | + | + | + | + |
| Pabst et al., 2014 | + | - | + | + | - | - | + |
| Steuwe et al., 2016 | - | - | + | + | + | + | + |
| Holder et al., 2017 | + | + | + | + | - | + | - |
| Meyers et al., 2017 | + | - | Self-reports | + | + | - | - |
| Slotema et al., | - | - | Self-reports | + | + | - | + |
| Steil et al., 2018 | + | - | - | + | + | + | + |
| De Jongh et al., 2020 | + | - | - | + | + | - | - |
PTSD = posttraumatic stress disorder.
3.2.2. Publication bias
The results for publication bias are presented in Table 3. The number of studies needed to change the results (i.e. the fail-safe number) of the RCTs varied between 14 and 57. For all randomized controlled, nonrandomized controlled and uncontrolled studies the fail-safe number varied between 52 and 3,279.
Table 3.
Results on the heterogeneity and publication bias for the studies included in the meta-analyses.
| Q | p | df | I2 | Fail-safe number | |
|---|---|---|---|---|---|
| PTSD RCTs | 2.56 | 0.47 | 3 | 0 | 56 |
| PTSD all studies | 47.24 | <.001 | 13 | 72.48 | 3,279 |
| Depression RCTs | 12.90 | 0.005 | 3 | 76.74 | 14 |
| Depression all studies | 22.34 | 0.004 | 8 | 64.18 | 436 |
| Anxiety RCTs | 0.79 | 0.67 | 2 | 0 | 0 |
| Anxiety all studies | 6.93 | 0.14 | 4 | 42.32 | 52 |
| Borderline symptoms RCTs | 4.15 | 0.13 | 2 | 51.82 | 6 |
| Borderline symptoms all studies | 15.73 | 0.015 | 6 | 61.86 | 142 |
| PTSD patients BPD RCTs | 2.56 | 0.47 | 3 | 0 | 56 |
| PTSD patients BPD all studies | 37.32 | <.001 | 12 | 67.85 | 2,188 |
| PTSD after 3 months RCTs | 6.11 | 0.11 | 3 | 50.91 | 57 |
| PTSD after 3 months all | 20.73 | 0.008 | 8 | 61.40 | 629 |
BPD = borderline personality disorder, PTSD = posttraumatic stress disorder, RCTs = randomized-controlled trials.
Based on the funnel plot for the meta-analysis regarding psychotherapy for the severity of PTSD, Egger’s regression intercept was 2.84 (t-value = 2.13, df = 12, p = 0.055), suggesting symmetry in the funnel plot.
Six meta-analyses could be conducted to determine the efficacy of the PTSD-focused psychotherapies for patients with comorbid personality disorders, for which purpose we evaluated the following outcome measures: change in 1) PTSD symptom severity, 2) the severity of depressive symptoms, 3) the severity of anxiety, 4) the severity of borderline symptoms, 5) the severity of PTSD symptoms in patients with BPD, and 6) PTSD symptom severity at follow-up (at least 3 months after treatment conclusion).
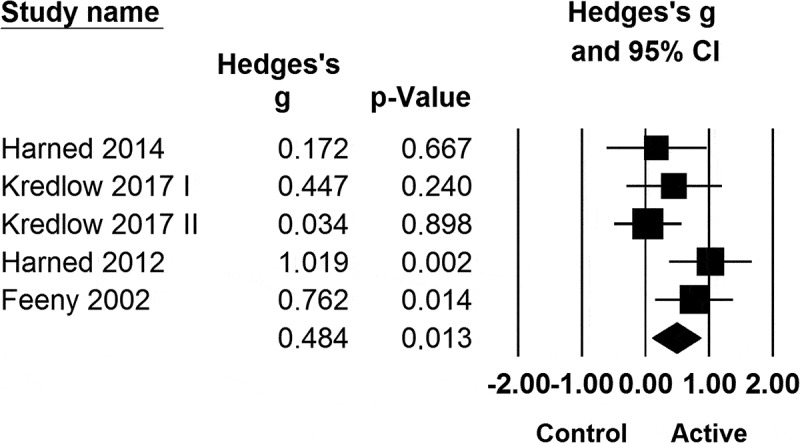
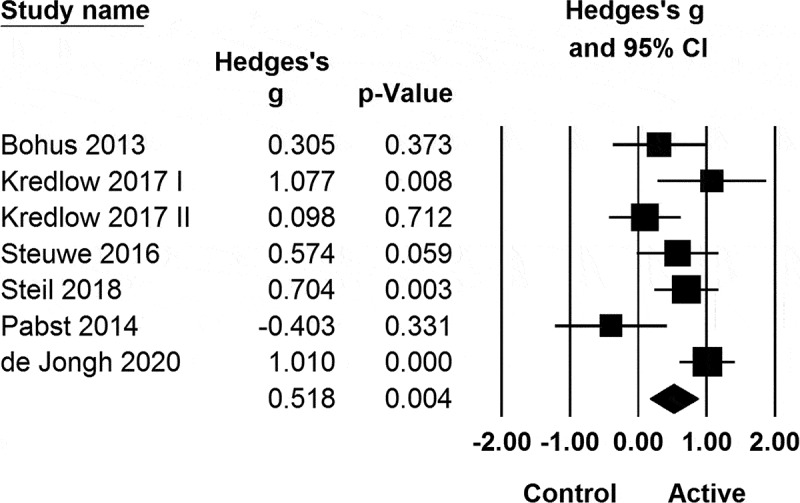
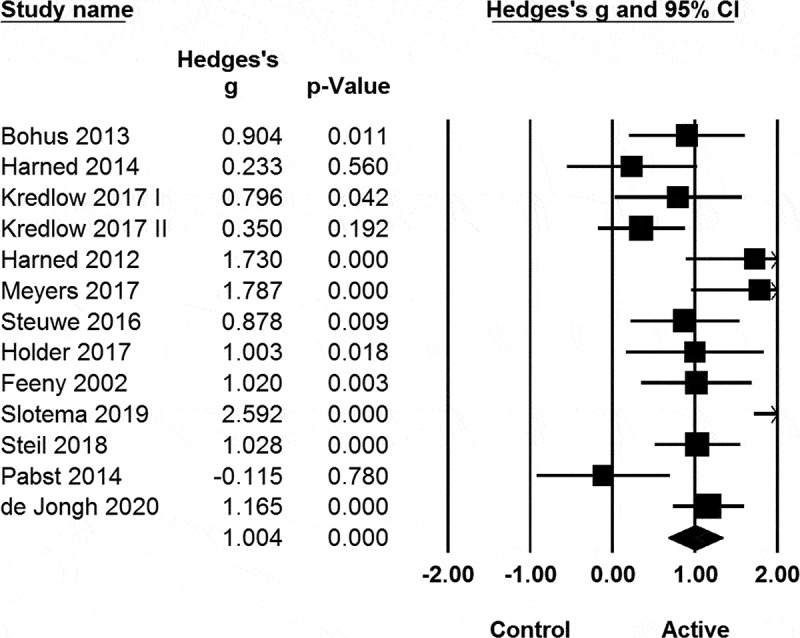
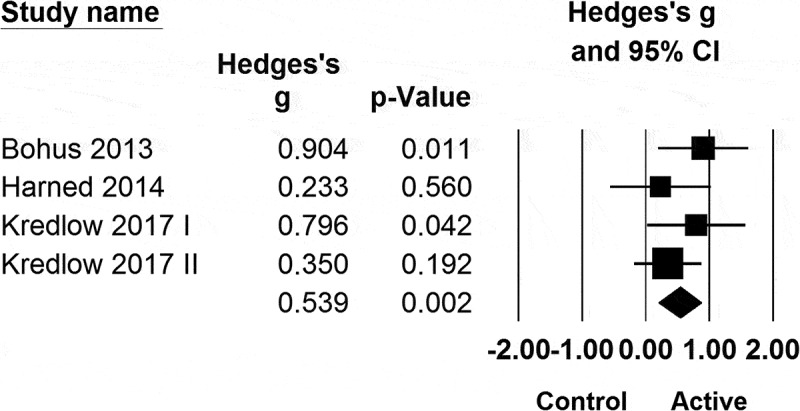
The results of the meta-analyses are presented in Table 4 and Figures 2–8. All RCTs included patients with BPD and significant SDs were found for post-treatment PTSD symptom severity (see Figure 2) and at 3-month follow-up or beyond. Looking at the randomized -, nonrandomized controlled and uncontrolled studies together, significant standardized effect sizes were found for symptom severity of PTSD, depression, anxiety, borderline, PTSD in BPD, and PTSD 3 months (or more) post-treatment. The Hedges’ gs for RCTs versus all studies were significantly lower for reductions in the symptoms of PTSD and anxiety (Q = 5.08, df = 1, p = 0.024 and Q = 5.89, df = 1, p = 0.015, respectively).
Figure 3.
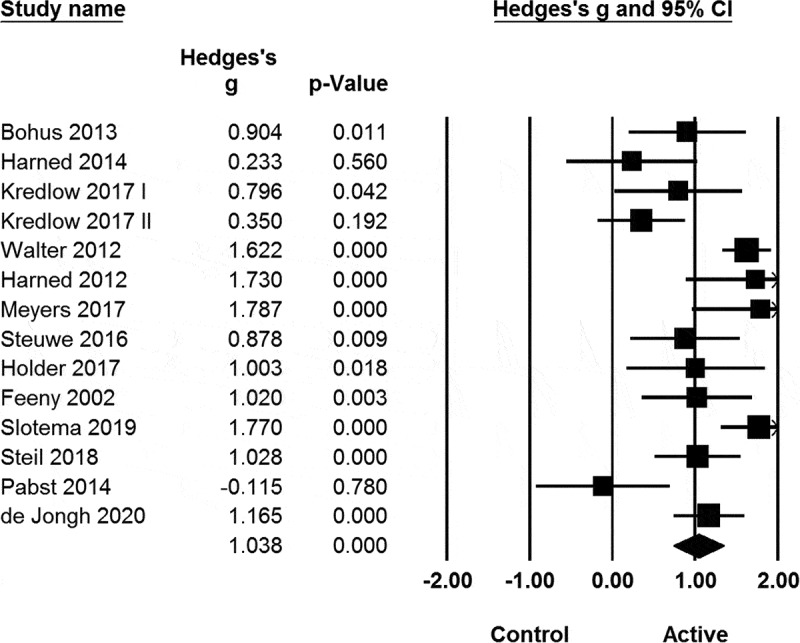
Meta-analysis of all studies exploring the effects of psychotherapy for posttraumatic stress disorder (PTSD) on the severity of PTSD in patients with personality disorders.
Figure 4.
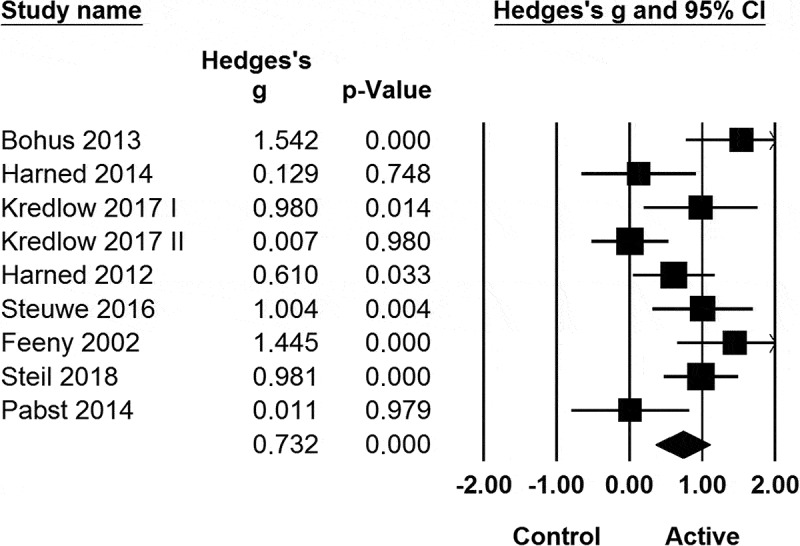
Meta-analysis of all studies exploring the efficacy of psychotherapy for posttraumatic stress disorder on the severity of depression in patients with personality disorders.
Figure 5.
Meta-analysis of all studies exploring psychotherapy for posttraumatic stress disorder on severity of anxiety in patients with personality disorders.
Figure 6.
Meta-analysis of all studies exploring psychotherapy for posttraumatic stress disorder on severity of borderline symptoms in patients with personality disorders.
Figure 7.
Meta-analysis of all studies exploring psychotherapy for posttraumatic stress disorder (PTSD) on severity of PTSD patients with borderline personality disorder.
Table 4.
Results of the meta-analyses of studies exploring PTSD-focused psychotherapy in patients with personality disorders.
| Studies n | Sample size n | Hedges’ g | Z | p | |
|---|---|---|---|---|---|
| PTSD RCTs | 4 | 141 | 0.54 | 3.17 | 0.002 |
| PTSD all studies | 14 | 430 | 1.04 | 6.75 | <.001 |
| Depression RCTs | 4 | 141 | 0.64 | 1.72 | 0.0085 |
| Depression all studies | 9 | 217 | 0.73 | 3.85 | <.001 |
| Anxiety RCTs | 3 | 108 | 0.17 | 0.89 | 0.37 |
| Anxiety all studies | 5 | 130 | 0.48 | 2.48 | 0.013 |
| Borderline symptoms RCTs | 3 | 115 | 0.43 | 1.56 | 0.12 |
| Borderline symptoms all studies | 7 | 204 | 0.52 | 2.87 | 0.004 |
| PTSD patients BPD RCTs | 4 | 141 | 0.54 | 3.17 | 0.002 |
| PTSD patients BPD all studies | 13 | 295 | 1.04 | 5.94 | <.001 |
| PTSD after 3 months RCTs | 4 | 141 | 0.82 | 3.19 | 0.001 |
| PTSD after 3 months all | 9 | 203 | 0.98 | 4.61 | <.001 |
BPD = borderline personality disorder, PTSD = posttraumatic stress disorder, RCT = randomized-controlled trial.
Figure 2.
Meta-analysis of the four randomized-controlled trials evaluating PTSD symptom severity after trauma-focused psychotherapy in patients with personality disorders.
Figure 8.
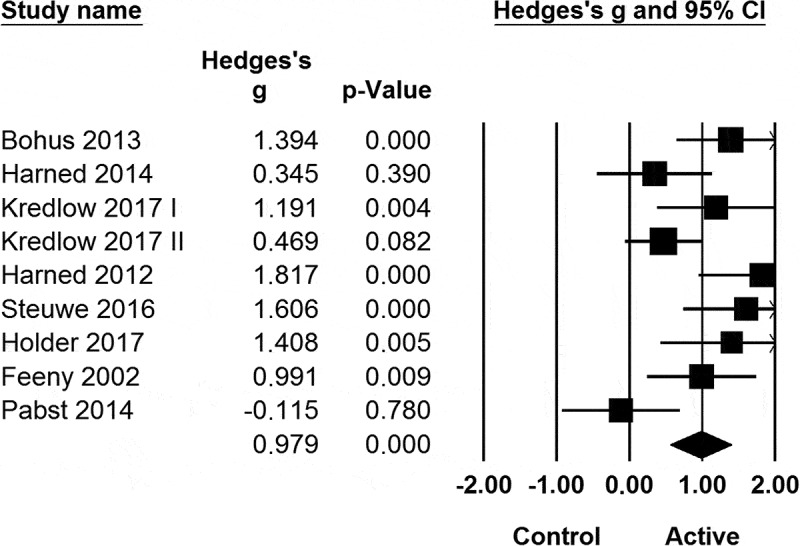
Meta-analysis of all studies exploring psychotherapy for posttraumatic stress disorder (PTSD) on severity of PTSD patients after at least three months of follow-up in patients with personality disorders.
3.2.3. Heterogeneity
Heterogeneity was found for effects on severity of PTSD (all studies), depressive symptoms (RCTs and all studies), borderline symptoms (all studies), patients with BPD (all studies) and severity of PTSD after at least 3 months of follow-up (all studies). Due to the small number of studies, it was not possible to conduct a meta-regression analysis including all parameters. As an alternative, correlations between effect sizes and parameters were computed per individual parameter. To correct for multiple testing we have used the Benjamini-Hochberg method. A total of 24 tests were performed. After correction three findings remained significant. With all studies analysed, the standardized effect sizes for PTSD symptom severity were lower for the patients with BPD compared to those with several types of personality disorders (Q = 7.70, df = 1, p = 0.006). Studies that offered targeted, stand-alone psychotherapy for PTSD rather than as an add-on treatment reached significantly higher SDs for the severity of depressive symptoms (Q = 6.94, df = 1, p = 0.008). In addition, significant differences in the standardized effect sizes for out- compared to inpatient treatment or a combination of the two were found for the severity of PTSD after at least 3 months of follow-up (Q = 11.01, df = 2, p = 0.004). No specific type of setting was found to be superior to the others.
4. Discussion
We conducted a meta-analysis and systematic review to evaluate the current evidence of the effects of PTSD treatments for patients with personality disorders on the severity of PTSD and other, comorbid symptoms, also looking at the risks presumed to be associated with trauma-focused interventions and (the mean weighted) dropout rates. Fourteen out of 17 studies included only patients with BPD. All studies found eligible for review explored psychotherapeutic interventions, with our meta-analyses showing psychotherapy for PTSD to be superior to the control conditions in the RCTs, reaching a moderate posttreatment standardized effect size of 0.54, which, at follow-up (minimum of 3 months after treatment completion) had increased to large (0.82). No significant change was observed in the severity of depression, anxiety, and borderline symptoms. Having also included the nonrandomized-controlled and uncontrolled studies, we found significant improvement for all outcomes (i.e. severity of PTSD, depression, anxiety, borderline symptoms, PTSD in patients with BPD, and PTSD symptom reductions at 3-month follow-up). With 0.48 to 1.04, standardized effect sizes were moderate to large. Our systematic review revealed there was no increase in self-injurious behaviour, suicide attempts, or hospitalizations during the PTSD interventions and the mean weighted dropout was 17%.
4.1. Moderator analyses
The results of the meta-analyses were not homogeneous with respect to the severity of PTSD (all studies), depressive symptoms (RCTs and all studies), borderline symptoms (all studies), patients with BPD (all studies) and severity of PTSD after at least 3 months of follow-up (all studies). The effect sizes for depression were higher if the PTSD treatment was offered as the primary intervention and not as an add-on to other treatments. Although heterogeneity was found for the severity of PTSD at least 3 months of follow-up, separate analyses for in-, outpatient treatment and the combination of the two did not show one setting to be better than the others. Standardized effect sizes for PTSD symptom reductions were higher in the studies including patients with various personality disorders than they were in the studies treating patients with BPD only. However, when our group compared the effects of EMDR in these two populations, we did not find any differences (Slotema et al., 2019).
To our knowledge, ours is the first systematic review focusing on the treatment of PTSD in patients with personality disorders. The significant treatment effects we found are in line with the effect sizes reported in previous meta-analyses in which no distinction was made between patients with or without comorbid personality disorders (Bisson et al., 2007; Carpenter et al., 2018; Chen et al., 2014; Ehring et al., 2014; Lewis et al., 2020). However, although in these studies an additional significant reduction in depression and anxiety symptoms was reported, our evaluation of RCTs failed to reveal comparable effects. Also, risks associated with psychotherapy for PTSD were not discussed in these earlier meta-analyses. Our mean weighted dropout rate of 17% is lower to the rate (22%) reported by Ehring et al. (2014) in their systematic review of PTSD treatments for patients having suffered childhood abuse and the rate (29%) Carpenter and colleagues recorded for CBT (2018). Furthermore, in their meta-analysis comparing psychotherapy and pharmacotherapy for PTSD, Lee et al. also reported an increase of the standardized effect size during follow-up (Lee et al., 2016).
The treatment effects we found for patients with personality disorders and PTSD are in line with the findings of studies exploring CBT, prolonged exposure, EMDR, and DBT in patients with other severe comorbid disorders such as major depression, bipolar disorder, schizophrenia, schizoaffective disorder, substance abuse, or anxiety and eating disorders (Mueser et al., 2015, 2008; Sannibale et al., 2013; Steil, Dyer, Priebe, Kleindienst, & Bohus, 2011; Van den Berg et al., 2015), while the dropout rates documented are lower than the rate we computed in the present review (Mueser et al., 2015, 2008; Van den Berg et al., 2015).
4.2. Implications for clinical practice and future research
Based on the studies evaluated, our review demonstrates that psychotherapy can effectively and safely reduce the severity of PTSD symptoms in patients with personality disorders. Given that no increases in adverse events were reported, our findings suggest there is no good reason to withhold trauma-focused treatments from these patients.
Although moderator analyses revealed better results for stand-alone psychotherapy for PTSD than for add-on trauma-focused treatments and for EMDR compared to all other PTSD interventions delivered, the number of studies and sample sizes were too low to draw any firm conclusions regarding the optimal treatment paradigm for PTSD in this population.
More RCTs with larger patient samples are needed to confirm our results. As in the majority of PTSD studies only patients with BPD participated, it would be of interest to explore the efficacy of psychotherapy in patients with other personality disorders. Also, it would be worth investigating whether these patient groups might benefit more or more quickly from psychotherapy aimed at helping them manage their personality disorder(s) if PTSD interventions were offered at an early stage after their primary diagnosis and treatment.
4.3. Limitations
The two major limitations of this meta-analysis and qualitative review are the small number of RCTs and small patient cohorts, necessitating caution when interpreting the efficacy and moderator-analysis results presented. More larger-scale RCTs of PTSD treatments in different patient groups with well-defined PTSD and comorbid conditions and control samples are urgently needed. As in the studies we reviewed the majority of patients were female and diagnosed with BPD, the results we obtained specifically concern these populations. Also, most studies did not use structural clinical interviews to diagnose PTSD. Finally, various types of psychotherapy were used for different kinds of traumas with different outcome measures being employed in small samples, again preventing firm conclusions regarding the most optimal type of and setting for PTSD treatments and patient groups most likely to benefit from intervention, making more research into the efficacy of PTSD treatments in patients with personality disorders indispensable.
4.4. Conclusions
A broad search of the literature revealed that psychotherapy was the only intervention for PTSD having been investigated in patients with personality disorders. With significant moderate to high standardized effect sizes and improvements having been maintained at least 3-months post-treatment, the meta-analyses of the four RCTs identified showed that patients with BPD had indeed benefitted from trauma-focused psychotherapy. Analyses of all studies showed similar effect sizes for reductions in PTSD, depression, anxiety, and borderline symptoms, PTSD severity in patients with BPD, with PTSD improvements also being maintained at follow-up (3 months or longer). Although further controlled research is warranted, based on these results, including the findings that the risks associated with the PTSD interventions examined were low and the mean-weighted dropout rate was 17%, we suggest that patients with comorbid personality disorders also profit from and should accordingly be offered psychological treatment for their PTSD.
Funding Statement
No funding was obtained for this study.
Author contribution
C.W. Slotema and I.H.A. Franken designed the study. C.W. Slotema and B. Wilhelmus conducted the literature search and data extraction. C.W. Slotema performed the statistical analyses. L.R. Arends assisted with the coding of studies and analyses. C.W. Slotema wrote the first draft of the manuscript and all authors contributed to and have approved the final manuscript.
Disclosure statement
The research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Albach, F., & Everaerd, W. (1992). Posttraumatic stress symptoms in victims of childhood incest. Psychotherapy and Psychosomatics, 57(4), 143–15. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . (2000). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Amir, M., Kaplan, Z., Efroni, R., & Kotler, M. (1999). Suicide risk and coping styles in posttraumatic stress disorder patients. Psychotherapy and Psychosomatics, 68(2), 76–81. [DOI] [PubMed] [Google Scholar]
- Atwoli, L., Stein, D. J., Koenen, K. C., & McLaughlin, K. A. (2015). Epidemiology of posttraumatic stress disorder: Prevalence, correlates and consequences. Current Opinion in Psychiatry, 28(4), 307–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamini, Y., & Hochberg, Y. (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of Royal Statistical Society, 57, 289–300. [Google Scholar]
- Bisson, J. I., Ehlers, A., Matthews, R., Pilling, S., Richards, D., & Turner, S. (2007). Psychological treatments for chronic post-traumatic stress disorder. British Journal of Psychiatry, 190(2), 97–104. [DOI] [PubMed] [Google Scholar]
- Bohus, M., Dyer, A. S., Priebe, K., Krüger, A., Kleindienst, N., Schmahl, C., … Steil, R. (2013). Dialectical behaviour therapy for post-traumatic stress disorder after childhood sexual abuse in patients with and without borderline personality disorder: A randomised controlled trial. Psychotherapy and Psychosomatics, 82(4), 221–233. [DOI] [PubMed] [Google Scholar]
- Carpenter, J. K., Andrews, L. A., Witcraft, S. M., Powers, M. B., Smits, J. A. J., & Hofmann, S. G. (2018). Cognitive behavioral therapy for anxiety and related disorders: A meta-analysis of randomized placebo-controlled trials. Depression and Anxiety, 35(6), 502–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, Y.-R., Hung, K.-W., Tsai, J.-C., Chu, H., Chung, M.-H., Chen, S.-R., … Chou, K. R. (2014). Efficacy of eye-movement desensitization and reprocessing for patients with posttraumatic-stress disorder: A meta-analysis of randomized controlled trials. PLoS ONE, 9(8), e103676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke, S. B., Rizvi, S. L., & Resick, P. A. (2008). Borderline personality characteristics and treatment outcome in cognitive-behavioral treatments for PTSD in female rape victims. Behavioral Therapy, 39(1), 72–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre, M., & Koenen, K. C. (2001). The impact of borderline personality disorder on process group outcome among women with posttraumatic stress disorder related to childhood abuse. International Journal of Group Psychotherapy, 51(3), 379–398. [DOI] [PubMed] [Google Scholar]
- De Jongh, A., Groenland, G. N., Sanches, S., Bongaerts, H., Voorendonk, E. M., & van Minnen, A. (2020). The impact of brief intensive trauma-focused treatment for PTSD on symptoms of borderline personality disorder. European Journal of Psychotraumatology, 11(1), 1721142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DerSimonian, R., & Laird, N. (1986). Meta-analysis in clinical trials. Controlled Clinical Trials, 7(3), 177–188. [DOI] [PubMed] [Google Scholar]
- Egger, M., Smith, G. D., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315(7109), 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehring, T., Welboren, R., Morina, N., Wicherts, J. M., Freitag, J., & Emmelkamp, P. M. G. (2014). Meta-analysis of psychological treatments for posttraumatic stress disorder in adult survivors of childhood abuse. Clinical Psychology Review, 34(8), 645–657. [DOI] [PubMed] [Google Scholar]
- Feeny, N. C., Zoellner, L. A., & Foa, E. B. (2002). Treatment outcome for chronic PTSD among female assault victims with borderline personality characteristics: A preliminary examination. Journal of Personality Disorders, 16(1), 30–40. [DOI] [PubMed] [Google Scholar]
- Harned, M. S., Korslund, K. E., Foa, E. B., & Linehan, M. M. (2012). Treating PTSD in suicidal and self-injuring women with borderline personality disorder: Development and preliminary evaluation of a dialectical behavior therapy prolonged exposure protocol. Behaviour Research and Therapy, 50(6), 381–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harned, M. S., Korslund, K. E., & Linehan, M. M. (2014). A pilot randomized controlled trial of dialectical behavior therapy with and without the dialectical behavior therapy prolonged exposure protocol for suicidal and self-injuring women with borderline personality disorder and PTSD. Behaviour Research and Therapy, 55, 7–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hembree, E. A., Cahill, S. P., & Foa, E. B. (2004). Impact of personality disorders on treatment outcome for female assault survivors with chronic posttraumatic stress disorder. Journal of Personality Disorders, 18(1), 117–127. [DOI] [PubMed] [Google Scholar]
- Higgins, J. P. T., & Thompson, S. G. (2002). Quantifying heterogeneity in meta-analysis. Statistics in Medicine, 21(11), 1539–1558. [DOI] [PubMed] [Google Scholar]
- Holder, N., Holliday, R., Pai, A., & Surís, A. (2017). Role of borderline personality disorder in the treatment of military sexual trauma-related posttraumatic stress disorder with cognitive processing therapy. Behavioural Medicine, 43(3), 184–190. [DOI] [PubMed] [Google Scholar]
- Khan, A. M., Dar, S., Ahmed, R., Bachu, R., Adnan, M., & Kotapati, V. P. (2018). Cognitive behavioral therapy versus eye movement desensitization and reprocessing in patients with post-traumatic stress disorder: Systematic review and meta-analysis of randomized clinical trials. Cureus, 10, e3250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kredlow, M. A., Szuhany, K. L., Lo, S., Xie, H., Gottlieb, J. D., Rosenberg, S. D., & Mueser, K. T. (2017). Cognitive behavioral therapy for posttraumatic stress disorder in individuals with severe mental illness and borderline personality disorder. Psychiatry Research, 249, 86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, D. J., Schnitzlein, C. W., Wolf, J. P., Vythilingam, M., Rasmusson, A. M., & Hoge, C. W. (2016). Psychotherapy versus pharmacotherapy for posttraumatic stress disorder: Systematic review and meta-analyses to determine first-line treatments. Depression and Anxiety, 33(9), 792–806. [DOI] [PubMed] [Google Scholar]
- Lewis, C., Roberts, N. P., Andrew, M., Starling, E., & Bisson, J. I. (2020). Psychological therapies for post-traumatic stress disorder in adults: Systematic review and meta-analysis. European Journal of Psychotraumatology, 11(1), 1729633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyers, L., Voller, E. K., McCallum, E. B., Thuras, P., Shallcross, S., Velasquez, T., & Meis, L. (2017). Treating veterans with PTSD and borderline personality symptoms in a 12-week intensive outpatient setting: Findings from a pilot program. Journal of Traumatic Stress, 30(2), 178–181. [DOI] [PubMed] [Google Scholar]
- Mueser, K. T., Gottlieb, J. D., Xie, H., Lu, W., Yanos, P. T., Rosenberg, S. D., … McHugo, G. J. (2015). Evaluation of cognitive restructuring for post-traumatic stress disorder in people with severe mental illness. British Journal of Psychiatry, 206(6), 501–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueser, K. T., Rosenberg, S. D., Xie, H., Jankowski, M. K., Bolton, E. E., Lu, W., … Wolfe, R. (2008). A randomized controlled trial of cognitive-behavioral treatment for posttraumatic stress disorder in severe mental illness. Journal of Consulting and Clinical Psychology, 76(2), 259–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pabst, A., Schauer, M., Bernhardt, K., Ruf-Leuschner, M., Goder, R., Elbert, T., & Seeck-Hirschner, M. (2014). Evaluation of narrative exposure therapy (NET) for borderline personality disorder with comorbid posttraumatic stress disorder. Clinical Neuropsychiatry, 11, 108–117. [Google Scholar]
- Pagura, J., Stein, M. B., Bolton, J. M., Cox, B. J., Grant, B., & Sareen, J. (2010). Comorbidity of borderline personality disorder and posttraumatic stress disorder in the U.S. population. Journal of Psychiatric Research, 44(16), 1190–1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal, R. (1997). The file drawer problem and tolerance for null results. Psychological Bulletin, 86(3), 638–641. [Google Scholar]
- Samuals, J., Eaton, W. W., Bienvenu, O. J., Brown, C. H., Costa, P. T., & Nestadt, G. (2002). Prevalence and correlates of personality disorders in a community sample. British Journal of Psychiatry, 180(6), 536–542. [DOI] [PubMed] [Google Scholar]
- Sannibale, C., Teesson, M., Creamer, M., Sitharthan, T., Bryant, R. A., Sutherland, K., … Peek-O’Leary, M. (2013). Randomized controlled trial of cognitive behaviour therapy for comorbid post-traumatic stress disorder and alcohol use disorders. Addiction, 108(8), 1397–1410. [DOI] [PubMed] [Google Scholar]
- Slotema, C. W., Blom, J. D., Niemantsverdriet, M. B. A., Deen, M., & Sommer, I. E. C. (2018). Comorbid diagnosis of psychotic disorders in borderline personality disorder: Prevalence and influence on outcome. Frontiers in Psychiatry, 9, 84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slotema, C. W., van den Berg, D. P. G., Driessen, A., Wilhelmus, B., & Franken, I. H. A. (2019). Feasibility of EMDR for posttraumatic stress disorder in patients with personality disorders: A pilot study. European Journal of Psychotraumatology, 10(1), 1614822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steil, R., Dittmann, C., Müller-Engelmann, M., Dyer, A., Maasch, A. M., & Priebe, K. (2018). Dialectical behaviour therapy for posttraumatic stress disorder related to childhood sexual abuse: A pilot study in an outpatient treatment setting. European Journal of Psychotraumatology, 9(1), 1423832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steil, R., Dyer, A., Priebe, K., Kleindienst, N., & Bohus, M. (2011). Dialectical behavior therapy for posttraumatic stress disorder related to childhood sexual abuse: A pilot study of an intensive residential treatment program. Journal of Traumatic Stress, 24(1), 102–106. [DOI] [PubMed] [Google Scholar]
- Steuwe, C., Rullkötter, N., Ertl, V., Berg, M., Neuner, F., Beblo, T., & Driessen, M. (2016). Effectiveness and feasilibility of narrative exposure therapy (NET) in patients with borderline personality disorder and posttraumatic stress disorder – A pilot study. BMC Psychiatry, 16(1), 254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ursano, R. J., Bell, C., Spencer, E., Friedman, M., Norwood, A., Pfeifferbaum, B., … Benedek, D. M. (2004). Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. American Journal of Psychiatry, 161(11 Suppl), 3–33. [PubMed] [Google Scholar]
- Van den Berg, D. P., de Bont, P. A., van der Vleugel, B. M., de Roos, C., de Jongh, A., van Minnen, A., & van der Gaag, M. (2015). Prolonged exposure vs eye movement desensitization and reprocessing vs waiting list for posttraumatic stress disorder in patients with a psychotic disorder: A randomized clinical trial. JAMA Psychiatry, 72(3), 259–267. [DOI] [PubMed] [Google Scholar]
- Walter, K. H., Bolte, T. A., Owens, G. P., & Chard, K. M. (2012). The impact of personality disorders on treatment outcome for veterans in posttraumatic stress disorder residential treatment program. Cognitive Therapy and Research, 36(5), 576–584. [Google Scholar]
- Zanarini, M. C., Frankenburg, F. R., Dubo, E. D., Sickel, A. E., Trikha, A., Levin, A., & Reynolds, V. (1998). Axis I comorbidity of borderline personality disorder. American Journal of Psychiatry, 155(12), 1733–1739. [DOI] [PubMed] [Google Scholar]
- Zanarini, M. C., Gunderson, J. G., Marino, M. F., Schwartz, E. O., & Frankenburg, F. R. (1989). Childhood experiences of borderline patients. Comprehensive Psychiatry, 30(1), 18–25. [DOI] [PubMed] [Google Scholar]


