ABSTRACT
Pandemic SARS-CoV-2 has caused unprecedented mortalities. Vaccine is in urgent need to stop the pandemic. Despite great progresses on SARS-CoV-2 vaccine development, the efficacy of the vaccines remains to be determined. Deciphering the interactions of the viral epitopes with the elicited neutralizing antibodies in convalescent population inspires the vaccine development. In this study, we devised a peptide array composed of 20-mer overlapped peptides of spike (S), membrane (M) and envelope (E) proteins, and performed a screening with 120 COVID-19 convalescent sera and 24 non-COVID-19 sera. We identified five SARS-CoV-2-specific dominant epitopes that reacted with above 40% COVID-19 convalescent sera. Of note, two peptides non-specifically interacted with most of the non-COVID-19 sera. Neutralization assay indicated that only five sera completely blocked viral infection at the dilution of 1:200. By using a peptide-compete neutralizing assay, we found that three dominant epitopes partially competed the neutralization activity of several convalescent sera, suggesting antibodies elicited by these epitopes played an important role in neutralizing viral infection. The epitopes we identified in this study may serve as vaccine candidates to elicit neutralizing antibodies in most vaccinated people or specific antigens for SARS-CoV-2 diagnosis.
KEYWORDS: SARS-CoV-2, COVID-19, epitope, neutralizing antibody, vaccine, diagnosis
Introduction
Since the outbreak of COVID-19 in Wuhan China in December 2019, it was endemic to all over the China within less than 1 month and now become pandemic in over 200 countries. The infected cases surged to over 10 million by the end of June 2020, with over 500,000 mortalities (https://www.who.int/emergencies/diseases/novel-coronavirus-2019). COVID-19 is caused by infection with a novel coronavirus SARS-CoV-2 [1–3]. Efficacy of several antiviral agents such as remdesivir and chloroquine remains uncertainty [4–6]. Vaccine development is in urgent need to stop the pandemic. Coronaviruses contain three structural proteins on the surface of virus membrane envelope: the spike (S), membrane (M) and envelop (E) proteins. S protrudes from the virion surface to form a spike and interacts with host receptor to mediate virus entry [7]. The spike protein (S) of SARS-CoV-2 interacts with host receptor ACE2 [2]. SARS-CoV-2 vaccine candidates include viral vector expressing SARS-CoV-2 spike protein (S) [8], the receptor-binding domain (RBD) [9] and inactivated virion [10]. With the start of the first clinical trial of a recombinant adenovirus type-5 (Ad5) vectored COVID-19 vaccine [8], there would be many other vaccine trials. Despite great progresses on SARS-CoV-2 vaccine development, there are still critical questions remain to be answered, such as which kind of antigens (epitopes) elicit robust neutralizing antibodies in most people; in the convalescent COVID-19 patients contain neutralizing antibodies, which viral epitopes are recognized by the neutralizing antibodies. Answers to these questions may guide the development of effective vaccines. In this study, we collected the sera of a convalescent COVID-19 cohort. By using a peptide array composed of 20-mer overlapped peptides of S, M and E, we identified several dominant SARS-CoV-2 specific linear epitopes that reacted with the convalescent sera. By using peptide-compete neutralizing assay, we found that some of these dominant epitopes partially competed the neutralization activity of several convalescent sera. These data provide information for developing novel vaccine candidates and antigens for specific antibody diagnosis.
Material and methods
Ethics statements
This study was approved by the ethics committee of Shanghai Public Health Clinical Center, and the procedures were carried out in accordance with approved guidelines. Informed consent was obtained from the subjects. Collection of the COVID-19 convalescent serum samples was approved under the study number YJ-2020-S077-02. The serum samples of patients with symptoms of acute respiratory infections were collected under the study number YJ-2018-S045-02.
Peptide array
According to a sequence of SARS-CoV-2 (Accession number, MT121215), 20-mer overlapped peptides covering the entire spike (S) region, the ectodomain of membrane (M), the loops between the TMs and representative regions of endomains of M and envelope (E) were synthesized (see Supplementary table 1) by GL Biochem (Shanghai, China) and purified by HPLC. Peptide array was manufactured by Suzhou Epitope (Suzhou, China). Peptides were printed onto activated integrated poly (dimethysiloxane) membrane (iPDMS) as described [11,12]. Briefly, synthesized peptides were dissolved in 30% acetonitrile solution (v/v) at a concentration of 1 mg/ml and then diluted to 0.2 mg/ml in printing buffer (0.3M PB, 0.2% glycerin, 0.01% Triton, 1.5% Mannitol). The iPDMS membranes were activated with a mixture of 0.1 M EDC and 0.1 M NHS for 30 min and rinsed with Mili-Q water before printing. The peptide array was prepared by printer SmartArrayer 48 with approximately 0.6 nl for each dot.
Serum screening
Sera were diluted (1:200) and incubated with peptide array. After wash, the peptide arrays were incubated with Horseradish peroxidase (HRP)-conjugated goat anti-human IgG. Dots were visualized by Super Signal Femto Maximum Sensitivity Substrate for Chemiluminescence (Thermo Fischer) and pictures were captured by a cool CCD. The chemiluminescence intensity of each dot was converted to signal-to-noise ratio (SNR) by subtracting the background intensity averaged from the intensity from blank dots. SNR equal or above 2 is considered as positive.
Cells
Vero E6 cells were maintained in Dulbecco’s modified eagle medium (DMEM)(Hyclone) containing 10% FBS (BI) supplemented with 1% penicillin, and streptomycin (Hyclone).
Virus and neutralization assay
SARV-CoV-2 virus experiment was carried out in the biosafety level 3 (BSL-3) laboratory in the Shanghai Medical College, Fudan University. SARV-CoV-2 virus strain nCoV-SH01 was isolated from a throat swab sample on Vero E6 cells [13], propagated and titrated on Vero E6 cells by a plague assay. For neutralization assay, 5 × 104 Vero E6 cells were seeded onto 96 well plates. Sera were diluted 1:100 in DMEM supplemented with 2% FBS, incubated with 100 PFU of SARV-CoV-2 virus at 37°C for 1 h, and then the mixture was added to equal volume of cell medium (the final dilution of serum is 1:200). After infection for 2 h, cells were washed once with DPBS and added with fresh media. For peptide competing experiment, sera were diluted 1:100 in DMEM supplemented with 2% FBS, incubated with 100 PFU of SARV-CoV-2 virus and indicated peptides at a concentration of 0.5 mg/ml at 37°C for 1 h, and then the mixture was added to equal volume of cell medium (the final dilution of serum is 1:200 and the final concentration of peptide is 0.25 mg/ml).
Quantitative real-time PCR
Supernatants from infected cells were mixed with Trizol LS (Invitrogen). RNAs were extracted by phenol/chloroform and precipitated by isopropanol. After wash with 70% ethanol, RNAs were dissolved in nuclease-free water and quantified by a Taqman-based real-time PCR with One Step PrimeScript RT–PCR kit (Takara) according to the manufacturers’ protocol with 400 nM of each primer (sense primer: GAA AAT AGG ACC TGA GCG CAC C, anti-sense primer: TGA CAA TAC AGA TCA TGG TTG CTT TGT) and 200 nM of probe (FAM- TAG ACG TGC CAC ATG CTT TTC CAC TGC TTC AGA C -BHQ1). The relative RNA levels were calculated by 2-ΔCT method [14].
COVID-19 screening
We selected throat swab samples of patients with symptoms of acute respiratory infections that were collected before the COVID-19 outbreak and extracted the nucleic acid and detected pathogens by Taqmen-based real-time PCR (see Supplementary table 3). COVID-19 diagnosis was performed by Quantitative real-time PCR as described above.
Total anti-SARS-CoV-2 S antibody titering
Total anti-SARS-CoV-2 S antibody levels in the sera were determined by a chemiluminescence microparticle immunoassay (CMIA) kit (2019-nCoV Ab, innoDx), in which the RBD of SARS-CoV-2 spike protein serves as an antigen. The sera were diluted 1:10 with PBS and loaded into an automatic platform (Caris200, innoDx) according to the manufacturer’s guidelines and the outputs (arbitrary chemiluminescence read, SO/CO and positive or negative conclusion) were recoded.
Data processing
MegAlign (DNAstar) was used for protein sequence alignment analysis. Transmembrane helices prediction was done by TMHMM program (http://www.cbs.dtu.dk/services/TMHMM-2.0/). Structure data of open state of S was retrieved (PDB, 6vyb) and visualized by UCSF Chimera.
Results
Identification of dominant linear B-cell epitopes of COVID-19 by a peptide array
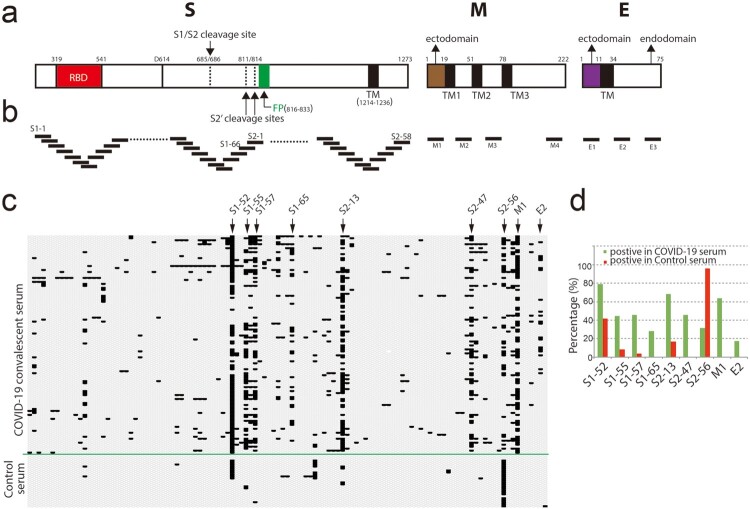
To map the dominant linear B-cell epitopes recognized by most COVID-19 patients, we designed a 20-mer overlapped peptide array encompassing the entire spike (S), the ectodomain of membrane (M), the loops between the transmembrane helices (TMs) and representative regions of endomains of M and envelope (E) proteins (Figure 1a and b) (see Supplementary table 1). We used the peptide array to perform a screening with convalescent sera from 120 COVID-19 patients and 24 sera collected from patients with symptoms of acute respiratory infections but with negative diagnosis of COVID-19 (see Supplementary table 3). The sera were diluted 1:200 and incubated with the peptide array, followed by incubated with HRP-conjugated anti-human IgG. Peptides reacting with the sera were visualized by chemiluminescent reagents. Of the 120 COVID-19 convalescent sera, 2 sera didn’t react with any peptide; 4 sera only reacted with one peptide in the peptide array. Peptides S1-52, S1-55, S1-57, S2-13, S2-47, M1 reacted with more than 40% COVID-19 sera (Figure 1c and d). Of note, S1-52 and S2-56 reacted with more than 40% COVID-19-negative control sera, indicating non-specific reaction (Figure 1c and d). We also detected about 17% serum reacted with a peptide (E2) in the endodomain of E whereas no reaction with the peptide in the ectodomain (E1) (Figure 1c and d). The topology of E protein remains controversial. Evidences indicate the N-terminal part is the ectodomain (Figure 1a) [15,16]. If the interaction of E endodomain with antibodies is due to the real topologically exposure remains to be clarified.
Figure 1.
Screening convalescent serum of COVID-19 by peptide array. (a) Schematic of SARS-CoV-2 virion structural proteins: spike (S), membrane (M) and envelope (E) proteins. In the diagram of S, the receptor-binding domain (RBD) is in red. Fusion peptide (FP) is in green. Black boxes indicate transmembrane helices (TM). Arrows indicate S1/S2 cleavage site and alternative S2′ cleavages sites, respectively. In the diagrams of M and E, the endodomians and ectodomains are indicated. The numbers above the diagrams indicate the positions (aa) of each domain. (b) Design of peptide array. 20-mer overlapped peptides covering the entire S, the ectodomain of M, the loops between the TMs and representative regions of endomains of M and E were synthesized and doted. (c and d) Convalescent sera from COVID-19 patients and control sera from non-COVID-19 patients (control serum) were diluted (1:200) and incubated with peptide array, followed by incubated with HRP-conjugated anti-human IgG. Peptide array was visualized by chemiluminescent reagents, scanned and quantified. The peptides with signal to noise above 2 were counted as positive (black bar). The positive peptides for each patient were plotted. Arrows indicate representative peptides. (d) The positive percentage of the indicated peptides.
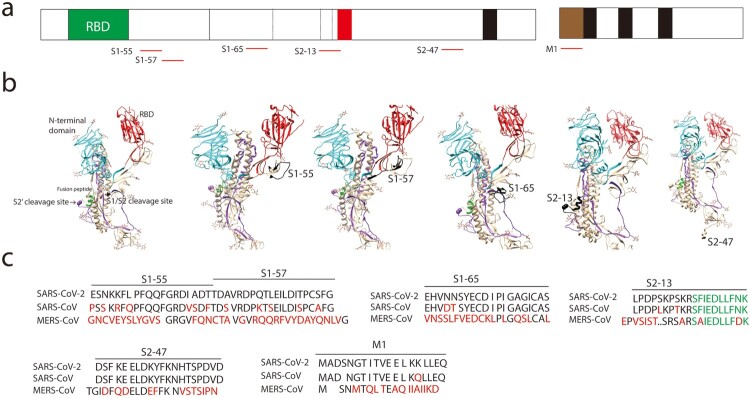
The peptides S1-52, S1-55, S1-57, S2-13, S2-47, M1 that reacted with more than 40% COVID-19 sera represented as dominant linear B-cell epitopes. We located these epitopes in a crystal structure of S in open sate (PBD, 6vyb) (Figure 2a and b). The peptides S1-52 and S1-55 were near the receptor-binding domain (RBD) (Figure 2a and b). The peptide S2-13 contained the alternative S2′ cleavages sites and fusion peptide (FP) (Figure 2a and b). Most of the peptide S2-47 is not available in the crystal structure (Figure 2a and b). Peptide S2-47 is conserved in SARS-CoV-2 and SARS-CoV whereas other peptide varied in SARS-CoV-2 and SARS-CoV (Figure 2c).
Figure 2.
Identification of dominant B-cell linear epitopes of SARS-CoV-2 virus particle. (a) Schematic of spike (S), membrane (M) and the dominant B-cell linear epitopes (red lines). (b) Locations of the dominant B-cell linear epitopes in the S structure. The S structure (open sate; PBD, 6vyb), N-terminal domain (cyan), RBD (red), fusion peptide (green). The B-cell linear epitopes are in black. Only part of the S2-47 is visible in the structure. (c) Alignment of the dominant B-cell linear epitopes. Different amino acids are in red. Fusion peptide in S2-13 is in green.
Less B-cell linear epitopes on receptor-binding domain (RBD) of spike protein (S)
Receptor-binding domain (RBD) of coronaviruses spike proteins interacts with host receptor to mediate virus entry and some antibodies against RBD potently neutralize viral infection [7]. We examined the reactions of the RBD peptides with the sera (Figure 3a). Except for S1-52, almost all the RBD peptides reacted with less than 10% sera, with peptides such as S1-31, S1-32, S1-34 and S1-35 that didn’t react with any serum (Figure 3b). Although the peptide S1-52 interacted with most sera, it also non-specifically interacted with control sera (Figure 3c). A poor-interaction peptide S1-31 was partially masked by the high-reaction peptide S1-52 in the crystal structures (Figure 3c), suggesting the poor reaction of this peptide was probably due to its poor accessibility. In contrast, the peptide S1-32 and the ACE-2 interacting interface (Figure 3a, in red) have good accessibility (Figure 3c) but still exhibited poor reactions (Figure 3b), suggesting poor reactions of peptides in RBD in general.
Figure 3.
Less B-cell linear epitopes on Receptor-binding domain (RBD) of Spike protein (S). (a) Amino acid sequence of RBD. Black bars indicate the corresponding peptides. The ACE-2 interacting interface was in red. (b) Reaction of COVID-19 convalescent sera with the peptides in RBD. The peptides with signal to noise above 2 were counted as positive (black bar). (c) Representative peptide (in black) in the structure of RBD (PBD, 6vyb).
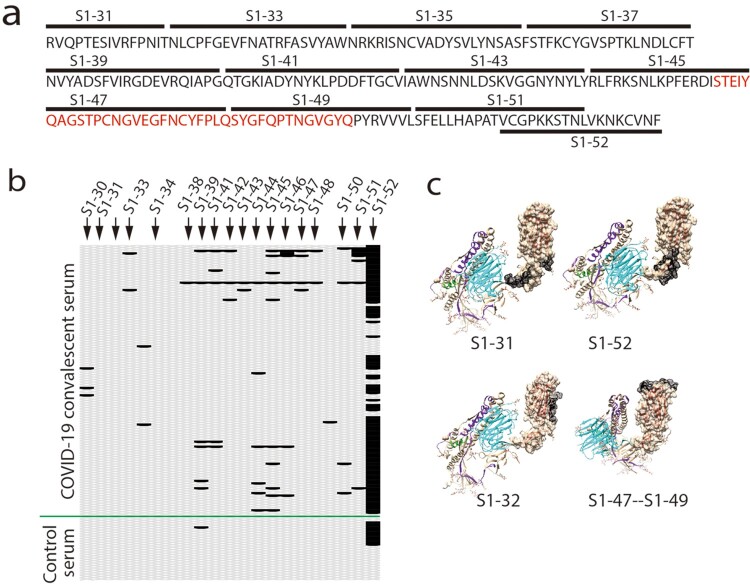
Neutralizing SARS-CoV-2 infection by COVID-19 convalescent serum
To explore the functional relevance of the identified B-cell linear epitopes and their elicited antibodies with the neutralizing activity, we first assessed the activities of the sera for the neutralization of SARS-CoV-2 virus infection. COVID-19 convalescent sera were diluted at 1:200 and incubated with 100 PFU (plague-forming unit) of virus. The neutralizing activity was assessed by reduction of viral infection-induced cytopathic effect (CPE) and quantification of viral RNA levels in the supernatants of the infected cells (Figure 4a). We used a SARS-CoV-2 strain nCoV-SH01 that we isolated from the throat swab sample of a COVID-19 patient [13]. Virus infection induces typical syncytial cytopathic effects on Vero E6 cells (see Supplementary Figure 1). Some COVID-19 convalescent sera could partially reduce (CPE+, CPE++) the CPE or completely blocked the appearance of CPE (CPE-) (see Supplementary Figure 1; Supplementary table 2). Of the 120 COVID-19 convalescent sera tested, at the dilution of 1:200, five sera completely blocked the appearance of CPE at 3 days post infection. And seven sera partially reduced the CPE or completely blocked the appearance of CPE in one of the duplicated wells (see Supplementary table 2). We also quantified the viral RNA levels in the supernatants of the infected cells at 3 days post infection with some representative samples. Sera P13, P18, P68, P98 and P107 that completely blocked the appearance of CPE also dramatically reduced the viral RNA levels (Figure 4b).
Figure 4.
Neutralizing SARS-CoV-2 infection by COVID-19 convalescent serum. (a) Schematic of experiment design. COVID-19 convalescent sera were diluted and incubated with SARS-CoV-2 before added to the media. At 48 h or 72 h post infection (p.i), the cytopathic effect (CPE) of the infected cells was examined. The viral RNAs in the supernatants were quantified by real-time PCR (q-PCR). (b) Quantification of the viral RNA levels in the supernatants from representative wells. Relative RNA levels to the mock-treated wells were plotted (n = 2). (c) Total anti-S antibody in the control sera and convalescent sera was examined by a chemiluminescence microparticle immunoassays (CMIA) assay and the reads were plotted. The sera with fully neutralizing activity were indicated in red.
As only five sera completely neutralized viral infection at a dilution of 1:200, we then determined the levels of anti-S antibody in the sera by a chemiluminescence method by using the RBD of SARS-CoV-2 spike protein as an antigen in the assay. As expected, we could not detect anti-S antibodies in the control sera (Figure 4c). In contrast, except for 2 sera (P89, P93), we detected variable but substantial anti-S antibodies in the COVID-19 convalescent sera (Figure 4c) (see Supplementary table 3). Sera with fully neutralizing activity had variable levels of total anti-S antibodies (Figure 4c, red). Sera such as P81, P99 had high levels of total anti-S antibodies but did not exert neutralizing activity (Figure 4b and c).
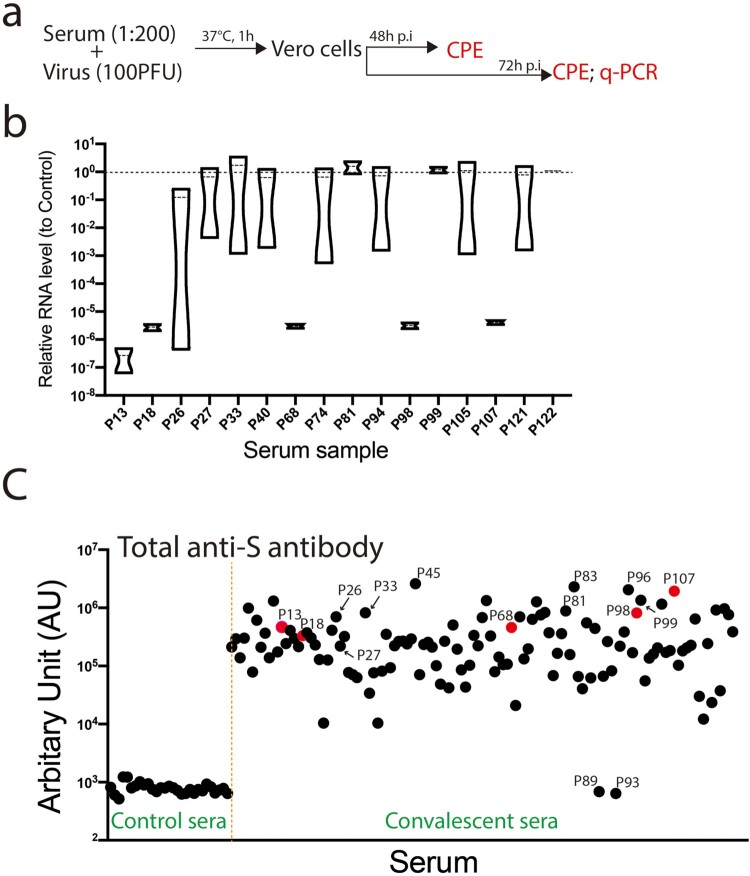
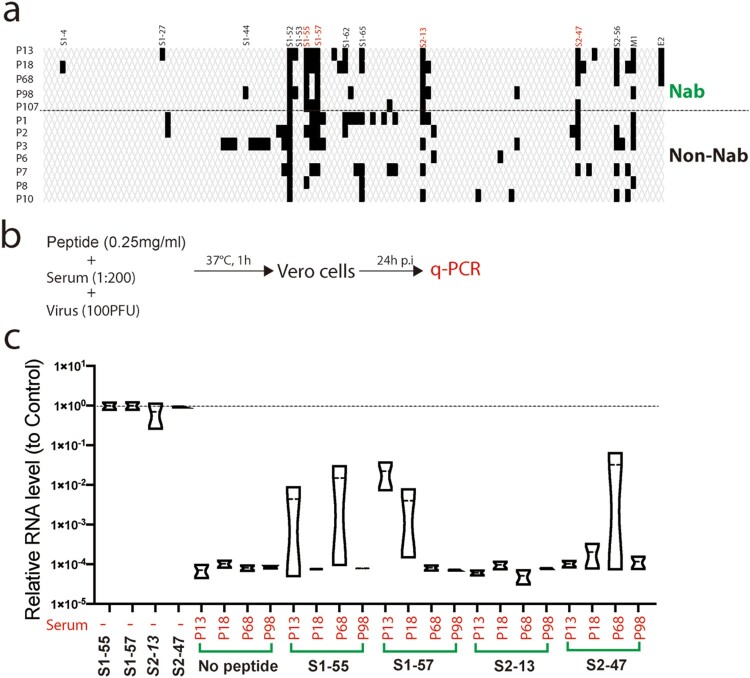
Competing the neutralizing activity of convalescent serum with dominant B-cell linear epitopes
Then we compared the peptide array reaction patterns of the neutralizing sera (Nab) with the patterns of several non-neutralizing sera (Non-Nab). All the Nabs reacted with the dominant epitopes S1-55, S1-57 and S2-13. In contrast, only part of the Non-nabs reacted with these epitopes (Figure 5a). Next, we evaluated if the antibodies against these epitopes play a role in activity of neutralizing viral infection. We performed a neutralizing experiment by using the peptide S1-55, S1-57, S2-13 and S2-47 compete the neutralizing activity of four neutralizing sera (Figure 5b). The peptides were added at a final concentration of to 0.25 mg/ml, at which, typically the peptide could completely block the corresponding antibodies [11]. Adding of the peptides alone didn’t affect viral infection. Out of the four sera tested, peptides S1-55, S1-57 and S2-47 partially competed the neutralizing activity of one or two of the sera (Figure 5c), suggesting that antibodies against these peptides partially contribute to the neutralizing activity of the sera.
Figure 5.
Competing the neutralizing activity of convalescent serum with dominant B-cell linear epitopes. (a) Reaction of the neutralizing antibodies (Nab) and non-neutralizing antibodies (Non-Nab) with the peptide array. The peptides with signal to noise above 2.1 were counted as positive (black bar). (b) Schematic of experiment design. Four neutralizing sera (P13, P18, P68 and P98) were diluted and incubated with SARS-CoV-2 and the peptides (S1-55, S1-57, S2-13 and S2-47), respectively before added to the media. At 24 p.i, the viral RNAs in the supernatants were quantified by q-PCR. Experiment was done in duplicated well for each serum (b) Quantification of the viral RNA levels in the supernatants from representative wells. Relative RNA levels to the mock-treated wells were plotted (n = 2).
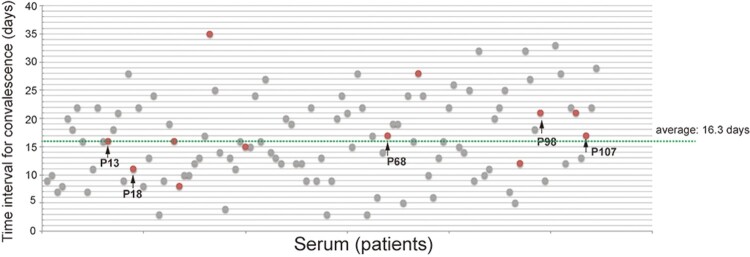
Relationship of the neutralizing activity of the sera with the progress of the COVID-19 disease
To explore if the relationship of the neutralizing activity of the sera with the progress of the COVID-19 disease, we retrospectively analysed the disease severity of the 120 COVID-19 patients. Eight patients experienced severe symptoms and patients who have sera with complete or partial neutralizing activity experienced asymptomatic or mild diseases (data not shown). We then examined the time intervals from the symptom onset to convalescence with SARS-CoV-2 triple negative diagnosis for throat swab, urine and feces. The average time interval for convalescence is 16.3 days. Patients with neutralizing antibodies (Figure 6, in red and arrows) had variable time interval for convalescence, ranging from 8 days to 35 days, which was similar with the patients without neutralizing antibodies (Figure 6).
Figure 6.
Time intervals from symptom onset to SARS-CoV-2 triple negative diagnosis. Time intervals from symptom onset to SARS-CoV-2 triple negative diagnosis for throat swab, urine and feces. Sera with neutralizing activity are in red. Arrows indicate fully neutralizing antibodies.
Discussion
To learn the profile of the B-cell linear epitopes recognized by COVID-19 cohort for guiding vaccine design and devising diagnosis reagents, we performed functional B-cell linear epitope mapping with the convalescent sera of a COVID-19 cohort. By using a 20-mer-peptide array covering the S, M and E, we identified SARS-CoV-2 dominant epitopes recognized by most COVID-19 convalescent sera (Figures 1 and 2) (Table 1). By using peptide-compete neutralizing assay, we found that epitopes in the peptides S1-55, S1-57 and S2-47 partially competed the neutralization activity of several convalescent sera (Figure 5) (Table 1), suggesting antibodies against these epitopes play an important role in neutralizing viral infection. As the convalescent serum is composed of different antibodies, it is expected that fully neutralization should be accomplished by the action of antibodies against these identified epitopes and probably other spatial epitopes. When we were preparing this manuscript, a similar study that used an 18-mer-peptide pool of spike proteins to screen 25 COVID-19 convalescent sera by ELISA was published. They identified two dominant epitopes that partially overlapped with the peptide S1-55 and S2-13 identified in this study [17]. And depletion of the COVID-19 convalescent sera by these two epitopes partially impaired the neutralizing activity of the convalescent sera [17]. In this study, in addition to these two peptides, we identified three other dominant epitopes: the epitopes in peptide S1-57 that is close to the peptide S1-55, the peptide S2-47 that is near the membrane proximal region of S and the ectodomain of M (Figures 1 and 2). Notably, peptide S1-57 competed the neutralizing activity of two sera out of four sera tested (Figure 5) (Table 1), suggesting the antibodies against this peptide play an import role in neutralizing activity. In contrast, peptide S2-13 didn't compete the neutralizing activity of the sera tested, which is inconsistent to the previous study [18]. The discrepancy might be due to the variation of the sera used.
Table 1. Summary of the identified peptides.
| Peptide | Sequence | Percentage (react with COVID-19 sera, n = 120) | Percentage (react with control sera, n = 24) | Compete neutralization of COVID-19 sera |
|---|---|---|---|---|
| S1-55 | ESNKKFLPFQ QFGRDIADTT | 44.5% | 8.33% | In 2 of 4 sera |
| S1-57 | DAVRDPQTLE ILDITPCSFG | 45.45% | 4.17% | In 2 of 4 sera |
| S1-65 | EHVNNSYECD IPIGAGICAS | 28.18% | 0 | Undetermined |
| S2-13 | LPDPSKPSKR SFIEDLLFNK | 68.18% | 16.67% | Not detected |
| S2-47 | DSFKEELDKY FKNHTSPDVD | 45.45% | 0 | In 1 of 4 sera |
| M1 | MADSNGTITV EELKKLLEQ | 63.64% | 0 | Undetermined |
We noticed two peptides S1-52 that is in the receptor-binding domain and S2-56 that is in the endomain of S highly reacted with SARS-CoV-2 negative sera (Figure 1), pointing to a risk for using the whole S or RBD as a reagent for diagnosis of SARS-CoV-2 antibodies. The dominant peptides S1-57 and M1 specifically reacted with COVID-19 sera and may provide good candidates for diagnosis reagents.
RBD of coronaviruses spike proteins mediate virus entry and antibodies against RBD potently neutralize viral infection. To our surprise, we detected much less interactions of the peptides in RBD with the sera, except for the peptide S1-52 (Figure 3). Of the 120 sera, only 5 sera completely neutralized and 7 sera partially neutralized viral infection at the dilution of 1:200. The relative low percentage of neutralizing antibody might be due to the poor recognition of RBD linear epitopes. Alternatively the most of the RBD epitopes are conformational epitopes. We cannot rule out the possibility that the non-neutralizing antibodies could sterilize viral infection by other mechanisms such as antibody-dependent cellular cytotoxicity (ADCC) [18].
In summary, we identified the dominant B-cell linear epitopes of SARS-CoV-2 in a COVID-19 cohort. Antibodies elicited by some of these antibodies played an important role in neutralizing viral infection. These epitopes may serve as a vaccine candidate to elicit neutralizing antibodies in most vaccinated people or a specific antigen for SARS-CoV-2 diagnosis.
Acknowledgements
We are grateful to professor Yumei Wen for her inspiration and encouragement; to all the staff of the biosafety level 3 laboratory at Shanghai Medical college, Fudan University for their excellent assistance; to all the volunteers for their generous donation; to Zhaoqin Zhu at the department of diagnosis for assistance for anti-S antibody tittering; to all the healthcare personnel involved in the diagnosis and treatment of patients in Shanghai Public Health Clinical Center.
Funding Statement
This work was supported in part by the National Science and Technology Major Project of China (2017ZX10103009), Key Emergency Project of Shanghai Science and Technology Committee (20411950103) and Development programs for COVID-19 of Shanghai Science and Technology Commission (20431900401). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Author contributions
Conceived the study: J. Chen, T. Ying, Z. Yi; conducted the study: K. Hu, Y. Wang, W. Song, R. Zhang, Z. Yi; clinical sample: Y. Ling, X. Zhang, H. Lu; Data analysis: Z. Yi, X. Zhang, K. Hu, Y. Wang; Manuscript draft: Z. Yi; Resources: Z. Yuan, H. Lu, Z. Yi.
References
- 1.Zhu N, Zhang D, Wang W, et al. . A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020 Feb 20;382(8):727–733. doi: 10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou P, Yang XL, Wang XG, et al. . A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020 Mar;579(7798):270–273. doi: 10.1038/s41586-020-2012-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen L, Liu W, Zhang Q, et al. . RNA based mNGS approach identifies a novel human coronavirus from two individual pneumonia cases in 2019 Wuhan outbreak. Emerg Microbes Infect. 2020 Dec;9(1):313–319. doi: 10.1080/22221751.2020.1725399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang Y, Zhang D, Du G, et al. . Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2020 May 16;395(10236):1569–1578. doi: 10.1016/S0140-6736(20)31022-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bonovas S, Piovani D.. Compassionate use of remdesivir in Covid-19. N Engl J Med. 2020 Jun 18;382(25):e101. doi: 10.1056/NEJMc2015312 [DOI] [PubMed] [Google Scholar]
- 6.Wong YK, Yang J, He Y.. Caution and clarity required in the use of chloroquine for COVID-19. Lancet Rheumatol. 2020 May;2(5):e255. doi: 10.1016/S2665-9913(20)30093-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Masters PS, Perlman S.. Coronaviridae. Fields virology, sixth edition: 825–858.
- 8.Zhu FC, Li YH, Guan XH, et al. . Safety, tolerability, and immunogenicity of a recombinant adenovirus type-5 vectored COVID-19 vaccine: a dose-escalation, open-label, non-randomised, first-in-human trial. Lancet. 2020 Jun 13;395(10240):1845–1854. doi: 10.1016/S0140-6736(20)31208-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brain D, Mou H, Zhang L, et al. . The SARS-CoV-2 receptor-binding domain elicits a potent neutralizing response without antibody-dependent enhancement. bioRxiv. 2020;2020.04.10.036418.
- 10.Gao Q, Bao L, Mao H, et al. . Rapid development of an inactivated vaccine candidate for SARS-CoV-2. Science. 2020 May 6. [DOI] [PMC free article] [PubMed]
- 11.Zhang H, Song Z, Yu H, et al. . Genome-wide linear B-cell epitopes of enterovirus 71 in a hand, foot and mouth disease (HFMD) population. J Clin Virol. 2018 Aug;105:41–48. doi: 10.1016/j.jcv.2018.06.001 [DOI] [PubMed] [Google Scholar]
- 12.Huang M, Ma Q, Liu X, et al. . Initiator integrated poly(dimethysiloxane)-based microarray as a tool for revealing the relationship between nonspecific interactions and irreproducibility. Anal Chem. 2015 Jul 21;87(14):7085–7091. doi: 10.1021/acs.analchem.5b00694 [DOI] [PubMed] [Google Scholar]
- 13.Zhang R, Yi Z, Wang Y, et al. . Isolation of a 2019 novel coronavirus strain from a coronavirus disease 19 patient in Shanghai. J Microbes Infect. 2020;15(1):15–20. [Google Scholar]
- 14.Livak KJ, Schmittgen TD.. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001 Dec;25(4):402–408. doi: 10.1006/meth.2001.1262 [DOI] [PubMed] [Google Scholar]
- 15.Corse E, Machamer CE.. The cytoplasmic tail of infectious bronchitis virus E protein directs Golgi targeting. J Virol. 2002 Feb;76(3):1273–1284. doi: 10.1128/JVI.76.3.1273-1284.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vennema H, Godeke GJ, Rossen JW, et al. . Nucleocapsid-independent assembly of coronavirus-like particles by co-expression of viral envelope protein genes. EMBO J. 1996 Apr 15;15(8):2020–2028. doi: 10.1002/j.1460-2075.1996.tb00553.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Poh CM, Carissimo G, Wang B, et al. . Two linear epitopes on the SARS-CoV-2 spike protein that elicit neutralising antibodies in COVID-19 patients. Nat Commun. 2020 Jun 1;11(1):2806. doi: 10.1038/s41467-020-16638-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Forthal DN, Finzi A.. Antibody-dependent cellular cytotoxicity in HIV infection. Aids. 2018 Nov 13;32(17):2439–2451. doi: 10.1097/QAD.0000000000002011 [DOI] [PMC free article] [PubMed] [Google Scholar]