Abstract
Objective: To conduct a pilot study of an intervention to decrease fall incidence and concerns about falling among individuals living with Spinal Cord Injury who use manual wheelchairs full-time.
Design: Pre/post. After a baseline assessment, a structured intervention was implemented. The assessment protocol was repeated 12 weeks after the baseline assessment.
Setting: Research laboratory and community.
Participants: 18 individuals living with SCI who use a manual wheelchair full-time with an average age of 35.78 ± 13.89 years, lived with SCI for 17.06 ± 14.6 years; 61.1% were female.
Intervention: A 1:1, 45 minute, in-person intervention focused on factors associated with falls and concerns about falling: transfers skills and seated postural control.
Outcome measures: Participants reported fall incidence and completed the Spinal Cord Injury Fall Concerns Scale, Community Participation Indicators and the World Health Organization Quality of Life – short version (WHOQOL-BREF). Transfer quality was assessed with the Transfer Assessment Instrument (TAI) and seated postural control with the Function In Seating Test (FIST).
Results: Recruitment, assessment and delivery of the intervention were successfully completed. After exposure to the intervention, fall incidence significantly decreased, (P = 0.047, dz = 0.507) and FIST scores improved (P = 0.035, dz = 0.54). Significant improvements were also found in the WHOQOL-BREF Physical (P = 0.05, dz = 1.566) and Psychological (P = 0.040, dz = 0.760) domains.
Conclusion: The feasibility of the structured intervention was established and the intervention has the potential to reduce fall incidence and improve quality of life among individuals living with SCI who use a wheelchair. Appropriately powered randomized controlled trials of the program are warranted.
Keywords: Accidental falls, Spinal cord injury, Wheelchair
Introduction
Falls are common among individuals living with Spinal Cord Injury (SCI) who use a manual wheelchair full-time. Between 30–65%1–3 of the population experiences at least one fall annually. Falls frequently occur during the performance of transfers, reaching for objects and wheelchair propulsion.3,4 Sung et al.5 examined the circumstances surrounding the most recent fall experienced by 23 individuals living with SCI who use a wheelchair full time. Results indicate that the most common activity being performed at the time of the fall was a transfer. Upon examination of the location, falls most frequently occurred in the bathroom and the street. Finally, surface conditions (e.g. slippery floor or a crack in the sidewalk) and being distracted were the most frequently cited attributions noted at the time of the fall.
As a result of a fall, individuals with SCI may experience physical injuries, develop a fear of falling and experience a decline in quality of life (QOL) and community participation.1
Falls frequently result in physical injuries. Forslund et al.3 found that 34% of individuals living with SCI who use a wheelchair full-time sustained at least one fall-related injury in a year. Ten percent of the injuries were classified as severe, including fractures and concussions.
Falls may also result in substantial psychosocial impairments. Even in the absence of a fall history, many individuals living with SCI who use a wheelchair full-time have concerns about falling.6,7 Such concerns can be detrimental to independence and QOL because they can limit a person’s willingness and confidence to participate in both home and community activities.6 The potential for fall-related concerns to impact QOL among people living with SCI heightens the importance of proactively identifying and mitigating these concerns.
Despite the high frequency and negative consequences associated with falls, no peer-reviewed fall prevention programs specific to individuals with SCI are described in the literature.4 This paper describes: (a) the feasibility of delivering and evaluating a brief, structured intervention; (b) the potential for that intervention to achieve two primary outcomes: reduce fall incidence and concerns about falling; (c) the potential for the intervention to achieve two secondary outcomes: improvement in QOL and community participation; and (d) the impact of the intervention on functional activities commonly associated with falls:4 transfer skills and seated postural control. We hypothesize that pre-/post-intervention measures will demonstrate significant reductions in fall incidence and concerns about falling and improvements in QOL and community participation.
Methods
To examine the feasibility and potential of the intervention to accomplish the objectives described above, a single group interventional study was implemented. The study protocol was approved by the IRB at the University of Illinois at Urbana-Champaign.
Participants were recruited from a micro-urban community between June 2015 and February 2017 via flyers posted in the community in areas frequented by individuals with SCI (e.g. physical therapy clinics, supportive living facility) and word of mouth. The recruitment goal for this study was 40 participants. Individuals were invited to participate in the study if they met the following self-reported inclusion criteria: history of SCI, at least 1 year post onset of SCI, 18 years old or older, full- time wheelchair user (use a wheelchair >40 hours per week), inability to ambulate outside of the home, and ability to transfer with moderate assistance or less (i.e. participant is able to perform 50–100% of the effort8)
Upon arrival at the testing location, the study protocol was described to each potential participant and an opportunity to ask questions was provided. Once all questions were answered, participants were asked to review the IRB-approved consent form, and if in agreement, sign the form.
Next, participants underwent a baseline assessment, as described below. After completion of the assessment, the intervention was implemented by a trained research assistant. Details regarding the intervention protocol and content are provided below and also described in Rice et al.9 After being exposed to the intervention, participants were asked to implement the techniques and exercises learned into their daily life over a period of 12 weeks. All participants were re-evaluated 12 weeks after the baseline assessment.
Feasibility
To examine the feasibility of delivering and evaluating the intervention, our research team examined recruitment and retention rates of study participants, adherence to the proposed program, safety of the program and the ability to collect primary and secondary outcomes.10
Baseline assessment protocol
Participants were asked to provide basic information about disability history and demographics, retrospectively report the number of falls sustained in the previous six months and the amount of previous training they received related to fall prevention and transfer skills. Using the Word Health Organization’s (WHO) definition,11 a fall was defined as “Inadvertently coming to rest on the ground, floor or other lower level, excluding intentional change in position to rest on furniture, walls or other objects.”
Participants were then asked to complete the Spinal Cord Injury Fall Concerns Scale (SCI-FCS)6 to assess concern about falling during 16 common activities of daily living. Participants are asked to mark on a 4-point scale how concerned they are about falling for each activity. Total scores range from 16 to 64 with higher scores indicating greater concerns about falling. Next, participants were asked to complete the World Health Organization Quality of Life – short version12 (WHOQOL-BREF) to evaluate QOL. The WHOQOL-BREF assess four different contexts of QOL including: physical capacity, psychological well-being, social relationships and environment. Scores range from 0 to 100 with higher scores indicating higher QOL. Finally, participants completed the Community Participation Indicators (CPI). The CPI evaluates two domains of community participation: participation in activities found to be important to the participant (importance) and control over participation (control).13 Scores are converted to a percentage score (0–100%) with a higher percent indicating higher levels of participation.
Following the completion of the self-reported measures described above, participants were asked to perform 4 transfers to/from a height-adjustable mat to evaluate the quality of their transfers using the Transfer Assessment Instrument 3.0 (TAI).14 The TAI is a validated outcome measure designed to evaluate transfer safety and quality in non-ambulatory individuals, including persons living with SCI. Participants are instructed to perform the transfer in their typical manner and are allowed to utilize assistive devices (such as transfer boards) or human assistance, as needed. Next, seated postural control was assessed with the Function in Sitting Test (FIST). The FIST is a clinical measure that rates participants’ ability to perform 14-seated postural tasks in a seated position15 and has been validated among individuals with SCI.16
Finally, participants were asked to prospectively report fall incidence for 3 months. Participants were provided a paper calendar and asked to place a mark on each day of the calendar on which they sustained a fall. The definitions of a “fall” was provided and verbally explained by a research assistant. Participants were provided with a self-addressed/postage paid enveloped and asked to return the calendar on a monthly basis. To assure compliance, follow up phone calls were made by a research assistant to participants every other week to remind them to stay up to date with their fall calendar.
Intervention
The intervention included an initial 1:1 session and follow up (every other week) phone calls. The 1:1 session occurred immediately after the baseline assessment and was led by a research assistant. The research assistant providing instruction is a certified athletic trainer, has a Master’s degree in Kinesiology and has a research focus on transfer skills and fall management among individuals using a wheelchair.17,18 Prior to implementation of the intervention, the research assistant received training from a physical therapist and accurately demonstrated the skills during a mock trial. Throughout the course of the intervention, periodic quality assurance checks were performed by a physical therapist to assure the education provided was accurate.
The intervention was developed by a physical therapist with over 10 years of clinical experience providing care to individuals with SCI. The person-centred19 intervention drew heavily from a physical therapy skill set and emphasized factors commonly associated with falls: transfers1,20–23 and seated postural control.1,20,24,25
The 1:1 session was designed to be delivered in approximately 45 minutes in a research laboratory setting by a trained research assistant who was aware of the outcomes sought. To support program fidelity, previously developed written transfer and exercise instructions and a transfer education video were utilized26,27. These materials were modified based on participant feedback and to meet the needs of individuals living with SCI who use a wheelchair full-time. To begin the session, the research assistant provided general instructions on transfer skills via both video presentation (i.e. Video #1) and verbal instructions. A detailed description of the transfer education is described in Rice et al.9 Briefly, the transfer education video broke down a transfer into three phases: set-up, flight, and end phases. Each component of the transfer was described, and common mistakes highlighted. While the video was playing, the research assistant highlighted specific aspects of the transfer that the participant was having difficulty performing or performing incorrectly, based on the participant’s baseline TAI scores. Transfer techniques highlighted to support successful performance include, but are not limited to, appropriate hand placement, foot placement and body positioning. For example, appropriate use of a handgrip to increase stability was discussed. In the video, different hand placements were shown, and justification provided regarding ideal placement. After completion of Video #1, participants were given the opportunity to practice the skills highlighted in the video. Specific feedback was provided by the research assistant, based on the participant’s unique needs. If a participant was having difficulty with a particular component(s) of a transfer, a block practice strategy28 was used by the research assistant until that component was mastered. Once mastered, the participant was asked to perform the entire transfer and integrate the new skills. The participant was then given written instructions that mirrored the instructions provided in Video #1. A copy of the transfer instructions is provided as an appendix associated with Rice et al.9
Next, participants were educated on a series of task-specific exercises designed to strengthen core (when present) and shoulder musculature and improve seated balance impairments using a video prevention. (Video #2) The research assistant provided clarification and further instruction, as needed. After completion of Video #2, participants demonstrated the exercises. If a participant had difficulty performing a particular exercise(s), modifications were made specific to the participant’s functional abilities. The research assistant subsequently provided instructions describing how each exercise could be progressed to become more difficult throughout the course of the intervention. Participants were instructed to perform the exercise routine 2–3 times per week; and complete an exercise log to indicate the extent of adherence to the exercise program. A written description of the exercise program was given to study participants is provided in Appendix A [see Supplemental data].
The intervention concluded with discussions about specific problems the participant was having within his or her own environment that caused falls or near falls. The research assistant helped participants problem solve through the specific challenges and provided recommendations on activity or environmental modifications.
Upon completion of the intervention, the participant was asked to integrate the education and exercise program into his or her daily activities. The research assistant noted any modifications to the transfer techniques or exercises on the instruction sheets. Participants were also given access to the two instructional videos, either via a link to a private YouTube channel or if the participant had limited internet access, a DVD. The research assistant asked each participant to watch both videos every other week.
Participant monitoring
After the intervention was implemented, each participant was called by the research assistant who provided the initial education every other week to inquire about adherence to the exercises and recommendations discussed during the in-person session. If participants reported that the exercises were too easy or difficult, adjustments were made. Participants also had an opportunity to ask questions about the transfer techniques and were reminded to watch the instructional transfer video every other week. Participants were asked to report the frequency of their falls during the past two weeks using a standardized script.
Follow up assessment protocol
Each study participant was asked to return for a follow up assessment 12 weeks after the baseline visit. The same outcome assessments, as described for the baseline assessment, were performed. Participants were also asked to provide feedback on the intervention. Specifically, they were asked if they changed the way they performed their transfers, if they found the transfer education helpful and to report the number of times they watched the transfer video and performed their exercise program.
Data analysis
Quantitative data were analyzed using SPSS version 22 (SPSS, Inc., Chicago, IL). An exploratory analysis was performed and Shapiro-Wilks testing found fall frequency to be non-normally distributed. All other variables of interest utilized ordinal data. To examine the differences pre- and post-exposure to the intervention, a generalized linear model was utilized. A secondary analysis was performed to examine the influence of the intervention among study participants based on the level of injury and completeness of injury (AIS level). Regarding the level of injury, two groups of participants were formed, those with a self-reported injury level at T9 and above and T10 and below. Participants were also divided into two groups based on the extent of injury: Group 1-AIS A and B, Group 2-AIS C and D. Effect sizes (d) were calculated using Cohen’s dz using the protocol established by Lakens.29 Significance was set a priori at P ≤ 0.05. No corrections were made for multiple comparisons due to the small sample size and the pilot nature of the study. Qualitative data were transcribed verbatim and coded by a study investigator who was not involved with the implementation of the intervention.
Results
Participants
Participants were an average of 35.78 ± 13.89 years old and lived with their SCI for an average of 17.06 ± 14.6 years. The majority of participants were female (n = 11, 61.1%). Level of injury ranged from C4-L3, AIS A-D. All participants used a manual wheelchair and performed transfers without assistance. Prior to the start of the study, 6 participants (33.3%) reported they had received prior education on fall prevention, and 14 reported (77.8%) they had previous transfer training. The majority of participants reported they had sustained a fall during a transfer (n = 17, 94.4%) prior to the commencement of the study. Please see Table 1 for additional details.
Table 1. Participant demographic and fear of falling data (n = 18).
| Variable | Results | |
|---|---|---|
| Age (m (SD)) | 35.78 (13.89) | |
| Time since injury (m (SD)) | 17.06 (14.60) | |
| Sex (n (%)) | Male | 7 (38.9) |
| Female | 11 (61.1) | |
| AIS level | A | 6 (33.3) |
| B | 1 (5.6) | |
| C | 8 (44.4) | |
| D | 1 (5.6) | |
| Unknown | 2 (11.1) | |
| Level of injury | Tetraplegia | 2 (11.1) |
| High Paraplegia (T1-T9) | 6 (33) | |
| Low Paraplegia (10 and below) | 10 (56) | |
| Are you afraid of falling? | Not at all | 9 (50) |
| Somewhat afraid | 5 (27.8) | |
| Fairly afraid | 4 (22.2) | |
| Do you think your fear of falling has made you cut down on any activities? | Yes | 3 (16.7) |
| No | 15 (83.3) | |
Feasibility
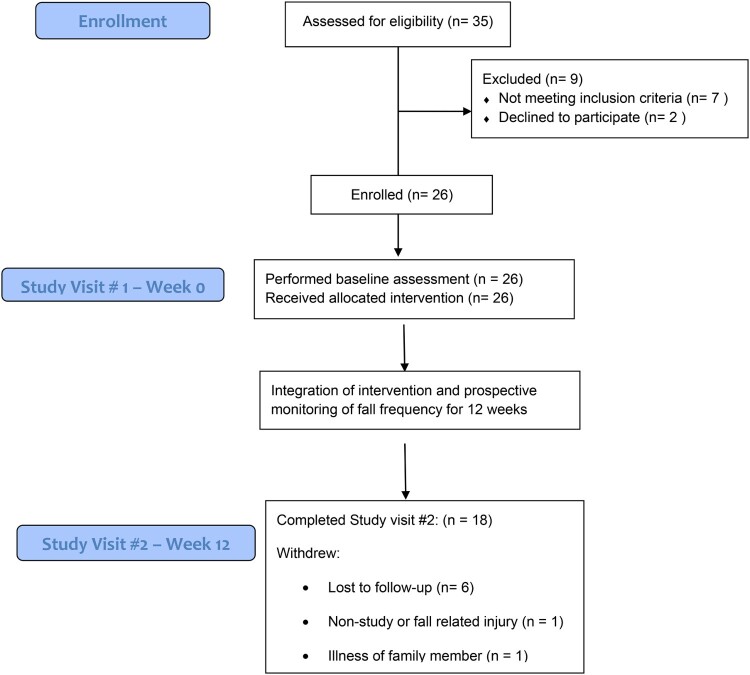
The research study was found to be feasible, however modifications may increase the impact of future research. We did not reach our initial recruitment goal of 40 participants. Thirty-five participants were screened, however only 26 (74%) were enrolled. Nine participants were excluded because they did not meet the inclusion criteria (n = 7) or declined to participate (n = 2). During the course of the study, 18 participants completed both study visits and 8 withdrew from the study (30%). Six participants were lost to follow up, 1 participant sustained a significant, non-study or fall-related injury, and 1 participant withdrew due to a serious illness experienced by a family member. Please see Fig. 1 for additional details. No significant differences were found in baseline data between participants who completed all study visits compared to those who withdrew. During the course of the study, no adverse events occurred and no injuries were reported by study participants associated with the intervention. Of the participants who completed both study visits, the outcomes of interest were able to be collected, as noted below.
Figure 1.
Enrollment and assessment diagram.
Primary outcomes: fall incidence and concerns about falling
After exposure to the intervention, fall incidence significantly decreased, (Pre: 1.37 ± 1.62 falls per month, Post: 0.67 ± 0.82, P = 0.047, dz = 0.507). Concerns about falling (SCI-FCS) also decreased (Pre: 22.72 ± 5.77, Post: 21.78 ± 0.5.26) but the results were not significant, P = 0.103. A moderate effect size was found, dz = 0.421.
Secondary outcomes: quality of life and community participation
Significant improvements following the intervention were found in the WHOQOL-BREF Physical Capacity (Pre: 67.83 ± 15.96, Post: 75.61 ± 16.38 P = 0.05, dz = 1.566) and Psychological Well-Being (Pre: 69.06 ± 14.67, Post: 76.17 ± 17.62, P = 0.040, dz = 0.760) domains. No significant differences were found among the WHOQOL-BREF social relationships and environment domains or CPI scores. Please see Table 2 for additional details.
Table 2. Quality of life and community participation results (n = 18).
| Outcome | Pre intervention | Post intervention | P value | Effect size | |
|---|---|---|---|---|---|
| World Health Organization-Quality of Life (Short Version) Domains | Physical health | 63.22 (12.59) | 75.61 (16.38) | 0.05* | 1.566 |
| Psychological | 65.56 (10.18) | 76.17 (17.62) | 0.04* | 0.760 | |
| Social relationships | 70.44 (25.11) | 67.28 (26.02) | 0.465 | 0.299 | |
| Environment | 81.44 (14.65) | 81.06 (13.46) | 0.438 | 0.036 | |
| Community participation indicators domains | Importance | 60.72 (11.78) | 58.87 (12.42) | 0.583 | 0.15 |
| Control | 71.85 (18.66) | 68.40 (19.29) | 0.308 | 0.18 |
*P ≤ 0.05.
Functional outcomes
Among the functional outcomes of interest, seated postural control, as measured by the FIST, significantly improved (Pre: 43.78 ± 6.74, Post: 45.17 ± 7.25, P = 0.035, dz = 0.54). TAI scores also improved but differences were not significant (Pre: 7.99 ± 0.93, Post: 8.17 ± 0.91, P = 0.131, dz = 0.383).
Subpopulations
Additional analysis was performed to examine the influence of the intervention based on the participant’s level of injury and extent of injury.
Upon examination of level of injury, a significant decrease in fall frequency was found among participants with an injury level T9 and above (Pre: 1.04 ± 1.49, Post: 0.43 ± 0.52, P = 0.049, dz = 0.53). In addition, a significant increase in the physical health domain of the WHOQOL-BREF was found (Pre: 68.88 ± 18.35, Post: 81.50 ± 11.57, P = 0.026, dz = 1.32) among individual with an injury level at T10 and below.
Related to completeness of injury, significant improvements were seen among individuals with self-reported AIS C and D in the WhOQOL-BREF physical health (Pre: 68.11 ± 9.61, Post: 75.89 ± 15.76, P = 0.56, dz = .79) and psychological health (Pre: 65.22 ± 12.53, Post: 75.78 ± 18.85, P = 0.041, dz = .97) domains. In addition, among individuals with self-reported AIS C and D levels, FIST scores also showed significant improvements (Pre: 47.00 ± 7.28, Post = 48.89 ± 6.47, P = 0.046, dz = .93)
Intervention feedback
Self-reported data revealed that participants watched the transfer video an average of 3 times (3.38 ± 2.87) during the course of the intervention, and that exercises were performed an average of 2 times (2.27 ± 1.28) per week. The majority of participants (83.3%) reported that they did not change the way they performed their transfers, but did find the transfer education helpful (n = 76.9%). Upon follow up, participants reported that the education helped to refine the transfer skill they had learned elsewhere.
Discussion
This pilot study examines the feasibility and the potential to achieve targeted outcomes of a brief intervention to decrease fall incidence and concerns about falling among individuals living with SCI who use a manual wheelchair full-time. The influence on secondary and functional outcomes was also evaluated. The feasibility of the study was established and results show promise. While future research is needed to examine the long-term influence of the program, this pilot study provides important preliminary evidence to support the use of a clinically feasible intervention to manage fall incidence among individuals living with SCI who use a manual wheelchair full-time.
The study was found to be feasible, however challenges were faced regarding recruitment and retention of study participants. The study was performed in a micro-urban environment with a limited SCI population and limited accessible public transportation. Performance of the intervention in one or more urban locations with larger populations of individuals living with SCI may help to recruit more participants and retain those enrolled. Accessible public transportation or funding transportation by taxi or a ride-sharing service may facilitate access to engage in study visits. In addition, collaboration with a hospital system may facilitate recruitment of individuals living with SCI. Finally, offering aspects of the education materials as an online program may help to increase access to education and reduce the travel burden placed on the study participants.
Self-reported fall incidence significantly decreased after exposure to the intervention and a moderate effect size was noted. Upon further examination of subpopulations of participants, a significant decrease in fall frequency was also found among individuals with self-reported injury levels at T9 and above. Due to the significant consequences associated with falls,3 decreasing incidence may have a positive impact on the health and well-being of individuals living with SCI who use a manual wheelchair full time. The education provided may be of particular importance to individuals with levels of injury above T9. At baseline, no significant difference existed in fall frequency between participants based on the level of injury (P = 0.546), however after the exposure to the intervention, individuals with levels of injury at T9 and above showed a significant decrease in fall frequency (P = 0.049).
No significant differences were found among concerns about falling, however a moderate effect size was noted. Comparable results were found in a fall management study targeting full-time wheelchair and scooter users living with Multiple Sclerosis (MS).9 Among ambulatory individuals, many different factors influence concerns about falling.30 Although the research specific to individuals living with SCI who use a wheelchair full time is limited6 it is likely that the factors influencing concerns about falling in this population are also complex.
As a result, a longer follow up period may be necessary for perceptions of study participants to change and concerns about falling to be effectively fully managed. Enhanced discussions during the follow up phone calls to address participants concerns and reinforcement of activities participants are doing well may increase confidence. Also, if a fall does occur, discussions should be held on strategies to prevent similar future falls. The intervention also may need to utilize a more comprehensive approach that includes the involvement of care providers and attention to fall risk factors beyond transfers and seated postural control. For example, wheelchair propulsion skills were not discussed in the current education program but are frequently noted as activities associated with falls.3,17
The development of fall management plans and recovery strategies may also be necessary. The importance of a post fall management plan has been established by Bisson et al.31 Among ambulatory older adults with MS, post fall management education has been successfully integrated in to a fall risk management program.32 Finally, delivery of the intervention by a licensed Physical or Occupational Therapist may enhance the impact of the program. Licensed clinical professionals have the knowledge base necessary to help participants problem solve through challenging situations and make feasible changes.
Currently, little is known about the connection between QOL and fall frequency/concerns about falling among individuals living with SCI who use a wheelchair full time. Forslund et al.,3 found that higher QOL reduces the odds of experiencing fall-related injuries among individuals living with SCI who use wheelchair full time. Our preliminary evidence indicates that significant improvements were found among the Physical and Psychological Health domains of the WHOQOL-BREF after exposure to the intervention. These domains evaluate items such as performance of activities of daily living, mobility, energy and fatigue (physical) and self-esteem and thinking/learning/concentration (psychological). Improvements in such activities are important for the health and well-being of individuals living with SCI. Upon further examination of subpopulations, significant improvements in the physical health domain were seen among individuals with self-reported levels of injury at T10 and below and AIS levels of C and D. Individuals with self-reported AIS levels of C and D show significant improvements in the psychological health domain. Scores also improved among individuals with self-reported injuries at T9 and above and with AIS levels of A and B however the results were not significant. Additional, more comprehensive education may be necessary to influence this group of participants with a greater extent of disability.
Significant improvements, however, were not seen in community participation. A lack of desired participation can result in significant negative consequences for individuals living with SCI who use a wheelchair full time.33 To encourage increased participation, providing targeted education on strategies to facilitate active participation in the community may be necessary. For example, discussions should be held on what is holding a participant back from engagement and how high-quality functional mobility skills can facilitate engagement.
After exposure to the intervention, significant improvements were also found in seated postural control. Similar results were found by Boswell-Ruys et al.34 after implementing a task-specific training program to improve unsupported sitting among individuals living with SCI who use a wheelchair full time. Improved seated postural control is not only important in the management of fall risk but is also associated with improvements in the performance of activities of daily living and independent living. Further analysis revealed that significant improvements were seen specifically among individuals with self-reported AIS C and D. Given the incomplete nature of the spinal cord injury, it is not surprising that the exercises had a greater influence on this group compared to individuals with AIS A and B.
Study limitations
This study evaluated a relatively small and homogeneous group of individuals living with Spinal Cord Injury who use manual wheelchairs full time. In addition, the low enrollment and high dropout rate may have resulted in an inclusion bias. As a result, findings cannot be generalized to a larger group of participants. Despite the limitation, the preliminary findings and feedback from study participants will provide an important resource on which a larger, more comprehensive program can be developed. In addition, finding will offer power estimates for future investigations.
Due to the home-based nature of the intervention, it is unclear the level at which participants actively engaged in the transfer practice and performance of the exercise program in their own homes. While follow up calls were done to remind participants of the program and inquire about the frequency of performance, the research team was unable to directly observe the practice sessions of study participants. Participants may have misreported the frequency of which they performed the exercises and practiced the transfer skills. In-person practice sessions and enhanced accountability may help to increase the engagement of participants.
Finally, self-reported fall frequency was retrospectively collected prior to the start of the intervention and prospectively monitored between the first and second study visit. Participants may have mis-reported their baseline fall frequency. Previous research, however, has found similar fall incidence rates among data collected retrospectively and prospectively.35
Future work
Further investigation is necessary to examine the long-term impact of the program, especially on complex variables such as concerns about falling and community participation. Additional outcome assessments, such as open-ended questions or semi-structured interviews, may be necessary to more fully examine complex variables such as concerns about falling and community participation. Performance of a randomized clinical trial will facilitate further examination of the program. In addition, expansion of the intervention to include additional topics, such as wheelchair propulsion skills and fall management plans may increase the impact of the program. Finally, the delivery of the program by a licensed physical or occupational therapist may help study participant implement important fall prevention changes into their daily activities.
Conclusion
Although future investigation is needed and limitations exist, this intervention program fills a void in the effort to provide evidence-based fall prevention services to individuals living with SCI who use a manual wheelchair full time and serves as an important resource on which future research and evidenced-based clinical practice in fall prevention for people living with SCI can be based.
Disclaimer Statements
Funding This study was funded by the Craig H. Neilsen Foundation, Psychosocial Research Grants, 323277.
Conflicts of interest The authors have no conflicts of interest to declare.
Supplementary Material
References
- 1.Nelson A, Ahmed S, Harrow J, Fitzgerald S, Sanchez-Anguiano A, Gavin-Dreschnack D.. Fall-related fractures in persons with spinal cord impairment: a descriptive analysis. SCI Nurs: A Publ Am Assoc Spinal Cord Inj Nurse . 2003;20(1):30–37. [PubMed] [Google Scholar]
- 2.Nelson AL, Groer S, Palacios P, Mitchell D, Sabharwal S, Kirby RL, et al. Wheelchair-related falls in veterans with spinal cord injury residing in the community: a prospective cohort study. Arch Phys Med Rehabil . 2010;91(8):1166–73. doi: 10.1016/j.apmr.2010.05.008 [DOI] [PubMed] [Google Scholar]
- 3.Forslund EB, Jorgensen V, Franzen E, Opheim A, Seiger Å, Ståhle A, et al. High incidence of falls and fall-related injuries in wheelchair users with spinal cord injury: A prospective study of risk indicators. J Rehabil Med . 2017;49(2):144–51. doi: 10.2340/16501977-2177 [DOI] [PubMed] [Google Scholar]
- 4.Rice LA, Ousley C, Sosnoff JJ.. A systematic review of risk factors associated with accidental falls, outcome measures and interventions to manage fall risk in non-ambulatory adults. Disabil Rehabil . 2015;37(19):1697–705. doi: 10.3109/09638288.2014.976718 [DOI] [PubMed] [Google Scholar]
- 5.Sung J, Trace Y, Peterson EW, Sosnoff JJ, Rice LA.. Falls among full-time wheelchair users with spinal cord injury and multiple sclerosis: a comparison of characteristics of fallers and circumstances of falls. Disabil Rehabil . 2019;41(4):389–95. doi: 10.1080/09638288.2017.1393111 [DOI] [PubMed] [Google Scholar]
- 6.Boswell-Ruys CL, Harvey LA, Delbaere K, Lord SR.. A falls concern Scale for people with spinal cord injury (SCI-FCS). Spinal Cord . 2010;48(9):704–9. doi: 10.1038/sc.2010.1 [DOI] [PubMed] [Google Scholar]
- 7.Butler Forslund E, Roaldsen KS, Hultling C, Wahman K, Franzen E.. Concerns about falling in wheelchair users with spinal cord injury–validation of the Swedish version of the spinal cord injury falls concern scale. Spinal Cord . 2016;54(2):115–19. doi: 10.1038/sc.2015.125 [DOI] [PubMed] [Google Scholar]
- 8.Dodds TA, Martin DP, Stolov WC, Deyo RA.. A validation of the functional independence measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil . 1993;74(5):531–6. doi: 10.1016/0003-9993(93)90119-U [DOI] [PubMed] [Google Scholar]
- 9.Rice LA, Isaacs Z, Ousley C, Sosnoff J.. Investigation of the feasibility of an intervention to manage fall risk in wheeled mobility device users with multiple Sclerosis. Int J MS Care . 2018;20(3):121–8. doi: 10.7224/1537-2073.2016-097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thabane L, Ma J, Chu R, Cheng J, Ismaila A, Rios LP, et al. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol . 2010;10:1. doi: 10.1186/1471-2288-10-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Faisal W, Beattie L, Fu H, James K, Kalula S, Krishnaswamy B, et al. WHO global report on falls prevention in older age. World Health Organization; 2007.
- 12.Lin MR, Hwang HF, Chen CY, Chiu WT.. Comparisons of the brief form of the World Health Organization Quality of Life and Short Form-36 for persons with spinal cord injuries. Am J Phys Med Rehabil . 2007;86(2):104–13. doi: 10.1097/01.phm.0000247780.64373.0e [DOI] [PubMed] [Google Scholar]
- 13.Heinemann AW, Magasi S, Bode RK, Hammel J, Whiteneck GG, Bogner J, et al. Measuring enfranchisement: importance of and control over participation by people with disabilities. Arch Phys Med Rehabil . 2013;94(11):2157–65. doi: 10.1016/j.apmr.2013.05.017 [DOI] [PubMed] [Google Scholar]
- 14.Tsai CY, Rice LA, Hoelmer C, Boninger ML, Koontz AM.. Basic psychometric properties of the transfer assessment instrument (version 3.0). Arch Phys Med Rehabil . 2013;94(12):2456–64. doi: 10.1016/j.apmr.2013.05.001 [DOI] [PubMed] [Google Scholar]
- 15.Gorman SL, Radtka S, Melnick ME, Abrams GM, Byl NN.. Development and validation of the Function In sitting test in adults with acute stroke. J Neurol Phys Ther: JNPT . 2010;34(3):150–60. doi: 10.1097/NPT.0b013e3181f0065f [DOI] [PubMed] [Google Scholar]
- 16.Abou L, Sung J, Sosnoff JJ, Rice LA.. Reliability and validity of the function in sitting test among non-ambulatory individuals with spinal cord injury. J Spinal Cord Med . 2019:1–8. doi: 10.1080/10790268.2019.1605749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sung J, Trace Y, Peterson EW, Sosnoff JJ, Rice LA.. Falls among full-time wheelchair users with spinal cord injury and multiple sclerosis: a comparison of characteristics of fallers and circumstances of falls. Disabil Rehabil. 2019;41(4):389–395. doi: 10.1080/09638288.2017.1393111 [DOI] [PubMed] [Google Scholar]
- 18.Worobey LA, Zigler CK, Huzinec R, Rigot SK, Sung J, Rice LA.. Reliability and validity of the revised transfer assessment Instrument. Top Spinal Cord Inj Rehabil . 2018;24(3):217–26. doi: 10.1310/sci2403-217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Entwistle VA, Watt IS.. Treating patients as persons: a capabilities approach to support delivery of person-centered care. Am J Bioeth . 2013;13(8):29–39. doi: 10.1080/15265161.2013.802060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen WY, Jang Y, Wang JD, Huang W-N, Chang C-C, Mao H-F, et al. Wheelchair-related accidents: relationship with wheelchair-using behavior in active community wheelchair users. Arch Phys Med Rehabil . 2011;92(6):892–8. doi: 10.1016/j.apmr.2011.01.008 [DOI] [PubMed] [Google Scholar]
- 21.Kirby RL, Ackroyd-Stolarz SA, Brown MG, Kirkland SA, MacLeod DA.. Wheelchair-related accidents caused by tips and falls among noninstitutionalized users of manually propelled wheelchairs in Nova Scotia. Am J Phys Med Rehabil . 1994;73(5):319–30. doi: 10.1097/00002060-199409000-00004 [DOI] [PubMed] [Google Scholar]
- 22.Kirby RL, Smith C.. Fall during a wheelchair transfer: a case of mismatched brakes. Am J Phys Med Rehabil . 2001;80(4):302–4. doi: 10.1097/00002060-200104000-00015 [DOI] [PubMed] [Google Scholar]
- 23.Thapa PB, Brockman KG, Gideon P, Fought RL, Ray WA.. Injurious falls in nonambulatory nursing home residents: a comparative study of circumstances, incidence, and risk factors. J Am Geriatr Soc . 1996;44(3):273–8. doi: 10.1111/j.1532-5415.1996.tb00913.x [DOI] [PubMed] [Google Scholar]
- 24.Dyer D, Bouman B, Davey M, Ismond KP.. An intervention program to reduce falls for adult in-patients following major lower limb amputation. Healthc Quart (Toronto, Ont) . 2008;11(3 Spec No.):117–21. doi: 10.12927/hcq.2008.19661 [DOI] [PubMed] [Google Scholar]
- 25.Saverino A, Benevolo E, Ottonello M, Zsirai E, Sessarego P.. Falls in a rehabilitation setting: functional independence and fall risk. Eura Medicophys . 2006;42(3):179–84. [PubMed] [Google Scholar]
- 26.Rice LA, Isaacs Z, Ousley C, Sosnoff J.. Investigation of the feasibility of an intervention to manage fall risk in Wheeled mobility device users with multiple Sclerosis. Int J MS Care. 2018;20(3):121–128. doi: 10.1177/0885066616668483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rice LA, Smith I, Kelleher AR, Greenwald K, Hoelmer C, Boninger ML.. Impact of the clinical practice guideline for preservation of upper limb function on transfer skills of persons with acute spinal cord injury. Arch Phys Med Rehabil . 2013;94(7):1230–46. doi: 10.1016/j.apmr.2013.03.008 [DOI] [PubMed] [Google Scholar]
- 28.Immink MA, Wright DL.. Motor programming during practice conditions high and low in contextual interference. J Exp Psychol Hum Percept Perform . 2001;27(2):423–37. doi: 10.1037/0096-1523.27.2.423 [DOI] [PubMed] [Google Scholar]
- 29.Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol . 2013;4:863. doi: 10.3389/fpsyg.2013.00863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peterson EW, Cho CC, Finlayson ML.. Fear of falling and associated activity curtailment among middle aged and older adults with multiple sclerosis. Mult Scler . 2007;13(9):1168–75. doi: 10.1177/1352458507079260 [DOI] [PubMed] [Google Scholar]
- 31.Bisson EJ, Peterson EW, Finlayson M.. Delayed initial recovery and long lie after a fall among middle-aged and older people with multiple sclerosis. Arch Phys Med Rehabil . 2015;96(8):1499–505. doi: 10.1016/j.apmr.2015.04.012 [DOI] [PubMed] [Google Scholar]
- 32.Finlayson M, Peterson EW, Cho C.. Pilot study of a fall risk management program for middle aged and older adults with MS. NeuroRehabilitation . 2009;25(2):107–15. doi: 10.3233/NRE-2009-0505 [DOI] [PubMed] [Google Scholar]
- 33.Liptak GS. Health and well being of adults with cerebral palsy. Curr Opin Neurol . 2008;21:136–42. doi: 10.1097/WCO.0b013e3282f6a499 [DOI] [PubMed] [Google Scholar]
- 34.Boswell-Ruys CL, Harvey LA, Barker JJ, Ben M, Middleton JW, Lord SR.. Training unsupported sitting in people with chronic spinal cord injuries: a randomized controlled trial. Spinal Cord . 2010;48(2):138–43. doi: 10.1038/sc.2009.88 [DOI] [PubMed] [Google Scholar]
- 35.Rapp K, Freiberger E, Todd C, Klenk J, Becker C, Denkinger M, et al. Fall incidence in Germany: results of two population-based studies, and comparison of retrospective and prospective falls data collection methods. BMC Geriatr . 2014;14:105. doi: 10.1186/1471-2318-14-105 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.