Abstract
Background
Understanding factors affecting recruitment and retention of health workers in rural and remote communities is necessary for proper policy development and the equitable achievement of Universal Health Coverage.
Aim
Review and synthesize the literature on interventions used to retain health workforce in rural and remote areas by low‐ and middle‐income countries (LMICs) in the Eastern Mediterranean Region (EMR).
Method
We carried out a narrative review of literature (peer‐reviewed and gray) on the distribution and retention of health workers in rural and remote areas in the LMICs of the EMR. Out of the 130 retrieved articles, 21 met the inclusion criteria and were studied using WHO's Global Recommendations For Increasing Access To Health Workers In Remote And Rural Areas Through Improved Retention (education, regulation, financial, and personal/professional) as the analytical framework for extractions.
Results
There is a dearth of literature on retention in rural areas in the EMR and a complete absence of evaluation studies for implemented intervention. Various LMICs in the EMR have implemented interventions across one or more of the WHO four categories, especially educational and regulatory interventions. Limitations in the number and quality of published studies, fragmented data, over‐representation of certain cadres in research and policies, and poor governance were chief barriers to the design, implementation, and evaluation of health workforce retention policies in rural and remote areas. The main challenges for EMR countries are in policy implementation and evaluation. Strengthening data governance and health information systems would improve evidence‐based policies and enhance retention in rural and remote areas.
Conclusions
There is a need for a focused research agenda supported by regional collaboration to guide policymakers on factors, challenges, and best practices that need to be considered for improving the distribution and retention of the health workforce by cadre, gender, and region.
Keywords: Eastern Mediterranean Region, health workforce, low‐ and middle‐income, policy, recruitment, retention, review, rural
What is known about the topic?
There is a global challenge in recruiting and retaining health workers in rural and remote communities, which is exacerbated in low‐ and middle‐income countries of the Eastern Mediterranean Region (EMR).
Understanding the push and pull factors affecting retention in rural and remote communities is essential for guiding the development of evidence‐based policies and interventions.
What this paper adds?
Synthesis of regional literature on the recruitment and retention policies and interventions of health workers in rural areas in the EMR; available literature is poor in terms of quantity and quality (no evaluation studies).
Of WHO's 4 categories of interventions, educational and regulatory interventions for the retention of health workers in remote areas of the EMR were more common than financial and professional interventions.
Retention in rural areas of the EMR could be enhanced by endorsing a focused research agenda, and scaling up information systems, supported by regional collaboration.
1. BACKGROUND
Building resilient and people‐centered health systems are foundational to advancing Universal Health Coverage (UHC) and ensuring that communities receive their right to health. 1 , 2 However, it is impossible to achieve health equity without adequate numbers of well‐trained and properly distributed health workers. The World Health Organization (WHO) estimated that more than a quarter of the world's countries do not have enough health workers, with a projected shortfall of 17 million by 2030. 3 The shortage of health workers, especially in rural and remote areas, remains a serious challenge to the attainment of UHC and the delivery of equitable health to all. 4 Such shortages are compounded and exacerbated by the ongoing conflicts that have pressured, weakened or degraded many health systems, especially in the Eastern Mediterranean Region (EMR). 1
This shortage in health workers in the EMR is caused by a variety of factors, including: (a) A shortfall in the production and availability of health workers. (b) Poor workforce planning, for example, gender imbalances (limiting the provision of acceptable and accessible care in a culturally conservative Region), disproportional production and distribution by cadre, over‐reliance on expatriate health workers, and inequitable geographic distribution. 5 , 6 (c) Migration and/or displacement in many countries in the EMR, especially as two thirds countries are affected by emergencies and conflict precipitating safety, security, and mobility concerns. 1 , 7 Other barriers include: unregulated competition from the private sector, lack of reliable and updated regional health workforce information, and poor workforce regulation and management. 5
Despite rapid urbanization, about half of the world's population lives in rural areas, with Africa and Asia hosting nearly 90% of the world's rural populations; statistics reveal rural‐urban inequities with the 10% urban populations are served by 75% of doctors and 62% of nurses. 8 This suggests the need to enhance the production, recruitment, deployment, and retention of rural‐practicing health workers of all cadres.
Retention of health workers, especially in rural and remote areas, is a challenge in all countries, from high‐income Canada, Australia, and Scotland to many low‐ and middle‐income countries (LMICs) in Africa and Asia, with fragile and understaffed health systems. 4 , 9 , 10 , 11 While strategies have been proposed and implemented in developed countries, such as the United States, New Zealand, and Japan, understanding the push and pull factors that affect retention in resource‐constrained settings is critical to creating context‐appropriate and evidence‐based policies and solutions. 11 Major push factors cited from the EMR, mirrored the global literature, particularly in LMICs, including: poor remuneration, poor working conditions, outmoded health facilities, shortages in equipment and supplies, limited career development opportunities, poor management, undervaluing work environment, professional isolation, limited career opportunities for spouses, and poor educational opportunities for children, among others. 6 , 8 , 12 , 13 , 14 , 15 Most countries also reported corruption, lack of regulation and poor management as leading factors affecting their job satisfaction and motivation to deploy to or remain in rural and remote areas. Better opportunities in Europe and North America and in the Gulf Cooperative Council (GCC) countries, gender and cultural restrictions, and insecurity were highlighted push factors for health workers in the EMR. 16 , 17 , 18
1.1. Health workforce maldistribution in the EMR's rural and remote areas
Most LMICs in the EMR have at least half of their populations residing in rural areas, and many of those countries have a critical shortage of health workforce, with a density lower than 23 doctors, nurses and midwives per 10 000 (Figure 1). 5 In addition to low economic standing and low densities of health workers, most of those countries are currently affected by crises (or are graded emergencies by the UN and WHO). This influences how these countries manage their human resources, especially as rural and remote areas tend be more vulnerable to poverty, scarcity, insecurity, and violence. 5
Figure 1.
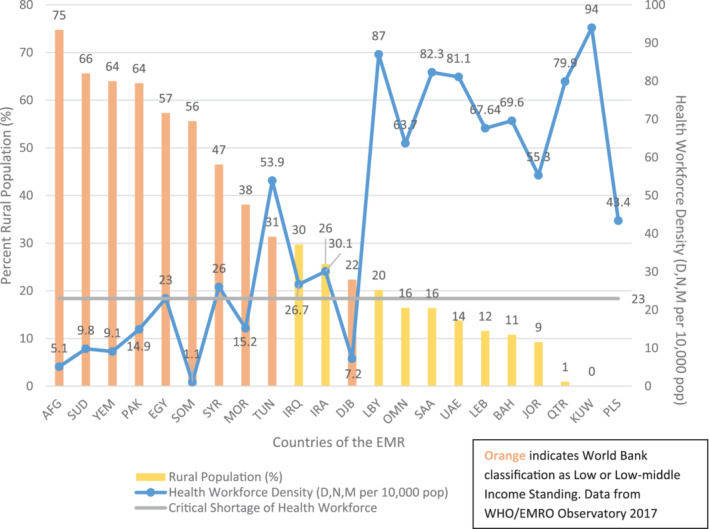
Rural population vs health workers density in EMR. EMR, Eastern Mediterranean Region
In addition to the critical shortage of health professionals facing a third of the countries in the EMR (Figure 1), there are three major trends observed regarding the geographic distribution of health workers in the Region. 19 Firstly, most health workers are concentrated in more urban areas (working in many secondary and tertiary health facilities). In Sudan, over 70% of skilled health professionals work in Khartoum, the capital, serving approximately 30% of the country's population. 13 In Somalia, 85% of health workers serve 40% of the population in the urban areas. 20 In Afghanistan, urban areas (where 25% of the population lives) host more than double the number of health workers residing in rural areas. Workforce densities indicate 36/10000 in urban compared to 16.7/10000 in rural areas. 14 In Kurdistan (Northern Iraq), 84% of doctors work in urban areas. 15 In Pakistan (64% rural), there are four times as many doctors in urban areas; when disaggregating the average density of physicians (eight physicians per 10 000)—in the urban areas, this ratio is 14.5/10000, whereas it is 3.6/10000 in the rural areas. 21 In Somalia (56% rural), only 9% of physicians are employed in rural settings. 20
Secondly, the overproduction of specialists across the entire Region further exacerbates the shortage of health workers in rural areas. In Lebanon and Iran, over 70% of physicians are specialized, leaving a shortage of general practitioners (who are generally more likely to reside in rural settings). 16 , 22 Afghanistan (75% rural) and Sudan (66%), the countries with the highest rural populations in the EMR, have 89% and 65% of specialists working in their respective capitals. 13 , 14
Thirdly, there is an uneven distribution of health workers in urban areas due to their preference for nonprimary (and often private) health settings. In Kurdistan (Northern Iraq), 74% of doctors work in hospitals and 23% work in primary healthcare centers (PHCs). 15 In Sudan, 67% of health workers are in secondary and tertiary settings. 13 These geographic maldistributions result in a concentration of physicians and specialists in urban areas further affects the staffing of health facilities in rural areas, often leaving nurses and nonphysicians acting as the primary‐care‐provider in some rural PHCs.
Despite the centrality of rural retention in EMR countries, most articles on the retention of health workers in rural and remote areas stem from middle‐ or high‐income countries, with limited examples from the EMR. 23 This article carries out a narrative review focused on outlining the interventions and strategies utilized to enhance health workforce retention in rural and remote areas in the LMICs of the EMR. This review further outlines the major, EMR specific, factors decreasing rural workforce retention in the EMR.
2. METHODS
A review of published and gray literature using PUBMED and Google Scholar, searching key terms and their variations related to: human resources for health (HRH), health workforce, health manpower, attrition, retention, incentives, recruitment, deployment, primary health, rural, remote, low‐ and middle‐income, Middle‐East, North Africa, and LMICs in the EMR. The Gulf Cooperation Council (GCC) countries in the EMR were not included in this review, as they either have almost no rural populations (Kuwait, Bahrain, and Qatar) or have small nomadic populations living in remote areas (Saudi Arabia, Oman, and the United Arab Emirates).
The national health strategies for the EMR countries, as well as the major WHO and World Bank publications on health workforce (eg, the World Health Report 2006 and the Global Strategy for HRH: Workforce 2030) were studied. A check of the reference list of all identified manuscripts/documents was carried out to identify additional relevant references, in the global and regional literature.
Since there is no universal precise definition for “rural and remote areas” as they depend on country‐classification based on population density and distance from urban‐centers, the definition used by WHO's global recommendations was adopted. WHO places “rural and remote areas” in the category of “underserved areas” which are “geographical areas where populations have limited access to qualified healthcare services and providers”; further, “rural” is defined as “an area that is not urban in nature; urban usually incorporates the population in a city or town, plus suburban areas outside or adjacent to city limits” while the definition for “remote” is not detailed. 11 Exclusion criteria included: urban slums, conflict zones, and refugee camps, as per this WHO definition.
The inclusion criteria for this review were the following: (a) articles published in English (Arabic and non‐English publications are rare and generally of poor quality), (b) focusing on LMICs in the EMR, (c) published after 2006 (to capture the most recent evidence), (d) focusing on health workforce in rural and remote areas (most had a primary healthcare focus), (e) manuscripts focusing on the retention of doctors, nurses, midwives and/or community health workers (literature is quite rare on other types of health workers), and (f) articles proposing actionable interventions for the retention of HRH in rural and remote areas.
The final review included literature discussing health workforce distribution, recruitment, retention, and HRH management, whether in primary health centers, or more broadly in rural and remote areas, in select LMICs in the EMR. Literature on dentists, pharmacists, and allied health workers were removed from final review due to limited information from the Region. To maintain the focus of this review, articles proposing aspirational and noncontextual recommendations, instead of specific actionable interventions to address rural retention, were removed from the final review.
In hopes of addressing the maldistributions and challenges of HRH recruitment and retention in rural and remote areas, WHO's “Global Recommendations For Increasing Access To Health Workers In Remote And Rural Areas Through Improved Retention” served as the analytical framework informing this review. 11 While there are various methods of classifying and understanding factors and interventions affecting rural retention, our findings are organized around the themes of the WHO Global Recommendations. This framework was chosen as due to its rigor as it is peer‐reviewed and published as recommendations by WHO but also for ease of knowledge‐translation as it provide a standardized approach to classify interventions given the diversity of health systems in the Region and globally.
3. RESULTS
The initial review yielded 130 articles related to health workforce retention issues in the LMICs in EMR. A title and abstract review screened out 69 articles and a total of 61 articles went for the full review, of which 40 were excluded as they did not provide evidence or accounts of actional interventions used to address retention in rural and remote areas. The final analysis included 21 articles meeting the inclusion criteria. Interventions were extracted and categorized according to the four types proposed in the WHO Global Recommendations (Figure 2). In general, Educational and Regulatory interventions were referenced most. In terms of the distribution of article by EMR countries, Afghanistan was most mentioned, followed Pakistan, Lebanon, Iran, and Sudan.
Figure 2.

Rural health workforce retention interventions in the LMIC of the EMR categorized by types of strategy. EMR, Eastern Mediterranean Region; LMIC, low‐ and middle‐income country
3.1. Addressing geographic maldistribution in EMR
According to the WHO Global Recommendations, the four main types of strategies that influence health workforce recruitment and retention in rural and remote areas are: education, regulation, financial incentives, and professional support. The findings of this study are categorized by each of the four types of interventions and summarized in Figure 2. A full summary of all the included articles in this review is offered in Table 1.
Table 1.
Interventions used to improve attraction, recruitment, and retention of health workers in rural and remote areas in select low‐ and middle‐income countries in the EMR (based on WHO recommendation) 11
| Countries/Categories | Education | Regulatory | Financial | Personal |
|---|---|---|---|---|
| Examples from the global recommendations 11 |
Students from rural background Health professional schools outside of major cities Clinical rotations in rural areas Curricula that reflects rural health issues Continuous professional development for rural health workers |
Enhanced scope of practice Different types of health workers Compulsory service Subsidized education for return of service |
Appropriate financial incentives |
Better living conditions Safe and supporting working environment Outreach support Career development programs Professional networks Public recognition |
| Afghanistan 14 |
Recruiting students from rural backgrounds (through community nursing [CHN] and midwifery education [CM]) Increasing more training institutes in remote provinces (through IHS/CME) National midwifery accreditation program (tailored to rural deployment) CHW/CHN/CM curricula are based on rural health issues Continuous professional development (refresher courses for CHW) Consideration of preferential admission to meet quotas and rural rotations |
Introducing new cadres Enhancing scope of practice, especially for CHN, CM |
Hardship allowances (double for women in rural care) |
Providing opportunities to male family members Public recognition measures, especially for community health workers, nurses and midwives Afghan midwifery Association (CPD, network) |
| Egypt 24 , 25 , 26 | Opening medical colleges and health institutes in rural areas | Raedat refiyat (RR): Female community health workers recruited and deployed in rural areas | Rural hardship allowances | MOH provides housing, attached to PHCs |
| Iraq 15 , 27 |
Bridge programs/certificates/diplomas in family medicine and nursing Establishing fellowships for CPD Online courses for in‐service training |
Mandatory 1 year service in rural PHC | Incentive bundles |
Improving living standards Creating compounds for health workers next to medical facilities |
| Islamic Republic of Iran 2 , 12 , 22 , 28 |
Opening medical colleges in rural areas Recruiting health workers from rural areas |
Compulsory service special underserved areas (usually in rural areas) Introducing behvarz (community health workers) |
Financial incentives | |
| Jordan 17 , 18 , 29 |
Continuous education (specialization in Family Medicine) Providing some internships in (rural) PHCs MOH initiative for rural medical schools rotations to enhance rural exposure |
Female community health workers recruited and deployed in rural areas (only in the South) | Rural hardship allowances | |
| Lebanon 2 , 16 , 17 , 30 | Targeted scholarships for rural background students, bonding return of service agreements |
Introducing a rural nurse cadre Improved supervisor support through preceptors |
Financial incentives (eg, bonuses, raises, tuition reimbursements) Rural reimbursement policies exist (but not effective or strong enough) |
Professional development through seminars, courses, and access to conferences, professional development Order of nurses (for those working in rural PHCs) Improving work environments and boosting infrastructure (through contracting out PHCs) |
| Pakistan 21 , 28 , 31 |
Changes in curricula Increasing number of training institutions in rural areas |
Introducing new cadres, such as lady health workers and lady health visitors, community midwives recruited from, trained and deployed to all districts Training male CHW |
Fringe benefits, housing facilities and career development opportunities (specifically for doctors) | |
| Somalia 20 , 28 |
Public‐private partnerships in training institutions to increase quality and access Course standardization and changes in curricula Expanding health training institutes in remote areas |
Introducing and training midlevel professionals such as midwives, nurses, sanitarians, allied health workers, lab techs Introducing CHWs, especially female health workers and community midwives 1 year mandatory national service post‐graduation (but poor implementation) |
Creating a multisource fund from UN donors to support CHWs Harmonizing salary remunerations for public health workers, Introducing standardized regular living salaries and special hardship allowances for rural, remote and insecure areas |
Introducing better gender‐policies Improving career development policies Introducing workplace safety and security measures Increasing available technologies and equipment Providing recognition and awards Establishing regulatory health professional councils and associations for licensing, networking, credentialing of new cadres |
| Sudan 13 , 32 , 33 | Increasing number of training institutions in rural areas |
Establishing law enforcement units in health facilities to ensure policy compliance Compulsory year in PHC (but poor enforcement) Introducing new cadres, recruiting and deploying lower cadres (nurses, med assistant and midwives) in rural areas |
Financial incentives Scholarships |
Upgrading PHC infrastructure and facilities Fringes, rural allowances, (such as health insurance, car ownership), housing subsidies Better gender‐policies to ensure female retention in rural areas |
Abbreviations: EMR, Eastern Mediterranean Region; PHCs, primary healthcare centers.
3.1.1. Interventions focused on education
Global literature revealed that targeted recruitment strategies from rural areas were more effective in enhancing rural retention. This is because rural trained medical and health students are more likely to remain practicing in their respective geographic contexts. 9 , 23 Most LMICs in the EMR have worked on increasing access to educational opportunities for rural students through building educational institutions or establishing pre‐service training programs in rural and remote areas. 12 , 17 , 26 , 34 On the other hand, Lebanon is recruiting rural students through targeted scholarships. 16 In Afghanistan, Pakistan, and Somalia, changes to the curricula have been proposed to improve competence in rural health, whereas Jordan introduced rotations and internships in rural settings to increase exposure. 14 , 18 , 21 Community‐based trainings have also been shown to yield higher retention, and have been implemented in Afghanistan, Sudan and Somalia. 14 , 20 , 32 Finally, with regards to in‐service trainings, Iraq, Jordan, and Somalia created bridging programs and online certifications to enhance Continuous Professional Development for health workers in rural areas. 27 , 29
3.1.2. Interventions focused on health workforce regulation
The shortage of health workers in rural areas, especially in PHCs, have supported the creation of competent rural‐specific health workforce. Task‐shifting, introducing new cadres, and expanding scopes of practice have been commonly implemented strategies in many resource‐constraint settings (especially in communities facing critical shortages and maldistribution and in post‐conflict settings). 8 , 9 , 10 , 35 Iran's 91 000 Beharvz and Pakistan's 100 000 Lady Health Workers are the first point of contact with their countries' respective rural primary health system; those community health workers are recruited from and deployed in rural areas, and are employed by MOH to provide basic health services and public health education in remote areas. 17 , 22 , 28 Afghanistan, Egypt, Jordan, Pakistan, Somalia, and Sudan have focused specifically on upscaling female community health workers (including community midwives) in hopes of addressing issues of culture‐competence, mobility, and accessibility of women in rural and remote areas. 14 , 20 , 28 , 32
Many countries in the EMR have introduced at least a 1‐year mandatory service in rural PHCs (eg, Iraq, Iran, Egypt, Sudan, and Somalia), however, it is difficult to monitor the implementation of this policy. 12 , 28 , 31 , 32 Weak governance and poor regulation have resulted in a lack of enforcement of these strategies in the Region. The lack of experience of fresh graduates also exacerbates already low motivation and attraction to work in rural PHCs and contributes to lowering retention. 8
Due to the conservative culture in the Region, especially in rural areas, having an available, mobile, and accessible gender‐balanced workforce is essential to ensuring universal health coverage and equitable access to care. To address this, some EMR countries developed focused efforts on increasing the number of female health workers in rural areas, and further ensuring their safety and integration in remote settings. Sudan and Somalia have created specific targets in their national plans focusing on gender‐policies to ensure female health worker retention, whereas Afghanistan has used a family‐based approach, encouraging and assisting the relocation of family members to these remote villages and health facilities. 14 , 20 , 32
3.1.3. Interventions focused on financial incentives
Egypt, Lebanon, Pakistan, and Sudan have offered fringe benefits like housing subsidies, health insurance, car ownership, or tuition reimbursements. 21 , 25 , 30 In Iran, over 75% of physicians considered income as a major motivating factor in rural retention, even physicians with rural backgrounds were more likely to remain in urban areas due to the significant income differences and opportunities in the urban and private sectors. 12 , 22 Loan repayment schemes, higher salaries and rural hardship allowances have been implemented regionally as a method to increase rural retention. 8 , 10 , 23
3.1.4. Interventions focused on personal and professional factors
Some EMR countries have attempted to improve the standard of living for health workers in rural and remote areas by upgrading the primary health centers' infrastructure, as seen in both Egypt and Iraq. 24 , 27 Lebanon, Afghanistan, and Pakistan have opted to contract‐out their PHCs in hopes of improving quality and efficiency, decreasing rural health workers workload and increasing workforce retention. 14 , 16 Creating professional networks specific to rural health workers (as by the Order of Nurses in Lebanon) and integrating community health professionals into their respective networks (such as the community midwives to the Afghan Midwifery Association), has helped in reducing professional isolation. Outreach activities such as telehealth and mobile clinics have been used to reduce professional isolation and increase connection and access, as seen widely in Africa, and regionally in Syria, Morocco, and Afghanistan. 36
3.2. Barriers to rural workforce retention in the EMR
While our literature search reported a variety of interventions aiming at enhancing the retention of health workers in rural and remote areas in the EMR, we have also unearthed a number of factors opposing these interventions and diluting their success. For example, the financial incentives for the rural retention of health workers are eclipsed by the competition with private urban hospitals especially in high‐income countries (whether in the GCC and the West). One study conducted with Lebanese nurses reported that 35% found that better job opportunities outside the country as a major reason to quit the job at rural PHC, only preceded by poor salaries at 55%. 17 Another study in Iraq indicated that one fourth of doctors immigrated immediately to the West following graduation, whereas physicians from Sudan and Pakistan have been known to migrate in cohorts to the Gulf, further exacerbating the shortage. 31 , 33 Additionally, in many post‐conflict countries, rural and remote health facilities are managed and financed by international donors and contracted NGOs resulting in unstandardized salaries and unfair remuneration, which may reduce motivation to stay in rural areas.
Furthermore, the lack of regulation, poor leadership and corruption remain top factors affecting job satisfaction and rural retention in some EMR LMICs. In Morocco, Iraq, Iran, and Egypt, moonlighting was reported as a top challenge related to health workforce management, where many physicians working in public rural clinics also run private clinics to make sufficient salaries. 12 , 15 , 25 , 36 Corrupt managerial practices in recruitment, transfers and promotions were listed as key demotivators. 26 , 29 In Egypt, over 70% of Egyptian physicians agree on the presence of bias in health workforce recruitment at primary, secondary and private health facilities. 26 Unfair treatment and lack of support from supervisors were cited as the most significant de‐motivator in a study in Iran, followed by poor management and lack of recognition. 22 Lack of respect and recognition, feeling underutilized and undervalued, were ubiquitously cited (especially for nurses) in the available regional literature; include: Morocco, Jordan, Iraq, Iran, and Lebanon. 29 , 30 , 36
Finally, security and gender‐related factors were two region‐specific demotivators for rural recruitment and retention that surfaced in the literature. Security of health workers is a major issue in the EMR as 86% of health workers injured globally were reported from the Region. 1 In Syria, 70% of the workforce had fled the country due to violence, and in one area under‐siege, up to 90% of the medical staff relocated. 7 In Afghanistan, Pakistan, and Somalia, gender‐related security issues deter many female health professionals from taking posts in insecure remote areas. 20 , 31 , 34 In addition to safety, regional literature indicated that it is more difficult for female health workers to relocate from urban settings to rural posts since the difficult commutes to remote locations may take away time from parenting. 24 , 31
4. DISCUSSION
Many LMICs in the EMR have introduced interventions to address health workforce shortages and geographic maldistribution and improve retention in rural and remote areas (Figure 2 and Table 1). While most EMR countries know the causes for poor retention in rural areas, and many have policies in place to address them, the main challenge relates to the implementation and evaluation of such interventions and policies.
4.1. Implementation of interventions by types and implications for policy
Of these four categories of interventions, educational and regulatory interventions are available, accessible and acceptable options that have been implemented in other resource‐limited contexts, as they offer some flexibility and short‐term solutions. 37 Financial incentives, on the other hand, are difficult to implement in the EMR due to poverty, competition from the private sector, and donor‐dependency. 4 These two types of interventions have been introduced to address geographic maldistributions of health workers in other developing countries in Asia including the Philippines, Thailand, Vietnam, and China, and numerous countries in sub‐Saharan Africa like Mozambique and DR Congo; however, most of these countries continue to face health and workforce disparities in underserved areas, indicating further evaluations of these policies. 9 , 11 , 19 While financial incentives are considered one of the leading push factors in both international and urban migration, it is contested that professional and social factors have a greater impact. 2 , 9 , 12
While most factors affecting health worker attraction and retention in rural areas are related to “professional and personal support,” these types of strategies are the most difficult to control as they relate to socio‐economic and political forces. For example, changing perspectives (of doctors and patients) to increase respect for other cadres, combatting corruption, nepotism, and patriarchy, or increasing gender‐inclusivity require profound and slow cultural shifts which often cannot be addressed solely through policies. 16 , 24 , 36 Insecurity in rural post‐conflict areas, also must be addressed but are usually outside a policy‐maker's control.
Our review revealed that various countries in the EMR region have implemented initiatives, with varying degrees of success, across one or more of the WHO framework four categories. Most countries in the EMR prioritize one or two types of strategies with few countries that have a comprehensive approach that covers the four categories. Policy makers should consider bundling of the four categories of interventions, in accordance with local context, in order improve retention of health workers in rural areas. 11
The global literature recommends the implementation of a bundle of interventions to address critical shortage and rural retention, reinforcing that a “one‐size‐fits‐all” health workforce retention strategy is unlikely to succeed. 8 For example, the bundling of both financial and nonfinancial incentives has been effective among rural Peruvian nurses and midwives where the most attractive package included a 75% increase in salary plus scholarship for a specialization, which increased rural job acceptance from 36% to 60%. 35 Another example from Afghanistan, showed that the introduction of interventions across the four categories contributed to increasing rural health workers density from 4.5 health workers per 10 000 (in 2009) to almost 17 health workers per 10 000 (in 2012). 14 Innovative solutions are required by the countries in the EMR as most are facing critical shortage of health workers compounded by geographic maldistributions, poverty, and crisis. Strategies should be made not only to address retention and maldistribution, but also to create cadres that are fit‐for‐rural practice and complementary to post‐conflict settings, that are able to staff recovering health systems to delivery basic health services and UHC.
4.2. Gaps and recommendations
This review is not without its limitations. This review relied on the publicly available data in select LMICs (where adequate literature can be obtained in English). The scope was limited to literature published in English in a Region where Arabic and French are also used languages. Literature was also limited to specific cadres in rural PHC settings. While this review categorizes rural health workforce retention interventions, it could not offer a systematic assessment of listed interventions due to the lack of evaluative studies.
Nonetheless, this review allows the sharing of experiences from the region, offers insights to policy makers highlighting some evidence‐based recommendations for policy and practice, focused on priority areas for research and collaboration.
4.2.1. Limited literature and lack of evaluations studies
Literature from the EMR is sparse, and many global systematic and literature reviews fail to reference the Region, likely due to the lack of detailed examples and case studies. Moreover, the greatest focus in the literature on voluntary migration, especially in LMICs, is on brain‐drain and international expatriation. Furthermore, there is a complete lack of literature documenting effectiveness of interventions used to address rural health workforce shortage. 9 , 23 This is indeed the most significant gap identified from our review of regional literature.
4.2.2. Weak, fragmented, and outdated health workforce databases
Outdated and fragmented data on the geographic distribution of health workers (especially in EMR's middle‐income countries) inhibit capturing the full health workforce information picture. Creating and updating health workforce information systems in the EMR is necessary. Countries should regularly gather disaggregated data, by geographic distribution, gender, cadre, and level of care, and update the information consistently. Indicators measuring retention such as: turnover rates, vacancies, and absenteeism, should be collected and made available at national or regional levels. This requires multistakeholder data collection and validation across ministries of finance, health, interior, information/statistics, education and planning, and the involvement and collaboration of other institutions. Improving health workforce information systems will not only allow opportunities to create evidence‐based policies and recommendations, but will also provide platforms to confirm that policies are being implemented, and will support the evaluation of their effectiveness. 6 , 9 , 10 , 23
4.2.3. Need for a focused research agenda supported by regional collaboration
Further research needs to be produced on the distributions of health workers and the factors affecting urban migration, by cadre, gender, and geographic distribution. Literature related to retention factors for cadres other than doctors and nurses is also needed. Many studies either group together multiple cadres (such as primary‐care physicians and nurses) or focus only one cadre's experience (in most cases, the literature focuses more heavily on physicians). Detailed analyses on the attitudes of different health professionals toward rural deployment is necessary for policymaking and planning. 38 Furthermore, while most regional literature on retention provided recommendations and policies on addressing shortages and geographic maldistributions, few countries have documented which interventions have been implemented and for how long. Investment in implementation and evaluation research in the Region is of utmost necessity to evaluate the effectiveness of health workforce retention strategies. Another recommendation is for high‐income countries/ GCC to extend research support to other countries in the Region, or lead joint/comparative efforts to improve Regional evidence. 2
5. CONCLUSION
The current snapshot on the retention of HRH in rural and remote areas in the EMR identifies opportunities for innovative policies and solutions that ensure health services are being provided to all persons, leaving no‐one behind, particularly those in rural areas. More comprehensive regional evidence must be generated to identify the most effective “bundle of interventions.” Strengthening all aspects of health systems, particularly governance, and increasing political commitment to health workforce are necessary not only to ensure adequate documentation, implementation, and monitoring of policies, but also to improve rural retention, health workforce shortages, and overall service delivery to achieve UHC.
FUNDING
The authors did not receive specific funding for this work.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
AUTHOR CONTRIBUTIONS
Conceptualization: Merette Khalil
Data curation: Merette Khalil
Formal analysis: Merette Khalil, Mohamad Alameddine
Methodology: Merette Khalil
Validation: Mohamad Alameddine
Visualization: Mohamad Alameddine
Writing ‐ original draft preparation: Merette Khalil, Mohamad Alameddine
Writing ‐ review and editing: Merette Khalil, Mohamad Alameddine
All authors have read and approved the final version of the manuscript.
Mohamad Alameddine had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
TRANSPARENCY STATEMENT
The authors, Merette Khalil and Mohamad Alameddine, affirm that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the health workforce development team in WHO's Eastern Mediterranean Regional Office for their support of this research and continued efforts in addressing health workforce challenges in the Region.
Khalil M, Alameddine M. Recruitment and retention strategies, policies, and their barriers: A narrative review in the Eastern Mediterranean Region. Health Sci Rep. 2020;3:e192 10.1002/hsr2.192
DATA AVAILABILITY STATEMENT
All the data reported in this manuscript are derived from public domain sources including PubMed and Google Scholar.
REFERENCES
- 1. Mahjour J, Rashidian A, Atta H, et al. Promote health, keep the world safe, serve the vulnerable in the eastern Mediterranean region. East Mediterr Health J. 2018;24(4):323‐324. [DOI] [PubMed] [Google Scholar]
- 2. Saleh S, Alameddine M, Mourad Y, Natafgi N. Quality of care in primary health care settings in the eastern Mediterranean region: a systematic review of the literature. Int J Qual Health Care. 2015;27(2):79‐88. [DOI] [PubMed] [Google Scholar]
- 3. WHO . 2016. “Global Strategy on Human Resources for Health: Workforce 2030. Geneva, Switzerland: .” WHO; http://www.who.int/hrh/resources/globstrathrh-2030/en/. Accessed February 1, 2020. [Google Scholar]
- 4. Zurn P, Vujicic M, Lemière C, et al. A technical framework for costing health workforce retention schemes in remote and rural areas. Hum Resour Health. 2011;9(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gedik G, Oweis A, Khalil M. Family practice multidisciplinary teams Family Practice in the Eastern Mediterranean Region: Universal Health Coverage and Quality Primary Care. WONCA Family Medicine. Vol 1 Baton Rouge, FL, USA: CRC Press; 2019. [Google Scholar]
- 6. Willis‐Shattuck M, Bidwell P, Thomas S, Wyness L, Blaauw D, Ditlopo P. Motivation and retention of health workers in developing countries: a systematic review. BMC Health Serv Res. 2008;8(1):247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fouad FM, Sparrow A, Tarakji A, et al. Health workers and the weaponisation of health Care in Syria: a preliminary inquiry for the lancet‐American University of Beirut Commission on Syria. Lancet. 2017;390(10111):2516‐2526. [DOI] [PubMed] [Google Scholar]
- 8. Araujo, Edson , and Maeda Akiko. How to Recruit and Retain Health Workers in Rural and Remote Areas in Developing Countries: A Guidance Note. Washington, DC, USA: The International Bank for Reconstruction and Development/The World Bank; 2013. [Google Scholar]
- 9. Henderson LN, Tulloch J. Incentives for retaining and motivating health workers in Pacific and Asian countries. Hum Resour Health. 2008;6(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mbemba GIC, Gagnon M‐P, Hamelin‐Brabant L. Factors influencing recruitment and retention of healthcare workers in rural and remote areas in developed and developing countries: an overview. J Public Health Afr. 2016;7(2):61‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. WHO . 2010. “Increasing Access to Health Workers in Remote and Rural Areas through Improved Retention”. Geneva, Switzerland: WHO; https://www.who.int/hrh/retention/guidelines/en/. Accessed February 1, 2020. [PubMed] [Google Scholar]
- 12. Daneshkohan A, Zarei E, Mansouri T, Maajani K, Ghasemi MS, Rezaeian M. Factors affecting job motivation among health workers: a study from Iran. Global J Health Sci. 2015;7(3):153‐160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Government of Sudan Federal Ministry of Health: Directorate General of Human Resources for Health Development. National Human Resource for Health Strategic Plan 2012‐2016; 2011.
- 14. Safi N, Naeem A, Khalil M, Anwari P, Gedik G. Addressing health workforce shortages and maldistribution in Afghanistan. East Mediterr Health J. 2018;24:951‐958. [DOI] [PubMed] [Google Scholar]
- 15. Shukor AR, Klazinga NS, Kringos DS. Primary care in an unstable security, humanitarian, economic and political context: the Kurdistan region of Iraq. BMC Health Serv Res. 2017;17(1):592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Alameddine M, Saleh S, El‐Jardali F, Dimassi H, Mourad Y. The retention of health human resources in primary healthcare centers in Lebanon: a national survey. BMC Health Serv Res. 2012;12(1):419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. El‐Jardali F, Murray SF, Dimassi H, et al. Intention to stay of nurses in current posts in difficult‐to‐staff areas of Yemen, Jordan, Lebanon and Qatar: a cross‐sectional study. Int J Nurs Stud. 2013;50(11):1481‐1494. [DOI] [PubMed] [Google Scholar]
- 18. Khatatbeh M, Alkhaldi S. Factors impact on turnover of Jordanian rural physicians. Int J Sci Appl Res. 2016;3:1‐9. [Google Scholar]
- 19. Lemiere C, Herbst C, Jahanshahi N, Smith E, Souca A. Reducing Geographical Imbalances of Health Workers in Sub‐Saharan Africa. Washington DC, USA: The World Bank; 2010. [Google Scholar]
- 20. Federal Government of Somali Republic Ministry of Human Development and Public Services: Directorate of Health. Health Sector Strategic Plan 2013‐2016; 2012.
- 21. Suhail A, Azhar A. Managing human resources in public health care system in South Asia: case study of Pakistan. South Asian J Hum Resour Manag. 2016;3(1):75‐83. [Google Scholar]
- 22. Tabrizi JS, Pourasghar F, Nikjoo RG. Status of Iran's primary health care system in terms of health systems control knobs: a review article. Iran J Public Health. 2017;46(9):1156‐1166. [PMC free article] [PubMed] [Google Scholar]
- 23. Lehmann U, Dieleman M, Martineau T. Staffing remote rural areas in middle‐ and low‐income countries: a literature review of attraction and retention. BMC Health Serv Res. 2008;8(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Farahat FM. Challenges facing female physicians in Egypt. Arch Environ Occup Health. 2009;64(2):121‐128. [DOI] [PubMed] [Google Scholar]
- 25. Ga AE‐A. Health coverage for workers in Egypt. Egypt J Occup Med. 2014;38(1):23‐42. [Google Scholar]
- 26. Elden K, Nesreen HIR, Wahby G. Improving health system in Egypt: perspectives of physicians. Egypt J Commun Med. 2016;34(1):45‐58. [Google Scholar]
- 27. Al Hilfi TK, Lafta R, Burnham G. Health services in Iraq. Lancet. 2013;381(9870):939‐948. [DOI] [PubMed] [Google Scholar]
- 28. El Feky S. Community Health Workers: A Strategy to Ensure Access to Primary Health Care Services. Cairo, Egypt: World Health Organization. Regional Office for the Eastern Mediterranean; 2016. [Google Scholar]
- 29. Mrayyan MT. Jordanian nurses' job satisfaction and intent to stay: comparing teaching and non‐teaching hospitals. J Prof Nurs. 2007;23(3):125‐136. [DOI] [PubMed] [Google Scholar]
- 30. Alameddine M, Khodr H, Mourad Y, Yassoub R, Abi Ramia J. Upscaling the recruitment and retention of human resources for health at primary healthcare centres in Lebanon: a qualitative study. Health Soc Care Community. 2016;24(3):353‐362. [DOI] [PubMed] [Google Scholar]
- 31. Shah SM, Zaidi S, Ahmed J, Rehman SU. Motivation and retention of physicians in primary healthcare facilities: a qualitative study from Abbottabad, Pakistan. Int J Health Policy Manag. 2016;5(8):467‐475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ebrahim E, Ghebreab L, Abdalgfar T, Juni MH. Health care system in Sudan: review and analysis of strength, weakness, opportunity, and threats (SWOT analysis). Sud J Med Sci. 2017;12:133. [Google Scholar]
- 33. Nurelhuda N, Bashir A, El Kogali S, Mustafa M, Kruk M, Abdel Aziz M. Encouraging junior doctors to work in rural Sudan: a discrete choice experiment. East Mediterr Health J. 2018;24(9):838‐845. [DOI] [PubMed] [Google Scholar]
- 34. Mansoor GF, Hill PS, Barss P. Midwifery training in post‐conflict Afghanistan: tensions between educational standards and rural community needs. Health Policy Plan. 2012;27(1):60‐68. [DOI] [PubMed] [Google Scholar]
- 35. Roome E, Raven J, Martineau T. Human resource management in post‐conflict health systems: review of research and knowledge gaps. Confl Heal. 2014;8(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Semlali H. Positive Practice Environments in Morocco. Global Health Workforce Alliance; IntraHealth; 2010. https://www.hrhresourcecenter.org/node/3391.html. Accessed February 1, 2020.
- 37. Goel S, Angeli F, Bhatnagar N, Singla N, Grover M, Maarse H. Retaining health workforce in rural and underserved areas of India: what works and what doesn't? A critical interpretative synthesis. Natl Med J India. 2016;29(4):212‐218. [PubMed] [Google Scholar]
- 38. Castro Lopes S, Guerra‐Arias M, Buchan J, Pozo‐Martin F, Nove A. A rapid review of the rate of attrition from the health workforce. Hum Resour Health. 2017;15(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data reported in this manuscript are derived from public domain sources including PubMed and Google Scholar.


