Abstract
Mobile technology provides a unique opportunity to expand access to evidence-based interventions. The objective of this study was to provide an update regarding use of technology in people with serious mental illness (SMI). In 2017, 403 people in treatment for SMI were surveyed. Technology use was common: 65.8% used a smartphone, 53.6% used the Internet on a computer or tablet in the past six months, and over two thirds (67.9%) used social media. Rates of technology and Facebook use were similar to rates among low-income Americans. Approximately three quarters were willing to use a device to access interventions for stress, health and mental health. Younger adults were more likely to use most forms of technology and social media compared to older adults, but willingness to try technology-delivered interventions did not vary by age. This survey supports the rationale for ongoing development and testing of digital interventions for people with SMI.
Introduction
Internet and mobile technologies provide a unique opportunity to deliver cost-effective interventions with on-demand access to support health, mental health, and wellness. Based on data from the Pew Research Center, the vast majority (89%) of American adults use the Internet, 95% own cell phones, 77% own smartphones, and most adults who access the Internet use social media sites such as Facebook® to connect with others (2018a, 2018b, 2018c). Overall, young people have the highest rates of mobile technology usage.
Although people in lower income brackets are making gains in device ownership and Internet access, they are still less likely to own smartphones and computers compared to those with higher incomes (Anderson, 2017). One important low-income group is people with serious mental illnesses (SMI; including disabling schizophrenia, bipolar disorder, and mood and anxiety disorders)(Kessler, Chiu, Demler, Merikangas, & Walters, 2005; Kessler et al., 2008). Research shows that this group can successfully engage in and benefit from technology-based interventions (Ben-Zeev et al., 2018), and individuals with SMI, like others, may naturally seek information and tools on the Internet (Sandoval, Torous, & Keshavan, 2017). While research on mobile device ownership and Internet use among adults with SMI has been increasing (Ben-Zeev, Davis, Kaiser, Krzsos, & Drake, 2013; Depp et al., 2010; Firth et al., 2015; Firth & Torous, 2015; Miller, Stewart, Schrimsher, Peeples, & Buckley, 2015), this group generally remains economically disadvantaged, thus it is not yet clear whether the “digital divide” has closed for people with SMI. In order for digital interventions to be feasible and scalable for people with SMI, the majority must have access to Internet-enabled devices, thus updated information is needed to understand whether and how individuals with SMI access and use smartphones, computers, and social media. The objective of this study was to provide an update regarding use of technology in people with SMI compared to other low income Americans, as well as their willingness to participate in interventions delivered by devices. We hypothesized that, among participants with SMI, technology use would be greater among young age groups compared to older age groups, and those with mood and anxiety disorder diagnoses compared to schizophrenia diagnosis.
Methods:
In the fall of 2017, a convenience sample of 403 people in treatment for serious mental illness SMI) at four community mental health centers in three U.S. states (two in New Hampshire, n=206; one in Rhode Island, n=86; and one in Michigan, n=111) were recruited via posters in community mental health center waiting rooms and by invitation from research staff. Participants completed an annonymous questionnaire including 21 questions about demographics, access to and use of technology, use of the Internet and social media, and willingness to try interventions delivered via cell phone or computer. Participants who wished to provide their contact information were included in a raffle for a gift with a value approximating $100. This study was completed in accordance with Good Clinical Practices and was deemed exempt from review by the State of New Hampshire Department of Health and Human Services Committee for the Protection of Human Subjects. Published information on Internet and technology use among U.S. low income respondents was obtained from the Pew survey website, published February 5, 2018, and downloaded on March 19, 2018.
Descriptive statistics were used to convey participant characteristics. Univariate logistic regression models were used to evaluate whether gender, age, diagnosis, and geographic location (state) were significantly associated with technology usage in participants with SMI. Multivariate logistic regression models were used to evaluate whether age group predicted technology use while adjusting for gender, diagnosis group and geographic location. Proportions using technology in this SMI survey sample and in the Pew U.S. national survey (Annonymous, 2018a, 2018b, 2018c) were visually displayed. Data were analyzed using IBM SPSS software, Version 25.
Results:
The study group included 403 survey respondents receiving services for SMI in community mental health clinics. As shown in Table 1, about half of the group (207; 51.4%) was female, with a mean age of 44.4 (SD=13.1) years. Over a third of the group (149; 38.0%) self-reported diagnoses of schizophrenia spectrum disorder, 92 (22.8%) reported bipolar disorder, 77 (19.1%) reported major depressive disorders (MDD), and 74 (18.4%) reported anxiety or another disorder. A small proportion (11; 2.7%) did not report a mental health diagnosis.
Table 1:
Characteristics and technology use among 403 adults with serious mental illness
| Demographics | ||
|---|---|---|
| Mean | SD | |
| Age | 44.4 | 13.1 |
| N | % | |
| Female gender | 205 | 51.4 |
| Diagnosis | ||
| Schizophrenia Spectrum | 149 | 37.0% |
| Bipolar | 92 | 22.8% |
| Major Depression | 77 | 19.1% |
| Anxiety/ Other | 74 | 18.4% |
| No diagnosis reported | 11 | 2.7% |
| Technology variables | N | % |
| Device type and place | ||
| Cell Phone | 357 | 88.6% |
| Smart phone | 265 | 65.8% |
| Used Internet on computer/tablet past 6 | ||
| months | 216 | 53.6% |
| Computer/tablet at home | 161 | 40.0% |
| Computer/tablet somewhere else | 123 | 30.5% |
| Friend/family | 49 | 12.2% |
| Library | 89 | 22.1% |
| Peer support center | 12 | 3.0% |
| Mental health center | 11 | 2.7% |
| Social media | ||
| 271 | 67.9% | |
| 67 | 16.8% | |
| Snapchat | 54 | 13.5% |
| 42 | 10.5% | |
| Other | 23 | 5.8% |
| Willing to try intervention on device | ||
| Intervention for health | 293 | 72.7% |
| Intervention for stress | 292 | 72.5% |
| Intervention for mental health | 306 | 75.9% |
Technology use was common (see Table 1): 88.6% (n=357) reported using a mobile phone, 65.8% (n=265) reported using a smartphone, and 53.6% (n=216) reported using the Internet on a computer or tablet in the past six months (40.0% at home, 30.5% at another location). Additionally, over two thirds (67.9%) of the group used social media, and almost three quarters of respondents with SMI were interested and willing to access interventions on an electronic device for stress (72.5%, n=292), for health (72.7%, n=293) and for mental health (75.9%, n= 306).
Technology use by age group is shown in Table 2. Univariate analyses showed that younger respondents with SMI were significantly more likely to use most forms of technology than adults with SMI in older age groups. Adults under 50 years of age were more likely to use a smartphone than adults over 50 (X2 = 59.2, df=3, p<.001), and young adults under 30 years old were more likely to use the Internet via computer/tablet at home than people in the other age groups (X2=35.3, df=3, p<.001. The younger age groups were more likely to be willing to use technology for interventions for mental health than those over 65 years of age (X2 9.5, df-=3, p=.023).
Table 2:
Characteristics and technology use among 403 adults with serious mental illness (SMI) by age group
| Characteristic | Age 18–29 | Age 30–49 | Age 50–64 | Age 65+ | ||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |
| Total | 65 | 16.1% | 174 | 43.2% | 137 | 34.0% | 20 | 5.0% |
| Female gender | 31 | 47.0% | 97 | 56.7% | 66 | 48.2% | 11 | 55.0% |
| Diagnosis | ||||||||
| Schizophrenia Spectrum | 22 | 33.8% | 59 | 34.5% | 58 | 43.3% | 9 | 47.4% |
| Bipolar | 17 | 26.2% | 43 | 25.1% | 27 | 20.1% | 4 | 21.1% |
| Major Depression | 9 | 13.8% | 31 | 18.1% | 31 | 23.1% | 5 | 26.3% |
| Anxiety/ Other | 17 | 26.2% | 38 | 22.2% | 18 | 13.4% | 1 | 5.3% |
| Device type and place | ||||||||
| Cell Phone | 59 | 90.8% | 161 | 92.5% | 117 | 85.4% | 16 | 80.0% |
| Smart phone*** | 53 | 82.8% | 138 | 79.3% | 67 | 49.3% | 6 | 30.0% |
| Computer/tablet at home*** | 45 | 68.2 % | 74 | 42.8 % | 34 | 24.8 % | 8 | 40.0% |
| Computer/tablet elsewhere | 24 | 36.4 % | 62 | 36.0 | 33 | 23.9% | 4 | 20.0% |
| Friend/family | 9 | 13.6% | 14 | 8.0% | 7 | 5.1% | 1 | 5.0% |
| Library | 15 | 22.7 % | 42 | 24.0% | 29 | 21.0% | 2 | 10.0% |
| Peer support center | 2 | 3.0% | 7 | 4.0% | 3 | 2.2% | 0 | 0.0% |
| Social media | ||||||||
| Facebook*** | 60 | 90.9% | 137 | 78.3 % | 66 | 47.8 % | 8 | 40.0% |
| Instagram*** | 22 | 33.3% | 30 | 17.1% | 14 | 10.1 % | 1 | 20.0% |
| Snapchat*** | 22 | 33.3 % | 24 | 13.7 % | 8 | 5.8% | 0 | 0 |
| 13 | 19.7% | 15 | 8.6% | 13 | 9.4% | 1 | 20.0% | |
| Other | 3 | 4.5% | 8 | 4.6% | 9 | 6.5% | 3 | 20.0% |
| Willing to try intervention on device | ||||||||
| for health | 47 | 71.2 % | 131 | 76.6% | 101 | 75.4 % | 11 | 57.9 % |
| for stress | 45 | 70.3 % | 135 | 78.9 % | 97 | 70.8 % | 12 | 60.0% |
| for mental health** | 52 | 78.8% | 140 | 82.4% | 101 | 75.4% | 10 | 52.6% |
= p<.01;
= p < .001
Regarding social media use, over two-thirds of respondents (67.9%; N=271) used Facebook, with use greater in adults under 50 compared to over 50 years of age (X2=57.4, df=3, p<.001. About one sixth (16.8%) of the group used Instagram, with greater use among young adults (X2=19.3, df=3, p<.001), 13.5% of the group used Snapchat, with adults under 50 more likely to use this form of social media (X2=32.3, df=3, p<.0011), and 10.5% (n=42) of the group (19% of young adults) used Twitter (not significantly different between age groups).
In multivariate logistic regressions assessing whether age group predicted technology use, adjusting for gender, diagnosis group and the geographic location (state in which the participant resided), younger age group significantly predicted smartphone use, home computer/tablet Internet use, and willingness to use a mobile program for mental health. Age group was not a predictor of having a cell phone, computer/Internet use at places other than home, and willingness to try a mobile program for stress or physical health.
In the multivariate logistic regressions, diagnosis and location also significant predictors of some types of technology use. Diagnosis category significantly predicted cell phone and smartphone use (anxiety groups greater than schizophrenia group; Wald = 13.6, df=3, p<.01 and Wald=11.1, df=3, p=.01), but not other technology use. State was also a significant predictor in adjusted models predicting use of computer/tablet Internet at places other than home (RI less than MI; Wald 13.1, df=2, p<.01) and willingness to use interventions for stress and health (MI greater than NH; Wald=14.2, df=2, p=.001, Wald = 7.6, df = 2, p=.02, respectively).
As shown in Figure 1, young adults had the highest rates of smartphone use. The proportion of SMI young adults using smartphones was numerically similar to general population young adults, but lower than low-income young adults. All age SMI survey respondents had similar rates of smartphone and Facebook usage overall compared to low-income adults. A numerically lower proportion of SMI participants used computers at home compared to general population Pew survey adults.
Figure 1:
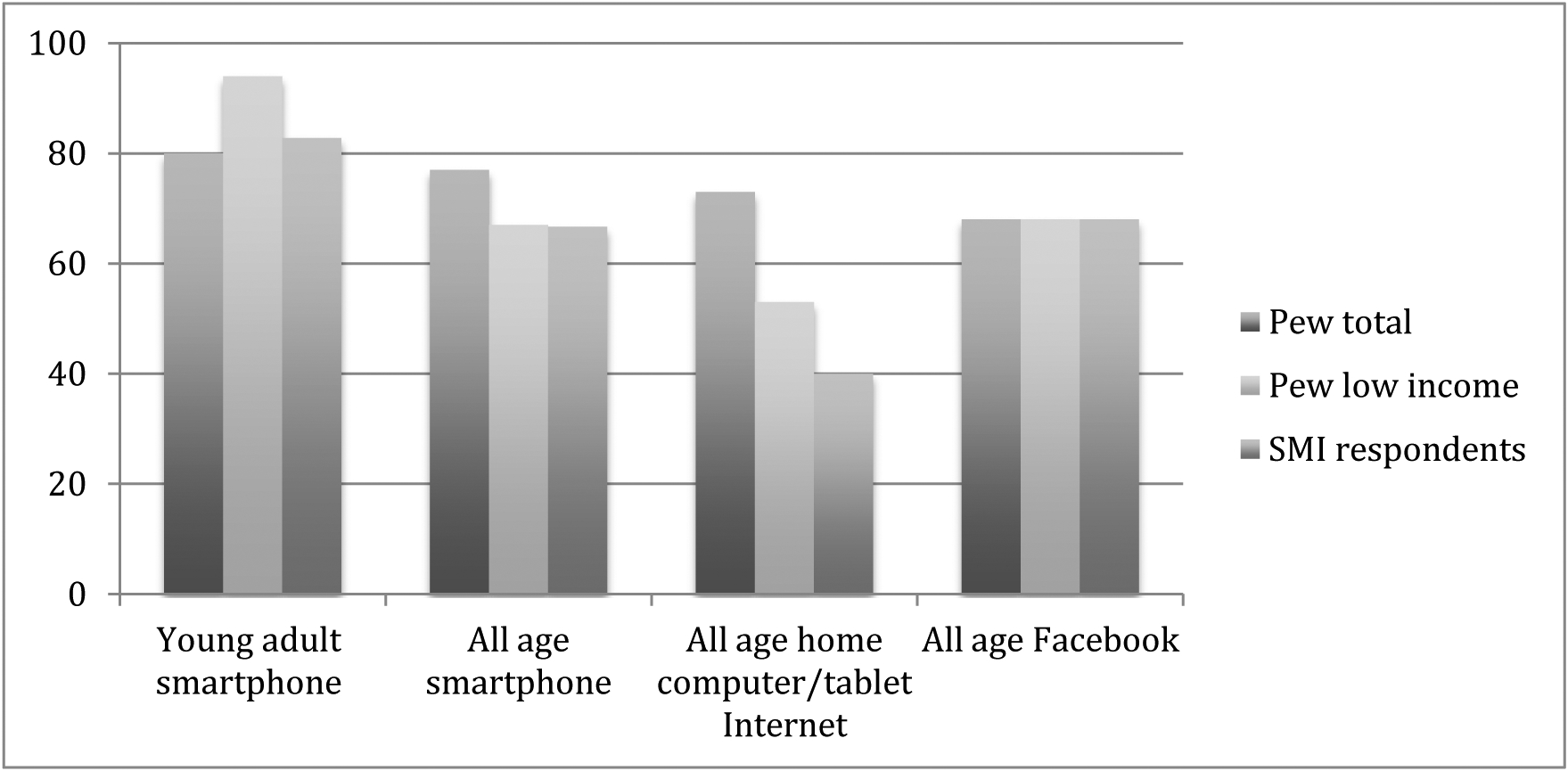
Technology and social media use in people with SMI, U.S. PEW survey all-income, and U.S. PEW survey low-income (less than $30,000/year)
Discussion
In this large, convenience sample of people with SMI receiving mental health services in three states, most reported access to and use of mobile devices, Internet, and social media. Not surprisingly, younger age groups reported the highest rates of use. The proportion of people with SMI using the Internet on mobile devices was comparable to proportions of low-income general Americans reported by the Pew U.S. national survey (2018a, 2018b, 2018c).
Our 2017 survey indicates higher rates of smartphone and computer Internet use compared to prior surveys (e.g. (Ben-Zeev et al., 2013; Firth et al., 2015)). The rise in the use of smartphones is being facilitated by national programs for people with disabilities and low income, such as SafeLink (safelinkwireless.com) or Lifeline with TruConnect (lifeline-free.truconnect.com), as well as the increasing availability of reasonably priced services. Nevertheless, people with schizophrenia, who tend to have the greatest level of disability and the lowest income levels, reported the lowest use of smartphones.
Internet-enabled devices and social media provide a venue to deliver interventions to assist people in managing their chronic health conditions, and this survey indicates that most people with SMI are willing: almost 75% of those completing our survey expressed a willingness to participate in digital interventions for health, mental health, and stress. These data indicating a high level of willingness to use technology to enhance mental health are similar to previous reports (Ben-Zeev et al., 2013), supporting the use of technological tools to expand access to and reach of evidence-based interventions. Technology can deliver science-based interventions with high fidelity, tailored to the user’s needs and preferences, with flexible levels of intensity, and on-demand capacity. Digital interventions can overcome problems with access due to distance, and such interventions have been developed and systematically deployed for mental health treatment in some countries (e.g., Headspace in Australia (Hodges, O’Brien, & McGorry, 2007)). Researchers have already begun to investigate use of devices to deliver interventions to improve management of mental health symptoms (Ben-Zeev et al., 2018; M. F. Brunette et al., 2016; Pratt, Naslund, Wolfe, Santos, & Bartels, 2015), co-occurring addiction (Deady, Mills, Teesson, & Kay-Lambkin, 2016), co-occurring health conditions, such as diabetes (Pratt et al., 2013), smoking cessation (M. F. Brunette et al., 2013; Mary F. Brunette, Ferron, Gottlieb, Devitt, & Rotondi, 2016) and obesity (Aschbrenner, Naslund, & Bartels, 2016; Naslund et al., 2016).
Technology-delivered interventions may compliment in-person interventions, delivering all or parts of evidence-based treatments such as cognitive-behavioral therapy. A growing body of research suggests that, while use of technology tools without facilitation may be minimal (Torous et al., 2017), clinical facilitation promotes their use and efficacy among people with SMI (Ben-Zeev, Drake, & Marsch, 2015), and such interventions may be more cost effective than intensive in-person only interventions (Iribarren, Cato, Falzon, & Stone, 2017).
This study has several important limitations. It provides information from a convenience sample at four community mental health centers in three states within the U.S.A., and therefore may not be representative of all people with SMI in the U.S.A. or in other countries. Diagnoses were self-reported and may be inconsistent with clinical diagnoses, and the survey was completed by a very small number of people with SMI over age 65, thus results among the oldest age group must be interpreted with caution. Nevertheless, survey respondents included participants across a variety of age and diagnostic categories from three states, providing an up-to-date description of technology, Internet and social media use among a broad group of people with SMI.
In conclusion, these survey data suggest that a growing number of people with SMI in the U.S.A. utilize smartphones, computers, and social media, and that the majority are willing to try interventions delivered via these devices to address stress, health and mental health problems. These data support the rationale for ongoing development and testing of digital interventions for people with SMI that could expand access to interventions to improve health and mental health.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of Interest
Author 1 received research support from Alkermes.. Author 2 has received research support from AssurEx, Avanir, Janssen, Novartis, Otsuka, Pfizer, Pine Rest Foundation, Priority Health, Network180, and Vanguard Research Group and serves on an advisory panel for the Vanguard Research Group. The other authors report no conflicts of interest.
References
- Anderson M (2017). Digital divide persists even as lower-income Americans make gains in tech adoption. Retrieved from Washington DC, USA: http://rsr.ch/2nB4eSF [Google Scholar]
- Annonymous. (2018a). Internet/Broadband Fact Sheet. Pew Research Center, Internet & Technology. [Google Scholar]
- Annonymous. (2018b, February 5, 2018). Mobile Fact Sheet. Pew Research Center Internet & Technology. Retrieved from http://www.Pewinternet.org/fact-sheet/mobile/ [Google Scholar]
- Annonymous. (2018c, February 5, 2018). Social Media Fact Sheet. Pew Research Center Internet & Technology. Retrieved from http://www.Pewinternet.org/fact-sheet/social-media/ [Google Scholar]
- Aschbrenner KA, Naslund JA, & Bartels SJ (2016). Technology-Supported Peer-to-Peer Intervention for People With Serious Mental Illness. Psychiatr Serv, 67(8), 928–929. doi: 10.1176/appi.ps.670801 [DOI] [PubMed] [Google Scholar]
- Ben-Zeev D, Brian RM, Jonathan G, Razzano L, Pashka N, Carpenter-Song E, … Scherer EA (2018). Mobile Health (mHealth) Versus Clinic-Based Group Intervention for People With Serious Mental Illness: A Randomized Controlled Trial. Psychiatr Serv, appips201800063. doi: 10.1176/appi.ps.201800063 [DOI] [PubMed] [Google Scholar]
- Ben-Zeev D, Davis KE, Kaiser S, Krzsos I, & Drake RE (2013). Mobile technologies among people with serious mental illness: opportunities for future services. Adm Policy Ment Health, 40(4), 340–343. doi: 10.1007/s10488-012-0424-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zeev D, Drake R, & Marsch L (2015). Clinical technology specialists. Bmj, 350, h945. [DOI] [PubMed] [Google Scholar]
- Brunette MF, Ferron JC, Drake RE, Devitt TS, Geiger PT, McHugo GJ, … Cook JA (2013). Carbon monoxide feedback in a motivational decision support system for nicotine dependence among smokers with severe mental illnesses. J Subst Abuse Treat, 45(4), 319–324. doi: 10.1016/j.jsat.2013.04.005 [DOI] [PubMed] [Google Scholar]
- Brunette MF, Ferron JC, Gottlieb J, Devitt T, & Rotondi A (2016). Development and usability testing of a web-based smoking cessation treatment for smokers with schizophrenia. Internet Interventions, 4, 113–119. doi: 10.1016/j.invent.2016.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunette MF, Rotondi AJ, Ben-Zeev D, Gottlieb JD, Mueser KT, Robinson DG, … Kane JM (2016). Coordinated Technology-Delivered Treatment to Prevent Rehospitalization in Schizophrenia: A Novel Model of Care. Psychiatr Serv, 67(4), 444–447. doi: 10.1176/appi.ps.201500257 [DOI] [PubMed] [Google Scholar]
- Deady M, Mills KL, Teesson M, & Kay-Lambkin F (2016). An Online Intervention for Co-Occurring Depression and Problematic Alcohol Use in Young People: Primary Outcomes From a Randomized Controlled Trial. Journal of Medical Internet Research, 18(3), e71. doi: 10.2196/jmir.5178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depp CA, Mausbach B, Granholm E, Cardenas V, Ben-Zeev D, Patterson TL, … Jeste DV (2010). Mobile interventions for severe mental illness: design and preliminary data from three approaches. J Nerv Ment Dis, 198(10), 715–721. doi: 10.1097/NMD.0b013e3181f49ea3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth J, Cotter J, Torous J, Bucci S, Firth JA, & Yung AR (2015). Mobile Phone Ownership and Endorsement of “mHealth” Among People With Psychosis: A Meta-analysis of Cross-sectional Studies. Schizophr Bull. doi: 10.1093/schbul/sbv132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth J, & Torous J (2015). Smartphone Apps for Schizophrenia: A Systematic Review. JMIR Mhealth Uhealth, 3(4), e102. doi: 10.2196/mhealth.4930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodges CA, O’Brien MS, & McGorry PD (2007). headspace: National Youth Mental Health Foundation: making headway with rural young people and their mental health. Aust J Rural Health, 15(2), 77–80. doi: 10.1111/j.1440-1584.2007.00868.x [DOI] [PubMed] [Google Scholar]
- Iribarren SJ, Cato K, Falzon L, & Stone PW (2017). What is the economic evidence for mHealth? A systematic review of economic evaluations of mHealth solutions. PLoS One, 12(2), e0170581. doi: 10.1371/journal.pone.0170581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, & Walters EE (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 617–627. doi: 10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Heeringa S, Lakoma MD, Petukhova M, Rupp AE, Schoenbaum M, … Zaslavsky AM (2008). Individual and societal effects of mental disorders on earnings in the United States: results from the national comorbidity survey replication. Am J Psychiatry, 165(6), 703–711. doi: 10.1176/appi.ajp.2008.08010126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller BJ, Stewart A, Schrimsher J, Peeples D, & Buckley PF (2015). How connected are people with schizophrenia? Cell phone, computer, email, and social media use. Psychiatry Res, 225(3), 458–463. doi: 10.1016/j.psychres.2014.11.067 [DOI] [PubMed] [Google Scholar]
- Naslund JA, Aschbrenner KA, Scherer EA, McHugo GJ, Marsch LA, & Bartels SJ (2016). Wearable devices and mobile technologies for supporting behavioral weight loss among people with serious mental illness. Psychiatry Res, 244, 139–144. doi: 10.1016/j.psychres.2016.06.056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratt SI, Bartels SJ, Mueser KT, Naslund JA, Wolfe R, Pixley HS, & Josephson L (2013). Feasibility and effectiveness of an automated telehealth intervention to improve illness self-management in people with serious psychiatric and medical disorders. Psychiatr Rehabil J, 36(4), 297–305. doi: 10.1037/prj0000022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratt SI, Naslund JA, Wolfe RS, Santos M, & Bartels SJ (2015). Automated telehealth for managing psychiatric instability in people with serious mental illness. J Ment Health, 24(5), 261–265. doi: 10.3109/09638237.2014.928403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandoval LR, Torous J, & Keshavan MS (2017). Smartphones for Smarter Care? Self-Management in Schizophrenia. Am J Psychiatry, 174(8), 725–728. doi: 10.1176/appi.ajp.2017.16090990 [DOI] [PubMed] [Google Scholar]
- Torous J, Staples P, Slaters L, Adams J, Sandoval L, Onnela JP, & Keshavan M (2017). Characterizing Smartphone Engagement for Schizophrenia: Results of a Naturalist Mobile Health Study. Clin Schizophr Relat Psychoses. doi: 10.3371/csrp.jtps.071317 [DOI] [PubMed] [Google Scholar]


